Abstract
Objective:
To evaluate the diagnostic value of lung ultrasound (LUS) for childhood community-acquired pneumonia (CAP).
Methods:
A case-control study was conducted among pediatric outpatients with suspected CAP who underwent LUS examination. Baseline data such as clinical manifestations were collected. Diagnostic performance was assessed using Pearson Chi-square tests, with CT scans as the gold standard. Specificity, sensitivity, positive predictive value (PPV), and negative predictive value (NPV) of LUS were analyzed.
Results:
The study included 246 patients who underwent both LUS and CT (observation group) and 111 controls who received concurrent chest x-ray and CT within one week. LUS demonstrated significantly higher sensitivity (91.30% vs. 75.00%, P < 0.001) than chest x-ray group, while specificity, PPV, and NPV showed no statistically significant (P > 0.05).
Conclusion:
LUS exhibits high concordance with CT in pediatric CAP diagnosis, demonstrating excellent screening and diagnostic value for childhood CAP.
1 Introduction
Community-acquired pneumonia (CAP) is a common respiratory disease in children where early and accurate diagnosis is crucial for reducing complications and mortality (1). Currently, CT scans provide detailed pulmonary imaging and are more accurate for diagnosing complex or severe CAP (2), but concerns about radiation exposure and cost restricted their application in pediatric populations (3, 4). In recent years, lung ultrasound (LUS) has gained attention in CAP diagnosis due to its radiation-free, convenient, and bedside operation (5–7). While numerous studies have analyzed the sensitivity and specificity of LUS for diagnosing pneumonia in adults, research in pediatric outpatient settings remains limited (8–10). This study aims to investigate the diagnostic value of LUS for childhood CAP through a large-scale analysis of pediatric outpatient cases.
2 Methods
2.1 Data collection and grouping
This is a retrospective case-control study. Clinical diagnosis and treatment were performed by pediatricians. All cases were managed according to the Diagnosis and Treatment Guidelines for Pediatric Community-Acquired Pneumonia (2019 Edition) issued by the National Health Commission of China. We enrolled children aged ≤14 years with suspected CAP who visited the pediatric outpatient department of Liuzhou People's Hospital between January 1, 2021, and September 7, 2024. Clinical data were extracted from medical record, including gender, age, underlying diseases, symptoms (fever, cough, chest pain, asthma), pulmonary signs (coarse breath sounds, wheezing sound, fixed crackles), and imaging findings. Patients with primary pulmonary/respiratory diseases or non-Chinese nationality were excluded. Data collection was implemented by Tingting Qin, Zengpo Huang and Qiuhui Lan. And standardization was implemented by Linglin Li and Zhixuan Tang. Zhao Ma was responsible for quality control.
Cases that underwent both LUS and CT scans were included in the observation group, while cases that underwent both x-ray and CT scan within one week included in the control group. Using CT scans as the gold standard, the specificity, sensitivity, positive predictive value (PPV), and negative predictive value (NPV) of LUS in diagnosis of CAP were analyzed. For more detail, the study design is presented in Figure 1.
Figure 1
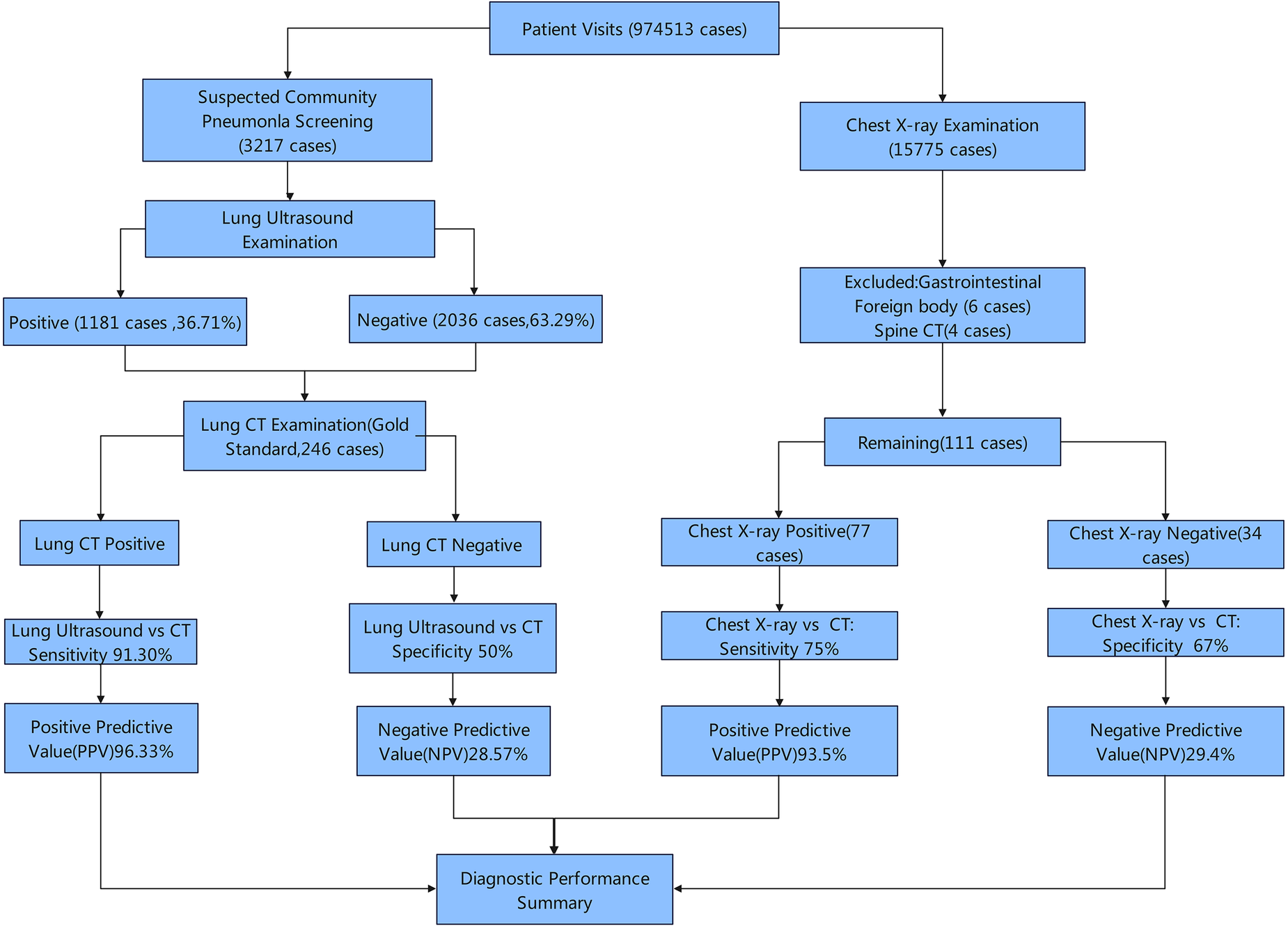
Study design.
The Voluson E8 ultrasound system from GE Healthcare Austria GmbH was used in this study. LUS was performed by the pediatric specialized team in the department of ultrasound medicine, with Lixue Cheng responsible for quality control. The presence of A-lines and sliding sign on LUS was defined as negative. In the observation group, different ultrasound images was subdivided into Observation Group 1–5:
Observation Group 1: consolidation or lung fragmentation signs (Figure 2).
Observation Group 2: diffuse B-lines (Figure 3).
Observation Group 3: multiple B-lines (defined as ≥3 B-lines in any intercostal space).
Observation Group 4: few B-lines (defined as <3 B-lines in any intercostal space).
Observation Group 5: hydrothorax.
Figure 2

Fragmentation sign (patient 1).
Figure 3

B-line (patient 2).
Chest x-ray and CT scan were implemented and diagnosed by the medical imaging center of Liuzhou People's Hospital.
This study has been approved by the Medical Ethics Committee of Liuzhou People's Hospital (No. KY-2023-075).
2.2 Statistical analysis
Data analysis was performed using IBM SPSS 24.0 software by Yijun Nie and Guofei Luo. Differences between the two groups were compared using Pearson Chi-square test or Fisher's exact test (α = 0.05).
3 Results
A total of 3,217 children with suspected CAP underwent LUS examination, with 1,181 cases (36.71%) testing positive and 2,036 cases (63.29%) negative. Among them, 246 patients who received concurrent LUS and chest CT scan within one week were enrolled in observation group, while 111 age-matched subjects undergoing the same examinations were selected as controls. Demographic details are presented in Table 1.
Table 1
| Demographic characteristics [n (%)] | Ultrasound positive group [n = 218 (89)] | Ultrasound negative group [n = 28 (11)] | X-ray Positive Group [n = 77 (69)] | X-ray negative group [n = 34 (31)] | P-valuea |
|---|---|---|---|---|---|
| Gender | 0.725 | ||||
| Male | 104 (48) | 13 (46) | 34 (44) | 19 (56) | |
| Female | 114 (52) | 15 (54) | 43 (56) | 15 (44) | |
| Age Group | <0.001 | ||||
| Under 1 month | 2 (1) | 0 | 0 | 0 | |
| 1 month–1 year | 61 (28) | 8 (29) | 2 | 1 | |
| Over 1 year | 155 (71) | 20 (71) | 75 | 33 | |
| Systemic symptoms | 0.054 | ||||
| Fever | 159 (73) | 19 (68) | |||
| Cough | 178 (82) | 28 (100) | |||
| Chest pain | 22 (10) | 1 (4) | |||
| Asthma | 96 (44) | 4 (14) | |||
| Signs | <0.001 | ||||
| Only coarse breath sounds | 102 (57) | 20 (76) | |||
| Wheezing sound | 41 (21) | 1 (15) | |||
| Fixed wet rales | 81 (22) | 0 | |||
| Ultrasound imaging characteristics | – | – | – | ||
| Consolidation | 113 (52) | 0 | |||
| Diffuse B-lines | 7 (3) | 0 | |||
| Multiple B-lines | 20 (9) | 0 | |||
| Few B-lines | 70 (32) | 0 | |||
| Hydrothorax | 8 (4) | 0 | |||
| A-line with sliding sign. | 0 | 28 (100) | |||
Demographic characteristics of children suspected of community-acquired pneumonia.
Pearson's Chi-Square Test.
Using chest CT scans as the gold standard, the diagnostic performance of LUS was evaluated as follows: sensitivity of 91.30%, specificity of 50%, PPV of 96.33% and NPV of 28.57%. The sensitivity of LUS was significantly higher than that of the chest x-ray group (P < 0.001), while the specificity, PPV and NPV showed no significantly difference (all P > 0.05), as illustrated in Table 2.
Table 2
| Group | TP | FP | FN | TN | Sensitivity (0.95CI) | Specificity (0.95CI) | PPV | NPV | Kappa |
|---|---|---|---|---|---|---|---|---|---|
| Ultrasound | 210 | 8 | 20 | 8 | 91.30% (87.67%–94.94%) | 50% (25.50%–74.50%) | 96.33% | 28.57% | 0.31 |
| Chest x-ray | 72 | 5 | 24 | 10 | 75.0% (66.34%–83.66%) | 66.67% (42.81%–90.52%) | 93.51% | 29.41% | 0.27 |
| P-valuea | <0.001 | 0.473 | 0.546 | 0.726 |
Comparison of the diagnostic performance of children community-acquired pneumonia between pulmonary ultrasound and chest x-ray.
TP, true positive; FP, false positive; FN, false negative; TN, true negative; PPV, positive predictive value; NPV, negative predictive value.
Pearson's Chi-Square Test.
Respectively, 113, 7, 20, 65 and 8 cases were subdivided into observation group 1–5 based on their different LUS images. The sensitivity (P < 0.001) and specificity (P < 0.05) showed significantly different than that of the chest x-ray group, while the PPV and NPV were no significantly difference, as shown in Table 3.
Table 3
| Group | TP | FP | FN | TN | Sensitivity (0.95CI) | Specificity (0.95CI) | PPV (0.95CI) | NPV (0.95CI) |
|---|---|---|---|---|---|---|---|---|
| Observation group 1 | 110 | 3 | 20 | 8 | 84.62% (78.26%–90.98%) | 72.73% (46.50%–98.96%) | 97.35% (94.34%, 100%) | 28.57% (11.74%–45.40%) |
| Observation group 2 | 7 | 0 | 20 | 8 | 25.93% (9.47%–42.39%) | 100% (1) | 100% (1) | 28.57% (11.74%–45.40%) |
| Observation group 3 | 20 | 0 | 20 | 8 | 50% (34.51%–65.49%) | 100% (1) | 100% (1) | 28.57% (11.74%–45.40%) |
| Observation group 4 | 65 | 5 | 20 | 8 | 76.47% (67.34%–85.60%) | 61.54% (35.21%–87.87%) | 92.86% (86.79%, 99.33%) | 28.57% (11.74%–45.40%) |
| Observation group 5 | 8 | 0 | 20 | 8 | 28.57% (11.74%–45.40%) | 100% (1) | 100% (1) | 28.57% (11.74%–45.40%) |
| Control group | 72 | 5 | 24 | 10 | 75% (66.34%–83.66%) | 66.67% (42.91%–90.43%) | 93.51% (88.00%, 99.02%) | 29.4% (13.91%–44.91%) |
| P-valuea | <0.001 | <0.05 | >0.05 | >0.05 |
Comparison of the diagnostic performance of children community-acquired pneumonia among different pulmonary ultrasound images and chest x-ray.
TP, true positive; FP, false positive; FN, false negative; TN, true negative; PPV, positive predictive value; NPV, negative predictive value.
Pearson's Chi-Square Test, and Fisher's Exact Probability.
4 Discussion
LUS has been widely applied in intensive care units, demonstrating significantly enhanced sensitivity for critically ill patients (11). However, most studies on CAP diagnosis, particularly outpatient CAP, have primarily focused on adults populations. Research indicates that LUS achieves a sensitivity of 93.4% and a specificity of 97.7% in diagnosing CAP in adults (12). Furthermore, studies have explored its role in emergency department settings, revealing both improved diagnostic accuracy and reduced diagnostic uncertainty (13). Additional dedicated studies have evaluated the diagnostic performance (sensitivity and specificity) of LUS for pneumonia in adults (14).
The sensitivity of LUS for diagnosing CAP in outpatient children was 91.30%, capable of detecting 91.30% of true positive cases with a low missed diagnosis rate. The diagnostic performance of outpatient lung ultrasound for childhood CAP was significantly higher than that of chest x-ray, with a statistically significant superiority (P < 0.001). However, the specificity of LUS was 50%, relatively low, suggesting a possibility of false positives. Therefore, if childhood CAP is high suspected clinically but LUS imaging is negative, further chest CT scans are recommended for evaluation. The PPV of LUS was 96.33%, meaning 96.33% of positive ultrasound results were true positives. This highlights its excellent performance in diagnosis and provides an advantage over chest x-ray, as a positive ultrasound can essentially confirm the diagnosis of childhood CAP. On the other hand, the NPV is 28.57%, indicating that only 28.57% of negative results were true negatives, which warrants caution in interpreting negative ultrasound findings. Overall, LUS exhibits high sensitivity and PPV in identifying childhood CAP, making it a more suitable initial screening tool than chest x-ray. Despite its lower specificity, negative ultrasound results should be comprehensively evaluated in conjunction with other diagnostic methods, such as CT scans. In the consolidation subgroup, it demonstrated a sensitivity of 84.62%, specificity of 72.73%, and a PPV of 97.35%. The consolidation sign, with their high sensitivity and specificity, serve as critical evidence for diagnosing childhood CAP via LUS.
Three cases showed lung consolidation on ultrasound but no abnormalities on chest CT in this study. Smaller consolidations may be less evident on CT imaging but can be visualized by LUS. Therefore, detection of small consolidations via LUS may suggest the early stage of pneumonia, which may warrant further investigation.
The limitations of this study include that only a small subset of cases underwent CT verification after pulmonary ultrasound results, leading to potential sample representativeness bias. Future multicenter, large-sample studies of ultrasound across diverse populations and healthcare settings may provide more strong evidence.
5 Conclusion
LUS demonstrates higher sensitivity than chest x-ray, suggesting superior diagnostic performance for childhood CAP, particularly in identifying lung consolidation and minor B-line signs. Considering its convenience, it may serve as an effective screening and diagnostic method in children CAP. For those who got positive symptoms and negative pulmonary ultrasound imaging, further chest CT scans are recommended to provide more comprehensive and accurate evidence for suspected cases.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Medical Ethics Committee of Liuzhou People's Hospital (Document Number: KY-2023-075). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
TQ: Investigation, Writing – original draft. ZH: Investigation, Writing – original draft. QL: Data curation, Methodology, Writing – review & editing. YN: Data curation, Methodology, Writing – review & editing. GL: Data curation, Writing – review & editing. LC: Investigation, Writing – review & editing. LL: Investigation, Writing – review & editing. ZT: Investigation, Writing – review & editing. ZM: Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The authors declare that financial support was received for the research and/or publication of this article. Self-funded Research Project of the Health Commission of Guangxi Zhuang Autonomous Region (Z20210288, Z-B20231358).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. In the preparation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
ZhongHDongX. Analysis of clinical characteristics and risk factors of severe adenovirus pneumonia in children. Front Pediatr. (2021) 9:566797. 10.3389/fped.2021.566797
2.
National Health Commission of the People’s Republic of China. Guidelines for the diagnosis and treatment of community-acquired pneumonia in children. Chin J Clin Infect Dis. (2019) 12(1):6–13. 10.3760/cma.j.issn.1674-2397.2019.01.002
3.
MandellLAWunderinkRGAnzuetoABartlettJGCampbellGDDeanNCet alInfectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. (2007) 44(Suppl 2):S27–72. 10.1086/511159
4.
ChavezMAShamsNEllingtonLENaithaniNGilmanRHSteinhoffMCet alLung ultrasound for the diagnosis of pneumonia in adults: a systematic review and meta-analysis. Respir Res. (2014) 15(1):50. 10.1186/1465-9921-15-50.
5.
LichtensteinDMézièreGBidermanPGepnerABarréO. The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med. (1997) 156(5):1640–6. 10.1164/ajrccm.156.5.96-07096
6.
LichtensteinD. Lung ultrasound in the critically ill. Curr Opin Crit Care. (2014) 20(3):315–22. 10.1097/MCC.0000000000000096
7.
VaughnVMDicksonRPHorowitzJKFlandersSA. Community-acquired pneumonia: a review. JAMA. (2024) 332(15):1282–95. 10.1001/jama.2024.14796
8.
OrsoDGuglielmoNCopettiR. Lung ultrasound in diagnosing pneumonia in the emergency department: a systematic review and meta-analysis. Eur J Emerg Med. (2018) 25(5):312–21. 10.1097/MEJ.0000000000000517
9.
ReissigAGramegnaAAlibertiS. The role of lung ultrasound in the diagnosis and follow-up of community-acquired pneumonia. Eur J Intern Med. (2012) 23(5):391–7. 10.1016/j.ejim.2012.01.003
10.
MusolinoAMDi SarnoLBuonsensoDMurcianoMChiarettiABoccuzziEet alUse of POCUS for the assessment of dehydration in pediatric patients-a narrative review. Eur J Pediatr. (2024) 183(3):1091–105. 10.1007/s00431-023-05394-2
11.
StaubLJMazzali BiscaroRRKaszubowskiEMauriciR. Lung ultrasound for the emergency diagnosis of pneumonia, acute heart failure, and exacerbations of chronic obstructive pulmonary disease/asthma in adults: a systematic review and meta-analysis. J Emerg Med. (2019) 56(1):53–69. 10.1016/j.jemermed.2018.09.009
12.
BoccatondaACoccoGD'ArdesDDelli PizziAVidiliGDe MoloCet alInfectious pneumonia and lung ultrasound. A Review. J Clin Med. (2023) 12(4):1402. 10.3390/jcm12041402
13.
JavaudinFMarjanovicNde CarvalhoHGaboritBLe BastardQBoucherEet alContribution of lung ultrasound in diagnosis of community-acquired pneumonia in the emergency department: a prospective multicentre study. BMJ Open. (2021) 11(9):e046849. 10.1136/bmjopen-2020-046849
14.
LongLZhaoHTZhangZYWangGYZhaoHL. Lung ultrasound for the diagnosis of pneumonia in adults: a meta-analysis. Medicine (Baltimore). (2017) 96(3):e5713. 10.1097/MD.0000000000005713
Summary
Keywords
children, community-acquired pneumonia, diagnostic value, lung ultrasound (LUS), outpatient
Citation
Qin T, Huang Z, Lan Q, Nie Y, Luo G, Cheng L, Li L, Tang Z and Ma Z (2025) Evaluation of the application value of ultrasound in the diagnosis of community-acquired pneumonia in children: a preliminary study based on large-scale outpatient cases. Front. Pediatr. 13:1582647. doi: 10.3389/fped.2025.1582647
Received
24 February 2025
Accepted
17 April 2025
Published
30 April 2025
Volume
13 - 2025
Edited by
Javier Rodriguez Fanjul, Hospital Germans Trias i Pujol, Spain
Reviewed by
Shereen AbdelMonem Mohamed, Cairo University, Egypt
Anna Maria Musolino, Bambino Gesù Children's Hospital (IRCCS), Italy
Updates
Copyright
© 2025 Qin, Huang, Lan, Nie, Luo, Cheng, Li, Tang and Ma.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhao Ma lzek@qq.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.