- 1Integrated Quality Laboratory Services, Lyon, France
- 2Division of Global Health Protection, Center for Global Health, Centers for Disease Control and Prevention, Atlanta, GA, United States
The pervasive nature of infections causing major outbreaks have elevated biosafety and biosecurity as a fundamental component for resilient national laboratory systems. In response to international health security demands, the Global Health Security Agenda emphasizes biosafety as one of the prerequisites to respond effectively to infectious disease threats. However, biosafety management systems (BMS) in low-medium income countries (LMIC) remain weak due to fragmented implementation strategies. In addition, inefficiencies in implementation have been due to limited resources, inadequate technical expertise, high equipment costs, and insufficient political will. Here we propose an approach to developing a strong, self-sustaining BMS based on extensive experience in LMICs. A conceptual framework incorporating 15 key components to guide implementers, national laboratory leaders, global health security experts in building a BMS is presented. This conceptual framework provides a holistic and logical approach to the development of a BMS with all critical elements. It includes a flexible planning matrix with timelines easily adaptable to different country contexts as examples, as well as resources that are critical for developing sustainable technical expertise.
Introduction
Before the recognition of the importance of biosafety at the World Health Organization's 58th World Health Assembly in 2005, biosafety has received increased attention in global health capacity building projects. Major international efforts have sought to advance a world safe and secure from infectious disease threats (1–4), especially as shown through the Global Health Security Agenda (GHSA), an international partnership of nearly 70 countries and major international organizations (such as WHO, OIE, FAO) engaged against infectious diseases (1). This GHSA encourages countries around the world to make new concrete commitments and transform global health security in support of the International Health Regulations (IHR) (5). Composed of 11 “action packages,” including biosafety and biosecurity, GHSA aims to reduce the ability of dangerous pathogens spreading rapidly within and across borders (2).
In the biosafety-biosecurity action package of the GHSA, the overarching goals are the: “Implementation of a comprehensive, sustainable and legally embedded national oversight program for biosafety and biosecurity, including the safe and secure use, storage, disposal, and containment of pathogens found in laboratories and a minimal number of holdings across the country, including research, diagnostic and biotechnology facilities. A cadre of biological risk management experts possesses the skillset to train others within their respective institutions. Strengthened, sustainable biological risk management best practices are in place using common educational materials. Rapid and culture-free diagnostics are promoted as a facet of biological risk management. The transport of infectious substances will also be taken into account” (6).
Despite these concrete targets, the biosafety-biosecurity action package is silent on concrete actions. The design and implementation of the requisite laboratory biosafety and biosecurity programs is inconsistent globally, especially in low- and middle-income countries (LMIC), with major gaps influenced by a variety of factors that include differences in national and local infrastructures, available funding and priorities, regulatory frameworks, and accessibility to expertise, training and equipment resources (3).
Many institutions, organizations and countries have worked on the development of biosafety management systems (BMS). BMS is based on a management system approach, which enables an organization to effectively identify, assess, control, and evaluate the biosafety and biosecurity risks inherent in its activity (7). However, they typically have focused only on few key elements of a national BMS, usually due to various constraints, such as budgetary limitations, time, or simply a limited understanding of what is a BMS (4–6, 8). Lessons from our extensive work in Burkina Faso (development of a national biosafety guideline, development of a biosafety and biosecurity assessment tool, conducting biosafety and biosecurity assessments, development of national biosafety regulations, and training of national assessors); other collaborations in Armenia, Burundi, Cameron, Guinea, Ghana, Georgia, Laos, Mauritania (organization of biosafety support, trainings and or assessments); Liberia and India (biosafety training, development of a national biosafety guideline, and specific support); Morocco (development of an laboratory infrastructure guideline); Sudan, Myanmar and Ethiopia (BSL3 assessments and/or trainings) (all unpublished), as well as observed gaps in various project countries which include: inadequate biosafety policies, lack of biosafety cabinet certification programs, lack of pre-service laboratory biosafety training curricula, absence of biosafety training packages and cascade training, and lack of IATA certified international shipment of infectious material capacities, have led us to a comprehensive and systems-based approach for a national BMS that can be sustainable and country-owned. Borrowing from our extensive global experience, we propose a conceptual framework outlining key steps to fulfill the biosafety expectations under the GHSA. We provide details to effectively strengthen biosafety and biosecurity capacities, through the development of sustainable biosafety management system (BMS) at country level.
Development of the System and Supporting Framework
Fundamental Considerations
There is of course no one-size-fits-all strategy to a biosafety management system; however, we identified common, key elements critical to establish a BMS. These 15 elements will fully capacitate a country in biosafety and biosecurity:
1) Creation of a National Biosafety Committee (NBC) and nomination of a National Biosafety Focal Person (NBFP) and a deputy NBFP
2) Development of biosafety and biosecurity national policies
3) Monitoring and evaluation of the implementation of the biosafety management framework
4) Organization of a biosafety and biosecurity training of trainers (for the core team of implementers)
5) Adaptation and development of the biosafety training package (for central and decentralized levels)
6) Identification, adaptation or development of a biosafety and safety laboratory assessment tool (BSS-LAT)
7) Conduct a national biosafety assessment using the developed BSS-LAT
8) Training of national BSS officers on assessment processes using the BSS-LAT
9) Development of a national biosafety and biosecurity guideline
10) Implementation of cascade trainings on biosafety and biosecurity at subnational levels
11) Adaptation and development of comprehensive national regulations on biosafety and biosecurity
12) Adaption, development, harmonization of national Standard Operating Procedures (SOPs) for biosafety and biosecurity
13) Reviewing and ensuring appropriate IATA training and certification at national level
14) Development or strengthening of (national) capacity of biomedical engineers to maintain biosafety equipment
15) Development and implementation of biosafety curricula for initial and recurrent trainings.
The key elements of the BMS framework that we propose are presented in Table 1. A number of them are interrelated; all we have found to be essential in establishing a sustainable and country-owned BMS. In addition to these 15 elements, there are three additional or supplemental elements that could be included in the BMS process but are less critical:
(a) Organization of a workshop on pathogen risk group classification,
(b) Development of a laboratory infrastructure guidelines, and
(c) Organization of a workshop on biobanking, including regulation and data protection.
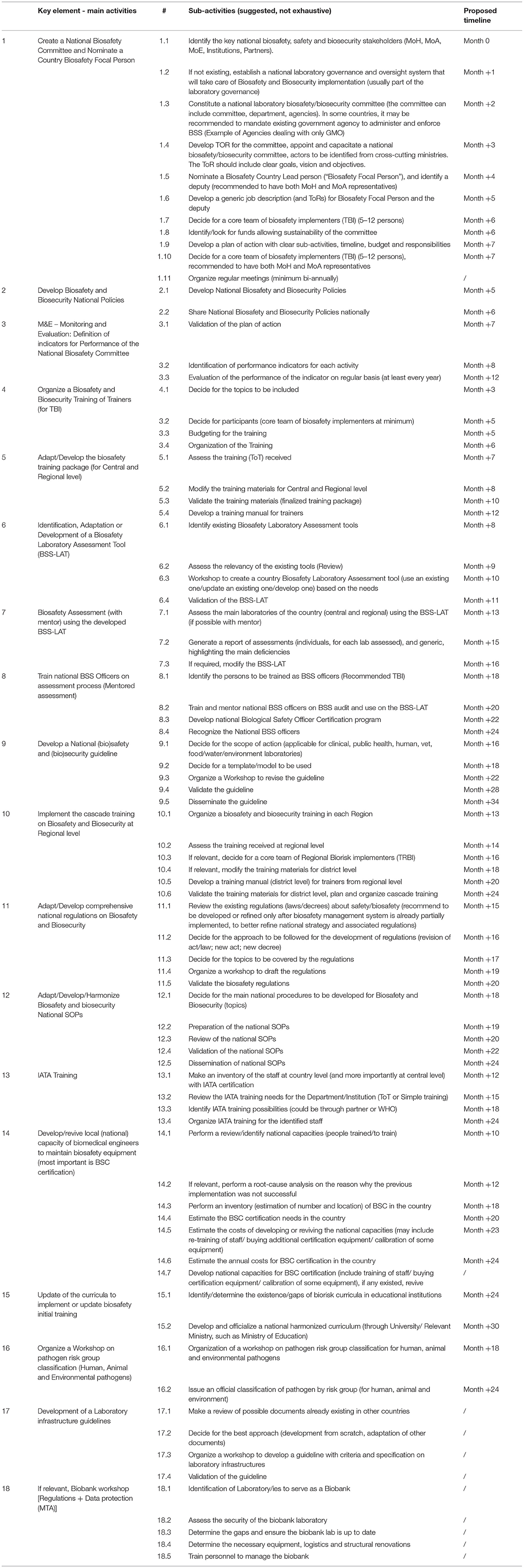
Table 1. Proposed combined framework approach based on 15 key elements, and detailed sub-activities.
The timeline proposed is intentionally aggressive in order to both elevate the importance of BMS in the national strategy and to prioritize the identification of gaps. Key contextual factors that should be considered by countries following this framework and timeline include, the size of the country, budget available, time dedicated by persons involved, and ease of the collaboration between governmental institutions and partners.
Development of Sustainability and Country Ownership
Implementation requires mentorship and guidance through the National Biosafety Committee and an implementation team composed of national or international specialist(s). In our experience, external technical assistance through best practices, examples, and objective feedback is beneficial. Public or private institutions, including professional biosafety associations can provide this expertise (9–11). Even with external technical assistance, the country should continue to maintain ownership of the implementation process, including leadership of the process, typically through the National Biosafety Focal Person (NBFP) and/or a National Biosafety Committee (NBC) (per our framework). Such leadership is an important aspect of national capacities (7), and is critical for implementation. Absence of leadership makes implementing a comprehensive national BMS all but impossible.
Development of Training
A major gap in developing and implementing a national BMS is the paucity of local knowledge and skills. This gap can be addressed through training of local experts who will become the champions and leaders of the BMS. Numerous training packages exist and can be delivered through various mechanisms – in-class training or online, either free or for a fee (12). Additionally, many reputable organizations provide biosafety training. Based on our experience, we recommend countries ensure training is performed according to local needs and requirements, that it includes identified topics of interest, and delivered according to the modalities defined by country policies and customs. These should include at a minimum simulation exercises that explore theoretical and practical aspects, opportunities for facilitated discussion and exchange of information, and include training materials in a format that allows updating and adaptation (such Microsoft Office, Google Docs). As with other activities mentioned here, support from external partners can be beneficial, provided leadership and ownership from the country is maintained.
A growing number of remote or virtual training solutions have become available in recent years and can even be used as curricula base (13). However, these tools should be thoroughly reviewed and preference given to materials of quality and adaptable to the local context. Public platforms such as YouTube? have also became a vast resource of training materials, here again, with a broad range of quality, but amendable to inclusion in training plans.
Locating Resources and Tools
Additional supporting resources (including training materials) and tools are widely available such as those offered by the Centers for Disease Control and Prevention (14), the World Health Organization (15), the U.S. National Institutes of Health (9), the Association of Public Health Laboratories (10), the American Biosafety Association (11), the International Federation of Biosafety Associations (16) and even universities [examples include the University of Tennessee (17), Yale University (18)]. Private agencies have also developed numerous biosafety resources. The difficulty is not in finding resources, but rather in identifying high-quality resources that can be adapted to the specific country context.
Dedicated Financial Resources Are Essential
A dedicated budget is vital to ensure that the proposed activities can be executed. Funds are critical to support training, infrastructure requirements including procurement of safety, information technology equipment, facility renovations, and implementation and monitoring activities. These financial resources should ideally be identified and driven from various channels, including government/ministry funding, vertical programs and partners. This approach to funding will help ensure collaboration of efforts and partners and reduce duplication or unnecessary activities that often are counterproductive to the end goals.
Toward a Sustainable System
We strongly believe that taking into consideration all 15 key elements from our framework is critical. Additionally, these actions should be developed in an integrated manner, ensuring the establishment of a sustainable system that can be country-owned. This BMS can be independent on individual expertise or donor projects, as it takes a long-term perspective and enhances national capacities and competencies on biosafety and associated skills.
Our team has been involved in implementing a number of these key elements of a biosafety management system through various international projects (unpublished). Lessons learnt through our experiences strongly suggest an integrated approach that considers all aspects of a BMS is optimal. To our knowledge this type of approach has not been implemented nor described previously. We offer this perspective and guidance to assist future projects, implementers and stakeholders to view the BMS in its totality using the critical elements that we have defined. In this way, it will ensure all the interrelated components of a national BMS are addressed and implemented in sustainable fashion to achieve the goals of the GHSA.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
The original concept of the manuscript was developed by AO, OK, and AP, who also drafted the manuscript. AN, AZ, AA, and LP contributed to the development of the approach presented in the manuscript and provided comments and revisions to the draft manuscript. All authors contributed to the article and approved the submitted version.
Funding
The development of this publication was supported by the Centers for Disease Control and Prevention (CDC), as part of the Global Health Security Agenda (GHSA).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors are thankful to the institutions, partners, stakeholders, and laboratories with which we collaborated on various aspects of biosafety, as they contributed to the origin of this perspective on biosafety management system.
References
1. Global Health Security Agenda. Global Health Security Agenda (GHSA). Action Packages. Available online at: https://ghsagenda.org/home/action-packages/ (accessed July 7, 2021).
2. Bakanidze L, Imnadze P, Perkins D. Biosafety and biosecurity as essential pillars of international health security and cross-cutting elements of biological nonproliferation. BMC Public Health. (2010) 10 (Suppl. 1):S12. doi: 10.1186/1471-2458-10-S1-S12
3. Mouillé B, Dauphin G, Wiersma L, Blacksell SD, Claes F, Kalpravidh W, et al. A tool for assessment of animal health laboratory safety and biosecurity: the safety module of the food and agriculture organization's laboratory mapping tool. Trop Med Infect Dis. (2018) 3:33. doi: 10.3390/tropicalmed3010033
4. Dickmann P, Sheeley H, Lightfoot N. Biosafety and biosecurity: a relative risk-based framework for safer, more secure, and sustainable laboratory capacity building. Front Public Health. (2015) 3:2296–565. doi: 10.3389/fpubh.2015.00241
5. Susanti I, Susilarini NK, Setiawaty V. Assessment of biorisk management implementation in NIHRD laboratory as national referral laboratory of emerging infectious diseases in Indonesia. Health Sci J Indonesia. (2018) 9:70–5. doi: 10.22435/hsji.v9i2.811
6. Khan E, Ahmed N, Temsamani KR, El-Gendy A, Cohen M, Hasan A, et al. Biosafety initiatives in BMENA region: identification of gaps and advances. Front Public Health. (2016) 4:2296–565. doi: 10.3389/fpubh.2016.00044
7. Albetkova A, Chaignat E, Gasquet P, Heilmann M, Isadore J, Jasir A, et al. A competency framework for developing global laboratory leaders. Front Public Health. (2019) 7:2296–565. doi: 10.3389/fpubh.2019.00199
8. Naroeni A, Bachtiar EW, Ibrahim F, Bela B, Kusminanti Y, Pujiriani I, et al. Challenges in implementing a biorisk management program at Universitas Indonesia: a checklist tool for biorisk management. Health Secur. (2016) 14:375–81. doi: 10.1089/hs.2016.0013
9. National Institute of Heath (NIH). Biosafety Guidance and Resources. Additional Resources. Available online at: https://osp.od.nih.gov/biotechnology/biosafety-guidance-and-resources/ (accessed November 27, 2019).
10. Association of Public Health Laboratories (APHL). Lab Biosafety & Biosecurity Resources. Available online at: https://www.aphl.org/programs/preparedness/Biosafety-and-Biosecurity/Pages/BB-Resources.aspx (accessed November 27, 2019).
11. American Biological Safety Association (ABSA). ABSA Page. Available online at: https://absa.org/ (accessed November 27, 2019).
12. Center for Disease Control and Prevention. Division of Laboratory System (DLS). Biosafety Trainings. Available online at: https://www.cdc.gov/safelabs/trainings.html (accessed November 27, 2019).
13. Ndolo DO, Wach M, Rüdelsheim P, Craig W. A curriculum-based approach to teaching biosafety through elearning. Front Bioeng Biotechnol. (2018) 6:2296–4185. doi: 10.3389/fbioe.2018.00042
14. Center for Disease Control and Prevention (CDC). Biosafety Resources and Tools. Available online at: https://www.cdc.gov/safelabs/resources-tools.html (accessed November 27, 2019).
15. World Health Organization (WHO). Biosafety. Available online at: https://www.who.int/ihr/publications/biosafety-video-series/en/ (accessed November 27, 2019).
16. International Federation of Biosafety Associations (IFBA). IFBA Page. Available online at: https://internationalbiosafety.org/resources/biosafety-biosecurity/ (accessed November 27, 2019).
17. University of Tennessee. Lab-Related Biosafety Resources. Available online at: https://biosafety.utk.edu/biosafety-program/resources/lab-resources/ (accessed November 27, 2019).
18. University of Yale. Biological Safety. Available online at: https://ehs.yale.edu/biological (accessed November 27, 2019).
Keywords: biosafety, safety, biosecurity, biorisk, framework, Global Health Security Agenda, capacities, system
Citation: Orelle A, Nikiema A, Zakaryan A, Albetkova AA, Rayfield MA, Peruski LF, Pierson A and Kachuwaire O (2021) National Biosafety Management System: A Combined Framework Approach Based on 15 Key Elements. Front. Public Health 9:609107. doi: 10.3389/fpubh.2021.609107
Received: 22 September 2020; Accepted: 28 June 2021;
Published: 23 July 2021.
Edited by:
Adam Fusheini, University of Otago, New ZealandReviewed by:
Emmanuel D. Jadhav, Ferris State University, United StatesAntonino Di Caro, Istituto Nazionale per le Malattie Infettive Lazzaro Spallanzani (IRCCS), Italy
Copyright © 2021 Orelle, Nikiema, Zakaryan, Albetkova, Rayfield, Peruski, Pierson and Kachuwaire. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Obert Kachuwaire, S2FjaHV3YWlyZUBpcWxzLm5ldA==
†Present address: Arnaud Orelle, Lab'Science, Nazelles-Négron, France
 Arnaud Orelle
Arnaud Orelle Abdoulaye Nikiema
Abdoulaye Nikiema Arsen Zakaryan
Arsen Zakaryan Adilya A. Albetkova
Adilya A. Albetkova Mark A. Rayfield2
Mark A. Rayfield2 Leonard F. Peruski
Leonard F. Peruski Obert Kachuwaire
Obert Kachuwaire