- 1School of Energy and Environment, University of Phayao, Phayao, Thailand
- 2Atmospheric Pollution and Climate Change Research Unit, School of Energy and Environment, University of Phayao, Phayao, Thailand
- 3School of Allied Health Science, University of Phayao, Phayao, Thailand
This mini-review aims to highlight both the positive and negative relationship between COVID-19 and air pollution and climate change based on current studies. Since, COVID-19 opened a bibliographic door to scientific production, so there was a limit to research at the moment. There were two sides to the relationship between COVID-19 and both air pollution and climate change. The associated with climate change, in particular, defines the relationship very loosely. Many studies have revealed a positive correlation between COVID-19 and each air pollutants, while some studies shown a negative correlation. There were a few studies that focused on the relationship between COVID-19 in terms of climate. Meanwhile, there were many studies explained the relationship with meteorological factors instead.
Introduction
COVID-19, an infectious respiratory infection, rapidly spread to other parts of China and eventually became a global epidemic (1–3). Several early studies shown that being in close proximity to anyone who has the disease increases the risk of infection (4–6). Furthermore, recent review papers state that there are two modes of COVID-19 transmission: direct and indirect. SARS-CoV-2 bioaerosol is transferred in direct mode through the air in the internal atmosphere in the form of droplet nuclei and other body fluids, as well as from mother to infant. In the indirect mode, infections are caused by fomites or the surfaces of furniture and fixtures in the immediate environment of an infected patient (7, 8). According to recent research, air pollutants are risk factors for infectious respiratory disease as well as COVID-19 (9–12). Air pollution can make patients more vulnerable to the disease and have a detrimental effect on their prognosis (13–15). This could be explained by enhanced angiotensin converting enzyme 2 (ACE-2) expression in respiratory epithelial cells exposed to air pollution (16). COVID-19 lockdown, on the other hand, has had numerous positive effects on the environment and energy consumption (17). It was loosely defined in terms of climate change and COVID-19. However, many of the underlying causes of climate change are also linked to an increase in pandemics through climate factors such as temperature, wind speed, and humidity (18–20). Recent studies have indicated a mostly negative relationship between COVID-19, air pollution, and climate change, for example, the relationship between climate change, environmental pollution, COVID-19, and mental health (21), and the influence of air pollution on COVID-19 mortality (22). However, further research is needed to determine if it is relevant or not. The highlight of this mini-review is the state of both the relationship between COVID-19 and air pollution and climate change, as well as revealing both positive and negative effects of the relationship.
The Relationship Between COVID-19, Air Pollution and Climate Change
Covid-19 and Air Pollution
The relationship between air pollution and coronavirus is ambiguous, which was indicated by both positive and negative correlation in the current studies (Figure 1). Many studies have revealed that air pollution increases the COVID-19 mortality rate, whereas COVID-19 lockdown could reduce air pollution level at the same time. There is some evidence from recent studies revealing that increased risk of COVID-19 infection is associated with exposure to higher air pollutant levels including PM2.5, PM10, CO, NO2, SO2, and O3. For example, Wu et al. (23) and Cole et al. (24), have found that long-term exposure to PM2.5 was associated with a substantial 11% increased risk of cardiovascular death and hospital admissions. In addition, according to a study conducted in Milan, Italy, all recorded daily new COVID-19 cases were positively correlated with the average surface PM2.5 and the daily maximum PM10 (25). Several studies discussed the relationship between O3 and NOx and COVID-19 but it was unclear in those studies. The current research discovered both a negative (26) and a positive (25) correlation between NOx and COVID-19 in various parts of the world. However, as the role in flagging SARS-CoV-2 transmission, O3 was importantly correlated with COVID-19 (27). Unfortunately, there has been relatively little research into the relationship between CO and SO2. Sangkham et al. (26) discovered that increases in CO and SO2 were correlated with decreases in the daily number of COVID-19 cases, while another study recently indicated that 1 g/m3 CO is associated with a 15.11% increase in the daily count of confirmed COVID-19 cases (28). Meanwhile, a SO2 concentration of 10 g/m3 was associated with a 7.79% decrease in the regular number of reported cases in China's 120 cities (28). As a result, there is insufficient evidence for conclusive findings for CO and SO2 in the current study, leading to these variables being both negatively and positively associated with SARS-CoV-2 transmission. At the same time, some studies indicated that COVID-19's indirect effect could help alleviate the problem of air pollution. For example, Mostafa et al. (29) reported a strong correlation between COVID-19 lockdown and a 15–33% reduction in NO2 and 5% reduction throughout CO in Egypt. Kumari and Toshniwal (30), studied a similar situation that occurred in India. They estimated that the COVID-19 lockdown could reduce PM10, PM2.5, NO2, and SO2 concentrations by 55, 49, 60, and 19%, respectively, in Delhi and Mumbai. This finding was corroborated by Wetchayont (31), who discovered that several air pollutant concentrations, including PM2.5, PM10, O3, and CO, showed a significant decline during the COVID-19 outbreak in Bangkok, Thailand.
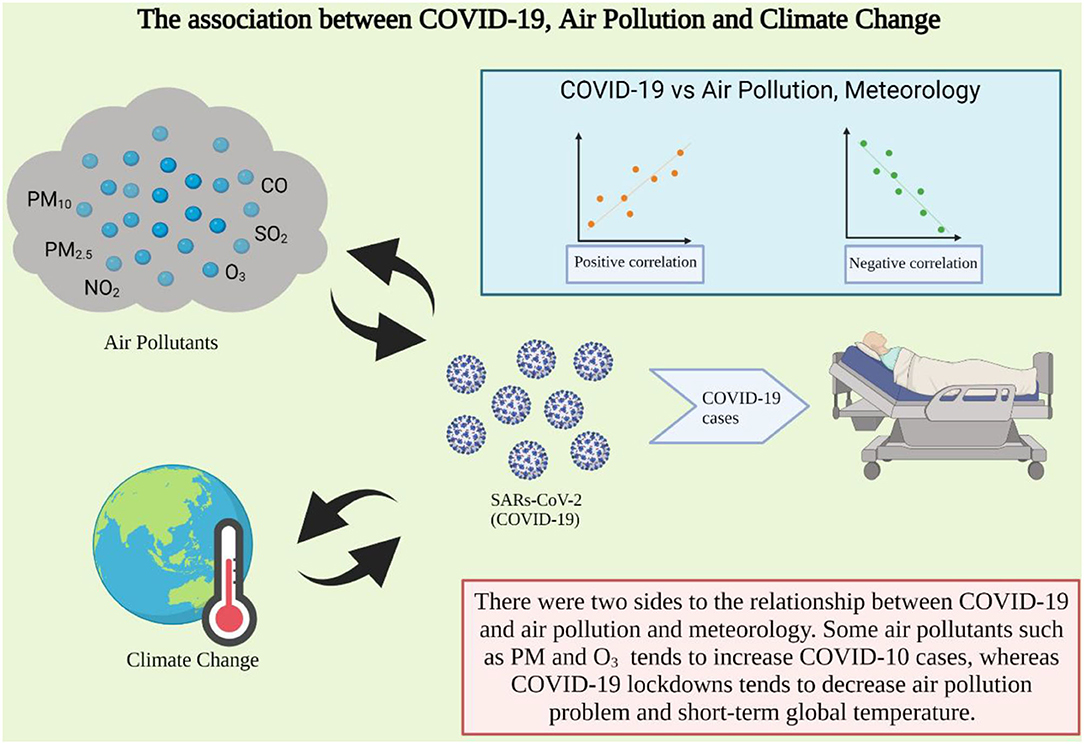
Figure 1. The association between COVID-19 and air pollution and climate change (Created with BioRender.com).
Covid-19 and Climate Change
When compared to air pollution, the link between COVID-19 and climate change is extremely ambiguous. Since COVID-19 events were detected in 2019, there was no clear evidence of climate change's effect on COVID-19, which is typically a long-term event (32). There was a recent review about climate change and the COVID-19 epidemic in Rodó et al. (33). They stated that both absolute humidity (AH) and temperature have been linked to influenza outbreaks and facilitated epidemic progression. In tropical regions, SARS-CoV-2 appears to have a higher airborne survival and transmission rate than the influenza virus. A blockade of aerosol transmission in the case of influenza virus has been described for temperature variations above 30°C. Whereas, the direct effect of the pandemic-driven response will be negligible, with a cooling a global temperature of around 0.01 ± 0.005°C by 2030 (34). This result was supported by the concept of anthropause that suggested that reduced human mobility during the pandemic will reveal critical aspects of our impact on animals, providing important guidance on how best to share space on this crowded planet (35). The global temperature signal, however, is anticipated to be small as a result of the pandemic's short-term dynamics. Another evidence that might correlate the relationship between climate and COVID-19 is using meteorological factors including the temperature, Relative Humidity (RH), AH, and Wind Speed (WS). Most studies in many countries, including Thailand, Singapore, India, and China, found a positive relationship between temperature and the daily number of COVID-19 cases (26, 36, 37). Several research, however, found a negative association between temperature and COVID-19 cases. Wu et al. (38) and To et al. (39), for example, discovered that rising temperatures were associated with a decrease in daily new cases of COVID-19 in Brazil and Canada. Other variables, such as RH (%), AH (g/m3), and WS (m/s), had a positive relationship with the number of COVID-19 cases in many countries, including Thailand and Turkey (26, 40). Furthermore, relative humidity was found to be negatively correlated with daily new COVID-19 cases by Wu et al. (38). Another research provided experimental results demonstrating that lower relative humidity promotes influenza virus transmission, confirming this weather effect (41). The SARS coronavirus's stability at low humidity can support its spread in communities in subtropical climates (such as Hong Kong) during the spring (42). For WS, the relationship with COVID-19 was identical to those of humidity and temperature, which have both positive (26) and negative (43) relationships. WS, on the other hand, may potentially affect SARS-CoV-2 in an indoor rather than outdoor environment among symptomatic and asymptotic cases due to sneezing and coughing in population-dense areas.
Conclusion
The conclusion is based on the current studies on the relationship between COVID-19 and air pollution and climate change. Many studies have shown that several air contaminants, including PM2.5, PM10, CO, NO2, SO2, and O3, increase COVID-19 mortality rates. However, some research suggests that COVID-19's indirect effect could help to reduce air pollution. Particulate matter has been linked to a rise in COVID-19 incidents. Although the current study lacks adequate evidence for conclusive findings for CO and SO2, which are both negatively and positively associated with SARS-CoV-2 transmission. Current research has discovered both a negative and a positive relationship between NOx and COVID-19 in different parts of the world. As a marker of SARS-CoV-2, O3 was found to be significantly associated with COVID-19 and air pollution-related infections. While there has been no conclusive evidence of the effect of climate change on COVID-19, which is typically a long-term phenomenon. A few studied suggested that SARS-CoV-2 has a higher airborne survival and transmission rate than the influenza virus in tropical areas. While the direct effect of the pandemic-driven response will reduce a global temperature by 2030. The relationship between temperature, humidity, and wind speed can be used to support the correlation between the atmosphere and COVID-19 events. Since there are uncertainty in the relationships between COVID-19 and air pollution and climate change, the meta-analysis should be conducted in the future work.
Author Contributions
TA: conceived and designed the manuscript, contributed reagents and materials, and wrote the paper. NP: editing and revised the paper. All authors contributed to the article and approved the submitted version.
Funding
This research project was supported by the Thailand Science Research and Innovation fund and the University of Phayao (Grant no. FF64-UoE015).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
I would like to thank Atmospheric Environment Research Unit, University of Phayao for financial support.
References
1. Gilbert M, Pullano G, Pinotti F, Valdano E, Poletto C, Boëlle Y, et al. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. (2020) 395:871–7. doi: 10.1016/S0140-6736(20)30411-6
2. Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World health organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. (2020) 76:71–6. doi: 10.1016/j.ijsu.2020.02.034
3. Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. (2020) 395:809–15. doi: 10.1016/S0140-6736(20)30360-3
4. Li H, Xu XL, Dai DW, Huang ZY, Ma Z, Guan YJ. Air pollution and temperature are associated with increased COVID-19 incidence: a time series study. Int J Infect Dis. (2020) 97:278–82. doi: 10.1016/j.ijid.2020.05.076
5. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061–9. doi: 10.1001/jama.2020.1585
6. Chan JFW, Yuan S, Kok KH, To KW, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. (2020) 395:514–23. doi: 10.1016/S0140-6736(20)30154-9
7. Eslami H, Jalili M. The role of environmental factors to transmission of SARS-CoV-2 (COVID-19). Amb Express. (2020) 10:1–8. doi: 10.1186/s13568-020-01028-0
8. Karia R, Gupta I, Khandait H, Yadav A, Yadav A. COVID-19 and its modes of transmission. SN Compr Clin Med. (2020) 2:1–4. doi: 10.1007/s42399-020-00498-4
9. Cai QC, Lu J, Xu QF, Guo QZ, Sun QW, Yang H, et al. Influence of meteorological factors and air pollution on the outbreak of severe acute respiratory syndrome. Public Health. (2007) 121:258–65. doi: 10.1016/j.puhe.2006.09.023
10. Horne BD, Joy EA, Hofmann MG, Gesteland PH, Cannon JB, Lefler JS, et al. Short-term elevation of fine particulate matter air pollution and acute lower respiratory infection. Am J Respir Crit Care Med. (2018) 198:759–66. doi: 10.1164/rccm.201709-1883OC
11. Xie J, Teng J, Fan Y, Xie R, Shen A. The short-term effects of air pollutants on hospitalizations for respiratory disease in Hefei, China. Int J Biometeorol. (2019) 63:315–26. doi: 10.1007/s00484-018-01665-y
12. Domingo JL, Marqu‘es M, Rovira J. Influence of airborne transmission of SARS-CoV- 2 on COVID-19 pandemic. A review. Environ Res. (2020) 188:109861. doi: 10.1016/j.envres.2020.109861
13. Brook RD, Rajagopalan S, Pope III CA, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. (2010) 121:2331–78. doi: 10.1161/CIR.0b013e3181dbece1
14. Pope III CA, Coleman N, Pond ZA, Burnett RT. Fine particulate air pollution and human mortality: 25+ years of cohort studies. Environ Res. (2020) 183:108924. doi: 10.1016/j.envres.2019.108924
15. Pope III CA, Burnett RT, Thurston GD, Thun MJ, Calle EE, Krewski D, et al. Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation. (2004) 109:71–7. doi: 10.1161/01.CIR.0000108927.80044.7F
16. Paital B, Agrawal PK. Air pollution by NO 2 and PM 2.5 explains COVID-19 infection severity by overexpression of angiotensin-converting enzyme 2 in respiratory cells: a review. Environ Chem Lett. (2020) 19:1–18. doi: 10.1007/s10311-020-01091-w
17. Mousazadeh M, Paital B, Naghdali Z, Mortezania Z, Hashemi M, Karamati Niaragh E, et al. Positive environmental effects of the coronavirus 2020 episode: a review. Environ Dev Sust. (2021) 1–23. doi: 10.1007/s10668-021-01240-3
18. Tan J, Mu L, Huang J, Yu S, Chen B, Yin J. An initial investigation of the association between the SARS outbreak and weather: with the view of the environmental temperature and its variation. J Epidemiol Commun Health. (2005) 59:186. doi: 10.1136/jech.2004.020180
19. Islam ARMT, Hasanuzzaman M, Azad MAK, Salam R, Toshi FZ, Khan MSI, et al. Effect of meteorological factors on COVID-19 cases in Bangladesh. Environ Dev Sustain. (2020) 1–24. doi: 10.1007/s10668-020-01016-1
20. Xie J, Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci Total Environ. (2020) 754:138201. doi: 10.1016/j.scitotenv.2020.138201
21. Marazziti D, Cianconi P, Mucci F, Foresi L, Chiarantini C, Della Vecchia A. Climate change, environment pollution, COVID-19 pandemic and mental health. Sci. Total Environ. (2021) 773:145182. doi: 10.1016/j.scitotenv.2021.145182
22. Ali N, Islam F. The effects of air pollution on COVID-19 infection and mortality-a review on recent evidence. Front Public Health. (2020) 8:57. doi: 10.3389/fpubh.2020.580057
23. Wu X, Braun D, Schwartz J, Kioumourtzoglou MA, Dominici FJSA. Evaluating the impact of long-term exposure to fine particulate matter on mortality among the elderly. Sci Adv. (2020) 6:eaba5692. doi: 10.1126/sciadv.aba5692
24. Cole MA, Ozgen C, Strobl E. Air pollution exposure and Covid-19 in dutch municipalities. Environ Resource Econ. (2020) 76:581–610. doi: 10.1007/s10640-020-00491-4
25. Zoran MA, Savastru RS, Savastru DM, Tautan MN. Assessing the relationship between surface levels of PM2.5 and PM10 particulate matter impact on COVID-19 in Milan, Italy. Sci Total Environ. (2020) 738:139825. doi: 10.1016/j.scitotenv.2020.139825
26. Sangkham S, Thongtip S, Vongruang P. Influence of air pollution and meteorological factors on the spread of COVID-19 in the Bangkok metropolitan region and air quality during the outbreak. Environ Res. (2021) 197:111104. doi: 10.1016/j.envres.2021.111104
27. Lolli S, Vivone G. The role of tropospheric ozone in flagging COVID-19 pandemic transmission. Bull Atmos Sci Technol. (2020) 1:551–5. doi: 10.21203/rs.3.rs-89804/v1
28. Zhu Y, Xie J, Huang F, Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci Total Environ. (2020) 727:138704. doi: 10.1016/j.scitotenv.2020.138704
29. Mostafa MK, Gamal G, Wafiq A. The impact of COVID 19 on air pollution levels and other environmental indicators-A case study of Egypt. J Environ Manage. (2021) 277:111496. doi: 10.1016/j.jenvman.2020.111496
30. Kumari P, Toshniwal D. Impact of lockdown measures during COVID-19 on air quality–a case study of India. Int J Environ Health Res. (2020). doi: 10.1080/09603123.2020.1778646. [Epub ahead of print].
31. Wetchayont P. Investigation on the impacts of COVID-19 lockdown and influencing factors on air quality in greater Bangkok, Thailand. Adv Meteorol. (2021) 2021:6697707. doi: 10.1155/2021/6697707
32. Amnuaylojaroen T. Projection of the precipitation extremes in thailand under climate change scenario RCP8.5. Front Environ Sci. (2021) 9:657810. doi: 10.3389/fenvs.2021.657810
33. Rodó X, San-José A, Kirchgatter K, López L. Changing climate and the COVID-19 pandemic: more than just heads or tails. Nat Med. (2021) 27:576–9. doi: 10.1038/s41591-021-01303-y
34. Forster PM, Forster HI, Evans MJ, Gidden MJ, Jones CD, Keller CA, et al. Current and future global climate impacts resulting from COVID-19. Nat Clim Chan. (2020) 10:913–9. doi: 10.1038/s41558-020-0883-0
35. Rutz C, Loretto MC, Bates AE, Davidson SC, Duarte CM, Jetz W, et al. COVID-19 lockdown allows researchers to quantify the effects of human activity on wildlife. Nat Ecol Evolut. (2020) 4:1156–9. doi: 10.1038/s41559-020-1237-z
36. Pani SK, Lin NH, RavindraBabu S. Association of COVID-19 pandemic with meteorological parameters over Singapore. Sci Total Environ. (2020) 740:140112. doi: 10.1016/j.scitotenv.2020.140112
37. Kumar G, Kumar RR. A correlation study between meteorological parameters and COVID-19 pandemic in Mumbai, India. Diabetes Metab Syndr. (2020) 14:1735–42. doi: 10.1016/j.dsx.2020.09.002
38. Wu Y, Jing W, Liu J, Ma Q, Yuan J, Wang Y, et al. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci Total Environ. (2020) 729:139051. doi: 10.1016/j.scitotenv.2020.139051
39. To T, Zhang K, Maguire B, Terebessy E, Fong I, Parikh S, et al. Correlation of ambient temperature and COVID-19 incidence in Canada. Sci Total Environ. (2021) 750:141484. doi: 10.1016/j.scitotenv.2020.141484
40. Sahin M. Impact of weather on COVID-19 pandemic in Turkey. Sci Total Environ. (2020) 728:138810. doi: 10.1016/j.scitotenv.2020.138810
41. Gardner EG, Kelton D, Poljak Z, Van Kerkhove M, von Dobschuetz S, Greer AL. A case-crossover analysis of the impact of weather on primary cases of Middle East respiratory syndrome. BMC Infect Dis. (2019) 19:113. doi: 10.1186/s12879-019-3729-5
42. Chan KH, Peiris JM, Lam SY, Poon LLM, Yuen KY, Seto WH. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv Virol. (2011) 2011:734690. doi: 10.1155/2011/734690
Keywords: COVID-19, air pollution, climate change, environment, environmental impact
Citation: Amnuaylojaroen T and Parasin N (2021) The Association Between COVID-19, Air Pollution, and Climate Change. Front. Public Health 9:662499. doi: 10.3389/fpubh.2021.662499
Received: 01 February 2021; Accepted: 10 June 2021;
Published: 06 July 2021.
Edited by:
Patrick Lott Kinney, Boston University, United StatesReviewed by:
Voltaire Alvarado Peterson, University of Concepcion, ChileRichard Stoffle, University of Arizona, United States
Abu Reza Md. Towfiqul Islam, Begum Rokeya University, Bangladesh
Mashura Shammi, Jahangirnagar University, Bangladesh
Milad Mousazadeh, Qazvin University of Medical Sciences, Iran
Copyright © 2021 Amnuaylojaroen and Parasin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Teerachai Amnuaylojaroen, dGVlcmFjaGFpLmFtQHVwLmFjLnRo; dGVlcmFjaGFpNEBnbWFpbC5jb20=
 Teerachai Amnuaylojaroen
Teerachai Amnuaylojaroen Nichapa Parasin
Nichapa Parasin