- 1Department of Public Health, Graduate School of Biomedical Sciences, Texas Tech University Health Sciences Center, Abilene, TX, United States
- 2University of Texas Health Science Center at Houston School of Public Health, Brownsville, TX, United States
- 3College of Science and Health, Charles R. Drew University of Medicine and Science, Los Angeles, CA, United States
- 4College of Communication, Boston University, Boston, MA, United States
This study tested whether a cancer education intervention affected promotores' self-efficacy to deliver an intervention to Hispanics and which psychosocial determinants of promotores influenced the number of Hispanic residents reached by promotores in the subsequent education intervention. A quasi-experimental, pre/post-design with a treatment group (no control) assessed differences for promotores (n = 136) before and after exposure to the cancer education intervention. The design also included a cross-sectional evaluation of the number of residents promotores reached with the educational intervention. After being trained, the promotores delivered the intervention to Hispanic residents (n = 1,469). Paired t-tests demonstrated increases in promotores' self-efficacy from pre- to post-intervention. Regression models assessed associations between the numbers of residents reached and select psychosocial determinants of promotores. Age and promotores' years of experience influenced their delivery of a cervical cancer education intervention to Hispanics, but not their delivery of breast or colorectal cancer education interventions. This is the first study to examine which psychosocial determinants influence promotores delivery of cancer education interventions. The outcomes potentially have implications for CHW interventions and training by examining this potential connection between CHWs' psychosocial determinants and intervention outcomes.
Introduction
“Promotores are everyday people who are already living, working and engrained in the community…They are the individuals others go to when they have problems, need advice or even just want to gossip over a cup of coffee” (1).
As frontline public health workers, promotores [community health workers (CHWs)], function as liaisons between health and social service providers and the priority population to facilitate access to services and improve the quality and cultural competence of service delivery through a wide array of skillsets. Promotores are trusted members of the community and have a remarkable understanding of the community, may work for pay or as volunteers, and usually share ethnicity, language, socioeconomic status, and life experiences with the community members they serve (2–4). Core functions of promotores/CHWs have included health education, promotion, outreach, case management, service coordination, informal counseling, social support, advocacy, referrals, and health behavior interventions (5, 6). The utilization of promotores in the United States has grown particularly in the past 10 years (7, 8) along with evidence supporting the effectiveness of promotores in delivering interventions (9–11). Numerous studies have highlighted the use of promotores and their effectiveness among Hispanic populations in helping their priority populations achieve positive health outcomes (5, 8–11).
Training involved in preparing promotores to conduct interventions is substantial and comprehensive and incorporates promotores in decision making and feedback regarding project implementation after the training (12–14). Yet, even with intensive training, like other conduits for the delivery of health education content, there are barriers to the implementation of interventions delivered by promotores (15, 16). An important translational science question is what characteristics of promotores influence the delivery of interventions (17, 18). Proven, effective interventions involving promotores delivered under highly controlled settings are fruitless if, in a practice setting, there are problems with the delivery of the intervention by promotores. A greater understanding of what characteristics influence that delivery is needed for the more efficient diffusion of interventions led by promotores.
This study seeks to fill this gap by examining the psychosocial determinants of promotores in relation to the delivery of a cancer education intervention to Hispanic residents. Few studies have looked at psychosocial determinants of promotores' delivery of an intervention (19), and no studies were found that focus on these psychosocial determinants of promotores specific to cancer education interventions. Psychosocial determinants are defined as the interaction of psychological factors (e.g., an individual's thoughts, self-efficacy, intentions, and behaviors) and social factors (e.g., education, employment, social norms and attitudes, social support and interactions, and socioeconomic conditions) that influence health status (20, 21).
This study focused on cancer delivered interventions among Hispanic populations given that cancer is the second leading cause of death among Hispanics (22); Hispanics are less likely to obtain cancer screenings (23, 24); Hispanics are often diagnosed and treated at later stages of cancer (25–27); and Hispanics face greater cancer survivorship barriers than non-Hispanic Whites (25, 27). Evidence suggests key factors contributing to poorer cancer outcomes in Hispanics include the following: socio-demographic factors such as poverty, lack of education and information, and lack of health insurance; language barriers; and low health literacy (26, 28–30). Furthermore, this study included information on cervical cancer education intervention since Hispanic females have the highest incidence and the second highest mortality rate of cervical cancer in the United States (25, 31) and face numerous barriers regarding cervical cancer prevention and screening (31–34).
This study had two main aims: (1) to test whether a cancer education intervention affects promotores' self-efficacy from pre- to post-training; and (2) to examine which psychosocial determinants of promotores might influence how many Hispanic residents receive cancer education interventions delivered by the promotores. Self-efficacy is an important outcome given its role in different health behavioral theories (e.g., Health Belief Model) as an antecedent of health behavior. It can be defined in terms of people's beliefs in their capability to perform a specific behavior to achieve an anticipated outcome (35). The psychosocial determinants of promotores examined included promotores' years of work experience, work status (paid or volunteer), self-efficacy to deliver cancer education to Hispanic residents, intention to use the information in his/her work and promotores' certification status.
Data and Methods
Parent Study
The parent study—ÉPICO: Education to Promote Improved Cancer Outcomes—was a cancer education intervention evaluated by an exploratory quasi-experimental, pre-test-post-test study design. The overall strategy of ÉPICO was to train and utilize promotores as learners and educators to deliver a cancer education intervention to Hispanic colonia residents. Community Health Workers/Promotores in Texas are certified, which means they have either completed a 160-h certification training as CHWs/Promotores or they obtained certification through at least 1,000 verified hours of work as a CHW/Promotora (36). Colonias are unincorporated sub-divisions lacking basic infrastructure and services (37). The study consisted of three separate training modules that were 8 h in length each (one 8-h training for breast cancer prevention, treatment and survivorship; one 8-h training for cervical cancer prevention, treatment and survivorship; and one 8-h training for colorectal cancer prevention, treatment and survivorship). While the curriculum covered the continuum of cancer prevention, treatment, and survivorship, each training had specific elements and evidence-based information for each section as well as covering information related to prevention, treatment, and survivorship throughout the 8-h trainings. Promotoroes could choose to attend one, two, or all three ÉPICO trainings, provided at different times during the project period. The selection criteria for participation was self-identification as a promotora and being at least 18 years of age.
The ÉPICO cancer education interventions were grounded in the socio-ecological model, the health belief model, the stages of change (transtheoretical) model, and evidence-based principles of adult learning theory—engaging promotores in an interactive environment based upon discussion and skill-building exercises (38, 39). The focus groups and surveys utilized constructs from the aforementioned theories; these theories also then provided a framework for the module content. For example, from the health belief model, the training materials addressed perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy (40). For a detailed outline of content for each ÉPICO cancer education intervention and for more information on methods, refer to previous publications on the ÉPICO study (41, 42).
Study Design
For the purposes of this manuscript, a quasi-experimental, pre-post, one group design was used for this exploratory study. Pre/post-tests assessed differences for promotores (n = 136) before and after exposure to the intervention on prevention, treatment, and survivorship for breast, cervical, or colorectal cancer. The design also included time-lagged evaluations of the number of residents promotores reached. Data were collected from promotores who attended an 8-h training on prevention/early detection, treatment, and healthy survivorship for breast, cervical, or colorectal cancers via pre/post-tests as the data collection instruments. These measures included an assessment of psychosocial determinants of the promotores. Data were collected from the promotores on the number of Hispanic residents they reached with a cancer intervention within the 2 months following their initial training. This data included intervention logs of the number of residents reached as the data collection instrument.
Study Setting
The study setting included 8-h trainings on prevention, treatment, and healthy survivorship for breast, cervical, or colorectal cancers for self-identified promotores conducted in four south Texas border counties. The trainings were conducted by six state-certified promotora instructors employed by the ÉPICO project at community partner facilities, including the following: academic partners (four trainings—two in Hidalgo County and two in Cameron County), a community resource center (one training, Hidalgo County), and a county-owned facility (one training, Cameron County). Promotores who received the ÉPICO promotora cancer education intervention then delivered the interventions to Hispanic colonia residents in the four counties as part of their regular promotora outreach and education responsibilities.
Recruitment and Procedures
Study participants included both promotores and Hispanic colonia residents. The study did not include a study size calculation. First, promotores serving Hispanic colonia residents in the four counties were recruited by emails to distribution lists, participants from previous trainings, partnering entities, the state Promotora/CHW Program contact list, and word of mouth. Study staff obtained informed consent, and participants filled out the pre-test questionnaire. ÉPICO certified instructors gave the 8-h trainings to the promotores, which covered detailed information on prevention, treatment, and healthy survivorship specific to either breast, cervical or colorectal cancers. The training included activities to ensure that the topics were learned and a review and practice time associated with the specifically designed intervention modules that were to be delivered to residents. After the training, promotores completed the post-test questionnaire, which included the pre-test measures and demographic and psychosocial measures. Second, within 2 months of receiving the training, promotores were given the option to implement the educational intervention with Hispanic colonia residents. The intervention for the residents consisted of the same topics—prevention, treatment, and healthy survivorship—for either breast, cervical, or colorectal cancers; the resident interventions covered broader, key points pertaining to these topics and included important facts, photos, questions and answers, and action planning. Promotores opting to deliver the cancer education interventions obtained consent, conducted the intervention (i.e., 1.5 h of education per cancer type with residents), collected resident collection pre/post-tests and evaluations, and returned study instruments to ÉPICO staff within 2 months of the initial ÉPICO promotora training. Promotores who educated at least 10 Hispanic colonia residents received a $25 Wal-Mart gift card. The promotores were not compensated through salary support for their time to provide the education to colonia residents.
Measures
The pre/post-tests had 15 knowledge and six self-efficacy survey items. Self-efficacy was measured using a Likert scale (low confidence: 1–2; medium confidence: 3–4; and high confidence: 5–6) and measured participants': (1) confidence in delivering (breast, cervical, colorectal) cancer prevention/early detection messages; (2) confidence in motivating others to take steps toward (breast, cervical, colorectal) cancer prevention/early detection; (3) confidence in developing (breast, cervical, colorectal) cancer treatment messages; (4) confidence in motivating others to obtain (breast, cervical, colorectal) cancer treatment; (5) confidence in delivering (breast, cervical, colorectal) survivorship messages; and (6) confidence in motivating others to take steps toward healthy (breast, cervical, colorectal) cancer survivorship behaviors. In addition, post-test included demographic and psychosocial measures. The dependent variable was the number of colonia residents who received the cancer education intervention by the promotores. This was determined from the promotores' intervention logs detailing the number of residents educated by cancer education module. The number of Hispanic colonia residents reached by promotores was treated as a continuous variable. We also examined the number of colonia residents reached by promotores per cancer type (i.e., breast, cervical, or colorectal).
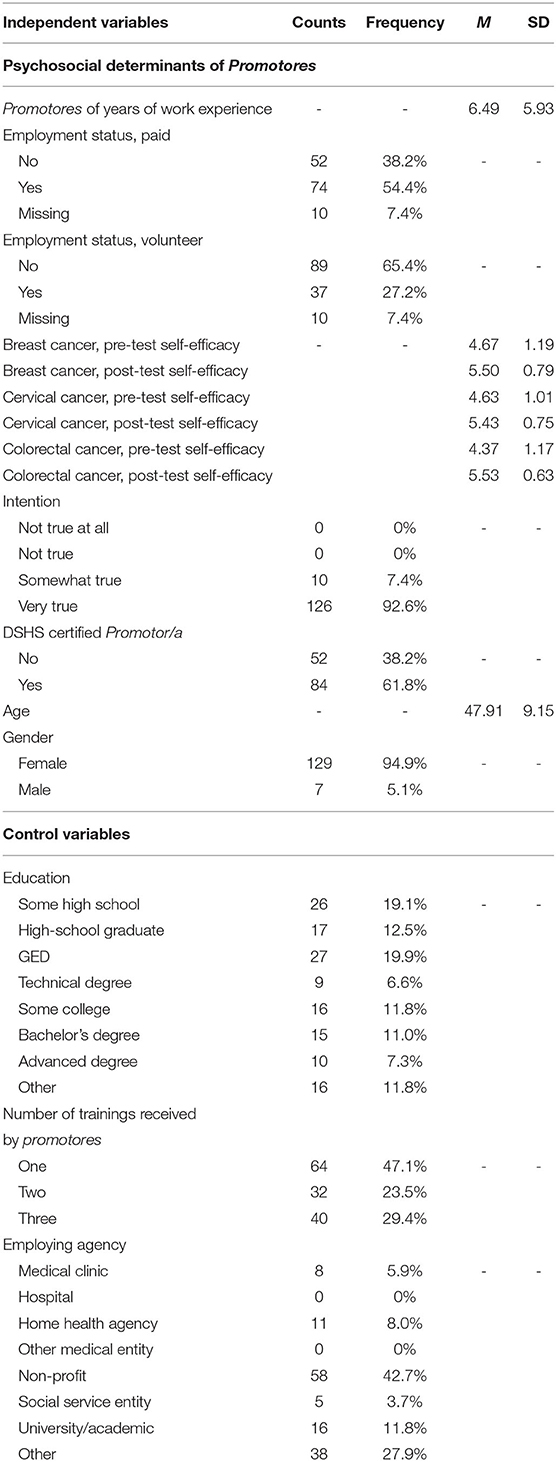
The independent variables were separated into two categories: psychosocial determinants of promotores and control variables. Psychosocial determinants of promotores included: (1) promotores' years of work experience; (2) work status (paid or volunteer); (3) self-efficacy in delivering cancer education to Hispanic colonia residents; (4) intention to use the information in his/her work (scale from 1 to 4 with 1 = not at all true, 2 = not true; 3 = somewhat true; and 4 = very true); and (5) certified promotor/a (yes/no). For promotores' self-efficacy, measures were recorded for each cancer type both pre- and post-training, (scale from 1 to 6, with low self-efficacy being 1 and high self-efficacy being 6). Three questions measured self-efficacy for each specific type of cancer module: (1) self-efficacy in delivering (breast, cervical, colorectal) cancer prevention/early detection messages; (2) self-efficacy in delivering (breast, cervical, colorectal) cancer treatment messages; and (3) self-efficacy in delivering (breast, cervical, colorectal) cancer survivorship messages. Cronbach alphas were used to test the reliability of the scale measuring the self-efficacy values. The self-efficacy variables for pre- and post-measures for breast, cervical, and colorectal cancers all had reliability values of α = 0.96 or higher (reported in Table 3).
Control variables included the following: (1) age (years of age); (2) gender (male/female); (3) education (with the following responses: some high school; high-school graduate; GED; technical degree; some college; Bachelor's degree; advanced degree); and (4) the number of cancer type trainings received by the promotores (with the following responses: one cancer type; two cancer types; and three cancer types).
This study was approved by the Committee for the Protection of Human Subjects (CPHS) at the University of Texas Health Science Center, and the parent study was approved by the Institutional Review Board (IRB) at Texas A&M University.
Data Analysis
Analyses were conducted using STATA 12.0 (43). Missing values were replaced with mean scores since data were missing in <5% of any variable (44). Factor analysis and Cronbach's alphas were run on each of the sets of self-efficacy items for pre- and post-measures for breast, cervical, and colorectal cancers. Paired t-tests for the pre- and post-self-efficacy scores were run to test for differences among the pre- and post-self-efficacy means for the three cancers; p-values < 0.05 were considered significant. Regression models were run to assess potential associations between the continuous dependent and continuous and dichotomous independent variables. Three regression models (one per cancer) assessed predictors and included statistically significant variables (p < 0.05) related to the dependent variable.
Results
A total of 136 promotores received the ÉPICO promotor/a training modules. Of those, 50% (68) delivered the cancer education intervention to 1,469 Hispanic colonia residents. Table 1 further details the number of residents receiving the specific cancer education interventions delivered by promotores. The psychosocial determinants and demographic control variables of the promotores who received at least one ÉPICO cancer education intervention are displayed Table 2. Promotores tended to be women (95%), had an average age of 48 (range of 20–73), had a high-school education or less (53%), had an average of 6.5 years of work experience as promotores (ranged from 0 to 25 years), and were Texas-certified promotores (68%). Hispanic colonia residents who received a cancer education invention delivered by these promotores included 450 residents receiving the breast cancer education intervention; 506 residents receiving the cervical cancer education intervention; and 513 residents receiving the colorectal cancer education intervention. The factor analysis followed a normal distribution, with no outliers and points randomly distributed about zero.
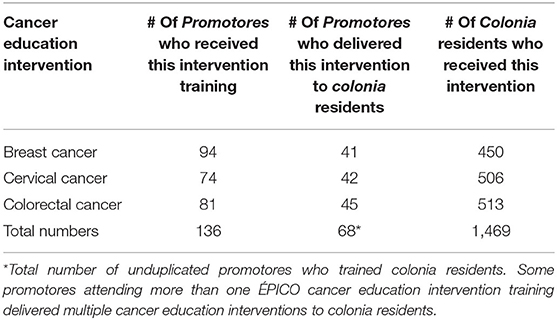
Table 1. The number of residents receiving the specific ÉPICO cancer education interventions delivered by Promotores.
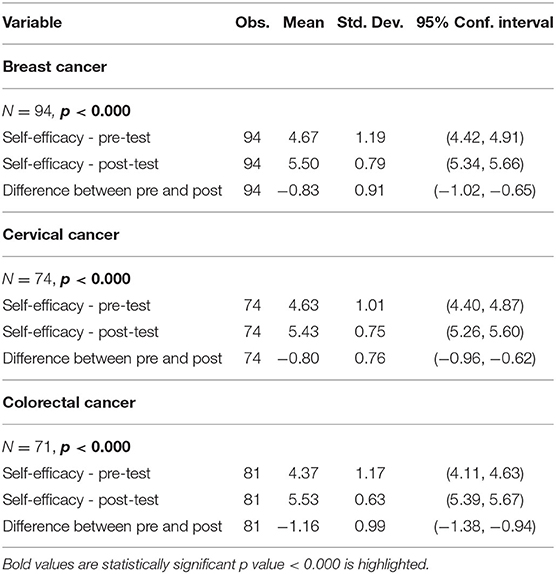
The paired t-test results for the pre- and post-promotora training self-efficacy scores on the three cancer topics are shown in Table 3. There were significant increases in promotores' pre- and post-training scores for each cancer specific training (p-values for all three cancers < 0.000).
Table 4 depicts results of the regression models examining whether there are significant psychosocial determinants associated with delivering cancer education; on breast cancer (model 1); on cervical cancer (model 2); and on colorectal cancer (model 3). For the delivery of cervical cancer education, promotores' years of work experience (P > |t| = 0.000), age (P > |t| = 0.003), and the number of promotor/a cancer trainings received (P > |t| = 0.001) were significant in the cervical cancer model, which included all of the independent and control variables. Additionally, the number of promotor/a cancer trainings received was also significant for breast cancer (P > |t| = 0.000) and colorectal cancer (P > |t| = 0.020). The R2-values for each module were as follows: R2 = 0.26 for breast cancer, R2 = 0.41 for cervical cancer, and R2 = 0.12 for colorectal cancer.
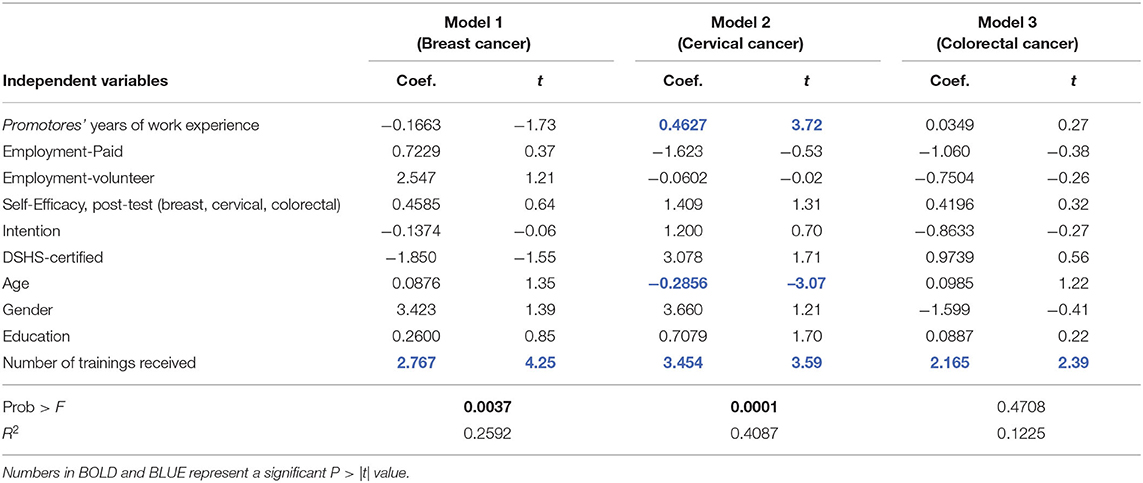
Table 4. Regression analysis for psychosocial variables predicting number of Colonia residents trained in cancer education (N = 136).
Discussion
This study is the first of its kind to examine which psychosocial determinants of promotores influence their delivery of cancer education interventions to Hispanic colonia residents. Results showed that promotores' years of work experience, promotores' age, and the number of cancer trainings received by promotores were significantly associated with the number of Hispanic colonia residents who received the cervical cancer education intervention. This is noteworthy because this is the first study to suggest which psychosocial determinants might affect the delivery of a cancer education intervention. In light of the burden of cervical cancer incidence and mortality on Hispanic females, interventions utilizing promotores in cervical cancer education interventions might consider these psychosocial determinants—age, promotores' years of work experience, and number of other relevant trainings—when recruiting promotores to implement interventions. Our results also suggest that psychosocial determinants of promotores are associated with intervention delivery—which constitutes a novel contribution to the literature.
Another important finding was the effectiveness of the cancer education interventions to increase promotores' self-efficacy pre- and post-training. We found that the changes between pre- and post-self-efficacy measures were significant for all three cancers and that the self-efficacy measures were reliable. Though self-efficacy was not found to be significant in these regression models to predict the number of residents reached, this finding of the cancer education interventions might have influenced other desired outcomes not examined in this study (such as increased knowledge of the residents receiving the intervention and higher residents' intentions to change behavior). Future studies could examine how this increased self-efficacy might have influenced additional outcomes of interest.
Lastly, of note in this study is what associations between variables were not found to be significant. First, the study examined breast, cervical, and colorectal cancer education interventions for Hispanic colonia residents, yet, only two psychosocial determinants were found to be significant for cervical cancer. This creates questions regarding why these factors were significant for one cancer and not the others—suggesting that promotora psychosocial determinants influencing intervention delivery to residents may be different depending the intervention topic—whether type of cancer or specific chronic disease. Second, though the study looked at numerous promotora psychosocial determinants, few were found to significantly impact their intervention delivery to colonia residents. This draws out another key question in terms of why these determinants—self-efficacy, promotores' certification status, intention to implement the intervention, gender, educational level, and work status—were not associated in this study with the delivery of an intervention to the priority population. Future research can examine these and other psychosocial determinants to further elucidate possible associations. For example, promotora marital status and work experience in occupations may be important psychosocial determinants influencing promotores' ability to voluntarily deliver cancer education interventions. Additionally, the regression models showed variance in the models, yet the psychosocial determinants were not significant in explaining this variance. This finding brings additional questions as to what else could explain the variance in the models if not the independent variables. This suggests that additional psychosocial determinants may need to be examined and also a larger sample size could yield significant results for these same psychosocial determinants. In this regard, the small sample size could be prone to Type II error. The results from this study demonstrate the need for future studies to continue investigating what psychosocial determinants of promotores do influence delivery of interventions since this is one of the first studies to do so.
Challenges and Limitations
The lack of a control group as well as the exploratory nature of this pre-post, one group design, quasi-experimental study limits this study's demonstration of causation. While comparisons of pre- and post-self-efficacy involve panel data permit inferences of causation, as does the implementation of time-lagged independent and dependent variables in the regression analysis, the study does not prove causation, for which further study is warranted to examine potential causal links. In addition, the results of this study may not be generalizable to all Hispanic groups and promotores because there may be significant variations among both promotores and Hispanic residents since the samples were not randomly selected or assigned to intervention condition. Another limitation was that the study did not use a study size calculation and also used a convenience sample so whether or not a randomized design would yield different or identical results is unclear. Further, response to study questions may have been influenced by subject's educational level or other factors and skew study results. For example, participants with lower educational and literacy levels may not have understood a question on the instruments and could have selected responses that did not accurately reflect their true responses—particularly if participants were not familiar with Likert-type responses. To address this limitation, pre- and post-instruments with third grade reading levels were used. Additionally, the instruments were read aloud to participants with time for them to select responses independently.
Further, the self-efficacy measurement was simplistic and a limitation. Future work can address this limitation through utilization of established markers (for example, “I am confident I can deliver breast cancer prevention information to Hispanics with lower literacy levels within the next 30 days.”). Another potential limitation is not controlling for promotora experience as well addressing employment status of the promotores. Future studies should consider how to measure and control for experience and type of employment of promotores. Non-response and missing data were also a potential limitation, which was handled by replacing missing values with mean scores given the low percentage of missing data. Lastly, another limitation was the small sample size, which could have contributed to type I error.
Conclusions
The major findings in this study point to the potential connection between promotores' psychosocial determinants and their influence on behavioral outcomes of program participants—which has been studied very little in the past. Knowing what psychosocial determinants that potentially improve behavioral and health outcomes of those served by promotores could help in the recruitment and training of promotores, which in turn, could yield greater health outcomes for the priority populations served by promotores. This study has a number of areas to expand upon. For instance, future studies should examine which psychosocial determinants of promotores may influence the delivery of an intervention to the priority population based on the specific type of cancer. Further, studies could explore additional psychosocial determinants and characteristics of promotores that might influence the delivery of an intervention that were not examined in this study such as acculturation, social capital, social support, health status, and relationships with the priority community. Also, additional inquiry is needed on how promotores' self-efficacy may influence subsequent indicators of resident training.
One strength of the study was the large number of promotores trained on the same cancer education interventions and then following them over time to assess the use of these interventions in practice. An additional strength of the study was the use of reliable measures to assess increases in self-efficacy to deliver cancer education interventions. Lastly, another strength of the study was the ability to connect psychosocial measures of promotores to examine the scope of their work—the number of Hispanic colonia residents who received the cancer education intervention delivered by promotores—and to contribute to this literature on which there is currently little information. Our findings are just a starting point for further research on which psychosocial determinants influence delivery of an intervention. Future research should focus on the T3 step of translational science—the identification of new questions (e.g., additional psychosocial determinants of promotores that might influence intervention delivery), barriers, and gaps through dissemination and implementation research. This is an iterative process that allows researchers to return to prior translational stages. Once goals are reached in the T3 step, additional studies can then engage in the T4 step of policy research. This might include looking at developing and implementing policies regarding the utilization of promotores in intervention in terms of promotores' psychosocial determinants.
In closing, this study examined which psychosocial determinants of promotores may influence the delivery of the intervention to the priority population based on the specific type of cancer and has numerous possibilities for areas of future research that could significantly impact research practice and design of cancer education interventions delivered by promotores.
Data Availability Statement
The datasets presented in this article are not readily available because the corresponding author conducted the research at a previous institution. Requests to access the datasets should be directed to https://nchwtc.tamhsc.edu/, Y2h3LXRyYWluaW5nQHRhbWhzYy5lZHU=.
Ethics Statement
The studies involving human participants were reviewed and approved by Committee for the Protection of Human Subjects (CPHS), University of Texas Health Science Center; Institutional Review Board (IRB), Texas A&M University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author's Note
This manuscript is part of a doctoral dissertation. St. John (2014). Psychosocial determinants of promotores and selected outcomes for a cancer education intervention implemented in South Texas colonias. Three-paper dissertation, ProQuest Dissertations, UMI Dissertation Publishing, http://www.proquest.com.
Author Contributions
JS was the PI on the original EPICO study and conducted this study as part of a dissertation. BR served as the dissertation committee chair and guided the study development, conduction, and analysis. She participated significantly to the writing and revising of the manuscript. HB and MV-S served on the dissertation committee and guided the study development, conduction, and analysis. They reviewed and revised the manuscript. CB was a Co-I on the original study and served on the dissertation committee. He played a significant role in analyzing the data and writing up the results. All authors contributed to the article and approved the submitted version.
Funding
This project was funded by the Cancer and Prevention Research Institute of Texas (# PP110241).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to acknowledge the promotora/CHW instructors and project staff who conducted the trainings and assisted in evaluation activities: Aracely Garibay, Lupita Garza, Leticia Gutierrez, Dinorah Martinez, Gabriela Robinson, Paula Saldaña, Denise Adame-Hernandez, and Katherine Nimmons.
References
1. Latino Leadership Council. Promotoras: Promoting Health in our Community. (2011). Available online at: http://latinoleadershipcouncil.wordpress.com/ (accessed April 15, 2013).
2. Grant M, Wilford A, Haskins L, Phakathi S, Mntambo N, Horwood CM. Trust of community health workers influences the acceptance of community-based maternal and child health services. Afr J Prim Health Care Fam Med. (2017) 9:e1–8. doi: 10.4102/phcfm.v9i1.1281
3. American Public Health Association. Community Health Workers. Retrieved from American Public Health Association (2020). Available online at: https://www.apha.org/apha-communities/member-sections/community-health-workers (accessed February 27, 2021).
4. Hellerstedt J. Community Health Workers | DSHS. Texas Department of State Health Services, Community Health Worker or Promotor(a) Training and Certification Program (2019). Available online at: https://www.dshs.state.tx.us/mch/chw.shtm (accessed February 27, 2021).
5. Hartzler AL, Tuzzio L, Hsu C, Wagner EH. Roles and functions of community health workers in primary care. Ann Fam Med. (2018) 16:240–5. doi: 10.1370/afm.2208
6. Snyder JE. Community Health Workers: Roles and Opportunities in Health Care Delivery System Reform. ASPE ISSUE BRIEF, Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation (2016). Available online at: http://aspe.hhs.gov (accessed February 27, 2021).
7. Koskan A, Friedman DB, Messias DK, Brandt HM, Walsemann K. Sustainability of promotora initiatives: program planners' perspectives. J Public Health Manag Pract. (2013) 19:E1–9. doi: 10.1097/PHH.0b013e318280012a
8. Bovbjerg RR, Eyster L, Ormond BA, Anderson T, Richardson E. The Evolution, Expansion, and Effectiveness of Community Health Workers. The Urban Institute (2014). Available online at: https://www.urban.org/research/publication/evolution-expansion-and-effectiveness-community-health-workers (accessed February 27, 2021).
9. Lairson DR, Kim J, Byrd T, Salaiz R, Shokar NK. Cost-effectiveness of community interventions for colorectal cancer screening: low-income Hispanic population. Health Promot Pract. (2018) 19:863–72. doi: 10.1177/1524839917750815
10. Luque JS, Logan A, Soulen G, Armeson KE, Garrett DM, Davila CB, et al. Systematic review of mammography screening educational interventions for hispanic women in the United States. J Cancer Educ. (2019) 34:412–22. doi: 10.1007/s13187-018-1321-0
11. Shokar NK, Byrd T, Salaiz R, Flores S, Chaparro M, Calderon-Mora J, et al. Against colorectal cancer in our neighborhoods (ACCION): a comprehensive community-wide colorectal cancer screening intervention for the uninsured in a predominantly Hispanic community. Prev Med. (2016) 91:273–80. doi: 10.1016/j.ypmed.2016.08.039
12. St John JA, Johnson C, Arandia G, Sharkey JR, Dean W. Empowerment of promotoras as promotora-researchers in the comidas saludables and gente sana en las colonias del sur de tejas (healthy food and health people in South Texas Colonias) program. J Prim Prevent. (2013) 34:41–57. doi: 10.1007/s10935-013-0296-1
13. Strachan DL, Källander K, Ten Asbroek AH, Kirkwood B, Meek SR, Benton L, et al. Interventions to improve motivation and retention of community health workers delivering integrated community case management (iCCM): stakeholder perceptions and priorities. Am J Trop Med Hyg. (2012) 87(Suppl. 5):111–9. doi: 10.4269/ajtmh.2012.12-0030
14. Whiteman LN, Gibbons MC, Smith WR, Stewart RW. Top 10 things you need to know to run community health worker programs: lessons learned in the field. South Med J. (2016) 109:579–82. doi: 10.14423/SMJ.0000000000000504
15. Haughton J, Takemoto ML, Schneider J, et al. Identifying barriers, facilitators, and implementation strategies for a faith-based physical activity program. Implement Sci Commun. (2020) 1:51. doi: 10.1186/s43058-020-00043-3
16. Ingram M, Reinschmidt KM, Schachter KA, Davidson CL, Sabo SJ, De Zapien JG, et al. Establishing a professional profile of community health workers: results from a national study of roles, activities and training. J Community Health. (2012) 37:529–37. doi: 10.1007/s10900-011-9475-2
17. Documet PI, Macia L, Boyzo R, Thompson AF, Amruthapuri R. Outcomes from a male-to-male promotores intervention in an emerging latino community. J Immigr Minor Health. (2020) 4:717–26. doi: 10.1007/s10903-019-00939-w
18. McDermott-Levy R, Weatherbie K. Health promotores' perceptions of their communities' health needs, knowledge, and resource needs in Rural Nicaragua. Public Health Nurs. (2020) 2:94–105. doi: 10.1111/j.1525-1446.2012.01047.x
19. Crispin N, Wamae A, Ndirangu M, Wamalwa D, Wangalwa G, Watako P, et al. Effects of selected socio-demographic characteristics of community health workers on performance of home visits during pregnancy: a cross-sectional study in Busia District, Kenya. Glob J Health Sci. (2012) 4:78–90. doi: 10.5539/gjhs.v4n5p78
20. Harding S, Read UM, Molaodi OR, Cassidy A, Maynard MJ, Lenguerrand E. The determinants of young adult social well-being and health (DASH) study: diversity, psychosocial determinants and health. Soc Psychiatry Psychiatr Epidemiol. (2015) 50:1173–88. doi: 10.1007/s00127-015-1047-9
21. Michels N, Vynckier L, Moreno LA, Beghin L, de la OA, Forsner M, et al. Mediation of psychosocial determinants in the relation between socio-economic status and adolescents' diet quality. Eur J Nutr. (2018) 57:951–63. doi: 10.1007/s00394-017-1380-8
22. American Cancer Society. Cancer Facts and Figures for Hispanics/Latinos, 2018-2020. Atlanta: American Cancer Society, Inc (2018). Available online at: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-hispanics-and-latinos/cancer-facts-and-figures-for-hispanics-and-latinos-2018-2020.pdf (accessed March 31, 2021).
23. Stanley SL, King JB, Thomas CC, Richardson LC. Factors associated with never being screened for colorectal cancer. J Community Health. (2013) 38:31–9. doi: 10.1007/s10900-012-9600-x
24. Valdovinos C, Penedo FJ, Isasi CR, Jung M, Kaplan RC, Giacinto RE, et al. Perceived discrimination and cancer screening behaviors in US Hispanics: the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. Cancer Causes Control. (2016) 27:27–37. doi: 10.1007/s10552-015-0679-0
25. Miller KD, Goding Sauer A, Ortiz AP, Fedewa SA, Pinheiro PS, Tortolero-Luna G, et al. Cancer Statistics for Hispanics/Latinos, 2018. Can J Clin. (2018) 68:425–45. doi: 10.3322/caac.21494
26. Yanez B, McGinty HL, Buitrago D, Ramirez AG, Penedo FJ. Cancer outcomes in Hispanics/Latinos in the United States: an integrative review and conceptual model of determinants of health. J Latina/o Psychol. (2016) 4:114–29. doi: 10.1037/lat0000055
27. Zhang C, Zhang C, Wang Q, Li Z, Lin J, Wang H. Differences in stage of cancer at diagnosis, treatment, and survival by race and ethnicity among leading cancer types. JAMA Netw Open. (2020) 3:e202950. doi: 10.1001/jamanetworkopen.2020.2950
28. Kyounghae K, Hae-Ra H. Potential links between health literacy and cervical cancer screening behaviors: a systematic review. Psycho-Oncology. (2015) 25:122–30. doi: 10.1002/pon.3883
29. Martinez TD, Medina-Ramirez P, Flores AM, Siegel R, Aguado LC. Unpacking hispanic ethnicity-cancer mortality differentials among hispanic subgroups in the United States, 2004–2014. Front Public Health. (2018) 6:219. doi: 10.3389/fpubh.2018.00219
30. Zavala VA, Bracci PM, Carethers JM, et al. Cancer health disparities in racial/ethnic minorities in the United States. Br J Cancer. (2021) 124:315–32. doi: 10.1038/s41416-020-01038-6
31. Mann L, Foley KL, Tanner AE, Sun CJ, Rhodes SD. Increasing cervical cancer screening among US Hispanics/Latinas: a qualitative systematic review. J Cancer Educ. (2015) 30:374–87. doi: 10.1007/s13187-014-0716-9
32. Heintzman J, Hatch B, Coronado G, Ezekiel D, Cowburn S, Escamilla-Sanches O, et al. Role of race/ethnicity, language, and insurance in use of cervical cancer prevention services among low-income Hispanic women, 2009-2013. Pre Chronic Dis. (2018) 15:170267. doi: 10.5888/pcd15.170267
33. Luque JS, Tarasenko YN, Maupin JN, Alfonso ML, Watson LC, Reyes-Garcia C, et al. Cultural beliefs and understandings of cervical cancer among Mexican immigrant women in Southeast Georgia. J Immig Minority Health. (2015) 17:713–21. doi: 10.1007/s10903-014-0117-5
34. Moore de Peralta A, Holaday B, McDonell JR. Factors affecting hispanic women's participation in screening for cervical cancer. J Immig Minority Health. (2015) 17:684–95. doi: 10.1007/s10903-014-9997-7
35. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. (1977) 84:191–215. doi: 10.1037/0033-295X.84.2.191
36. Texas State Department of Health Services. Community Health Worker or Promotor(a) Training and Certification Program. (2021). Available online at: https://dshs.texas.gov/chw.aspx (accessed August 8, 2021).
37. Texas State Energy Conservation Office. Colonias Initiatives (2003-2007). Available online at: http://www.seco.cpa.state.tx.us/colonias/ (accessed April 8, 2013).
38. Mukhalalati BA, Taylor A. Adult learning theories in context: a quick guide for healthcare professional educators. J Med Educ Curr Dev. (2019) 6:1–10. doi: 10.1177/2382120519840332
39. Ramírez DM, Vea L, Field JA, Baker PB, Gandolfi AJ, Maier RM. Transferable training modules: building environmental education opportunities with and for mexican community health workers (Promotores de Salud). Fam Commun Health. (2017) 40:306–15. doi: 10.1097/FCH.0000000000000111
40. Champion VL. Instrument development for health belief model constructs. Adv Nurs Sci. (1984) 6:73–85. doi: 10.1097/00012272-198404000-00011
41. St John J, Beaudoin CE, Nimmons K, Adame D, Ory M. Promotores and ÉPICO: a model for implementing a cancer training and education program among Hispanics with increased cancer risk. Texas Public Health J. (2013) 65:20–4.
42. Nimmons K, Beaudoin C, St John JA. The outcome evaluation of a CHW cancer prevention intervention: testing individual and multilevel predictors among hispanics living along the Texas-Mexico border. J Can Educ. (2017) 32:183–89. doi: 10.1007/s13187-015-0930-0
43. StataCorp. STATA Data Analysis and Statistical Software (Version 12.0) [computer software]. (2013). Available online at: http://stata.com/ (accessed February 27, 2021).
Keywords: training, Hispanics, cancer education intervention, promotores, community health worker, psychosocial determinants
Citation: St. John J, Reininger B, Balcazar H, Valerio-Shewmaker MA and Beaudoin CE (2021) What About Promotores? Promotores' Psychosocial Determinants That Influenced the Delivery of a Cervical Cancer Education Intervention to Hispanics. Front. Public Health 9:689616. doi: 10.3389/fpubh.2021.689616
Received: 01 April 2021; Accepted: 03 August 2021;
Published: 10 September 2021.
Edited by:
Tam Ha, University of Wollongong, AustraliaReviewed by:
Beti Thompson, Fred Hutchinson Cancer Research Center, United StatesCarlos Miguel Rios-González, National University of Caaguazú, Paraguay
Copyright © 2021 St. John, Reininger, Balcazar, Valerio-Shewmaker and Beaudoin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julie St. John, anVsaWUuc3Qtam9obkB0dHVoc2MuZWR1
 Julie St. John
Julie St. John Belinda Reininger
Belinda Reininger Hector Balcazar3
Hector Balcazar3 Melissa A. Valerio-Shewmaker
Melissa A. Valerio-Shewmaker