- 1Institute of Psychology, Alps-Adria University, Klagenfurt am Woerthersee, Austria
- 2Department of Social Policy and Intervention, University of Oxford, Oxford, United Kingdom
- 3MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, Glasgow, United Kingdom
- 4Department of Psychology, University of Bremen, Bremen, Germany
- 5School of Psychology, Bangor University, Wales, United Kingdom
- 6Department of Psychology, Babeş-Bolyai University, Cluj-Napoca, Romania
Background: Hunger can influence healthy development of children and has been shown to be associated with other determinants of child health, such as violence within the family and maternal (mental) health problems. Whilst the majority of research has been conducted in high-income countries with vulnerable populations, less is known about the circumstances in low-and-middle-income countries. This study explored the experience of hunger in vulnerable families in three Southeastern European countries, and simultaneously examined relationships with four sets of risk factors—lack of financial, mental, familial, and social resources.
Methods: Families (N = 140) were recruited for a parenting intervention targeting child behavioral problems. Baseline data was collected on hunger, socioeconomic characteristics, mental health and wellbeing, family violence (i.e., child maltreatment and intimate partner violence), and social and emotional support. Univariate and multivariable risk factors of hunger were examined cross-sectionally with regression models.
Results: Overall, 31% of families experienced at least one form of hunger in the last month. Worse family functioning, current intimate partner violence, and more instances of child neglect showed univariate associations with family hunger. In hierarchical analysis, five risk factors remained significantly associated with the experience of hunger: lower adult educational, literacy level, emotional support, more children in the household and higher scores on parental depression, anxiety, and stress.
Conclusions: Hunger in Southeastern European families, among families with children showing elevated behavioral problems, was associated with more family violence, but specifically poorer mental health and less emotional support above and beyond socio-structural strains. Adapting parenting interventions to support the primary caregiver in getting more access to emotional support may potentially also change hunger and its association with health and violence. However, this hypothetical pathway of change needs explicit testing.
Introduction
Undernutrition and hunger are affecting children around the world (1). Poor nutrition has detrimental effects on children's health, as well as on their physical, mental and social development (2–4). Consequences of undernutrition can include weakened immunity, susceptibility to long-term developmental delays or deficits, and increased risk of death, as well as prolonged negative effects on learning and economic performance (5–7). Undernutrition can result from illness, food shortage, inappropriate childcare or feeding practices, or a combination of these factors (5). Different causes of hunger may therefore be associated with different risk profiles. Having limited resources to purchase a variety of foods is often referred to as “food insecurity,” that is inadequate physical, social and economic access to nutritious and safe food (8).
Food insecurity and its potential consequence of experiencing hunger are two among many social and environmental determinants of child health. A range of these social and environmental factors have been found to cluster together, potentially creating chaotic living conditions for families (9) and reflecting a broader context of family adversity and trauma that can reinforce each other across generations (10, 11).
Food insecurity and the experience of hunger are closely linked to the socioeconomic status of the household (12). Food insecurity occurs alongside other forms of social inequality (13) and has therefore been interpreted as a proxy for poverty and economic hardship. Bocquire et al. (14) found relationships between food insecurity and adult age (younger), adult gender (women), family structure (single parents with children), and poorer material and housing conditions (non-home owners and lower income). Associations with indicators of family financial resources have further been reported in studies from Canada, England, Finland, France and the USA (15–19).
Shortage of food supply, and poverty in general, have been directly linked to poorer health of parents and children. Physical health problems occurring in residents of households with food insecurity include obesity/overweight due to overconsumption of low-cost, high-energy foods (20), hypertension and diabetes (21). Mental health problems include depression (13, 22, 23) and anxiety or psychological distress (24, 25). Families living with food insecurity also commonly experience feelings of shame, failure, desperation or being unfairly judged by others (25–28). Impacts on mental health, such as depression and wellbeing, limit the managerial capacity of caregivers (e.g., organizing and planning of food provision, motivation to shop and prepare food) (29, 30). This in turn can be overwhelming for parents and further influence the experience of food insecurity (e.g., feeling lack of control over the food environment) as well as impact the parent-child relationship by comprising parent-child attachment (31). Since mental health problems have also been shown to precede food insecurity and heighten its consequences (13, 32), it is unclear if hunger is indeed a causal risk factor for these adverse developmental outcomes for families or if hunger is rather a correlate, or a marker of these outcomes.
The abovementioned detrimental impacts of food insecurity can be particularly persistent if social resources of families are limited. Supportive relationships and social or instrumental support, either from within the family or outside, have been identified as buffers against the experience of adversity in food insecure households (33, 34). If a family member is additionally experiencing depression, s/he may have fewer supportive relationships (35) and an inability to connect with services that can assist with food hardship (29). Single female-headed households are at increased risk of experiencing food insecurity and poverty (12, 13, 30). Simultaneously, this group is also at increased risk of experiencing mental health problems and domestic violence (29).
Negative relationships, particularly in the form of family violence (i.e., child maltreatment and intimate partner violence), have been found more frequently in families residing in food insecure households or those affected by poverty. For instance, Jackson et al. (36) showed that child exposure to violence and/or victimization in the home early in life was almost six times higher in households experiencing persistent food insecurity (across three assessment waves) compared to food secure households. Similarly, plenty of evidence indicates that intimate partner violence (37–39) and hostile parenting (40) are prevalent in food insecure households. These circumstances suggest that familial resources are low. The consequences of victimization can easily impede the caregiver's capacity to meet family food needs since attention is mainly focused on safety and protecting the children (30). Several authors have highlighted the interplay amongst these risk factors, suggesting that food insecurity and family violence are driven by the same social and environmental risk factors (11, 29, 38, 39, 41), all of which can diminish mental health, especially if persistent (25, 42), and lead to more violent family interactions (43, 44).
While studies reporting the prevalence of hunger/food insecurity and family violence have focused on countries across the world, the majority of studies examining the relationships outlined above have mainly been conducted in the US and Europe. The focus has less frequently been on countries, for instance, in Southeastern Europe, many of which are classified as low-and middle-income countries (LMIC) (45). As such they experience higher rates of food insecurity, exposure to economic hardship, mental health issues, low levels of support and violence or victimization that can have far-reaching consequences on the health and development of children. These countries are more strained by economic hardship on a macro-contextual level and therefore offer a good opportunity to examine prevalence of hunger and associated risk profiles. Although these risk factors co-occur with the experience of hunger, most studies currently undertaken have not simultaneously examined relationships between these sets of risk factors but rather focused either on one or two sets only at the same time (such as mental health and family violence). Therefore, the aim of this study was to simultaneously examine associations between four sets of risk factors—lack of financial, mental, familial and social resources—and the experience of hunger in families living in three low-and middle-income Southeastern European countries. The primary goal was to identify those variables that are independently associated with and contribute incrementally to the phenomenon of hunger in LMICs.
Methods
Study Sample and Procedure
Data for the present study came from the pre-assessment of the feasibility phase of the RISE project, a multi-phase project with the overall goal of adapting, optimizing and testing a parenting intervention in three Southeastern European LMIC, using the Multiphase Optimization Strategy (MOST) and dimensions of the RE-AIM framework (46). Data for this first phase were simultaneously collected in North Macedonia, Republic of Moldova and Romania in 2018. The recruitment settings varied by country study site. Recruitment in Moldova was conducted in urban settings in Chisinau through youth-friendly health centers and at a local NGO targeting adults and youth with substance use disorder and HIV/AIDS. In Romania, recruitment was conducted in collaboration with educators in Cluj-Napoca and a community based organization in semi-rural village 80 miles from the city. Lastly, participants in North Macedonia were recruited in urban communities in Skopje at primary schools, kindergartens, family counseling services, and a community organization serving Roma families. Participants were recruited through flyers (e.g., via NGO's, kindergarten, schools); referrals by psychologists, social workers or teachers; social media pages of the local study institutes within each country; radio/TV advertisement; word-of-mouth by other parents and community leaders/ champions; door-to-door approaches; non-governmental and governmental organizations working with children and parents. Once potential study participants were connected to the study personnel, informed about the study and pre-screened for eligibility, an assessment was scheduled to gather consent and determine final eligibility. Participants needed to be aged 18 years or older, the primary caregiver of a child aged between 2 and 9 years, living in the same household as the target child for at least four nights a week and planning to do so during the course of the study, reporting elevated levels of behavior problems in the target child, agreeing to participate in the Parenting for Lifelong Health (PLH) for Young Children programme, and providing informed consent to participate in the study. Parents that either exhibited severe mental health problems or severe learning disabilities, or had been referred to child protection services due to child abuse were not eligible to participate in the study. Data collection took place either at participants' homes, the study institutes or any agreed-on location. Administration of consent forms and questionnaires was done with a Computer-Assisted Self-Interviewing (“CASI”) method with electronic-tablet technology. Trained data assessors read out questions if parents were unable to read, and assisted participants to type responses into the tablet if they were uncomfortable with or unable to use the tablet. In order to increase willingness to report stigmatizing experiences (47), audio-CASI was used, to administer sensitive items on the questionnaires (e.g., regarding child maltreatment/harsh parenting or intimate partner violence). RISE was approved by the human research ethics committee of the University of Klagenfurt and local ethics committees in North Macedonia, Moldova and Romania.
Measurement Tools
All measurement tools that were not already available in the country-specific languages were translated and back-translated for the current project.
Demographic/Socioeconomic Factors
Participants reported on demographic and socioeconomic characteristics about themselves as well as their child. These included parent and child age and gender, parent education and literacy level, or number of children living in the household.
Experience of Hunger
Household hunger was assessed using three items on food shortage and hunger within the family that were based on the “Hunger Scale” (48–50). These items included: (1) “Do you ever run out of money to buy food for your home?”, (2) “Do you ever cut the size of meals or skip any meals because there is not enough food in the house?”, and (3) “Do you or any of your children go to bed hungry because there is not enough food to eat?”. Parents responded with yes or no. If parents confirmed the occurrence of hunger in the household, they were asked if it happened during the past 30 days, and subsequently, if it happened more than 5 times in the past 30 days. In the current study, individual incidences were examined and the overall prevalence was analyzed (i.e., experience of at least one form of hunger in the past 30 days).
Family Violence Factors
To assess harsh parenting, parents reported on 14 items which were based on the ISPCAN Child Abuse Screening Tool-Intervention scale (ICAST-I) (51, 52) and the Child Maltreatment Screener by Slep et al. (53). Four items assessed physical abuse (e.g., “In the past 4 weeks, how often did you discipline your child by slapping, spanking, or hitting with your hand?”), seven items assessed emotional abuse (e.g., “In the past 4 weeks, how often did you shout, yell or scream at your child?”) and three items assessed neglect (e.g., “How often in the past month did your child not get the food or drink that he/she needed even when there was money to pay for it?”). To assess the frequency of each behavior, the response scale ranged from 0 = “Never” to 8 = “8 or more times” in the past month. In this study, data for each of the three harsh parenting types were dichotomized to indicate the prevalence within the past month (i.e., previous harsh parenting or not).
Intimate partner violence was also assessed using questions from several sources. Participants reported on 15 victimizing and 14 perpetrating behaviors adapted from the Brief Screening Instrument for Partner Maltreatment by Heyman et al. (54) and the revised Conflict Tactics Scale (CTS2S) short form and full version (55, 56). Items in the current study referred to abuse within the last month (rather than the past year) and were assessed on a 9-point scale (0 = “Never happened” to 8 = “8 or more times” in the past month), with an additional response for incidents that happened in the past but not within the last month. Overall frequencies of victimization and perpetration (respective sum of items) were used as an indication of the level of severity, with possible ranges in the past month from 0 to 112 and 0 to 104. Due to non-normality, both variables were log transformed. Both measures of family violence were administered with an anonymous self-report response format. Parents who had trouble reading were able to enter their answers through audio-recorded instructions. This is the recommended method for data collection of sensitive problems to reduce underreporting (53, 54, 57).
Well-Being and Mental Health Factors
Parents provided information about their well-being and mental health via two widely used and validated measurement tools (58–60). The WHO-5 Well-Being Scale (61) measures parental psychological well-being on a 5-item scale. Parents indicated the well-being they experienced in the past month—original period was 2 weeks (e.g., “My daily life has been filled with things that interest me”) based on a 6-point Likert scale from 0 = “At no time” to 5 = “All of the time.” In the present study, the percentage score was used ranging from 0 to 100 (i.e., raw sum score multiplied by four) (62). Higher scores indicated better well-being. Internal reliability was acceptable (Cronbach's alpha = 0.77). Mental health was assessed using the Depression, Anxiety and Stress Scale (DASS, 21 items) (63). Participants reported on the frequency of symptoms in the previous week using a modified Likert scale (0 = “Never”, 1 = “Sometimes”, 2 = “Often”, 3 = “Always”; e.g., “I felt that I had nothing to look forward to”). The total DASS score ranged from 0 to 63 with higher scores indicating more psychological distress. Internal reliability was excellent (Cronbach's alpha = 0.91).
Social and Family Support Factors
The next set of parent-reported questions related to family functioning and emotional support. Parent perceived social support was measured using the emotional support subscale of the Medical Outcome Study Social Support Survey (MOS-SSS, eight items) (64). Parents reported how often they receive emotional support (e.g., “Someone you can count on to listen to when you need to talk”) using a 5-point Likert-like scale (1 = “None of the time” to 5 = “All of the time”). Higher mean scores indicated more emotional support. This scale has previously shown excellent test-retest reliability (α = 0.72–0.78) and internal consistency (α = 0.91–0.97) (65, 66), which was also found for the current study sample (α = 0.96). To assess family functioning, the general functioning subscale of the Family Assessment Device short form (FAD, 12 items) was used (67). Responses on each item (ranging from 1 = “Strongly agree” to 4 = “Strongly disagree”) were averaged after reverse coding where appropriate. Higher mean scores indicated more problems in family functioning. Previous studies have shown that the FAD is a valid instrument for assessing family outcomes in clinical trials with good internal consistency (68, 69). Similarly, in the current sample the internal consistency was good (α = 0.81).
Data Analysis
Variables were inspected for non-normality and outliers. Where necessary, variables were either transformed or non-parametric tests were used. To ensure similarity of distributions across countries for merging the samples, differences were examined across the three countries, using ANOVAs for continuous variables and chi-square tests for categorical variables. To examine univariate relationships between the experience of hunger and the four sets of determinants (i.e., socioeconomic/demographic, family violence, mental health, social and family support), Independent sample t-tests, Mann Whitney tests and chi-square tests were performed depending on the scale of the measure. Significant variables from within each of the four sets of determinants were selected and then combined into a hierarchical logistic regression model to evaluate the change in variance explained. Variables were entered in the following order: Step 1—socioeconomic/demographic variables, Step 2—family violence related variables, Step 3—mental health-related variables, and Step 4—social and family support variables. Study country was entered as two dummy variables in Step 1 reflecting Moldova vs. Macedonia/Romania (dummy 1) and Romania vs. Macedonia/ Moldova (dummy 2), selecting Macedonia as reference category. Due to the high correlation between both intimate partner violence variables (rho = 0.75), models were run separately including victimization and perpetration, respectively, in Step 2. Results were the same and thus, only results with victimization are presented. Statistical significance was set at p < 0.05.
Results
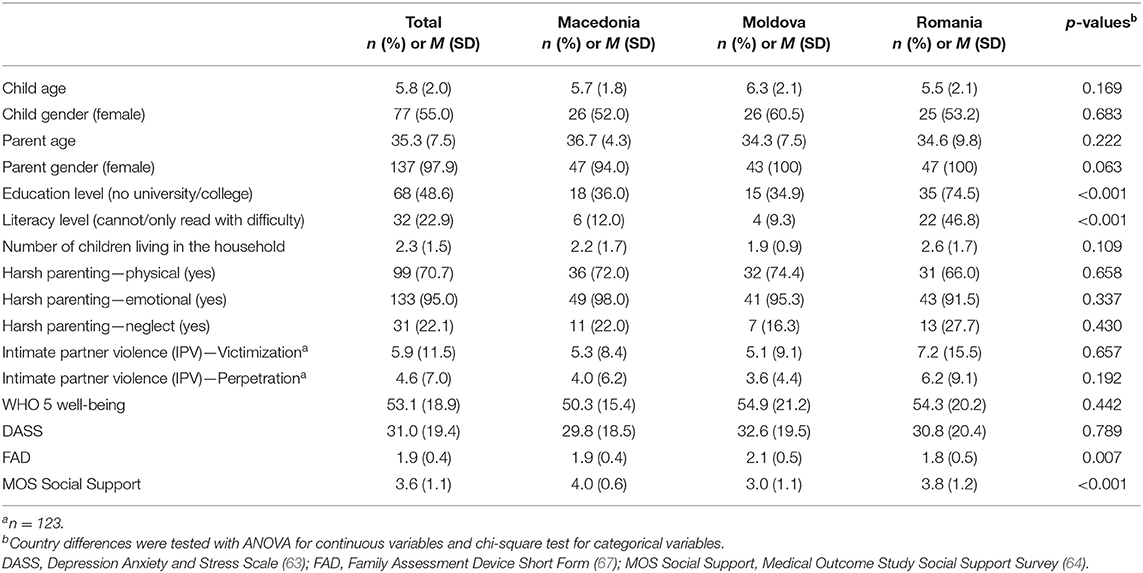
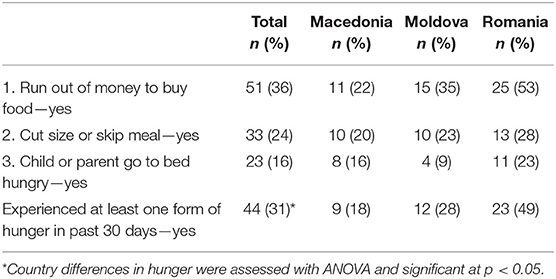
Of the 253 parents who were pre-screened, 162 were eligible (39 were ineligible and 52 could not be scheduled for an assessment). A further 22 parents were excluded at the final eligibility testing, leaving 140 eligible parents who consented and participated in the pre-assessment. Of those, 123 (87.9%) were currently in a relationship. Participant characteristics are presented in Table 1, also separated by country. Few country differences existed. The Romanian sample included a larger number of parents without a university or college degree and in line with this, a higher number of illiterate parents compared to the other two countries (both p < 0.001). Moldova showed more family dysfunction than Romania and less social support compared to the other two countries (both p < 0.05). Table 2 shows that 31% of the total sample experienced at least one form of hunger in the past 30 days. The proportion was highest in Romania (49%). In total, 19% experienced at least one form of hunger more than 5 times in the past 30 days and 6% experienced all three forms of hunger in the past 30 days. Table 3 shows the univariate relationships between the experience of hunger (i.e., at least one form of hunger in the past month) and all risk factors. Those that were significant were carried forward into the final hierarchical logistic regression model (see Table 4). Each step added significantly to the variance in the experience of hunger with the full models explaining 74% of the total variance. Three risk factors related to the socioeconomic/demographic, one to the mental health and one to the social and family support set, respectively. The odds of experiencing hunger were higher if the parent (i) had no university/college degree (OR = 13.79), (ii) could not, or could only read with difficulty (OR = 9.33), (iii) had more children living in their household (OR = 1.79), (iv) was more psychologically distressed (OR = 1.05), or (v) had less emotional support (OR = 0.22).
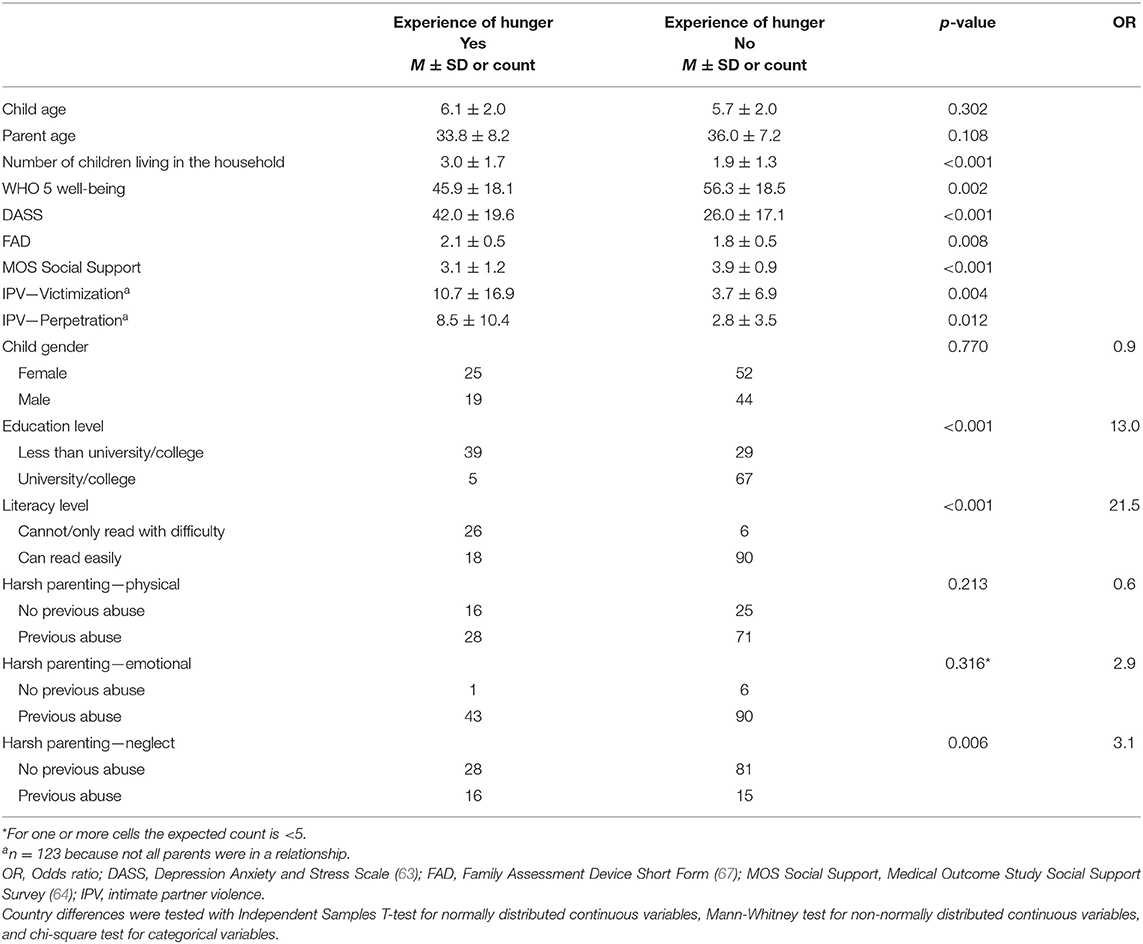
Table 3. Univariate relationships between the experience of hunger (i.e., at least one form of hunger in the past month) and risk factors (N = 140).
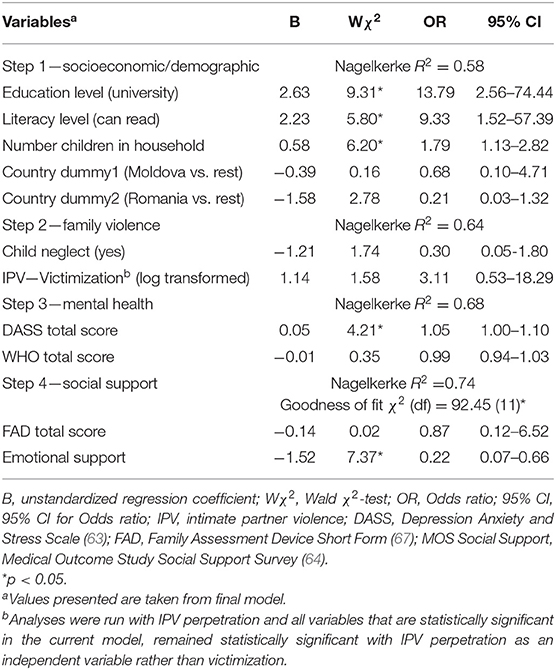
Table 4. Hierarchical logistic regression for the experience of hunger (i.e., at least one form of hunger in the past month) and four sets of risk factors.
Discussion
The aim of this study was to explore the reported levels of hunger in families with elevated levels of child behavioral problems living in three Southeastern European countries as well as to examine associations between four sets of risk factors and the experience of hunger. Risk factors were divided into socioeconomic/demographic, family violence, mental health-related, and social or family support factors. One third of the sample experienced at least one form of hunger in the past month, with differences apparent between countries. The majority of the risk factors explored showed a univariate association with the experience of hunger and together explained more than 70% of the variance. In the final model, five risk factors remained significant, particularly highlighting the role of socioeconomic/demographic risks compared to all other sets of risk factors.
Using the Food Insecurity Experience Scale (70) across 28 European Union countries (71), a prevalence of 18% of households experiencing a moderate (4%) to severe (14%) inability to access food has been reported. The prevalence in the European Commonwealth of Independent States identifying former parts of the Soviet Union (including Moldova) was similar with 17% of households reporting moderate (2%) to severe (15%) inability to access food. While the rate seen in the current sample was higher (31%), this is probably related to the difference in the recruitment and thus vulnerability of the selected sample, but also due to the measurement tools used (e.g., food insecurity measure vs. experience of hunger measure). Due to the lower income and higher poverty rates in comparison to even the newer European member states, food insecurity has been reported to be a concern for a large proportion of the population in Romania (72) and Moldova (73, 74), and likely also in North Macedonia since it is also a LMIC.
Three socioeconomic/demographic factors were associated with the experience of hunger. This is in line with previous studies. Smith et al. (33) found that three of the five characteristics that were associated with the largest increase in the likelihood of experiencing food insecurity around the world included low education levels, low household income, and being unemployed. The other two included less social capital and weak social networks which also align with findings of the current study and are discussed below. Economic/financial resources, or hardship on the other end of the continuum, are well known buffers, or risk factors. Extended exposure to poverty, especially during early childhood, has adverse impacts, with hunger being one of them (75, 76). Families living in circumstances of socioeconomic disadvantage are not only more likely to reside in food insecure households but also experience other, overlapping family adversities, such as family violence (29), mental health difficulties (25, 77), substance abuse (78, 79), and reported child behavioral problems (13).
Although intimate partner violence (both victimization and perpetration) and child neglect, but not physical or emotional abuse, showed a univariate association with the experience of hunger, none of the family violence factors remained significant once entered into the hierarchical regression model. Other studies have found consistent relationships, for instance, between food insecurity and domestic violence (OR = 2.36, 95% CI: 1.18–4.73) (13) or children witnessing physical violence in the home (moderate-to-severe food insecurity, OR = 2.66, 95% CI: 2.26–3.09) (41). Notably, many of the previous studies highlighting relationships between food insecurity and family violence did not simultaneously examine the range of risk factors that were explored in the current study. This may be one reason why the strength of association with family violence factors was diluted, once other risk factors were taken into consideration. This does not indicate that domestic violence is not a relevant risk factor, but suggests that the relationship between domestic violence and food insecurity may be mediated by other risk factors.
In the current study, a higher score on the Depression, Anxiety and Stress scale was associated with slightly higher odds of experiencing hunger (OR = 1.05, 95% CI 1.00–1.10) whilst a higher well-being score only showed a trend in lower odds of experiencing hunger (OR = 0.99, 95% CI 0.94–1.03). This is in line with a range of previous studies presenting a close link between food insecurity and poorer mental health and specific psychological stressors. According to Jones et al. (80), these associations are found across the globe, independent of socioeconomic status. Also drawing on the 2014 Gallup World Poll (81), Frongillo et al. (82) indicated that food insecurity was strongly negatively associated with subjective well-being as well when measured in a large global sample (above 120,000 participants from 138 countries). We only found a small association which was no longer significant when other sets of risk factors were simultaneously included. At present, a bidirectional relationship is accepted in that food insecurity can both reflect but also engender cascading mental health challenges (41).
Finally, social and family support factors were examined. Interestingly, in the current study no association was seen between general family functioning (“In times of crisis we can turn to each other for support” or “We are able to make decisions about how to solve problems”) and the experience of hunger, whilst a significant association was found for emotional support. Although the latter measure includes questions such as “Someone to give you good advice about a crisis” or “Someone to confide in or talk to about yourself or your problems” which could also refer to family members, this measure of support potentially captures support from the wider social network. Associations between food insecurity and weaker social networks (i.e., dissatisfied with ability to make friends) or less social capital (i.e., cannot count on friends and family in times of need) were found using data including 134 countries (33). Tsai et al. (34), whose measure assessed emotional or instrument support provided by a family member (i.e., intimate partner, mother or father), found that instrumental social support functioned as a buffer against adverse impacts of food insecurity. These findings suggest that the effect might be related to the type of support received, rather than the person or proximity from which support is provided.
Findings of the current study have to be considered in the light of possible limitations. The current sample may not be representative of the average North Macedonian, Moldovan and Romanian parent since participants were selected for a parenting intervention focused on child behavioral problems and were reporting child behavioral problems as a recruitment criterion. In addition to the interplay of risk factors mentioned above, families reporting child behavioral problems may also be more likely to experience all the other family adversities (13). The current sample may therefore have been more likely to report experiencing hunger. Due to the cross-sectional nature of the data no statement could be made about the direction of relationships. The current data were sourced from the feasibility pilot phase of RISE (46). Consequently, analyses were exploratory, the sample size was small, limiting the ability to conduct sub-sample analyses and further group comparisons, and the assessment of the experience of hunger was not the main focus of the study with only three items included for measurement. However, other studies, such as Bocquier et al. (14) used a single-item to assess food insecurity (“Which of the following statements best described the food currently consumed in respondents' household?”), and our items are very similar to three of the seven used by Wehler et al. (30) from the Community Childhood Hunger Identification Project. Advantages include capturing the perspective of parents in three Southeastern European countries that have not been specifically targeted for this research focus before and the fact that several risk factor sets were assessed simultaneously with concurrent measurement of all variables. Finally, there is potential bias of underreporting relating to self-reported measurement of family violence. In order to minimize social desirability bias or underreporting, audio-CASI (i.e., computer assisted self-interviewing) was used in the present study, allowing participants (even if illiterate) to respond to questions without the assistance of the interviewer. Further, prevalence rates found in the current sample are similar to other studies of intimate partner violence in the past year [e.g., 10.1% (83) or 18.3% (84) compared to 11.5% in this sample].
Findings from our study indicate that the risk factors related to the experience of hunger in the three Southeastern European countries North Macedonia, Republic of Moldova and Romania are similar to those reported for other countries. Given increasing evidence in the literature that the abovementioned factors are intertwined, examination of this complex interplay by modeling more comprehensive relationships (e.g., through path modeling) seems warranted. Further investigations utilizing tools that are comparable to other studies and including larger and more representative samples will additionally advance our understanding of commonality and representativeness of findings obtained from less frequently studied populations. If comparable, it should be considered whether or not attempts to simultaneously address a range of family adversities (food insecurity, psychological well-being, family violence), for instance through providing intimate partner violence and mental health resources, as has been done via the Women, Infants, Children (WIC) Nutrition Program in the United States (29), are also useful in other countries or are unsuitable due to cultural and systemic differences. Additionally, testing the benefit of pairing parenting interventions with economic strengthening programmes targeted at food insecurity may be particularly useful for LMIC. The current results relating to emotional support are promising because controlling for a number of other types of risk, emotional support appeared to be an important variable in this cross-sectional interplay. Further investigation about change in emotional support following participation in an intervention program and its impact on hunger seem warranted, particularly since group-based programs, such as PLH which is applied in the RISE study, offer the potential to generate social support (85).
Data Availability Statement
The datasets generated for this study will not be made publicly available according to the EU funder approved data management plan. Data from the RISE study will only be made publicly accessible at the end of the study period and after publication of the related study results. Requests to access these datasets should be directed to Professor Heather Foran, aGVhdGhlci5mb3JhbkBhYXUuYXQ=.
Ethics Statement
The studies involving human participants were reviewed and approved by the human research ethics committee of the University of Klagenfurt, the local ethics committees in North Macedonia, Moldova and Romania. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AB, HF, NH, JH, and JL contributed to the conception and design of the study. EJ managed the data, performed the statistical analysis, and wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This project has received funding from the European Union's Horizon 2020 research and innovation program under grant agreement No. 779318. Funding includes financial, material, and personnel support. Time period for funding: 1 January 2018 to 31 December 2021. Contact details: European Commission, DG Research and Innovation, 1049 Bruxelles, Belgium. The funder was not and will not be involved in the design of the study, the collection, analysis and interpretation of data, or the writing of the protocol. Funding was also provided to EJ from the Faculty of Humanities at the Alps-Adria University Klagenfurt to cover the article processing charges.
Conflict of Interest
JL and JH are co-developers of PLH for Young Children, which is licensed under a Creative Commons 4.0 Non-commercial No Derivatives license, and one of the co-founders of the Parenting for Lifelong Health initiative, receive occasional fees for providing training and supervision to facilitators and coaches, and have participated (and are participating) in a number of research studies involving the program, as an investigator, and the University of Oxford, and Bangor University receive research funding for these. JL is also the Executive Director of Clowns Without Borders South Africa, a non-profit institution responsible for the dissemination of the program in Africa and East Africa. Likewise, JH is the director of the Children's Early Intervention Trust, a non-profit institution responsible for the dissemination of the program in Europe and led the evaluation of the program in a pre-post trial in Montenegro and contributed to the trial in the Philippines. NH serves as an international advisory board member for the Triple P program.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This publication was supported by the Faculty of Humanities at the Alps-Adria University Klagenfurt. We thank the RISE research team including all facilitators, data assessors, process monitors, programme coordinators, research coordinators, and principal investigators in North Macedonia, Republic of Moldova, and Romania. We are grateful for the support of the local institutions, organizations, associations, stakeholders, and parents in participant recruitment. Finally, we thank the scientific consultants (Linda Collins), the DSMB (Robert McMahon and Terje Ogden), the DPO (Peter Schartner), and the EU for funding.
References
1. Swinburn BA, Kraak VI, Allender S, Atkins VJ, Baker PI, Bogard JR, et al. The global syndemic of obesity, undernutrition, and climate change: the lancet Commission report. Lancet. (2019) 393:791–846. doi: 10.1016/S0140-6736(18)32822-8
2. Pettoello-Mantovani M, Ehrich J, Sacco M, Ferrara P, Giardino I, Pop TL. Food insecurity and children's rights to adequate nutrition in Europe. J Pediatr. (2018) 198:329–30.e1. doi: 10.1016/j.jpeds.2018.04.042
3. Cook JT, Black M, Chilton M, Cutts D, Ettinger de Cuba S, Heeren TC, et al. Are food insecurity's health impacts underestimated in the U.S. Population? Marginal food security also predicts adverse health outcomes in young U.S. children and mothers. Adv Nutr. (2013) 4:51–61. doi: 10.3945/an.112.003228
4. Ramsey R, Giskes K, Turrell G, Gallegos D. Food insecurity among Australian children: potential determinants, health and developmental consequences. J Child Health Care. (2011) 15:401–16. doi: 10.1177/1367493511423854
5. Dodos J, Altare C, Bechir M, Myatt M, Pedro B, Bellet F, et al. Individual and household risk factors of severe acute malnutrition among under-five children in Mao, Chad: a matched case-control study. Arch Public Health. (2018) 76:35. doi: 10.1186/s13690-018-0281-5
6. World Health Organization. Management of Severe Malnutrition: A Manual for Physicians and Other Senior Health Workers. Geneva: World Health Organization (1999).
7. World Health Organization, UNICEF, WFP, UN System Standing Committee on Nutrition. Community-Based Management of Severe Acute Malnutrition: A Joint Statement by the World Health Organization, the World Food Programme, the United Nations System Standing Committee on Nutrition and the United Nations Children's Fund. (2007). Available online at: https://www.who.int/maternal_child_adolescent/documents/a91065/en/ (accessed March 1, 2020)
8. Committee on World Food Security. Global Strategic Framework for Food Security and Nutrition. Rome: Food and Agricultural Organization (2012).
9. Evans GW, Gonnella C, Marcynyszyn LA, Gentile L, Salpekar N. The role of chaos in poverty and children's socioemotional adjustment. Psychol Sci. (2005) 16:560–5. doi: 10.1111/j.0956-7976.2005.01575.x
10. Chilton M, Knowles M, Bloom SL. The intergenerational circumstances of household food insecurity and adversity. J Hunger Environ Nutr. (2017) 12:269–97. doi: 10.1080/19320248.2016.1146195
11. Chilton M, Knowles M, Rabinowich J, Arnold KT. The relationship between childhood adversity and food insecurity: 'It's like a bird nesting in your head'. Public Health Nutr. (2015) 18:2643–53. doi: 10.1017/S1368980014003036
12. Coleman-Jensen A, Rabbitt M, Gregory C, Singh A. Household Food Security in the United States in 2014. Economic Research Report No. ERR-194. U.S. Department of Agriculture; Economic Research Service (2015).
13. Melchior M, Caspi A, Howard LM, Ambler AP, Bolton H, Mountain N, et al. Mental health context of food insecurity: a representative cohort of families with young children. Pediatrics. (2009) 124:e564–72. doi: 10.1542/peds.2009-0583
14. Bocquier A, Vieux F, Lioret S, Dubuisson C, Caillavet F, Darmon N. Socio-economic characteristics, living conditions and diet quality are associated with food insecurity in France. Public Health Nutr. (2015) 18:2952–61. doi: 10.1017/S1368980014002912
15. Kirkpatrick SI, Tarasuk V. Food insecurity in Canada: considerations for monitoring. Can J Public Health. (2008) 99:324–7. doi: 10.1007/BF03403765
16. Martin-Fernandez J, Grillo F, Parizot I, Caillavet F, Chauvin PJBPH. Prevalence and socioeconomic and geographical inequalities of household food insecurity in the Paris region, France, 2010. BMC Public Health. (2013) 13:486. doi: 10.1186/1471-2458-13-486
17. Rose D. Economic determinants and dietary consequences of food insecurity in the United States. J Nutr. (1999) 129(2S Suppl):517s−20s. doi: 10.1093/jn/129.2.517S
18. Sarlio-Lahteenkorva S, Lahelma E. Food insecurity is associated with past and present economic disadvantage and body mass index. J Nutr. (2001) 131:2880–4. doi: 10.1093/jn/131.11.2880
19. Tingay RS, Tan CJ, Tan NC, Tang S, Teoh PF, Wong R, et al. Food insecurity and low income in an English inner city. J Public Health Med. (2003) 25:156–9. doi: 10.1093/pubmed/fdg032
20. Pan L, Sherry B, Njai R, Blanck HM. Food insecurity is associated with obesity among US adults in 12 states. J Acad Nutr Dietetics. (2012) 112:1403–9. doi: 10.1016/j.jand.2012.06.011
21. Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. (2010) 140:304–10. doi: 10.3945/jn.109.112573
22. Weigel MM, Armijos RX, Racines M, Cevallos W, Castro NP. Association of household food insecurity with the mental and physical health of low-income urban ecuadorian women with children. J Environ Public Health. (2016) 2016:5256084. doi: 10.1155/2016/5256084
23. Whitaker RC, Phillips SM, Orzol SM. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. (2006) 118:e859–68. doi: 10.1542/peds.2006-0239
24. Carter KN, Kruse K, Blakely T, Collings S. The association of food security with psychological distress in New Zealand and any gender differences. Social Sci Med 1982. (2011) 72:1463–71. doi: 10.1016/j.socscimed.2011.03.009
25. Knowles M, Rabinowich J, Ettinger de Cuba S, Cutts DB, Chilton M. “Do you wanna breathe or eat?”: Parent perspectives on child health consequences of food insecurity, trade-offs, and toxic stress. Matern Child Health J. (2016) 20:25–32. doi: 10.1007/s10995-015-1797-8
26. Bernal J, Frongillo EA, Jaffe K. Food insecurity of children and shame of others knowing they are without food. J Hunger Environ Nutr. (2016) 11:180–94. doi: 10.1080/19320248.2016.1157543
27. Hamelin AM, Beaudry M, Habicht JP. Characterization of household food insecurity in Quebec: food and feelings. Social Sci Med 1982. (2002) 54:119–32. doi: 10.1016/S0277-9536(01)00013-2
28. Williams PL, MacAulay RB, Anderson BJ, Barro K, Gillis DE, Johnson CP, et al. “I would have never thought that i would be in such a predicament”: voices from women experiencing food insecurity in Nova Scotia, Canada. J Hunger Environ Nutr. (2012) 7:253–70. doi: 10.1080/19320248.2012.704740
29. Hernandez DC, Marshall A, Mineo C. Maternal depression mediates the association between intimate partner violence and food insecurity. J Women's Health 2002. (2014) 23:29–37. doi: 10.1089/jwh.2012.4224
30. Wehler C, Weinreb LF, Huntington N, Scott R, Hosmer D, Fletcher K, et al. Risk and protective factors for adult and child hunger among low-income housed and homeless female-headed families. Am J Public Health. (2004) 94:109–15. doi: 10.2105/AJPH.94.1.109
31. Zaslow M, Bronte-Tinkew J, Capps R, Horowitz A, Moore KA, Weinstein D. Food security during infancy: implications for attachment and mental proficiency in toddlerhood. Matern Child Health J. (2009) 13:66–80. doi: 10.1007/s10995-008-0329-1
32. Pryor L, Lioret S, van der Waerden J, Fombonne É, Falissard B, Melchior M. Food insecurity and mental health problems among a community sample of young adults. Social Psychiatr Psychiatr Epidemiol. (2016) 51:1073–81. doi: 10.1007/s00127-016-1249-9
33. Smith MD, Rabbitt MP, Coleman-Jensen A. Who are the world's food insecure? New evidence from the Food and Agriculture Organization's Food Insecurity Experience Scale. World Dev. (2017) 93:402–12. doi: 10.1016/j.worlddev.2017.01.006
34. Tsai AC, Tomlinson M, Comulada WS, Rotheram-Borus MJ. Food insufficiency, depression, and the modifying role of social support: evidence from a population-based, prospective cohort of pregnant women in peri-urban South Africa. Social Sci Med 1982. (2016) 151:69–77. doi: 10.1016/j.socscimed.2015.12.042
35. Mitchell RE, Hodson CA. Coping with domestic violence: social support and psychological health among battered women. Am J Comm Psychol. (1983) 11:629–54. doi: 10.1007/BF00896600
36. Jackson DB, Lynch KR, Helton JJ, Vaughn MG. Food insecurity and violence in the home: investigating exposure to violence and victimization among preschool-aged children. Health Educ Behav. (2018) 45:756–63. doi: 10.1177/1090198118760683
37. Breiding MJ, Basile KC, Klevens J, Smith SG. Economic insecurity and intimate partner and sexual violence victimization. Am J Prev Med. (2017) 53:457–64. doi: 10.1016/j.amepre.2017.03.021
38. Chilton M, Rabinowich J, Woolf N. Very low food security in the USA is linked with exposure to violence. Public Health Nutr. (2014) 17:73–82. doi: 10.1017/S1368980013000281
39. Sun J, Knowles M, Patel F, Frank DA, Heeren TC, Chilton M. Childhood adversity and adult reports of food insecurity among households with children. Am J Prev Med. (2016) 50:561–72. doi: 10.1016/j.amepre.2015.09.024
40. Parke RD, Coltrane S, Duffy S, Buriel R, Dennis J, Powers J, et al. Economic stress, parenting, and child adjustment in Mexican American and European American families. Child Dev. (2004) 75:1632–56. doi: 10.1111/j.1467-8624.2004.00807.x
41. Jackson DB, Johnson KR, Vaughn MG. Household food insufficiency and children witnessing physical violence in the home: do family mental illness and substance misuse moderate the association? Matern Child Health J. (2019) 23:961–70. doi: 10.1007/s10995-018-02725-w
42. Heflin CM, Siefert K, Williams DR. Food insufficiency and women's mental health: findings from a 3-year panel of welfare recipients. Social Sci Med 1982. (2005) 61:1971–82. doi: 10.1016/j.socscimed.2005.04.014
43. Jackson DB, Vaughn MG. Household food insecurity during childhood and adolescent misconduct. Prev Med. (2017) 96:113–7. doi: 10.1016/j.ypmed.2016.12.042
44. Nair P, Schuler ME, Black MM, Kettinger L, Harrington D. Cumulative environmental risk in substance abusing women: early intervention, parenting stress, child abuse potential and child development. Child Abuse Neglect. (2003) 27:997–1017. doi: 10.1016/S0145-2134(03)00169-8
45. The World Bank Group. World Bank Country and Lending Groups. (2019). Available online at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed March 1, 2020)
46. Frantz I, Foran HM, Lachman JM, Jansen E, Hutchings J, Baban A, et al. Prevention of child mental health problems in Southeastern Europe: a multicentre sequential study to adapt, optimise and test the parenting programme 'Parenting for Lifelong Health for Young Children', protocol for stage 1, the feasibility study. BMJ Open. (2019) 9:e026684. doi: 10.1136/bmjopen-2018-026684
47. Phillips AE, Gomez GB, Boily MC, Garnett GP. A systematic review and meta-analysis of quantitative interviewing tools to investigate self-reported HIV and STI associated behaviours in low- and middle-income countries. Int J Epidemiol. (2010) 39:1541–55. doi: 10.1093/ije/dyq114
48. Labadarios D, Maunder E, Steyn N, MacIntyre U, Swart R, Gericke G, et al. National food consumption survey in children aged 1-9 years: South Africa (1999). For Nutr. (2003) 56:106–9.
49. Labadarios D, Steyn NP, Maunder E, MacIntryre U, Gericke G, Swart R, et al. The National Food Consumption Survey (NFCS): South Africa, 1999. Public Health Nutr. (2005) 8:533–43. doi: 10.1079/PHN2005816
50. Swindale A, Bilinsky P. Development of a universally applicable household food insecurity measurement tool: process, current status, and outstanding issues. J Nutr. (2006) 136:1449s−52s. doi: 10.1093/jn/136.5.1449S
51. Runyan DK, Dunne MP, Zolotor AJ, Madrid B, Jain D, Gerbaka B, et al. The development and piloting of the ISPCAN Child Abuse Screening Tool-Parent version (ICAST-P). Child Abuse Neglect. (2009) 33:826–32. doi: 10.1016/j.chiabu.2009.09.006
52. Runyan DK, Dunne MP, Zolotor AJ. Introduction to the development of the ISPCAN child abuse screening tools. Child Abuse Neglect. (2009) 33:842–5. doi: 10.1016/j.chiabu.2009.08.003
53. Slep AMS, Heyman RE, Snarr JD, Foran HM. Practical tools for assessing child maltreatment in clinical practice and public health settings. In: Foran HM, Beach S, Slep AMS, Heyman RE, Wamboldt M, editors. Family Problems and Violence: Reliable Assessment and the ICD-11. New York, NY: Springer (2013). pp. 159–84.
54. Heyman RE, Slep AMS, Snarr JD, Foran HM. Practical tools for assessing partner maltreatment in clinical practice and public health settings. In: Foran HM, Beach SRH, Slep AMS, Heyman RE, Wamboldt MZ, editors. Family Problems and Family Violence: Reliable Assessment and the ICD-11. New York, NY: Springer (2013). pp. 43–70.
55. Straus MA, Douglas EM. A short form of the revised conflict tactics scales, and typologies for severity and mutuality. Violence Victims. (2004) 19:507–20. doi: 10.1891/vivi.19.5.507.63686
56. Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2) development and preliminary psychometric data. J Fam Issues. (1996) 17:283–316. doi: 10.1177/019251396017003001
57. Meinck F, Steinert J, Sethi D, Gilbert R, Bellis M, Alink L, et al. Measuring and Monitoring National Prevalence of Child Maltreatment: A Practical Handbook. Copenhagen: World Health Organization Regional Office for Europe (2016).
58. Topp CW, Ostergaard SD, Sondergaard S, Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosomatics. (2015) 84:167–76. doi: 10.1159/000376585
59. Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. (2005) 44:227–39. doi: 10.1348/014466505X29657
60. Ng F, Trauer T, Dodd S, Callaly T, Campbell S, Berk M. The validity of the 21-item version of the Depression Anxiety Stress Scales as a routine clinical outcome measure. Acta Neuropsychiatr. (2007) 19:304–10. doi: 10.1111/j.1601-5215.2007.00217.x
61. Staehr JK. The use of well-being measures in primary health care-the DepCare project. In: World Health Organization - Regional Office for Europe, editor. Well-Being Measures in Primary Health Care-the DepCare Project. Geneva: World Health Organization (1998).
62. World Health Organization. Well-Being Measures in Primary Health Care - the DepCare Project. Copenhagen: WHO Regional Office for Europe (1998).
63. Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. Sydney: Psychology Foundation of Australia (1995).
64. Sherbourne CD, Stewart AL. The MOS social support survey. Social Sci Med. (1991) 32:705–14. doi: 10.1016/0277-9536(91)90150-B
65. Giangrasso B, Casale S. Psychometric properties of the Medical Outcome Study Social Support Survey with a general population sample of undergraduate students. Social Indic Res. (2014) 116:185–97. doi: 10.1007/s11205-013-0277-z
66. Moser A, Stuck AE, Silliman RA, Ganz PA, Clough-Gorr KM. The eight-item modified Medical Outcomes Study Social Support Survey: psychometric evaluation showed excellent performance. J Clin Epidemiol. (2012) 65:1107–16. doi: 10.1016/j.jclinepi.2012.04.007
67. Epstein NB, Baldwin LM, Bishop DS. The McMaster family assessment device. J Marit Fam Ther. (1983) 9:171–80. doi: 10.1111/j.1752-0606.1983.tb01497.x
68. Boterhoven de Haan KL, Hafekost J, Lawrence D, Sawyer MG, Zubrick SR. Reliability and validity of a short version of the general functioning subscale of the McMaster Family Assessment Device. Fam Process. (2015) 54:116–23. doi: 10.1111/famp.12113
69. Byles J, Byrne C, Boyle MH, Offord DR. Ontario Child Health Study: Reliability and validity of the general functioning subscale of the McMaster Family Assessment Device. Fam Process. (1988) 27:97–104. doi: 10.1111/j.1545-5300.1988.00097.x
70. Ballard TJ, Kepple AW, Cafiero C. The Food Insecurity Experience Scale: Development of a Global Standard for Monitoring Hunger Worldwide. Technical Paper. Rome: FAO (2013).
71. Pereira AL, Handa S, Holmqvist G. Prevalence and correlates of food insecurity among children across the globe. In: Innocenti Working Paper 2017-09. Florence: UNICEF Office of Research (2017).
72. Cupak A, Pokrivcak J, Rizov M, Alexandri C, Luca L. Economic development and food demand in central and eastern European countries: the case of Romania. In: 142nd Seminar. Budapest: European Association of Agricultural Economists (2014).
73. Messer E. Rising food prices, social mobilizations, and violence: conceptual issues in understanding and responding to the connections linking hunger and conflict. NAPA Bull. (2009) 32:12–22. doi: 10.1111/j.1556-4797.2009.01025.x
74. Wehrheim P, Wiesmann D. Food security analysis and policies for transition countries. eJADE Electron J Agric Dev Econ. (2006) 3:112–43.
75. Bradley RH, Corwyn RF. Socioeconomic status and child development. Ann Rev Psychol. (2002) 53:371–99. doi: 10.1146/annurev.psych.53.100901.135233
76. McLoyd VC. Socioeconomic disadvantage and child development. Am Psychol. (1998) 53:185–204. doi: 10.1037/0003-066X.53.2.185
77. Anderson F, Howard L, Dean K, Moran P, Khalifeh H. Childhood maltreatment and adulthood domestic and sexual violence victimisation among people with severe mental illness. Social Psychiatr Psychiatr Epidemiol. (2016) 51:961–70. doi: 10.1007/s00127-016-1244-1
78. Corvo K, Carpenter EHJJoFV. Effects of parental substance abuse on current levels of domestic violence: a possible elaboration of intergenerational transmission processes. J Fam Violence. (2000) 15:123–35. doi: 10.1023/A:1007557626788
79. McLaughlin KA, Green JG, Alegria M, Jane Costello E, Gruber MJ, Sampson NA, et al. Food insecurity and mental disorders in a national sample of U.S. adolescents. J Am Acad Child Adolesc Psychiatr. (2012) 51:1293–303. doi: 10.1016/j.jaac.2012.09.009
80. Jones AD. Food insecurity and mental health status: a global analysis of 149 Countries. Am J Prev Med. (2017) 53:264–73. doi: 10.1016/j.amepre.2017.04.008
82. Frongillo EA, Nguyen HT, Smith MD, Coleman-Jensen A. Food insecurity is associated with subjective well-being among individuals from 138 Countries in the 2014. Gallup World Poll. J Nutr. (2017) 147:680–7. doi: 10.3945/jn.116.243642
83. Zorrilla B, Pires M, Lasheras L, Morant C, Seoane L, Sanchez LM, et al. Intimate partner violence: last year prevalence and association with socio-economic factors among women in Madrid, Spain. Eur J Public Health. (2009) 20:169–75. doi: 10.1093/eurpub/ckp143
84. Foran HM, Slep AMS, Heyman RE. Prevalences of intimate partner violence in a representative U.S. Air Force sample. J Consult Clin Psychol. (2011) 79:391–7. doi: 10.1037/a0022962
Keywords: hunger, food insecurity, violence, mental health, support, socioeconomic status
Citation: Jansen E, Lachman JM, Heinrichs N, Hutchings J, Baban A and Foran HM (2020) Hunger in Vulnerable Families in Southeastern Europe: Associations With Mental Health and Violence. Front. Public Health 8:115. doi: 10.3389/fpubh.2020.00115
Received: 27 September 2019; Accepted: 23 March 2020;
Published: 15 April 2020.
Edited by:
Zheng Feei Ma, Universiti Sains Malaysia Health Campus, MalaysiaReviewed by:
Ivana Kulhánová, Charles University, CzechiaMaria Melchior, Institut National de la Santé et de la Recherche Médicale (INSERM), France
Copyright © 2020 Jansen, Lachman, Heinrichs, Hutchings, Baban and Foran. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elena Jansen, ZWxlbmEuamFuc2VuQGFhdS5hdA==
 Elena Jansen
Elena Jansen Jamie M. Lachman2,3
Jamie M. Lachman2,3 Adriana Baban
Adriana Baban Heather M. Foran
Heather M. Foran