- 1Nursing Office, Renmin Hospital of Wuhan University, Wuhan, China
- 2Department of Cardiovascular Surgery, Renmin Hospital of Wuhan University, Wuhan, China
- 3The Nephrology Division and Dialysis Transplant Center, Renmin Hospital of Wuhan University, Wuhan, China
- 4Department of Hepatobiliary Surgery, Renmin Hospital of Wuhan University, Wuhan, China
- 5Department of Psychiatry, Renmin Hospital of Wuhan University, Wuhan, China
Objectives: The coronavirus disease 2019 (COVID-19) pandemic may have an impact on the psychological distress of organ transplant recipients. We aimed to assess the status of psychological distress and its association with quality of life (QoL) in organ transplant recipients during the COVID-19 pandemic.
Materials and Methods: A cross-sectional survey was carried out with 305 organ transplant recipients during March 30 and April 2, 2020, in Wuhan. Psychological distress comprised depression, anxiety, insomnia, and post-traumatic stress disorder (PTSD), which were assessed using the Patient Health Questionnaire-9, the seven-item Generalized Anxiety Disorder questionnaire, the Insomnia Severity Index, and Impact of event scale-revised. QoL was assessed using the Chinese version of the short Form 36-item health survey.
Results: The prevalence of depression, anxiety, insomnia, and PTSD in organ transplant recipients was 13.4, 6.9, 11.8, and 30.5%, respectively. Organ transplant recipients with depression had significantly lower scores in all eight dimensions of QoL compared with participants without depression (all p < 0.05). Lower scores on the QoL dimensions of role physical, bodily pain, general health, vitality, role emotional, and mental health were found in organ transplant recipients with anxiety, insomnia, or PTSD compared with their counterparts without the respective disorder (all p < 0.05).
Limitation: The cross-sectional study design limited us to make causal conclusion and the influence of potential confounders cannot be ruled out.
Conclusions: Psychological distress was prevalent in organ transplant recipients during the COVID-19 pandemic, and those with depression, anxiety, insomnia, and PTSD had poorer QoL. Therefore, timely psychological counseling, COVID-19 related health education, and essential community medical services should be provided to organ transplant recipients to relieve their psychological distress, and to improve their QoL.
Introduction
The outbreak of coronavirus disease 2019 (COVID-19), first reported in China (1), has become a pandemic. As of November 22, 2020, more than 57.8 million confirmed cases and 1.3 million deaths had been reported worldwide (2). During the COVID-19 pandemic, the psychological distress among the population can be prominent because of social isolation, uncertainty of the future, fear of being infected, and overwhelming negative news portrayal in mass media coverage (3, 4). The mechanisms that people get into psychological distress are implicated, for instance, Serafini et al. found that extreme sensory processing patterns show a complex association with depression, and impulsivity, alexithymia, and hopelessness (5). Numerous studies have proven that both healthcare workers and the general public were associated high psychological burden during this crisis (6). It was suggested that psychological interventions targeting high-risk populations with heavy psychological distress are in urgent need, and the importance of protective factors including sufficient medical resources, up-to-date and accurate information, and precautionary measures should be stressed (6, 7).
End-stage organ failure is a serious condition associated with an increased risk of mortality (8, 9). Organ transplantation is often the only treatment for patients with end-stage organ failure. The number of patients undergoing organ transplantation is increasing (10), with more than 100,000 organ transplantations performed annually worldwide (11), and a post-transplant survival exceeding 85-90% in the first year and 70-75% at 5 years (12). Kidney transplantation is the most frequent, globally, followed by liver and heart transplantations. Patients with end-stage organ failure suffer from severe physical and psychological symptoms (13). QoL is a major index to the evaluate the efficacy of medical intervention among patients with end-stage organ failure. Organ transplantation has been demonstrated to be the best treatment both for quality of life (QoL) and cost effectiveness (14–16).
Organ transplant recipients are patients who have received organ transplantation. A large proportion of organ transplant recipients suffer psychological distress, including symptoms of depression (17), anxiety (18), and post-traumatic stress disorder (PTSD) (11). During the COVID-19 pandemic, moderate to severe depression and anxiety were demonstrated to be independently associated with increased risk of low QoL among healthcare workers (19). Affected by the COVID-19 pandemic, organ transplant recipients may suffer more apparent psychological distress than before, and as a result may endure worsen QoL. Nevertheless, the status of psychological distress during the COVID-19 pandemic and its association with QoL in organ transplant recipients is unknown. Therefore, this study involved a cross-sectional survey with organ transplant recipients to assess their level of psychological distress and QoL, and explore the association between the two, during the COVID-19 pandemic.
Materials and Methods
Study Participants
This cross-sectional study was conducted between March 30 and April 2, 2020. It was approved by the Clinical Research Ethics Committee of Renmin Hospital of Wuhan University (WDRY2020-K004). Organ transplant recipients were identified from the medical records of Renmin Hospital of Wuhan University. Individuals were included if they underwent kidney, heart, or liver transplantation from January 2015 to December 2019, and were excluded if they died, could not complete the questionnaires, or refused to sign the informed consent. 305 from 342 invited organ transplant recipients (with a response rate of 89.2%) agreed to participate in this study and signed the informed consent before their participation. In the informed consent forms, participants were encouraged to seek psychological assistance through a free online psychological support system, in which psychologist and psychiatrist could provide online psychological assistance (20).
Assessment of Psychological Distress
As described in our previous studies (4, 21), symptoms of depression, anxiety, insomnia, and PTSD were assessed using the Patient Health Questionnaire-9 (PHQ-9) (22), 7-item Generalized Anxiety Disorder (GAD-7) questionnaire (23), Insomnia Severity Index (ISI) (24), and Impact of Event Scale-Revised (IES-R) (24), respectively. The cut-off scores for identifying major depression, anxiety, insomnia, and PTSD are 10, 10, 15, and 22, on the respective scales. The validity and reliability of these instruments have been confirmed in Chinese population (25–28).
Assessment of QoL
QoL was evaluated using the Chinese version of the Short Form 36-Item Health Survey (SF-36) (29). The SF-36 comprises 36 items that cover eight dimensions: physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE), and mental health (MH). The score for each dimension ranges from 0 to 100, with higher values indicating better functioning and fewer limitations.
Assessment of Covariates
Covariates were collected by questionnaires, including age, gender, marital status, education level, living location, living condition, type of organ transplantation, post-operative time, comorbidities, and worry about infection.
Statistical Analysis
Data analysis was conducted using SPSS version 20.0 (IBM Corp., Armonk, New York, United States). The associations between sociodemographic variables, psychological distress, and QoL were analyzed by the analysis of variance (ANOVA) or the Wilcoxon rank sum test where appropriate. The significance level was set as α = 0.05.
Results
Characteristics of Organ Transplant Recipients
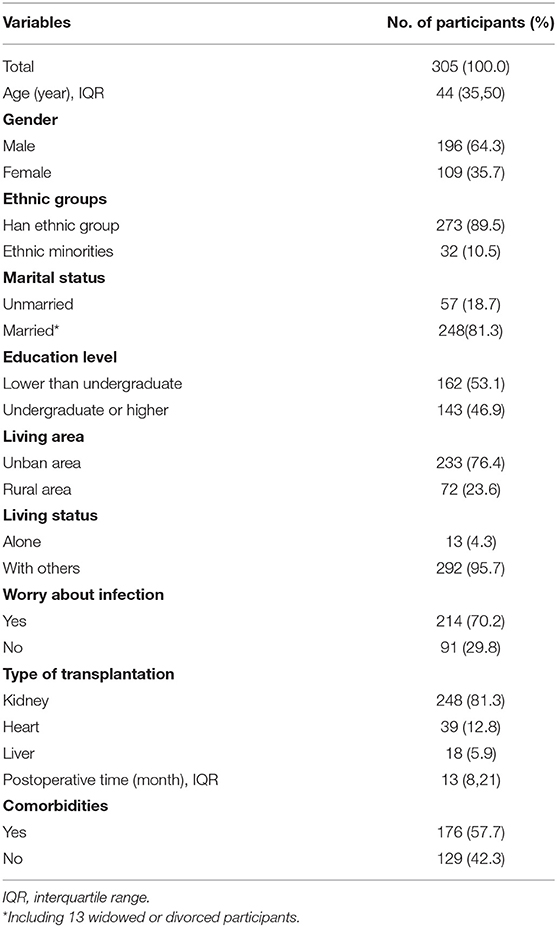
Table 1 presents the characteristics of the organ transplant recipients in this study. Participants were 196 males and 109 females, with a mean (SD) age of 43.1 (10.7) years. A total of 248 (81.3%) were kidney transplant recipients, 39 (12.8) were heart transplant recipients, and 18 (5.9%) were liver transplant recipients. The median post-operative time was 17.1 months. The participants tended to be of Han ethnic group (89.5%), be married (81.3%), have an educational level of less than undergraduate (53.1%), live in an urban area (76.4%), live with others (95.7%), worry about infection (70.2%), and have comorbidities (57.7%).
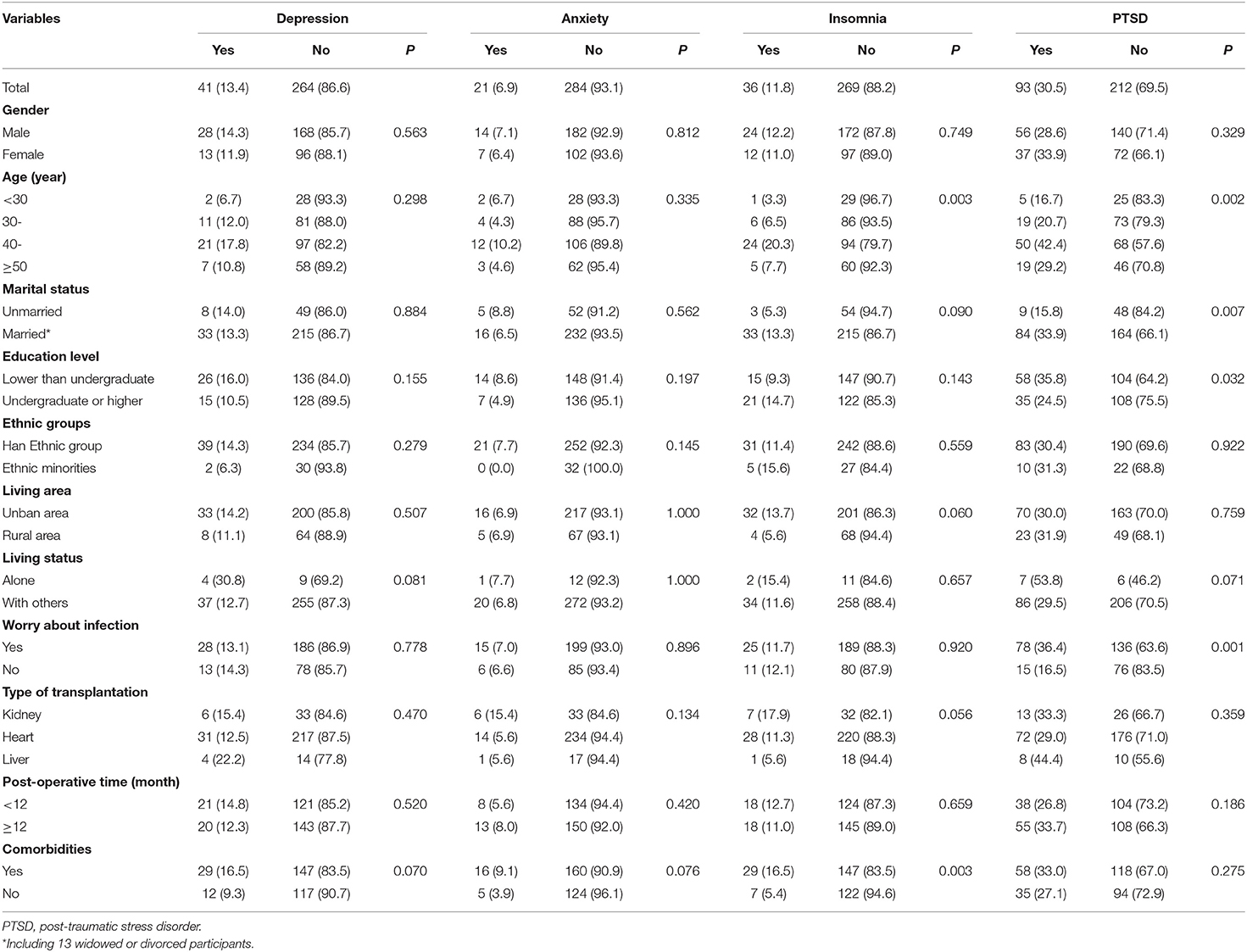
Psychological Distress
Table 2 presents the status of psychological distress in organ transplant recipients during the COVID-19 pandemic. The estimated prevalence of depression, anxiety, insomnia, and PTSD was 13.4, 6.9, 11.8, and 30.5%, respectively. Older organ transplant recipients had a higher prevalence of insomnia than younger ones. Participants with comorbidities had a higher prevalence of insomnia than those without. A higher prevalence of PTSD was observed in those of older age, married, having an education level lower than undergraduate, and being worried about infection compared to their respective counterparts.
QoL
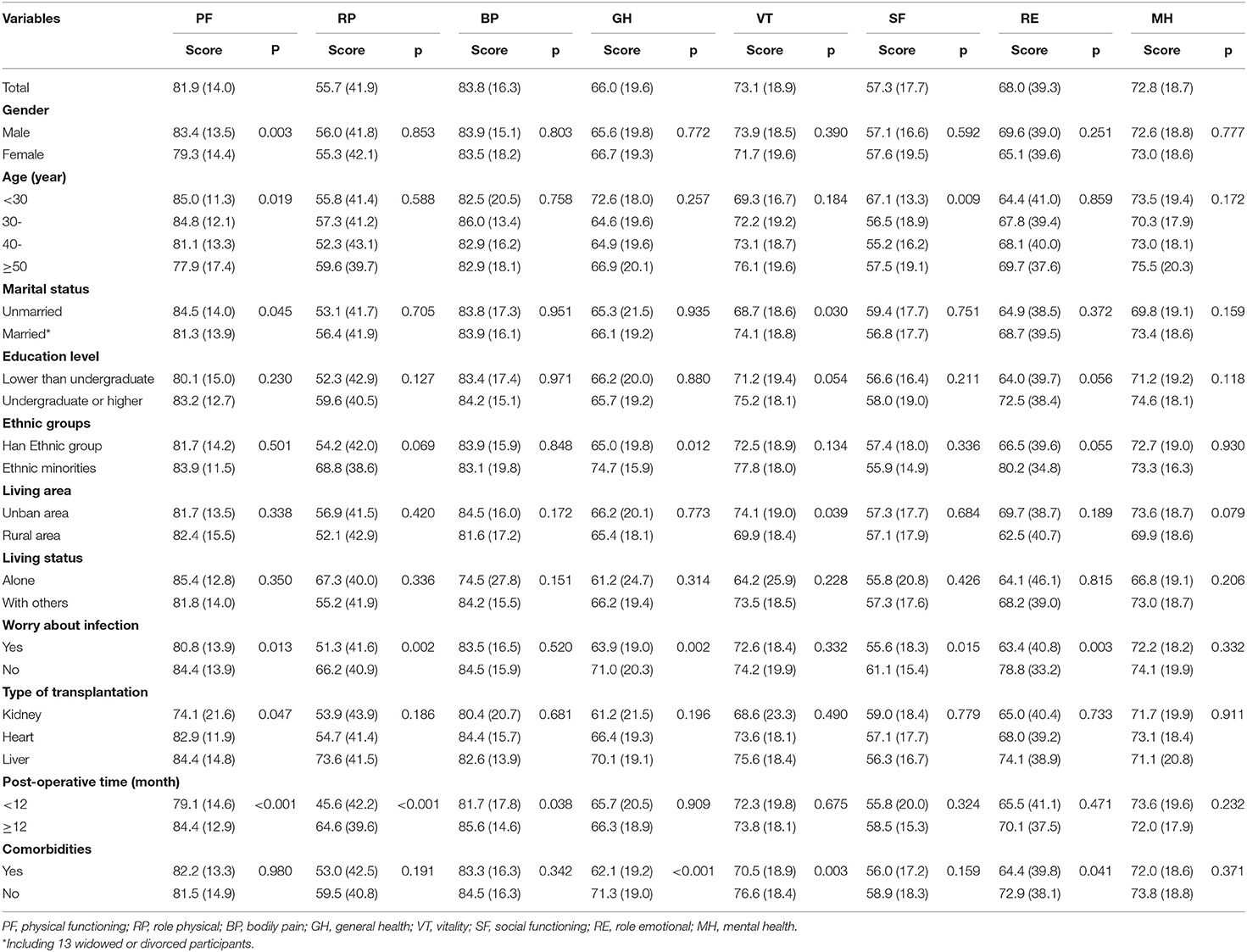
Table 3 displays the status of QoL in organ transplant recipients during the COVID-19 pandemic. The mean scores (standard deviation) for the eight SF-36 dimensions (PF, RP, BP, GH, VT, SF, RE, and MH) were 81.9 (14.0), 55.7 (41.9), 83.8 (16.3), 66.0 (19.6), 73.1 (18.9), 57.3 (17.7), 68.0 (39.3), and 72.8 (18.7). Males had higher PF scores compared with females. Younger participants had higher PF and SF scores than older ones. Unmarried participants had higher PF scores and lower VT scores than their counterparts. Those worried about infection had lower scores on PF, RP, GH, SF, and RE than those who were not worried. Participants who had undergone organ transplantation within 1 year had lower scores on PF and RP compared with those who had undergone transplantation more than 1 year before. Lower GH, VT, and RE scores were observed in participants with comorbidities compared with those without.
Association of Psychological Distress With QoL
Table 4 shows the results regarding the association of psychological distress with QoL in organ transplant recipients during the COVID-19 pandemic. Organ transplant recipients with depression had significantly lower scores in all eight dimensions of QoL compared with those without depression (all p < 0.05). Lower scores on RP, BP, GH, VT, RE, and MH were found in organ transplant recipients with anxiety, insomnia, or PTSD compared with those without the respective disorder (all p < 0.05).
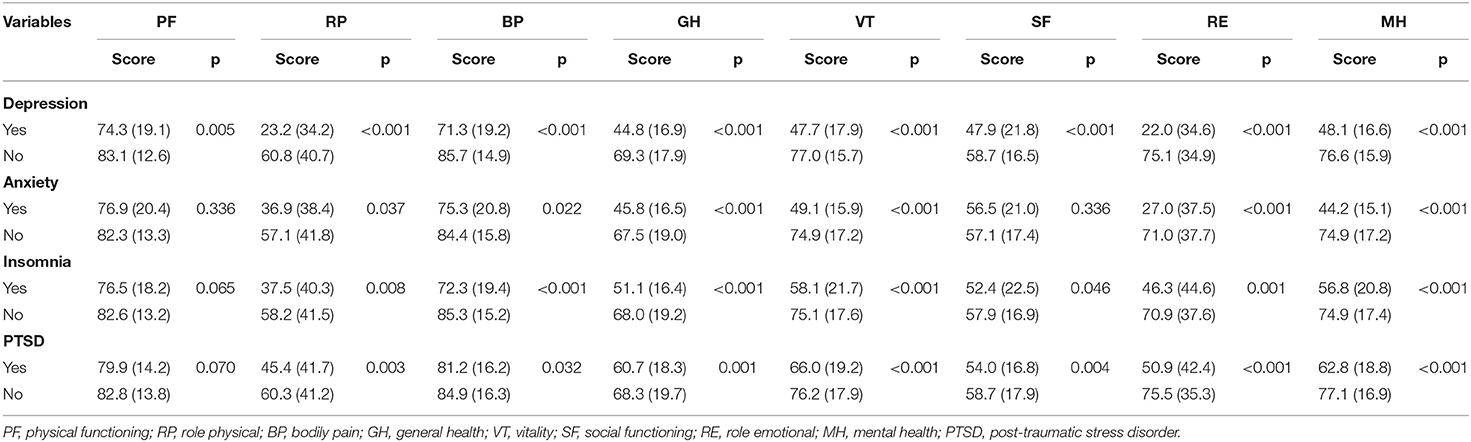
Table 4. Association of psychological distress with quality of life in organ transplant recipients during COVID-19 pandemic.
Discussion
In this study, the estimated prevalence of depression, anxiety, insomnia, and PTSD in organ transplant recipients was 13.4, 6.9, and 11.8, and 30.5%, respectively. Overall, during the COVID-19 pandemic, organ transplant recipients with psychological distress had poorer QoL than those without psychological distress. More specifically, organ transplant recipients with depression experienced poorer QoL in all the eight dimensions of SF-36 than those without depression, and organ transplant recipients with anxiety, insomnia, and PTSD showed reduced performance in six dimensions of SF-36, namely RP, BP, GH, VT, RE, and MH, relative to their counterparts without the respective disorder. The prevalence of depression and anxiety in organ transplant recipients was in consistent with previous studies, which reported a prevalence of depression ranging from 13 to 37% (17), and a prevalence of anxiety ranging from 3 to 18% (18, 30). The prevalence of PTSD in organ transplant recipients seemed to be higher than that in a prospective cohort study, which found that the prevalence of PTSD in liver transplant recipients before transplantation and at 1-year post-transplantation was 10.5 and 6.3%, respectively (31). It has been suggested that more organ transplant recipients suffered from PTSD during the COVID-19 pandemic compared with normal conditions (31). However, the difference in PTSD prevalence might be partially attributed to variations in study populations, assessment tools, and the time of assessment. When compared with general population, organ transplant recipients had higher prevalence of depression and insomnia, lower prevalence of anxiety, and similar prevalence of PTSD, during the same stage of COVID-19 pandemic in China (32, 33).
Organ transplant recipients have been found to exhibit various forms of psychological distress such as depression, anxiety, and stress associated with physical and psychosocial stress factors such as life-threatening illness, transplant surgery, pain, and intensive care unit stays with mechanical ventilation and possible delirium (11). Although psychological problems may decrease after transplantation as patient outcomes and QoL improve (34), one-third of heart transplant recipients experienced high levels of psychological distress in the year following transplantation (35, 36). Notably, being a public health emergency, the COVID-19 pandemic has had a significant psychological impact on both the general population and healthcare workers. Prior to this study, the status of psychological distress in transplant recipients during the COVID-19 pandemic was unknown. Since this study found that psychological distress is prevalent in organ transplant recipients, we therefore suggest that more attention be paid to the mental health status of this patient population and social support be provided for them during the COVID-19 pandemic.
QoL in organ transplant recipients could be improved post-transportation. Based on a review, in all included studies that used the SF 36 to assess QoL, the PF scores of elderly transplant recipients were significantly higher compared to their age-adjusted norms, while the BP, GH, VT, SF, RE, and MH scores did not differ significantly (37). This has brought hope for organ transplant recipients to reach an acceptable level of QoL after transplantation. However, the QoL in organ transplant recipients could be affected by several factors, such as age, educational level, employment status, family support, and negative emotional states (38). In this study, we provided evidence that symptoms of depression, anxiety, insomnia, and PTSD were associated with poorer QoL in organ transplant recipients. Our findings highlight the importance of implementing essential measures to relieve organ transplant recipients' psychological distress and improve their QoL.
To the best of our knowledge, this is the first study to assess the status of psychological distress and its association with QoL in organ transplant recipients during the COVID-19 pandemic. However, our study had several limitations. We analyzed cross-sectional data from a limited number of participants, and all the variables were self-reported; thus, there is a possibility of recall and misclassification bias, which may lead to misleading results. In addition, our study was conducted during the COVID-19 pandemic, and there was no baseline data that obtained before the outbreak of COVID-19; therefore, we could not assess whether or not the status of psychological distress in organ transplant recipients was more severe during the COVID-19 pandemic. Moreover, the prevalence of psychological distress may decline over time after transplantation; therefore, the present findings should be further confirmed using longitudinal data.
Conclusions
In conclusion, the current study indicated that psychological distress was prevalent in organ transplant recipients during the COVID-19 pandemic. Moreover, organ transplant recipients with depression, anxiety, insomnia, and PTSD had poorer QoL than their counterparts without the respective disorder. Timely psychological counseling, COVID-19 related health education, and essential community medical services should thus be provided to organ transplant recipients to relieve their psychological distress, and improve their QoL.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Clinical Research Ethics Committee of Renmin Hospital of Wuhan University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors contributed substantially to the conception and design, reviewed the manuscript, and approved the submitted version of the manuscript.
Funding
This work was supported by the National Key R & D Program of China (2018YFC1314600) as a grant for ZL, from the Ministry of Science and Technology of People's Republic of China (URL: http://www.most.gov.cn/). The funder played no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors wish to express their gratitude to all investigators and participants of the studies included in this analysis.
References
1. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497-506. doi: 10.1016/S0140-6736(20)30183-5
2. World Health Organization. (2021). Available online at: https://covid19.who.int/ (accessed March 31, 2021).
3. Bo H-X, Li W, Yang Y, Wang Y, Zhang Q, Cheung T, et al. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. (2020) 1-7. doi: 10.1017/S0033291720000999
4. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Network Open (2020) 3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976
5. Serafini G, Gonda X, Canepa G, Pompili M, Rihmer Z, Amore M, et al. Extreme sensory processing patterns show a complex association with depression, and impulsivity, alexithymia, and hopelessness. J Affect Disord. (2017) 210:249-57. doi: 10.1016/j.jad.2016.12.019
6. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - a systematic review and meta-analysis. Psychiatry Res. (2020) 291:113190. doi: 10.1016/j.psychres.2020.113190
7. Amerio A, Bianchi D, Santi F, Costantini L, Odone A, Signorelli C, et al. Covid-19 pandemic impact on mental health: a web-based cross-sectional survey on a sample of Italian general practitioners. Acta Bio-Med. (2020) 91:83-8. doi: 10.23750/abm.v91i2.9619
8. Cornet AD, Issa AI, van de Loosdrecht AA, Ossenkoppele GJ, Strack van Schijndel RJ, Groeneveld AB. Sequential organ failure predicts mortality of patients with a haematological malignancy needing intensive care. Eur J Haematol. (2005) 74:511-6. doi: 10.1111/j.1600-0609.2005.00418.x
9. Poves Prim I, Fabregat Pous J, García Borobia FJ, Jorba Martí R, Figueras Felip J, Jaurrieta Mas E. Early onset of organ failure is the best predictor of mortality in acute pancreatitis. Rev Esp Enferm Dig. (2004) 96:705-9, 709-13. doi: 10.4321/S1130-01082004001000005
10. Gezginci E, Kosucu SN, Goktas S, Sahin E. Relationship between depression and healthy lifestyle behaviors of patients with history of transplant. Transplant Proc. (2019) 51:2367-72. doi: 10.1016/j.transproceed.2019.01.185
11. Davydow DS, Lease ED, Reyes JD. Posttraumatic stress disorder in organ transplant recipients: a systematic review. Gen Hosp Psychiatry. (2015) 37:387-98. doi: 10.1016/j.genhosppsych.2015.05.005
12. Yu XY, Wang Y, Zhong H, Dou QL, Song YL, Wen H. Diagnostic value of serum procalcitonin in solid organ transplant recipients: a systematic review and meta-analysis. Transplant Proc. (2014) 46:26-32. doi: 10.1016/j.transproceed.2013.07.074
13. Klindtworth K, Oster P, Hager K, Krause O, Bleidorn J, Schneider N. Living with and dying from advanced heart failure: understanding the needs of older patients at the end of life. BMC Geriatr. (2015) 15:125. doi: 10.1186/s12877-015-0124-y
14. Czyzewski L, Frelik P, Wyzgal J, Szarpak L. Evaluation of quality of life and severity of depression, anxiety, and stress in patients after kidney transplantation. Transplant Proc. (2018) 50:1733-7. doi: 10.1016/j.transproceed.2018.04.026
15. Parmar A, Vandriel SM, Ng VL. Health-related quality of life after pediatric liver transplantation: a systematic review. Liver Transpl. (2017) 23:361-74. doi: 10.1002/lt.24696
16. Beilby S, Moss-Morris R, Painter L. Quality of life before and after heart, lung and liver transplantation. N Z Med J. (2003) 116:U381.
17. Kugler C, Bara C, von Waldthausen T, Einhorn I, Haastert B, Fegbeutel C, et al. Association of depression symptoms with quality of life and chronic artery vasculopathy: a cross-sectional study in heart transplant patients. J Psychosom Res. (2014) 77:128-34. doi: 10.1016/j.jpsychores.2014.06.007
18. Dew MA, Kormos RL, DiMartini AF, Switzer GE, Schulberg HC, Roth LH, et al. Prevalence and risk of depression and anxiety-related disorders during the first three years after heart transplantation. Psychosomatics. (2001) 42:300-13. doi: 10.1176/appi.psy.42.4.300
19. Suryavanshi N, Kadam A, Dhumal G, Nimkar S, Mave V, Gupta A, et al. Mental health and quality of life among healthcare professionals during the COVID-19 pandemic in India. Brain Behav. (2020) 10:e01837. doi: 10.1002/brb3.1837
20. Wang Y, Tang S, Yang C, Ma S, Bai H, Cai Z, et al. Psychological intervention in Fangcang shelter hospitals for COVID-19 in China. Psychiatry Clin Neurosci. (2020) 74:618-9. doi: 10.1111/pcn.13149
21. Wang Y, Ma S, Yang C, Cai Z, Hu S, Zhang B, et al. Acute psychological effects of Coronavirus Disease 2019 outbreak among healthcare workers in China: a cross-sectional study. Transl Psychiatry. (2020) 10:348. doi: 10.1038/s41398-020-01031-w
22. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606-13. doi: 10.1046/j.1525-1497.2001.016009606.x
23. Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092-7. doi: 10.1001/archinte.166.10.1092
24. Bastien CH, Vallieres A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297-307. doi: 10.1016/S1389-9457(00)00065-4
25. Wu KK, Chan KS. The development of the Chinese version of impact of event scale–revised (CIES-R). Soc Psychiatry Psychiatr Epidemiol. (2003) 38:94-8. doi: 10.1007/s00127-003-0611-x
26. Yu DS. Insomnia severity index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. (2010) 66:2350-9. doi: 10.1111/j.1365-2648.2010.05394.x
27. Tong X, An D, McGonigal A, Park SP, Zhou D. Validation of the Generalized Anxiety Disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. (2016) 120:31-6. doi: 10.1016/j.eplepsyres.2015.11.019
28. Chen S, Fang Y, Chiu H, Fan H, Jin T, Conwell Y. Validation of the nine-item Patient Health Questionnaire to screen for major depression in a Chinese primary care population. Asia Pac Psychiatry. (2013) 5:61-8. doi: 10.1111/appy.12063
29. Li L, Wang HM, Shen Y. Chinese SF-36 health survey: translation, cultural adaptation, validation, and normalisation. J Epidemiol Commun Health. (2003) 57:259. doi: 10.1136/jech.57.4.259
30. Dew MA, DiMartini AF, DeVito Dabbs AJ, Fox KR, Myaskovsky L, Posluszny DM, et al. Onset and risk factors for anxiety and depression during the first 2 years after lung transplantation. Gen Hosp Psychiatry. (2012) 34:127-38. doi: 10.1016/j.genhosppsych.2011.11.009
31. Annema C, Drent G, Roodbol PF, Metselaar HJ, Van Hoek B, Porte RJ, et al. A prospective cohort study on posttraumatic stress disorder in liver transplantation recipients before and after transplantation: prevalence, symptom occurrence, and intrusive memories. J Psychosom Res. (2017) 95:88-93. doi: 10.1016/j.jpsychores.2017.01.012
32. Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. (2020) 87:40–8. doi: 10.1016/j.bbi.2020.04.028
33. Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. (2020) 3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053
34. Cannavo A, Passamonti SM, Vincenti D, Aurelio MT, Torelli R, Poli F, et al. Quality of life before and after transplantation in solid organ recipients referred to the North Italy transplant program (NITp): a cross-sectional study. Transplant Proc. (2019) 51:1692-8. doi: 10.1016/j.transproceed.2019.02.034
35. Crawford I, Hogan T, Silverman MJ. Effects of music therapy on perception of stress, relaxation, mood, and side effects in patients on a solid organ transplant unit: a randomized effectiveness study. Arts Psychother. (2013) 40:224-9. doi: 10.1016/j.aip.2013.02.005
36. Dew MA, Roth LH, Schulberg HC, Simmons RG, Kormos RL, Trzepacz P, et al. Prevalence and predictors of depression and anxiety-related disorders during the year after heart transplantation. Gen Hosp Psychiatry. (1996) 18:S48-61. doi: 10.1016/S0163-8343(96)00077-1
37. Kniepeiss D, Wagner D, Pienaar S, Thaler HW, Porubsky C, Tscheliessnigg KH, et al. Solid organ transplantation: technical progress meets human dignity a review of the literature considering elderly patients' health related quality of life following transplantation. Ageing Res Rev. (2012) 11:181-7. doi: 10.1016/j.arr.2011.06.003
Keywords: coronavirus disease, organ transport, psychological distress, quality of life, cross-sectional study
Citation: Cai Z, Cai X, Song Y, Wang D, Zhang Y, Ma S, Tang S, Bai H, Tan H, Li R, Yao L, Liu Z, Wang G and Wang Y (2021) Psychological Distress and Its Association With Quality of Life in Organ Transplant Recipients During COVID-19 Pandemic. Front. Psychiatry 12:690295. doi: 10.3389/fpsyt.2021.690295
Received: 02 April 2021; Accepted: 27 May 2021;
Published: 24 June 2021.
Edited by:
Elnara Shafiyeva, Baku State University, AzerbaijanReviewed by:
Alessandro Rossi, University of Siena, ItalyGianluca Serafini, San Martino Hospital (IRCCS), Italy
Copyright © 2021 Cai, Cai, Song, Wang, Zhang, Ma, Tang, Bai, Tan, Li, Yao, Liu, Wang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ying Wang, d2FuZ3lpbmdAd2h1LmVkdS5jbg==; Gaohua Wang, d2doNjQwMkAxNjMuY29t
 Zhongxiang Cai1
Zhongxiang Cai1 Simeng Ma
Simeng Ma Zhongchun Liu
Zhongchun Liu