- 1York Health Economics Consortium, University of York, York, UK
- 2Sackler Faculty of Medicine, Schneider Children's Medical Center, Institute of Gastroenterology, Nutrition and Liver Diseases, Tel-Aviv University, Tel-Aviv, Israel
- 3Department of Paediatrics, The Medical University of Warsaw, Warsaw, Poland
Background: The health effects of conventional yogurt have been investigated for over a century; however, few systematic reviews have been conducted to assess the extent of the health benefits of yogurt.
Objective: The aim of this scoping review was to assess the volume of available evidence on the health effects of conventional yogurt.
Methods: The review was guided by a protocol agreed a priori and informed by an extensive literature search conducted in November 2013. Randomized controlled trials were selected and categorized according to the eligibility criteria established in the protocol.
Results: 213 studies were identified as relevant to the scoping question. The number of eligible studies identified for each outcome were: bone health (14 studies), weight management and nutrition related health outcomes (81 studies), metabolic health (6 studies); cardiovascular health (57 studies); gastrointestinal health (24 studies); cancer (39 studies); diabetes (13 studies), Parkinson's disease risk (3 studies), all-cause mortality (3 studies), skin complaints (3 studies), respiratory complaints (3 studies), joint pain/function (2 studies); the remaining 8 studies reported a variety of other outcomes. For studies of a similar design and which assessed the same outcomes in similar population groups, we report the potential for the combining of data across studies in systematic reviews.
Conclusions: This scoping review has revealed the extensive evidence base for many outcomes which could be the focus of systematic reviews exploring the health effects of conventional yogurt consumption.
Introduction
Yogurt consumption has been associated with health and well-being for hundreds of years, but scientific research efforts on the potential health effects of conventional yogurt mainly started during the last century. Conventional yogurt contains a large quantity of nutrients essential for health and has relatively low calorie content, making it a high nutritional density product. In addition, the changes in milk constituents that occur during lactic acid fermentation influence the nutritional and physiological value of yogurt (Hewitt and Bancroft, 1985; Bianchi-Salvadori, 1986; Bourlioux and Pochart, 1988; Adolfsson et al., 2004). The efficacy of yogurt has been investigated in relation to a wide range of separate and overlapping outcomes including weight management (Burns et al., 1998), type 2 diabetes (O'Connor et al., 2014), cardiovascular disease risk (Buyuktuncer et al., 2013), bone health (Heaney et al., 2002), dental health (Telgi et al., 2013), the risk of various forms of cancer (Kurahashi et al., 2008), gastrointestinal (GI) health (Pashapour and Iou, 2006; Ballesta et al., 2008), lactose intolerance (Adibi et al., 2009), malnutrition (Sazawal et al., 2013), immunological parameters (Olivares et al., 2006), and overall mortality (Goldbohm et al., 2011). While a range of research designs have been employed to examine the health effects of yogurt, including observational studies (Cramer et al., 1989; Arslantas et al., 2008; Dawczynski and Jahreis, 2009) and experimental studies (Bonjour et al., 2013; Douglas et al., 2013), systematic reviews (and meta-analyses when appropriate) have been conducted in relation to only a few health outcomes (Tong et al., 2011; Aune et al., 2012, 2013; Soedamah-Muthu et al., 2012; Gao et al., 2013; O'sullivan et al., 2013).
The objective of this scoping review was to assess the volume of evidence for the health effects of yogurt consumption. The scoping review focused on conventional yogurt as defined by the Codex Alimentarius. The Codex Alimentarius Commission was established in the 1960s by the Food and Agriculture Organization of the United Nations (FAO) and the World Health Organization (WHO) and represents an international reference point for food safety and consumer protection (WHO, 2006). The standard for fermented milks (CODEX STAN 243-2003) (Codex Committee on Milk and Milk Products, 2010) defines yogurt as specifically characterized by the presence of the symbiotic starter cultures Streptococcus thermophilus and Lactobacillus delbrueckii subsp. bulgaricus (Codex Committee on Milk and Milk Products, 2010). Furthermore, it states that yogurt obtained through fermentation of milk by cultures of Streptococcus thermophilus and any other Lactobacillus species should be named through the use of an appropriate qualifier in conjunction with the word yogurt. This has commonly lead to the designation “probiotic yogurt” for fermented milk products containing a different micro-organism with a proven health benefit when taken in adequate amounts (WHO, 2001), and based on the rather widespread opinion that the conventional yogurt starter cultures should not be considered as probiotics.
This scoping review does not concern the tremendous amount of research findings on specific probiotic strains that has been generated during the past 20 years but concentrates on identifying the available evidence base on the generic health effects of conventional yogurt; an analysis undertaken as the first stage to inform potential future systematic reviews.
Methods
This scoping review was conducted using relevant methods of the systematic review process up to the point of data extraction. It is reported in accordance with the PRISMA reporting guidelines statement and checklist (Liberati et al., 2009) up to that point. The scoping review does not include the detailed data extraction, quality assessment and synthesis of a full systematic review, but is conducted with the aim of being objective, extensive and transparent. The scoping review was guided by a protocol (available for download from www.yhec.co.uk), which was agreed before the searches were conducted.
Studies considered eligible for the scoping review were epidemiological studies, cohort studies, open label studies and randomized controlled trials (RCTs). Case reports, letters, comments, and editorials were not eligible for inclusion. Eligible studies had to fulfill the requirement of examining the effect of oral consumption of conventional yogurt in the general population, in relation to a range of health outcomes, with a few specific exclusions. Studies that only examined the health effects of yogurt in the following situations were excluded: human populations with specific diseases; any animal population; in vitro studies and studies using technologies that simulate the stomach environment. We also excluded studies if they only assessed the yogurt interventions in relation to any of the following: fecal count outcomes; outcomes relating to stomach flora; overall assessments of diets where yogurt is only one factor and not reported separately; dental health, lactose intolerance; contagious diseases; treatment of infectious GI/respiratory tract diseases; studies reporting laboratory or immunological parameters only; inflammatory diseases; autoimmune diseases; eye diseases (e.g., age-related macular degeneration) and cataracts; vaginitis; or studies of yogurt interference with antibiotic uptake.
Studies investigating conventional yogurt as either a single intervention or in combination with any other non-probiotic substance were eligible for inclusion. Studies that compared conventional yogurt with any non-probiotic yogurt, any non-yogurt substance, or placebo were also eligible. Studies of yogurt supplemented with probiotics, fermented milk products, such as kefir and kumys, fermented baby formula, or milk were not eligible for the scoping review.
Data Sources and Search Strategy
An extensive literature search was conducted during November 2013 in a range of relevant databases to identify studies investigating the health effects of yogurt. The search was limited to conventional yogurt as defined by the Codex Alimentarius international food standards for fermented milks (CODEX STAN 243-2003) (Codex Committee on Milk and Milk Products, 2010).
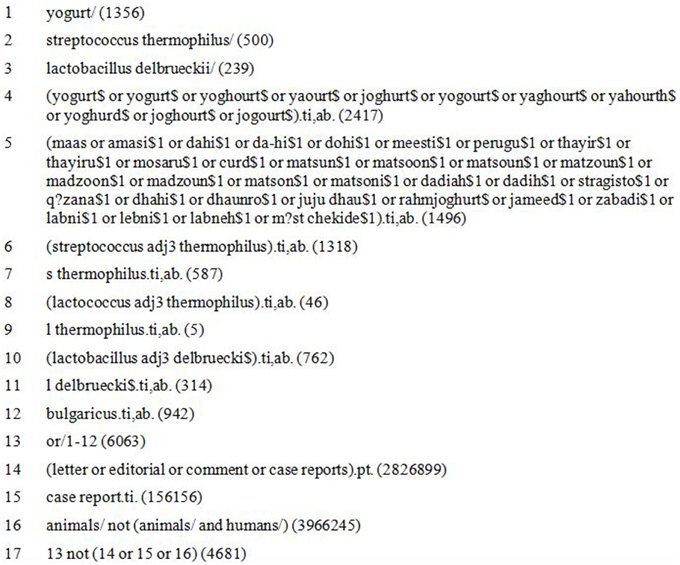
The full list of databases searched is included in Supplementary Table B. The searches were not limited by date or language. Information on ongoing or recently completed studies, unpublished research, and research reported in the gray literature was identified by searching selected major relevant conference proceedings from the past 3 years. Gray literature was identified via OAISTER, OpenGray and NTIS. The search strategy involved only search terms for conventional yogurts, including many synonyms used in different parts of the world for this traditional foodstuff, as shown in the Medline search strategy (Figure 1).
Reference lists of relevant reviews, trials and studies were used to identify any additional studies that might be eligible for inclusion.
Study Selection
Record selection was undertaken using several passes. The first pass was undertaken by one reviewer (SB) in order to rapidly remove obviously irrelevant records such as research undertaken in animals or case reports. Second pass record selection was undertaken by two reviewers (JE, SB) independently, using the title and abstract of records. The full text of included studies was then assessed for relevance by one of the authors (JE) and checked by a second independent reviewer (SB). Discrepancies were resolved through discussion and where necessary by consulting a third reviewer.
Data Extraction
One researcher (JE) extracted selected data from the full papers of each of the included studies using a standardized template into an Excel spreadsheet, and a second researcher (SB) checked the extraction. In the absence of full paper copies or when only abstracts were available, data were extracted from the abstracts alone. Details of the information extracted from the included studies are listed in Supplementary Table C.
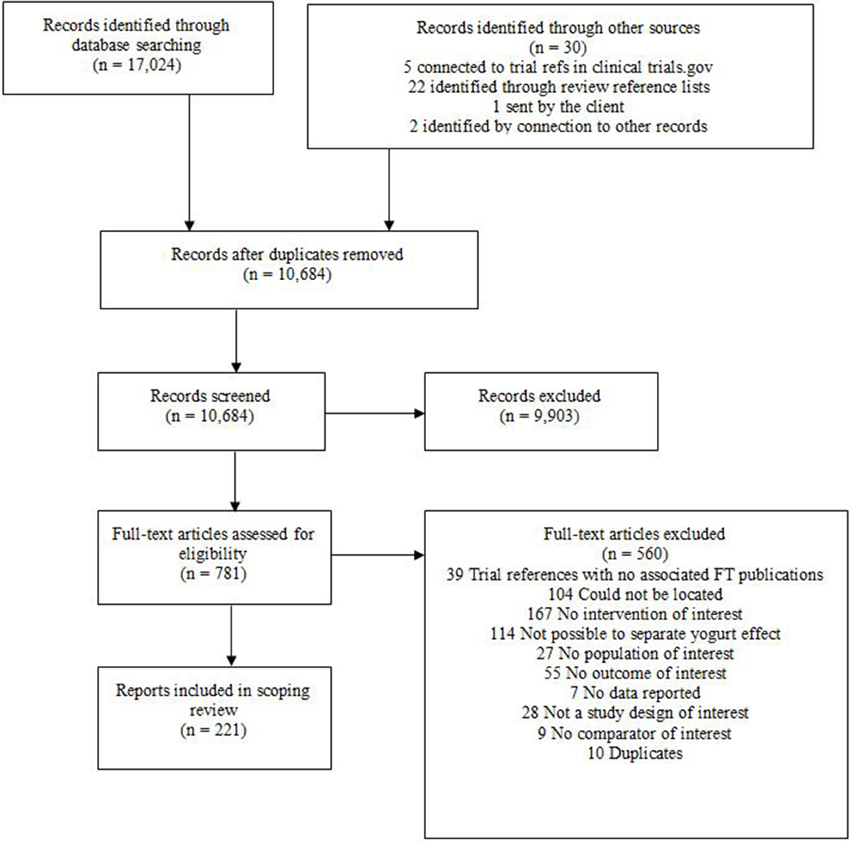
At the data extraction stage some studies, on closer inspection, proved ineligible. The number of records lost at this stage of the review process is documented in the PRISMA flow diagram (Figure 2).
Results
A total of 17,024 records were identified by the searches and an additional 30 records through other sources. After de-duplication 10,684 records were taken forward for title and abstract screening. A further 9,903 records were excluded by the second pass, leaving 781 records for full text assessment. Of these 560 were excluded in the third pass leaving a total of 221 eligible studies. The number of studies identified by the searches at the various selection stages is reported in a PRISMA study flow diagram (Figure 2). Of these, 213 studies were available with either an English abstract or English full text and are included in the categorization. Studies available only as abstracts were included in this scoping review, because there was generally sufficient information to suggest potential eligibility.
We grouped study designs into broad categories for the purpose of this report, to provide information on the type of study, rather than the internal quality of the study. Generally, the RCTs, cohort studies (not population-based cohort studies) and cross-over trials had small study sizes, with 100 participants or fewer entering the studies. Cross-sectional studies and population-based (or large hospital-based) cohort studies had the largest study numbers, ranging from hundreds to tens of thousands of participants being enrolled. Case-control and case-cohort studies generally involved numbers of participants in the hundreds or thousands.
Reported Outcomes
The outcomes reported in eligible studies were: bone health (14 studies) (Motegi et al., 2001; Heaney et al., 2002; Berberidis et al., 2004; Sorenson et al., 2004; Arslantas et al., 2008; Jha et al., 2010; Uenishi and Nakamura, 2010; Bener and El Ayoubi, 2012; Nasrollahi et al., 2012; Sahni et al., 2012, 2013a,b; Bonjour et al., 2013; Feart et al., 2013), weight management and nutrition-related health outcomes (81 studies) (Jordan et al., 1981; Thompson et al., 1982; Bazzarre et al., 1983; Massey, 1984; McNamara et al., 1989; Sullivan et al., 1989; Rolls et al., 1991, 1994, 1995; Trapp et al., 1993; Vandewater and Vickers, 1996; Oosthuizen et al., 1998; Campbell et al., 1999, 2000; Burns et al., 2000, 2001, 2002; Hoffman et al., 2000; Zandstra et al., 2000; Mensink et al., 2002; Mossavar-Rahmani et al., 2002; O'Donovan et al., 2003; Rodriguez-Artalejo et al., 2003; Chien et al., 2004; Sorenson et al., 2004; King et al., 2005; Rosado et al., 2005; Yae et al., 2005; Zemel et al., 2005; Logan et al., 2006; Nobre et al., 2006; Tsuchiya et al., 2006; Albertson et al., 2007; Dewan et al., 2007, 2009; Diepvens et al., 2007, 2008; Nazare et al., 2007; Snijder et al., 2007; Beydoun et al., 2008; Bonet Serra et al., 2008; Vergnaud et al., 2008; van der Zander et al., 2008; Almiron-Roig et al., 2009; Berkey et al., 2009; Jordão et al., 2009; White et al., 2009; Chapelot and Payen, 2010; Hursel et al., 2010; Keast et al., 2010, 2013; Lluch et al., 2010; Ortinau et al., 2010, 2012a,b, 2013; Pounis et al., 2010; Blom et al., 2011; Clegg et al., 2011; Jodkowska et al., 2011; Joshi et al., 2011; Margolis et al., 2011; Mozaffarian et al., 2011; Pordeus Luna et al., 2011; Schusdziarra et al., 2011; Smit et al., 2011; Thomas et al., 2011; Bener and El Ayoubi, 2012; Dougkas et al., 2012; Hogenkamp et al., 2012; Salakidou et al., 2012; Azadbakht et al., 2013; Buyuktuncer et al., 2013; Douglas et al., 2013; Meneton et al., 2013; Mensah and Otoo, 2013; Sazawal et al., 2013; Stritecka and Hlubik, 2013; Wang et al., 2013; Dawczynski et al., 2013; O'Connor et al., 2014), metabolic health (6 studies) (Snijder et al., 2007; Beydoun et al., 2008; Bonet Serra et al., 2008; White et al., 2009; Troy et al., 2010; Kim, 2013), cardiovascular health (57 studies) (Hepner et al., 1979; Rossouw et al., 1981; Thompson et al., 1982; Bazzarre et al., 1983; Jaspers et al., 1984; Massey, 1984; Cramer et al., 1989; McNamara et al., 1989; Sullivan et al., 1989; Freudenheim et al., 1991; Trapp et al., 1993; Oosthuizen et al., 1998; Iso et al., 1999; Mensink et al., 2002; Nakamura et al., 2002; Tavani et al., 2002; Steffen and Jacobs, 2003; Chien et al., 2004; Sorenson et al., 2004; Trautwein et al., 2004, 2005; Ganji and Kafai, 2004a,b; Steffen et al., 2005; Yae et al., 2005; Korpela et al., 2006; Rudkowska et al., 2007, 2008; Snijder et al., 2007; Bonet Serra et al., 2008; Masala et al., 2008; Niittynen et al., 2008; van der Zander et al., 2008; Wang et al., 2008, 2012, 2013; Dawczynski and Jahreis, 2009; Khandelwal et al., 2009; Larsson et al., 2009; Bonthuis et al., 2010; Sadrzadeh-Yeganeh et al., 2010; Clegg et al., 2011; Goldbohm et al., 2011; Ivey et al., 2011; Radler et al., 2011; Recio et al., 2011; Zhang et al., 2011; Amir Shaghaghi, 2012; Gouni-Berthold et al., 2012; Soedamah-Muthu et al., 2012; Azadbakht et al., 2013; Buyuktuncer et al., 2013; Javed et al., 2013; Kim, 2013; Meneton et al., 2013; Dawczynski et al., 2013), GI health (24 studies) (Niv et al., 1963; Dehesa et al., 1986; Porkka et al., 1988; Boudraa et al., 1989, 1990, 2001; Karabocuoglu et al., 1993; Trapp et al., 1993; Bhatnagar et al., 1998; Teuri and Korpela, 1998; Nakamura et al., 2000, 2001; Vazquez Martinez et al., 2005; Pashapour and Iou, 2006; Conway et al., 2007; Ranasinghe et al., 2007; Ballesta et al., 2008; Rafeey et al., 2008; Haenni et al., 2009; Pilipenko et al., 2009; Eren et al., 2010; Clegg et al., 2011; Frank et al., 2012; Isakov et al., 2013), cancer (39 studies) (Cook-Mozaffari et al., 1979; Le et al., 1986; Cramer et al., 1989; van't Veer et al., 1989; Peters et al., 1992; Kampman et al., 1994, 2000; Boutron et al., 1996; Shannon et al., 1996; Kocic et al., 1997; Ronco et al., 2002; Radosavljevic et al., 2003; Vlajinac et al., 2003; Juarranz Sanz et al., 2004; Kojima et al., 2004; Sakauchi et al., 2004; Sorenson et al., 2004; Kesse et al., 2005, 2006; Lin et al., 2005; Gallus et al., 2006; Genkinger et al., 2006; Mommers et al., 2006; Hsu et al., 2007; Janoutova et al., 2007; Matsumoto et al., 2007; Ornelas et al., 2007; Park et al., 2007; Heck et al., 2008; Kurahashi et al., 2008; Bonthuis et al., 2010; Karagianni et al., 2010; Djonovic and Arsenijevic, 2011; Pala et al., 2011; Faber et al., 2012; Kawakita et al., 2012; Reyhani et al., 2012; Duarte-Salles et al., 2013; Murphy et al., 2013), and diabetes (13 studies) (Nakamura et al., 2002; Sorenson et al., 2004; Choi et al., 2005; Liu et al., 2006; Kirii et al., 2009; Margolis et al., 2011; Dougkas et al., 2012; Sluijs et al., 2012; Soedamah-Muthu et al., 2012; Gheller et al., 2013; Grantham et al., 2013; Wang et al., 2013; O'Connor et al., 2014). Supplementary Tables D–J provide details of the studies identified in this scoping review for the outcomes of interest, presented in separate tables for each outcomecategory.
Twenty-two studies assessed other outcomes: Parkinson's disease risk (3 studies) (Chen et al., 2007; Miyake et al., 2011; Kyrozis et al., 2013), all-cause mortality (3 studies) (Bonthuis et al., 2010; Goldbohm et al., 2011; Soedamah-Muthu et al., 2012), skin complaints (3 studies) (Uenishi et al., 2004, 2008; Kim et al., 2010), respiratory complaints (3 studies) (Miyake et al., 2010, 2012; Maslova et al., 2012), joint pain/function (2 studies) (Martinez-Puig et al., 2013; Morina et al., 2013). The remaining 8 studies assessed a variety of other health outcomes: benign breast disease risk (Berkey et al., 2013), estrogen metabolism (Campbell et al., 1999), general mental/ psychological health (Crichton et al., 2010), minor health complaints (Hyland and Sodergren, 1998), immune function (Makino et al., 2010), general health (Mossavar-Rahmani et al., 2002), age of menarche (Ramezani Tehrani et al., 2013), and allergic symptoms (Trapp et al., 1993). Details of these studies are included in Supplementary Table K.
RCTs made up a large proportion of the weight management and nutritional health (23%), cardiovascular health (26%) and GI health studies (33%). Cross-sectional studies made up a large proportion of the weight management and nutritional health (18%), cardiovascular health (18%), metabolic health (50%) and bone health (50%) studies. Cohort studies made up a large proportion of the cancer (21%), cardiovascular health (26%), GI health (29%), other (41%), and diabetes (46%) studies. Cross-over trials were a common study design for cardiovascular health (19%) and weight management and nutritional (40%) health studies. Case-control and case-cohort studies were generally less common, although case-control studies were the most common study design in the cancer studies (59%) group.
We identified which studies might be similar enough to be suitable for combination in meta-analyses; details are included in Supplementary Table A.
Discussion
Our scoping review shows that there is a substantial evidence base for investigating the health effects of conventional yogurt and that this evidence base is largest around weight management and nutrition-related health outcomes, cardiovascular health, GI health and cancer.
In principle, a systematic review with a narrative (textual) synthesis can be undertaken for outcomes with no evidence or little evidence, but when there is a larger evidence base there is greater opportunity for more robust assessments of effects. We suggest there are opportunities for meta-analyses among this evidence base where we have found studies that seem to be of similar design, investigating similar interventions and populations, and using the same outcome measures. The study population size is important, due to the inability to achieve significant results with small sample size.
Our results provide a useful evidence base for those interested in developing future nutritional interventions with conventional yogurt. Researchers planning new studies should ideally design them in the light of well-conducted systematic reviews (Al-Shahi Salman et al., 2014). This evidence base provides information which can both inform study design and provide the information for such systematic reviews. Based on this scoping review, three systematic reviews have already been undertaken: two of these included meta-analyses on the role of conventional yogurt in GI health in children (Patro-Golab et al., 2015a,b), and the third is ongoing and examines the effect of conventional yogurt on weight management outcomes.
Limitations of this Scoping Review
Studies only available as abstracts (e.g., conference abstracts) were included in this scoping review. Many of these studies would require further information from study authors to confirm their full eligibility to contribute to individual systematic review questions.
Some studies, particularly those by the same author(s) may contain the same, or part of the same, populations. As part of a full systematic review, duplicated or partly duplicated study populations would be identified and not pseudoreplicated. Because a scoping review involves only a high-level overview of study characteristics, we could not identify such duplicated populations with certainty, so there may exist a low degree of double counting in this scoping review.
Due to the limited level of data extraction undertaken in a scoping review, the assessment of the potential for combining studies in a meta-analysis must come with the caveat that some studies, especially those for which full study details were not available or reported may not, following assessment of the full study details, be eligible for meta-analysis. We highlight the need to contact authors where there is a lack of clarity about the eligibility of studies with respect to the design, population, intervention, comparator and/or outcomes. This scoping review did not assess the quality of eligible studies. In a full systematic review, the impact of including studies that are categorized with a high risk of bias may be explored in the meta-analyses via subgroup analyses.
The searches were conducted in November 2013. The volume of studies was such that processing took much longer than expected. However, the full strategies are presented in the supplementary files and this should make updating the scoping review relatively straightforward.
Conclusion
This scoping review identified a number of outcomes for which there exists substantial primary evidence that may be suitable for systematic review and potentially meta-analysis. Future systematic reviews of selected outcomes may provide further evidence for the health effects of yogurt consumption. Our results provide a useful evidence base for those interested in developing future nutritional interventions with conventional yogurt.
Author Contributions
RS developed the idea for the study; JG designed the research. JE, JG, and SB conducted the research; JE and JG analyzed data. SB, JE, and JG co-wrote the report and the paper, with comments and edits from RS and HS. All authors take responsibility for final content. All authors read and approved the final manuscript.
Conflict of Interest Statement
YHEC was commissioned to conduct the scoping review with funding provided by Danone Institute International. Danone Institute International had no role in the design, analysis or writing of this article. RS has participated as a clinical investigator, or advisory board member, or consultant or speaker for Abbott, Danone, Enzymotec, Ferrero, Nestle Nutrition Institute, Nutricia and Teva. HS has received funding from Danone Institute International. YHEC (JG, JE, SB) has received funding from Danone Institute International to conduct this scoping review.
Acknowledgments
YHEC was commissioned to conduct the scoping review with funding provided by Danone Institute International. Prof. Irene Lenoir-Wijnkoop, Public Health Nutrition, Faculty of Sciences, Utrecht University, The Netherlands gave peer review comments on this manuscript. In preparation of this manuscript, editorial assistance was provided by Lisa Buttle PhD, of Chill Pill Media LLP. Project assistance was also provided by Mary Edwards, York Health Economics Consortium.
Supplementary Material
The Supplementary Material for this article can be found online at: http://journal.frontiersin.org/article/10.3389/fphar.2015.00246
Abbreviations
GI, gastrointestinal; RCT, randomized controlled trial.
References
Adibi, P., Mirshahzadeh, P., and Sadeghizadeh, A. (2009). Dairy intolerance syndrome in Iranian young adult. J. Res. Med. Sci. 14, 357–366.
Adolfsson, O., Meydani, S. N., and Russell, R. M. (2004). Yogurt and gut function. Am. J. Clin. Nutr. 80, 245–256.
Albertson, A. M., Holschuh, N. M., and Eldridge, A. L. (2007). Yogurt consumption in the United States: effect on nutrient intakes and body measures in adults 19+ years. FASEB J. 21, A1061.
Almiron-Roig, E., Grathwohl, D., Green, H., and Erkner, A. (2009). Impact of some isoenergetic snacks on satiety and next meal intake in healthy adults. J. Hum. Nutr. Diet. 22, 469–474. doi: 10.1111/j.1365-277X.2009.00978.x
Al-Shahi Salman, R., Beller, E., Kagan, J., Hemminki, E., Phillips, R. S., Savulescu, J., et al. (2014). Increasing value and reducing waste in biomedical research regulation and management. Lancet 383, 176–185. doi: 10.1016/S0140-6736(13)62297-7
Amir Shaghaghi, M. (2012). Evaluation of the Lipid-lowering Efficacy of a Water Dispersible Formulation of Free Sterols Versus Plant Sterol Esters in Humans Consuming a Supplemented Dairy Product [thesis]. Winnipeg: University of Manitoba.
Arslantas, D., Metintas, S., Unsal, A., Isikli, B., Kalyoncu, C., and Arslantas, A. (2008). Prevalence of osteoporosis in middle Anatolian population using calcaneal ultrasonography method. Maturitas 59, 234–241. doi: 10.1016/j.maturitas.2008.01.007
Aune, D., Lau, R., Chan, D. S. M., Vieira, R., Greenwood, D. C., Kampman, E., et al. (2012). Dairy products and colorectal cancer risk: a systematic review and meta-analysis of cohort studies. Ann. Oncol. 23, 37–45. doi: 10.1093/annonc/mdr269
Aune, D., Norat, T., Romundstad, P., and Vatten, L. J. (2013). Dairy products and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Am. J. Clin. Nutr. 98, 1066–1083. doi: 10.3945/ajcn.113.059030
Azadbakht, L., Haghighatdoost, F., Karimi, G., and Esmaillzadeh, A. (2013). Effect of consuming salad and yogurt as preload on body weight management and cardiovascular risk factors: a randomized clinical trial. Int. J. Food Sci. Nutr. 64, 392–399. doi: 10.3109/09637486.2012.753039
Ballesta, S., Velasco, C., Borobio, M. V., Argüelles, F., and Perea, E. J. (2008). [Fresh versus pasteurized yogurt: comparative study of the effects on microbiological and immunological parameters, and gastrointestinal comfort]. Enferm. Infecc. Microbiol. Clin. 26, 552–557. doi: 10.1157/13128271
Bazzarre, T. L., Wu, S.-M. L., and Yuhas, J. A. (1983). Total and High Density Lipo Protein Cholesterol Concentrations Following Yoghurt and Calcium Supplementation. Nutr. Rep. Int. 28, 1225–1232.
Bener, A., and El Ayoubi, H. R. (2012). The role of vitamin D deficiency and osteoporosis in breast cancer. Int. J. Rheum. Dis. 15, 554–561. doi: 10.1111/1756-185x.12017
Berberidis, C., Potoupnis, M., Sakellariou, G., Sapakos, J., Manologlou, K., and Goulios, A. (2004). Epidemiology study about risk factors for low bone density in old greek men and women. Calcif. Tissue Int. 74(Suppl. 1):S66.
Berkey, C. S., Colditz, G. A., Rockett, H. R., Frazier, A. L., and Willett, W. C. (2009). Dairy consumption and female height growth: prospective cohort study. Cancer Epidemiol. Biomarkers Prev. 18, 1881–1887. doi: 10.1158/1055-9965.EPI-08-1163
Berkey, C. S., Willett, W. C., Tamimi, R. M., Rosner, B., Frazier, A. L., and Colditz, G. A. (2013). Dairy intakes in older girls and risk of benign breast disease in young women. Cancer Epidemiol. Biomarkers Prev. 22, 670–674. doi: 10.1158/1055-9965.EPI-12-1133
Beydoun, M. A., Gary, T. L., Caballero, B. H., Lawrence, R. S., Cheskin, L. J., and Wang, Y. (2008). Ethnic differences in dairy and related nutrient consumption among US adults and their association with obesity, central obesity, and the metabolic syndrome. Am. J. Clin. Nutr. 87, 1914–1925.
Bhatnagar, S., Singh, K. D., Sazawal, S., Saxena, S. K., and Bhan, M. K. (1998). Efficacy of milk versus yogurt offered as part of a mixed diet in acute noncholera diarrhea among malnourished children. J. Pediatr. 132, 999–1003. doi: 10.1016/S0022-3476(98)70398-1
Bianchi-Salvadori, B. (1986). Intestinal microflora: the role of yogurt in the equilibrium of the gut ecosystem. Int. J. Immunothe. 3(Suppl. II), 9–18.
Blom, W. A., Abrahamse, S. L., Bradford, R., Duchateau, G. S., Theis, W., Orsi, A., et al. (2011). Effects of 15-d repeated consumption of Hoodia gordonii purified extract on safety, ad libitum energy intake, and body weight in healthy, overweight women: a randomized controlled trial. Am. J. Clin. Nutr. 94, 1171–1181. doi: 10.3945/ajcn.111.020321
Bonet Serra, B., Quintanar Rioja, A., Viana Arribas, M., Iglesias-Gutierrez, E., and Varela-Moreiras, G. (2008). The effects of yogurt with isomer enriched conjugated linoleic acid on insulin resistance in obese adolescents. [Spanish] Efectos del yogur enriquecido con isomeros del acido linoleico conjugado, sobre resistencia a la insulina en adolescentes obesos. Rev. Esp. Pediatr. 64, 94–100.
Bonjour, J. P., Benoit, V., Payen, F., and Kraenzlin, M. (2013). Consumption of yogurts fortified in vitamin D and calcium reduces serum parathyroid hormone and markers of bone resorption: a double-blind randomized controlled trial in institutionalized elderly women. J. Clin. Endocrinol. Metab. 98, 2915–2921. doi: 10.1210/jc.2013-1274
Bonthuis, M., Hughes, M. C., Ibiebele, T. I., Green, A. C., and van der Pols, J. C. (2010). Dairy consumption and patterns of mortality of Australian adults. Eur. J. Clin. Nutr. 64, 569–577. doi: 10.1038/ejcn.2010.45
Boudraa, G., Benbouabdellah, M., Hachelaf, W., Boisset, M., Desjeux, J. F., and Touhami, M. (2001). Effect of feeding yogurt versus milk in children with acute diarrhea and carbohydrate malabsorption. J. Pediatr. Gastroenterol. Nutr. 33, 307–313. doi: 10.1097/00005176-200109000-00015
Boudraa, G., Touhami, M., Pochart, P., Soltana, R., Mary, J. Y., and Desjeux, J. F. (1989). Comparative effects of yogurt and milk on persistant diarrhea in early-childhood - preliminary-results [from the International Conference on Fermented Milk, Paris, Dec 14-16, 1989]. Fermented Milks 229–232.
Boudraa, G., Touhami, M., Pochart, P., Soltana, R., Mary, J. Y., and Desjeux, J. F. (1990). Effect of feeding yogurt versus milk in children with persistent diarrhea. J. Pediatr. Gastroenterol. Nutr. 11, 509–512. doi: 10.1097/00005176-199011000-00011
Bourlioux, P., and Pochart, P. (1988). Nutritional and health properties of yogurt. World Rev. Nutr. Diet. 56, 217–258. doi: 10.1159/000416229
Boutron, M. C., Faivre, J., Marteau, P., Couillault, C., Senesse, P., and Quipourt, V. (1996). Calcium, phosphorus, vitamin, D., dairy products and colorectal carcinogenesis: a French case-control study. Br. J. Cancer 74, 145–151. doi: 10.1038/bjc.1996.330
Burns, A. A., Lindmark, L., Livingstone, M. B. E., Mullaney, U., Rowland, I., and Welch, R. W. (1998). Consumption of yoghurt containing modified fat increases satiety and reduces subsequent food intake. Proc. Nutr. Soc. 57, 121a.
Burns, A. A., Livingstone, M. B. E., Welch, R. W., Dunne, A., and Rowland, I. R. (2002). Dose-response effects of a novel fat emulsion (Olibra (TM))on energy and macronutrient intakes up to 36 h post-consumption. Eur. J. Clin. Nutr. 56, 368–377. doi: 10.1038/sj.ejcn.1601326
Burns, A. A., Livingstone, M. B., Welch, R. W., Dunne, A., Reid, C. A., and Rowland, I. R. (2001). The effects of yoghurt containing a novel fat emulsion on energy and macronutrient intakes in non-overweight, overweight and obese subjects. Int. J. Obes. Relat. Metab. Disord. 25, 1487–1496. doi: 10.1038/sj.ijo.0801720
Burns, A. A., Livingstone, M. B., Welch, R. W., Dunne, A., Robson, P. J., Lindmark, L., et al. (2000). Short-term effects of yoghurt containing a novel fat emulsion on energy and macronutrient intakes in non-obese subjects. Int. J. Obes. Relat. Metab. Disord. 24, 1419–1425. doi: 10.1038/sj.ijo.0801430
Buyuktuncer, Z., Fisunoglu, M., Guven, G. S., Unal, S., and Besler, H. T. (2013). The cholesterol lowering efficacy of plant stanol ester yoghurt in a Turkish population: a double-blind, placebo-controlled trial. Lipids Health Dis. 12:91. doi: 10.1186/1476-511X-12-91
Campbell, C. G., Chew, B. P., Luedecke, L. O., and Shultz, T. D. (2000). Yogurt consumption does not enhance immune function in healthy premenopausal women. Nutr. Cancer 37, 27–35. doi: 10.1207/S15327914NC3701_3
Campbell, C. G., Luedecke, L. O., and Shultz, T. D. (1999). Yogurt consumption and estrogen metabolism in healthy premenopausal women. Nutr. Res. 19, 531–543. doi: 10.1016/S0271-5317(99)00019-6
Chapelot, D., and Payen, F. (2010). Comparison of the effects of a liquid yogurt and chocolate bars on satiety: a multidimensional approach. Br. J. Nutr. 103, 760–767. doi: 10.1017/S000711450999225X
Chen, H., O'Reilly, E., McCullough, M. L., Rodriguez, C., Schwarzschild, M. A., Calle, E. E., et al. (2007). Consumption of dairy products and risk of parkinson's disease. Am. J. Epidemiol. 165, 998–1006. doi: 10.1093/aje/kwk089
Chien, Y. W., Liao, F. H., Chen, S. J., Chen, Y. F., Chen, C. F., and Shieh, M. J. (2004). Effectiveness of weight loss by using yogurt commercial meals. Nutr. Sci. J. 29, 222–229.
Choi, H. K., Liu, S., and Curhan, G. (2005). Intake of purine-rich foods, protein, and dairy products and relationship to serum levels of uric acid: the Third National Health and Nutrition Examination Survey. Arthritis Rheum. 52, 283–289. doi: 10.1002/art.20761
Clegg, M. E., McKenna, P., McClean, C., Davison, G. W., Trinick, T., Duly, E., et al. (2011). Gastrointestinal transit, post-prandial lipaemia and satiety following 3 days high-fat diet in men. Eur. J. Clin. Nutr. 65, 240–246. doi: 10.1038/ejcn.2010.235
Codex Committee on Milk Milk Products. (2010). Codex Standard for Fermented Milks (CODEX STAN 243-2003). New Zealand: Codex Alimentarius.
Conway, S., Hart, A., Clark, A., and Harvey, I. (2007). Does eating yogurt prevent antibioticmassociated diarrhoea? A placebo-controlled randomised controlled trial in general practice. Br. J. Gen. Pract. 57, 953–959. doi: 10.3399/096016407782604811
Cook-Mozaffari, P. J., Azordegan, F., Day, N. E., Ressicaud, A., Sabai, C., and Aramesh, B. (1979). Esophageal Cancer Studies in the Caspian Littoral of Iran Results of a Case Control Study. Br. J. Cancer 39, 293–309. doi: 10.1038/bjc.1979.54
Cramer, D. W., Harlow, B. L., Willett, W. C., Welch, W. R., Bell, D. A., Scully, R. E., et al. (1989). Galactose consumption and metabolism in relation to the risk of ovarian cancer. Lancet 2, 66–71. doi: 10.1016/S0140-6736(89)90313-9
Crichton, G. E., Murphy, K. J., and Bryan, J. (2010). Dairy intake and cognitive health in middle-aged South Australians. Asia Pac. J. Clin. Nutr. 19, 161–171.
Dawczynski, C., and Jahreis, G. (2009). Prevention of cardiovascular diseases with milk products supplemented with long-chain omega-3-fatty acids. Ernahrungs-Umschau 56, 618–625.
Dawczynski, C., Massey, K. A., Ness, C., Kiehntopf, M., Stepanow, S., Platzer, M., et al. (2013). Randomized placebo-controlled intervention with n-3 LC-PUFA-supplemented yoghurt: effects on circulating eicosanoids and cardiovascular risk factors. Clin. Nutr. 32, 686–696. doi: 10.1016/j.clnu.2012.12.010
Dehesa, A., García, I. C., Castañeda, C., Fragoso, T., Sagaró, E., and Soler, J. (1986). Yogurt as therapy in chronic diarrhea by giardiasis. Rev. Cubana Pediatr. 58, 198–205.
Dewan, P., Kaur, I., Chattopadhya, D., A Faridi, M. M., and Agarwal, K. N. (2007). A pilot study on the effects of curd (dahi) and leaf protein concentrate in children with protein energy malnutrition (PEM). Indian J. Med. Res. 126, 199–203.
Dewan, P., Kaur, I. R., Faridi, M. M., and Agarwal, K. N. (2009). Cytokine response to dietary rehabilitation with curd (Indian dahi) and leaf protein concentrate in malnourished children. Indian J. Med. Res. 130, 31–36.
Diepvens, K., Soenen, S., Steijns, J., Arnold, M., and Westerterp-Plantenga, M. (2007). Long-term effects of consumption of a novel fat emulsion in relation to body-weight management. Int. J. Obes. 31, 942–949. doi: 10.1038/sj.ijo.0803532
Diepvens, K., Steijns, J., Zuurendonk, P., and Westerterp-Plantenga, M. S. (2008). Short-term effects of a novel fat emulsion on appetite and food intake. Physiol. Behav. 95, 114–117. doi: 10.1016/j.physbeh.2008.05.006
Djonovic, N. D. J., and Arsenijevic, S. A. (2011). Nutrition, obesitas and larynx cancer. Obes. Rev. 12:251. doi: 10.1111/j.1467-789X.2011.00889.x
Dougkas, A., Minihane, A. M., Givens, D. I., Reynolds, C. K., and Yaqoob, P. (2012). Differential effects of dairy snacks on appetite, but not overall energy intake. Br. J. Nutr. 108, 2274–2285. doi: 10.1017/S0007114512000323
Douglas, S. M., Ortinau, L. C., Hoertel, H. A., and Leidy, H. J. (2013). Low, moderate, or high protein yogurt snacks on appetite control and subsequent eating in healthy women. Appetite 60, 117–122. doi: 10.1016/j.appet.2012.09.012
Duarte-Salles, T., Fedirko, V., Trichopoulou, A., Bamia, C., Romieu, I., and Jenab, M. (2013). Dairy products, calcium and risk of hepatocellular carcinoma in the European prospective investigation into cancer and nutrition (EPIC) Study. J. Hepatol. 58, S260. doi: 10.1016/S0168-8278(13)60640-6
Eren, M., Dinleyici, E. C., and Vandenplas, Y. (2010). Clinical efficacy comparison of Saccharomyces boulardii and yogurt fluid in acute non-bloody diarrhea in children: a randomized, controlled, open label study. Am. J. Trop. Med. Hyg. 82, 488–491. doi: 10.4269/ajtmh.2010.09-0529
Faber, M. T., Jensen, A., Sogaard, M., Hogdall, E., Hogdall, C., Blaakaer, J., et al. (2012). Use of dairy products, lactose, and calcium and risk of ovarian cancer Y results from a Danish case-control study. Int. J. Gynecol. Cancer 22, S42. doi: 10.3109/0284186x.2011.636754
Feart, C., Lorrain, S., Ginder Coupez, V., Samieri, C. L., Letenneur, L., Paineau, D., et al. (2013). Mediterranean diet adherence and risk of fractures in older persons: results from the three-city study. Ann. Nutr. Metab. 63, 759–760. doi: 10.1007/s00198-013-2421-7
Frank, S., Linder, K., Kullmann, S., Heni, M., Ketterer, C., Cavusoglu, M., et al. (2012). Fat intake modulates cerebral blood flow in homeostatic and gustatory brain areas in humans. Am. J. Clin. Nutr. 95, 1342–1349. doi: 10.3945/ajcn.111.031492
Freudenheim, J. L., Russell, M., Trevisan, M., and Doemland, M. (1991). Calcium Intake and Blood Pressure in Blacks and White. Ethn. Dis. 1, 114–122.
Gallus, S., Bravi, F., Talamini, R., Negri, E., Montella, M., Ramazzotti, V., et al. (2006). Milk, dairy products and cancer risk (Italy). Cancer Causes Control 17, 429–437. doi: 10.1007/s10552-005-0423-2
Ganji, V., and Kafai, M. (2004a). Dietary patterns are related to serum total homocysteine concentrations in the US. FASEB J. 18, Abst.105.2.
Ganji, V., and Kafai, M. R. (2004b). Frequent consumption of milk, yogurt, cold breakfast cereals, peppers, and cruciferous vegetables and intakes of dietary folate and riboflavin but not vitamins B-12 and B-6 are inversely associated with serum total homocysteine concentrations in the US population. Am. J. Clin. Nutr. 80, 1500–1507.
Gao, D., Ning, N., Wang, C., Wang, Y., Li, Q., Meng, Z., et al. (2013). Dairy products consumption and risk of type 2 diabetes: systematic review and dose-response meta-analysis. PLoS ONE 8:e73965. doi: 10.1371/journal.pone.0073965
Genkinger, J. M., Hunter, D. J., Spiegelman, D., Anderson, K. E., Arslan, A., Beeson, W. L., et al. (2006). Dairy products and ovarian cancer: a pooled analysis of 12 cohort studies. Cancer Epidemiol. Biomarkers Prev. 15, 364–372. doi: 10.1158/1055-9965.EPI-05-0484
Gheller, B., McCormick, M., Li, A., Anini, Y., Bellissimo, N., Hamilton, J., et al. (2013). Dairy snack reduces glycaemia in normal weight children. FASEB J. 27:Abstract 1074.9.
Goldbohm, R. A., Chorus, A. M., Galindo Garre, F., Schouten, L. J., and van den Brandt, P. A. (2011). Dairy consumption and 10-y total and cardiovascular mortality: a prospective cohort study in the Netherlands. Am. J. Clin. Nutr. 93, 615–627. doi: 10.3945/ajcn.110.000430
Gouni-Berthold, I., Schulte, D. M., Krone, W., Lapointe, J. F., Lemieux, P., Predel, H. G., et al. (2012). The whey fermentation product malleable protein matrix decreases TAG concentrations in patients with the metabolic syndrome: a randomised placebo-controlled trial. Br. J. Nutr. 107, 1694–1706. doi: 10.1017/S0007114511004843
Grantham, N. M., Magliano, D. J., Hodge, A., Jowett, J., Meikle, P., and Shaw, J. E. (2013). The association between dairy food intake and the incidence of diabetes in Australia: the Australian Diabetes Obesity and Lifestyle Study (AusDiab). Public Health Nutr. 16, 339–345. doi: 10.1017/S1368980012001310
Haenni, A., Sundberg, B., Yazdanpandah, N., Viberg, A., and Olsson, J. (2009). Effect of fat emulsion (Fabuless) on orocecal transit time in healthy men. Scand. J. Gastroenterol. 44, 1186–1190. doi: 10.1080/00365520903131999
Heaney, R. P., Rafferty, K., and Dowell, M. S. (2002). Effect of yogurt on a urinary marker of bone resorption in postmenopausal women. J. Am. Diet. Assoc. 102, 1672–1674. doi: 10.1016/S0002-8223(02)90356-1
Heck, J. E., Sapkota, A., Vendhan, G., Roychowdhury, S., Dikshit, R. P., Jetly, D. H., et al. (2008). Dietary risk factors for hypopharyngeal cancer in India. Cancer Causes Control 19, 1329–1337. doi: 10.1007/s10552-008-9204-z
Hepner, G., Fried, R., St Jeor, S., Fusetti, L., and Morin, R. (1979). Hypocholesterolemic effect of yogurt and milk. Am. J. Clin. Nutr. 32, 19–24.
Hewitt, D., and Bancroft, H. J. (1985). Nutritional value of yogurt. J. Dairy Res. 52, 197–207. doi: 10.1017/S002202990002402X
Hoffman, D. J., Roberts, S. B., Verreschi, I., Martins, P. A., de Nascimento, C., Tucker, K. L., et al. (2000). Regulation of energy intake may be impaired in nutritionally stunted children from the shantytowns of Sao Paulo, Brazil. J. Nutr. 130, 2265–2270.
Hogenkamp, P. S., Cedernaes, J., Chapman, C. D., Vogel, H., Hjorth, O. C., Zarei, S., et al. (2012). Calorie Anticipation and Food Intake (Calorie anticipation alters food intake after low-caloric not high-caloric preloads. Obesity 21, 1548–1553. doi: 10.1002/oby.20293
Hsu, C. C., Chow, W. H., Boffetta, P., Moore, L., Zaridze, D., Moukeria, A., et al. (2007). Dietary risk factors for kidney cancer in Eastern and Central Europe. Am. J. Epidemiol. 166, 62–70. doi: 10.1093/aje/kwm043
Hursel, R., van der Zee, L., and Westerterp-Plantenga, M. S. (2010). Effects of a breakfast yoghurt, with additional total whey protein or caseinomacropeptide-depleted alpha-lactalbumin-enriched whey protein, on diet-induced thermogenesis and appetite suppression. Br. J. Nutr. 103, 775–780. doi: 10.1017/S0007114509992352
Hyland, M. E., and Sodergren, S. C. (1998). Relationship between lifestyle and minor health complaints: evidence for two clusters of association. J. Nutr. Environ. Med. 8, 233–246. doi: 10.1080/13590849862005
Isakov, V., Pilipenko, V., Shakhovskaya, A., and Tutelyan, V. (2013). Efficacy of inulin enriched yogurt on bowel habits in patients with irritable bowel syndrome with constipation: a pilot study. FASEB J. 27:Abstract lb426.
Iso, H., Stampfer, M. J., Manson, J. E., Rexrode, K., Hennekens, C. H., Colditz, G. A., et al. (1999). Prospective study of calcium, potassium, and magnesium intake and risk of stroke in women. Stroke 30, 1772–1779. doi: 10.1161/01.STR.30.9.1772
Ivey, K. L., Lewis, J. R., Hodgson, J. M., Zhu, K., Dhaliwal, S. S., Thompson, P. L., et al. (2011). Association between yogurt, milk, and cheese consumption and common carotid artery intima-media thickness and cardiovascular disease risk factors in elderly women. Am. J. Clin. Nutr. 94, 234–239. doi: 10.3945/ajcn.111.014159
Janoutova, G., Kollarova, H., Horakova, D., Cizek, L., Reif, R., Starczewski, J., et al. (2007). Nutritional risk factors for kidney cancer. Klinicka Onkologie 20, 294–297.
Jaspers, D. A., Massey, L. K., and Luedecke, L. O. (1984). Effect of consuming yoghurts prepared with 3 culture strains on human serum lipoproteins. J. Food Sci. 49, 1178–1181. doi: 10.1111/j.1365-2621.1984.tb10422.x
Javed, S., Ahmad, R., Nawaz, S., and Saeed, S. (2013). Comparative studies on the hypocholestrimic effect of branded and conventional yoghurt. Healthmed 71, 92–97.
Jha, R. M., Mithal, A., Malhotra, N., and Brown, E. M. (2010). Pilot case-control investigation of risk factors for hip fractures in the urban Indian population. BMC Musculoskelet. Disord. 11:49. doi: 10.1186/1471-2474-11-49
Jodkowska, M., Oblacinska, A., Tabak, I., and Radiukiewicz, K. (2011). Differences in dietary patterns between overweight and normal-weight adolescents. Med. Wieku Rozwoj. 15, 266–273.
Jordan, H. A., Levitz, L. S., Utgoff, K. L., and Lee, H. L. (1981). Role of food characteristics in behavioral change and weight loss. J. Am. Diet. Assoc. 79, 24–29.
Jordão, R. E., Bernardi, J. L. D., and Barros Filho, A. D. A. (2009). Introdução alimentar e anemia em lactentes do município de Campinas (SP) Feeding pattern and anemia in infants in the city of Campinas, São Paulo, Brazil. Rev. Paul. Pediatr. 27, 381–388. doi: 10.1590/S0103-05822009000400006
Joshi, N. A., Albertson, A. M., and Bell, E. (2011). Yogurt intake is associated with favorable nutrient intake and healthy body measures in US women: results from NHANES 2007-08. FASEB J. 25:Abstract 783.5.
Juarranz Sanz, M., Soriano Llora, T., Calle Puron, M. E., Martinez Hernandez, D., Gonzalez Navarro, A., and Dominguez Rojas, V. (2004). Influence of the diet on the development of colorectal cancer in a population of Madrid. [Spanish] Influencia de la dieta en la aparicion del cancer colorrectal en una poblacion de Madrid. Rev. Clin. Esp. 204, 355–361. doi: 10.1016/S0014-2565(04)71484-8
Kampman, E., Goldbohm, R. A., van den Brandt, P. A., and van 't Veer, P. (1994). Fermented dairy products, calcium, and colorectal cancer in The Netherlands Cohort Study. Cancer Res. 54, 3186–3190.
Kampman, E., Slattery, M. L., Caan, B., and Potter, J. D. (2000). Calcium, vitamin, D., sunshine exposure, dairy products and colon cancer risk (United States). Cancer Causes Control 11, 459–466. doi: 10.1023/A:1008914108739
Karabocuoglu, M., Sokucu, S., Gokcay, G., Ucsel, R., and Ozenoglu, A. (1993). The effect of diet on carbohydrate malabsorption during acute diarrhea. Cocuk Sagligi ve Hastaliklari Dergisi 36, 11–16.
Karagianni, V., Merikas, E., Georgopoulos, F., Gikas, A., Athanasopoulos, N., Malgarinos, G., et al. (2010). Risk factors for colorectal polyps: findings from a Greek case-control study. Rev. Med. Chir. Soc. Med. Nat. Iasi 114, 662–670.
Kawakita, D., Sato, F., Hosono, S., Ito, H., Oze, I., Watanabe, M., et al. (2012). Inverse association between yoghurt intake and upper aerodigestive tract cancer risk in a Japanese population. Eur. J. Cancer Prev. 21, 453–459. doi: 10.1097/CEJ.0b013e32834f75b5
Keast, D. R., Albertson, A. M., Gugger, C. K., and Holschuh, N. M. (2010). Yogurt, dairy, calcium, and vitamin D intake are associated with lower body fat measures in US children: results from NHANES 2005-2008. FASEB J. 24:Abstract 811.15.
Keast, D. R., Albertson, A. M., Gugger, C. K., and Holschuh, N. M. (2013). Yogurt consumption by US children is associated with higher protein, calcium and vitamin D intake, lower dietary fat, and lower body fat: results from the National Health and Nutrition Examination Survey (NHANES 2005-2008). FASEB J. 27:Abstract 847.18.
Kesse, E., Bertrais, S., Astorg, P., Jaouen, A., Arnault, N., Galan, P., et al. (2006). Dairy products, calcium and phosphorus intake, and the risk of prostate cancer: results of the French prospective SU.VI.MAX (Supplementation en Vitamines et Mineraux Antioxydants) study. Br. J. Nutr. 95, 539–545. doi: 10.1079/BJN20051670
Kesse, E., Boutron-Ruault, M. C., Norat, T., Riboli, E., and Clavel-Chapelon, F. (2005). Dietary calcium, phosphorus, vitamin, D., dairy products and the risk of colorectal adenoma and cancer among French women of the E3N-EPIC prospective study. Int. J. Cancer 117, 137–144. doi: 10.1002/ijc.21148
Khandelwal, S., Demonty, I., Jeemon, P., Lakshmy, R., Mukherjee, R., Gupta, R., et al. (2009). Independent and interactive effects of plant sterols and fish oil n-3 long-chain polyunsaturated fatty acids on the plasma lipid profile of mildly hyperlipidaemic Indian adults. Br. J. Nutr. 102, 722–732. doi: 10.1017/S0007114509297170
Kim, J. (2013). Dairy food consumption is inversely associated with the risk of the metabolic syndrome in Korean adults. J. Hum. Nutr. Diet. 26(Suppl. 1), 171–179. doi: 10.1111/jhn.12098
Kim, J., Ko, Y., Park, Y. K., Kim, N. I., Ha, W. K., and Cho, Y. (2010). Dietary effect of lactoferrin-enriched fermented milk on skin surface lipid and clinical improvement of acne vulgaris. Nutrition 26, 902–909. doi: 10.1016/j.nut.2010.05.011
King, N. A., Craig, S. A., Pepper, T., and Blundell, J. E. (2005). Evaluation of the independent and combined effects of xylitol and polydextrose consumed as a snack on hunger and energy intake over 10 d. Br. J. Nutr. 93, 911–915. doi: 10.1079/BJN20051431
Kirii, K., Mizoue, T., Iso, H., Takahashi, Y., Kato, M., Inoue, M., et al. (2009). Calcium, vitamin D and dairy intake in relation to type 2 diabetes risk in a Japanese cohort. Diabetologia 52, 2542–2550. doi: 10.1007/s00125-009-1554-x
Kocic, B., Jankovic, S., Marinkovic, J., Petrovic, B., Tiodorovic, B., and Filipovic, S. (1997). Diet and breast cancer. Arch. Oncol. 5, 71–73.
Kojima, M., Wakai, K., Tamakoshi, K., Tokudome, S., Toyoshima, H., Watanabe, Y., et al. (2004). Diet and colorectal cancer mortality: results from the Japan Collaborative Cohort Study. Nutr. Cancer 50, 23–32. doi: 10.1207/s15327914nc5001_4
Korpela, R., Tuomilehto, J., Högström, P., Seppo, L., Piironen, V., Salo-Väänänen, P., et al. (2006). Safety aspects and cholesterol-lowering efficacy of low fat dairy products containing plant sterols. Eur. J. Clin. Nutr. 60, 633–642. doi: 10.1038/sj.ejcn.1602362
Kurahashi, N., Inoue, M., Iwasaki, M., Sasazuki, S., Tsugane, A. S., and Japan Public Health Center-Based Prospective Study Group. (2008). Dairy product, saturated fatty acid, and calcium intake and prostate cancer in a prospective cohort of Japanese men. Cancer Epidemiol. Biomarkers Prev. 17, 930–937. doi: 10.1158/1055-9965.EPI-07-2681
Kyrozis, A., Ghika, A., Stathopoulos, P., Vassilopoulos, D., Trichopoulos, D., and Trichopoulou, A. (2013). Dietary and lifestyle variables in relation to incidence of Parkinson's disease in Greece. Eur. J. Epidemiol. 28, 67–77. doi: 10.1007/s10654-012-9760-0
Larsson, S. C., Männistö, S., Virtanen, M. J., Kontto, J., Albanes, D., and Virtamo, J. (2009). Dairy foods and risk of stroke. Epidemiology 20, 355–360. doi: 10.1097/EDE.0b013e3181935dd5
Lê, M. G., Moulton, L. H., Hill, C., and Kramar, A. (1986). Consumption of dairy produce and alcohol in a case-control study of breast cancer. J. Natl. Cancer Inst. 77, 633–636.
Liberati, A., Altman, D. G., Tezlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J., et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. doi: 10.1136/bmj.b2700
Lin, J., Zhang, S. M., Cook, N. R., Manson, J. E., Lee, I. M., and Buring, J. E. (2005). Intakes of calcium and vitamin D and risk of colorectal cancer in women. Am. J. Epidemiol. 161, 755–764. doi: 10.1093/aje/kwi101
Liu, S., Choi, H. K., Ford, E., Song, Y., Klevak, A., Buring, J. E., et al. (2006). A prospective study of dairy intake and the risk of type 2 diabetes in women. Diabetes Care 29, 1579–1584. doi: 10.2337/dc06-0256
Lluch, A., Hanet-Geisen, N., Salah, S., Salas-Salvado, J., L'Heureux-Bouron, D., and Halford, J. C. G. (2010). Short-term appetite-reducing effects of a low-fat dairy product enriched with protein and fibre. Food Qual. Prefer. 21, 402–409. doi: 10.1016/j.foodqual.2009.10.001
Logan, C. M., McCaffrey, T. A., Wallace, J. M. W., Robson, P. J., Welch, R. W., Dunne, A., et al. (2006). Investigation of the medium-term effects of Olibra (TM) fat emulsion on food intake in non-obese subjects. Eur. J. Clin. Nutr. 60, 1081–1091. doi: 10.1038/sj.ejcn.1602422
Makino, S., Ikegami, S., Kume, A., Horiuchi, H., Sasaki, H., and Orii, N. (2010). Reducing the risk of infection in the elderly by dietary intake of yoghurt fermented with Lactobacillus delbrueckii ssp. bulgaricus OLL1073R-1. Br. J. Nutr. 104, 998–1006. doi: 10.1017/S000711451000173X
Margolis, K. L., Wei, F., de Boer, I. H., Howard, B. V., Liu, S., Manson, J. E., et al. (2011). A diet high in low-fat dairy products lowers diabetes risk in postmenopausal women. J. Nutr. 141, 1969–1974. doi: 10.3945/jn.111.143339
Martinez-Puig, D., Moller, I., Fernandez, C., and Chetrit, C. (2013). Efficacy of oral administration of yoghurt supplemented with a preparation containing hyaluronic acid (Mobilee) in adults with mild joint discomfort: a randomized, double-blind, placebo-controlled intervention study. Med. J. Nutrition Metab. 6, 63–68. doi: 10.1007/s12349-012-0108-9
Masala, G., Bendinelli, B., Versari, D., Saieva, C., Ceroti, M., Santagiuliana, F., et al. (2008). Anthropometric and dietary determinants of blood pressure in over 7000 Mediterranean women: the European Prospective Investigation into Cancer and Nutrition-Florence cohort. J. Hypertens. 26, 2112–2120. doi: 10.1097/HJH.0b013e32830ef75c
Maslova, E., Halldorsson, T. I., Strøm, M., and Olsen, S. F. (2012). Low-fat yoghurt intake in pregnancy associated with increased child asthma and allergic rhinitis risk: a prospective cohort study. J. Nutr. Sci. 1:e5. doi: 10.1017/jns.2012.5
Massey, L. K. (1984). Effect of changing milk and yogurt consumption on human nutrient intake and serum lipoproteins. J. Dairy Sci. 67, 255–262. doi: 10.3168/jds.S0022-0302(84)81297-7
Matsumoto, M., Ishikawa, S., Nakamura, Y., Kayaba, K., and Kajii, E. (2007). Consumption of dairy products and cancer risks. J. Epidemiol. 17, 38–44. doi: 10.2188/jea.17.38
McNamara, D. J., Lowell, A. E., and Sabb, J. E. (1989). Effect of yogurt intake on plasma lipid and lipoprotein levels in normolipidemic males. Atherosclerosis 79, 167–171. doi: 10.1016/0021-9150(89)90121-4
Meneton, P., Kesse-Guyot, E., Fezeu, L., Galan, P., Hercberg, S., and Menard, J. (2013). Distinctive unhealthy eating pattern in free-living middle-aged hypertensives when compared with dyslipidemic or overweight patients. J. Hypertens. 31, 1554–1563. doi: 10.1097/HJH.0b013e32836130f8
Mensah, M. O., and Otoo, G. E. (2013). Dairy product consumption and the nutritional status of preschool children in Accra, Ghana. Ann. Nutr. Metab. 63, 740. doi: 10.1159/000354245
Mensink, R. P., Ebbing, S., Lindhout, M., Plat, J., and van Heugten, M. M. (2002). Effects of plant stanol esters supplied in low-fat yoghurt on serum lipids and lipoproteins, non-cholesterol sterols and fat soluble antioxidant concentrations. Atherosclerosis 160, 205–213. doi: 10.1016/S0021-9150(01)00562-7
Miyake, Y., Sasaki, S., Tanaka, K., and Hirota, Y. (2010). Dairy food, calcium and vitamin D intake in pregnancy, and wheeze and eczema in infants. Eur. Respir. J. 35, 1228–1234. doi: 10.1183/09031936.00100609
Miyake, Y., Tanaka, K., Fukushima, W., Sasaki, S., Kiyohara, C., Tsuboi, Y., et al. (2011). Lack of association of dairy food, calcium, and vitamin D intake with the risk of Parkinson's disease: a case-control study in Japan. Parkinsonism Relat. Disord. 17, 112–116. doi: 10.1016/j.parkreldis.2010.11.018
Miyake, Y., Tanaka, K., Okubo, H., Sasaki, S., and Arakawa, M. (2012). Dairy food, calcium and vitamin D intake and prevalence of allergic disorders in pregnant Japanese women. Int. J. Tuberc. Lung Dis. 16, 255–261. doi: 10.5588/ijtld.11.0173
Mommers, M., Schouten, L. J., Goldbohm, R. A., and van den Brandt, P. A. (2006). Dairy consumption and ovarian cancer risk in the Netherlands Cohort Study on Diet and Cancer. Br. J. Cancer 94, 165–170. doi: 10.1038/sj.bjc.6602890
Morina, D., Sola, R., Valls, R. M., Lopez de Frutos, V., Montero, M., Giralt, M., et al. (2013). Efficacy of a low-fat yogurt supplemented with a rooster comb extract on joint function in mild knee pain patients: a subject-level meta-analysis. Ann. Nutr. Metab. 63:1386. doi: 10.1159/000354245
Mossavar-Rahmani, Y., Garland, C. F., Caan, B., Herbert, J. R., Wodarski, L. A., Vitolins, M. Z., et al. (2002). Yogurt consumption is associated with healthy behavior in postmenopausal women. Clin. J. Womens. Health 2, 128–134. doi: 10.1053/cjwh.2002.130404
Motegi, K., Toyokawa, S., Nishikawa, H., Ohki, K., and Kano, K. (2001). An epidemiological study of the relationship between diet in the past and bone mineral density based on a survey of women aged 50 years and over in two public health centers, Ibaraki Prefecture. Jpn J. Health Hum. Ecol. 67, 116–126. doi: 10.3861/jshhe.67.116
Mozaffarian, D., Hao, T., Rimm, E. B., Willett, W. C., and Hu, F. B. (2011). Changes in diet and lifestyle and long-term weight gain in women and men. N. Engl. J. Med. 364, 2392–2404. doi: 10.1056/NEJMoa1014296
Murphy, N., Norat, T., Ferrari, P., Jenab, M., Bueno-de-Mesquita, B., Skeie, G., et al. (2013). Consumption of dairy products and colorectal cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC). PLoS ONE 8:e72715. doi: 10.1371/journal.pone.0072715
Nakamura, T., Agata, K., Nishida, S., Shirasu, Y., and Iino, H. (2001). Effects of yogurt supplemented with brewer's yeast cell wall on intestinal environment and defecation in healthy female adults. Biosci. Microflora 20, 27–34. doi: 10.12938/bifidus1996.20.27
Nakamura, T., Hitomi, Y., Yoshida, M., Shirasu, Y., Tsukui, T., and Shimasaki, H. (2002). Effect of yogurt supplemented with brewer's yeast cell wall on levels of blood lipids in normal and hypercholesterolemic adults. J. Oleo Sci. 51, 323–334. doi: 10.5650/jos.51.323
Nakamura, T., Nishida, S., and Iino, H. (2000). Influence of fermented milk (yogurt) containing brewer's yeast cell wall at relatively low doses and over-ingestion on defecation and bowel movement in humans. Pharmacometrics 59, 57–63.
Nasrollahi, F., Haghani, H., and Nikpour, S. (2012). Life style factors related to women's osteoporosis. Osteoporos. Int. 23:S386. doi: 10.1007/s00198-012-1928-7
Nazare, J. A., de la Perrière, A. B., Bonnet, F., Desage, M., Peyrat, J., Maitrepierre, C., et al. (2007). Daily intake of conjugated linoleic acid-enriched yoghurts: effects on energy metabolism and adipose tissue gene expression in healthy subjects. Br. J. Nutr. 97, 273–280. doi: 10.1017/S0007114507191911
Niittynen, L. H., Jauhiainen, T. A., Poussa, T. A., and Korpela, R. (2008). Effects of yoghurt enriched with free plant sterols on the levels of serum lipids and plant sterols in moderately hypercholesterolaemic subjects on a high-fat diet. Int. J. Food Sci. Nutr. 59, 357–367. doi: 10.1080/09637480701554137
Niv, M., Levy, W., and Greenstein, N. M. (1963). Yogurt in the treatment of infantile diarrhea. Clin. Pediatr. 2, 407–411.
Nobre, L. N., Bressan, J., Costa Sobrinho, P. D. S., Costa, N. M. B., Minin, V. P. R., and Cecon, P. R. (2006). Volume of light yogurt and subjective appetite sensations in normal-weight and overweight men. [Portuguese] Volume de iogurte light e sensacoes subjetivas do apetite de homens eutroficos e com excesso de peso. Revista de Nutricao 19, 591–600. doi: 10.1590/S1415-52732006000500007
O'Connor, L. M., Lentjes, M. A., Luben, R. N., Khaw, K. T., Wareham, N. J., and Forouhi, N. G. (2014). Dietary dairy product intake and incident type 2 diabetes: a prospective study using dietary data from a 7-day food diary. Diabetologia 57, 909–917. doi: 10.1007/s00125-014-3176-1
O'Donovan, D., Feinle-Bisset, C., Wishart, J., and Horowitz, M. (2003). Lipase inhibition attenuates the acute inhibitory effects of oral fat on food intake in healthy subjects. Br. J. Nutr. 90, 849–852. doi: 10.1079/BJN2003971
Olivares, M., Paz Díaz-Ropero, M., Gómez, N., Sierra, S., Lara-Villoslada, F., Martín, R., et al. (2006). Dietary deprivation of fermented foods causes a fall in innate immune response. Lactic acid bacteria can counteract the immunological effect of this deprivation. J. Dairy Res. 73, 492–498. doi: 10.1017/S0022029906002068
Oosthuizen, W., Vorster, H. H., Vermaak, W. J., Smuts, C. M., Jerling, J. C., Veldman, F. J., et al. (1998). Lecithin has no effect on serum lipoprotein, plasma fibrinogen and macro molecular protein complex levels in hyperlipidaemic men in a double-blind controlled study. Eur. J. Clin. Nutr. 52, 419–424. doi: 10.1038/sj.ejcn.1600580
Ornelas, I. J., Galvan-Potrillo, M., and López-Carrillo, L. (2007). Protective effect of yoghurt consumption on Helicobacter pylori seropositivity in a Mexican population. Public Health Nutr. 10, 1283–1287. doi: 10.1017/S1368980007696372
Ortinau, L. C., Culp, J. M., Hoertel, H. A., Douglas, S. M., and Leidy, H. J. (2010). The effects of low vs. higher protein yogurt consumed as afternoon snacks on appetite control and time to dinner request in healthy women. FASEB J. 24:Abstract 820.34.
Ortinau, L. C., Culp, J. M., Hoertel, H. A., Douglas, S. M., and Leidy, H. J. (2012a). Comparison of a higher protein yogurt vs. other commonly consumed afternoon snacks on time to meal request. FASEB J. 26.
Ortinau, L. C., Culp, J. M., Hoertel, H. A., Douglas, S. M., and Leidy, H. J. (2012b). The effects of low vs. higher protein yogurt consumed as afternoon snacks on appetite control and time to dinner request in healthy women. FASEB J. 26.
Ortinau, L. C., Culp, J. M., Hoertel, H. A., Douglas, S. M., and Leidy, H. J. (2013). The effects of increased dietary protein yogurt snack in the afternoon on appetite control and eating initiation in healthy women. Nutr. J. 12:71. doi: 10.1186/1475-2891-12-71
O'sullivan, T. A., Hafekost, K., Mitrou, F., and Lawrence, D. (2013). Food sources of saturated fat and the association with mortality: a meta-analysis. Am. J. Public Health 103, e31–e42. doi: 10.2105/ajph.2013.301492
Pala, V., Sieri, S., Berrino, F., Vineis, P., Sacerdote, C., Palli, D., et al. (2011). Yogurt consumption and risk of colorectal cancer in the Italian European prospective investigation into cancer and nutrition cohort. Int. J. Cancer 129, 2712–2719. doi: 10.1002/ijc.26193
Park, Y., Mitrou, P. N., Kipnis, V., Hollenbeck, A., Schatzkin, A., and Leitzmann, M. F. (2007). Calcium, dairy foods, and risk of incident and fatal prostate cancer: the NIH-AARP Diet and Health Study. Am. J. Epidemiol. 166, 1270–1279. doi: 10.1093/aje/kwm268
Pashapour, N., and Iou, S. G. (2006). Evaluation of yogurt effect on acute diarrhea in 6-24-month-old hospitalized infants. Turk. J. Pediatr. 48, 115–118.
Patro-Golab, B., Shamir, R., and Szajewska, H. (2015a). Yogurt for treating acute gastroenteritis in children: systematic review and meta-analysis. Clin Nutr. 34, 818–824. doi: 10.1016/j.clnu.2014.09.004
Patro-Golab, B., Shamir, R., and Szajewska, H. (2015b). Yogurt for treating antibiotic-associated diarrhea: systematic review and meta-analysis. J. Nutr. 31, 796–800. doi: 10.1016/j.nut.2014.11.013
Peters, R. K., Pike, M. C., Garabrant, D., and Mack, T. M. (1992). Diet and Colon Cancer in Los-Angeles County, California. Cancer Causes Control 3, 457–473. doi: 10.1007/BF00051359
Pilipenko, V. I., Burliaeva, E. A., Shakhovskaia, A. K., and Isakov, V. A. (2009). Efficacy of using inulin fortified fermented milk products in patients with functional constipation. Vopr. Pitan. 78, 56–61.
Pordeus Luna, R. C., de Oliveira, A. F., Torres Barbosa, F. P., Marinho Albuquerque, T., and de Moraes, R. M. (2011). Low habitual consumption of food sources of vitamin E in the child population. Rev. Inst. Adolfo Lutz 70, 213–219.
Porkka, L., Salminen, E., and Salminen, S. (1988). The effects of lactulose-sweetened yogurt on the rate of gastric emptying and intestinal transit in healthy human volunteers. Zeitschrift fuer Ernaehrungswissenschaft 27, 150–154. doi: 10.1007/BF02024719
Pounis, G., Risvas, G., Farajian, P., Panagiotakos, D., and Zampelas, A. (2010). Evidence regarding high consumption of low-calorie foods among overweight and obese children in Greece. Obes. Rev. 11, 420. doi: 10.1111/j.1467-789X.2010.00763-7.x
Radler, U., Stangl, H., Lechner, S., Lienbacher, G., Krepp, R., Zeller, E., et al. (2011). A combination of (-3) polyunsaturated fatty acids, polyphenols and L-carnitine reduces the plasma lipid levels and increases the expression of genes involved in fatty acid oxidation in human peripheral blood mononuclear cells and HepG2 cells. Ann. Nutr. Metab. 58, 133–140. doi: 10.1159/000327150
Radosavljevic, V., Jankovic, S., Marinkovic, J., and Djokic, M. (2003). Fluid intake and bladder cancer. A case control study. Neoplasma 50, 234–238.
Rafeey, M., Ostadrahimi, A., Boniadi, M., Ghorashi, Z., Alizadeh, M. M., and Hadafey, V. (2008). Lactobacillus acidophilus yogurt and supplement in children with acute diarrhea: a clinical trial. Res. J. Med. Sci 2, 13–18.
Ramezani Tehrani, F., Moslehi, N., Asghari, G., Gholami, R., Mirmiran, P., and Azizi, F. (2013). Intake of dairy products, calcium, magnesium, and phosphorus in childhood and age at menarche in the Tehran Lipid and Glucose Study. PLoS ONE 8:e57696. doi: 10.1371/journal.pone.0057696
Ranasinghe, J. G. S., Gamlath, G., Samitha, S., and Abeygunawardena, A. S. (2007). Prophylactic use of yoghurt reduces antibiotic induced diarrhoea in children. Sri Lanka J. Child Health 36, 53–56.
Recio, I., Contreras, M., Gomez-Sala, B., Vazquez, C., Fernandez-Escribano, M., and Del Campo, R. (2011). Effect of a casein hydrolysate containing novel peptides in hypertensive subjects. Ann. Nutr. Metab. 58, 16–17. doi: 10.1159/000334393
Reyhani, M., Fahami, F., Mosharaf, S. H., and Tarkesh, N. (2012). The relationship between the amount of dairy products and animal proteins consumption and breast cancer in isfahani women. J. Zanjan Univ. Med. Sci. 20, 45–54.
Rodríguez-Artalejo, F., García, E. L., Gorgojo, L., Garcés, C., Royo, M. A., Martín Moreno, J. M., et al. (2003). Consumption of bakery products, sweetened soft drinks and yogurt among children aged 6-7 years: association with nutrient intake and overall diet quality. Br. J. Nutr. 89, 419–429. doi: 10.1079/BJN2002787
Rolls, B. J., Dimeo, K. A., and Shide, D. J. (1995). Age-related impairments in the regulation of food intake. Am. J. Clin. Nutr. 62, 923–931.
Rolls, B. J., Kim, S., McNelis, A. L., Fischman, M. W., Foltin, R. W., and Moran, T. H. (1991). Time course of effects of preloads high in fat or carbohydrate on food intake and hunger ratings in humans. Am. J. Physiol. 260(4 Pt 2), R756–R763.
Rolls, B. J., Kim-Harris, S., Fischman, M. W., Foltin, R. W., Moran, T. H., and Stoner, S. A. (1994). Satiety after preloads with different amounts of fat and carbohydrate: implications for obesity. Am. J. Clin. Nutr. 60, 476–487.
Ronco, A. L., De Stéfani, E., and Dáttoli, R. (2002). Dairy foods and risk of breast cancer: a case-control study in Montevideo, Uruguay. Eur. J. Cancer Prev. 11, 457–463. doi: 10.1097/00008469-200210000-00008
Rosado, J. L., Diaz, M., Gonzalez, K., Griffin, I., Abrams, S. A., and Preciado, R. (2005). The addition of milk or yogurt to a plant-based diet increases zinc bioavailability but does not affect iron bioavailability in women. J. Nutr. 135, 465–468.
Rossouw, J. E., Burger, E. M., Van der Vyver, P., and Ferreira, J. J. (1981). The effect of skim milk, yoghurt, and full cream milk on human serum lipids. Am. J. Clin. Nutr. 34, 351–356.
Rudkowska, I., AbuMweis, S. S., Nicolle, C., and Jones, P. J. (2008). Cholesterol-lowering efficacy of plant sterols in low-fat yogurt consumed as a snack or with a meal. J. Am. Coll. Nutr. 27, 588–595. doi: 10.1080/07315724.2008.10719742
Rudkowska, I., AbuMweis, S. S., Nicolle, C., and Jones, P. J. H. (2007). Plant sterols consumed in low-fat yogurt as a snack lower cholesterol. FASEB J. 21, A156.
Sadrzadeh-Yeganeh, H., Elmadfa, I., Djazayery, A., Jalali, M., Heshmat, R., and Chamary, M. (2010). The effects of probiotic and conventional yoghurt on lipid profile in women. Br. J. Nutr. 103, 1778–1783. doi: 10.1017/S0007114509993801
Sahni, S., Tucker, K., Kiel, D., Quach, L., Casey, V., and Hannan, M. (2012). Positive association of dairy intake with bone mineral density (BMD) depends on vitamin d intake: the framingham original cohort. J. Bone Miner. Res. 27:Poster MO0322.
Sahni, S., Tucker, K. L., Kiel, D. P., Quach, L., Casey, V. A., and Hannan, M. T. (2013a). Milk and yogurt consumption are linked with higher bone mineral density but not with hip fracture: the Framingham Offspring Study. Arch. Osteoporos. 8:119. doi: 10.1007/s11657-013-0119-2
Sahni, S., Tucker, K. L., Kiel, D. P., Quach, L., Casey, V., and Hannan, M. T. (2013b). Effect of dairy intake on bone mineral density (BMD) is only beneficial with higher vitamin D (VitD) intakes: the framingham original cohort. FASEB J. 27:Abstract 106.5.
Sakauchi, F., Mori, M., Washio, M., Watanabe, Y., Ozasa, K., Hayashi, K., et al. (2004). Dietary habits and risk of urothelial cancer death in a large-scale cohort study (JACC Study) in Japan. Nutr. Cancer 50, 33–39. doi: 10.1207/s15327914nc5001_5
Salakidou, C., Kaffe, E., Burini, G., Tsinteris, V., and Moulas, A. N. (2012). Yogurt fortified with vitamin d: a study for bioavailability of vitamin D in a dairy product. Ann. Nutr. Metab. 60, 142. doi: 10.1159/000337881
Sazawal, S., Habib, A., Dhingra, U., Dutta, A., Dhingra, P., Sarkar, A., et al. (2013). Impact of micronutrient fortification of yoghurt on micronutrient status markers and growth - a randomized double blind controlled trial among school children in Bangladesh. BMC Public Health 13:514. doi: 10.1186/1471-2458-13-514
Schusdziarra, V., Hausmann, M., Sassen, M., Kellner, M., Mittermeier, J., and Erdmann, J. (2011). Relationship between breakfast calories, daily energy intake and consumption of food items. [German] Beziehung zwischen Fruhstuckskalorien, taglicher Energieaufnahme und Lebensmittelverzehr. Aktuel. Ernahrungsmed. 36, 232–240. doi: 10.1055/s-0031-1276868
Shannon, J., White, E., Shattuck, A. L., and Potter, J. D. (1996). Relationship of food groups and water intake to colon cancer risk. Cancer Epidemiol. Biomarkers Prev. 5, 495–502.
Sluijs, I., Forouhi, N. G., Beulens, J. W., van der Schouw, Y. T., Agnoli, C., Arriola, L., et al. (2012). The amount and type of dairy product intake and incident type 2 diabetes: results from the EPIC-InterAct Study. Am. J. Clin. Nutr. 96, 382–390. doi: 10.3945/ajcn.111.021907
Smit, H. J., Keenan, E., Kovacs, E. M., Wiseman, S. A., Peters, H. P., Mela, D. J., et al. (2011). No efficacy of processed Fabuless (Olibra) in suppressing appetite or food intake. Eur. J. Clin. Nutr. 65, 81–86. doi: 10.1038/ejcn.2010.187
Snijder, M. B., van der Heijden, A. A., van Dam, R. M., Stehouwer, C. D., Hiddink, G. J., Nijpels, G., et al. (2007). Is higher dairy consumption associated with lower body weight and fewer metabolic disturbances? The Hoorn Study. Am. J. Clin. Nutr. 85, 989–995.
Soedamah-Muthu, S. S., Verberne, L. D., Ding, E. L., Engberink, M. F., and Geleijnse, J. M. (2012). Dairy consumption and incidence of hypertension: a dose-response meta-analysis of prospective cohort studies. Hypertension 60, 1131–1137. doi: 10.1161/HYPERTENSIONAHA.112.195206
Sorenson, A. W., Pfister, R., Smith, K., and Delhumeau, C. (2004). Identifying the role of milk and milk products on nutritional and health issues for adults fifty years of age and older. FASEB J. 18, Abst. 582.5.
Steffen, L. M., and Jacobs, D. R. (2003). Relation between dairy food intake and plasma lipid levels: the CARDIA Study. Aust. J. Dairy Technol. 58, 92–97.
Steffen, L. M., Kroenke, C. H., Yu, X., Pereira, M. A., Slattery, M. L., Van Horn, L., et al. (2005). Associations of plant food, dairy product, and meat intakes with 15-y incidence of elevated blood pressure in young black and white adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am. J. Clin. Nutr. 82, 1169–1177; quiz 363–364.
Stritecka, H., and Hlubik, P. (2013). Effects of a fermented milk product enriched with protein and fibre to satiation and weight reduction. Ann. Nutr. Metab. 63, 436. doi: 10.1159/000354245
Sullivan, A. D. M. M. L., Murray, R. M., and Mackeigan, B. (1989). The effect of a whey-basserum cholesterol of adult males. Can Diet Assoc. 50, 233–237.
Tavani, A., Gallus, S., Negri, E., and La Vecchia, C. (2002). Milk, dairy products, and coronary heart disease. J. Epidemiol. Commun. Health 56, 471–472. doi: 10.1136/jech.56.6.471
Telgi, R. L., Yadav, V., Telgi, C. R., and Boppana, N. (2013). In vivo dental plaque pH after consumption of dairy products. Gen. Dent. 61, 56–59.
Teuri, U., and Korpela, R. (1998). Galacto-oligosaccharides relieve constipation in elderly people. Ann. Nutr. Metab. 42, 319–327. doi: 10.1159/000012751
Thomas, D. T., Wideman, L., and Lovelady, C. A. (2011). Effects of a dairy supplement and resistance training on lean mass and insulin-like growth factor in women. Int. J. Sport Nutr. Exerc. Metab. 21, 181–188.
Thompson, L. U., Jenkins, D. J., Amer, M. A., Reichert, R., Jenkins, A., and Kamulsky, J. (1982). The effect of fermented and unfermented milks on serum cholesterol. Am. J. Clin. Nutr. 36, 1106–1111.
Tong, X., Dong, J. Y., Wu, Z. W., Li, W., and Qin, L. Q. (2011). Dairy consumption and risk of type 2 diabetes mellitus: a meta-analysis of cohort studies. Eur. J. Clin. Nutr. 65, 1027–1031. doi: 10.1038/ejcn.2011.62
Trapp, C. L., Chang, C. C., Halpern, G. M., Keen, C. L., and Gershwin, M. E. (1993). The Influence of Chronic Yogurt Consumption on Populations of Young and Elderly Adults. Int. J. Immunother. 9, 53–64.
Trautwein, E. A., Doornbos, A. M., Meynen, E. M., and Duchateau, G. S. (2005). The cholesterol-lowering effect of a plant sterol ester enriched yoghurt single-shot drink consumed with or without a meal. FASEB J. 19 (4, Suppl. S, Pt 1), A416.
Trautwein, E. A., Noakes, M., Clifton, P. M., and Doornbos, A. M. (2004). Intake of plant sterol ester enriched milk and yoghurt effectively lowers plasma lipids in modestly hypercholesterolemic subjects. FASEB J. 18, Abst. 362.4.
Troy, L. M., Jacques, P. F., Vasan, R. S., and McKeown, N. M. (2010). Dairy intake not associated with metabolic syndrome but milk and yogurt intake is inversely associated with prevalence of hypertension in middle-aged adults. FASEB J. 24:Abstract 324.5.
Tsuchiya, A., Almiron-Roig, E., Lluch, A., Guyonnet, D., and Drewnowski, A. (2006). Higher satiety ratings following yogurt consumption relative to fruit drink or dairy fruit drink. J. Am. Diet. Assoc. 106, 550–557. doi: 10.1016/j.jada.2006.01.004
Uenishi, K., and Nakamura, K. (2010). Intake of dairy products and bone ultrasound measurement in late adolescents: a nationwide cross-sectional study in Japan. Asia Pac. J. Clin. Nutr. 19, 432–439.
Uenishi, T., Sugiura, H., Tanaka, T., and Uehara, M. (2008). Role of foods in irregular aggravation of skin lesions in children with atopic dermatitis. J. Dermatol. 35, 407–412. doi: 10.1111/j.1346-8138.2008.00494.x
Uenishi, T., Sugiura, H., and Uehara, M. (2004). The importance of foods in childhood atopic dermatitis: with special reference to cases with irregular aggravation of the disease. [Japanese]. Skin Res. 3(Suppl. 4), 93–97.
van der Zander, K., Bots, M. L., Bak, A. A., Koning, M. M., and de Leeuw, P. W. (2008). Enzymatically hydrolyzed lactotripeptides do not lower blood pressure in mildly hypertensive subjects. Am. J. Clin. Nutr. 88, 1697–1702. doi: 10.3945/ajcn.2008.26003
Vandewater, K., and Vickers, Z. (1996). Higher-protein foods produce greater sensory-specific satiety. Physiol. Behav. 59, 579–583. doi: 10.1016/0031-9384(95)02113-2
van't Veer, P., Dekker, J. M., Lamers, J. W., Kok, F. J., Schouten, E. G., Brants, H. A., et al. (1989). Consumption of fermented milk products and breast cancer: a case-control study in The Netherlands. Cancer Res. 49, 4020–4023.
Vázquez Martínez, C., Alfred Konning, M., Yuste Grijalba, F. J., and Abraíra Santos, V. (2005). Application of GIQLI questionnaire to two groups of healthy yogurt consumers. Nutr. Hosp. 20, 420–428.
Vergnaud, A. C., Péneau, S., Chat-Yung, S., Kesse, E., Czernichow, S., Galan, P., et al. (2008). Dairy consumption and 6-y changes in body weight and waist circumference in middle-aged French adults. Am. J. Clin. Nutr. 88, 1248–1255.
Vlajinac, H. D., Pekmezovic, T. D., Adanja, B. J., Marinkovic, J. M., Kanazir, M. S., Suvajdzic, N. D., et al. (2003). Case-control study of multiple myeloma with special reference to diet as risk factor. Neoplasma 50, 79–83.
Wang, H., Livingston, K. A., Fox, C. S., Meigs, J. B., and Jacques, P. F. (2013). Yogurt consumption is associated with better diet quality and metabolic profile in American men and women. Nutr. Res. 33, 18–26. doi: 10.1016/j.nutres.2012.11.009
Wang, H., Livingston, K. A., Meigs, J. B., and Jacques, P. F. (2012). Yogurt consumption, blood pressure, and incident hypertension: a longitudinal study in the framingham heart study. Hypertension 60:Abstract 188.
Wang, L., Manson, J. E., Buring, J. E., Lee, I. M., and Sesso, H. D. (2008). Dietary intake of dairy products, calcium, and vitamin D and the risk of hypertension in middle-aged and older women. Hypertension 51, 1073–1079. doi: 10.1161/HYPERTENSIONAHA.107.107821
White, K. M., Bauer, S. J., Hartz, K. K., and Baldridge, M. (2009). Changes in body composition with yogurt consumption during resistance training in women. Int. J. Sport Nutr. Exerc. Metab. 19, 18–33.
WHO. (2001). Health and Nutritional Properties of Probiotics in Food Including Powder Milk with Live Lactic Acid Bacteria. Geneva: Food and Agricultural Organization of the United Nations and World Health Organization.
WHO. (2006). Understanding The Codex Alimentarius. Rome.: Food and Agricultural Organization of the United Nations and World Health Organization.
Yae, J. H., Oh, Y. K., Joo, B. K., Lee, J. H., Jang, Y., Liponkoski, L., et al. (2005). Plant stanol esters in low-fat yogurt reduces total and low-density lipoprotein cholesterol and low-density lipoprotein oxidation in normocholesterolemic and mildly hypercholesterolemic subjects. Nutr. Res. 25, 743–753. doi: 10.1016/j.nutres.2005.08.004
Zandstra, E. H., Mathey, M. F., Graaf, C., and van Staveren, W. A. (2000). Short-term regulation of food intake in children, young adults and the elderly. Eur. J. Clin. Nutr. 54, 239–246. doi: 10.1038/sj.ejcn.1600927
Zemel, M. B., Richards, J., Mathis, S., Milstead, A., Gebhardt, L., and Silva, E. (2005). Dairy augmentation of total and central fat loss in obese subjects. Int. J. Obes. 29, 391–397. doi: 10.1038/sj.ijo.0802880
Keywords: yogurt, health outcomes, review, effects, evidence
Citation: Glanville JM, Brown S, Shamir R, Szajewska H and Eales JF (2015) The scale of the evidence base on the health effects of conventional yogurt consumption: findings of a scoping review. Front. Pharmacol. 6:246. doi: 10.3389/fphar.2015.00246
Received: 26 August 2015; Accepted: 12 October 2015;
Published: 30 October 2015.
Edited by:
Dominique J. Dubois, Université libre de Bruxelles, BelgiumReviewed by:
Sunita Nair, Capita India Pvt. Ltd., IndiaLorenzo Morelli, Università Cattolica del Sacro Cuore, Italy
Copyright © 2015 Glanville, Brown, Shamir, Szajewska and Eales. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julie M. Glanville, anVsaWUuZ2xhbnZpbGxlQHlvcmsuYWMudWs=
 Julie M. Glanville
Julie M. Glanville Sam Brown1
Sam Brown1 Raanan Shamir
Raanan Shamir Jacqualyn F. Eales
Jacqualyn F. Eales