- 1Toronto East General Hospital, Toronto, ON, Canada
- 2Sunnybrook Health Sciences Centre, Toronto, ON, Canada
- 3Health Services, Division for Intellectual and Developmental Disabilities, National Institute of Child Health and Human Development, Ministry of Social Affairs, Jerusalem, Israel
- 4MSR Israel Center for Medical Simulation, Chaim Sheba Medical Center, Tel Hashomer National Education Center, Ramat Gan, Israel
Introduction: Newborn babies in need of critical medical attention are normally admitted to the neonatal intensive care unit (NICU). These infants tend to be preterm, have low birth weight, and/or have serious medical conditions. Neonatal survival varies, but progress in perinatal and neonatal care has notably diminished mortality rates. In this selected review, we examine and compare the NICU mortality rates and etiologies of death in different countries.
Methods: A literature search was conducted in Ovid MEDLINE, OLDMEDLINE, EMBASE Classic, and EMBASE. The primary endpoint was the mortality rates in NICUs. Secondary endpoints included the reasons for death and the correlation between infant age and mortality outcome. For the main analysis, we examined all infants admitted to NICUs. Subgroup analyses included extremely low birth weight infants (based on the authors’ own definition), very low birth weight infants, very preterm infants, preterm infants, preterm infants with a birth weight of ≤1,500 g, and by developed and developing countries.
Results: The literature search yielded 1,865 articles, of which 20 were included. The total mortality rates greatly varied among countries. Infants in developed and developing countries had similar ages at death, ranging from 4 to 20 days and 1 to 28.9 days, respectively. The mortality rates ranged from 4 to 46% in developed countries and 0.2 to 64.4% in developing countries.
Conclusion: The mortality rates of NICUs vary between nations but remain high in both developing and developed countries.
Introduction
Newborn babies in need of critical medical attention are normally admitted to the neonatal intensive care unit (NICU) (1). These infants tend to be preterm (i.e., born before 37 weeks of pregnancy) and have a low birth weight and/or serious medical conditions (1). The combination of advanced technology and a trained medical team (including neonatologists, nurses, respiratory therapists, occupational therapists, dieticians, and lactation consultants) in the NICU effectively provides specialized care for patients (1, 2). Health care professionals are often required to conduct complex assessments, execute highly intensive therapies, and make instant modifications based on the infant’s response in order to intervene before life-threatening conditions emerge (3).
Neonatal survival varies with the quality of medical care (4). Prematurity, congenital anomalies, and perinatal asphyxia are the main causes of death in babies (5). In developed countries, newborns typically die from unpreventable causes, such as congenital abnormalities, whereas the majority of infants in developing countries die from preventable conditions, including infections, birth asphyxia, and prematurity (6). In-hospital mortality rates of NICUs significantly impact infant mortality (7, 8). Infant mortality rates may be stratified into two cohorts by time: neonatal (normally defined as birth – 28 days) and postneonatal (29–364 days) (8). Due to complications from premature births, birth defects, maternal health conditions, difficult labor and delivery, and insufficient access to appropriate care during delivery, approximately two-thirds of all newborn deaths occur in the neonatal period (8). A fraction of NICU deaths in the postneonatal period are attributable to conditions originating from the neonatal period (7).
Progress in perinatal and neonatal care has notably diminished mortality and has improved the health of premature infants admitted to NICUs (9–13). Several publications have reported these findings (14–16), and others have noted the immense variations in mortality rates among NICUs (17, 18). However, no review to date has addressed the similarities and differences between various nations in NICU mortality rates and causes of death. If available, this information could help clinicians, researchers, and policymakers in identifying regions of high need for the provision of limited NICU resources. As such, the purpose of this selected review was to examine and compare the NICU mortality rates and etiologies of death across various countries.
Materials and Methods
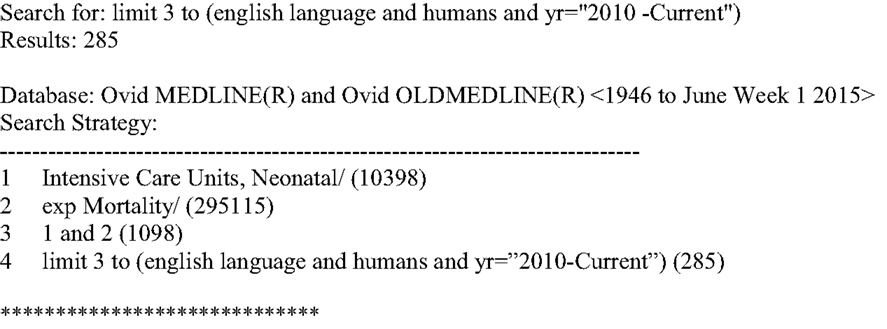
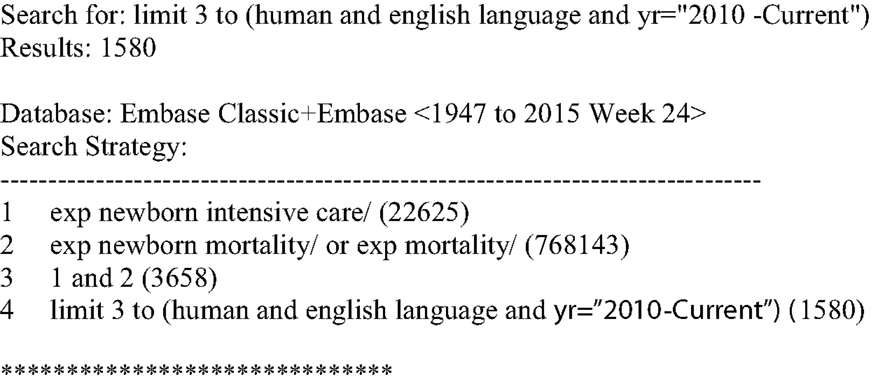
A literature search was conducted in Ovid MEDLINE and OLDMEDLINE (1946 to June Week 1, 2015) and EMBASE Classic and EMBASE (1947–2015 Week 24). The key search terms were “neonatal intensive care units” and “mortality” (see Figures 1 and 2). Titles and abstracts were screened to identify if studies were relevant for full-text screening, after which full-texts were included if they met the pre-specified inclusion criteria.
Selection Criteria
Articles were selected for full-text screening if the title or abstract mentioned mortality in addition to either “neonatal intensive care unit” and/or “NICU.” Another requirement was that there had to be a numerical mortality outcome following admittance to the NICU. Articles that did not have mortality rate statistics were excluded. Only English language studies were included. Duplicates of articles found in each database, as well as non-original research and small (i.e., <5 patients) studies, were excluded.
Data Extraction and Endpoints
The primary endpoint was the in-hospital mortality rate, which was defined as the number of deceased individuals divided by the sample size. Secondary endpoints included the reasons for death and the correlation between infant age and mortality outcome. For the main analysis, we examined all infants admitted to NICUs. Based on the authors’ own definition, the subgroup analyses were extremely low birth weight infants, very low birth weight infants, very preterm infants, preterm infants, and preterm infants with a birth weight of ≤1,500 g. We also grouped studies based on whether they came from developed or developing countries as classified by the United Nations (19).
Results
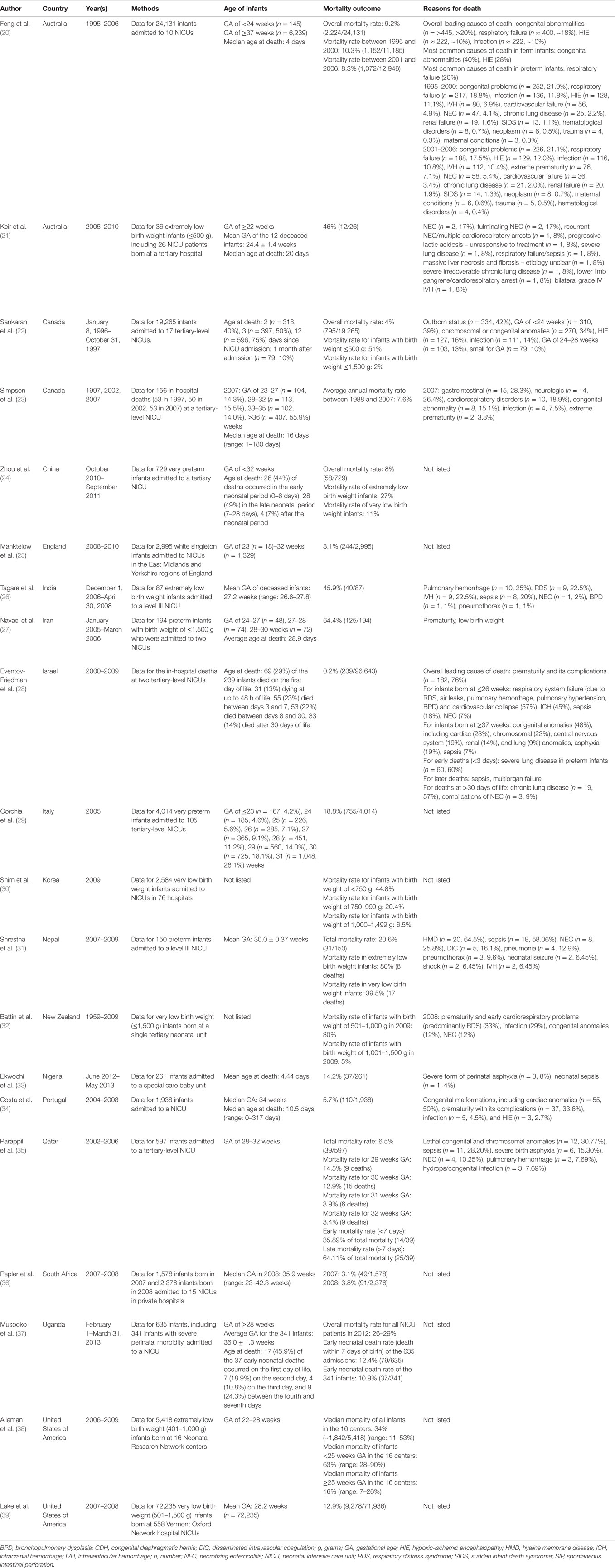
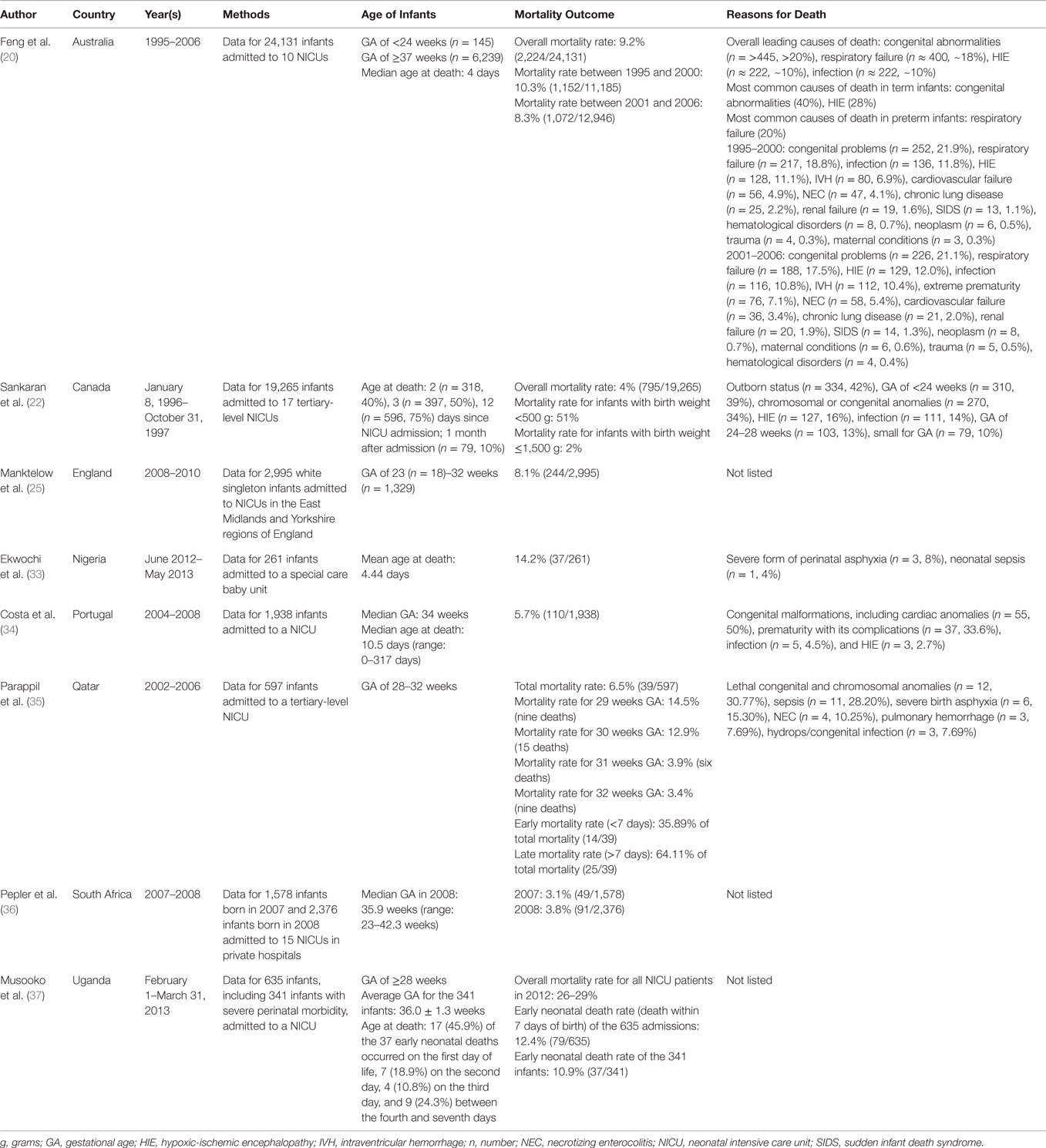
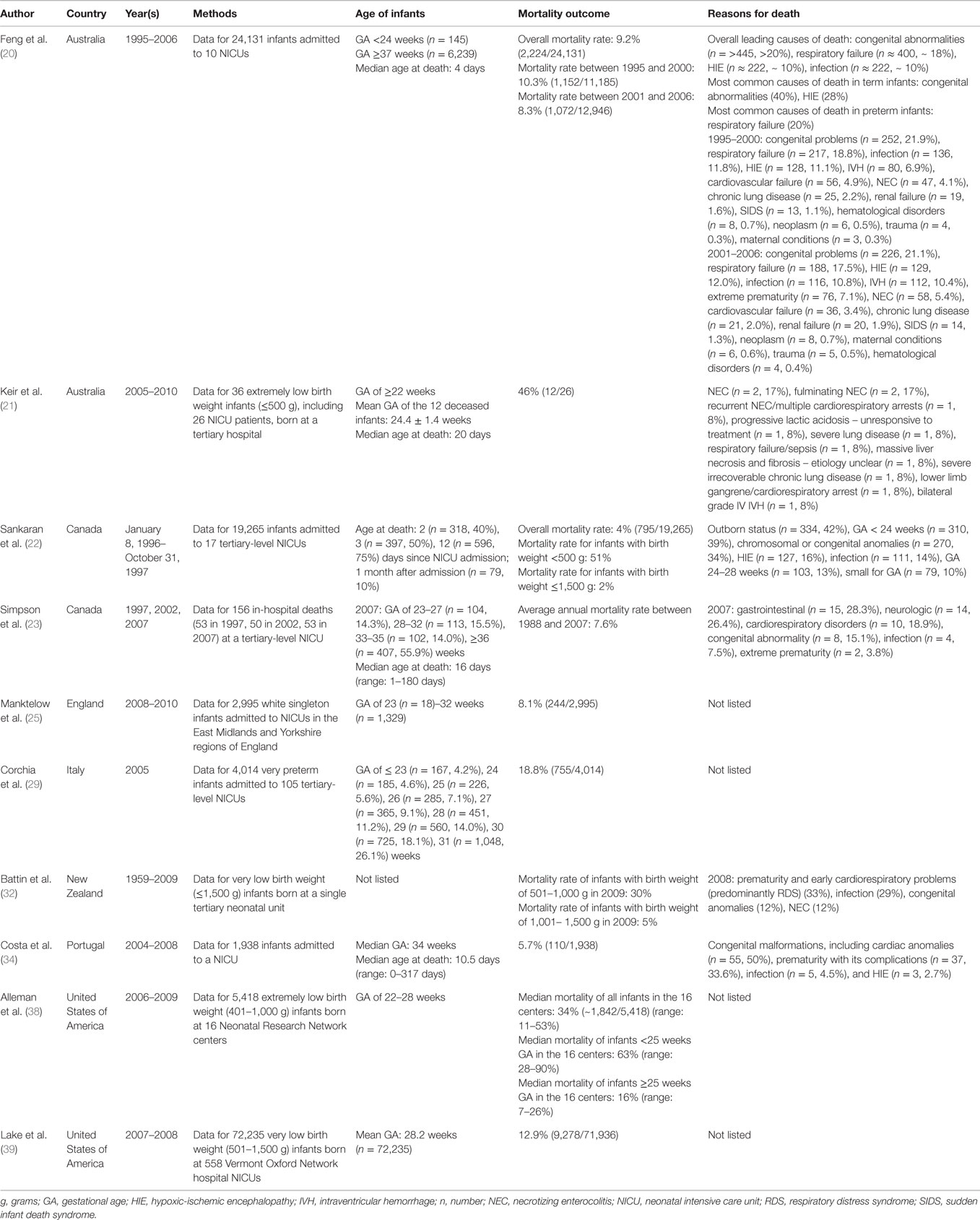
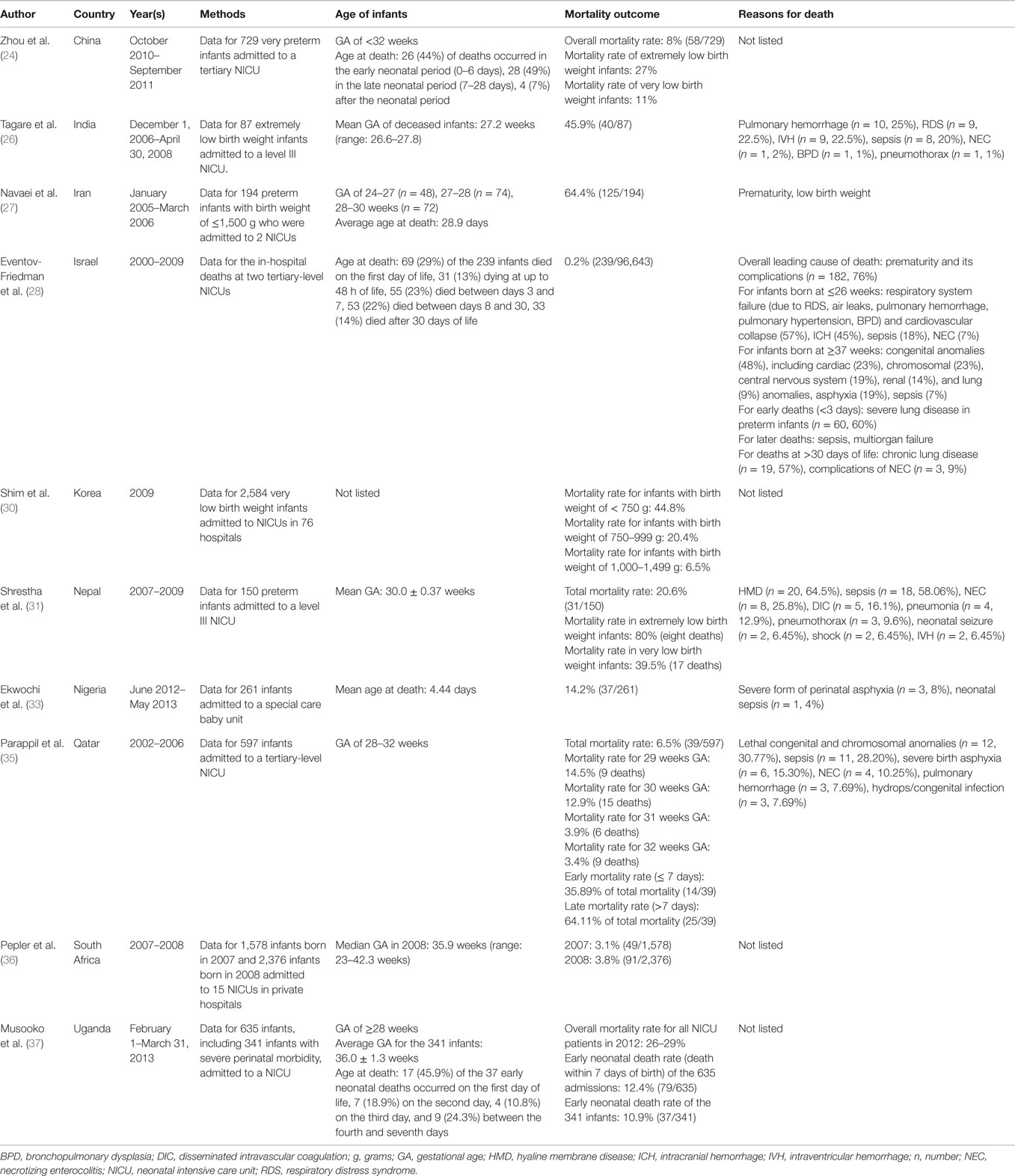
The literature search yielded 1,865 articles, with 285 from MEDLINE and 1,580 from EMBASE. Of those, 40 articles were identified for full-text review as specified by the inclusion criteria; 20 of the 40 articles were rejected after full-text review. Some of the reasons for exclusion were the absence of numerical mortality rates, lack/absence of relevant information regarding NICU mortality, and repeat data. Of the 20 remaining articles (20–39), eight reported on any infants admitted to NICUs (20, 22, 25, 33–37), three reported on the outcomes of extremely low birth weight infants (≤500 g, 401–1,000 g) (21, 26, 38), three others reported on the outcomes of very low birth weight infants (≤1,500 g) (30, 32, 39), two discussed all in-hospital deaths (23, 28), two focused on the outcomes of very preterm infants [<32 weeks gestational age (GA)] (24, 29), one involved the outcomes of preterm infants [<37 weeks GA] (31) and one reported on the outcomes of preterm infants with a birth weight of ≤1,500 g (27) (Table 1).
Mortality Rates in Overall Admissions to NICUs
Eight studies reported the mortality outcomes for all admissions to the NICU (20, 22, 25, 33–37), five of which examined the age of infants at death (20, 22, 33, 34, 37). Musooko et al. (37) noted that 45.9% (17/37) of infants with early neonatal deaths (death within 7 days of birth) and those with severe perinatal morbidity died on the first day of life in Uganda. The reported median age at death was 4 days in Australia (20), 4.4 days in Nigeria (33), and 10.5 days in Portugal (34). Sankaran et al. (22) found that 75% (596/795) of deceased infants passed away 12 days since NICU admission in Canada (Table 2).
The total mortality rates varied between countries. The overall in-hospital mortality rates were reported to be 3.1 and 3.8% in South Africa in 2007 and 2008, respectively (36), 4% in Canada from January 1996 to October 1997 (22), 5.7% in Portugal between 2004 and 2008 (34), 6.5% in Qatar from 2002 to 2006 (35), 8.1% in England between 2008 and 2010 (25), 9.2% in Australia across 1995–2006 (20), 14.2% in Nigeria between June 2012 and May 2013 (33), and 26–29% in Uganda in 2012 (37).
Five publications (20, 22, 33–35) investigated the etiologies of death in NICUs. Congenital and/or chromosomal abnormalities/malformations were common causes of death in Australia [greater than 20% (445/2,224)] (20), Canada [34% (270/795)] (22), Portugal [50% (55/110)] (34), and Qatar [30.77% (12/39)] (35). The common pathologies that led to death were hypoxic-ischemic encephalopathy (HIE) and infection. Though not as prevalent as congenital abnormalities, HIE and infection were still reported as common causes of death in Australia (10% (222/2,224) for both) (20), Canada [HIE = 16% (127/795); infection = 14% (111/795)] (22), Portugal [HIE = 2.7% (3/111); infection = 4.5% (5/110)] (34), and Qatar [hydrops/congenital infection = 7.69% (3/39)] (35).
Severe forms of perinatal asphyxia and neonatal sepsis were among the primary reasons for death in Nigeria [asphyxia = 8% (3/37); sepsis = 4% (1/37)] (33) and Qatar [asphyxia = 15.30% (6/39); sepsis = 28.20% (11/39)] (35). Other common causes of death in the NICU included respiratory failure in Australia [18% (400/2,224)] (20), outborn status in Canada [42% (334/795)] (22), GA less than 24 weeks in Canada [39% (310/795)] (22), GA between 24 and 28 weeks in Canada [13% (103/795)] (22), small size and/or weight for GA in Canada [10% (79/795)] (22), very low birth weight in Nigeria [0.8% (0.3/37)] (33), complications of prematurity in Portugal [33.6% (37/110)] (34), necrotizing enterocolitis (NEC) in Qatar [10.25% (4/39)] (35), and pulmonary hemorrhage in Qatar [7.69% (3/39)] (35).
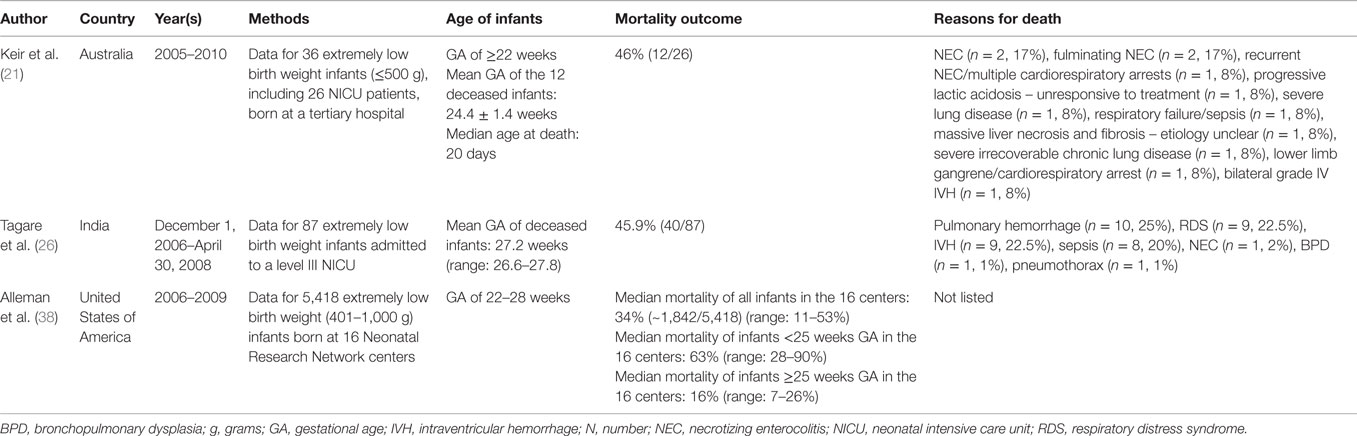
Mortality Rates in Extremely Low Birth Weight Infants (≤500 g, 401–1,000 g)
Three studies reported the mortality outcomes for extremely low birth weight infants (21, 26, 38). Each study had its own definition of extremely low birth weight infants. For instance, Keir et al. (21) defined extremely low birth weight as ≤500 g, while Alleman et al. (38) defined extremely low birth weight as 401–1,000 g.
Two articles (21, 26) studied the mean age of infants with extremely low birth weights. Keir et al. (21) found that the mean GA of the deceased infants was 24.4 ± 1.4 weeks in Australia, while Tagare et al. (26) noted that the mean GA of the late infants was 27.2 weeks in India (Table 3). Mortality rates were reported to be 34% in United States between 2006 and 2009 (38), 45.9% in India between December 2006 and April 2008 (26), and 46% in Australia between 2005 and 2010 (21).
Two publications (21, 26) investigated the etiologies of death of extremely low birth weight infants. In Australia, NEC [17% (2/12)] and fulminating NEC [17% (2/12)] were the two most common causes of death (21). In India, the leading reasons of death were pulmonary hemorrhage [25% (10/40)], respiratory distress syndrome [RDS, 22.5% (9/40)], intraventricular hemorrhage [IVH, 22.5% (9/40)], and sepsis [20% (8/40)] (26).
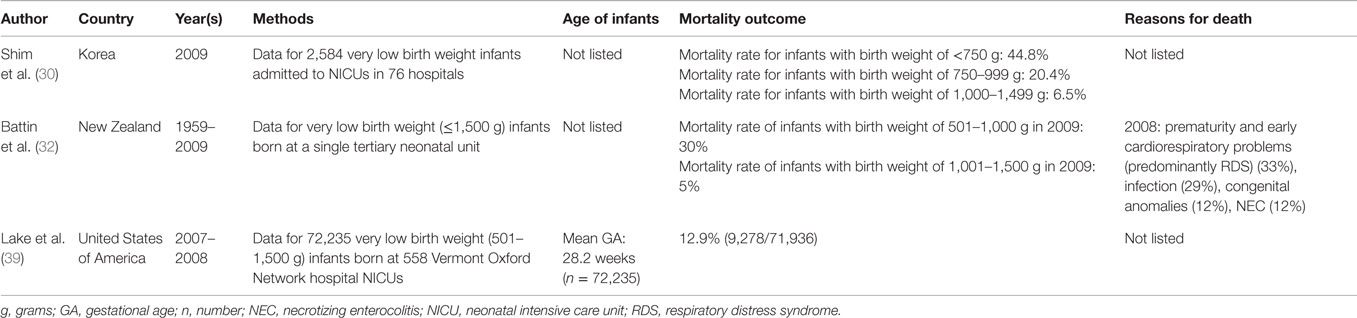
Mortality Rates in Very Low Birth Weight Infants (≤1,500 g)
Three studies reported the mortality outcomes for very low birth weight infants (30, 32, 39). The overall in-hospital mortality rates were reported to be 5% in New Zealand for infants with birth weight of 1,001–1,500 g in 2009 (32), 6.5% in Korea for infants with birth weight of 1,000–1,499 g in 2009 (30), 12.9% in United States of America between 2007 and 2008 (39), 20.4% in Korea for infants with birth weight of 750–999 g in 2009 (30), 30% in New Zealand for infants with birth weight of 501–1,000 g in 2009 (32), and 44.8% in Korea for infants with birth weight of <750 g in 2009 (30) (Table 4).
Battin et al. (32) investigated the etiologies of death in infants with very low birth weights. During 2008, in a NICU in New Zealand, prematurity and early cardiorespiratory problems (predominantly RDS) (33%), infection (29%), congenital anomalies (12%), and NEC (12%) were the leading causes of death (32).
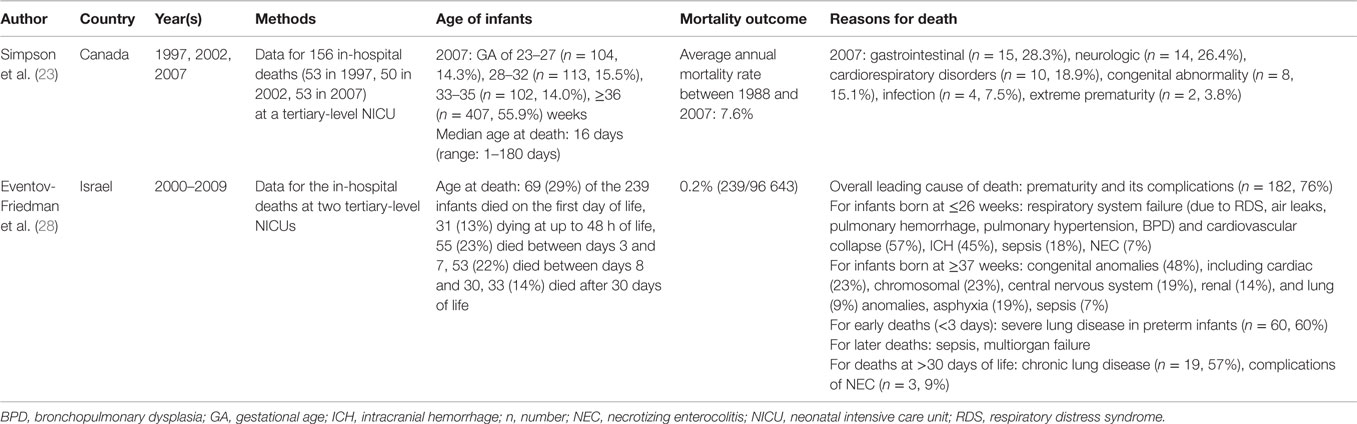
Mortality Rates in Overall In-Hospital Deaths
Two studies reported on all in-hospital deaths at a NICU, for which both trials defined the in-hospital mortality as all inpatient deaths during the study period (23, 28). However, each study calculated the in-hospital mortality rate differently; Simpson et al. (23) computed the figure per 100 admissions, while Eventov-Friedman et al. (28) did it per 1,000 live births. Simpson et al. (23) reported that the median age at death was 16 days in Canada (23), and Eventov-Friedman et al. (28) noted that 29% (69/239) of deceased infants died on the first day of life in Israel. The overall in-hospital mortality rates were reported as 0.2% in Israel between 2000 and 2009 (28), and 7.6% in Canada between 1988 and 2007 (23). Prematurity and its complications was a common cause of death; in Israel, 76% (182/239) of late infants died from these circumstances (28), but only 3.8% (2/53) of perished neonates died from extreme prematurity in Canada (23). The other leading reasons of death in Canada were gastrointestinal disorders [28.3% (15/53)], neurologic disorders [(26.4% (14/53)], cardiorespiratory disorders [18.9% (10/53)], congenital abnormalities [15.1% (8/53)], and infection [7.5% (4/53)] (23) (Table 5).
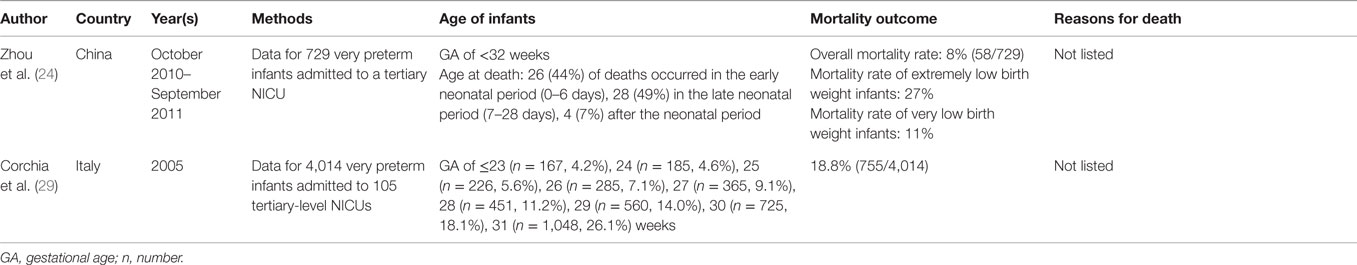
Mortality Rates in Very Preterm Infants (<32 Weeks GA)
Two studies reported the mortality outcomes for very preterm infants (24, 29). Zhou et al. (24) examined the age at death, noting that 49% (28/58) of deceased infants died in the late neonatal period (7–28 days). The overall in-hospital mortality rates were noted to be 8% in China between October 2010 and September 2011 (24), and 18.8% in Italy in 2005 (29) (Table 6).
Mortality Rates in Preterm Infants (<37 Weeks GA)
One study reported the mortality outcomes for preterm infants (31). The overall in-hospital mortality rate was 20.6% in Nepal between 2007 and 2009 (31) (Table 7). Additionally, the primary etiologies of death were hyaline membrane disease [HMD, 64.5% (20/31)], sepsis [58.06% (18/31)], and NEC [25.8% (8/31)] (31).
Age of Death and Mortality Rates of Developed and Developing Countries
Of the 20 articles included in this selected review (20–39), 10 reported on the NICU mortality outcomes in developed countries (20–23, 25, 29, 32, 34, 38, 39) and 10 reported on those of developing countries (24, 26–28, 30, 31, 33, 35–37).
Infants in developed and developing countries had similar ages at death, ranging from 4 to 20 days (20–23, 34) (Table 8) and 1 to 28.9 days (24, 27, 28, 33, 37) (Table 9), respectively. The mortality rates ranged from 4 to 46% in developed countries (20–23, 25, 29, 32, 34, 38, 39) and 0.2 to 64.4% in developing countries (24, 26–28, 30, 31, 33, 35–37).
Discussion
The age at death for all infants admitted to NICUs globally ranged from 1 to 12 days (20, 22, 25, 33–37). Similarly, deaths in the NICU tended to occur on the first and sixteenth days of life in Israel and Canada, respectively (23, 28). By contrast, very preterm (24) and preterm infants with birth weight of ≤1,500 g (27) were the infants with the oldest age at death. Zhou et al. (24) reported that approximately half [49% (28/58)] of late very preterm infants died in the late neonatal period (7–28 days). Navaei et al. (27) found that the average age at death for preterm infants with birth weight of ≤1,500 g was 28.9 days. It is surprising that very preterm infants had a longer life span than all NICU patients. The delayed mortality in premature infants suggests that a greater percentage of preterm neonates are surviving the immediate conditions of prematurity, only to contract lethal complications later (23). This may be due to the substantial improvements in supportive efforts for these high-risk patients in the first week(s) of life (23). However, it is unclear whether this increased survival for very preterm infants and preterm infants with birth weight of ≤1,500 g is attributable to improved medical care or lengthened suffering prior to death (23).
Consistent with the findings above, studies analyzing the outcomes of all infants admitted to NICUs (20, 22, 25, 33–37) and all in-hospital deaths (23, 28) reported the lowest mortality rates. The mortality rates were 0.2% in Israel (28) and 7.6% in Canada (23), while it ranged from 3.1 to 29% globally (20, 22, 25, 33–37). The mortality rates for the other articles, in ascending order, are as follows: very low birth weight infants [5–44.8%] (30, 32, 39), very preterm infants [8–18.8%] (24, 29), preterm infants (20.6%) (31), and extremely low birth weight infants [34–6%] (21, 26, 27, 38). Among all included analyses, the overall mortality rates for all infants admitted to NICUs and all in-hospital deaths are the lowest, as the study samples include both higher and lower-risk neonates. Conversely, infants who were born premature and with very low birth weight had more severe issues, putting them at a very high risk for death.
The mortality rate of NICUs varies but remains high in both developing and developed countries. Prematurity is a very common etiology of death, as very low birth weight infants (32), infants who died in hospital (23, 28), and preterm infants with very low birth weight (27) were all prematurely born. This could be attributable to the large number of preterm births; in fact, in 2005, the World Health Organization estimated that 12.9 million births of all births (9.6%) in the world were preterm (40).
The findings of this selected review are important for NICUs. Through examining the etiologies of death in different countries, further insight is provided, allowing care providers, policymakers, and researchers to address improvements on areas that will most benefit patients (23). Also, by comparing and contrasting various mortality rates and the age of infants at death, it provides NICUs with many different comparators.
The limitations of our study were that all information was taken from study cohorts. Another weakness was the heterogeneity in the definitions of medical terms (e.g., extremely low birth weight).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Stanford Children’s Health. California: Stanford Medicine 2015 (2015). Available from: http://www.stanfordchildrens.org/en/topic/default?id=the-neonatal-intensive-care-unit-nicu-90-P02389
2. Stanford Children’s Health. California: Stanford Medicine 2015 (2015). Available from: http://www.stanfordchildrens.org/en/topic/default?id=procedures-and-equipment-in-nicu-90-P02358
3. Boxwell G. Neonatal Intensive Care Nursing. New York, NY: Routledge (2010). Available from: http://samples.sainsburysebooks.co.uk/9781135154615_sample_843707.pdf
4. Yinger NV, Ransom EL. Why Invest in Newborn Health?. Washington, DC: Population Reference Bureau (2003). p. 1–5.
5. Mathews TJ, Miniño AM, Osterman MJ, Strobino DM, Guyer B. Annual summary of vital statistics: 2008. Pediatrics (2011) 127(1):146–57. doi:10.1542/peds.2010-3175
6. Jehan I, Harris H, Salat S, Zeb A, Moben N, Pasha O, et al. Neonatal mortality: risk factors and causes: a prospective population based cohort study in Pakistan. Bull World Health Organ (2009) 87:130–8. doi:10.2471/BLT.08.050963
7. Jacob J, Kamitsuka M, Clark RH, Kelleher AS, Spitzer AR. Etiologies of NICU deaths. Pediatrics (2015) 135(1):e59–65. doi:10.1542/peds.2014-2967
8. Grand Rounds CDC, Centers for Disease Control and Prevention (CDC). CDC grand rounds: public health approaches to reducing U.S. infant mortality. MMWR Morb Mortal Wkly Rep (2013) 62(31):625–8.
9. Stahlman MT. Newborn intensive care: success or failure? J Pediatr (1984) 105:162–7. doi:10.1016/S0022-3476(84)80386-8
10. Hack M, Wright LL, Shankaran S, Tyson JE, Horbar JD, Bauer CR, et al. Very low birth weight outcomes of the national institute of child health and human development neonatal network, November 1989 to October 1990. Am J Obstet Gynecol (1995) 172:457–64. doi:10.1016/0002-9378(95)90557-X
11. Horwood SP, Boyle MP, Torrance GW, Sinclair JC. Mortality and morbidity of 500 to 1,499 gram birth weight infants live-born to residents of a defined geographic region before and after neonatal intensive care. Pediatrics (1982) 69:613–20.
12. Lee KS, Paneth N, Gartner LM, Pearlman MA, Gruss L. Neonatal mortality: an analysis of the recent improvement in the United States. Am J Public Health (1980) 70:15–21. doi:10.2105/AJPH.70.1.15
13. Williams RL, Chen PM. Identifying the sources of the recent decline in perinatal mortality rates in California. N Engl J Med (1982) 306:207–14. doi:10.1056/NEJM198201283060404
14. Joseph KS, Kramer MS. Recent trends in Canadian infant mortality rates: effect of changes in registration of live newborns weighing less than 500 g. CMAJ (1996) 155:1047–52.
15. Health Statistics at a Glance [CD-ROM]. Ottawa, ON: Statistics Canada (1999). Cat no 82F0075XCB.
16. Lee SK, McMillan DD, Ohlsson A, Pendray M, Synnes A, Whyte R, et al. Variations in practice and outcomes in the Canadian NICU network: 1996-1997. Pediatrics (2000) 106(5):1070–9. doi:10.1542/peds.106.5.1070
17. Horbar JD, Badger J, Lewit EM, Rogowski J, Shiono PH. Hospital and patient characteristics associated with variation in 28-day mortality rates for very low birth weight infants. Pediatrics (1997) 99:149–56. doi:10.1542/peds.99.2.149
18. Stevenson DK, Wright LL, Lemons JA, Oh W, Korones SB, Papile LA, et al. Very low birth weight outcomes of the national institute of child health and human development neonatal research network, January 1993 through December 1994. Am J Obstet Gynecol (1998) 179:1632–9. doi:10.1016/S0002-9378(98)70037-7
19. United Nations (2015). Available from: http://www.un.org/en/development/desa/policy/wesp/wesp_current/2012country_class
20. Feng Y, Abdel-Latif ME, Bajuk B, Lui K, Oei JL. Causes of death in infants admitted to Australian neonatal intensive care units between 1995 and 2006. Acta Paediatr (2013) 102:e17–23. doi:10.1111/apa.12039
21. Keir A, McPhee A, Wilkinson D. Beyond the borderline: outcomes for inborn infants born at ≤500 grams. J Paediatr Child Health (2014) 50:146–52. doi:10.1111/jpc.12414
22. Sankaran K, Chien LY, Walker R, Seshia M, Ohlsson A, Lee SK, et al. Variations in mortality rates among Canadian neonatal intensive care units. CMAJ (2002) 166(2):173–8.
23. Simpson CDA, Ye XY, Hellmann J, Tomlinson C. Trends in cause-specific mortality at a Canadian outborn NICU. Pediatrics (2010) 126(6):e1538–44. doi:10.1542/peds.2010-1167
24. Zhou WQ, Mei YB, Zhang XY, Li QP, Kong XY, Feng ZC. Neonatal outcomes of very preterm infants from a neonatal intensive care center. World J Pediatr (2014) 10(1):53–8. doi:10.1007/s12519-013-0445-x
25. Manktelow BN, Seaton SE, Field DJ, Draper ES. Population-based estimates of in-unit survival for very preterm infants. Pediatrics (2013) 131(2):e425–32. doi:10.1542/peds.2012-2189
26. Tagare A, Chaudhari S, Kadam S, Vaidya U, Pandit A, Sayyad MG. Mortality and morbidity in extremely low birth weight (ELBW) infants in a neonatal intensive care unit. Indian J Pediatr (2013) 80(1):16–20. doi:10.1007/s12098-012-0818-5
27. Navaei F, Aliabady B, Moghtaderi J, Moghtaderi M, Kelishadi R. Early outcome of preterm infants with birth weight of 1500 g or less and gestational age of 30 weeks or less in Isfahan city, Iran. World J Pediatr (2010) 6(3):228–32. doi:10.1007/s12519-010-0204-1
28. Eventov-Friedman S, Kanevsky H, Bar-Oz B. Neonatal end-of-life care: a single-center NICU experience in israel over a decade. Pediatrics (2013) 131(6):e1889–96. doi:10.1542/peds.2012-0981
29. Corchia C, Orlando SM. Level of activity of neonatal intensive care units and mortality among very preterm infants: a nationwide study in Italy. J Matern Fetal Neonatal Med (2012) 25(12):2739–45. doi:10.3109/14767058.2012.703721
30. Shim JW, Kim MJ, Kim EK, Park HK, Song ES, Lee SM, et al. The impact of neonatal care resources on regional variation in neonatal mortality among very low birth weight infants in Korea. Paediatr Perinat Epidemiol (2013) 27:216–25. doi:10.1111/ppe.12033
31. Shrestha S, Dangol Singh S, Shrestha M, Shrestha RPB. Outcome of preterm babies and associated risk factors in a Hospital. JNMA J Nepal Med Assoc (2010) 49(180):286–90.
32. Battin MR, Knight DB, Kuschel CA, Howie RN. Improvement in mortality of very low birthweight infants and the changing pattern of neonatal mortality: The 50-year experience of one perinatal centre. J Paediatr Child Health (2012) 48:596–9. doi:10.1111/j.1440-1754.2012.02425.x
33. Ekwochi U, Ndu IK, Nwokoye IC, Ezenwosu OU, Amadi OF, Osuorah DIC. Pattern of morbidity and mortality of newborns admitted into the sick and special care baby unit of Enugu state University Teaching Hospital, Enugu state. Niger J Clin Pract (2014) 17(3):346–51. doi:10.4103/1119-3077.130238
34. Costa S, Rodrigues M, Centeno MJ, Martins A, Vilan A, Brandão O, et al. Diagnosis and cause of death in a neonatal intensive care unit – How important is autopsy? J Matern Fetal Neonatal Med (2011) 24(5):760–3. doi:10.3109/14767058.2010.520047
35. Parappil H, Rahman S, Salama H, Rifai HA, Parambil NK, Ansari WE. Outcomes of 28+1 to 32+0 weeks gestation babies in the state of Qatar: finding facility-based cost effective options for improving the survival of preterm neonates in low income countries. Int J Environ Res Public Health (2010) 7:2526–42. doi:10.3390/ijerph7062526
36. Pepler PT, Uys DW, Nel DG. Predicting mortality and length-of-stay for neonatal admissions to private hospital neonatal intensive care units: a South African retrospective study. Afr Health Sci (2012) 12(2):166–73. doi:10.4314/ahs.v12i2.14
37. Musooko M, Kakaire O, Nakimuli A, Nakubulwa S, Nankunda J, Osinde MO, et al. Incidence and risk factors for early neonatal mortality in newborns with severe perinatal morbidity in Uganda. Int J Gynaecol Obstet (2014) 127:201–5. doi:10.1016/j.ijgo.2014.05.017
38. Alleman BW, Bell EF, Li L, Dagle JM, Smith PB, Ambalavanan N, et al. Individual and center-level factors affecting mortality among extremely low birth weight infants. Pediatrics (2013) 132(1):e175–84. doi:10.1542/peds.2012-3707
39. Lake ET, Staiger D, Horbar J, Cheung R, Kenny MJ, Patrick T, et al. Association between hospital recognition for nursing excellence and outcomes of very low-birth-weight infants. JAMA (2012) 307(16):1709–16. doi:10.1001/jama.2012.504
Keywords: neonatal intensive care unit, mortality rate, prematurity
Citation: Chow S, Chow R, Popovic M, Lam M, Popovic M, Merrick J, Stashefsky Margalit RN, Lam H, Milakovic M, Chow E and Popovic J (2015) A selected review of the mortality rates of neonatal intensive care units. Front. Public Health 3:225. doi: 10.3389/fpubh.2015.00225
Received: 17 August 2015; Accepted: 22 September 2015;
Published: 07 October 2015
Edited by:
Frederick Robert Carrick, Carrick Institute, USAReviewed by:
Jugesh Chhatwal, Christian Medical College & Hospital, IndiaSusan Elizabeth Esposito, Life University, USA
Linda Mullin Elkins, Life University, USA
Copyright: © 2015 Chow, Chow, Popovic, Lam, Popovic, Merrick, Stashefsky Margalit, Lam, Milakovic, Chow and Popovic. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ruth Naomi Stashefsky Margalit, MSR Israel Center for Medical Simulation, Chaim Sheba Medical Center, Tel Hashomer National Education Center, 203 Haefroni Road, Atzmon-Segev 20170, Israel,cnV0aC5tYXJnYWxpdEBzaGViYS5oZWFsdGguZ292Lmls
 Selina Chow
Selina Chow Ronald Chow
Ronald Chow Mila Popovic1
Mila Popovic1 Michael Lam
Michael Lam Marko Popovic
Marko Popovic Joav Merrick
Joav Merrick Ruth Naomi Stashefsky Margalit
Ruth Naomi Stashefsky Margalit Henry Lam
Henry Lam Milica Milakovic
Milica Milakovic