- 1College of Public Health, Medical and Veterinary Sciences, James Cook University, Cairns, QLD, Australia
- 2Australian Institute of Tropical Health and Medicine, James Cook University, Cairns, QLD, Australia
Background: Cannabis harms among Indigenous populations in Australia, New Zealand, Canada and the United States may be magnified by poorer health and heavy use. However, little direct evidence is available to evaluate cannabis' impacts. In communities in remote northern Queensland (Australia) where cannabis has become endemic, opportunities to support change were investigated.
Methods: Opportunistically recruited participants (aged 15–49 years) discussed their cannabis use history in interviews in two waves of population sampling in Cape York (Queensland). Wave 1 included 429 people (235 males and 194 females); and wave 2 included 402 people (228 males and 174 females). Current users (used cannabis during the year before interview) described frequency of use, amount consumed, expenditure and dependence symptoms. Other substance use was recorded for 402 people at wave 2.
Results: Wave 1: 69% reported lifetime use and 44% current use. Males (55%) were more likely than females (30%) to be current users (P < 0.001). Most (96%) current users described at least weekly use; nearly half (48%) were “heavy” users (≥6 cones/session at least once/week) and 77% met cannabis dependence criteria. Three communities spent up to $AUD14,200/week on cannabis, around $AUD2.0 million/year, or around 9% of community people's total income on cannabis. The majority (79%) of current users wanted to quit or reduce their cannabis use. Wave 2: no difference was observed in the proportion of lifetime (69%, |z| = 0.04, P = 0.968) or current cannabis users (39%, |z| = 1.39, P = 0.164); nor current use among males (71%, |z| = 0.91, P = 0.363) or females (62%, |z| = 0.36, P = 0.719). However, a significant reduction in current users by 15% (|z| = 2.36, P = 0.018) was observed in one community. Of 105 wave 1 current users re-assessed in 2, 29 (27%) had ceased use. These participants reported cost and family commitments as reasons to change and that social support and employment enabled abstinence. Current and lifetime cannabis use were closely associated with all other substance use, particularly tobacco and alcohol (both P > 0.001).
Conclusions: High rates of heavy cannabis use in remote Australian Indigenous communities warrant action. Successful cessation among some individuals suggests that significant opportunities are available to support change even where cannabis use may be endemic.
Introduction
While cannabis remains the most widely used illicit substance worldwide, its use has generally decreased in countries like the United States, Canada, New Zealand and Australia (1). In contrast, rates of cannabis use in the Indigenous populations of these developed economies are 1.3–1.9 times higher than respective national averages (2–5). Systematic evidence is lacking on the specific impacts of cannabis in Indigenous populations, and on how to assist Indigenous peoples to reduce harms.
In the general population, cannabis use is associated with symptoms of: anxiety (6), depression (6–8), dependence (6, 7, 9), and withdrawal (10–12), acute cognitive impairment (13), possible long-term cognitive impairment (14), and schizophrenia (13, 15–17); with evidence that cannabis causes psychosis (15, 18–20) becoming stronger (17, 21, 22). Normalization of cannabis use within some sectors of the community (23), and polarized debates about cannabis policy (24), may have diverted attention from its impacts in marginalized and impoverished populations, where harms from most forms of substance use are magnified by the higher prevalence of heavier, riskier patterns of use. Heavier use and significant mental health impacts of cannabis are known in American Indian populations (25), for instance, with very early uptake first nations youth in the United States (26, 27) and Canadian (28). Indigenous Australians, according to national surveys, use cannabis at around 1.6 times the national rate (22). However, these estimates do not include the most remote community populations, such as those in Australia's far north (Northern Territory and north Queensland). These populations are among the more severely disadvantaged and socially excluded populations in the country and have a disproportionate share of a largely preventable chronic disease burden, including that linked with substance misuse (29).
Cannabis became more readily available in remote Indigenous Australian communities just over 20 years ago. Its use was undetected in the 1980s (30) and surged from the late 1990s to as high as 60% in some age groups, more than double national rates (31). Even with such brief exposure, in the Northern Territory's remote Arnhem Land region, high proportions of young users continued to report regular cannabis use between 2001 and 2006 (32, 33). Such use was associated with dependence (33), depression (7), auditory hallucinations, suicidal ideation (7, 32), and imprisonment (34, 35). In similar remote communities in north-eastern Australia (Queensland's Cape York), cannabis users and the communities in which they live may also suffer a heavy burden of cannabis-related harms (36, 37).
Cannabis use is a neglected public health issue in Australia's remote Indigenous communities (38), despite their consistently expressed concerns about its impacts (35, 39). This paper provides evidence from a survey of cannabis use in remote Indigenous communities in north Queensland that describes patterns of use, harms and attitudes toward cannabis.
Methods
Hypotheses
Data included in the present analysis comprises semi-structured interviews conducted with participants before and after a community level intervention, with additional participants recruited at the second time-point. It is, therefore, not a before and after study, but represents a sizable sample from each site in two waves of sampling. This study hypothesized:
1. An overall reduction in current users as a result of growing awareness of cannabis harms suggested in the consultations, as well as social marketing activities that occurred between sampling waves.
2. Qualitative examination of those who had ceased using cannabis between the first and second waves would suggest common important factors influencing their decisional balance.
Setting
Cape York in far north Queensland covers ~211,000 km2 with a population of around 20,000 (outside its major regional center and towns). Included are 11,700 Aboriginal and/or Torres Strait Islander (Indigenous) Australians living in 12 very small, self-governing communities with populations ranging from <200 to 2,500 people. Although English is widely spoken, it is usually a second language (or a creole), and many traditional practices are maintained (40). Vehicle access is via unsealed roads, which close for several months in the annual wet season.
Consultation throughout 2007–2008 established community permissions for the study (36). Communities were selected to broadly represent the contemporary settlement pattern for Indigenous people in the region: one near a regional center (Community A); another on Cape York's wet tropical east coast (Community B); and a third on the west coast in drier savannah country (Community C). The three study communities had a combined Indigenous population of 2,187, with 1,172 of these aged 15–49 years at census in 2011 (41).
Queensland Government departments of Health, Education and Police have a presence in all communities. All communities have primary healthcare clinics (PHCs) staffed by allied health workers, including drug and alcohol treatment workers, who periodically fly in from regional centers during the working week. The PHCs also employ local Indigenous health workers and nurses who live in the communities.
There is no published evidence available for the use of illicit drugs other than cannabis in these communities. The sale of alcohol is locally prohibited and its possession and carriage has been tightly restricted since 2008 across Cape York (42).
Participants and Sampling
Participant Recruitment
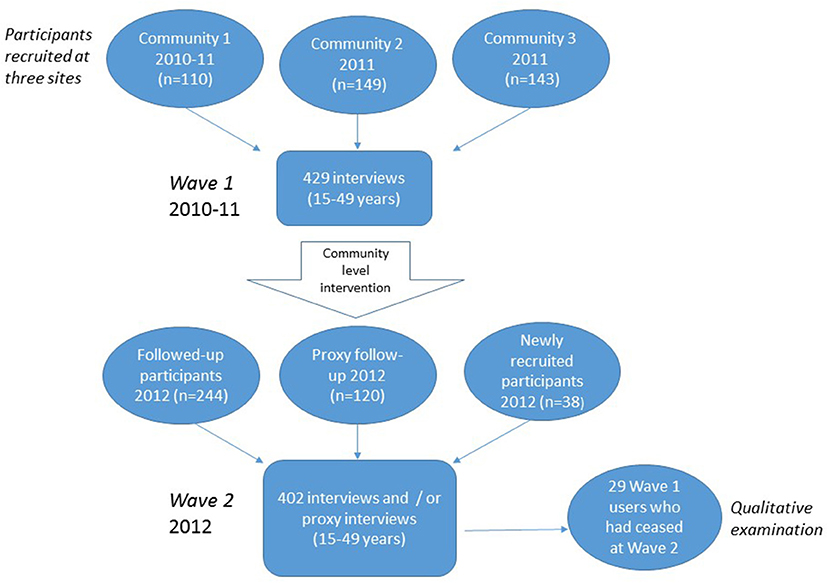
Data collection at two time-points and its and use in the analysis is shown in Figure 1. Participants were approached for the first wave of interviews between May 2010 and October 2011 as a baseline for a community level demand reduction program. The second wave occurred between May and December 2012, including those participants who were followed up as well as newly recruited participants. This analysis uses all available data from the two waves of sampling to explore inter- and intra-community variations. In practice, because of the brief time between samples in each community, sampling was more-or-less continuous across the three communities as a whole. Research staff visited the communities for 3–5 days, traveling from the regional center (Cairns, 800–1,000 km by road). With stigmatized or illegal behaviors the subject of interest, random sampling in these small community settings is ethically unsustainable (32–34). Recruitment was therefore opportunistic, following strategies used in the Arnhem Land (NT) studies (31, 34), and targeting younger age groups. Researchers alerted communities at least 2 weeks in advance of visits, spending 3 to 5 days in the community each time. Project personnel approached participants outside of the PHC, the community store or in the street and at work places and homes, usually with the paid assistance of a local person.
Wave 1 Interviews
We used a conversational approach, employed routinely in these localities to work across cultural barriers (33). Semi-structured interviews documented demographics, and lifetime cannabis use. Interviews lasted from 10 min—if participants had little or no experience with cannabis or offered only brief responses— to 30 min, if participants engaged in rich “yarning” about their experiences with cannabis. Current users were asked about frequency of use, age of first/last use, estimated quantity used and weekly expenditure on cannabis. Five severity of dependence scale (SDS) questions were administered to current users (40). Open-ended questions elicited qualitative information from current and former cannabis users about any intentions to change and reasons why.
Wave 2 Interviews and Proxy Assessments
In the second wave, researchers recruited new participants to the study and attempted to follow-up all of the original participants. Proxy reports for current or former cannabis use were sought at wave 2 for all participants interviewed at wave 1. Proxy data for use status was used where the participant could not be interviewed at wave 2, a strategy used previously in Arnhem Land (43). In addition to lifetime cannabis use, participants provided data about current and lifetime use of alcohol, tobacco, volatile substances, and other illicit drugs. The SDS questions were administered to current users where the participants consented.
Data
Cannabis Use
As in previous studies (32), self-reported cannabis use was described as “never” (never tried cannabis), “former” [tried cannabis once or had not smoked it for ≥12 months, consistent with national data (22)] and “current” (had tried or used cannabis within the past 12 months). Mean duration of use, calculated from age first used and age last used, took account of any significant breaks due to e.g., hospitalization, pregnancy, working or studying away from the community, prison or detention.
Frequency of Cannabis Use–Current Users
Self-reported frequency of cannabis use among current users was categorized as in previous studies: “daily” (5–7 times/week), “weekly” (1–4 times/week), or “monthly” (1–2 times/month) (33).
Defining “Heavy” Cannabis Use
Reported quantities of cannabis used ranged widely from “one cone a session” to “more than twenty,” making precise quantification difficult. To address a wide diversity of consumption levels and patterns (32), “heavy” use was defined as ≥6 cones per session at least once per week, in line with criteria used in the Arnhem Land (NT) studies.
Weekly Expenditure on Cannabis
Current users were asked to estimate the usual number of “foils” or “sachets” purchased weekly or fortnightly, the price paid ($AUD) and how many people they shared with.
Cannabis Dependence
Dependence in current users was assessed using the five-item SDS, with scores depicted as a colored chart to address literacy barriers and using a cut-off score ≥3 symptoms experienced in the preceding 3 months (40).
Defining “Trying to Quit”
Further questions, asked of current users who expressed any desire to change, distinguished those who wished to reduce cannabis from those who wished to stop altogether. “Trying to quit” included those who reported current active quit attempts or who reported avoiding cannabis use at some time during the preceding 12 months.
Reasons for Cessation
Qualitative examination of a subset of interviews with participants who were current users at wave 1 but had ceased cannabis use at wave 2, summarized the principal reasons reported for quitting, barriers to quitting and the resources used to support quitting.
Data Analysis
Quantitative data was analyzed in SPSS (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp). Qualitative data was stored in spreadsheets and imported into NVivo™. Categorical data were compared using the Chi square statistic with 95% confidence intervals. Ordinal variables were compared using the Wilcoxon rank-sum test.
Ethics Approval
The Human Research Ethics Committees of James Cook University and the Cairns and Hinterland Health Services District provided ethical approvals. Study results were provided back to the study communities and their lead agencies after the survey was completed in order to stimulate local action and advocacy among key stakeholder groups.
Results
Sample
In total, 429 participants aged 15–49 years were interviewed in the first wave of data collection, equivalent to 37% (= 429/1,172) of the estimated total community populations in this age group. The sample included 55% males (n = 235) and 45% females (n = 194). This differed from the 2011 census (43) proportions of 49% males and 51% females (|z| = 2.06, P = 0.033) in these age groups in the study communities. The proportion of participants (49% = 203/429) aged 15–24 years in the sample was considerably greater than recorded in the census (28%) (|z| = 7.28, P < 0.001).
In the second wave, approximately 12 months later, data were collected for 402 people, including: 244 wave 1 participants who completed follow-up interviews; 120 proxy assessments of wave 1 participants; and 38 new participants. Proportions of males (n = 228, 57%) and females (n = 174, 43%) were similar to the first wave (|z| = 0.56, P = 0.575), and similarly different to the 2011 census (|z| = 2.68, P = 0.007). Overrepresentation of younger participants aged 15–24 years (37% = 149/402) compared to the census data (28%) (|z| = 3.42, P > 0.001), was more pronounced than at wave 1 (|z| = 2.99, P = 0.003).
Patterns of Use at Wave 1
Reported Lifetime Cannabis Use Varied Across the Communities and Gender Groups
The proportions of the sample reporting cannabis use at least once in their lifetime ranged from 54 to 81% across the communities (69% overall) (Table 1A). In community C, almost half the participants (46%) had never used cannabis, whereas in community A, this was true of fewer than one in five (19%) (Table 1A).
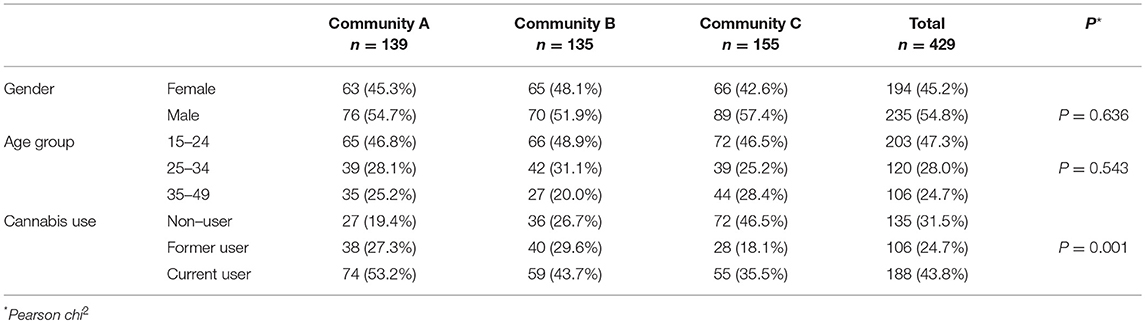
Table 1A. Demographic characteristics and cannabis use in 429 people (235 males and 194 females, aged 15–49 years) interviewed at wave 1 in three Cape York communities, far north Queensland, Australia, 2010–2011.
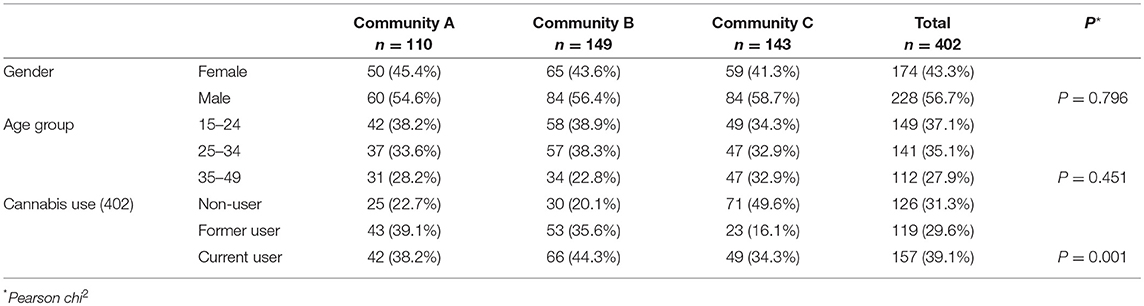
Table 1B. Demographic characteristics and cannabis use in 402 people (228 males and 174 females, aged 15–49 years) with data at wave 2 (followed-up, 244; proxy, 120; or newly recruited, 38) in three Cape York communities, far north Queensland, Australia, 2012.
Overall, males (77%) were more likely to report lifetime use than females (59%) (P < 0.001). Age-standardized rates were 78% of males, 52% of females and 65% overall. However, the differences in the crude proportions of lifetime users also varied across communities: A (86% males, 75% females, P = 0.105); B (79% males, 69% females, P = 0.299) and with women less likely to have ever tried cannabis in community C only (69% males, 33% females, P < 0.001).
The proportion of lifetime users (71%) in the younger participants (aged 15–24 years) was similar (66%) to older participants (aged 25–49 years) (P = 0.221) and varied little across the communities.
Current Users
Males were generally more likely to report current cannabis use in the sample in all three communities: A (66% males, 38% females, P = 0.001); B (51% males, 35% females, P = 0.060) and C (49% males, 17% females, P < 0.001) and around three times more likely overall (55% males, 30% females, P < 0.001). Age standardized rates were 55% for males and 26% for females, 40% overall.
Age of Uptake and Duration of Use Among Current Users
Table 2A describes the patterns of cannabis use among 188 current users, comprised of 69% males (n = 130) and 31% females (n = 58). Their median age was 24 years, with males around 2 years older than females (P = 0.063). Participants had used cannabis for up to 30 years (median = 11 years for males, = 6 years for females, P = 0.003). Age of first use was similar in males and females (median = 16 years, P = 0.714) (Table 2A).
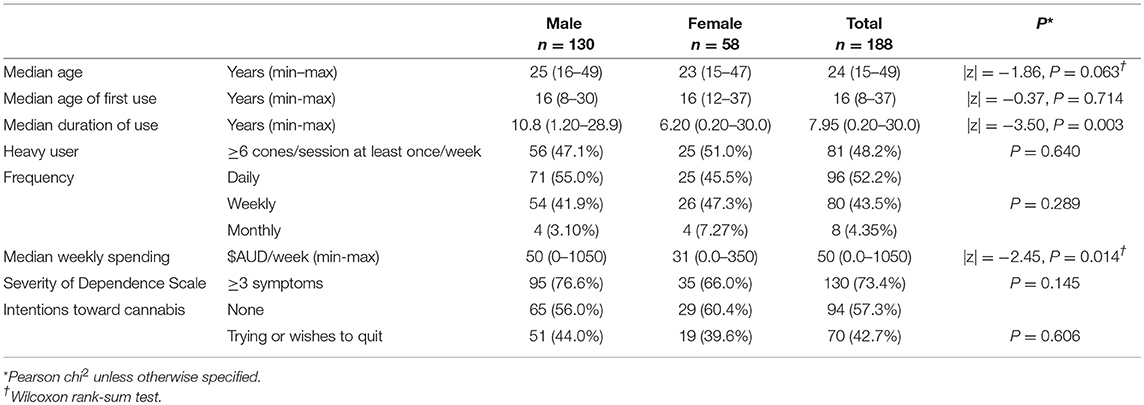
Table 2A. Patterns of cannabis use by gender in 188 current users (aged 15–49 years) interviewed at wave 1 in three Cape York communities, far north Queensland, Australia, 2010–2011.
Patterns of Current Use
Almost half (48%) of the 168 current users, for whom information was available were “heavy users” with similar proportions in males (47%) and females (51%) (P = 0.640 Table 2A). Half (52%) of 184 current users reported using cannabis on a daily basis, another 43% used it on a weekly basis. The majority used cannabis regularly, with little difference between males (97%) and females (93%) (Table 2A).
Style of Cannabis Use and Expenditure by Current Users
The nominated preferred style of use in all three communities was hand-made “bucket bong,” a negative pressure device constructed from a bottomless bottle with a cone piece inserted into the lid, plunged into a larger container of water to draw the smoke in to be inhaled from the bottle. Almost all current and former users reported that they mixed tobacco with cannabis.
Across the communities, participants reported that cannabis was purchased from dealers (i.e., not cultivated in the community), with further distribution within the community through on-selling or sharing. Cannabis was mostly supplied in aluminum “foils” or plastic “sachets” with prices ranging from $AUD20 to $AUD50 per unit. Users reported considerable variation in the unit quantity and quality of cannabis material, often premixed with tobacco.
Males tended to spend more on purchasing cannabis than females, $AUD50/week compared with $AUD31/week (|z| = 2.45, P = 0.014, Table 2A). With current users comprising 44% (= 188/429) of the sample, this means there may be 514 (= 188/429*1,172) current users in the 15–49 years age group in the three communities overall. A crude estimate of total expenditure on cannabis in this age group in these three communities is $AUD39,000 per week (= 514/188*$AUD14,200/week) equivalent to just over $AUD2.0 million/year.
Severity of Cannabis Dependence (SDS) in Current Users
Three quarters (73%) of the current users met criteria for cannabis dependence (SDS ≥ 3), with similar proportions in males (77%) and females (66%) (P = 0.145), Table 2A). Data not shown indicates that similar proportions of current users met dependence criteria in both the younger (74%, 15–24 years) and older (73%, 25–49 years) age groups (P = 0.813). Those in the “heavy use” category were no more likely than other current users to meet criteria for cannabis dependence (P = 0.787). Current users who met dependence criteria, however, spent more on cannabis (median spend = A$50/week) than those who did not (median spend = A$38/week) (|z| = 2.09, P = 0.036).
Patterns of Use at Wave 2
Reported Lifetime Cannabis Use Varied Across the Communities and Gender Groups
Shown in Table 1B, the proportions of the sample reporting cannabis use at least once in their lifetime ranged from 79 to 50% across the communities (69% overall) which was not different to wave 1 (|z| = 0.04, P = 0.968). In community C, half (50%) had never used cannabis, whereas in community A, this was true of less than a quarter (23%). No significant differences in proportions of non-users were recorded between wave 1 and wave 2 samples across the communities: A (19% wave 1, 23% wave 2 |z| = 0.64, P = 0.522); B (27% wave 1, 20% wave 2, |z| = 1.30, P = 0.194) and community C (46% wave 1, 50% wave 2, |z| = 0.55 P = 0.582).
Overall, at wave 2, males (78%) were more likely to report lifetime use than females (56%) (P < 0.001). Age standardized rates of lifetime cannabis use were 80% for males and 53% for females overall. However, the differences in the crude proportions of lifetime users also varied across communities: A (85% males, 68% females, P = 0.034); B (86% males, 72% females, P = 0.043) and strongest in community C (67% males, 27% females, P < 0.001). As for the sample at wave 1, the proportion of lifetime users at wave 2 (68%) in the younger participants (aged 15–24 years) was similar (69%) to older participants (aged 25–49 years) (P = 0.947) and varied little across the communities.
Current Users at Wave 2
No statistically significant difference was detected in the proportion of cannabis users in the overall sample at wave 1 (n = 188, 44%) compared to wave 2 (n = 157, 39%) (|z| = 1.39, P = 0.164). Shown in Table 2B, age standardized rate of current use among males was 52% and 21% for females. A significant reduction of 15% in current users (53 to 38%, |z| = 2.36, P = 0.018) was recorded in community A. The proportion of heavy users in the sample at wave 2 (63%) was higher than at wave 1 (51%) (|z| = 2.40, P = 0.016). Compared to wave 1, the proportion of males (71%, |z| = 0.91, P = 0.363), females (62%, |z| = 0.36, P = 0.719) and younger users (69%, |z| = 0.62, P = 0.535) reporting more than three symptoms of dependence were not different at wave 2. The median weekly spending at wave 2 of $50 per week was not different to wave 1 overall, with a similar difference between males and females ($55 and $30 per week, respectively (|z| = 2.57, P = 0.010).
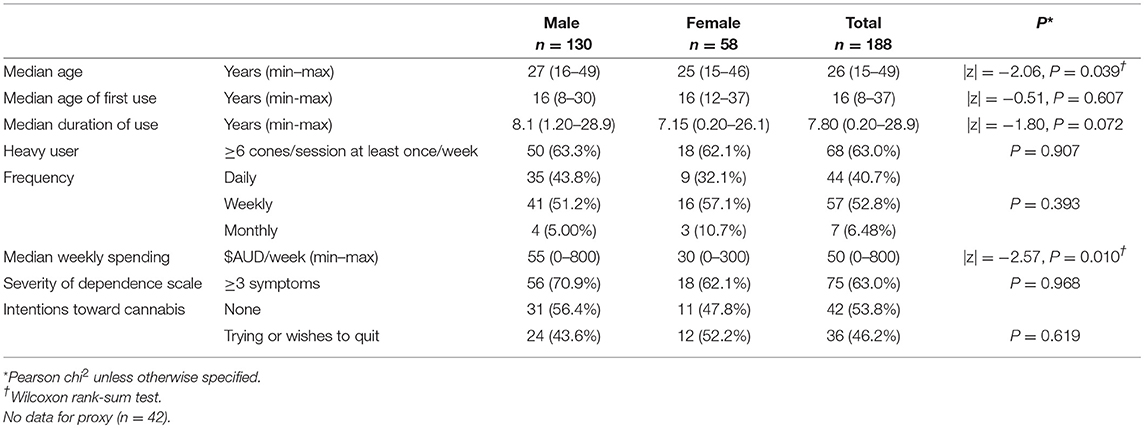
Table 2B. Patterns of cannabis use by gender in 157 current users (aged 15–49 years) with wave 2 data, either followed up (88) or newly recruited (27) in three Cape York communities, far north Queensland, Australia, 2010–2011.
Lifetime and Current Substance Use at Wave 2
Lifetime use of cannabis was linked with lifetime use of tobacco, alcohol and other illicit substances (P < 0.001). Current use of cannabis (39%) was strongly associated with current use of tobacco (74%, P < 0.001) and alcohol (64%, P < 0.001). Seven participants reported current inhalant use and all of these were current cannabis users.
Qualitative Information
Quit Intentions Among Current Users
Of 188 current users at wave 1, 164 provided information about their intentions to stop or reduce cannabis use. Overall, 70 current users (43%) indicated they were trying or wanted to quit (Table 2A), including 10% (n = 16) actively trying to quit at wave 1. At wave 2, 46% (36/78) said they wanted to change.
Reasons for Change Among Participants Who Ceased Using Cannabis Between Wave 1 and Wave 2
Twenty-nine participants who were “current users” at wave 1 (2011) were no longer using cannabis at wave 2 (2012). This included 14 women and 15 men, with no obvious differences in distribution across age groups, genders or communities.
Among 15 men, 11 said they wanted to quit, including five who were then making a quit attempt when first interviewed in 2011. Two had said they wished to cut down and only one had said that he did not want to quit. Nine of these men explained their reasoning: it was too expensive or a waste of money (3); family as the principal reason for quitting, particularly concern for their children (4); and health reasons or getting older (2). Among 14 women who had ceased cannabis use, 5 had indicated a desire to quit at wave 1, including 2 actively trying to quit. A further two said they would like to cut down and three who did not answer the question nonetheless discussed earlier quit attempts. Seven explained their reasoning: family (including children and pregnancy) (4) or for work (3).
Only men in this group of successful quitters mentioned the expense of cannabis as a reason to stop, perhaps reflecting the tendency for men to spend more on cannabis and suggesting that women are probably more likely to source cannabis from partners or family members. One young man described how he demonstrated for himself how much money he was wasting by collecting the packaging:
“Started collecting sachets this year. Ten sachets is $500. I've spent $1000 on that silly thing this year.”
Resources that enabled cessation mentioned by these 29 participants included: keeping busy with work; childcare or cultural activities; or spending time with non-using friends and family. For example, a young woman said that she would “get help from sisters and brothers because they understand” (Table 3). Conversely, cue exposure and normalization was a barrier to cessation for the young man referring to “other boys, temptation” (Table 3 “Barriers in context”).Only one person mentioned health services as a possible strategy to support cessation.
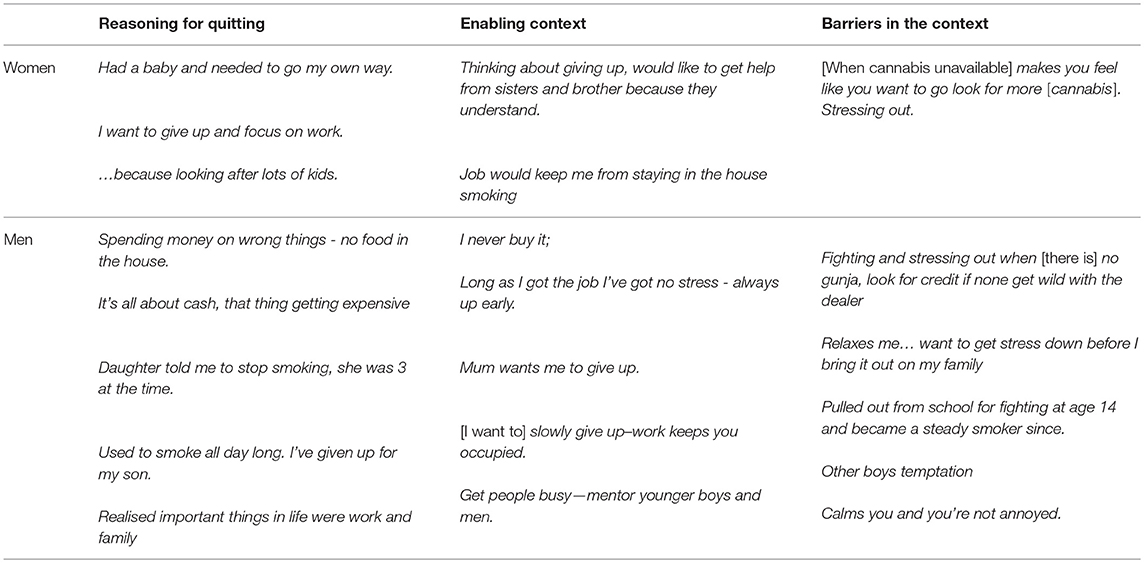
Table 3. Participant reasoning for successful quit attempts between wave 1 and wave 2 and enablers and barriers mentioned.
This 22-year old man described a variety of arguments and opportunities that he believed would support cannabis cessation:
“Put food on the table; buy power card; get the outstations going; get cattle; hunting. [It causes] fighting and stressing out…”
Selected quotes summarized in Table 3 describe reasons for quitting, and similar enablers and barriers in context.
Discussion
Although there was some variation in the crude rates across the participating communities in Cape York, age-standardized rates of lifetime cannabis use of 65% (78% for males and 52% for females) found in this study are higher than in the general Australian population where just under half of those in comparable age groups report lifetime use (22). The age-standardized proportions of current cannabis users at wave 1 in the study (55% of males and 26% of females aged 15–49 years), 40% overall, are similar to 67% males and 22% females (aged 13–36 years), and around 50% overall, documented in Arnhem Land (NT) in 2001 (34), most of whom were still users at follow-up in 2005–06 (38). Again similar to Arnhem Land (34), around half (48%) of the current users in this study were categorized as “heavy users,” with most (>90%) using cannabis at least weekly (Table 2A).
The highest rate of past year cannabis use reported nationally in 2010 was 25% for males (aged 20–29 years) and 19% for females (aged 18–19 years) (2). In this study, however, almost all the current cannabis users reported at least past month use, compared with < 6% (aged ≥14 years) past month use nationally. It is noteworthy that between 1998 and 2007, in Australia generally, there was a sharp decline in cannabis use from 17.9 to 9.1%. This included a decline from 36.5 to 13.8% in the NT and from 17.5 to 9.5% in Queensland (2). At the same time in the NT (31), however, and now documented in far north Queensland, cannabis use probably increased to become the significant challenge for cannabis users and the general community population that it is today.
Opportunities to Address Cannabis Use
Although crude rates of lifetime use found in the study were very high (69%), it is encouraging that more than a third of lifetime users had succeeded in quitting in the samples. Among 29 people who had ceased using cannabis at wave 2, pregnancy among women (44) and perceived barriers of withdrawal stress (45), limited recourse to clinical support and the importance of the social context (46) have been reported as challenges to quitting cannabis in other populations. Adults in other populations have seldom reported employment and financial impacts cessation drivers, perhaps reflecting the extremely limited employment opportunities and young age of many of the users in the current study.
Self-selection of a supportive environment, important in self-initiated cessation (44), is difficult in remote Indigenous Australian communities. Cannabis use is normalized among close-knit family groups living in generally overcrowded housing. Cue exposure is high and opportunities for meaningful long-term employment are limited. Intensified cessation support from health services is warranted but, as noted in other high-risk populations (46, 47), these must be proactive in incorporating latent and active strategies already embedded in the local social context (13). For example, interventions may incorporate the effects of widespread trauma (48), cultural perspectives (49), and social support (50). Work readiness programs may assist those seeking to quit, especially if aligned with genuine employment opportunities.
Widespread community concern about youth uptake and its effects on mental health is a prevention opportunity. It is generally recognized that young people should be advised that early cannabis use may bring serious long-term harms (51) and, as the following quote demonstrates, Indigenous community members recognize this, exemplified by the following quote from an interview with a woman in her early twenties:
“Young kids start and then build up and don't stop. Get addicted early.”
Efforts to reduce adolescent uptake also need to target the social context in which cannabis is used to add strength to a focus on individual decisional balance (52). Social marketing to support others' cessation might be used to better effect than raising awareness of individual level harms. Resourcing and policy to support youth engagement in school or training and strong social supports are critical.
Local financial impacts are significant, with high cost a frequently reported negative consequence for current users (36, 53). The crude estimate of the local cannabis trade at ~$AUD39,000/week in this small population of around 2,187 people is similar to estimates a decade ago for NT communities ($AUD19,000–$AUD32,000/week for 2,649 people) (33). The gross annual income of the Indigenous members of the three communities in this study is approximately $25.1 million (43), of which, the local cannabis market may constitute around 9%. This parallels the widely voiced concern about broader adverse impacts on families and community and concerns about financial impacts reported during earlier consultation (35). Since similar impacts have been documented for similar remote NT communities (33) this information could be incorporated into motivational strategies and general social marketing to encourage support for those seeking to quit.
Cannabis Dependence, “Heavy Use” and Weekly Expenditure
The association between cannabis dependence [probably reinforced by nicotine (54)] and weekly expenditure on cannabis by current users (P = 0.023) confirms concerns about adverse financial impacts of trafficking and addiction in users. The expected association between cannabis dependence and “heavy use” was not apparent, perhaps because of the narrow range of levels of use found. Notwithstanding the challenges of measuring “heavy use,” the precise nature of the experience of cannabis dependence in these settings, where resources such as cannabis and money to purchase it are shared, requires further research into the social underpinnings of addiction in this population.
Study Limitations
This sample was not randomly selected, but included more than one-third of males and females aged 15–49 years in the study communities, and nearly half of the 15–24 year-olds at each site. While there was bias in the overall sample toward younger and hard-to-reach males, the proportions of males and females in these age groups were broadly consistent across the communities (Tables 1A,B). Therefore, gross differences between communities in prevalence of cannabis use are less likely to be distorted by this sampling bias although the overall sample results may not be generalizable.
Conclusions
The high rate of heavy and problematic cannabis use in remote Indigenous Australian communities is clearly not isolated to one part of northern Australia as reported in the limited available literature on the topic (32, 33). Substantial numbers of users in our sample were seeking to quit, which may be encouraging for people living in the participant communities. We can no longer overlook the opportunities revealed in this modest study to assist similar community populations to reduce cannabis use and address its local harms.
Indigenous populations living in similarly isolated communities elsewhere in the world, where fundamental asymmetries of social and economic power are most stark, may be especially vulnerable to experiencing cannabis harms (29, 37). Indigenous vulnerability to heavy episodic substance use reflects socioeconomic disadvantage relative to the wider economic situation (55) in a population along with a range of social (56), family (20, 39), and systemic factors (57–59). The influences of these factors on regional and ethnic variations in rates of cannabis use within nations like Australia are poorly understood and should be further investigated (21).
Author Contributions
VG was the lead project officer during wave 1 of data collection and the final part of wave 2. She performed the statistical calculations and wrote the first draft. AC designed the study, advised on statistical analysis methods, and approved the final manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors sincerely thank the three study communities, who must remain, for their warm welcome, and interview participants for sharing their stories. Community leaders and service providers are acknowledged for their cooperation and guidance. Members of the research team are acknowledged for their contributions during the project-Data collection: Yana O'Brien, Beatrice Lawrence, Winston Paul, Ray Genn, Michelle Fitts, Jan Robertson, Bernadette Rogerson, Susan Jacups, Brett Walsh, Eddie Buli, Jo Jarden Celia Demarchi, and India Bohanna. Thanks to Melissa Kirk for support with data processing. Thanks to Mick Dowie, Garry Hunter, John Harris, and Kevin Goan of the Queensland Police Service for their support to establish the study. This research was supported by NHMRC project grant #601002 from the National Health and Medical Research Council of Australia.
References
1. UNODC. World Drug Report 2012. Sales No. E.12.XI.1. Vienna: United Nations Office of Drugs and Crime. (2012). Available online at: http://www.unodc.org/documents/data-and-analysis/WDR2012/WDR_2012_web_small.pdf (Accessed January, 2013).
2. Australian Institute of Health and Welfare. (2007) National Drug Strategy Household Survey: Detailed findings. Canberra, ACT: AIHW. Drug statistics series no. 22. Cat. no. PHE 107. (2008). Available online at: http://www.aihw.gov.au/publication-detail/?id=6442468195 (Accessed March, 2018).
3. Ministry of health. Drug Use in New Zealand: Key Results of the 2007/08 New Zealand Alcohol and Drug Use Survey. Wellington: Ministry of Health (2007). Available online at: http://www.health.govt.nz/publication/drug-use-new-zealand-key-results-2007-08-new-zealand-alcohol-and-drug-use-survey (Accessed January 2018).
4. The First Nations Information Governance Centre. The First Nations Information Governance Centre, First Nations Regional Health Survey (RHS) Phase 2 (2008/10) National Report on Adults, Youth Children Living in First Nations Communities. Ottawa, ON: The First Nations Information Governance Centre. (2012) Available online at: http://www.rhs-ers.ca/sites/default/files/First_Nations_Regional_Health_Survey_2008-10_National_Report.pdf (Accessed January 2018).
5. Copeland WE, Hill S, Costello EJ, Shanahan L. Cannabis use and disorder from childhood to adulthood in a longitudinal community sample with American Indians. J Am Acad Child Adolesc Psychiatry (2017) 56:124–32.e2. doi: 10.1016/j.jaac.2016.11.006
6. Coffey C, Carlin JB, Degenhardt L, Lynskey M, Sanci L, Patton GC. Cannabis dependence in young adults: an Australian population study. Addiction (2002) 97:187–94. doi: 10.1046/j.1360-0443.2002.00029.x
7. Lee KSK, Clough AR, Jaragba MJ, Conigrave KM, Patton GC. Heavy cannabis use and depressive symptoms in three aboriginal communities in Arnhem Land, Northern Territory. Med J Aust. (2008) 188:605–8.
8. Bovasso GB. Cannabis abuse as a risk factor for depressive symptoms. Focus (2003) 1:158–62. doi: 10.1176/foc.1.2.158
9. Roffman R, Stephens RS. Cannabis Dependence: Its Nature, Consequences and Treatment. Cambridge: Cambridge University Press (2006).
10. van der Pol P, Liebregts N, de Graaf R, Korf DJ, van den Brink W, van Laar M. Predicting the transition from frequent cannabis use to cannabis dependence: a three-year prospective study. Drug Alcohol Depend. (2013) 133:352–9. doi: 10.1016/j.drugalcdep.2013.06.009
11. Grotenhermen F. Pharmacokinetics and pharmacodynamics of cannabinoids. Clin Pharmacokinet. (2003) 42:327–60. doi: 10.2165/00003088-200342040-00003
12. Budney AJ, Moore BA, Vandrey RG, Hughes JR. The time course and significance of cannabis withdrawal. J Abnorm Psychol. (2003) 112:393. doi: 10.1037/0021-843X.112.3.393
13. Solowij N, Michie PT. Cannabis and cognitive dysfunction: parallels with endophenotypes of schizophrenia? J Psychiatry Neurosci. (2007) 32:30–52.
14. Baker ST, Yücel M, Fornito A, Allen NB, Lubman DI. A systematic review of diffusion weighted MRI studies of white matter microstructure in adolescent substance users. Neurosci Biobehav Rev. (2013) 37:1713–23. doi: 10.1016/j.neubiorev.2013.06.015
15. Arseneault L, Cannon M, Witton J, Murray RM. Causal association between cannabis and psychosis: examination of the evidence. Br J Psychiatry (2004) 184:110–7. doi: 10.1192/bjp.184.2.110
16. Cohen M, Solowij N, Carr V. Cannabis, cannabinoids and schizophrenia: integration of the evidence. Aust N Z J Psychiatry (2008) 42:357–68. doi: 10.1080/00048670801961156
17. Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet (2007) 370:319–28. doi: 10.1016/S0140-6736(07)61162-3
18. McLaren JA, Silins E, Hutchinson D, Mattick RP, Hall W. Assessing evidence for a causal link between cannabis and psychosis: a review of cohort studies. Int J Drug Policy (2010) 21:10–9. doi: 10.1016/j.drugpo.2009.09.001
19. Degenhardt L, Hall W. Is cannabis use a contributory cause of psychosis? Can J Psychiatry (2006) 51:556–65. doi: 10.1177/070674370605100903
20. Macleod J, Oakes R, Copello A, Crome I, Egger M, Hickman M, et al. Psychological and social sequelae of cannabis and other illicit drug use by young people: a systematic review of longitudinal, general population studies. Lancet (2004) 363:1579–88. doi: 10.1016/S0140-6736(04)16200-4
21. Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet (2012) 379:55–70. doi: 10.1016/S0140-6736(11)61138-0
22. Australian Institute of Health and Welfare. National Drug Strategy Household Survey 2016: Detailed Findings. Canberra, ACT: AIHW (2017).
23. Haines-Saah RJ, Johnson JL, Repta R, Ostry A, Young ML, Shoveller J, et al. The privileged normalization of marijuana use–an analysis of Canadian newspaper reporting, 1997–2007. Crit Public Health (2014) 24:47–61. doi: 10.1080/09581596.2013.771812
24. Hall W. The adverse health effects of cannabis use: what are they, and what are their implications for policy? Int J Drug Policy (2009) 20:458–66. doi: 10.1016/j.drugpo.2009.02.013
25. Stinson FS, Ruan WJ, Pickering R, Grant BF. Cannabis use disorders in the USA: prevalence, correlates and co-morbidity. Psychol Med. (2006) 36:1447–60. doi: 10.1017/S0033291706008361
26. Herring RD. Substance use among Native American Indian youth: a selected review of causality. J Counsel Dev. (1994) 72:578–84. doi: 10.1002/j.1556-6676.1994.tb01685.x
27. Walls M, Hartshorn KJS, Whitbeck LB. North American indigenous adolescent substance use. Addict Behav. (2013) 38:2103–9. doi: 10.1016/j.addbeh.2013.01.004
28. Lemstra M, Rogers M, Moraros J, Caldbick S. Prevalence and risk indicators of alcohol abuse and marijuana use among on-reserve First Nations youth. Paediatr Child Health (2013) 18:10–4. doi: 10.1093/pch/18.1.10
29. Vos T, Barker B, Begg S, Stanley L, Lopez AD. Burden of disease and injury in Aboriginal and Torres Strait Islander Peoples: the Indigenous health gap. Int J Epidemiol. (2009) 38:470–7. doi: 10.1093/ije/dyn240
30. Fleming J, Watson C, McDonald D, Alexander K. Drug use patterns in Northern territory aboriginal communities 1986–1987. Drug Alcohol Rev. (1991) 10:367–80. doi: 10.1080/09595239100185421
31. Clough AR, Guyula T, Yunupingu M, Burns CB. Diversity of substance use in eastern Arnhem Land (Australia): patterns and recent changes. Drug Alcohol Rev. (2002) 21:349–56. doi: 10.1080/0959523021000023207
32. Clough AR, Lee KSK, Cairney S, Maruff P, O'Reilly B, D'Abbs P, et al. Changes in cannabis use and its consequences over 3 years in a remote indigenous population in northern Australia. Addiction (2006) 101:696–705. doi: 10.1111/j.1360-0443.2006.01393.x
33. Lee KS, Conigrave KM, Clough AR, Dobbins TA, Jaragba MJ, Patton GC. Five-year longitudinal study of cannabis users in three remote Aboriginal communities in Arnhem Land, Northern Territory, Australia. Drug Alcohol Rev. (2009) 28:623–30. doi: 10.1111/j.1465-3362.2009.00067.x
34. Clough AR, D'Abbs P, Cairney S, Gray D, Maruff P, Parker R, et al. Emerging patterns of cannabis and other substance use in Aboriginal communities in Arnhem Land, Northern Territory: a study of two communities. Drug Alcohol Rev. (2004) 23:381–90. doi: 10.1080/09595230412331324509
35. Select Committee on Substance Abuse in the Community. Substance Abuse in Remote Communities: Confronting the Confusion and Disconnection. Volume Two: Transcripts of Hearings and Official Briefings, 29 November 2005–26 July 2007, Legislative Assembly of the Northern Territory, Darwin (2007). Available online at: https://parliament.nt.gov.au/__data/assets/pdf_file/0006/367899/VOL-2-FOR-SEPT-07-REPORT-final.pdf
36. Robertson-Mcmahon J, Dowie R. Cannabis: a cloud over our community. Of Substance (2008) 6:28–9. Available online at: https://researchonline.jcu.edu.au/17689/
37. Hunter EM, Gynther BD, Anderson CJ, Onnis L–aL, Nelson JR, Hall W, et al. Psychosis in indigenous populations of Cape York and the Torres Strait. Med J Aust. (2012) 196:133–5. doi: 10.5694/mja11.10118
38. Lee KSK, Conigrave KM, Patton GC, Clough AR. Cannabis use in remote Indigenous communities in Australia: endemic yet neglected. Med J Aust. (2009) 190:228–9.
39. Wild R, Anderson P. Little Children are Sacred”: Report of the Northern Territory Board of Inquiry into the Protection of Aboriginal Children from Sexual Abuse. Darwin, NT: Northern Territory Government (2007). Available online at: http://www.inquirysaac.nt.gov.au/pdf/bipacsa_final_report.pdf
40. Martin G, Copeland J, Gates P, Gilmour S. The Severity of Dependence Scale (SDS) in an adolescent population of cannabis users: reliability, validity and diagnostic cut-off. Drug Alcohol Depend. (2006) 83:90–3. doi: 10.1016/j.drugalcdep.2005.10.014
41. Census Data: QuickStats [database on the Internet]. ABS. (2011) Available online at: http://www.abs.gov.au/websitedbs/censushome.nsf/home/quickstats (Accessed July 16, 2017).
42. Margolis SA, Ypinazar VA, Muller R, Clough A. Increasing alcohol restrictions and rates of serious injury in four remote Australian Indigenous communities. Med J Aust. (2011) 194:503–6. Available online at: https://www.mja.com.au/system/files/issues/194_10_160511/mar11485_fm.pdf
43. Clough AR, Cairney S, D'Abbs P, Parker R, Maruff P, Gray D, et al. Measuring exposure to cannabis use and other substance use in remote aboriginal populations in Northern Australia: evaluation of a 'community epidemiology' approach using proxy respondents. Addict Res Theory (2004) 12:261–74. doi: 10.1080/16066350410001667143
44. Chen K, Kandel DB. Predictors of cessation of marijuana use: an event history analysis. Drug Alcohol Depend. (1998) 50:109–21. doi: 10.1016/S0376-8716(98)00021-0
45. Copersino ML, Boyd SJ, Tashkin DP, Huestis MA, Heishman SJ, Dermand JC, et al. Quitting among non-treatment-seeking marijuana users: reasons and changes in other substance use. Am J Addict. (2006) 15:297–302. doi: 10.1080/10550490600754341
46. Boyd SJ, Tashkin DP, Huestis MA, Heishman SJ, Dermand JC, Simmons MS, et al. Strategies for quitting among non-treatment-seeking marijuana smokers. Am J Addict. (2005) 14:35–42. doi: 10.1080/10550490590899835
47. Graham VE, Campbell S, West C, Clough AR. Substance misuse intervention research in remote Indigenous Australian communities since the NHMRC ‘Roadmap'. Aust N Z J Public Health (2017) 41:424–31. doi: 10.1111/1753-6405.12691
48. Honorato B, Caltabiano N, Clough AR. From trauma to incarceration: exploring the trajectory in a qualitative study in male prison inmates from north Queensland, Australia. Health Just. (2016) 4:3. doi: 10.1186/s40352-016-0034-x
49. Leske S, Harris MG, Charlson FJ, Ferrari AJ, Baxter AJ, Logan JM, et al. Systematic review of interventions for Indigenous adults with mental and substance use disorders in Australia, Canada, New Zealand and the United States. Aust N Z J Psychiatry (2016) 50:1040–54. doi: 10.1177/0004867416662150
50. Bandiera FC, Atem F, Ma P, Businelle MS, Kendzor DE. Post-quit stress mediates the relation between social support and smoking cessation among socioeconomically disadvantaged adults. Drug Alcohol Depend. (2016) 163:71–6. doi: 10.1016/j.drugalcdep.2016.03.023
51. Stockings E, Hall WD, Lynskey M, Morley KI, Reavley N, Strang J, et al. Prevention, early intervention, harm reduction, and treatment of substance use in young people. Lancet Psychiatry (2016) 3:280–96. doi: 10.1016/S2215-0366(16)00002-X
52. Tsai J, Little M, Sussman S. Self-Initiated Cannabis Use Cessation in Adolescents and Emerging Adults. Handbook of Cannabis and Related Pathologies. London: Elsevier (2017). p. 1036–46. doi: 10.1016/B978-0-12-800756-3.00125-3
53. Bohanna I, Clough AR. Cannabis use in cape york indigenous communities: high prevalence, mental health impacts and the desire to quit. Drug Alcohol Rev. (2012) 31:580–4. doi: 10.1111/j.1465-3362.2011.00405.x
54. Clough AR. Associations between tobacco and cannabis use in remote indigenous populations in Northern Australia. Addiction (2005) 100:346–53. doi: 10.1111/j.1360-0443.2005.01040.x
55. Daniel JZ, Hickman M, Macleod J, Wiles N, Lingford-Hughes A, Farrell M, et al. Is socioeconomic status in early life associated with drug use? A systematic review of the evidence. Drug Alcohol Rev. (2009) 28:142–53. doi: 10.1111/j.1465-3362.2008.00042.x
56. Kunitz SJ. Risk factors for polydrug use in a Native American population. Subst Use Misuse (2008) 43:331–9. doi: 10.1080/10826080701202783
57. Gray D, Saggers S. The evidence base for responding to substance misuse in indigenous minority populations. In: Preventing Harmful Substance Use: The Evidence Base for Policy and Practice. Hoboken, NJ: John Wiley & Sons Ltd (2009). pp. 381–393.
58. Dudgeon P, Wright M, Paradies Y, Garvey D, Walker I. The Social, Cultural and Historical Context of Aboriginal and Torres Strait Islander Australians. In: Working Together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice Canberra: Australian Government Department of the Prime Minister and Cabinet (2010). p. 25–42.
Keywords: cannabis (marijuana), indigenous, remote communities, substance use prevalence, cannabis abstinence, cannabis cessation
Citation: Graham VE and Clough AR (2018) Cannabis Use Among Remote Indigenous Australians: Opportunities to Support Change Identified in Two Waves of Sampling. Front. Public Health 6:310. doi: 10.3389/fpubh.2018.00310
Received: 29 March 2018; Accepted: 09 October 2018;
Published: 02 November 2018.
Edited by:
James Steven Ward, South Australian Health and Medical Research Institute, AustraliaReviewed by:
Diana Grigsby, University of Illinois at Urbana-Champaign, United StatesPradeep Nair, Central University of Himachal Pradesh, India
Copyright © 2018 Graham and Clough. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Veronica E. Graham, dmVyb25pY2EuZ3JhaGFtQG15LmpjdS5lZHUuYXU=
 Veronica E. Graham
Veronica E. Graham Alan R. Clough2
Alan R. Clough2