- 1Physical Activity Research and Community Implementation, Human Nutrition, Foods, and Exercise, Virginia Tech, Blacksburg, VA, United States
- 2Center for Population Health and Management, Texas A&M University, College Station, TX, United States
- 3Department of Environmental and Occupational Health, School of Public Health, Texas A&M University, College Station, TX, United States
- 4Department of Health Promotion and Behavior, College of Public Health, The University of Georgia, Athens, GA, United States
- 5Walgreens Center for Health and Wellbeing Research, Deerfield, IL, United States
- 6Department of Health Promotion, College of Public Health, University of Nebraska Medical Center, Omaha, NE, United States
- 7Department of Family Medicine, School of Medicine, University of Colorado, Aurora, IL, United States
The RE-AIM Framework is a planning and evaluation model that has been used in a variety of settings to address various programmatic, environmental, and policy innovations for improving population health. In addition to the broad application and diverse use of the framework, there are lessons learned and recommendations for the future use of the framework across clinical, community, and corporate settings. The purposes of this article are to: (A) provide a brief overview of the RE-AIM Framework and its pragmatic use for planning and evaluation; (B) offer recommendations to facilitate the application of RE-AIM in clinical, community, and corporate settings; and (C) share perspectives and lessons learned about employing RE-AIM dimensions in the planning, implementation, and evaluation phases within these different settings. In this article, we demonstrate how the RE-AIM concepts and elements within each dimension can be applied by researchers and practitioners in diverse settings, among diverse populations and for diverse health topics.
Introduction
Dissemination and implementation (D&I) research addresses the “how and why” related to strategies for information sharing (dissemination) and intervention integration (implementation) for the purposes of enhancing evidence-based program delivery and population health (1–5). The advancement of D&I science requires a focus on the wide-scale adoption, implementation, and generalizability of program and policy impacts. With well over 100 different models and frameworks utilized in the field (6), researchers and practitioners can become overwhelmed when selecting (and attempting to apply) the most appropriate model/framework for their scientific inquiry or initiative.1
The purposes of this article are to: (A) provide a brief overview of the RE-AIM Framework and its pragmatic use for planning and evaluation; (B) offer recommendations to facilitate the application of RE-AIM in clinical, community, and corporate settings; and (C) share perspectives and lessons learned about employing RE-AIM elements in the planning, implementation, and evaluation phases within these different settings. In this article, we demonstrate how RE-AIM concepts and elements can be applied by researchers and practitioners in diverse settings, among diverse populations, and for diverse health topics.
The RE-AIM Framework
The RE-AIM Framework (7, 8) is often used in D&I research (9, 10), which encompasses essential translational research elements. RE-AIM was identified as the most frequently used model or framework between 2000 and 2016 for D&I grant applications submitted to the National Institutes of Health and Centers for Disease Control and Prevention (CDC) (11). This widespread use is, in part, due to the flexibility to address different public health concerns in a practical manner understandable by practitioners and policy makers. The acronym RE-AIM stands for reach (How do I reach those who need a specific intervention?), efficacy/effectiveness (How do I know my intervention is working?), adoption (How do I design for dissemination and develop organizational support to deliver my intervention?), implementation (How do I ensure the intervention is feasible and delivered properly?), and maintenance (How do I ensure long-term benefits and institutionalization of the intervention and continued community capacity for D&I?).
Applying RE-AIM challenges researchers and practitioners to ask fundamental questions about complex issues before, during, and after the implementation of a putative program in “real world” settings. Among the many strengths of RE-AIM is its robust structure that facilitates broad use across settings (e.g., organization, regional, rural), populations (e.g., age, race/ethnicity, occupation/role), topics (e.g., disease, behavior), and interventions (e.g., demonstration, experimental, translational, longitudinal, multi-level). While the basic RE-AIM dimensions have remained constant since its development in the 1990s (7), its use has evolved over time with new applications in clinical (12), community (13), and corporate (14) settings. A recent systematic review (15) reported health-care (49%) and community (46%) settings applied RE-AIM in empirical or evaluative interventions most frequently; however, no such interventions were reported in corporate settings. As such, efforts are needed to understand the use of RE-AIM in multiple settings. Researchers and practitioners are encouraged to use the RE-AIM framework for beginning with the end in mind, designing for dissemination, and evaluating relevant dimensions across intervention and setting factors. Such deliberate RE-AIM application will contribute to the replicability and generalizability of planned interventions and thus yield optimal public health impact.
Pragmatic Use of RE-AIM for Planning and Evaluation
The RE-AIM Framework can be used to direct the planning of new or ongoing interventions and systematic evaluations that include a complex interplay of individual and organizational outcomes (10). Fully employing RE-AIM can speed the translation of effective interventions in practice settings, while demonstrating impact and representativeness (9, 10). Yet, utilizing the full framework may require substantial human, data, and analytic resources that may not be available or feasibly acquired across typical clinical, community, or corporate settings (16). This is especially true in settings where decision-making may be based on a small subset of RE-AIM dimensions coupled with organizational priorities and resources.
Settings must consider the temporality of assessment for each RE-AIM dimension, which may need to occur prospectively, concurrently, and/or retrospectively to determine the impact of an initiative. While employing RE-AIM before an intervention begins is ideal to ensure careful and strategic local planning, in some cases this is not possible. Some organizational practices may be the result of opportunistic intervention, rollout from a central administrative site, innovation testing; corporate, policy, or organizational directive; or quality control and enhancement—each of which has distinct challenges in aligning the evaluation with initiative strategies.
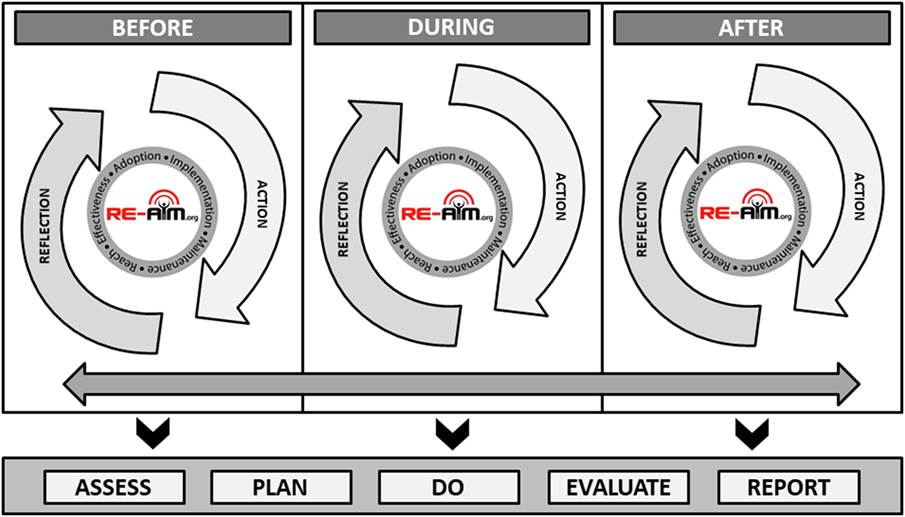
Figure 1 illustrates the application of RE-AIM based on the starting temporal stage of an intervention or initiative, that is if the RE-AIM planning and evaluation is initiated before, during, or after an initiative has been completed. Each temporal starting point includes reflective processes in which researchers or practitioners can gather information (assess) and think critically about the relevance of each RE-AIM dimension (plan). Each stage also includes active processes where those applying RE-AIM can initiate and implement plans for interventions or initiatives (do), process gathered information based on predetermined criteria (evaluate), and engage partners and stakeholders in interpretation to support decision-making (report). The bidirectional arrow along the temporal stages indicate the iterative nature of these processes, each building upon one another to provide cumulative input for advancement and refinement based evolving priorities, challenges, and observed impacts (2, 17). The importance of Figure 1 is to address the iterative nature of applying RE-AIM in planning and evaluation and how new data are taken into consideration and used to engage in a planning and action process.
As the bidirectional arrow suggests, the end of an initiative is the beginning of another (i.e., sustained implementation, adapted implementation, or implementation of an alternative solution), thus the process is cyclical and ongoing. While it is not feasible to always employ RE-AIM before an intervention or initiative begins, this figure indicates that the process can begin at any temporal stage. At all stages, researchers and practitioners are encouraged to APDER: Assess (using relevant RE-AIM dimensions and available data); Plan (based on best science, program priorities, stakeholder and organizational values, and available resources); Do (based on predetermined plans using defined procedures/protocols and supporting appropriate adaptations as needed during implementation); Evaluate (based on criteria necessary for decision-making and iterative adjustment); and Report (to, and plan for follow-up with, key stakeholders).
The RE-AIM website2 hosts a planning and evaluation document, which includes prompts and considerations across all five RE-AIM dimensions by temporal stage within a project,3 which is also available as a supplemental table to this manuscript (see Appendix A in Supplementary Material). Selected examples of common pragmatic considerations are described below.
Engaging key stakeholders (e.g., policy makers, service delivery personnel, members from the population intended to benefit from the work) is important for guiding pragmatic evaluations using RE-AIM. Researchers and practitioners should partner with organizational decision-makers to identify the necessary information required to determine priorities, justify the need for intervention, sustain implementation, and/or broaden adoption. For example, if a strategy is delivered by a single organization with a centralized delivery infrastructure, issues related to reach and effectiveness (as well as implementation costs and sustainability) may be more relevant than adoption (18). Conversely, when attempting to scale-up or scale-out an effective intervention across a number of sites (within or across organizations), issues related to implementation quality/fidelity and adoption may be considered more important than documenting the intervention’s effectiveness in new and diverse settings (19, 20).
Pragmatically measuring RE-AIM outcomes (21) includes leveraging data already collected within the organizational setting to reduce evaluation costs and enhance local relevance. For example, imagine a health-care system will employ a multi-leveled intervention to enhance diabetes control by promoting physical activity. The intervention includes screening, brief counseling, referral to internal or external resources for physical activity. A pragmatic evaluation of this approach may include using electronic health records to assess the reach and representativeness of participants, changes in physical activity based on clinical screenings over time, and the number of referrals made (22). Based on priorities and available resources, it may be less pragmatic for the health-care system to assess patients’ use of external resources for physical activity or their actual physical activity levels. However, if a similar multi-level intervention were implemented in a community setting, accessing electronic health records may be politically, legally or cost-prohibitive, or less relevant; rather, documenting participants’ physical activity with pedometers/accelerometers and tracking facility utilization are prioritized.
Available resources for evaluation are often limited in “real world” non-academic community and clinical settings. In most settings, resources are allocated to the intervention’s delivery and management to maximize enrollment/engagement. Therefore, the pragmatic selection and use of existing measures is helpful to reduce data collection burden. However, the use of existing measures can also introduce resource needs associated with data extraction, case de-identification, and statistical analyses and data management that may exceed organizational skillsets and typical reporting procedures.
Examples of RE-AIM in Different Settings
In this section, we provide examples of RE-AIM application in three major types of settings. In addition to these examples, Table 1 contains additional recommendations for using RE-AIM by temporal stages of an intervention (i.e., before, during, after) across clinical, community, and corporate settings. The purpose of this table is to document the consistency of topics to be considered when applying RE-AIM across settings, while highlighting the unique factors framing the contextualization of RE-AIM within settings.
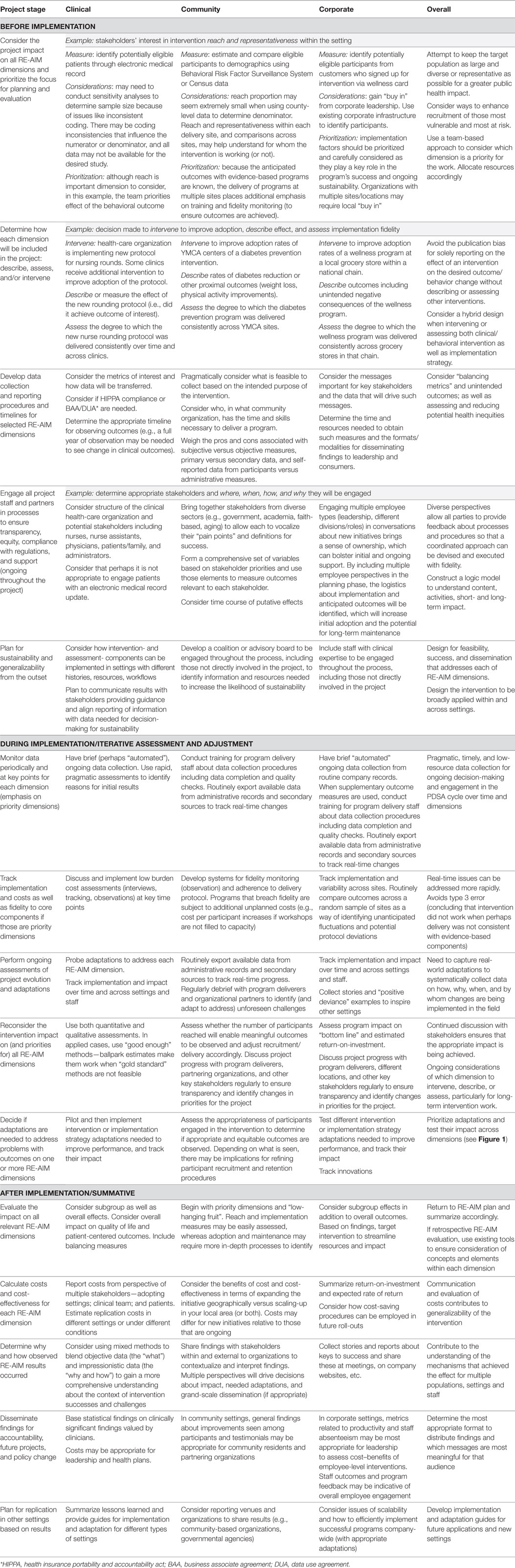
Table 1. Examples of applying RE-AIM dimension(s) in different settings across different phases of projects.
Clinical Health-care Setting
Esteemed professional organizations and societies (e.g., The Institute of Medicine, National Academies of Medicine, and Society of Behavioral Medicine) have called for health systems to assess key health behaviors, mental health, and social measures, and address an actionable set of social determinants of health. Leveraging these opportunities, the My Own Health Report (MOHR) consortium tested a brief, evidence-based online and interactive health risk assessment and feedback tool (MyOwnHealthReport.org). The online aid included patient-reported items on health risk behaviors, mental health, substance use, demographics, and patient preferences (23).
The MOHR project tested the interactive patient-report and feedback system in a cluster randomized trial of 18 primary care clinics across five states. RE-AIM was used to plan, adapt, and evaluate the system using a low-cost pragmatic implementation strategy. RE-AIM was used in the planning stages to develop strategies feasible for low-resource settings with patients most in need (e.g., federally qualified health centers and other diverse clinics including rural, suburban, and urban clinics). Inclusion criteria were purposively broad for clinics and patients, and time demands on patients and staff were kept to a minimum. The implementation plan involved a high degree of flexibility and allowed each clinic to recruit patients, administer the MOHR, simultaneously provide feedback, use assessment/feedback modalities, select languages (English or Spanish), and place in their clinic workflow. In terms of RE-AIM, this plan addressed reach, adoption, and implementation issues.
RE-AIM was used iteratively to monitor and adjust recruitment strategies (reach) and feedback and goal setting print-out delivery to patients and health-care team members (implementation). Content on print-outs were reinforced by practical webinars providing training about motivational interviewing and collaborative goal setting. The intervention was purposefully brief, low-cost (publicly available), and addressed impact (effectiveness) through standardized assessment and feedback content (23).
Results are summarized elsewhere (24), but in brief, the intervention produced high levels of reach (49% of all eligible patients, including those not contacted), adoption (18 of 30 diverse, low-income clinics approached participated), implementation (all eight risk factors assessed significantly more often in intervention patients; assessment, and print-outs delivered consistently), and effectiveness (intervention superior to randomized paired control clinics on goal setting for 6 of 8 behaviors and changes on 5 of the 8 health behavior and mental health issues). The program was not, however, maintained in any of the settings following conclusion of the study.
To achieve high levels of reach, adoption, and implementation, it was necessary to allow considerable flexibility and customization about how the MOHR was delivered while keeping the content of the intervention standard (23–25). The study was conducted inexpensively and rapidly by the standards of controlled trials (25) and demonstrated use of RE-AIM for planning, adaptation, and evaluation. The lack of setting maintenance was due to the inability to integrate the intervention into the existing health records (several different EHR systems were used) and intervention costs while modest (primarily staff time) that exceeded reimbursement provided by Medicare for annual wellness exams.
Community Setting
The RE-AIM framework was adopted in the mid-2000s for use by community-based grantees in the aging services and public health networks funded through the Administration for Community Living (26). Use of RE-AIM was part of the grant solicitation, and state grantees were expected to employ RE-AIM in their planning and evaluation of selected evidence-based interventions for managing chronic conditions. RE-AIM was chosen because of its alignment with funder goals to: “(1) develop the systems necessary to support the ongoing implementation and sustainability of evidence-based programs for older adults; (2) develop multi-sector community partnerships to enhance program accessibility and extend program capacity; (3) reach the maximum number of at-risk older adults who could benefit from the programs; and (4) deliver evidence-based programs with fidelity” (27). Consultants from the CDC Healthy Aging Research Network (28) provided technical assistance to the grantees (spanning 27 states), who were primarily aging services or public health practitioners, about how RE-AIM elements could be incorporated into their grant processes.
A questionnaire was administered to state grantees to assess the utility of the RE-AIM framework and the integration of RE-AIM elements into different planning, implementation, evaluation, and monitoring processes. Grantees reported RE-AIM was useful for planning, implementation, and evaluation and relevant for various stakeholders (e.g., evaluators, providers, community leaders, and policy makers) (26). For example, RE-AIM influenced grantee decisions about program selection, target populations, and assessment/evaluation tools. Despite the availability of technical assistance, some respondents reported difficulties in use of RE-AIM, especially adopting the framework as a whole. It was not clear if findings reflected grantees’ preferences for adopting single RE-AIM elements over the framework as a whole or if they lacked resources needed to fully assess and track all RE-AIM dimensions.
Over the past decade, RE-AIM utilization has been encouraged in other national-, state-, and local-level community-based initiatives designed to improve the healthy aging. Examples include the CDC’s Initiatives on Assuring Healthy Caregivers (29), Health Foundation of South Florida Healthy Aging Regional Collaborative (30), and the United Way Healthy Aging and Independent Living Initiative (31).
The RE-AIM framework has been valuable for helping community practitioners ask important questions during program planning, implementation, dissemination, and evaluation. However, there is often more use of and adherence to the individual RE-AIM concepts than the model as a whole, which is complicated by the changing lexicon in the field. For example, although the concepts remain consistent, recent federal aging initiatives use terms such as “scalability” and “sustainability” instead of “reach” and “maintenance.” Involvement in these aging initiatives reinforces the strong commonality between the study of aging and the RE-AIM framework: both are dynamic processes, evolving over time, and changing with the social context. For continued relevance, frameworks need to be pragmatic, fluid, and adaptable. It is a testimony to RE-AIM that its basic concepts are now mainstreamed and widely integrated into community practice.
Corporate Setting
While theoretically as relevant and useful to corporations, the uptake of RE-AIM in corporate settings has been less frequent relative to application in clinical and community settings. Similar to other settings, corporate settings are interested in offering evidence-based programs to their consumers because programs with demonstrated efficacy/effectiveness are most likely to result in positive outcomes, which ultimately satisfies key consumers and stakeholders, and sustains programs (maintenance). Large corporations can have substantial reach because of their infrastructure and support resources (implementation) that enable rapid employment and embedding of the RE-AIM dimensions. This infrastructure allows for systematic program adoption, dissemination, and implementation supported by centralized communication channels and support staff.
The relevance and usefulness of RE-AIM in corporate settings can be demonstrated by closely examining one large US-based corporation, Walgreens. With its 8,175 locations across the US and 87 million rewards account holders, Walgreens has tremendous potential to reach consumers and impact public health. Even a program offered only to Walgreens’ 250,000 employees can have an impact similar to implementing a program to every resident of a moderate-size city.
With an emphasis on trust, care, and accessibility, Walgreens aims to deliver programs that improve its participants’ health and well-being. This is really no different than the goals of many non-profit, community-based organizations. What is different, however, is that Walgreens’ size and geographic dispersion makes the task of D&I somewhat daunting in terms of logistics and capital needed to initiate a system-wide intervention. Cost and perceived value are the primary reasons that health promotion programs are sustained or discontinued at the community- and corporate-level (Rhodes and Glasgow, unpublished).4 For example, the incentivized digital health program—Balance Rewards for healthy choices (BRhc)—was implemented in 2014 as a resource-efficient solution to assist Walgreens patients track health behaviors. The value of BRhc has been demonstrated by higher adherence to hypertension and diabetes medications among its users and has shown to promote physical activity among younger adults with chronic conditions (32–34). This program has a vast reach with over one million users, and the digital format of the program moderates the ongoing costs of implementation.
Based on its unique position and infrastructure (like many large corporations), Walgreens has exceeded the capability of many health care and community organizations to deliver an intervention with grand-scale reach, adoption, impact, and a maintained presence. However, substantial challenges still exist. Corporations need to value the initial investments and be convinced of adequate return-on-investment for thorough, consistent education and training of delivery staff to achieve reliable results over time (both clinical and financial). If programs are not selected, implemented, and evaluated with the utmost care, the potential patient- and organizational-level loss can be quite damaging. This is a powerful reason to advocate for expanding the application of RE-AIM within corporate settings. Utilizing RE-AIM in corporate settings can produce returns on financial investments while providing benefits to intended populations that are sustained over time.
Discussion
This article provided a brief overview of the RE-AIM Framework and its pragmatic use for planning and evaluation while also offering recommendations to facilitate the application of RE-AIM in clinical, community, and corporate settings. Further, this article shared perspectives and lessons learned about employing RE-AIM dimensions in the planning, implementation, and evaluation phases within different settings. Due to nature and restrictions of perspective articles, we focused on limited examples of clinical, community, and corporate work. However, these detailed examples describe initial decision-making, iterative application of RE-AIM processes, and impact on public health outcomes. Similar processes can be applied in other settings for health-related outcomes. Notably, not all evaluations include all RE-AIM dimensions, and there is no right or wrong answer related to which dimensions on which to focus an evaluation. The primary dimensions deserving attention will vary by community, stakeholder and organizational priories and resources as well as the intervention settings, populations, desired outcomes, and topics. While the processes for reflection and action may differ between clinical, community, and clinical settings based on a unique set of priorities and logistics, the general considerations for applying RE-AIM remain common. To conclude, we discuss lessons learned and recommendations for how RE-AIM can be employed across settings to enhance population health in the future.
A fundamental issue across settings is whether to comprehensively apply the full RE-AIM framework or use a more limited and “strategic” approach to include only certain RE-AIM dimensions. This issue of a full versus pragmatic use of RE-AIM has recently been discussed in detail elsewhere (9, 10, 16, 22, 35), but this topic is especially relevant for applied and unfunded (or underfunded) clinical, community, and corporate non-research settings. For applied settings, the full RE-AIM Framework is best used initially at the outset and planning of a project, and then, select dimensions can be used during and after the program to guide implementation, evaluation, and/or reporting. Initial focus should focus on rough estimates of desired impact for each RE-AIM dimension, followed by decisions about: (A) which dimensions are most important for this project; (B) which dimensions should be measured given limited resources; and (C) which dimensions will be targeted for improvement. This type of pragmatic approach can engage key stakeholders through the use of existing data to determine intervention success (36). A pragmatic approach is intended to allow clinical, community, and corporate settings consider the entirety of the framework during planning, but then identify actionable RE-AIM information about the most relevant dimensions to determine if a given initiative should be abandoned, refined, sustained, scaled-up, or scaled-out (16).
Given challenges with funding (e.g., more competition to obtain limited resources) in clinical, community, and corporate settings, it is essential to consider strategies to reduce costs and leverage available resources. An interesting concept, frequent need, and important area of study is the “de-implementation” of programs and program elements that appear ineffective, too expensive, or produce unanticipated negative outcomes. Such issues need to be identified in “real time” so an intervention can be quickly modified or discontinued. The urgency of conserving costs and alleviating unnecessary spending (especially at the detriment of community well-being and health equity) highlights the need for ongoing reflection about the RE-AIM dimensions throughout the temporal stages of the intervention. As the RE-AIM framework is used to drive implementation efforts, the same framework can (and should) be used to guide and evaluate de-implementation efforts (37).
A new area of RE-AIM application involves its iterative use to provide ongoing, rapid assessments of progress, then using these results to guide program adaptations (38, 39). For example, early tracking of enrollment (reach) may reveal that key segments of the target population (e.g., low-income patients, those most at risk) are not participating in the intervention. Efforts can then be redirected (and tested) to improve subsequent participation rates. Although RE-AIM was initially used primarily for post hoc program evaluation, it was deemed useful for program planning starting in 2005 (40). Iterative uses of brief, practical measures of targeted RE-AIM dimensions are new and anticipated to grow, which warrants additional research in this area (2).
Our collective experience across clinical, community, and corporate settings indicates the need for greater attention to contextual factors. Often, the most efficient ways to assess contextual factors (the “how and why”) are qualitative or mixed-method approaches (41, 42). Such impressionistic approaches can be helpful to identify conditions under which a program is successful and reasons for such results. The Practical, Robust Implementation, and Sustainability Framework (PRISM) (43) extension of the RE-AIM model may be particularly useful for this purpose because it specifies contextual factor types that may be related to results about different RE-AIM dimensions.
The field of public health has evolved to accommodate changes in societal demographics, the environment, and impacts on the social determinants of health. In fact, such changes have caused new health-related issues and complications that spurned the creation of new fields (e.g., nutrigenomics, computational social science, behavioral economics). As fields advance, so do their need for sophisticated implementation and evaluation efforts to account for increasing complexity (e.g., big data from multiple sources/levels, nested influence and integrated variables, innovative intervention designs and statistical methodologies, systems issue and unanticipated consequences). We anticipate that the application of RE-AIM will expand to these new fields and offer a robust framework for advancing research, practice, and policy. For example, as new fields emerge and existing fields advance, the demand for multi-disciplinary collaboration grows. The RE-AIM Framework is recommended for use as a model to promote inter-professional education (using the community as the classroom) to train the next generation of scholars.
Finally, whereas much of the health promotion literature shows a publication bias toward initial effectiveness data only, using the RE-AIM framework increases the likelihood that that population-level public health impact is captured. Specifically, RE-AIM dimensions allow for the investigation of the degree to which an initiative can be adopted and delivered broadly, have the ability for sustained and consistent implementation at a reasonable cost reach large numbers of people especially those who can most benefit, produce replicable and long-lasting behavior changes. To assist with these challenges, there are RE-AIM planning and evaluation guides on the www.re-aim.org website (44).
Conclusion
Our experience with clinical, community, and corporate initiatives highlights the importance of several factors for promoting the use of RE-AIM dimensions and methods. Calls to action include actions to: (A) recognize that technical assistance will be important for users from clinical, community, corporate, and/or academic settings to understand each RE-AIM element and how the different elements relate to one another; (B) utilize RE-AIM as a whole, but know it is acceptable to track the most relevant individual elements based on local interests and resources; and (C) give attention to common RE-AIM concepts and elements within each dimension—as well as potential measures—to bridge interventions across various clinical, community and corporate settings.
Author Contributions
All authors contributed to the conceptualization of the manuscript and its content. All authors contributed to the full manuscript as well as reviewed and approved the final version of the manuscript.
Conflict of Interest Statement
No financial conflicts of interest to report. All authors are members of the National Working Group on RE-AIM Planning and Evaluation Framework (www.re-aim.org).
Funding
The authors would like to acknowledge all members of the National Working Group on RE-AIM Planning and Evaluation Framework (www.re-aim.org). The authors would also like to acknowledge funding support for author contributions: MO and MS contributions supported through ACL SUSTAIN for Better Health and Health Care for Older Adults 90CS0065-01. PE contributions supported by Great Plains IDEA CTR U54 GM115458-01. RE contributions partially supported by IMPlementation to Achieve Clinical Transformation (IMPACT): the Colorado Training Program from the NIH K12 HL137862.
Supplementary Material
The Supplementary Material for this article can be found online at https://www.frontiersin.org/articles/10.3389/fpubh.2018.00071/full#supplementary-material.
Appendix A. Planning and evaluation document, which includes prompts and considerations across all five RE-AIM dimensions by temporal stage within a project (http://www.re-aim.org/resources-and-tools/self-rating-quiz/).
Footnotes
- ^www.dissemination-implementation.org.
- ^www.re-aim.org.
- ^http://re-aim.org/wp-content/uploads/2016/08/Planning-and-Evaluation-Tool.pdf.
- ^Rhodes WRD, Glasgow RE. Stakeholder perspectives on costs and resource expenditures: addressing economic issues most relevant to patients, providers and clinics. Unpublished.
References
1. Bauer MS, Damschroder L, Hagedorn H, Smith J, Kilbourne AM. An introduction to implementation science for the non-specialist. BMC Psychol (2015) 3:32. doi:10.1186/s40359-015-0089-9
2. Gaglio B, Glasgow RE. Evaluation approaches for dissemination and implementation research. 2nd ed. In: Brownson RC, Colditz GA, Proctor E, editors. Dissemination and Implementation Research in Health: Translating Science to Practice. New York, NY: Oxford University Press (2017). p. 327–56.
3. Proctor EK, Brownson RC. Measurement issues in dissemination and implementation research. In: Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and Implementation Research in Health: Translating Science to Practice. New York, NY: Oxford University Press (2012). p. 261–80.
4. Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci (2013) 8:139. doi:10.1186/1748-5908-8-139
5. Rabin BA, Brownson RC, Haire-Joshu D, Kreuter MW, Weaver NL. A glossary for dissemination and implementation research in health. J Public Health Manag Pract (2008) 14(2):117–23. doi:10.1097/01.PHH.0000311888.06252.bb
6. Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med (2012) 43(3):337–50. doi:10.1016/j.amepre.2012.05.024
7. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health (1999) 89(9):1322–7. doi:10.2105/AJPH.89.9.1322
8. National Working Group on RE-AIM Planning and Evaluation Framework. RE-AIM Website (2018). Available from: http://www.re-aim.org (accessed March 1, 2018).
9. Gaglio B, Shoup JA, Glasgow RE. The RE-AIM framework: a systematic review of use over time. Am J Public Health (2013) 103(6):e38–46. doi:10.2105/AJPH.2013.301299
10. Kessler RS, Purcell EP, Glasgow RE, Klesges LM, Benkeser RM, Peek CJ. What does it mean to “employ” the RE-AIM model? Eval Health Prof (2013) 36(1):44–66. doi:10.1177/0163278712446066
11. Vinson CASK, Kerner JF. Dissemination and implementation research in community and public health settings. 2nd ed. In: Brownson RCG, Proctor E, editors. Dissemination and Implementation Research in Health. New York, NY: Oxford Press (2017). p. 359–83.
12. National Healthcare Quality and Disparities Report. (2016). Available from: https://www.ahrq.gov/research/findings/nhqrdr/nhqdr16/index.html (accessed March 1, 2018).
13. MacQueen KM, McLellan E, Metzger DS, Kegeles S, Strauss RP, Scotti R, et al. What is community? An evidence-based definition for participatory public health. Am J Public Health (2001) 91(12):1929–38. doi:10.2105/AJPH.91.12.1929
14. Organization for Economic Co-operation and Development. Glossary of Statistical Terms. (2007). Available from: http://ec.europa.eu/eurostat/ramon/coded_files/OECD_glossary_stat_terms.pdf (accessed March 1, 2018).
15. Harden SM, Gaglio B, Shoup JA, Kinney KA, Johnson SB, Brito F, et al. Fidelity to and comparative results across behavioral interventions evaluated through the RE-AIM framework: a systematic review. Syst Rev (2015) 4:155. doi:10.1186/s13643-015-0141-0
16. Glasgow RE, Estabrooks PA. Pragmatic applications of RE-AIM for health care initiatives in community and clinical settings. Prev Chronic Dis (2018) 15:170271. doi:10.5888/pcd15.170271
17. Institute for Healthcare Improvement. Plan-Do-Study-Act (PDSA) Worksheet. (2018). Available from: http://www.ihi.org/resources/Pages/Tools/PlanDoStudyActWorksheet.aspx (accessed March 1, 2018).
18. Estabrooks P, Wilson KE, McGuire TJ, Harden SM, Ramalingam NS, Schoepke L, et al. A quasi-experiment to assess the impact of a scalable, community-based weight loss program: combining reach, effectiveness, and cost. J Gen Intern Med (2017) 32:24–31. doi:10.1007/s11606-016-3971-0
19. Johnson SB, Harden SM, Estabrooks PA. Uptake of evidence-based physical activity programs: comparing perceptions of adopters and nonadopters. Transl Behav Med (2016) 6(4):629–37. doi:10.1007/s13142-015-0371-7
20. Harden SM, Johnson SB, Almeida FA, Estabrooks PA. Improving physical activity program adoption using integrated research-practice partnerships: an effectiveness-implementation trial. Transl Behav Med (2017) 7(1):28–38. doi:10.1007/s13142-015-0380-6
21. Glasgow RE, Riley WT. Pragmatic measures: what they are and why we need them. Am J Prev Med (2013) 45(2):237–43. doi:10.1016/j.amepre.2013.03.010
22. Stoutenberg M, Galaviz KI, Lobelo F, Joy E, Heath G, Hurber A, et al. A pragmatic application of the RE-AIM framework for evaluating the implementation of physical activity as a standard of care in health settings. Prev Chronic Dis (2018). (in press).
23. Krist AH, Glenn BA, Glasgow RE, Balasubramanian BA, Chambers DA, Fernandez ME, et al. Designing a valid randomized pragmatic primary care implementation trial: the my own health report (MOHR) project. Implement Sci (2013) 8:73. doi:10.1186/1748-5908-8-73
24. Krist AH, Glasgow RE, Heurtin-Roberts S, Sabo RT, Roby DH, Gorin SN, et al. The impact of behavioral and mental health risk assessments on goal setting in primary care. Transl Behav Med (2016) 6(2):212–9. doi:10.1007/s13142-015-0384-2
25. Glasgow RE, Kessler RS, Ory MG, Roby D, Gorin SS, Krist A. Conducting rapid, relevant research: lessons learned from the My Own Health Report project. Am J Prev Med (2014) 47(2):212–9. doi:10.1016/j.amepre.2014.03.007
26. Ory MG, Altpeter M, Belza B, Helduser J, Zhang C, Smith ML. Perceived utility of the RE-AIM framework for health promotion/disease prevention initiatives for older adults: a case study from the U.S. evidence-based disease prevention initiative. Front Public Health (2014) 2:143. doi:10.3389/fpubh.2014.00143
27. Department of Health and Human Services AoA. Empowering Older People to Take More Control of Their Health Through Evidence-Based Prevention Programs: A Public/Private Collaboration. Washington, DC: Government Printing Office (2006). Contract No.: OMB Approval No 0985-0018; HHS-2006-AoA-BP-0611.
28. Belza B, Altpeter M, Smith ML, Ory MG. The healthy aging research network: modeling collaboration for community impact. Am J Prev Med (2017) 52(3s3):S228–32. doi:10.1016/j.amepre.2016.09.035
29. Centers for Disease Control and Prevention and the Kimberly-Clark Corporation. Assuring Healthy Caregivers, A Public Health Approach to Translating Research into Practice: The RE-AIM Framework. Neenah, WI: Kimberly-Clark Corporation (2008). Available from: https://www.cdc.gov/aging/caregiving/assuring.htm (accessed March 1, 2018).
30. Health Foundation of South Florida. Healthy Aging Regional Collaborative. (2008). Available from: http://www.healthyagingsf.org/ (accessed March 1, 2018).
31. Department of Disabilities, Aging and Independent Living. Healthy Aging and Independent Living Initiative, Evaluation Report 2014 Annual Report. (2015). Available from: http://dail.vermont.gov/ (accessed March 1, 2018).
32. Smith-Ray RL, Nikzad N, Singh T, Jiang JZ, Taitel MS, Quer G, et al. Physical activity trends of adults with chronic conditions participating in a digital health program. Poster Presented at the Annual Meeting of the Society of Behavioral Medicine, New Orleans, LA (2018).
33. Taitel M, Jiang J, Akinbosoye O, Orr G. The relationship between online activity & biometric tracking and medication adherence among members with hypertension. Society of Behavioral Medicine 36th Annual Meeting. San Antonio, CA (2015).
34. Taitel M, Jiang J, Akinbosoye O, Orr G. The relationship between online activity and biometric tracking and medication adherence among members with diabetes. American Diabetes Association’s 75th Scientific Sessions. Boston, MA (2015).
35. Estabrooks PA, Allen KC. Updating, employing, and adapting: a commentary on What does it mean to “employ” the RE-AIM model. Eval Health Prof (2013) 36(1):67–72. doi:10.1177/0163278712460546
36. Glasgow RE. What does it mean to be pragmatic? Pragmatic methods, measures, and models to facilitate research translation. Health Educ Behav (2013) 40(3):257–65. doi:10.1177/1090198113486805
37. Gupta DM, Boland RJ Jr, Aron DC. The physicians’ experience of chancing clinical practice: a struggle to unlearn. Implement Sci (2017) 12(28). doi:10.1186/s13012-017-0555-2
38. Chambers DA, Norton WE. The adaptome: advancing the science of intervention adaptation. Am J Prev Med (2016) 51(4 Suppl 2):S124–31. doi:10.1016/j.amepre.2016.05.011
39. Hall TL, Holtrop JS, Dickinson LM, Glasgow RE. Understanding adaptations to patient-centered medical home activities: the PCMH adaptations model. Transl Behav Med (2017) 7(4):861–72. doi:10.1007/s13142-017-0511-3
40. Klesges LM, Estabrooks PA, Dzewaltowski DA, Bull SS, Glasgow RE. Beginning with the application in mind: designing and planning health behavior change interventions to enhance dissemination. Ann Behav Med (2005) 29(Suppl):66–75. doi:10.1207/s15324796abm2902s_10
41. Palinkas LA, Aarons GA, Horwitz S, Chamberlain P, Hurlburt M, Landsverk J. Mixed method designs in implementation research. Adm Policy Ment Health (2011) 38(1):44–53. doi:10.1007/s10488-010-0314-z
42. Aarons GA, Fettes DL, Sommerfeld DH, Palinkas L. Mixed methods for implementation research: application to evidence-based practice implementation and staff turnover in community based organizations providing child welfare services. Child Maltreat (2012) 17(1):67–79. doi:10.1177/1077559511426908
43. Feldstein AC, Glasgow RE. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt Comm J Qual Patient Saf (2008) 34(4):228–43. doi:10.1016/S1553-7250(08)34030-6
Keywords: translation, health promotion, knowledge transfer, implementation science, evaluation framework, dissemination and implementation research
Citation: Harden SM, Smith ML, Ory MG, Smith-Ray RL, Estabrooks PA and Glasgow RE (2018) RE-AIM in Clinical, Community, and Corporate Settings: Perspectives, Strategies, and Recommendations to Enhance Public Health Impact. Front. Public Health 6:71. doi: 10.3389/fpubh.2018.00071
Received: 04 January 2018; Accepted: 22 February 2018;
Published: 22 March 2018
Edited by:
Mary Evelyn Northridge, New York University, United StatesReviewed by:
Melissa Bopp, Pennsylvania State University, United StatesKatie M. Heinrich, Kansas State University, United States
Copyright: © 2018 Harden, Smith, Ory, Smith-Ray, Estabrooks and Glasgow. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Samantha M. Harden, aGFyZGVuLnNhbWFudGhhQHZ0LmVkdQ==
 Samantha M. Harden
Samantha M. Harden Matthew Lee Smith
Matthew Lee Smith Marcia G. Ory
Marcia G. Ory Renae L. Smith-Ray
Renae L. Smith-Ray Paul A. Estabrooks6
Paul A. Estabrooks6