- 1Singapore Institute for Clinical Sciences (SICS), Agency for Science, Technology and Research (A*STAR), Singapore, Singapore
- 2School of Management and Communication, Republic Polytechnic, Singapore, Singapore
The impact of prenatal maternal mental health on offspring socioemotional development is substantial and enduring. Existing literature primarily focuses on the effects of psychological distress during pregnancy, emphasizing adverse child outcomes. Recent studies, however, highlight the unique impact of positive maternal mental health on child outcomes. To elucidate the differential associations of maternal psychological distress and positive mental health during pregnancy with child outcomes, we conducted a systematic literature search and random-effects meta-analyses on studies investigating the associations of prenatal maternal mental health with child socioemotional development. Our analyses, comprising 74 studies with 321,966 mother-child dyads across 21 countries, revealed significant associations of prenatal psychological distress with both adverse and positive child socioemotional outcomes. Notably, the effect sizes for the association of psychological distress with positive child outcomes were smaller compared to adverse outcomes. Positive prenatal mental health, on the other hand, was significantly associated with positive socioemotional outcomes but not adverse outcomes. This meta-analysis highlights the independence of negative and positive prenatal mental health constructs and their distinct relationships with child socioemotional development. The findings underscore the importance of considering the positive spectrum of maternal mental health and developmental outcomes to enhance our understanding of prenatal influences on child development.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=335227, identifier CRD42022335227.
Introduction
The impact of maternal mental health on child outcomes is of global significance (1, 2). Notably, the annual economic burden of inadequate perinatal mental health in the United Kingdom has been approximated at £8.1 billion (3). Depressive symptoms experienced by mothers during pregnancy are strongly associated with the risk of depression in the offspring (4, 5). Beyond depression, fetal development is intricately shaped by a diverse spectrum of prenatal mental health factors. Furthermore, it is worth noting that the ramifications of prenatal mental health on offspring persist even when accounting for postpartum maternal mental well-being (6, 7).
Nonetheless, it is crucial to recognize that mental health encompasses more than the mere absence of mental disorders. The World Health Organization (8) defines health as the state of “complete physical, mental, and social well-being and not merely the absence of disease or infirmity” (p. 1). Negative and positive mental health, far from being opposing extremes along a single continuum, are discrete constructs characterized by distinct biological correlates, antecedents, and outcomes (9–11). Children grappling with symptoms of mental illness might concurrently exhibit positive mental health marked by favorable psychological attributes (12). Similarly, the absence of mental illness may not necessarily signify a high level of positive mental health or overall mental well-being (13). As such, it becomes imperative to explore both the domains of negative and positive mental health to understand holistically how maternal mental health influences offspring socioemotional development.
Furthermore, a growing body of evidence reveals that the determinants of negative and positive dimensions of child development diverge distinctly. Parental mental health predicted mental ill-health but not well-being, while school connectedness and friendships predicted well-being in children but not poor mental health (14). A recent twin study echoed this divergence, revealing that factors safeguarding individuals from mental illnesses differ substantially from those fostering well-being (15). Adverse early life circumstances may influence negative child outcomes, such as emotional or behavioral difficulties, without extending the same impact to positive well-being (16). Despite emerging publications on this subject [e.g., (17–19)], the potential influence of positive states within maternal mental health remains predominantly overlooked. Therefore, our focus lies in investigating whether maternal psychological distress and positive mental health during pregnancy exert dissimilar effects on the distinct domains (i.e., negative versus positive) of a child's socioemotional development.
Equally pivotal is the consideration of the consistent impact of prenatal maternal mental health. It is unclear whether the strength of the association between prenatal maternal mental health and developmental outcomes in offspring remains uniform across the various stages of development. As children mature, their reliance on parental influence naturally wanes, while the significance of broader sociocultural contexts beyond the confines of home gains prominence (14). In the trajectory of individual growth, peers progressively wield greater influence on socioemotional development, a phenomenon particularly conspicuous during adolescence, characterized by growing independence from parents (20). Adolescents may seek to satisfy their attachment needs through peers rather than parents (21). Consequently, it is plausible that while the influence of prenatal exposure to poor maternal mental health remains noteworthy, its strength could potentially wane. This raises the possibility that the impact of prenatal maternal mental health might vary in accordance with developmental stages, potentially receding in later periods. Alternatively, theoretical models suggest that early life adversity during specific neurodevelopmental periods steers individuals onto persistent trajectories transcending contexts (22–24). Despite its direct relevance to child development theories, this issue, to our knowledge, has yet to undergo systematic examination.
This meta-analysis holds two primary aims. Firstly, we seek to synthesize and analyze the existing body of research that explores connections between prenatal maternal mental health and developmental outcomes in offspring spanning infancy through adolescence (up to 18 years). Secondly, we endeavor to draw a comparative analysis between associations of psychological distress and positive mental health during pregnancy with offspring socioemotional development. Psychological distress includes symptoms of depression, anxiety, and stress (25). Positive mental health encompasses positive affect, satisfaction with life, optimism, and subjective well-being (26–28). Do the impacts of prenatal psychological distress differ from those of positive mental health based on the specific domain of socioemotional development? Additionally, we explore whether the associations between prenatal psychological distress or positive mental health and offspring development demonstrate consistent patterns across varying stages of development.
Methods
Literature search
The protocol of this meta-analysis was pre-registered in PROSPERO (ID = CRD42022335227). We searched for English language, peer-reviewed, longitudinal studies on prenatal maternal mental health and child outcomes in PsycINFO, ScienceDirect, PubMed, and EBSCOhost in June 2022 (see Supplementary Table S1 for details of the search strategy). These databases were chosen for their comprehensive coverage and accessibility to the authors. There was no restriction on date of publication. The search was limited to English language, peer-reviewed publications. The search results were compiled in Endnote and duplicates were removed before screening against the inclusion criteria. Additionally, we manually searched the reference lists of pertinent review articles to identify any relevant studies that might have been missed during the database search. Such studies were subsequently included in our analysis.
Selection process
Articles were screened for: (a) a prospective design that spanned from pregnancy to post-pregnancy, (b) had measures of maternal mental health (e.g., depression, anxiety, positive mental health) during pregnancy, (c) had measures of the child socioemotional development (e.g., externalizing symptoms, prosocial behaviors), and (d) the child was assessed at or below age of 18 years. The inclusion and exclusion criteria followed the SPIDER checklist [(29); Supplementary Table S2].
The articles were first independently screened against the inclusion criteria by title and abstract by two reviewers. Full texts were examined if there were disagreements between the coders or it was unclear if the study was eligible to be included based on its title and abstract. The study was removed if both reviewers agreed that it did not meet the inclusion criteria. In the event of disagreement between the coders, the two coders would discuss and attempt to reach a consensus (0.02%). If disagreement persisted, the decision of the study's eligibility was determined by the first author (DYP).
Data extraction and quality assessment
Data was extracted independently from shortlisted articles using a pre-designed data extraction form. The extracted data included: last name of first author, year of publication, country of study, name of the birth cohort (if applicable), sample size, average age of mothers during pregnancy, average gestational age, age of child during assessment, gender of child, measures of prenatal mental health, measures of child socioemotional development, and the relevant results. The extracted data was double-checked for error by a second reviewer. The developmental stage of the child was derived from the child's age based on Erikson's Psychosocial Developmental Stages. The location of the study was recoded to reflect the continent the study was situated.
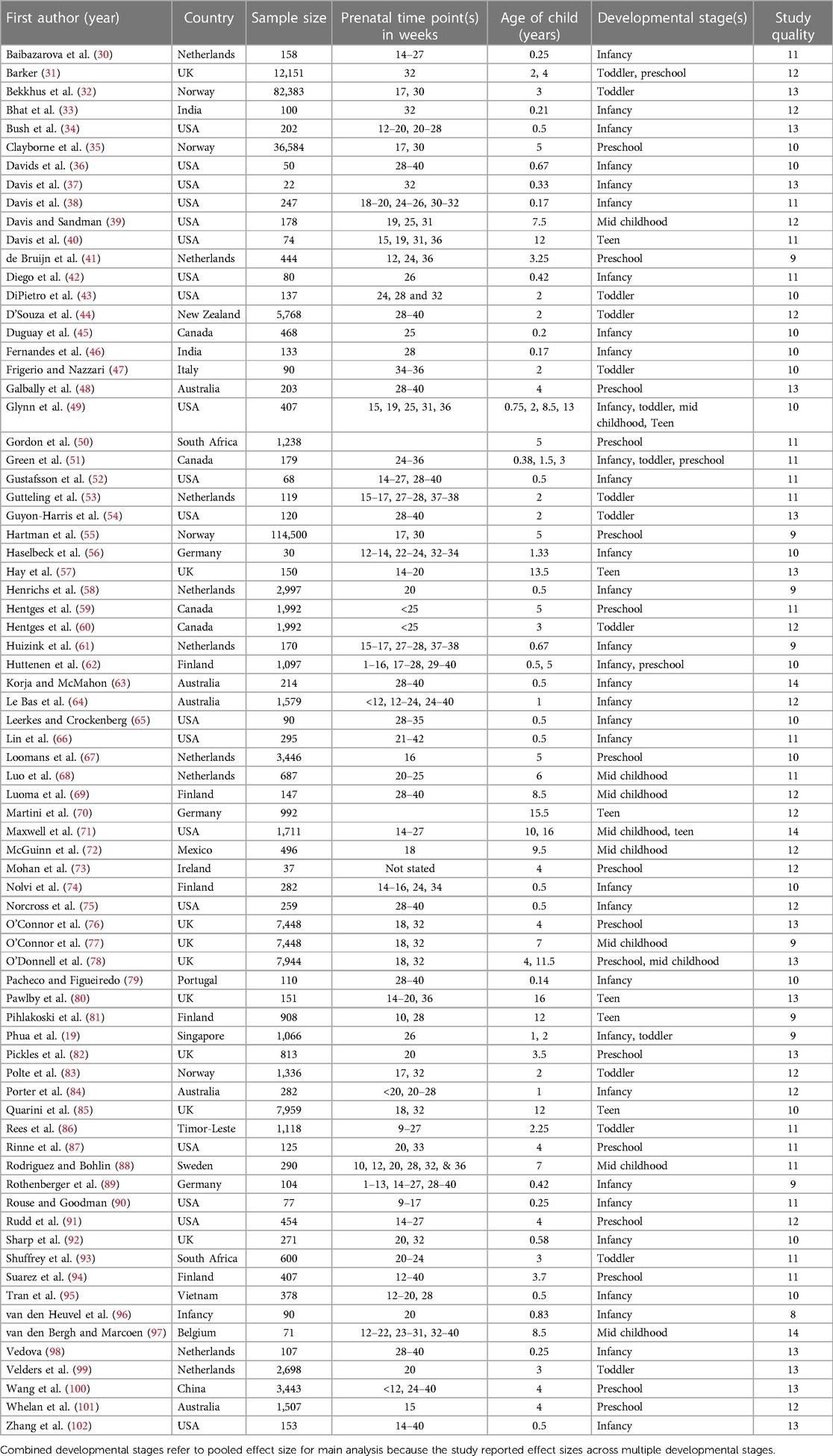
It was possible for multiple effect sizes to be extracted from a study due to different developmental stage, type of prenatal mental health, and type of child outcome. If there were multiple effect sizes of the same domain of prenatal mental health, child outcome, and developmental stage within a single, an average effect size was calculated. If there were studies with overlapping samples (e.g., from the same birth cohort study), the study with more data points (e.g., provided gender-specific effects or effects across multiple developmental stages) or bigger sample size was selected. Studies that did not provide information about the measures, developmental stage of child, or independent associations between prenatal mental health and child outcomes were excluded. Studies that were included in the meta-analysis were assessed on their quality based on the NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (Table 1).
Analysis strategy
Individual effect sizes were transformed to Fisher's Z and analyzed in Comprehensive Meta Analysis v3 software. The results were also transformed back to Pearson r and reported with the z′ scores for ease of interpretation. The effects of negative and positive mental health on negative and positive child outcomes were analyzed separately because the directionality of effects was likely to be different. Prediction intervals for the effect sizes were also calculated if there were at least five studies in the computation of mean effect size (103). Publication bias was assessed by the funnel plot and Egger's regression test. If significant publication bias was detected, the trim-and-fill method was used to test if additional studies would change the results of the meta-analysis.
Results
Study sample
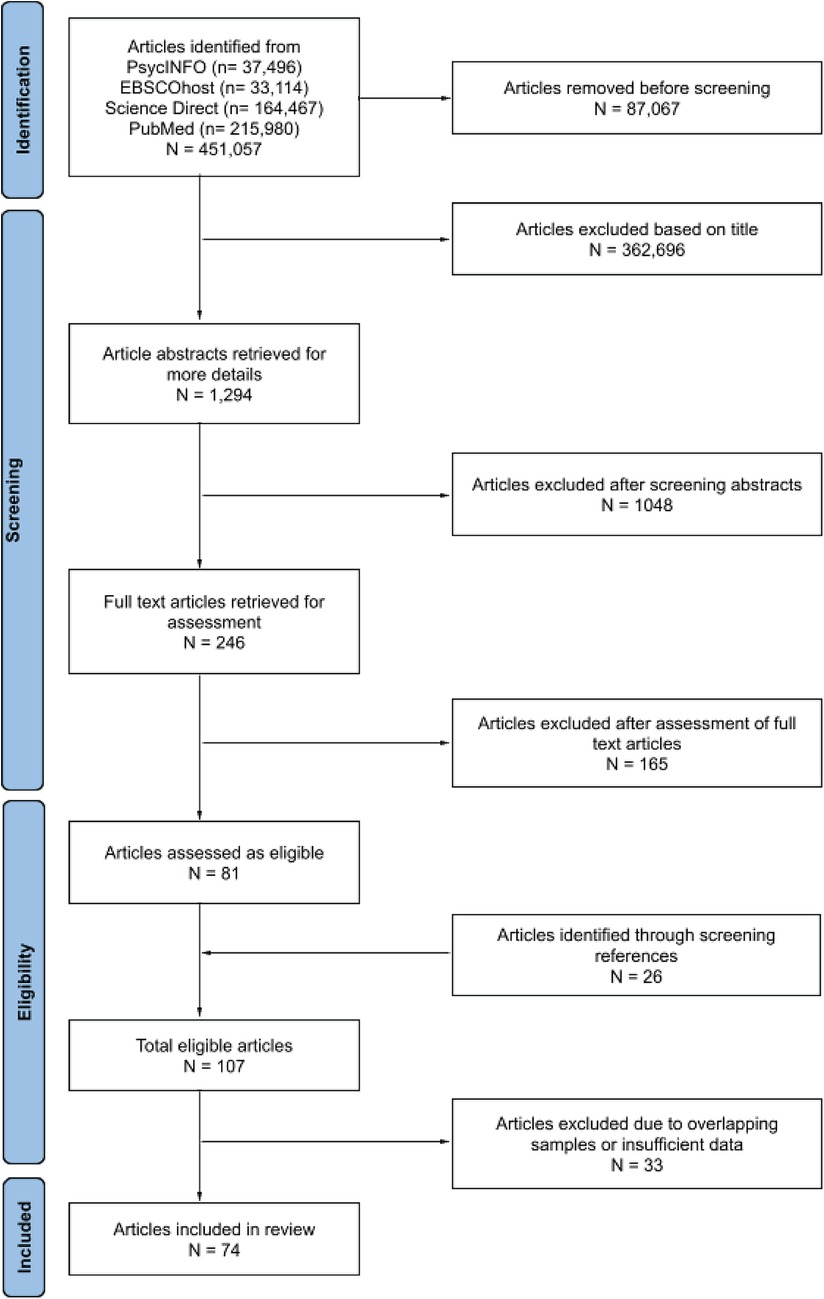
There were 451,057 titles from the initial search on the four databases. Seventy-four studies with 321,966 mother-child dyads were retained for the meta-analysis (see Figure 1 for the PRISMA flowchart). The sample sizes ranged from 22 to 114,500 dyads (mean = 4,353, median = 286; see Table 1 for characteristics of included studies).
Psychological distress on adverse outcomes
Maternal psychological distress (e.g., depression, anxiety, stress) during pregnancy was significantly associated with adverse child outcomes (71 studies: r = 0.161, z′ = 0.162, SEz′ = 0.01, CIz′ 95% = 0.14, 0.18, p < .001; see Figure 2 for forest plot). The adverse child outcomes included measures of emotion dysregulation, aggressive behavior, internalizing and externalizing problems, distress to novelty, negative affect or mood, negative reactivity, depression, anxiety, fearfulness, hyperactivity, inattention, peer or behaviors problems, or socioemotional problems in general. According to the prediction interval, 95% of comparable populations would report a correlation coefficient between 0.159 and 0.299. There was significant heterogeneity in the associations of psychological distress with adverse child outcomes (Q = 790.59, df = 70, p < .001). 91.45% of the observed variance was due to variance in true effects and not due to sampling error. The funnel plot and Egger test did not detect significant publication bias in the results (, t(69) = 0.03, p = .97; Supplementary Figure S1A).
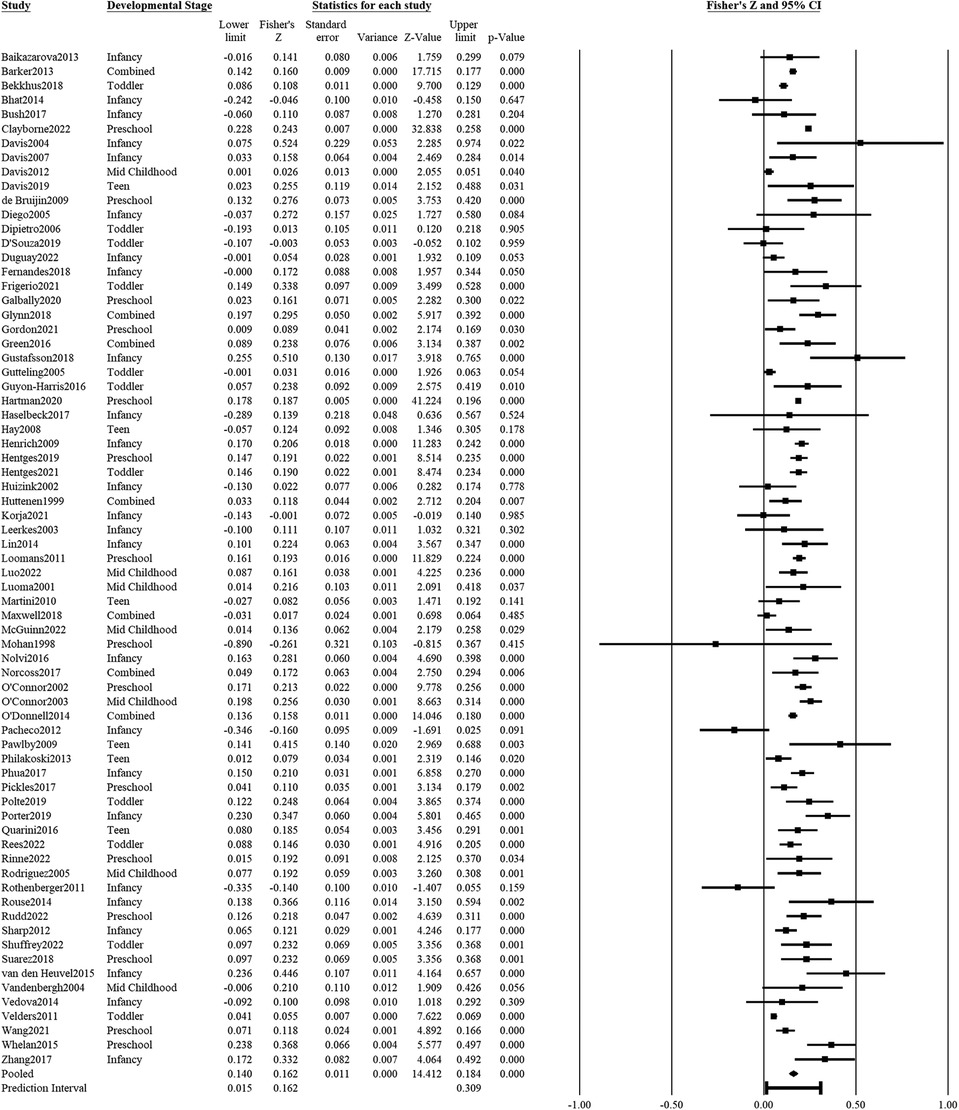
Figure 2. Effect sizes (in Fisher's Z) and forest plots for associations of prenatal maternal psychological distress and negative socioemotional outcome for the child. Combined refers to studies that had participants across multiple developmental stages and the effect sizes were averaged for this analysis.
Ten studies provided gender-specific effect sizes of associations of prenatal psychological distress with adverse child outcomes. There was no significant difference in the effect sizes of the associations of psychological distress with adverse outcomes between male (r = 0.196, z′ = 0.1988, SEz′ = 0.020, CIz′ 95% = 0.160, 0.238) and female (r = 0.196, z′ = 0.199, SEz′ = 0.022, CIz′ 95% = 0.155, 0.243) children (Q < 0.001, df = 1, p = .99). Due to the low number of studies that provided gender-specific data, we were not able to estimate if the gender differences in effect sizes differ across different developmental stages.
Two meta-regression models were estimated to examine the moderating effect of developmental stages and location on the effect sizes of associations of prenatal psychological distress with adverse child outcomes. With infants as the reference group, none of the developmental stages had a significant moderating effect on the size of the associations of psychological distress with either adverse or positive child outcomes (−0.03 < βs < 0.03, ps > .30). Developmental stage accounted for 13% of the total between-study variance. With North America as the reference group, the continent where the data was collected did not significantly moderate the effect of psychological distress on adverse child outcomes (−0.04 < βs < −0.002, ps > .40). Location accounted for almost 0% of the between-study variance of effect sizes.
Psychological distress on positive outcomes
Maternal psychological distress during pregnancy showed a significant and inverse association with positive child outcomes (15 studies: r = z′ = −0.06, SEz′ = 0.02, CI 95% = −0.10, −0.01, p = .018; Figure 3). Positive child outcomes included adaptive skills, prosocial behaviors or relations, positive affect or mood, empathy, excitability, positive reactivity, or general socioemotional competence. The prediction interval for 95% of comparable populations was between r = −0.09 and 0.05. There was significant heterogeneity in effect sizes of the associations of psychological distress with positive child outcomes (Q = 55.61, df = 14, p < .001), with 74.8% of the variance in effect sizes being true variance. The funnel plot and Egger test did not detect significant publication bias (, t(13) = 0.57, p = .58; Supplementary Figure S1B).
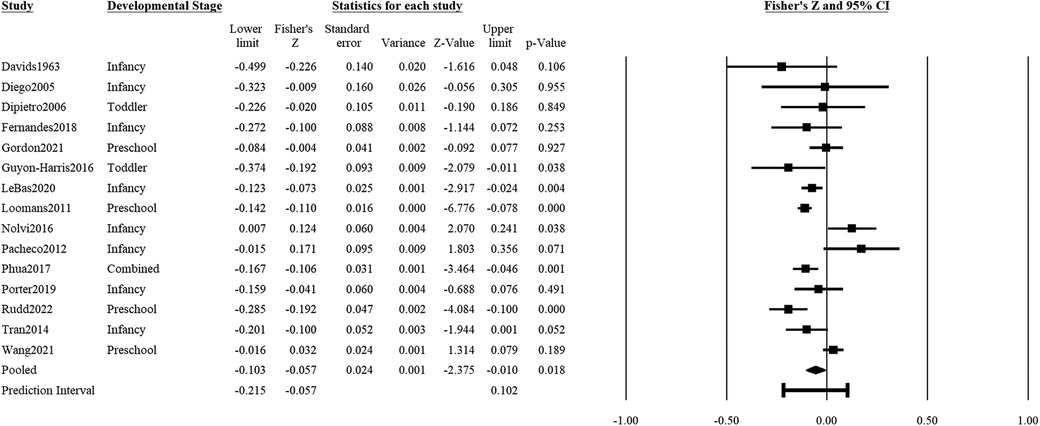
Figure 3. Effect sizes (in Fisher's Z) and forest plots for associations of prenatal maternal psychological distress and positive socioemotional outcome for the child. Combined refers to studies that had participants across multiple developmental stages and the effect sizes were averaged for this analysis.
Two studies provided gender-specific effects of psychological distress on positive child outcomes. As such, a subgroup analysis by gender was not possible. In addition, no studies reported the effect of psychological distress on outcomes in mid-childhood and adolescence. With infancy as the reference group, there was no significant difference in effect size between outcomes of infants vis-à-vis outcomes of toddlers (β = −0.09, CI 95% = −0.27, 0.10, p = .37) nor preschoolers (β = −0.04, CI 95% = −0.14, 0.07, p = .50). With North America as the reference group, studies in Europe reported significantly bigger effect size than studies in North America (β = 0.16, CI 95% = 0.03, 0.29, p = .022); the effect sizes of studies in other continents were not significantly different from North American studies (ps > 0.09).
Positive mental health on adverse outcomes
Positive maternal mental health (e.g., uplifts or positive mood) during pregnancy was not significantly associated with adverse child outcomes (5 studies: r = z′ = −0.02, SEz′ = 0.02, CIz′ 95% = −0.06, 0.02, p = .35; Figure 4). The prediction interval of effect sizes was estimated to be between r = −0.19 and 0.083. There was significant heterogeneity in associations of positive prenatal mental health with adverse child outcomes (Q = 9.66, df = 4, p = .047), with true variance in effect sizes estimated to be 58.6% of what was collated in this study. There was no indication of publication bias based on the funnel plot and Egger test (, t(3) = 0.04, p = .97; Supplementary Figure S1C).
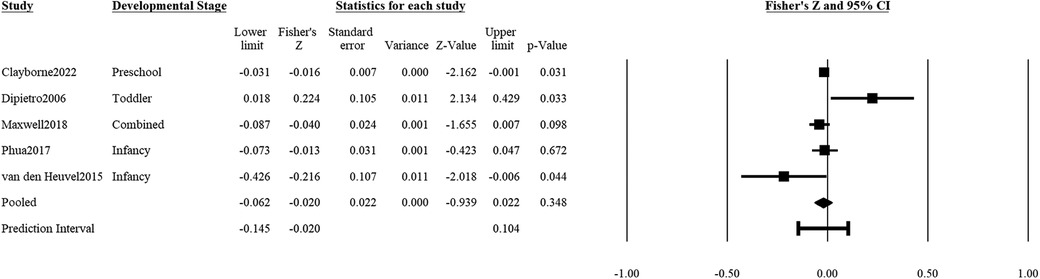
Figure 4. Effect sizes (in Fisher's Z) and forest plots for associations of prenatal maternal positive mental health and negative socioemotional outcome for the child. Combined refers to studies that had participants across multiple developmental stages and the effect sizes were averaged for this analysis.
Only one study (35) reported a gender-specific effect size of positive prenatal mental health on adverse child outcomes. There were also insufficient studies to conduct meta-regressions on the moderating effect of developmental stage or continent.
Positive mental health on positive outcomes
Positive maternal mental health during pregnancy was significantly associated with positive child outcomes (2 studies: r = z′ = 0.12, SEz′ = 0.05, CI 95% = 0.003, 0.018, p = .021; Figure 5). An accurate estimation of the prediction interval was not possible due to the low number of studies (104). Q-statistic showed that there was no significant heterogeneity in the effects of positive prenatal mental health and positive child outcomes (Q = 1.41, df = 1, p = .24), but 71.1% of the observed variance was likely to be due to sampling error (I2 = 28.94). The non-significant heterogeneity is likely due to the low number of studies.
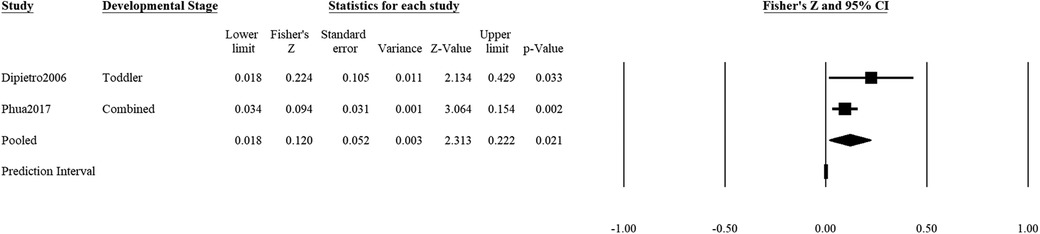
Figure 5. Effect sizes (in Fisher's Z) and forest plots for associations of prenatal maternal positive mental health and positive socioemotional outcome for the child. Combined refers to studies that had participants across multiple developmental stages and the effect sizes were averaged for this analysis.
Discussion
This meta-analysis aimed to comprehensively explore the nuanced associations between maternal psychological distress and positive mental health during pregnancy and the diverse facets of child socioemotional development, encompassing various developmental stages, domains of development, and geographical locations. Importantly, our investigation revealed no significant evidence of publication bias or moderation by study location, underscoring the robustness of our findings.
Our study has significantly contributed to the discourse by discerning that the impact of maternal psychological distress and positive mental health during pregnancy exhibits specificity with respect to child outcomes. Specifically, our results indicate that prenatal psychological distress exhibits stronger associations with adverse child outcomes, whereas positive prenatal mental health demonstrates stronger associations with positive outcomes. This distinct pattern highlights the independence of negative and positive mental health constructs (9, 10, 19), substantiating the need for separate investigations into maternal mental ill-health and well-being. Furthermore, these findings underscore the necessity of exploring both negative and positive developmental trajectories in children to provide a more comprehensive understanding of their socioemotional development.
Intriguingly, while prenatal psychological distress exhibited significant associations with child outcomes, the association was notably weak. This aligns with prior meta-analyses that similarly reported modest associations between poor prenatal mental health and various child outcomes. Maternal prenatal anxiety was significantly, but weakly, associated with preterm births and low birthweight (105). In another meta-analysis, the odds of adverse socioemotional development for children with mothers who experienced prenatal depression and anxiety were likewise small, with odds ratios of 1.76 and 1.47, respectively (106). Beyond the prenatal period, maternal depression also displayed weak correlations with socioemotional problems (0.15 < rs < 0.24) and positive affect (r = −0.10) in children (107). Thus, our study underscores the multi-faceted nature of influences on child socioemotional development, emphasizing the importance of considering a broad range of factors in future research.
Comparably, the association between positive prenatal mental health and positive child outcomes rivaled the effect size observed for the association between psychological distress and adverse outcomes. Particularly, the effect size for positive prenatal mental health was even greater than that for the association between psychological distress and positive outcomes. This finding echoes existing literature demonstrating the distinct impacts of positive and negative maternal mental health on specific child outcomes. For instance, positive antenatal maternal mental health is associated with positive cognitive, language, social, and competence development of the child, with no corresponding significant association for negative antenatal mental health (19). This absence of overlap in predictors of socioemotional difficulties and well-being has also been observed in adolescent samples (17). Thus, our study accentuates the necessity of embracing a comprehensive understanding of maternal mental health across the entire spectrum and its influence on child development by incorporating measurements of positive development.
A pivotal finding from our analysis emerged in the context of developmental stages. Contrary to our initial expectations, the strength of the association between psychological distress and adverse socioemotional development remained consistent across developmental stages. This consistency is somewhat surprising given our anticipation that the effects of prenatal mental health might diminish over time due to mitigating factors from the broader sociocultural environment. It is plausible that prenatal mental health may set individuals or families on trajectories that perpetuate adverse early life circumstances (22–24). The persistence of prenatal ill-health symptoms beyond pregnancy into childhood supports this notion (108–110).
Due to the limited number of studies, our analyses predominantly centered on the relationship between prenatal psychological distress and adverse child outcomes. This emphasis on the negative spectrum of mental health and development mirrors the current state of the field. While health is intrinsically characterized by complete well-being and not just the absence of illness, perinatal mental health or well-being is often operationalized solely as the nonexistence of depressive or anxiety symptoms (111). We echo the call from fellow researchers in advocating for an expansion of our exploration into maternal mental health and child development to encompass the positive spectrum of constructs (11, 13, 15, 17, 112).
Limitations
This meta-analysis must be interpreted in light of the limitations. Foremost, the scarcity of studies delving into positive mental health and child outcomes constrained our ability to conduct exhaustive analyses on these dimensions. Second, the diverse mental health and socioemotional development measures were amalgamated into overarching negative and positive categories. For example, there was no differentiation between depression and anxiety (i.e., psychological distress), optimism and positive affect (i.e., positive mental health), internalizing and externalizing symptoms (i.e., negative socioemotional outcome), nor prosocial behaviors and positive affectivity (i.e., positive socioemotional outcome). This oversimplification might not accurately capture the nuances that certain aspects of mental health or child development hold. These complexities could potentially be moderated by factors such as gender, developmental stages, and dimensions that were not encapsulated in this meta-analysis. Longitudinal research has revealed gender-specific differences in the risk and protective factors for internalizing and externalizing symptoms during adolescence (113). The intricate nuances outlined above signify a significant research gap, impinging on the depth of our comprehension of the intricate relationship between maternal mental health and child development.
Furthermore, our study's scope was confined to the pregnancy period, preventing us from investigating the endurance of prenatal mental health symptoms and their subsequent impact on child development. However, extant data from various birth cohorts suggest a substantial persistence of maternal depression and anxiety symptoms from pregnancy into childhood (114–116). Notably, children whose mothers experienced enduring mental health symptoms throughout the peripartum period displayed elevated odds of manifesting internalizing problems in comparison to their peers (117).
It is also essential to recognize that child development is inherently multifactorial and complex. While this study emphasizes the significance of prenatal mental health as a potential influential factor, child development is shaped by a myriad of interrelated influences, including genetics, environmental factors, and broader familial dynamics. Ultimately, a child's socioemotional well-being develops from an intricate interplay of genetic, environmental, and maternal factors. Our study contributes to the expanding body of evidence that highlights the significance of maternal mental health during pregnancy, particularly emphasizing the distinctive contribution of positive mental health to child socioemotional development.
Conclusion
This study validates the existing body of literature by reaffirming the substantial link between prenatal maternal mental health and the socioemotional development of children. Moreover, the observed associations between prenatal psychological distress and child outcomes, while significant, were consistently weaker than anticipated, urging us to unveil the moderating influences at play. An illustrative instance of such moderation is evident in the work of Goodman et al. (107), which showed the impact of maternal depression symptoms on offspring socioemotional development being amplified within families facing limited economic resources.
By unveiling the distinct impacts of psychological distress and positive mental health across domains and developmental stages, our findings advocate for a comprehensive approach to maternal well-being and child development. It is imperative that we broaden our perspective to encompass the positive spectrum of both mental health and child development. While averting adverse socioemotional outcomes remains pivotal, nurturing the positive socioemotional growth of children assumes equal significance. The contexts for interventions and public health initiatives aimed at preventing ill-health and promoting well-being diverge significantly, necessitating distinct strategies to maximize the potential of the next generation.
Data availability statement
The raw data supporting the conclusions of this article will be made available upon request to the corresponding author, without undue reservation.
Author contributions
DP conceptualized and designed the study. All authors contributed to the literature search, data extraction, and organization of the database. DP and CC performed the statistical analysis. DP wrote the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study is supported by A*STAR #C211618004.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1221232/full#supplementary-material
References
1. International Monetary Fund. The IMF and the millennium development goals (2015). Available at: https://www.imf.org/external/np/exr/facts/pdf/mdg.pdf
2. World Health Organization. Mental health action plan 2013–2020 (2013). Available at: http://apps.who.int/iris/bitstream/10665/89966/1/9789241506021_eng.pdf
3. Bauer A, Parsonage M, Knapp M, Lemmi V, Adelaja B. The costs of perinatal mental health problems. London, UK (2014). Available at: https://www.nwcscnsenate.nhs.uk/files/3914/7030/1256/Costs_of_perinatal_mh.pdf
4. Pearson RM, Evans J, Kounali D, Lewis G, Heron J, Ramchandani PG, et al. Maternal depression during pregnancy and the postnatal period: risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry. (2013) 70(12):1312–9. doi: 10.1001/jamapsychiatry.2013.2163
5. Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. Am J Psychiatry. (2006) 163(6):1001–8. doi: 10.1176/ajp.2006.163.6.1001
6. Glover V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract Res Clin Obstet Gynaecol. (2014) 28(1):25–35. doi: 10.1016/j.bpobgyn.2013.08.017
7. Huizink AC, Mulder EJ, Buitelaar JK. Prenatal stress and risk for psychopathology: specific effects or induction of general susceptibility? Psychol Bull. (2004) 130(1):115. doi: 10.1037/0033-2909.130.1.115
8. World Health Organization. Preamble to the constitution of the World Health Organization as adopted by the international health conference. New York: Official Records of the World Health Organization (1948). Available at: http://apps.who.int/gb/bd/PDF/bd47/EN/constitution-en.pdf
9. Huppert FA, Whittington JE. Evidence for the independence of positive and negative well-being: implications for quality of life assessment. Br J Health Psychol. (2003) 8(1):107–22. doi: 10.1348/135910703762879246
10. Phua DY, Kee MZL, Meaney MJ. Positive maternal mental health, parenting, and child development. Biol Psychiatry. (2020) 87(4):328–37. doi: 10.1016/j.biopsych.2019.09.028
11. Ryff CD, Dienberg Love G, Urry HL, Muller D, Rosenkranz MA, Friedman EM, et al. Psychological well-being and ill-being: do they have distinct or mirrored biological correlates? Psychother Psychosom. (2006) 75(2):85–95. doi: 10.1159/000090892
12. Sharpe H, Patalay P, Fink E, Vostanis P, Deighton J, Wolpert M. Exploring the relationship between quality of life and mental health problems in children: implications for measurement and practice. Eur Child Adolesc Psychiatry. (2016) 25(6):659–67. doi: 10.1007/s00787-015-0774-5
13. Keyes CL. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consult Clin Psychol. (2005) 73(3):539–48. doi: 10.1037/0022-006X.73.3.539
14. Patalay P, Fitzsimons E. Correlates of mental illness and wellbeing in children: are they the same? Results from the UK millennium cohort study. J Am Acad Child Adolesc Psychiatry. (2016) 55(9):771–83. doi: 10.1016/j.jaac.2016.05.019
15. Hofgaard LS, Nes RB, Røysamb E. Introducing two types of psychological resilience with partly unique genetic and environmental sources. Sci Rep. (2021) 11(1):8624. doi: 10.1038/s41598-021-87581-5
16. Rees G. The association of childhood factors with children’s subjective well-being and emotional and behavioural difficulties at 11 years old. Child Indic Res. (2018) 11(4):1107–29. doi: 10.1007/s12187-017-9479-2
17. Lereya ST, Patalay P, Deighton J. Predictors of mental health difficulties and subjective wellbeing in adolescents: a longitudinal study. JCPP Adv. (2022) 2(2):e12074. doi: 10.1002/jcv2.12074
18. Monteiro F, Fonseca A, Pereira M, Canavarro MC. Is positive mental health and the absence of mental illness the same? Factors associated with flourishing and the absence of depressive symptoms in postpartum women. J Clin Psychol. (2021) 77(3):629–45. doi: 10.1002/jclp.23081
19. Phua DY, Kee MKZL, Koh DXP, Rifkin-Graboi A, Daniels M, Chen H, et al. Positive maternal mental health during pregnancy associated with specific forms of adaptive development in early childhood: evidence from a longitudinal study. Dev Psychopathol. (2017) 29(5):1573–87. doi: 10.1017/S0954579417001249
20. Hay I, Ashman AF. The development of adolescents’ emotional stability and general self-concept: the interplay of parents, peers, and gender. Int J Disabil Dev Educ. (2003) 50(1):77–91. doi: 10.1080/1034912032000053359
21. Markiewicz D, Lawford H, Doyle AB, Haggart N. Developmental differences in adolescents’ and young adults’ use of mothers, fathers, best friends, and romantic partners to fulfill attachment needs. J Youth Adolesc. (2006) 35(1):121–34. doi: 10.1007/s10964-005-9014-5
22. Hakamata Y, Suzuki Y, Kobashikawa H, Hori H. Neurobiology of early life adversity: a systematic review of meta-analyses towards an integrative account of its neurobiological trajectories to mental disorders. Front Neuroendocrinol. (2022) 65:100994. doi: 10.1016/j.yfrne.2022.100994
23. Korkeila J, Vahtera J, Nabi H, Kivimäki M, Korkeila K, Sumanen M, et al. Childhood adversities, adulthood life events and depression. J Affect Disord. (2010) 127(1):130–8. doi: 10.1016/j.jad.2010.04.031
24. Luby JL, Barch D, Whalen D, Tillman R, Belden A. Association between early life adversity and risk for poor emotional and physical health in adolescence: a putative mechanistic neurodevelopmental pathway. JAMA Pediatr. (2017) 171(12):1168–75. doi: 10.1001/jamapediatrics.2017.3009
25. Burnette JL, Knouse LE, Vavra DT, O’Boyle E, Brooks MA. Growth mindsets and psychological distress: a meta-analysis. Clin Psychol Rev. (2020) 77:101816. doi: 10.1016/j.cpr.2020.101816
26. Huppert FA, Baylis N, Keverne B. Introduction: why do we need a science of well-being? Philos Trans R Soc B. (2004) 359(1449):1331–2. doi: 10.1098/rstb.2004.1519
27. Keyes CL. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. (2002) 43(2):207–22. doi: 10.2307/3090197
28. Ryff CD, Keyes CLM. The structure of psychological well-being revisited. J Pers Soc Psychol. (1995) 69(4):719–27. doi: 10.1037/0022-3514.69.4.719
29. Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. (2012) 22(10):1435–43. doi: 10.1177/1049732312452938
30. Baibazarova E, van de Beek C, Cohen-Kettenis PT, Buitelaar J, Shelton KH, van Goozen SHM. Influence of prenatal maternal stress, maternal plasma cortisol and cortisol in the amniotic fluid on birth outcomes and child temperament at 3 months. Psychoneuroendocrinology. (2013) 38(6):907–15. doi: 10.1016/j.psyneuen.2012.09.015
31. Barker ED. The duration and timing of maternal depression as a moderator of the relationship between dependent interpersonal stress, contextual risk and early child dysregulation. Psychol Med. (2013) 43(8):1587–96. doi: 10.1017/S0033291712002450
32. Bekkhus M, Lee Y, Nordhagen R, Magnus P, Samuelsen SO, Borge AIH. Re-examining the link between prenatal maternal anxiety and child emotional difficulties, using a sibling design. Int J Epidemiol. (2018) 47(1):156–65. doi: 10.1093/ije/dyx186
33. Bhat A, Chowdayya R, Selvam S, Khan A, Kolts R, Srinivasan K. Maternal prenatal psychological distress and temperament in 1–4 month old infants—a study in a non-western population. Infant Behav Dev. (2015) 39:35–41. doi: 10.1016/j.infbeh.2014.12.002
34. Bush NR, Jones-Mason K, Coccia M, Caron Z, Alkon A, Thomas M, et al. Effects of pre- and postnatal maternal stress on infant temperament and autonomic nervous system reactivity and regulation in a diverse, low-income population. Dev Psychopathol. (2017) 29(5):1553–71. doi: 10.1017/S0954579417001237
35. Clayborne ZM, Nilsen W, Torvik FA, Gustavson K, Bekkhus M, Gilman SE, et al. Positive maternal mental health attenuates the associations between prenatal stress and children’s internalizing and externalizing symptoms. Eur Child Adolesc Psychiatry. (2022) 32:1781–94. doi: 10.1007/s00787-022-01999-4
36. Davids A, Holden RH, Gray GB. Maternal anxiety during pregnancy and adequacy of mother and child adjustment eight months following childbirth. Child Dev. (1963) 34(4):993–1002. doi: 10.2307/1126541
37. Davis EP, Snidman N, Wadhwa PD, Glynn LM, Schetter CD, Sandman CA. Prenatal maternal anxiety and depression predict negative behavioral reactivity in infancy. Infancy. (2004) 6(3):319–31. doi: 10.1207/s15327078in0603_1
38. Davis EP, Glynn LM, Schetter CD, Hobel C, Chicz-Demet A, Sandman CA. Prenatal exposure to maternal depression and cortisol influences infant temperament. J Am Acad Child Adolesc Psychiatry. (2007) 46(6):737–46. doi: 10.1097/chi.0b013e318047b775
39. Davis EP, Sandman CA. Prenatal psychobiological predictors of anxiety risk in preadolescent children. Psychoneuroendocrinology. (2012) 37(8):1224–33. doi: 10.1016/j.psyneuen.2011.12.016
40. Davis EP, Hankin BL, Glynn LM, Head K, Kim DJ, Sandman CA. Prenatal maternal stress, child cortical thickness, and adolescent depressive symptoms. Child Dev. (2019) 91(2):e432–50. doi: 10.1111/cdev.13252
41. de Bruijn ATCE, van Bakel HJA, van Baar AL. Sex differences in the relation between prenatal maternal emotional complaints and child outcome. Early Hum Dev. (2009) 85(5):319–24. doi: 10.1016/j.earlhumdev.2008.12.009
42. Diego MA, Field T, Hernandez-Reif M. Prepartum, postpartum and chronic depression effects on neonatal behavior. Infant Behav Dev. (2005) 28(2):155–64. doi: 10.1016/j.infbeh.2005.02.002
43. DiPietro JA, Novak MFSX, Costigan KA, Atella LD, Reusing SP. Maternal psychological distress during pregnancy in relation to child development at age two. Child Dev. (2006) 77(3):573–87. doi: 10.1111/j.1467-8624.2006.00891.x
44. D’Souza S, Crawford CN, Buckley J, Underwood L, Peterson ER, Bird A, et al. Antenatal determinants of early childhood talking delay and behavioural difficulties. Infant Behav Dev. (2019) 57:101388. doi: 10.1016/j.infbeh.2019.101388
45. Duguay G, Garon-Bissonnette J, Lemieux R, Dubois-Comtois K, Mayrand K, Berthelot N. Socioemotional development in infants of pregnant women during the COVID-19 pandemic: the role of prenatal and postnatal maternal distress. Child Adolesc Psychiatry Ment Health. (2022) 16(1):28. doi: 10.1186/s13034-022-00458-x
46. Fernandes M, Srinivasan K, Menezes G, Ramchandani PG. Prenatal depression, fetal neurobehavior, and infant temperament: novel insights on early neurodevelopment from a socioeconomically disadvantaged Indian cohort. Dev Psychopathol. (2018) 30(3):725–42. doi: 10.1017/S0954579418000615
47. Frigerio A, Nazzari S. Antenatal maternal anxiety, maternal sensitivity and toddlers’ behavioral problems: an investigation of possible pathways. Early Hum Dev. (2021) 157:105364. doi: 10.1016/j.earlhumdev.2021.105364
48. Galbally M, Watson SJ, Keelan J, MacMillan KK, Power J, Ijzendoorn MV, et al. Maternal perinatal depression, circulating oxytocin levels and childhood emotional disorders at 4 years of age: the importance of psychosocial context. J Psychiatr Res. (2020) 130:247–53. doi: 10.1016/j.jpsychires.2020.07.010
49. Glynn LM, Howland MA, Sandman CA, Davis EP, Phelan M, Baram TZ, et al. Prenatal maternal mood patterns predict child temperament and adolescent mental health. J Affect Disord. (2018) 228:83–90. doi: 10.1016/j.jad.2017.11.065
50. Gordon S, Rotheram-Fuller E, Rezvan P, Stewart J, Christodoulou J, Tomlinson M. Maternal depressed mood and child development over the first five years of life in South Africa. J Affect Disord. (2021) 294:346–56. doi: 10.1016/j.jad.2021.07.027
51. Green CG, Babineau V, Jolicoeur-Martineau A, Bouvette-Turcot A-A, Minde K, Sassi R, et al. Prenatal maternal depression and child serotonin transporter linked polymorphic region (5-HTTLPR) and dopamine receptor D4 (DRD4) genotype predict negative emotionality from 3 to 36 months. Dev Psychopathol. (2016) 29(3):901–17. doi: 10.1017/S0954579416000560
52. Gustafsson HC, Sullivan EL, Nousen EK, Sullivan CA, Huang E, Rincon M, et al. Maternal prenatal depression predicts infant negative affect via maternal inflammatory cytokine levels. Brain Behav Immun. (2018) 73:470–81. doi: 10.1016/j.bbi.2018.06.011
53. Gutteling BM, de Weerth C, Willemsen-Swinkels SHN, Huizink AC, Mulder EJH, Visser GHA, et al. The effects of prenatal stress on temperament and problem behavior of 27-month-old toddlers. Eur Child Adolesc Psychiatry. (2005) 14(1):41–51. doi: 10.1007/s00787-005-0435-1
54. Guyon-Harris K, Huth-Bocks A, Lauterbach D, Janisse H. Trajectories of maternal depressive symptoms across the birth of a child: associations with toddler emotional development. Arch Women’s Mental Health. (2016) 19(1):153–65. doi: 10.1007/s00737-015-0546-8
55. Hartman S, Eilertsen EM, Ystrom E, Belsky J, Gjerde LC. Does prenatal stress amplify effects of postnatal maternal depressive and anxiety symptoms on child problem behavior? Dev Psychol. (2020) 56(1):128–37. doi: 10.1037/dev0000850
56. Haselbeck C, Niederberger U, Kulle A, Wache K, Brauner E, Gutermuth M, et al. Prenatal maternal distress seems to be associated with the infant’s temperament and motor development: an explorative study. J Neural Transm. (2017) 124(7):881–90. doi: 10.1007/s00702-017-1712-0
57. Hay DF, Pawlby S, Waters CS, Sharp D. Antepartum and postpartum exposure to maternal depression: different effects on different adolescent outcomes. J Child Psychol Psychiatry. (2008) 49(10):1079–88. doi: 10.1111/j.1469-7610.2008.01959.x
58. Henrichs J, Schenk JJ, Schmidt HG, Velders FP, Hofman A, Jaddoe VWV, et al. Maternal pre- and postnatal anxiety and infant temperament. The generation R study. Infant Child Dev. (2009) 18(6):556–72. doi: 10.1002/icd.639
59. Hentges RF, Graham SA, Plamondon A, Tough S, Madigan S. A developmental cascade from prenatal stress to child internalizing and externalizing problems. J Pediatr Psychol. (2019) 44(9):1057–67. doi: 10.1093/jpepsy/jsz044
60. Hentges RF, Graham SA, Plamondon A, Tough S, Madigan S. Bidirectional associations between maternal depression, hostile parenting, and early child emotional problems: findings from the all our families cohort. J Affect Disord. (2021) 287:397–404. doi: 10.1016/j.jad.2021.03.056
61. Huizink AC, De Medina PGR, Mulder EJ, Visser GH, Buitelaar JK. Psychological measures of prenatal stress as predictors of infant temperament. J Am Acad Child Adolesc Psychiatry. (2002) 41(9):1078–85. doi: 10.1016/S0378-3782(02)00075-0
62. Huttenen MO, Martin RP, Noyes J, Wisenbaker J, Huttunen MO. Prediction of early childhood negative emotionality and inhibition from maternal distress during pregnancy. Merrill Palmer Q. (1999) 45(3):370–91.
63. Korja R, McMahon C. Maternal prenatal mood problems and lower maternal emotional availability associated with lower quality of child’s emotional availability and higher negative affect during still-face procedure. Infancy. (2021) 26(6):901–19. doi: 10.1111/infa.12428
64. Le Bas GA, Youssef GJ, Macdonald JA, Mattick R, Teague SJ, Honan I, et al. Maternal bonding, negative affect, and infant social-emotional development: a prospective cohort study. J Affect Disord. (2021) 281:926–34. doi: 10.1016/j.jad.2020.11.031
65. Leerkes EM, Crockenberg SC. The impact of maternal characteristics and sensitivity on the concordance between maternal reports and laboratory observations of infant negative emotionality. Infancy. (2003) 4(4):517–39. doi: 10.1207/S15327078IN0404_07
66. Lin B, Crnic KA, Luecken LJ, Gonzales NA. Maternal prenatal stress and infant regulatory capacity in Mexican Americans. Infant Behav Dev. (2014) 37(4):571–82. doi: 10.1016/j.infbeh.2014.07.001
67. Loomans EM, der Stelt OV, van Eijsden M, Gemke RJBJ, Vrijkotte T, den Bergh BRHV. Antenatal maternal anxiety is associated with problem behaviour at age five. Early Hum Dev. (2011) 87(8):565–70. doi: 10.1016/j.earlhumdev.2011.04.014
68. Luo M, Pappa I, Cecil CAM, Jansen P, van Ijzendoorn MH, Kok R. Maternal psychological problems during pregnancy and child externalizing problems: moderated mediation model with child self-regulated compliance and polygenic risk scores for aggression. Child Psychiatry Hum Dev. (2022) 53(4):654–66. doi: 10.1007/s10578-021-01154-1
69. Luoma I, Tamminen T, Kaukonen P, Laippala P, Puura K, Salmelin R, et al. Longitudinal study of maternal depressive symptoms and child well-being. J Am Acad Child Adolesc Psychiatry. (2001) 40(12):1367–74. doi: 10.1097/00004583-200112000-00006
70. Martini J, Knappe S, Beesdo-Baum K, Lieb R, Wittchen H-U. Anxiety disorders before birth and self-perceived distress during pregnancy: associations with maternal depression and obstetric, neonatal and early childhood outcomes. Early Hum Dev. (2010) 86(5):305–10. doi: 10.1016/j.earlhumdev.2010.04.004
71. Maxwell SD, Fineberg AM, Drabick DA, Murphy SK, Ellman LM. Maternal prenatal stress and other developmental risk factors for adolescent depression: spotlight on sex differences. J Abnorm Child Psychol. (2018) 46(2):381–97. doi: 10.1007/s10802-017-0299-0
72. McGuinn LA, Tamayo-Ortiz M, Rosa MJ, Harari H, Osorio-Valencia E, Schnaas L, et al. The influence of maternal anxiety and cortisol during pregnancy on childhood anxiety symptoms. Psychoneuroendocrinology. (2022) 139:105704. doi: 10.1016/j.psyneuen.2022.105704
73. Mohan D, Fitzgerald M, Collins C. The relationship between maternal depression (antenatal and pre-school stage) and childhood behavioural problems. Ir J Psychol Med. (1998) 15(1):10–3. doi: 10.1017/S0790966700004602
74. Nolvi S, Karlsson L, Bridgett DJ, Korja R, Huizink AC, Kataja E-L, et al. Maternal prenatal stress and infant emotional reactivity six months postpartum. J Affect Disord. (2016) 199:163–70. doi: 10.1016/j.jad.2016.04.020
75. Norcross PL, Leerkes EM, Zhou N. Examining pathways linking maternal depressive symptoms in infancy to children’s behavior problems: the role of maternal unresponsiveness and negative behaviors. Infant Behav Dev. (2017) 49:238–47. doi: 10.1016/j.infbeh.2017.09.009
76. O’Connor TG, Heron J, Golding J, Beveridge M, Glover V. Maternal antenatal anxiety and children’s behavioural/emotional problems at 4 years: report from the avon longitudinal study of parents and children. Br J Psychiatry. (2002) 180(6):502–8. doi: 10.1192/bjp.180.6.502
77. O’Connor TG, Heron J, Golding J, Glover V; ALSST. Maternal antenatal anxiety and behavioural/emotional problems in children: a test of a programming hypothesis. J Child Psychol Psychiatry. (2003) 44(7):1025–36. doi: 10.1111/1469-7610.00187
78. O’Donnell KJ, Glover V, Barker ED, O’Connor TG. The persisting effect of maternal mood in pregnancy on childhood psychopathology. Dev Psychopathol. (2014) 26(2):393–403. doi: 10.1017/S0954579414000029
79. Pacheco A, Figueiredo B. Mother’s depression at childbirth does not contribute to the effects of antenatal depression on neonate’s behavioral development. Infant Behav Dev. (2012) 35(3):513–22. doi: 10.1016/j.infbeh.2012.02.001
80. Pawlby S, Hay DF, Sharp D, Waters CS, O'Keane V. Antenatal depression predicts depression in adolescent offspring: prospective longitudinal community-based study. J Affect Disord. (2009) 113(3):236–43. doi: 10.1016/j.jad.2008.05.018
81. Pihlakoski L, Sourander A, Aromaa M, Rönning JA, Rautava P, Helenius H, et al. Do antenatal and postnatal parental psychological distress, and recognized need of help predict preadolescent’s psychiatric symptoms? The finnish family competence cohort study. Child Psychiatry Hum Dev. (2013) 44(2):305–19. doi: 10.1007/s10578-012-0326-x
82. Pickles A, Sharp H, Hellier J, Hill J. Prenatal anxiety, maternal stroking in infancy, and symptoms of emotional and behavioral disorders at 3.5 years. Eur Child Adolesc Psychiatry. (2017) 26(3):325–34. doi: 10.1007/s00787-016-0886-6
83. Polte C, Junge C, von Soest T, Seidler A, Eberhard-Gran M, Garthus-Niegel S. Impact of maternal perinatal anxiety on social-emotional development of 2-year-olds, a prospective study of Norwegian mothers and their offspring. Matern Child Health J. (2019) 23(3):386–96. doi: 10.1007/s10995-018-2684-x
84. Porter E, Lewis AJ, Watson SJ, Galbally M. Perinatal maternal mental health and infant socio-emotional development: a growth curve analysis using the MPEWS cohort. Infant Behav Dev. (2019) 57:101336. doi: 10.1016/j.infbeh.2019.101336
85. Quarini C, Pearson RM, Stein A, Ramchandani PG, Lewis G, Evans J. Are female children more vulnerable to the long-term effects of maternal depression during pregnancy? J Affect Disord. (2016) 189:329–35. doi: 10.1016/j.jad.2015.09.039
86. Rees SJ, Mohsin M, Klein L, Steel Z, Tol W, Dadds M, et al. The impact of maternal depressive symptoms and traumatic events on early childhood mental health in conflict-affected Timor-Leste. BJPsych Open. (2022) 8(2):e51. doi: 10.1192/bjo.2022.20
87. Rinne GR, Davis EP, Mahrer NE, Guardino CM, Charalel JM, Shalowitz MU, et al. Maternal depressive symptom trajectories from preconception through postpartum: associations with offspring developmental outcomes in early childhood. J Affect Disord. (2022) 309:105–14. doi: 10.1016/j.jad.2022.04.116
88. Rodriguez A, Bohlin G. Are maternal smoking and stress during pregnancy related to ADHD symptoms in children? J Child Psychol Psychiatry. (2005) 46(3):246–54. doi: 10.1111/j.1469-7610.2004.00359.x
89. Rothenberger SE, Resch F, Doszpod N, Moehler E. Prenatal stress and infant affective reactivity at five months of age. Early Hum Dev. (2011) 87(2):129–36. doi: 10.1016/j.earlhumdev.2010.11.014
90. Rouse MH, Goodman SH. Perinatal depression influences on infant negative affectivity: timing, severity, and co-morbid anxiety. Infant Behav Dev. (2014) 37(4):739–51. doi: 10.1016/j.infbeh.2014.09.001
91. Rudd KL, Cheng SS, Cordeiro A, Coccia M, Karr CJ, LeWinn KZ, et al. Associations between maternal stressful life events and perceived distress during pregnancy and child mental health at age 4. Res Child Adolesc Psychopathol. (2022) 50(8):977–86. doi: 10.1007/s10802-022-00911-7
92. Sharp H, Pickles A, Meaney M, Marshall K, Tibu F, Hill J. Frequency of infant stroking reported by mothers moderates the effect of prenatal depression on infant behavioural and physiological outcomes. PLoS One. (2012) 7(10):e45446. doi: 10.1371/journal.pone.0045446
93. Shuffrey LC, Sania A, Brito NH, Potter M, Springer P, Lucchini M, et al. Association of maternal depression and anxiety with toddler social-emotional and cognitive development in South Africa: a prospective cohort study. BMJ Open. (2022) 12(4):e058135. doi: 10.1136/bmjopen-2021-058135
94. Suarez A, Lahti J, Czamara D, Lahti-Pulkkinen M, Knight AK, Girchenko P, et al. The epigenetic clock at birth: associations with maternal antenatal depression and child psychiatric problems. J Am Acad Child Adolesc Psychiatry. (2018) 57(5):321–8.e2. doi: 10.1016/j.jaac.2018.02.011
95. Tran TD, Biggs B-A, Tran T, Simpson JA, de Mello MC, Hanieh S, et al. Perinatal common mental disorders among women and the social and emotional development of their infants in rural Vietnam. J Affect Disord. (2014) 160:104–112. doi: 10.1016/j.jad.2013.12.034
96. van den Heuvel MI, Johannes MA, Henrichs J, Van den Bergh BRH. Maternal mindfulness during pregnancy and infant socio-emotional development and temperament: the mediating role of maternal anxiety. Early Hum Dev. (2015) 91(2):103–8. doi: 10.1016/j.earlhumdev.2014.12.003
97. Van den Bergh BRH, Marcoen A. High antenatal maternal anxiety is related to adhd symptoms, externalizing problems, and anxiety in 8- and 9-year-olds. Child Dev. (2004) 75(4):1085–97. doi: 10.1111/j.1467-8624.2004.00727.x
98. Vedova DAM. Maternal psychological state and infant’s temperament at three months. J Reprod Infant Psychol. (2014) 32(5):520–34. doi: 10.1080/02646838.2014.947472
99. Velders FP, Dieleman G, Henrichs J, Jaddoe VWV, Hofman A, Verhulst FC, et al. Prenatal and postnatal psychological symptoms of parents and family functioning: the impact on child emotional and behavioural problems. Eur Child Adolesc Psychiatry. (2011) 20(7):341–50. doi: 10.1007/s00787-011-0178-0
100. Wang X, Xie J, Wu Y, Wu X, Yan S, Xu Y, et al. Gender-specific effect of pregnancy-related anxiety on preschooler’s emotional and behavioral development: a population-based cohort study. J Affect Disord. (2021) 279:368–76. doi: 10.1016/j.jad.2020.10.014
101. Whelan YM, Leibenluft E, Stringaris A, Barker ED. Pathways from maternal depressive symptoms to adolescent depressive symptoms: the unique contribution of irritability symptoms. J Child Psychol Psychiatry. (2015) 56(10):1092–100. doi: 10.1111/jcpp.12395
102. Zhang W, Finik J, Dana K, Glover V, Ham J, Nomura Y. Prenatal depression and infant temperament: the moderating role of placental gene expression. Infancy. (2017) 23(2):211–31. doi: 10.1111/infa.12215
103. Borenstein M, Higgins JPT, Hedges LV, Rothstein HR. Basics of meta-analysis: i2 is not an absolute measure of heterogeneity. Res Synth Methods. (2017) 8(1):5–18. doi: 10.1002/jrsm.1230
104. Spineli LM, Pandis N. Prediction interval in random-effects meta-analysis. Am J Orthod Dentofacial Orthop. (2020) 157(4):586–8. doi: 10.1016/j.ajodo.2019.12.011
105. Ding X-X, Wu Y-L, Xu S-J, Zhu R-P, Jia X-M, Zhang S-F, et al. Maternal anxiety during pregnancy and adverse birth outcomes: a systematic review and meta-analysis of prospective cohort studies. J Affect Disord. (2014) 159:103–10. doi: 10.1016/j.jad.2014.02.027
106. Madigan S, Oatley H, Racine N, Fearon RMP, Schumacher L, Akbari E, et al. A meta-analysis of maternal prenatal depression and anxiety on child socioemotional development. J Am Acad Child Adolesc Psychiatry. (2018) 57(9):645–57.e8. doi: 10.1016/j.jaac.2018.06.012
107. Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev. (2011) 14(1):1–27. doi: 10.1007/s10567-010-0080-1
108. Fihrer I, McMahon CA, Taylor AJ. The impact of postnatal and concurrent maternal depression on child behaviour during the early school years. J Affect Disord. (2009) 119(1):116–23. doi: 10.1016/j.jad.2009.03.001
109. Horwitz SM, Briggs-Gowan MJ, Storfer-Isser A, Carter AS. Persistence of maternal depressive symptoms throughout the early years of childhood. J Women’s Health. (2009) 18(5):637–45. doi: 10.1089/jwh.2008.1229
110. Milgrom J, Gemmill AW, Bilszta JL, Hayes B, Barnett B, Brooks J, et al. Antenatal risk factors for postnatal depression: a large prospective study. J Affect Disord. (2008) 108(1):147–57. doi: 10.1016/j.jad.2007.10.014
111. Allan C, Carrick-Sen D, Martin CR. What is perinatal well-being? A concept analysis and review of the literature. J Reprod Infant Psychol. (2013) 31(4):381–98. doi: 10.1080/02646838.2013.791920
112. Henrichs J, Witteveen AB. Commentary: promoting positive mental health during pregnancy—reflections on Lähdepuro et al. (2022). J Child Psychol Psychiatry. (2022) 64(5):817–9. doi: 10.1111/jcpp.13727
113. Cotter KL, Wu Q, Smokowski PR. Longitudinal risk and protective factors associated with internalizing and externalizing symptoms among male and female adolescents. Child Psychiatry Hum Dev. (2016) 47(3):472–85. doi: 10.1007/s10578-015-0580-9
114. Cents RAM, Diamantopoulou S, Hudziak JJ, Jaddoe VWV, Hofman A, Verhulst FC, et al. Trajectories of maternal depressive symptoms predict child problem behaviour: the generation R study. Psychol Med. (2013) 43(1):13–25. doi: 10.1017/S0033291712000657
115. Heron J, O’Connor TG, Evans J, Golding J, Glover V. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affect Disord. (2004) 80(1):65–73. doi: 10.1016/j.jad.2003.08.004
116. Kee MZL, Ponmudi S, Phua DY, Rifkin-Graboi A, Chong YS, Tan KH, et al. Preconception origins of perinatal maternal mental health. Arch Women’s Mental Health. (2021) 24(4):605–18. doi: 10.1007/s00737-020-01096-y
Keywords: prenatal mental health, positive mental health, socioemotional development, perinatal influence, depression, early life, anxiety
Citation: Phua DY, Chew CSM, Tan YL, Ng BJK, Lee FKL and Tham MMY (2023) Differential effects of prenatal psychological distress and positive mental health on offspring socioemotional development from infancy to adolescence: a meta-analysis. Front. Pediatr. 11:1221232. doi: 10.3389/fped.2023.1221232
Received: 12 May 2023; Accepted: 29 August 2023;
Published: 14 September 2023.
Edited by:
Karen Tabb, University of Illinois at Urbana-Champaign, United StatesReviewed by:
J. Carolyn Graff, University of Tennessee Health Science Center (UTHSC), United StatesMaria Fernanda Pineros Leano, Boston College, United States
© 2023 Phua, Chew, Tan, Ng, Lee and Tham. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Desiree Y. Phua ZGVzaXJlZV9waHVhQHNpY3MuYS1zdGFyLmVkdS5zZw==
 Desiree Y. Phua
Desiree Y. Phua Chermaine S. M. Chew1
Chermaine S. M. Chew1 Yang Lik Tan
Yang Lik Tan