- 1Department of Pediatric Surgery, Qilu Hospital of Shandong University, Jinan, Shandong, China
- 2Department of Pediatric Surgery, Children’s Hospital of Nanjing Medical University, Nanjing, Jiangsu, China
Objective: Postoperative complications after surgery for congenital biliary dilatation (CBD) can be life-threatening and often necessitate redo surgery. We aimed to predict postoperative complications in patients with CBD using machine learning (ML) algorithms.
Study design: Data from pediatric patients with CBD who were surgically treated at our hospital between July 2014 and July 2023 was retrospectively analyzed. Multiple logistic regression and lasso regression were used to screen risk factors. Predictive models were developed using seven ML algorithms and the better-performing model was selected.
Results: A total of 211 patients were included in the final analysis. Among these, 31 patients experienced complications (cholangitis: 14 patients; pancreatitis: 21 patients).Risk factors for complications identified by variable screening were preoperative perforation, Todani classification type IV-A (type 4A), days of removal of drainage (removal drainage), and serum amylase. Predictors of postoperative cholangitis were preoperative perforation, preoperative cholangitis, type 4A, removal drainage, anemia, level of serum albumin and amylase. Preoperative perforation, cholangitis, serum gamma-glutamyl transferase and amylase were predictors of postoperative pancreatitis. Finally, logistic regression was selected to develop the clinical prediction model for postoperative complications, cholangitis, and pancreatitis.
Conclusions: We developed nomograms to predict postoperative complications, cholangitis, and pancreatitis after surgery for CBD using ML.
1 Introduction
Congenital biliary dilatation (CBD), also known as choledochal cyst, is a rare developmental malformation of the biliary system with a higher incidence in females (approximately male–female ratio 1:3) (1, 2). The incidence of CBD is highest in Asia (approximately 1/1,000 in Japan, and 0.3% in South Korea). In contrast, the incidence in western countries is much lower (one in 50,000–150,000) (3). Approximately 2/3 of patients with CBD are detected during childhood (4).
The typical clinical manifestations of CBD are abdominal pain, jaundice, and abdominal mass. Inadequate treatment can lead to liver function impairment, malnutrition, pancreatitis, bile duct perforation, and even cancer (5, 6). The first-choice treatment of CBD is complete excision with Roux-en-Y hepaticojejunostomy. With the recent advances in minimally invasive techniques, laparoscopic and robotic treatment are increasingly being used in CBD surgery.
Irrespective of the surgical approach (open or laparoscopic surgery), patients with CBD may develop postoperative complications such as anastomotic fistula, anastomotic stenosis, cholangitis, and pancreatitis. These complications can even be life-threatening (7), CBD-related complications are a concern of much debate (8, 9). However, there are no clinical prediction models for postoperative complications of CBD.
In this study, we discussed the risk factors for complications associated with laparoscopic surgical treatment of pediatric CBD. We used machine learning (ML) algorithms to construct a prediction model and develop a nomogram to provide a basis for preventing complications associated with CBD.
2 Material and methods
This study was approved by the Hospital ethical review committee. The presentation of this work follows the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) criteria (10).
2.1 Study population
This was a single-center, retrospective cohort study. Clinical data, test parameters, and demographic data of pediatric patients (age < 18 years) with CBD treated between July 2014 and July 2023 were extracted from the electronic medical records. The inclusion criteria were as follows: 1) CBD diagnosed by preoperative imaging and clinical symptoms; 2) patients who underwent surgical treatment at our hospital and the diagnosis of CBD confirmed during the surgical procedure; 3) regular follow-up for more than one year. The exclusion criteria were as follows: 1) patients who underwent other procedures simultaneously; 2) patients with concomitant severe liver, kidney, lung, or other diseases; 3) incomplete data.
2.2 Definitions
CBD types: CBD was classified using the Todani classification of the Alonzo-Lej classification system (11).
Preoperative cholangitis (Pre-cholangitis): cholangitis was confirmed by postoperative pathology.
Postoperative cholangitis (Post-cholangitis): the presence of clinical symptoms of abdominal pain, jaundice, fever, and laboratory tests confirming abnormal liver function postoperatively.
Postoperative pancreatitis (Post-pancreatitis): No pancreatitis or pancreatitis was controlled preoperatively but pancreatitis developed postoperatively.
2.3 Data collection and outcomes
Data regarding the patient factors [sex, age, weight, anemia, preoperative perforation, preoperative cholangitis, whether the type of CBD was type 4A (11), and whether the shape of the cyst was cystic], surgical and clinical information (duration of surgery, intraoperative blood loss, intraoperative blood transfusion, duration of hospital stay, postoperative hospital stay, and removal of drainage), and pre-operative laboratory results and radiological data [cyst diameter, white blood cell count (WBC), platelet count (PLT), aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transferase (GGT), AST to Platelet Ratio Index (APRI), alkaline phosphatase (AKP), total bilirubin (TBIL), direct bilirubin (DBIL), total protein, albumin, amylase, and lipase] were extracted from the electronic medical records.
2.4 Machine learning model building
2.4.1 Selection of risk factors
Variables were screened by the least absolute shrinkage and selection operator (LASSO) regression analysis with 10-fold cross-validation and multivariate logistic regression. Predictive models were constructed for each of the screened variables. The covariance of all explanatory variables was assessed using a correlation matrix. Possible interaction terms were tested, revealing no significant interactions.
2.4.2 Pre-processing of data
To maintain data integrity, factors with a substantial proportion of missing values (>20%) were excluded from the analysis. For variables with missing data, imputation was performed using the mean or median value, depending on the data type. The number of positive events was increased by a factor of five due to the low incidence of postoperative cholangitis and pancreatitis. The dataset was split into a training set (70%) and a test set (30%). Additionally, the data were standardized to ensure consistency in scale and range.
2.4.3 Model selection
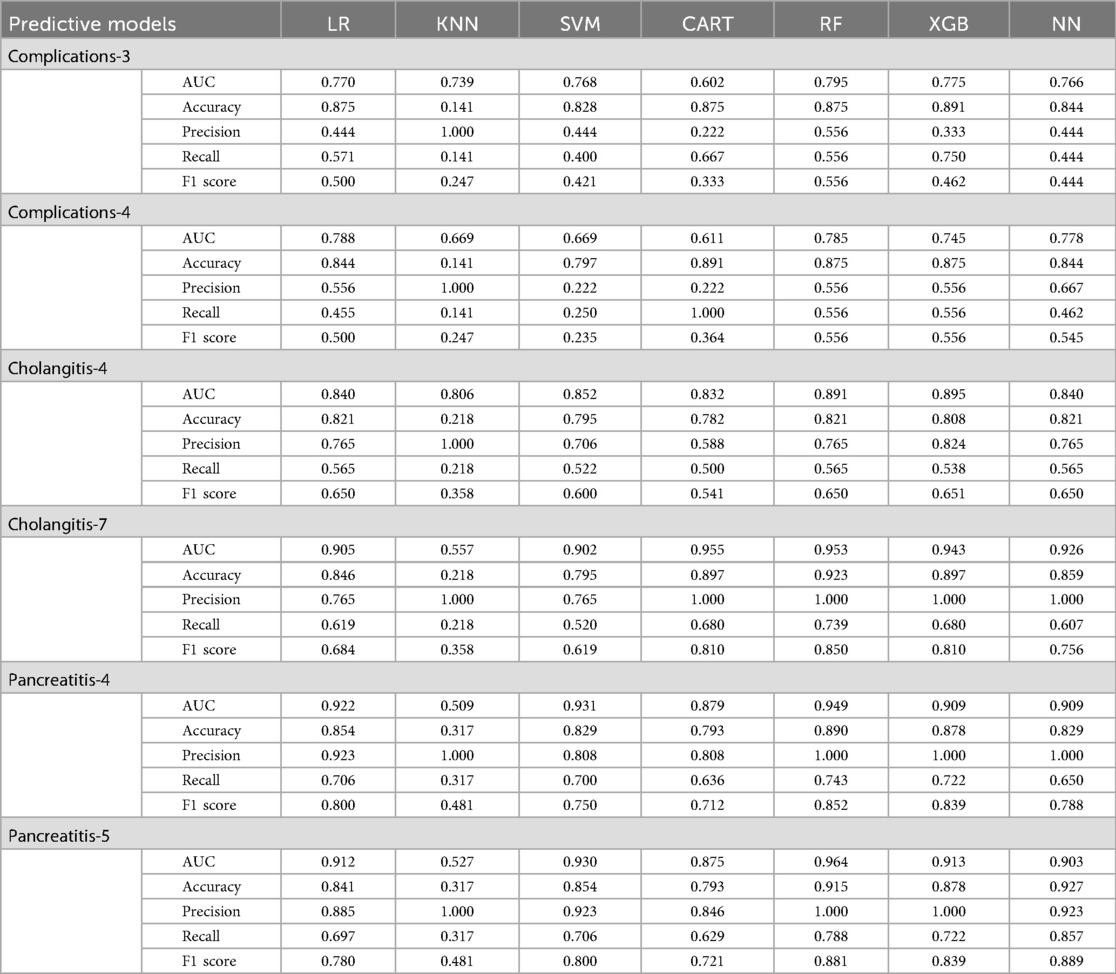
Logistic regression (LR), Support Vector Machine (SVM), K-nearest neighbours (KNN), Random Forest (RF), Extreme Gradient Boosting (XGB), Classification and Regression Tree (CART), and Neural Network (NN) were used to develop the prediction models respectively. All the developed models were compared using performance metrics including specificity, sensitivity (recall), accuracy, precision, receiver operating characteristics (ROC) and F1 statistics. Finally, the models with better performance were selected.
2.5 Statistical analyses
The SPSS 26.0 (IBM SPSS Statistics 26.0) and R software programs were used for statistical analysis. The normality of the distribution of continuous variables was assessed using the Shapiro–Wilk test. Normally distributed variables were compared using the t-test while the rank sum test was used for skewed variables. χ2 test was used to compare categorical variables. Univariate and multivariate logistic analyses were performed to identify variables affecting complications. ML algorithms were applied to determine the best predictive model. Statistical significance was defined as P < 0.05.
3 Results
3.1 Characteristics of the study population
A total of 211 patients (54 male; mean age: 3.39 years) were included in the final analysis. Of these, 31 patients experienced complications (cholangitis: 14 patients; pancreatitis: 21 patients). Besides, 4 patients developed calculus, 3 patients presented with intestinal obstruction, and 1 patient developed an anastomotic fistula. All the complications were resolved after treatment. Type-4A CBD was present in 59 patients. We randomly assigned the patients to the training and validation sets in a ratio of 7:3. The characteristics are summarized in Table 1.
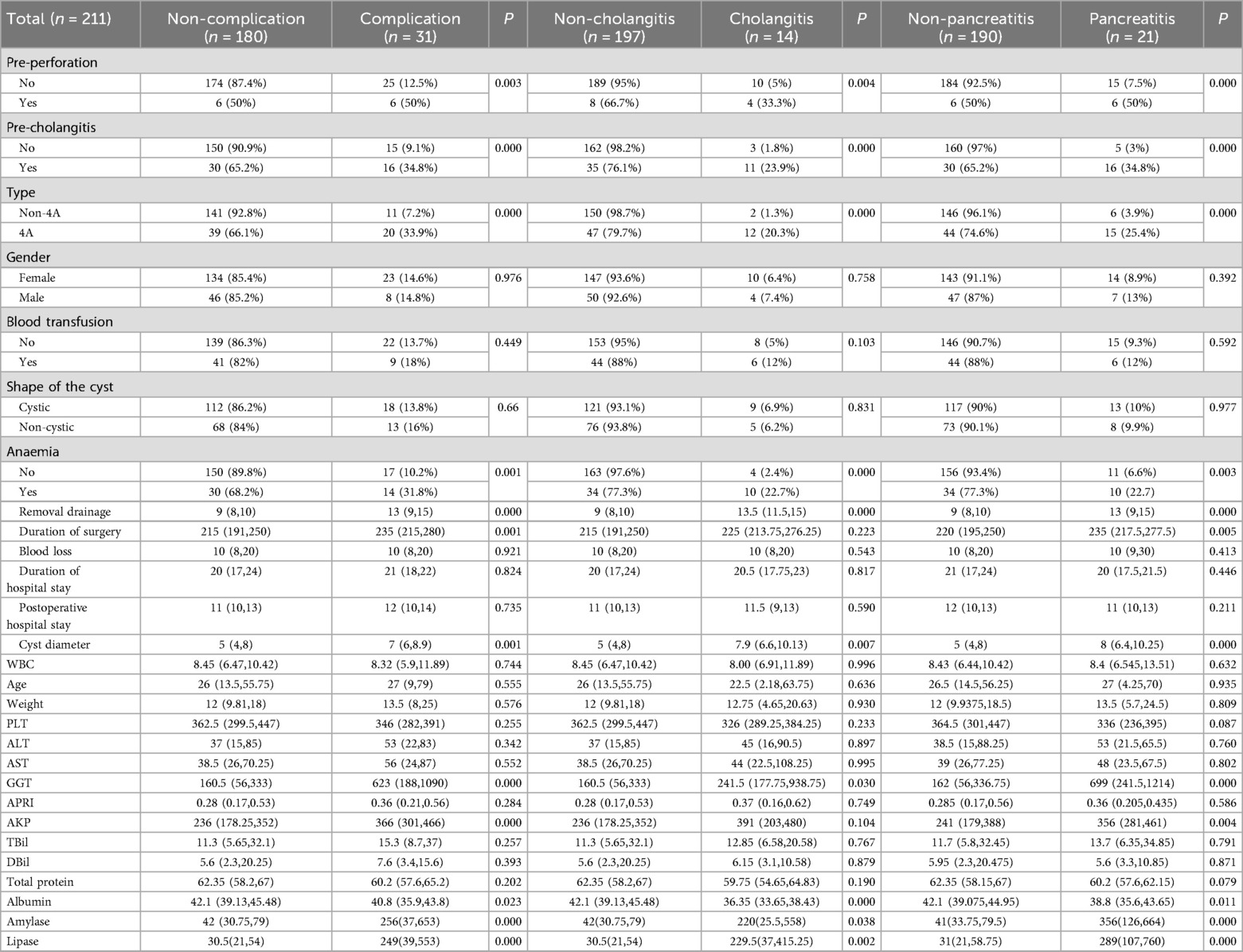
Table 1. Baseline characteristics of included patients stratified by complication, cholangitis and pancreatitis.
3.2 Variable selection
Multivariate analysis showed an association between pre-perforation (P = 0.02), type 4A (P = 0.034), removal drainage (P = 0.049), and serum amylase (P = 0.006) with the development of postoperative complications. Pre-perforation (P = 0.014), pre-cholangitis (P = 0.042), anemia (P = 0.026), and serum albumin (P = 0.033) were associated with post-cholangitis. Pre-perforation (P = 0.012), pre-cholangitis (P = 0.002), type 4A (P = 0.048), GGT (P = 0.015), and amylase (P = 0.025) were associated with post-pancreatitis. Patients with pre-perforation had a significantly higher incidence of overall postoperative complications, including cholangitis and pancreatitis. Patients with preoperative cholangitis had a significantly higher incidence of postoperative pancreatitis and cholangitis. Type 4A classification was significantly associated with an increased incidence of postoperative complications, particularly pancreatitis. Details are shown in Figure 1.
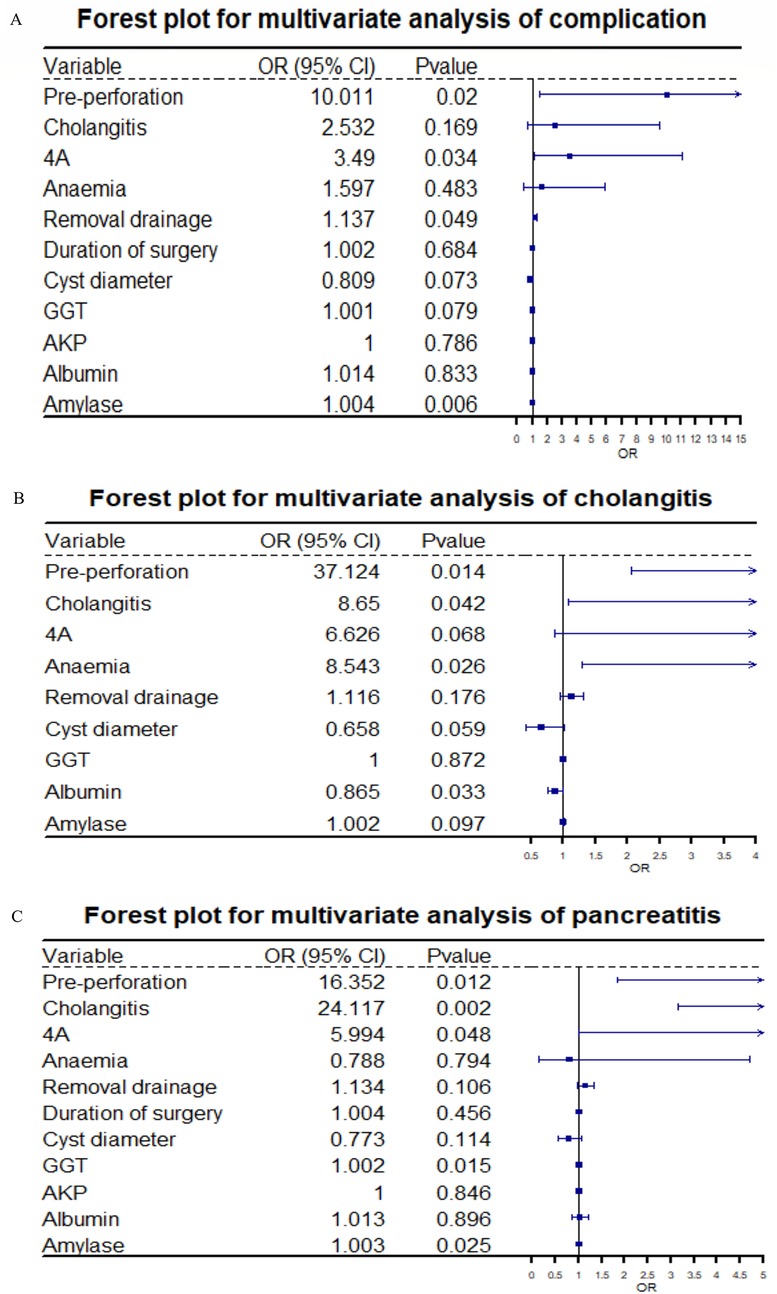
Figure 1. Panels A, B, and C respectively present the forest plots of multivariate logistic regression analysis results for total complications, cholangitis, and pancreatitis. On the far left of the figures are the variables included in the regression analysis; to the right of each variable are the corresponding results of the multivariate analysis, namely the odds ratio (OR) values and P-values.
A Lasso regression analysis was conducted on all variables. The results showed that the independent variables for complications, cholangitis, and pancreatitis decreased from 27 to 3 (removal drainage, GGT, amylase), 7 (pre-perforation, pre-cholangitis, type 4A, removal drainage, anemia, albumin, amylase), and 4 (pre-perforation, pre-cholangitis, GGT, amylase), respectively (Figure 2).
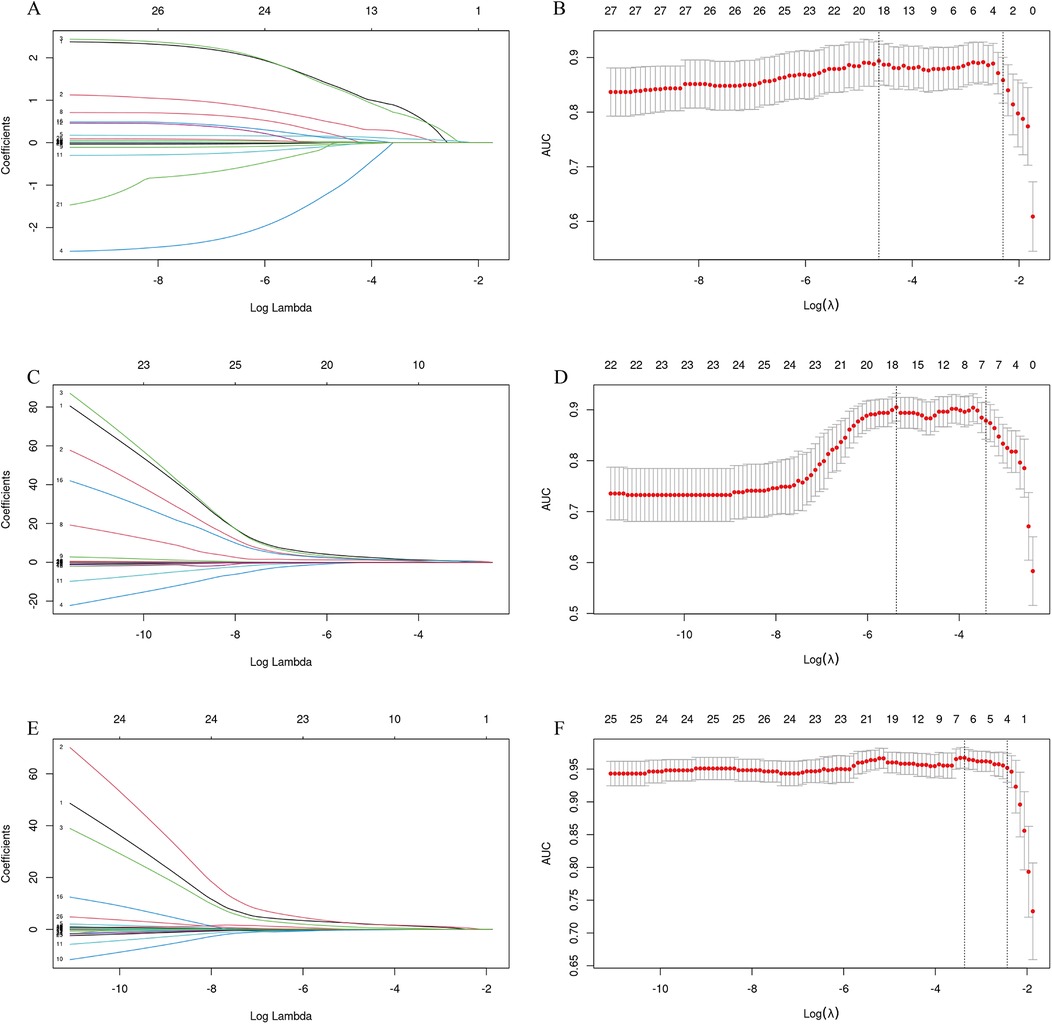
Figure 2. LASSO regression analysis was used to select risk factors. (A,C,E) The process of selecting the optimal value of the parameter λ in the Lasso regression model of complications, cholangitis and pancreatitis by the cross-validation method. The vertical dashed lines indicate the λ value corresponding to the minimum cross-validation error (left) and the λ value increased by one standard error (right). The minimum standard of complications includes removal drainage, GGT, amylase. Predictive minimum criteria for cholangitis includes pre-perforation, pre-cholangitis, type 4A, removal drainage, anemia, albumin, amylase. The minimum criteria for prediction of pancreatitis includes pre-perforation, pre-cholangitis, GGT, amylase. (B,D,F) The variable selection path of LASSO regression for complications, cholangitis and pancreatitis based on the optimal log λ, along with the corresponding coefficient changes at different λ values. Each colored line represents the coefficient of each feature.
Model construction was conducted using variables selected through lasso regression and multivariate analysis separately. The collinearity was assessed using the variance inflation factor (VIF). VIF > 5 was considered indicative of severe multicollinearity between variables. The results confirmed the lack of collinearity among the selected variables (Supplementary Tables S1–S3).
3.3 Model construction and comparison
We used seven ML algorithms to construct predictive models for the three outcomes. Multivariate-logistics and multivariate-neural networks had the highest area under the ROC curve for predicting complications.
The variables screened by Lasso regression for predicting cholangitis (seven variables) performed significantly better than the multivariate analysis. KNN had the smallest area under the ROC curve in the prediction model. All other models showed excellent performance.
The performance of the models constructed from the factors screened by multivariate analysis and lasso regression did not differ significantly, and we selected the model with fewer factors included (four factors) for convenience. LR, SVM, and RF performed better in predicting pancreatitis (Table 2).
To better interpret and apply the model, we used LR to predict the three outcomes and develop nomograms.
3.4 Development and verification of nomograms
Nomograms were developed to predict complications of cholangitis and pancreatitis, based on the screened independent risk factors (Figure 3). The calibration curves showed a high degree of consistency between the predicted and observed probabilities, demonstrating the high accuracy of the predictive models (Figure 4). Decision curve analysis was used to facilitate decision-making when evaluating the clinical applicability (Figure 5).
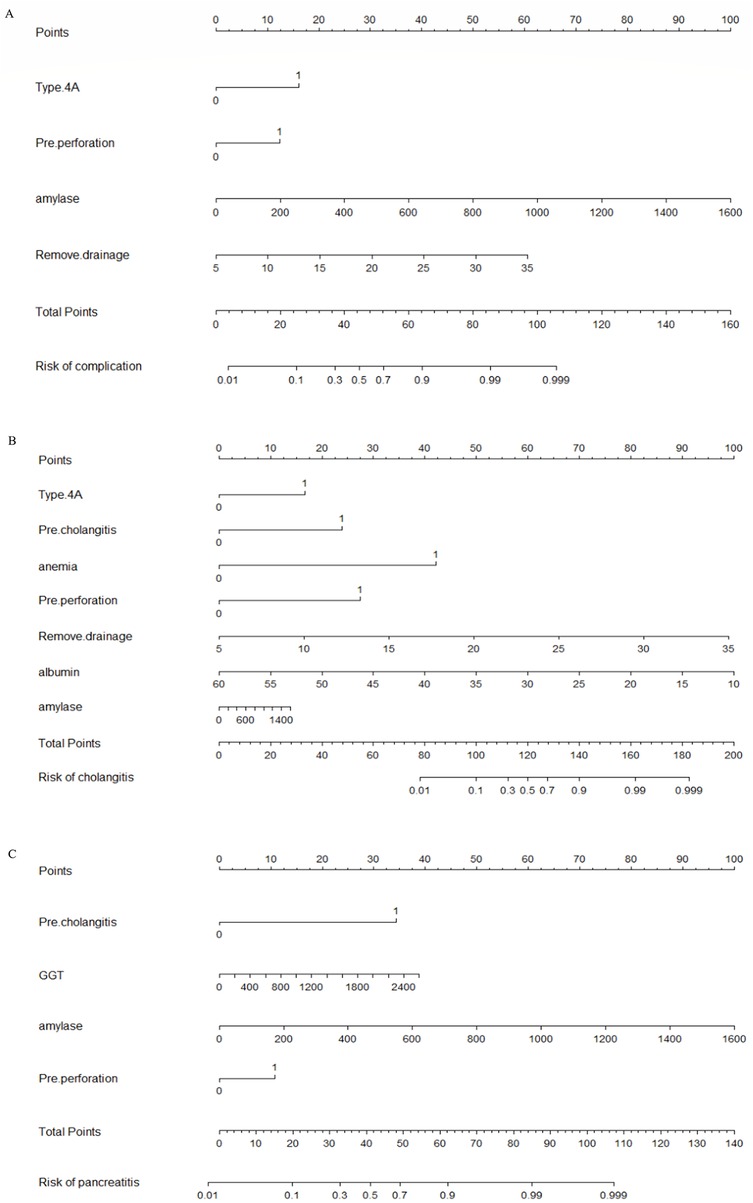
Figure 3. Nomogram for predicting postoperative complications in CBD. (A) Nomogram for predicting postoperative complications in CBD. The left column displays the scoring bar (at the top) and four parameters, each of which is scored with a vertical line to the scoring bar based on different parameter values. The total score is calculated, and a vertical line is drawn from the total score bar down to the “Risk of complications” section to obtain the probability of complications for the patient. (B) The nomogram for predicting postoperative cholangitis following CBD procedures. The leftmost column displays a scoring axis (top section) alongside seven predictive parameters. Each parameter is assigned a corresponding score via a vertical alignment to the top scoring bar, determined by its specific value. After calculating the total score, a vertical line is projected downward from the total score axis to the “Risk of cholangitis section”, thereby determining the patient's individualized probability of developing cholangitis. (C) Nomogram for predicting postoperative pancreatitis following CBD surgery. The leftmost column displays the scoring axis (top section) along with four predictive parameters. Each parameter connects vertically to the top scoring axis, with its corresponding score determined by its specific value. After calculating the total score, a vertical line is drawn downward from the total score axis to the “Risk of pancreatitis” area, thereby determining the individualized probability of the patient developing pancreatitis.
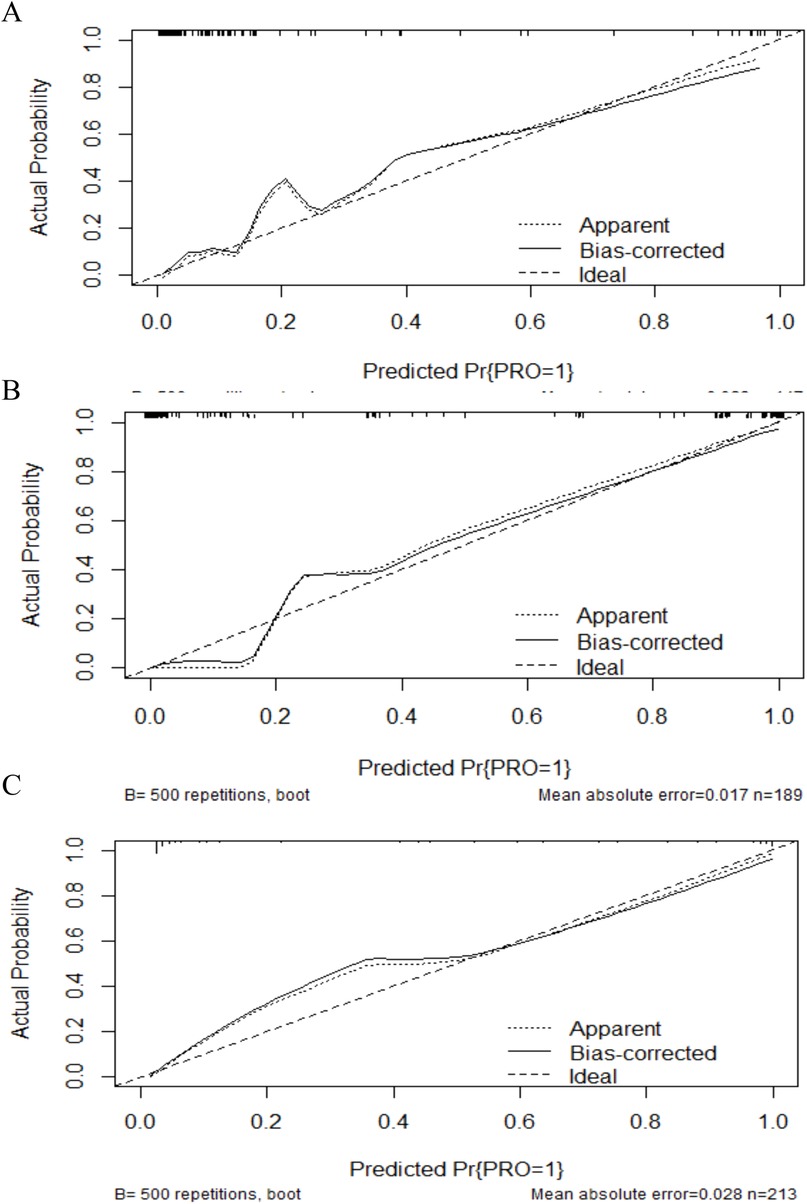
Figure 4. Calibration plot for predicting postoperative complications in CBD. (A) The calibration plot analysis result of complications. (B) The calibration plot analysis result of cholangitis. (C) The calibration plot analysis result of pancreatitis. The Y-axis scale represents the actual probability of complications, while the X-axis scale displays the predicted values calculated using the model. The dashed line indicates the fit between the original predicted values and the actual values, whereas the solid line represents the relationship between the calibrated predicted values and the actual values. Our predicted values show a high consistency with the observed values.
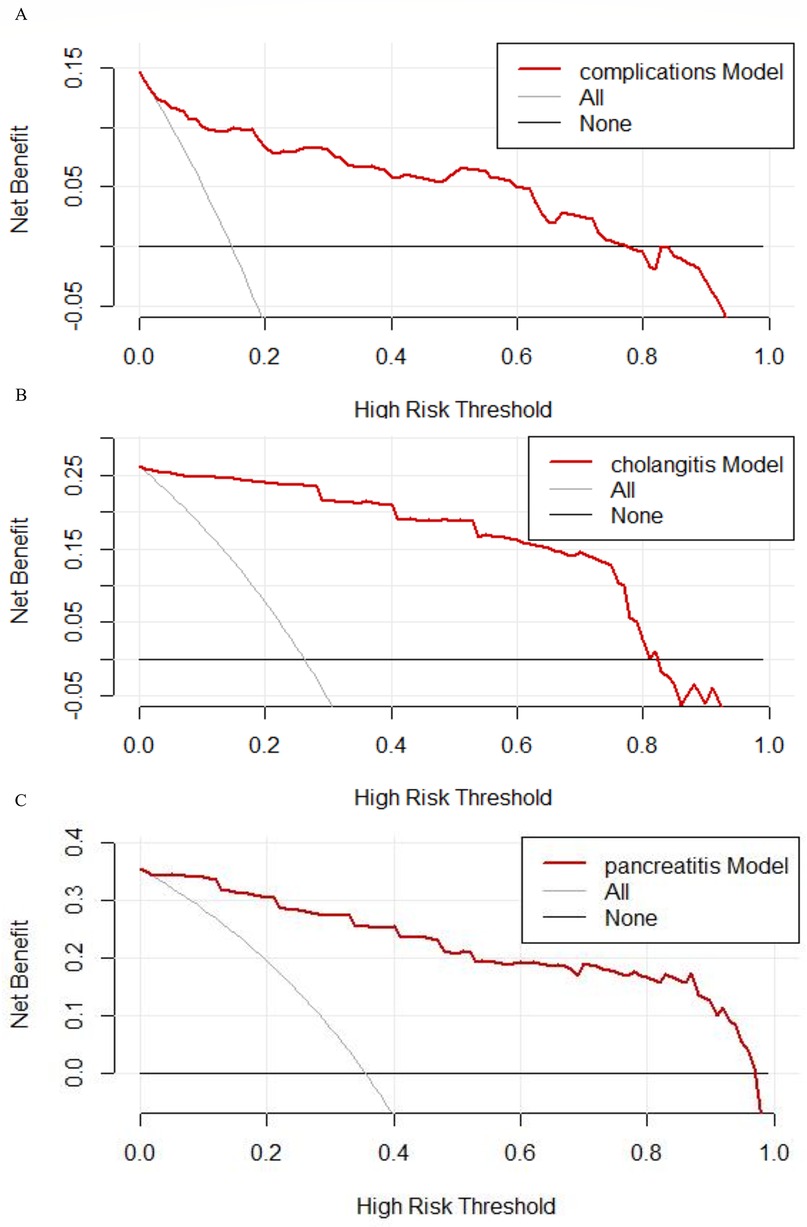
Figure 5. Decision curve for predicting postoperative complications in CBD. (A) The decision curve analysis result of complications. (B) The decision curve analysis result of cholangitis. (C) The decision curve analysis result of pancreatitis. The net benefit is calculated at different threshold probabilities. The black curve represents the scenario in which no interventions are implemented, while the gray curve represents the scenario in which interventions are applied to all patients.
4 Discussion
In this study, we analyzed the clinical data of 211 patients and used seven ML algorithms to develop predictive models for complications, cholangitis, and pancreatitis after CBD surgery. By comparison, LR showed superior clinical predictive values, with AUCs of 0.788, 0.905, and 0.922 for the prediction of complications, cholangitis, and pancreatitis, respectively, in the internal validation dataset. Additionally, we developed nomograms to facilitate the clinical application of the models.
CBD is a common structural abnormality of the bile ducts that may lead to complications such as bile duct stones, pancreatitis, biliary tract infections, and even bile duct cancer. The overall complication rate may reach 60%, while the cancer incidence may be as high as 26% in patients aged over 40 (12, 13). Therefore, research on the complications of CBD is imperative.
Our analysis revealed that preoperative perforation is a significant risk factor for postoperative complications, cholangitis, and pancreatitis. This finding highlights the critical warning value of preoperative perforation, indicating a greater severity of the disease. Notably, this association has not been highlighted in previous studies. The underlying mechanism may involve persistent local chronic inflammation following perforation, leading to significant adhesion formation (14). In previous studies, patients with perforations were younger and had significantly higher levels of GGT and C-reactive protein (CRP) (15–17). Patients with perforations also had higher WBCs and lower albumin levels (18). In our study, the incidence of complications and pancreatitis was higher in type-4A category, which is consistent with previous findings (19, 20). Extended duration of postoperative drainage days has been found to be associated with the development of postoperative complications. This may be attributable to the fact that prolonged time to drainage implies more localized exudation and severe inflammation.
Based on our study, patients identified as high-risk by the model (e.g., those with preoperative biliary perforation, Todani type 4A, or significant elevation of serum amylase) should undergo preoperative interventions. Specifically, modifiable factors (e.g., hypoalbuminemia, anemia) should be addressed through nutritional support—such as albumin supplementation and iron therapy—to enhance tissue healing capacity. Postoperatively, patients at high risk should be closely monitored for changes in the characteristics of drainage fluid, and individualized follow-up plans should also be established (e.g., closer follow-up and monitoring). Furthermore, priority should be given to early warning and intervention for severe complications. For example, in patients at high risk of cholangitis, prophylactic antibiotics should be administered postoperatively, and potential abnormalities (e.g., biliary stones) should be promptly addressed.
Some limitations of this study should be acknowledged. 1) This was a single-centre study with no external data validation. 2) Due to the limited follow-up duration, we did not find bile duct cancer during the follow-up period, which precluded prediction of bile duct cancers. We will continue to conduct longer follow-ups to obtain data on bile duct cancers. 3) The number of patients who experienced complications was limited, which remains a study limitation. Despite these shortcomings, there are many strengths of our study. This study is the first predictive model about postoperative complications, cholangitis, and pancreatitis after surgery for CBD. Additionally, we developed nomograms for clinical application.
5 Conclusion
We developed and validated a prediction model for postoperative complications of cholangitis and pancreatitis after surgery for CBD. Clinical application of the model can help prevent postoperative complications of CBD.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://data.mendeley.com/datasets/hxhkgwv2pv/1.
Ethics statement
The studies involving humans were approved by Scientific Research Ethics Committee of Qilu Hospital of Shandong University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
YZ: Writing – review & editing, Investigation, Software, Writing – original draft, Conceptualization, Visualization, Data curation, Formal analysis, Methodology. XZ: Visualization, Writing – review & editing, Conceptualization, Investigation, Methodology, Formal analysis, Writing – original draft, Data curation, Software. XR: Data curation, Investigation, Methodology, Writing – review & editing, Formal analysis, Visualization. DS: Investigation, Software, Writing – review & editing, Visualization, Formal analysis. JW: Investigation, Writing – review & editing, Software, Project administration, Formal analysis. AL: Funding acquisition, Conceptualization, Project administration, Methodology, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by Shandong University Qilu Hospital Development Fund (34641390220001).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2025.1654592/full#supplementary-material
References
1. Wang SE, Chen SC, Shyr BU, Shyr YM. Robotic assisted excision of type I choledochal cyst with Roux-en-y hepaticojejunostomy reconstruction. Hepatobiliary Surg Nutr. (2017) 6(6):397–400. doi: 10.21037/hbsn.2017.01.15
2. Hamada Y, Ando H, Kamisawa T, Itoi T, Urushihara N, Koshinaga T, et al. Diagnostic criteria for congenital biliary dilatation 2015. J Hepatobiliary Pancreat Sci. (2016) 23(6):342–6. doi: 10.1002/jhbp.346
3. Kamisawa T, Kaneko K, Itoi T, Ando H. Pancreaticobiliary maljunction and congenital biliary dilatation. Lancet Gastroenterol Hepatol. (2017) 2(8):610–8. doi: 10.1016/s2468-1253(17)30002-x
4. Kim NY, Chang EY, Hong YJ, Park S, Kim HY, Bai SJ, et al. Retrospective assessment of the validity of robotic surgery in comparison to open surgery for pediatric choledochal cyst. Yonsei Med J. (2015) 56(3):737–43. doi: 10.3349/ymj.2015.56.3.737
5. Jang JY, Yoon YS, Kang MJ, Kwon W, Park JW, Chang YR, et al. Laparoscopic excision of a choledochal cyst in 82 consecutive patients. Surg Endosc. (2013) 27(5):1648–52. doi: 10.1007/s00464-012-2646-0
6. Woo R, Le D, Albanese CT, Kim SS. Robot-assisted laparoscopic resection of a type I choledochal cyst in a child. J Laparoendosc Adv Surg Tech A. (2006) 16(2):179–83. doi: 10.1089/lap.2006.16.179
7. Metcalfe MS, Wemyss-Holden SA, Maddern GJ. Management dilemmas with choledochal cysts. Arch Surg. (2003) 138(3):333–9. doi: 10.1001/archsurg.138.3.333
8. Fujishiro J, Masumoto K, Urita Y, Shinkai T, Gotoh C. Pancreatic complications in pediatric choledochal cysts. J Pediatr Surg. (2013) 48(9):1897–902. doi: 10.1016/j.jpedsurg.2012.12.038
9. Tanaka Y, Tainaka T, Hinoki A, Shirota C, Sumida W, Yokota K, et al. Risk factors and outcomes of bile leak after laparoscopic surgery for congenital biliary dilatation. Pediatr Surg Int. (2021) 37(2):235–40. doi: 10.1007/s00383-020-04791-0
10. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. (2007) 370(9596):1453–7. doi: 10.1016/s0140-6736(07)61602-x
11. Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. (1977) 134(2):263–9. doi: 10.1016/0002-9610(77)90359-2
12. Dou J, Jiang N, Zeng J, Wang S, Tian S, Shan S, et al. Novel 3D morphological characteristics for congenital biliary dilatation diagnosis: a case-control study. Int J Surg. (2024) 110(5):2614–24. doi: 10.1097/js9.0000000000001204
13. Ishibashi H, Shimada M, Kamisawa T, Fujii H, Hamada Y, Kubota M, et al. Japanese Clinical practice guidelines for congenital biliary dilatation. J Hepatobiliary Pancreat Sci. (2017) 24(1):1–16. doi: 10.1002/jhbp.415
14. Kamisawa T, Ando H, Suyama M, Shimada M, Morine Y, Shimada H. Japanese Clinical practice guidelines for pancreaticobiliary maljunction. J Gastroenterol. (2012) 47(7):731–59. doi: 10.1007/s00535-012-0611-2
15. Zhang G, Wang H, Hu J, Yang C, Tan B, Hu J, et al. A nomogram for predicting choledochal cyst with perforaation. Pediatr Surg Int. (2024) 40(1):129. doi: 10.1007/s00383-024-05710-3
16. Fukuzawa H, Urushihara N, Miyakoshi C, Kajihara K, Kawahara I, Isono K, et al. Clinical features and risk factors of bile duct perforation associated with pediatric congenital biliary dilatation. Pediatr Surg Int. (2018) 34(10):1079–86. doi: 10.1007/s00383-018-4321-6
17. Zhang S, Cai D, Chen Q, Zhang Y, Chen K, Jin Y, et al. Value of serum GGT level in the timing of diagnosis of choledochal cyst perforation. Front Pediatr. (2022) 10:921853. doi: 10.3389/fped.2022.921853
18. Kim YJ, Kim SH, Yoo SY, Kim JH, Jung SM, Lee S, et al. Comparison of clinical and radiologic findings between perforated and non-perforated choledochal cysts in children. Korean J Radiol. (2022) 23(2):271–9. doi: 10.3348/kjr.2021.0169
19. Tanaka R, Nakamura H, Yoshimoto S, Okunobo T, Satake R, Doi T. Postoperative anastomotic stricture following excision of choledochal cyst: a systematic review and meta-analysis. Pediatr Surg Int. (2022) 39(1):30. doi: 10.1007/s00383-022-05293-x
Keywords: congenital biliary dilatation choledochal cyst, complications, machine learning, cholangitis, pancreatitis
Citation: Zhou Y, Zhang X, Ren X, Sun D, Wang J and Li A (2025) Nomograms for postoperative complications in congenital biliary dilatation: a retrospective cohort study. Front. Pediatr. 13:1654592. doi: 10.3389/fped.2025.1654592
Received: 26 June 2025; Accepted: 9 October 2025;
Published: 28 October 2025.
Edited by:
Qi Li, The First Affiliated Hospital of Xi'an Jiaotong University, ChinaReviewed by:
Mohammed Abu El-Hamd, Sohag University, EgyptKoshiro Sugita, Kagoshima University Hospital, Japan
Chiyoe Shirota, Nagoya University, Japan
Copyright: © 2025 Zhou, Zhang, Ren, Sun, Wang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aiwu Li, bGlhaXd1QHFpbHVob3NwaXRhbC5jb20=
†These authors have contributed equally to this work
 Yu Zhou
Yu Zhou Xintao Zhang
Xintao Zhang Xue Ren
Xue Ren Dong Sun
Dong Sun Jian Wang
Jian Wang Aiwu Li
Aiwu Li