- 1Department of Psychiatry, National Clinical Research Center for Mental Disorders, and National Center for Mental Disorders, The Second Xiangya Hospital of Central South University, Changsha, Hunan, China
- 2The Second Affiliated Hospital, Hunan University of Chinese Medicine, Changsha, Hunan, China
Introduction: Mental health issues such as insomnia may exhibit unique interaction patterns among high-stress populations, with educational attainment potentially playing a distinctive role. However, the current mental health status of researchers at the forefront of scientific advancement has not garnered widespread attention. This study tested whether anxiety and psychological resilience jointly mediate the association between insomnia and depressive symptoms among Chinese researchers, and whether these pathways are moderated by educational attainment.
Methods: A cross-sectional online survey was conducted among researchers from 19 provinces in China between September and November 2023, and valid responses from 645 participants were analyzed using the Insomnia Severity Index, the Generalized Anxiety Disorder-7 as a measure of generalized anxiety symptoms, the Patient Health Questionnaire-9, and the Connor–Davidson Resilience Scale. Partial correlation and chain mediation analysis were applied to examine the relationships between insomnia, anxiety, resilience, and depression, while multi-group structural equation modeling (SEM) assessed differences between researchers with and without doctoral degrees.
Results: The proportion meeting the ISI screening threshold (≥ 8) was higher in researchers aged ≥ 40 and in those with doctoral degrees. In mediation models, insomnia severity demonstrated a direct association with depressive symptoms (effect: 38.31%) and indirect associations via anxiety and resilience (total effect: 61.69%). Specifically, the chain mediation effect formed by anxiety and resilience showed a suppressing effect of 0.66%, while the independent mediating effects of anxiety and resilience were 64.36% (enhancing effect) and 2.01% (suppressing effect), respectively. Multi-group SEM analyses further revealed stronger anxiety-resilience-depression linkages in researchers without doctoral degrees, highlighting their heightened vulnerability.
Discussion: Overall, insomnia is centrally associated with depression among researchers through a dual pathway involving anxiety and resilience, with the protective role of resilience being more complex among non-doctoral researchers, underscoring the need for targeted interventions such as sleep hygiene programs and resilience training to mitigate mental health risks in academic settings.
Introduction
Scientific researchers constitute a professional group at heightened risk of psychological distress, with higher rates of insomnia, anxiety, and depression compared to the general workforce (1). Similar patterns have been observed in other cognitively intensive occupational groups such as female scientists (2) and healthcare workers (3), underscoring that such professionals face heightened vulnerability in sleep and mood disturbances. Although demanding workloads, competitive promotion requirements being widely recognized as external pressures, mental health levels are the central concern requiring attention, which remain insufficiently investigated in this population. Recent large-scale studies indicate that psychological morbidity among researchers is not only more prevalent than in many other professional groups, but also tends to be more persistent, underscoring the need for exploring its underlying mechanisms (4, 5).
Insomnia has been a salient risk factor in this context. Beyond its high prevalence in knowledge-intensive populations, insomnia is now established as a causal antecedent for depression (6). Longitudinal and meta-analytic evidence across diverse cohorts consistently shows that sleep disturbances predict subsequent onset of depressive symptoms (7, 8). Existing mechanism studies indicate that sleep disorders trigger excessive vigilance, cognitive-emotional dysregulation, and impair prefrontal control functions, which in turn lead to the generation of negative emotions (9). These findings suggest that sleep problems may serve as an early warning sign for broader mental health vulnerabilities among researchers.
Generalized anxiety symptoms represent another critical dimension of mental health status. It is frequently observed as a comorbidity of both insomnia and depression and often precedes the onset of depressive episodes (10). Anxiety symptoms may aggravate sleep disorders by perpetuating hypervigilance and increasing emotional vulnerability, thereby accelerating the transition from insomnia to depression. Existing studies employ the Generalized Anxiety Disorder-7 (GAD-7) scale as a method for screening anxiety symptoms, thus, this study utilizes this scale to assess the level of the anxiety dimension (11). At the same time, psychological resilience has been widely recognized as a protective factor that buffers the influences of stress and sleep disruption (12). It is generally accepted that well resilient individuals often demonstrate more flexible emotion regulation and better recovery from negative experiences, which can mitigate the escalation of distress into depression.
Importantly, longitudinal evidence indicates a reciprocal association between anxiety and resilience (13). In this three-wave cross-lagged study, higher anxiety predicted subsequent reductions in resilience, whereas greater resilience predicted lower later anxiety and depression. Similar studies also indicate that resilience can buffer the mental-health impact of stressors, by moderating the association between pandemic-related impact and anxiety symptoms (14). Occupational studies in medical staff and other frontline workers have reported chain-mediation models, in which pathways of elevated anxiety together with diminished resilience indirectly lead to depression (1, 15). Such findings provide preliminary support for an interactive model of mental health factors, yet this mechanism has rarely been tested among academic researchers, whose psychological profiles may be distinct.
Against this backdrop, we attempt to construct a chained mediation model of mental health levels among Chinese academic researchers, examining how anxiety and psychological resilience mediate the association between insomnia and depressive symptoms. Based on prior evidence, insomnia is expected to show a positive association with depressive symptoms. More critically, we aimed to test an indirect pathway in which higher insomnia is related to heightened anxiety, and resilience further contributes to the link with depression. Furthermore, we examine whether these pathways vary with educational attainment, and recognize that higher educational level may shape distinct psychological processes. By delineating these direct and indirect pathways in academic researchers, the study seeks to clarify how sleep disturbance, anxiety, and resilience interrelate, offering recommendations and references for prevention and intervention methods regarding mental health issues for researchers and research institutions.
Methods
Participants and procedure
We conducted an anonymous, cross-sectional online survey of university-affiliated researchers across 19 provinces in China from September 1 to November 21, 2023. This study was conducted in accordance with the ethical principles of the Declaration of Helsinki and its later amendments. The study protocol received approval from the Ethics Committee of the Second Xiangya Hospital. Participants provided electronic informed consent prior to their involvement. Participation was entirely voluntary, and respondents retained the right to withdraw at any time without penalty. Eligible participants were required to hold a full-time or part-time research position at a Chinese university, college, or research institute, encompassing roles such as postdoctoral researchers, faculty, and research staff. Additionally, they were required to have engaged in research-related work during their employment with 18 ≤ age ≤ 65. Individuals who were full-time students without a formal research appointment, international scholars in China primarily for temporary training, or those unable to provide informed consent were excluded from the study. After data collection, we implemented strict quality control procedures. 1) All questions were set as mandatory, and incomplete questionnaires were not collected. 2) A minimum completion time of > 80 seconds was established as a reasonable threshold. 3) For the scale sections, the standard deviation (SD) of responses from each participant was calculated, and questionnaires with an SD of 0 were excluded. Two independent reviewers evaluated whether the questionnaires met the inclusion criteria, and any discrepancies were resolved by a third researcher.
Self-reported general information
A self-developed form collected demographics and background information, including age, gender, education level (doctoral vs non-doctoral), professional title, research output, and work environment.
Psychometric scales
For assessment of insomnia symptoms, the Insomnia Severity Index (ISI) (16, 17) was used. The ISI contains 7 items assessing insomnia severity, with total scores ranging from 0 to 28. Scores ≥ 8 indicated screening-defined insomnia. Cronbach’s α in this study was 0.925. Additionally, the Generalized Anxiety Disorder 7-item Scale (GAD-7) (18–20) was selected for assessment of anxiety symptoms;This 7-item scale was initially developed to screen for generalized anxiety disorder but has been widely validated as a dimensional measure of general anxiety symptom severity in both clinical and non-clinical populations. Scores from 0 to 21 and higher scores reflect greater anxiety severity. A cutoff of ≥ 5 indicated screening-defined anxiety symptoms. Cronbach’s α was 0.932. For assessment of depressive symptoms, the Patient Health Questionnaire 9-item Scale (PHQ-9) (21, 22). The PHQ consists of 9 items evaluating depressive symptoms. Scores ≥ 5 indicated the presence of depression. Cronbach’s α was 0.951. Meanwhile, regarding assessment of psychological resilience, the 10-item version of the Connor-Davidson Resilience Scale (CD-RISC) (12, 23, 24) was utilized to measure the level of psychological resilience among participants, and after verification, its Cronbach’s α coefficient in this study was 0.954, achieving an excellent standard of internal consistency reliability.
Statistical analyses
Analyses were performed in SPSS 26.0; figures were generated in GraphPad Prism 8. Categorical variables were compared using chi-square tests (or Fisher’s exact where cell counts were small). Because scale scores (PHQ, GAD, and ISI) deviated from normality, between-group differences were assessed with Mann–Whitney U tests; results are presented alongside medians and IQRs. Two-sided significance was set at p<0.05.
Prior to performing correlation analysis, we conducted Harman’s single-factor test on all scale items as an exploratory screen for common-method variance given the conceptual proximity of anxiety and depression constructs. We then estimated partial correlations among ISI, GAD, PHQ, and CD-RISC, controlling for age and sex. Two-sided p values from this correlation matrix were adjusted within-family using the Benjamini–Hochberg false discovery rate (FDR), correlations were considered statistically significant at p-fdr<0.05.
Chain mediation analysis
We estimated a chain mediation model in PROCESS v4.0 (25), specifying ISI as the independent variable, PHQ as the dependent variable, and GAD (M1) and CD-RISC (M2) as mediators; age and gender were included as covariates. We used 5,000 bootstrap resamples to obtain bias-corrected 95% confidence intervals; indirect effects were considered significant when CIs did not include zero. Because the data are cross-sectional, the sequential model is used to test indirect pathways consistent with the proposed ordering; inferences are limited to statistical mediation rather than causation.
Multi-group structural equation model analysis
To assess potential differences between doctoral and non-doctoral researchers, we conducted a multi-group structural equation model (SEM) in AMOS 26, retaining the same configuration as the chain mediation model for comparability. Structural paths were constrained equal across groups, and χ² difference tests evaluated group differences.
Results
Participant characteristics
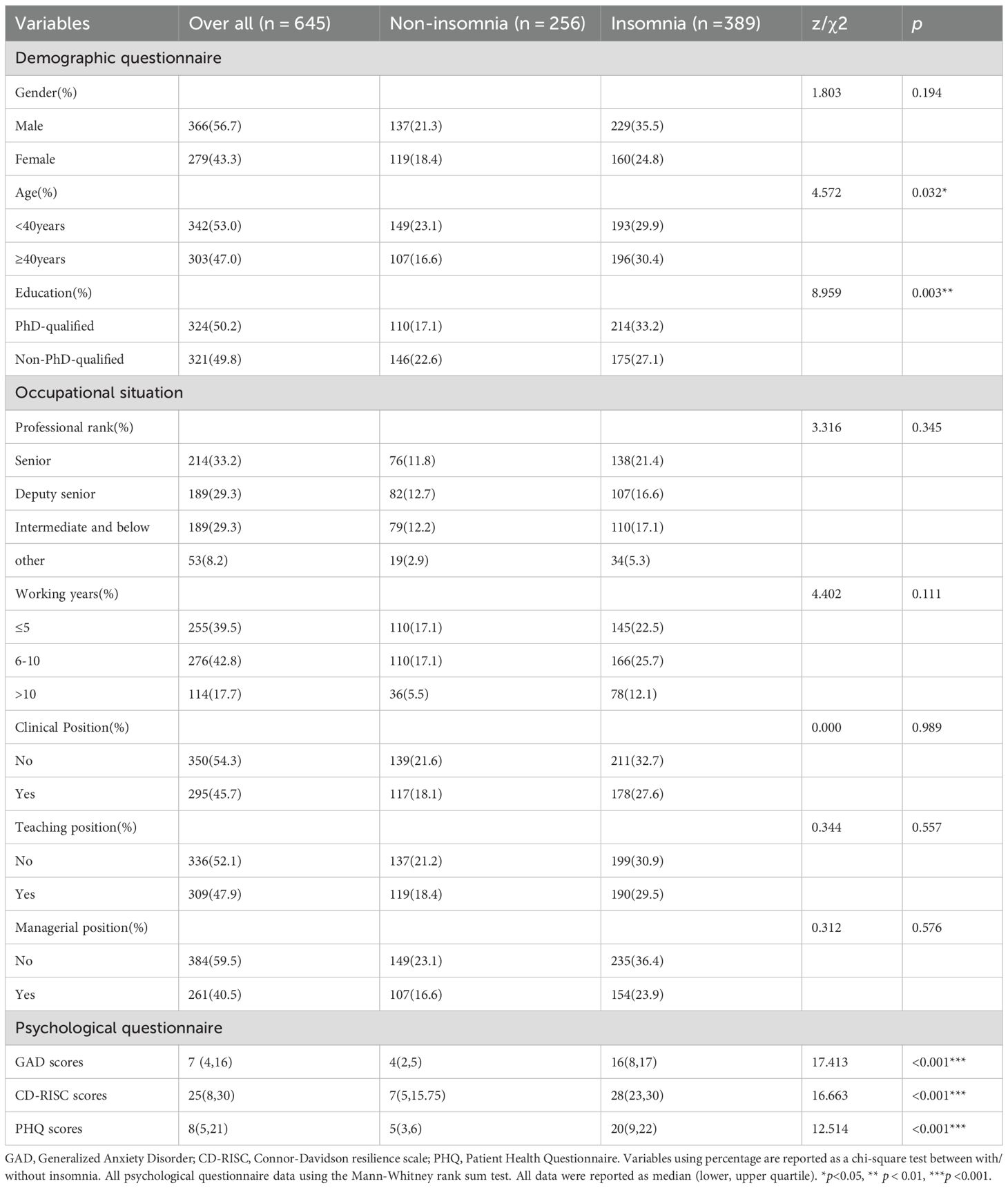
A total of 821 questionnaires were submitted, of which 645 valid responses were retained after quality control. The proportion meeting the ISI screening threshold (≥ 8) was higher in participants aged ≥ 40 than in those < 40 (64.7% vs 56.4%; χ²(1)=4.57, p = 0.032; OR = 1.41, 95%CI[1.03–1.94]) and in doctoral vs non-doctoral researchers (66.0% vs 54.5%; χ²(1)=8.96, p = 0.003; OR = 1.62, 95%CI[1.18–2.23]). No significant differences were observed in gender, professional rank, working years, or working roles. Participants who screened positive for insomnia (ISI≥8) showed higher scores on anxiety (GAD), depression (PHQ) and resilience (CD-RISC), compared with non-insomnia counterparts (all p<0.001). (Table 1; Supplementary Figure 1).
Correlation analysis
Partial correlations controlling for age and gender revealed that ISI scores were positively associated with GAD, PHQ and CD-RISC scores (all p-fdr<0.01). These associations remained consistent across subgroups defined by educational attainment (Supplementary Table 1).
Chain mediation model in the full sample
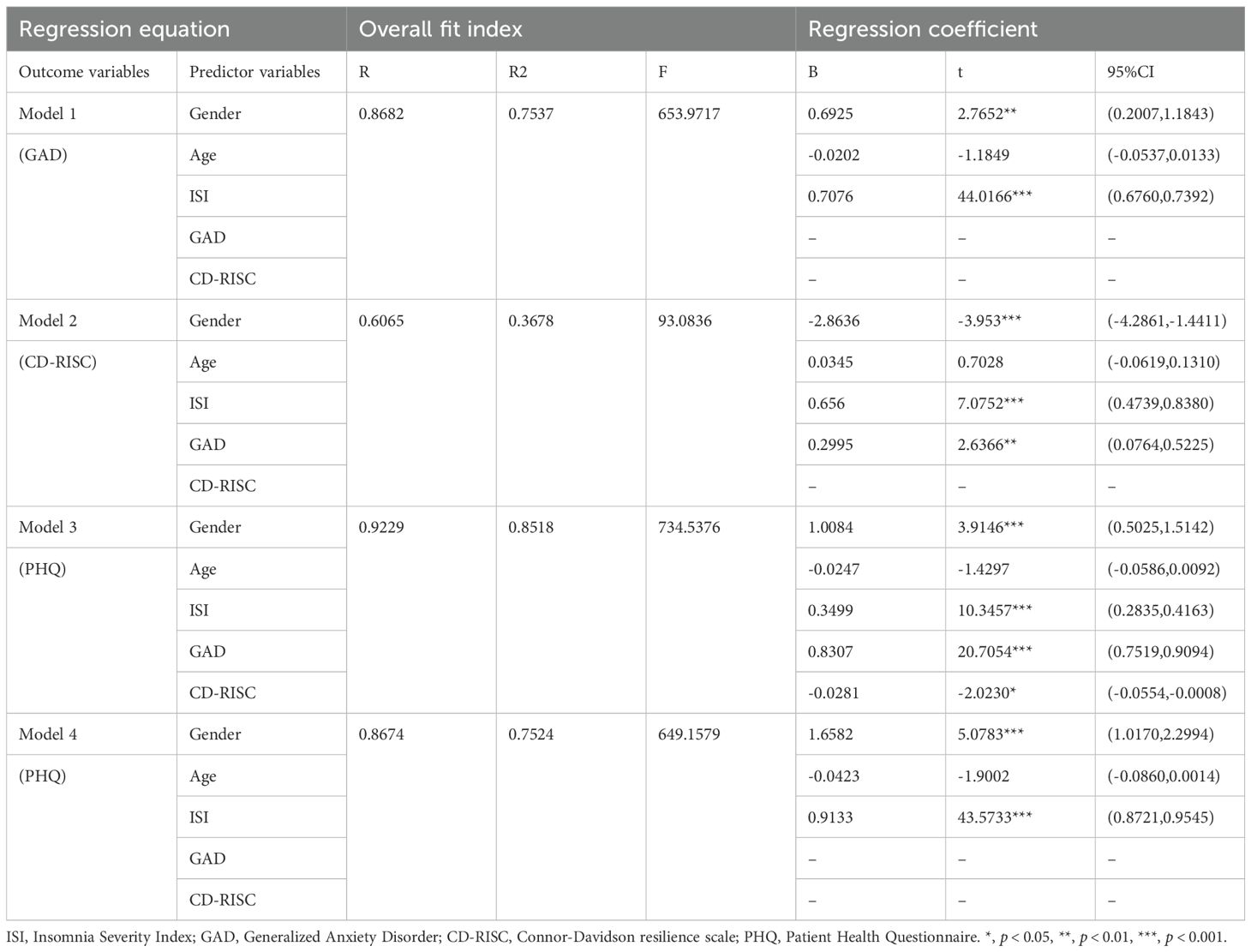
In the chain mediation model, the insomnia had a significant positive effect on anxiety (B = 0.7076, p<0.001), resilience (B = 0.6560, p<0.001) and depression (B = 0.3499, p<0.001). In turn, resilience exerted a significant negative effect on depression (B=–0.0281, p<0.05) (Table 2, Figure 1). The indirect effect was further confirmed using bootstrapping with 5,000 resamples, and the 95% confidence interval excluded zero, indicating robust mediation effects (Figure 1).
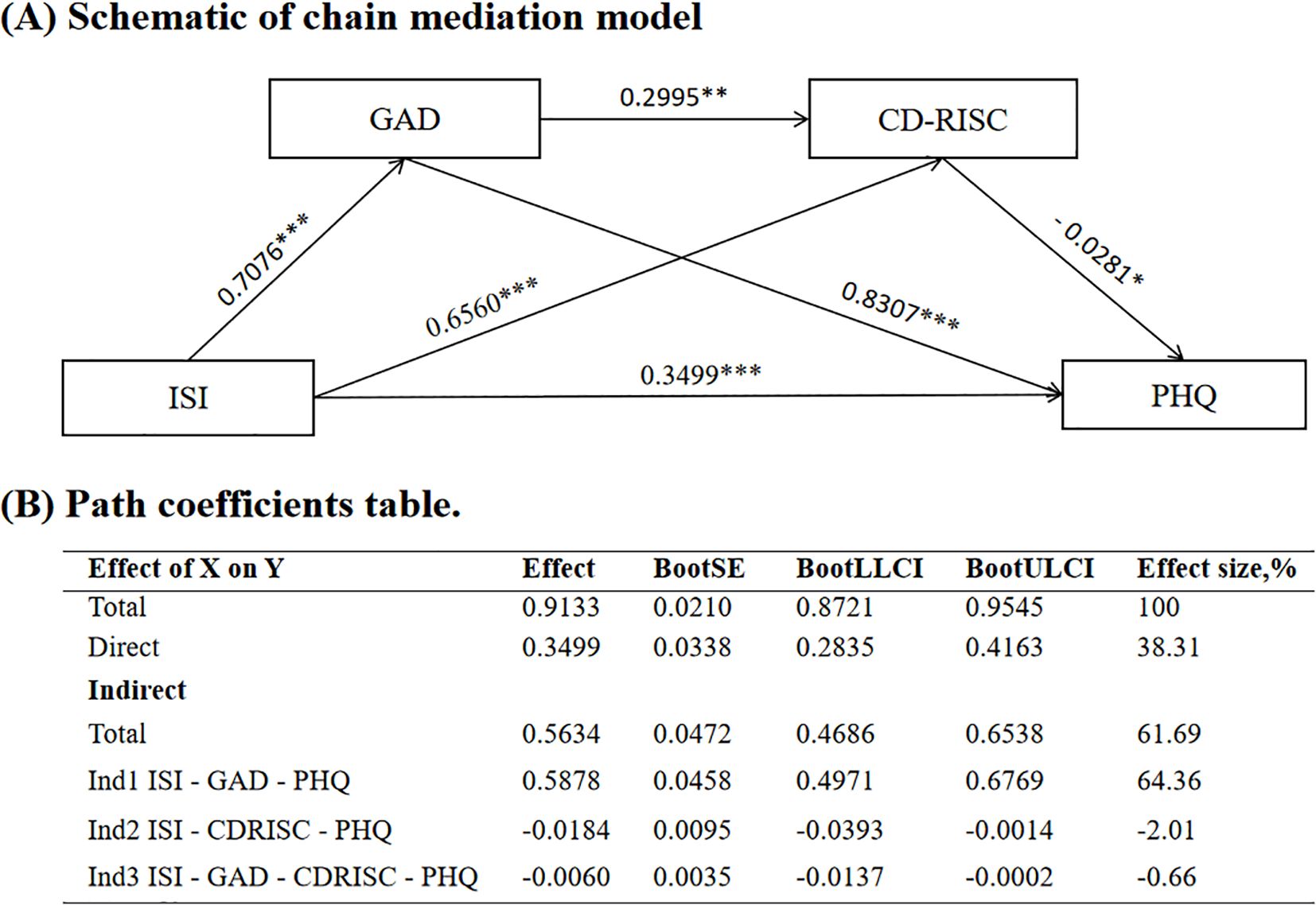
Figure 1. Mediation model of anxiety and resilience between insomnia and depression. (A) Schematic of chain mediation model; (B) Path coefficients table. ISI, Insomnia Severity Index; GAD, Generalized Anxiety Disorder; CD-RISC, Connor-Davidson resilience scale; PHQ, Patient Health Questionnaire. SE, standard error; LLCI, lower limit of confidence interval; ULCI, upper limit of confidence interval. *p < 0.05, **p < 0.01, ***p < 0.001.
Multi-group SEM analysis by education
Multi-group SEM analysis demonstrated an acceptable fit for both doctoral and non-doctoral groups (Figure 2). Among the six hypothesized structural paths, three showed significant group differences when constrained to be equal: GAD → CD-RISC (Δχ²=15.931, p<0.001), CD-RISC → PHQ (Δχ²=21.806, p<0.001), and ISI → CD-RISC (Δχ²=7.476, p = 0.006). Directionally, CD-RISC → PHQ was negative among doctoral researchers but positive among non-doctoral peers (Figure 2).
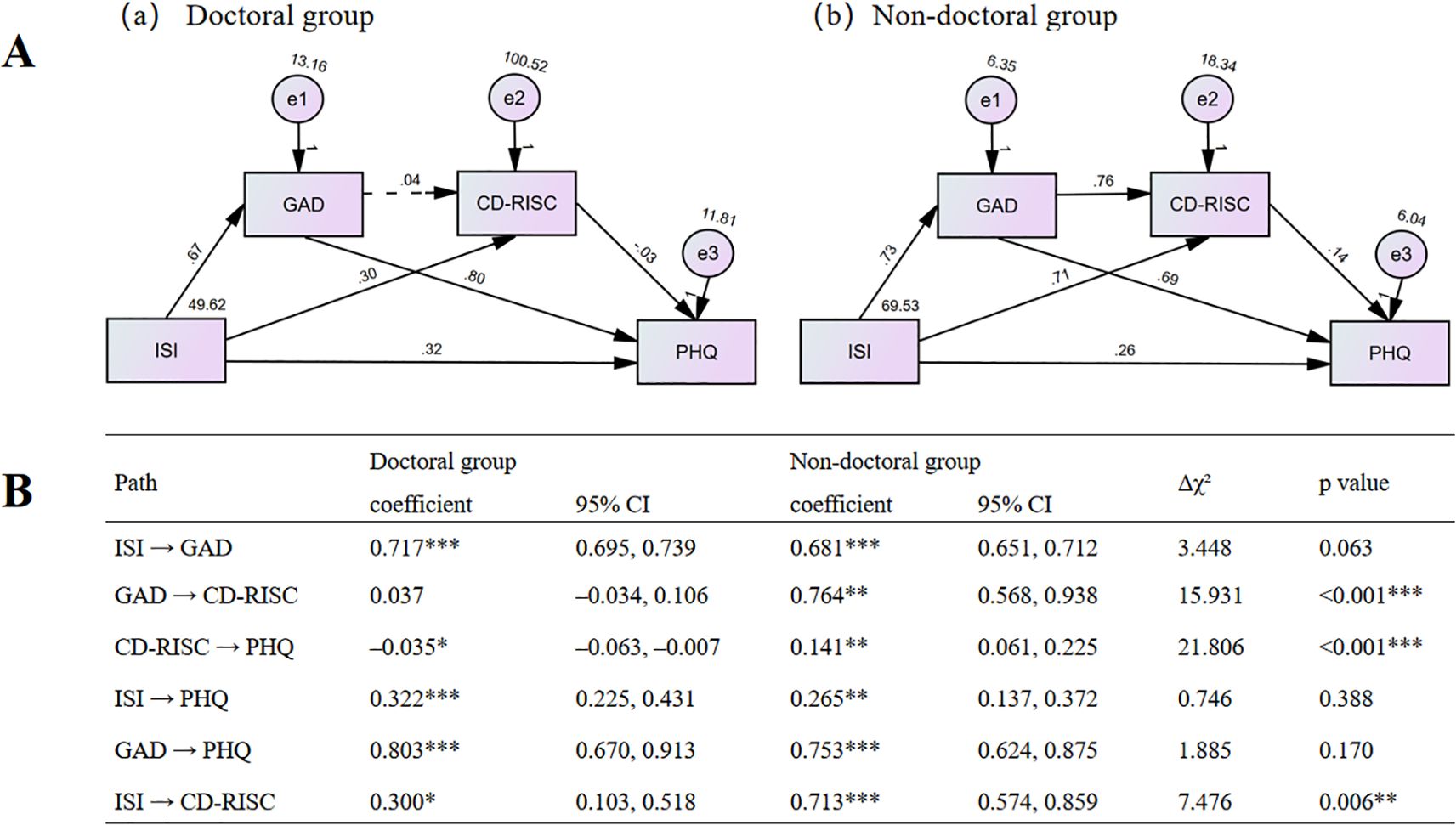
Figure 2. Path diagrams and comparative path coefficients for doctoral and non-doctoral groups. (A) Path diagrams of the M-SEM for the doctoral (a) and non-doctoral (b) groups without path constraints; (B) Path Coefficients by Group and Chi-square Difference Tests. Estimates are standardized coefficients. CI = 95% confidence interval. Δχ² is the chi-square difference between the constrained model (each path fixed equal across groups) and the unconstrained model (all paths freely estimated). All chi-square tests used df = 1. *p<0.05, **p < 0.01, ***p <0.001.
Discussion
This study examined how insomnia, anxiety, and psychological resilience jointly relate to depressive symptoms in academic researchers, and whether these relations differ by educational level. The research findings are reflected in three aspects. First, insomnia emerged as a central factor of depression, being associated with higher anxiety symptom levels among those who screened positive for insomnia, as well as with indirect statistical associations from sleep disturbance to affective symptoms in the models. Second, anxiety symptoms showed a strong indirect association of the link between insomnia and depression. Third, the role of resilience was more nuanced: while resilience explained a smaller share of indirect effects, its association with depressive symptoms varied by educational level—showing a negative path in researchers with doctoral degree but a positive path in researchers without doctoral degree in the multi-group SEM analysis. Together, these models suggest that insomnia is a central factor of mental health problems in Chinese researchers, whereas the contribution of resilience is educational level dependent.
Insomnia symptoms, as one of the most prevalent mental health issues (26, 27), can prospectively predict the onset of anxiety and depressive symptoms (28). This finding has been supported by multiple longitudinal studies and meta-analyses (29–31). In our model, severe insomnia symptoms co-occurred with higher levels of depression, and insomnia was specified as an upstream correlate; higher insomnia severity was associated with higher anxiety and with depressive symptoms. We speculate that impaired emotion regulation and circadian disruption channel sleep problems into mood dysregulation via anxiety symptoms (32). At the same time, resilience also plays a certain regulatory role in this process.
The mediation models demonstrated that anxiety symptoms accounted for the largest share of the indirect association between insomnia and depressive symptoms. Existing research of insomnia mechanism suggests that, persisting sleep disturbances may exacerbate cognitive–emotional processes intensify, which leading to heightened anxiety symptoms and in turn contribute to depressive burden (30). Bidirectional relationships among sleep disturbance, anxiety, and depression have been found among Chinese cohort studies, and these links are persistent (28, 31). Moreover, evidence from adolescent and young adult populations demonstrates similar sequential patterns: nightmares and sleep disruption predict cognitive deficits and suicidal ideation through combined effects of anxiety and depression (33, 34). Intervention studies provide empirical evidence: RCTs of CBT-I reduce insomnia and are often accompanied by improvements in anxiety and depression, with some studies reporting anxiety reduction as a mediator of mood change (35, 36). Further research suggests that CBT-I alters emotional brain responses by neurocognitive and circadian rhythm interventions, which also support this perspective (37, 38). Collectively, these converging strands position anxiety as a proximal and modifiable correlate of depressive outcomes in high-stress professional contexts.
We also observed a complex role of psychological resilience in the relationship between insomnia and depression among academic professionals. Multigroup structural equation modeling indicated that the moderating effect of resilience on depressive symptoms varied by educational attainment: a negative impact was observed among individuals holding a doctoral degree, whereas a positive impact emerged among those without one. This contrast may stem from differences in occupational resources and autonomy between the two groups. Possessing a doctoral degree is typically associated with greater job security, professional autonomy, and supportive networks (39). These conditions may foster the individuals resilience by promoting recovery and regulating, thereby exerting a protective effect (40). In contrast, non-doctoral researchers often face heightened job insecurity, heavier life burdens, and stronger dependence on supervisors (41, 42). Their resilience may manifest as a passive coping style characterized by endurance and perseverance which can lead to emotional exhaustion and a positive association with depressive symptoms (43, 44).
Cultural values provide a critical contextual framework for understanding how resilience is expressed among Chinese academics. Rooted in Confucian traditions that emphasize diligence, conscientiousness, and collective expectations (45), Chinese researchers often experience substantial normative pressure. Within this cultural milieu, resilience is frequently conceptualized as “endurance” or “persistence”, while emotional suppression is sometimes regarded as an appropriate form of emotion regulation (46). Such cultural expectations shape both doctoral and non-doctoral researchers alike, yet their behavioral consequences diverge due to disparities in access to resources. For those with greater autonomy and occupational security, such as doctoral scholars, perseverance can be transformed into an active and strategic form of resilience that aligns with long-term professional growth (47). Conversely, for non-doctoral researchers with limited resources and fewer alternative coping strategies, the same cultural emphasis may confine their resilience to a passive endurance mode, thereby heightening their vulnerability to psychological distress (48). Hence, culture interacts dynamically with structural factors to jointly shape the mental health outcomes of resilience (49).
Our finding underscores that the psychological benefits of resilience are not universal but are substantially moderated by occupational structure and cultural context. Accordingly, mental health interventions targeting academic populations should adopt a more precise stratified strategies. For resource-limited groups such as non-doctoral and early-career researchers, interventions should prioritize the alleviation of structural stressors, including clarifying job roles, providing transparent career development pathways, and establishing effective supervisory support systems (50–52). Building on this foundation, the implementation of evidence-based approaches such as Cognitive Behavioral Therapy for Insomnia (CBT-I) and Mindfulness-Based Stress Reduction (MBSR) may help individuals transition from passive endurance to adaptive self-regulation (53). Ultimately, institutional efforts toward equitable resource allocation and the institutionalization of a supportive research culture represent the fundamental path to ensuring the sustainable psychological well-being of the entire scientific ecosystem (54).
This study has several limitations. First, the design is cross-sectional; temporal ordering cannot be determined, and causal inferences require longitudinal and intervention designs. We specified an a priori ordering and estimated indirect associations with bias-corrected bootstraps, but longitudinal follow-ups would clarify temporal dynamics. Second, all measures were based on self-report scales, which may introduce common-method bias and underreporting of psychological distress due to social desirability or stigma surrounding mental health in academic settings. The absence of diagnostic screening for past or current psychiatric disorders also limits the ability to distinguish subclinical symptoms from clinical conditions. Future studies could combine self-report data with objective sleep indices, clinical assessments, and diagnostic screening to improve measurement precision and validity. Finally, we focused on the core pathway and did not include several work-environment variables (e.g., workload patterns, shift schedules) that could further refine effect estimates; future studies can add these to enhance the practical significance of research.
Conclusion
In conclusion, our findings support a model in which insomnia and anxiety form the principal pathway to depressive symptoms among researchers, whereas the influence of resilience varies across educational and occupational contexts. Interventions that target sleep health, reduce anxiety, and address modifiable features of the work environment—alongside calibrated resilience-building—are likely to deliver the most reliable mental-health benefit in academic settings.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Second Xiangya Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LH: Funding acquisition, Writing – original draft. YH: Data curation, Writing – original draft. BG: Data curation, Writing – original draft. TL: Visualization, Writing – original draft. PW: Visualization, Writing – original draft. MZ: Software, Writing – original draft. QR: Software, Writing – original draft. HW: Writing – review & editing. XC: Funding acquisition, Project administration, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This work was supported by the Science and Technology Innovation Projects of Hunan Province (2024RC3051) and the Fundamental Research Funds for the Central Universities of Central South University (2024ZZTS0956).
Acknowledgments
The authors sincerely thank all academic researchers who participated in the survey for their valuable time and input, and the university administrators who helped disseminate the questionnaire.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. The authors used AI-based language editing tools (ChatGPT, OpenAI, San Francisco, USA) to assist in improving the English expression. All scientific content, interpretations, results, and conclusions are completed by the authors.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1709399/full#supplementary-material
References
1. Xinjie D, Runlian H, Ahmed O, Cho E, and Chung S. Mediating role of viral anxiety and insomnia in relationship between work-related stress and depression among cold chain workers during COVID-19 pandemic. J Korean Med Sci. (2023) 38:e338. doi: 10.3346/jkms.2023.38.e338
2. Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. (1996) 1:27–41. doi: 10.1037/1076-8998.1.1.27
3. Liu Y, Zhang Q, Jiang F, Zhong H, Huang L, Zhang Y, et al. Association between sleep disturbance and mental health of healthcare workers: A systematic review and meta-analysis. Front Psychiatry. (2022) 13:919176. doi: 10.3389/fpsyt.2022.919176
4. Evans TM, Bira L, Gastelum JB, Weiss LT, and Vanderford NL. Evidence for a mental health crisis in graduate education. Nat Biotechnol. (2018) 36:282–4. doi: 10.1038/nbt.4089
6. Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. (2011) 135:10–9. doi: 10.1016/j.jad.2011.01.011
7. Hertenstein E, Feige B, Gmeiner T, Kienzler C, Spiegelhalder K, Johann A, et al. Insomnia as a predictor of mental disorders: A systematic review and meta-analysis. Sleep Med Rev. (2019) 43:96–105. doi: 10.1016/j.smrv.2018.10.006
8. Blake MJ, Trinder JA, and Allen NB. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: Implications for behavioral sleep interventions. Clin Psychol Rev. (2018) 63:25–40. doi: 10.1016/j.cpr.2018.05.006
9. Altena E, Micoulaud-Franchi JA, Geoffroy PA, Sanz-Arigita E, Bioulac S, and Philip P. The bidirectional relation between emotional reactivity and sleep: From disruption to recovery. Behav Neurosci. (2016) 130:336–50. doi: 10.1037/bne0000128
10. Alvaro PK, Roberts RM, and Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. (2013) 36:1059–68. doi: 10.5665/sleep.2810
11. Hinz A, Klein AM, Brähler E, Glaesmer H, Luck T, Riedel-Heller SG, et al. Psychometric evaluation of the Generalized Anxiety Disorder Screener GAD-7, based on a large German general population sample. J Affect Disord. (2017) 210:338–44. doi: 10.1016/j.jad.2016.12.012
12. Connor KM and Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
13. Lau WKW. The role of resilience in depression and anxiety symptoms: A three-wave cross-lagged study. Stress Health. (2022) 38:804–12. doi: 10.1002/smi.3136
14. Traunmüller C, Stefitz R, Schneider M, and Schwerdtfeger A. Resilience moderates the relationship between the psychological impact of COVID-19 and anxiety. Psychol Health Med. (2023) 28:1861–72. doi: 10.1080/13548506.2021.1955137
15. Chen D, Ni Y, Lu J, Wang Y, Qi Q, and Zhai H. Examining the impact of perceived stress, anxiety, and resilience on depression among medical staff after COVID-19 quarantine: a chain mediation analysis. Front Public Health. (2023) 11:1250623. doi: 10.3389/fpubh.2023.1250623
16. Manzar MD, Jahrami HA, and Bahammam AS. Structural validity of the Insomnia Severity Index: A systematic review and meta-analysis. Sleep Med Rev. (2021) 60:101531. doi: 10.1016/j.smrv.2021.101531
17. Bastien CH, Vallières A, and Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
18. Spitzer RL, Kroenke K, Williams JB, and Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
19. Henderson LC, Antony MM, and Koerner N. Psychometric properties of the Generalized Anxiety Disorder Inventory in a Canadian sample. J Psychopharmacol. (2014) 28:440–8. doi: 10.1177/0269881114525672
20. Basińska BA and Kwissa-Gajewska Z. Psychometric properties of the Polish version of the Generalized Anxiety Disorder Scale (GAD-7) in a non-clinical sample of employees during pandemic crisis. Int J Occup Med Environ Health. (2023) 36:493–504. doi: 10.13075/ijomeh.1896.02104
21. Kroenke K, Spitzer RL, and Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
22. Stocker R, Tran T, Hammarberg K, Nguyen H, Rowe H, and Fisher J. Patient Health Questionnaire 9 (PHQ-9) and General Anxiety Disorder 7 (GAD-7) data contributed by 13,829 respondents to a national survey about COVID-19 restrictions in Australia. Psychiatry Res. (2021) 298:113792. doi: 10.1016/j.psychres.2021.113792
23. Sharif Nia H, She L, Froelicher ES, Marôco J, Moshtagh M, and Hejazi S. Psychometric evaluation of the Connor-Davidson Resilience Scale among Iranian population. BMC Psychiatry. (2023) 23:92. doi: 10.1186/s12888-023-04580-8
24. Cheng C, Dong D, He J, Zhong X, and Yao S. Psychometric properties of the 10-item Connor-Davidson Resilience Scale (CD-RISC-10) in Chinese undergraduates and depressive patients. J Affect Disord. (2020) 261:211–20. doi: 10.1016/j.jad.2019.10.018
25. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: Guilford Press (2013).
26. Ford DE and Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? Jama. (1989) 262:1479–84. doi: 10.1001/jama.1989.03430110069030
27. Perlis ML, Posner D, Riemann D, Bastien CH, Teel J, and Thase M. Insomnia. Lancet. (2022) 400:1047–60. doi: 10.1016/S0140-6736(22)00879-0
28. Mao X, Zhang F, Wei C, Li Z, Huang C, Sun Z, et al. The impact of insomnia on anxiety and depression: a longitudinal study of non-clinical young Chinese adult males. BMC Psychiatry. (2023) 23:360. doi: 10.1186/s12888-023-04873-y
29. Li L, Wu C, Gan Y, Qu X, and Lu Z. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry. (2016) 16:375. doi: 10.1186/s12888-016-1075-3
30. Riemann D, Krone LB, Wulff K, and Nissen C. Sleep, insomnia, and depression. Neuropsychopharmacology. (2020) 45:74–89. doi: 10.1038/s41386-019-0411-y
31. Meaklim H, Saunders WJ, Byrne ML, Junge MF, Varma P, Finck WA, et al. Insomnia is a key risk factor for persistent anxiety and depressive symptoms: A 12-month longitudinal cohort study during the COVID-19 pandemic. J Affect Disord. (2023) 322:52–62. doi: 10.1016/j.jad.2022.11.021
32. Meyer N, Harvey AG, Lockley SW, and Dijk DJ. Circadian rhythms and disorders of the timing of sleep. Lancet. (2022) 400:1061–78. doi: 10.1016/S0140-6736(22)00877-7
33. Zhang LG, Cheng LF, Wang TT, Wang LL, Zhou SJ, Luo YH, et al. Chain mediating effect of insomnia, depression, and anxiety on the relationship between nightmares and cognitive deficits in adolescents. J Affect Disord. (2023) 322:2–8. doi: 10.1016/j.jad.2022.10.047
34. Guo Z, Han X, Kong T, Wu Y, Kang Y, Liu Y, et al. The mediation effects of nightmares and depression between insomnia and suicidal ideation in young adults. Sci Rep. (2024) 14:9577. doi: 10.1038/s41598-024-58774-5
35. Scott AJ, Webb TL, Martyn-St James M, Rowse G, and Weich S. Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Med Rev. (2021) 60:101556. doi: 10.1016/j.smrv.2021.101556
36. Freeman D, Sheaves B, Goodwin GM, Yu LM, Nickless A, Harrison PJ, et al. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry. (2017) 4:749–58. doi: 10.1016/S2215-0366(17)30328-0
37. Furukawa Y, Sakata M, Yamamoto R, Nakajima S, Kikuchi S, Inoue M, et al. Components and delivery formats of cognitive behavioral therapy for chronic insomnia in adults: A systematic review and component network meta-analysis. JAMA Psychiatry. (2024) 81:357–65. doi: 10.1001/jamapsychiatry.2023.5060
38. Trauer JM, Qian MY, Doyle JS, Rajaratnam SM, and Cunnington D. Cognitive behavioral therapy for chronic insomnia: A systematic review and meta-analysis. Ann Intern Med. (2015) 163:191–204. doi: 10.7326/M14-2841
39. Sauermann H and Roach M. Science PhD career preferences: levels, changes, and advisor encouragement. PloS One. (2012) 7:e36307. doi: 10.1371/journal.pone.0036307
40. Davydov DM, Stewart R, Ritchie K, and Chaudieu I. Resilience and mental health. Clin Psychol Rev. (2010) 30:479–95. doi: 10.1016/j.cpr.2010.03.003
41. Meng Q and Wang G. A research on sources of university faculty occupational stress: a Chinese case study. Psychol Res Behav Manage. (2018) 11:597–605. doi: 10.2147/PRBM.S187295
42. Cao J, Dai T, Dong H, Chen J, and Fan Y. Research on the mechanism of academic stress on occupational burnout in Chinese universities. Sci Rep. (2024) 14:12166. doi: 10.1038/s41598-024-62984-2
43. Valóta I, Rodrigo da Silva Pimentel R, Neroni Stina Saura AP, Marques da Silva R, Siqueira Costa Calache AL, and José Dos Santos M. Fatigue and resilience in Master’s and PhD students in the Covid-19 pandemic in Brazil: A cross-sectional study. PloS One. (2023) 18:e0295218. doi: 10.1371/journal.pone.0295218
44. Palagini L, Moretto U, Novi M, Masci I, Caruso D, Drake CL, et al. Lack of resilience is related to stress-related sleep reactivity, hyperarousal, and emotion dysregulation in insomnia disorder. J Clin Sleep Med. (2018) 14:759–66. doi: 10.5664/jcsm.7100
45. Oyserman D, Coon HM, and Kemmelmeier M. Rethinking individualism and collectivism: evaluation of theoretical assumptions and meta-analyses. Psychol Bull. (2002) 128:3–72. doi: 10.1037/0033-2909.128.1.3
46. Sai L, Luo S, Ward A, and Sang B. Development of the tendency to use emotion regulation strategies and their relation to depressive symptoms in chinese adolescents. Front Psychol. (2016) 7:1222. doi: 10.3389/fpsyg.2016.01222
47. Cheng P, Kalmbach DA, Hsieh HF, Castelan AC, Sagong C, and Drake CL. Improved resilience following digital cognitive behavioral therapy for insomnia protects against insomnia and depression one year later. Psychol Med. (2023) 53:3826–36. doi: 10.1017/S0033291722000472
48. Zhou S, Chen J, Lin H, Ye Y, Xiao Y, Ouyang N, et al. Associations among workplace bullying, resilience, insomnia severity, and subjective wellbeing in chinese resident doctors. Front Psychiatry. (2022) 13:840945. doi: 10.3389/fpsyt.2022.840945
49. Mei Y, Yang X, Gui J, Li Y, Zhang X, Wang Y, et al. The relationship between psychological resilience and depression among the diabetes patients under the background of “dynamic zero COVID-19”: the mediating role of stigma and the moderating role of medication burden. Front Public Health. (2023) 11:1124570. doi: 10.3389/fpubh.2023.1124570
50. Amer S, Elotla SF, Ameen AE, Shah J, and Fouad AM. Occupational burnout and productivity loss: A cross-sectional study among academic university staff. Front Public Health. (2022) 10:861674. doi: 10.3389/fpubh.2022.861674
51. Sweeney E, Cui Y, Yu ZM, Dummer TJB, DeClercq V, Forbes C, et al. The association between mental health and shift work: Findings from the Atlantic PATH study. Prev Med. (2021) 150:106697. doi: 10.1016/j.ypmed.2021.106697
52. Rehman E, Alotaibi KA, Rehman S, and Ahmad M. Effect of work schedule flexibility as a moderator in the relationship between job stress and wellbeing in pharmacy practice. Sci Rep. (2025) 15:24097. doi: 10.1038/s41598-025-10523-y
53. Brückner HA, Ell J, Kalon L, Strahler J, Ducki A, Riemann D, et al. Effectiveness of digital cognitive behavioral therapy for insomnia in nurses with shift work sleep disorder: Results of a randomized controlled trial. Int J Nurs Stud. (2025) 169:105112. doi: 10.1016/j.ijnurstu.2025.105112
Keywords: insomnia, depression, resilience, education level, researcher
Citation: Han L, He Y, Gong B, Liu T, Wen P, Zhong M, Ren Q, Wang H and Chen X (2025) Insomnia and depression in Chinese academic researchers: mediation by anxiety and resilience with differences among researchers by educational level. Front. Psychiatry 16:1709399. doi: 10.3389/fpsyt.2025.1709399
Received: 20 September 2025; Accepted: 31 October 2025;
Published: 21 November 2025.
Edited by:
Carlos Laranjeira, Polytechnic Institute of Leiria, PortugalReviewed by:
Rosa Cristina Lopes, Coimbra Nursing School, PortugalSaeid Yazdi-Ravandi, Hamadan University of Medical Sciences, Iran
Copyright © 2025 Han, He, Gong, Liu, Wen, Zhong, Ren, Wang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xudong Chen, eHVkb25nY2hlbkBjc3UuZWR1LmNu; Hui Wang, MjAyMzIwOTZAc3R1LmhudWNtLmVkdS5jbg==
 Lin Han
Lin Han Yuanrui He1
Yuanrui He1 Hui Wang
Hui Wang Xudong Chen
Xudong Chen