- 1Clinical Nursing Teaching and Research Section, The Second Xiangya Hospital, Central South University, Changsha, China
- 2Geriatric Department, The Second Xiangya Hospital, Central South University, Changsha, China
- 3Xiangya School of Public Health, Central South University, Changsha, China
Urinary incontinence (UI) is a common problem among older adults. This study investigated the prevalence of UI in nursing home residents aged ≥75 years in China and examined potential risk factors associated with UI and its subtypes. Data were collected during face-to-face interviews using a general questionnaire, the International Consultation Incontinence Questionnaire Short-Form, and the Barthel Index. A total of 551 participants aged ≥75 years residing in Changsha city were enrolled from June to December 2018. The UI prevalence rate among nursing home residents aged ≥75 years was 24.3%. The most frequent subtype was mixed (M) UI (38.1%), followed by urge (U) UI (35.1%), stress (S) UI (11.9%), and other types (14.9%). In terms of severity, 57.5% had moderate UI, while 35.1% had mild and 7.5% had severe UI. Constipation, immobility, wheelchair use, cardiovascular disease (CVD), and pelvic or spinal surgery were significant risk factors for UI. Participants with a history of surgery had higher risks of SUI (odds ratio [OR] = 4.87, 95% confidence interval [CI]: 1.55–15.30) and UUI (OR = 1.97, 95% CI: 1.05–3.71), those who were immobile or used a wheelchair had higher rates of MUI (OR = 11.07, 95% CI: 4.19–29.28; OR = 3.36, 95% CI: 1.16–9.78) and other UI types (OR = 7.89, 95% CI: 1.99–31.30; OR = 14.90, 95% CI: 4.88–45.50), those with CVD had a higher rate of UUI (OR = 2.25, 95% CI: 1.17–4.34), and those with diabetes had a higher risk of UUI (OR = 2.250, 95% CI: 1.14–4.44). Use of oral antithrombotic agents increased UUI risk (OR = 4.98, 95% CI: 2.10–11.85) whereas sedative hypnotic drug use was associated with a higher risk of MUI (OR = 3.62, 95% CI: 1.25–10.45). Each UI subtype has distinct risk factors, and elderly residents of nursing homes with a history of CVD and pelvic or spinal surgery who experience constipation should be closely monitored. Reducing time spent in bed and engaging in active rehabilitation including walking and muscle strengthening may aid in UI prevention and treatment.
Introduction
Urinary incontinence (UI) is defined by International Continence Society (ICS) as complaint of involuntary loss of urine (1). It's common in elderly patients and usually play a major role in independent person in the community or dependent person in the nursing home (2, 3). UI affects nearly 40% of women aged 80 years and older, 10–35% of older men, and up to 80% of long-term care residents and can severely impair an individual's quality of life (QoL) (4, 5) because of the associated hygiene and social problems (6). Therefore, healthcare providers need to demonstrate sensitivity in evaluating and discussing UI, particularly with older adults.
There are three major subtypes of UI—urge (U), stress (S), and mixed (M)—which have different risk factors and etiologies (7). UUI and SUI are the most common subtypes in older persons, while MUI is the combination of both types (8). UI is a risk factor for mortality in the elderly (9–11) and is closely related to declines in cognitive function and performance of activities of daily living (ADL) as well as age, obesity, diabetes, loss of independence, depression and anxiety levels, and agitation (8, 11–14). It is important to clarify the association between UI and cardiovascular risk factors through screening (14) to prevent the development of cardiovascular disease (CVD). However, there is little known about the prevalence of UI in the elderly population of China.
There are many factors that affect urinary incontinence in older adults, such as age, frailty, depression, neurologic conditions, cognitive impairment, mobility impairment, lower urinary tract symptoms (15–18), race, education, hypertension, smoking, diabetes, increased parity, higher body mass index, and oral hormone therapy, and radical prostatectomy for prostate cancer in men (15, 16, 19–21). However, in the very old population, whether there are more special factors of UI or not for this high-risk population, these are worthy of our consideration.
The aims of this study was to determine the prevalence of UI in the very old population (aged ≥ 75 years old) in nursing homes, examine potential risk factors associated with UI and its subtypes, which may provide evidence for further development of UI strategies for this high-risk populations.
Materials and Methods
Study Design
This nursing institution-based cross-sectional study was carried out with face-to-face surveys conducted between June and December 2018 among older adults residing in Changsha city, the capital of Hunan province, China. Changsha is located in the east of Hunan, with an area of 11,819.5 km2. Changsha comprises Furong, Tianxin, Yuelu, Kaifu, Yuhua, and Wangcheng districts; Changsha and Ningxiang counties; and Liuyang city. The study involved 20 of the 83 nursing homes in Changsha, with over 551 nursing home residents enrolled.
Study Population
Older adults ≥75 years old who had resided for a minimum of 1 year in the study area with normal cognition and communication ability were eligible to participate. Mentally unstable nursing home residents with life-threatening diseases were excluded. The study was approved by the Medical Ethics Committee of Central South University. Written informed consent to participate in the study was provided by the participants or their legal guardian/next of kin.
Study Size
The sample size was calculated using the formula n = μα2π (1–π)/δ2, where α is 0.05; π is the prevalence rate of UI, which was taken to be 25.0% from a previous study (22); and δ is 0.15 π. Based on this calculation, the minimum sample size for this study was determined as 512.
Survey Instrument
A questionnaire for collecting data on general characteristics was used in the face-to-face interview. The data included age, nationality, marital status, occupation, source of income, education level, and medical history, among other characteristics. Height and weight were measured with the same ruler and electronic scales for each participant.
UI was assessed using the International Consultation Incontinence Questionnaire—Short Form (ICIQ-SF), which continues to be the most internationally used questionnaire and has been translated into over 60 languages (23). It comprises three scored items and an unscored self-diagnosis item to determine the prevalence, frequency, and severity of urinary leakage and its impact on QoL (24). The sum of scores for the three items ranging from 0 to 21, and higher scores indicating increased UI severity and greater impact on QoL. The scale has demonstrated high internal reliability in British patients at a urology clinic and in a community-based study (Cronbach's α = 0.95) (24, 25). Mild UI was defined as < 7 points; moderate UI as 7–14 points; and severe UI as >14 points.
ADL performance was significantly associated with UI (12), the Barthel Index (BI) was used to assess each individual's ADL performance (Cronbach's α = 0.93) (12). This 100-point clinical rating index includes 10 items related to self-care ability (i.e., bowels, bladder, grooming, toilet use, feeding, dressing, and bathing) and mobility (i.e., transfer, mobility, and stairs), with a higher score indicating a lower level of physical dependence. The Barthel index scores are classified as follows: 0–20 points: total dependency; 21–60 points: high-level dependency; 61–90 points: mid-level dependency; 91–99 points: low-level dependency; 100 points: total independence (26).
Data Analysis
EpiData v3.1 (https://www.epidata.dk/index.htm) and SPSS v25.0 (IBM Corp., Armonk, NY, USA) were used for data management and analysis, respectively. Numerical variables are expressed as the mean ± standard deviation (SD) and categorical variables as frequency and percentage. Differences in frequency distributions between groups were assessed with Pearson χ2 tests, and determinants of UI and its subtypes were assessed using binary logistic regression (LR) models. For all tests, 2-tailed p < 0.05 were considered statistically significant.
Results
General Characteristics of Older Adults in Nursing Homes
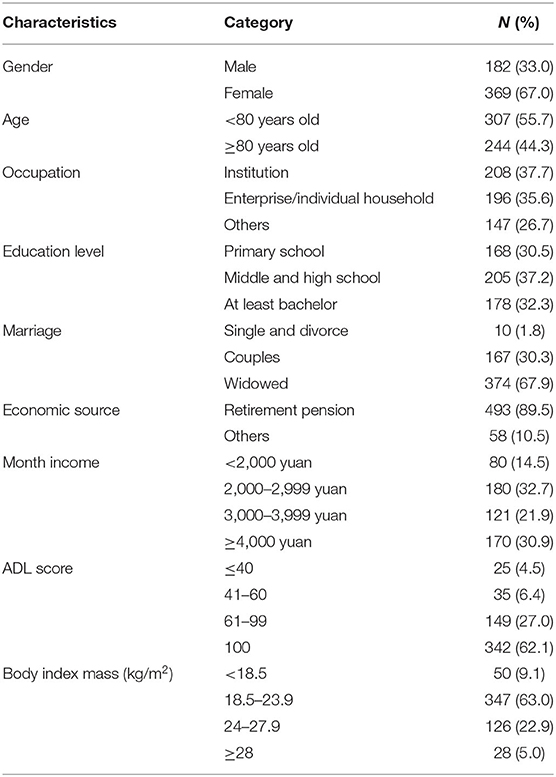
Of the 551 study participants, 67.0% were female; 55.7% were 70–79 years old, 44.3% were >80 years old, and the mean age (±SD) was 84.16 (±4.84) years. In terms of education level, 37.2% of participants had completed middle or high school and almost 40% had >40 years of work experience. Most participants had been married; 30.5% were still married and 67.9% were widowed. In most cases, the source of income was retirement pension (89.5%), and only 14.5% of participants had a monthly income <2,000 yuan. In terms of functional status, 62.1% of participants were fully independent in ADL as measured by BI; 6.4% were impaired, and 4.5% were disabled. Based on body mass index (BMI), 22.9% of participants were overweight and 5.1% were obese (BMI ≥ 28 kg/m2) (Table 1).
UI Prevalence in the Geriatric Population of Nursing Homes
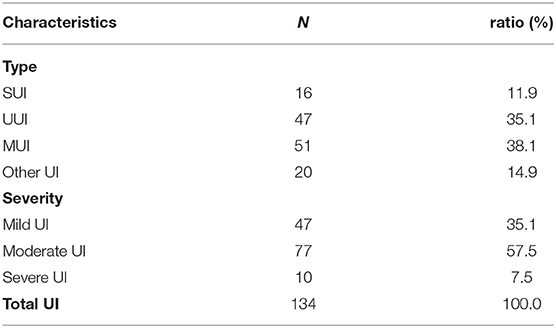
We found 134 UI in all 551 participants, with a UI prevalence rate of 24.3%. Of which MUI accounted to 38.1%; UUI 35.1%; SUI 11.9%; and other types 14.9%; 57.5% of UI was moderate UI, 35.1 % was mild UI, and 7.5% had severe UI (Table 2).
General Characteristics of UI in the Geriatric Population
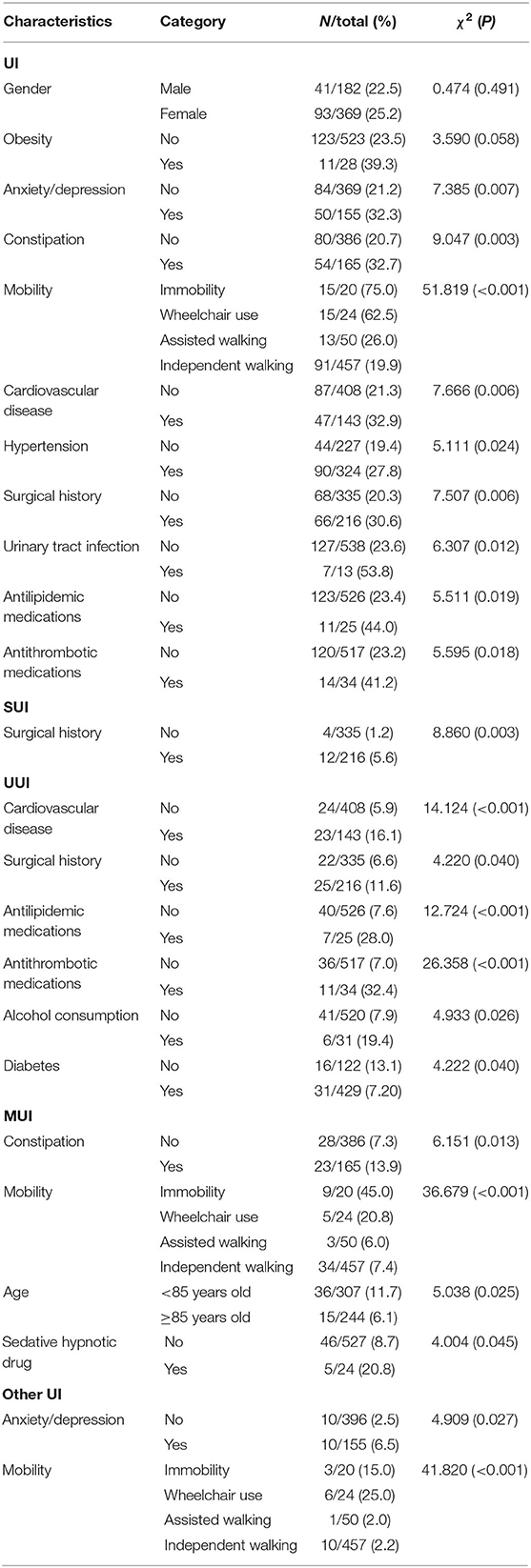
There was no difference in UI prevalence between males (22.5%) and females (25.2%) or between obese (23.5%) and non-obese (39.3%) participants. Anxiety and depression were associated with higher rates of UI (32.3%, χ2 = 7.39, p = 0.007) and other types of UI (6.5%, χ2 = 4.91, p = 0.027). In terms of functional status, immobile participants had a higher frequency of UI and MUI (75.0%, 45.0%), whereas those who could walk independently had a low rate of UI (19.9%) (χ2 = 51.82, p < 0.001). Mobility was a strong predictor of MUI and other UI types (χ2 = 36.68, p < 0.001, χ2 = 41.82, p < 0.001). Participants with a history of hypertension or urinary tract infection (UTI) had a higher rates of UI than those without this medical history (hypertension: 27.8% vs. 19.4%, χ2 = 5.11, p = 0.024; UTI: 53.8% vs. 23.6%, χ2 = 6.31, p = 0.012). Participants with constipation had higher rates of UI and MUI than those without constipation (UI: 32.7% vs. 20.7%, χ2 = 6.31, p = 0.012; MUI: 13.9% vs. 7.3%, χ2 = 6.15, p = 0.013). Participants with a history of CVD had a higher rate of UI and UUI (UI: 32.9% vs. 21.3%, χ2 = 7.67, p = 0.006; UUI: 16.1% vs. 5.9%, χ2 = 14.12, p < 0.001) and those with a history of surgery had a higher rate of UI (30.6% vs. 20.3%, χ2 = 7.51, p = 0.006), SUI (5.6% vs. 1.2%, χ2 = 8.86, p = 0.003), and UUI (11.6%, χ2 = 4.22, p = 0.040) than those without these in their medical history. Finally, participants who were taking oral antilipidemic and antithrombotic medications had higher rates of UI than those who were not taking these drugs (antilipidemics: 44.0%, χ2 = 5.51, p = 0.019; antithrombotics: 44.1%, χ2 = 5.60, p = 0.018) (Table 3).
Factors Associated With UI and Its Subtypes
Binary LR was carried out to evaluate the association between UI, SUI, and other types of UI (dependent variable, dichotomized into UI vs. no UI, SUI vs. no SUI, and other UI vs. no other UI) and general characteristics of UI (covariates: anxiety/depression, constipation, mobility, CVD, hypertension, history of surgery, UTI, antilipidemic and antithrombotic medications). UI-related characteristics that were significant on Pearson χ2 tests were entered into the LR model by backward stepwise regression, with mobility as the last categorical covariate (independent walking; α In = 0.05, α Out = 0.10).
Binary LR was used to assess the independent association between UUI (dependent variable, dichotomized into UUI vs. no UUI) and general characteristics of UI and MUI (covariates: anxiety/depression, constipation, mobility, CVD, hypertension, history of surgery, UTI, antilipidemic and antithrombotic medicines, alcohol consumption, and diabetes). All UI- and UUI-related characteristics that were significant in Pearson χ2 tests were entered into model by backward stepwise regression, with mobility as the last categorical covariate (independent walk; probability for stepwise entry = 0.05, removal = 0.10). The binary LR model was used to assess the independent association between MUI (dependent variable, dichotomized into MUI vs. no MUI) and general characteristics of MUI (covariates: anxiety/depression, constipation, mobility, CVD, hypertension, surgical history, UTI, antilipidemic and antithrombotic medicines, age, and sedative/hypnotic drugs). All UI- and MUI-related characteristics that were significant in Pearson χ2 tests were entered into the model by backward stepwise regression, with mobility as the last categorical covariate (independent walking; probability for stepwise entry = 0.05, removal = 0.10). The multivariate-adjusted odds ratios (ORs) and their 95% confidence intervals (CIs) and p-values were calculated. All analyses met the goodness-of-fit criterion as determined with the Hosmer–Lemeshow tests.
The results showed that constipation, immobility, wheelchair use, CVD, and history of surgery were significant risk factors for UI (Table 3). Participants with a history of surgery had a higher risk of SUI (OR = 4.87, 95% CI: 1.55–15.30) and UUI (OR = 1.97, 95% CI: 1.05–3.71), and immobile and wheelchair-assisted older adults had a higher frequency of MUI (OR = 11.07, 95% CI: 4.19–29.28; OR = 3.36, 95% CI: 1.16–9.78) and other types of UI (OR = 7.89, 95% CI: 1.99–31.30; OR = 14.90, 95% CI: 4.88–45.50). Compared to participants with no history of CVD, those with CVD history reported a higher frequency of UUI (OR = 2.25, 95% CI: 1.17–4.34). Participants with diabetes were more likely to experience UUI than those without diabetes (OR = 2.250, 95% CI: 1.14–4.44). Use of oral antithrombotic drugs was associated with a higher risk for UUI (OR = 4.98, 95% CI: 2.10–11.85), and a history of sedative hypnotic drug use was associated with a higher risk of MUI (OR = 3.62, 95% CI: 1.25–10.45) (Table 4).
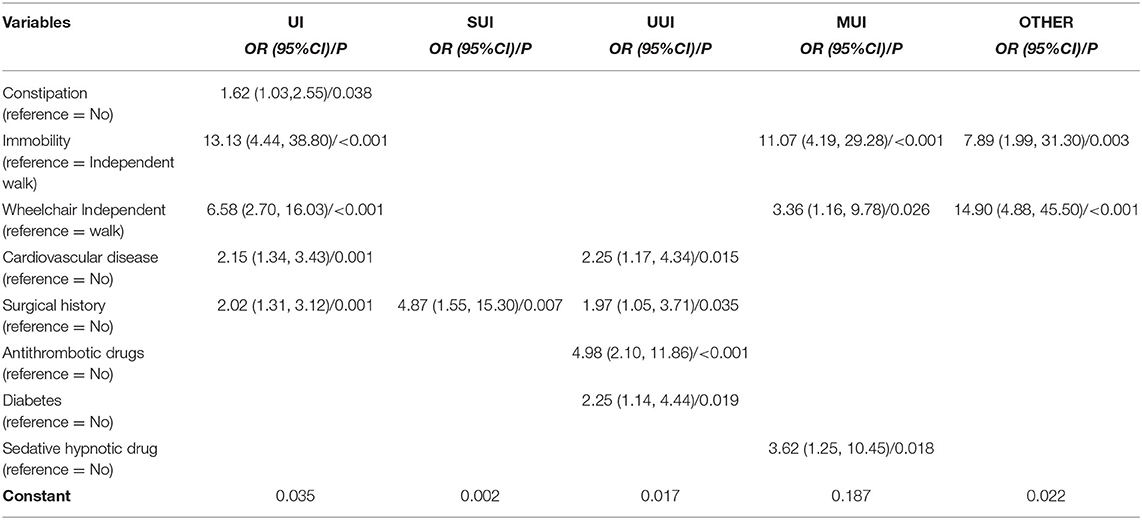
Table 4. Multivariate logistic regression model with UI and subtypes in the geriatric population of nursing homes.
Discussion
In this study, the UI prevalence of nursing home residents aged ≥75 years was 24.3%, which is lower than that reported in other studies of individuals aged ≥65 years (4, 22). General good health, consciousness, and good cognitive ability may explain the lower rate in our cohort. Our results showed that CVD was a risk factor for UI and UUI, which was in line with previous findings that UI had a high prevalence among heart failure patients (27, 28). As bladder function is affected by many cardiovascular risk factors, UI is a possible consequence of metabolic syndrome (14). Water–sodium retention and impaired bladder function are associated with CVD, while diuretics used in CVD treatment may lead to nocturia and increase the occurrence of UI (29). Despite patients' perception that diuretics are unpleasant and make it difficult for them to leave their home, patients in one study were generally compliant with their medication regime; nonetheless, nearly half experienced urine leakage, and most found urgency and incontinence bothersome (28). The assessment and management of UI or UUI in patients with CVD warrant further exploration.
The relationship between mobility in ADL and UI and its subtypes was evaluated based on immobility, wheelchair dependence, and assisted and independent walking. Immobility and wheelchair dependence were found to be risk factors for UI, MUI, and other UI types in the study participants, which is in accordance with earlier observations (29, 30). The use of walking aids and activity training may reduce or prevent the occurrence of UI in the elderly (30, 31); thus, promoting walking ability may be effective in preventing UI in nursing home residents.
Constipation has been shown to increase the risk of UI in the elderly (29, 32), which is consistent with our findings. The anatomy and angle of the urethra may be altered with chronic constipation, leading to problems such as overactive bladder (OAB), urinary retention, and UI (32, 33); conversely, treatment of constipation may prevent UI.
In contrast to a previous study (34), we found no relationship between diabetes and UI in older adults; however, diabetes can lead to glycosuria and has been shown to be associated with UUI risk in multiple models. In one study, diabetes was associated with increased urination frequency and urine volume and thereby exacerbated UI and OAB by osmotic diuresis (35). Thus, stabilizing blood glucose level is a potential strategy for preventing UUI.
A history of pelvic or spinal surgery was an independent risk factor for UI and two subtypes (SUI and UUI). Damage to nerves or connective tissues near or in the bladder can occur during surgery (29), and radical pelvic dissection can result in direct and indirect injury to the pelvic plexuses, resulting in SUI and UUI (36). UI prevalence was reported to be higher among patients who had undergone spinal surgery (37).
Sedative hypnotic and antithrombotic drug use was identified as a determinant of MUI risk in our cohort. Insomnia is among the most common sleep disorders in the geriatric population (38), and the use of nighttime sedatives in this group may lead to nocturnal enuresis by inducing a deep sleep from which an individual fails to awaken in order to void (36). Antithrombotic drugs that inhibit platelet or coagulation factors are commonly prescribed drugs for preventing and treating cardiovascular disorder (39). Repeated low doses of aspirin can block arachidonic acid receptors and inhibit thromboxane A2 production by acetylating a serine residue near the narrow catalytic site of the cyclooxygenase (COX)-1 channel (40); and high doses of aspirin inhibit both COX-1 and COX-2, which have anti-inflammatory and analgesic effects (41). Oral aspirin potentially inhibits COX and decreases prostaglandin (PGE)2, a regulator of inflammation and metabolism (42) that acts through the G protein-coupled PGE2 receptors (EP) 1, EP2, EP3, and EP4. EP1 and EP3 activation in the detrusor muscle of the bladder induces muscle contraction, whereas EP4 activation causes muscle relaxation (43). Aspirin may target EP1, EP2, EP3, and EP4 to reduce bladder sphincter contraction and detrusor relaxation, leading to involuntary urine leakage, although the precise underlying mechanism remains to be determined.
Obesity was not a significant risk factor for UI in our cohort in the binary LR model, which is inconsistent with previous findings (14, 44). Obesity was previously reported as a risk factor for UI, although the observed trends are contradictory, with decreased SUI and increased MUI rates found to be associated with higher BMI (44). Older males with a reduction in strength but not increases in body or fat mass were linked to an increased frequency of UI (45). Changes in body composition including an increase and redistribution of fat mass occur in old age, and current BMI classification may not accurately reflect the associated physical risks in the elderly, who may require age-specific BMI cut-off points (46). Thus, BMI in itself should not be considered as an independent predictor of UI in the geriatric population but should be considered in the context of fat mass, muscle strength, or other indicators.
Conclusion
In this study, we found that distinct factors contribute to the risk of different UI subtypes. Our results indicate that care providers in nursing homes should pay particular attention to residents with a history of CVD and pelvic or spinal surgery who are at risk of UI and may benefit from the treatment of constipation, less time spent in bed, and active training in walking and muscle strengthening. Further study is needed into the relationship between the use of antithrombotic drugs and UI, and age-specific BMI cut-off points in the elderly population must be established to determine how these factors influence UI risk.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Medical Ethics Committee of Zhejiang Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
HTan and HTai designed the study. SL and HW performed the experiments. HTai wrote the manuscript and analyzed the data. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by National key research and development plan named Research on the construction and evaluation of a comprehensive demonstration base for prevention and control of elderly syndrome (2020YFC2008606) and Nursing Research Fund of the Second Xiangya Hospital in 2018 (2018-YHL-33).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. D'Ancona C, Haylen B, Oelke M, Abranches-Monteiro L, Arnold E, Goldman H, et al. The International Continence Society (ICS) report on the terminology for adult male lower urinary tract and pelvic floor symptoms and dysfunction. Neurourol Urodyn. (2019) 38:433–77. doi: 10.1002/nau.23897
2. Chutka DS, Fleming KC, Evans MP, Evans JM, Andrews KL. Urinary incontinence in the elderly population. Mayo Clin Proc. (1996) 71:93–101. doi: 10.4065/71.1.93
3. Acharya S, Ghimire S, Jeffers EM, Shrestha N. Health care utilization and health care expenditure of Nepali older adults. Front Public Health. (2019) 7:24. doi: 10.3389/fpubh.2019.00024
4. Vaughan CP, Markland AD, Smith PP, Burgio KL, Kuchel GA. Report and research agenda of the American geriatrics society and national institute on aging bedside-to-bench conference on urinary incontinence in older adults: a translational research agenda for a complex geriatric syndrome. J Am Geriatr Soc. (2018) 66:773–82. doi: 10.1111/jgs.15157
5. Troko J, Bach F, Toozs-Hobson P. Predicting urinary incontinence in women in later life: A systematic review. Maturitas. (2016) 94:110–6. doi: 10.1016/j.maturitas.2016.09.006
6. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. Standardisation Sub-committee of the International Continence Society. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. (2002) 21:167–78. doi: 10.1002/nau.10052
7. Fong E, Nitti VW. Urinary incontinence. Prim Care. (2010) 37:599–612. doi: 10.1016/j.pop.2010.04.008
8. Minassian VA, Drutz HP, Al-Badr A. Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet. (2003) 82:327–38. doi: 10.1016/s0020-7292(03)00220-0
9. Taufik Ramli MH, Lodz NA, Abdul Aziz FA, Maw Pin T, Alias N, Abdul Mutalip MH, et al. Relationship between urinary incontinence and quality of life of older persons in Malaysia. Geriatr Gerontol Int. (2020) 20:38–42. doi: 10.1111/ggi.14028
10. Damián J, Pastor-Barriuso R, García López FJ, de Pedro-Cuesta J. Urinary incontinence and mortality among older adults residing in care homes. J Adv Nurs. (2017) 73:688–99. doi: 10.1111/jan.13170
11. Yoshioka T, Kamitani T, Omae K, Shimizu S, Fukuhara S, Yamamoto Y. Urgency urinary incontinence, loss of independence, and increased mortality in older adults: A cohort study. PLoS ONE. (2021) 16:e0245724. doi: 10.1371/journal.pone.0245724
12. Li HC, Chen KM, Hsu HF. Modelling factors of urinary incontinence in institutional older adults with dementia. J Clin Nurs. (2019) 28:4504–12. doi: 10.1111/jocn.15039
13. Cheng S, Lin D, Hu T, Cao L, Liao H, Mou X, et al. Association of urinary incontinence and depression or anxiety: A meta-analysis. J Int Med Res. (2020) 48:300060520931348. doi: 10.1177/0300060520931348
14. John G. Urinary incontinence and cardiovascular disease: A narrative review. Int Urogynecol J. (2020) 31:857–63. doi: 10.1007/s00192-019-04058-w
15. Vaughan CP, Goode PS, Burgio KL, Markland AD. Urinary incontinence in older adults. Mt Sinai J Med. (2011) 78:558–70. doi: 10.1002/msj.20276
16. Offermans MP, Du Moulin MF, Hamers JP, Dassen T, Halfens RJ. Prevalence of urinary incontinence and associated risk factors in nursing home residents: a systematic review. Neurourol Urodyn. (2009) 28:288–94. doi: 10.1002/nau.20668
17. Skelly J, Flint AJ. Urinary incontinence associated with dementia. J Am Geriatr Soc. (1995) 43:286–94. doi: 10.1111/j.1532-5415.1995.tb07341.x
18. Bogren MA, Hvarfwén E, Fridlund B. Urinary incontinence among a 65-year old Swedish population: medical history and psychosocial consequences. Vard Nord Utveckl Forsk. (1997) 17:21–4. doi: 10.1177/010740839701700304
19. Veronese N, Soysal P, Stubbs B, Marengoni A, Demurtas J, Maggi S, et al. Association between urinary incontinence and frailty: a systematic review and meta-analysis. Eur Geriatr Med. (2018) 9:571–78. doi: 10.1007/s41999-018-0102-y
20. Batmani S, Jalali R, Mohammadi M, Bokaee S. Prevalence and factors related to urinary incontinence in older adults women worldwide: a comprehensive systematic review and meta-analysis of observational studies. BMC Geriatr. (2021) 21:212. doi: 10.1186/s12877-021-02135-8
21. Zhou HH, Shu B, Liu TZ, Wang XH, Yang ZH, Guo YL. Association between parity and the risk for urinary incontinence in women: A meta-analysis of case-control and cohort studies. Medicine. (2018) 97:e11443. doi: 10.1097/MD.0000000000011443
22. Kim MS, Lee SH. Prevalence rate and associated factors of urinary incontinence among nursing home residents. Taehan Kanho Hakhoe Chi. (2008) 38:92–100. doi: 10.4040/jkan.2008.38.1.92
23. Uren AD, Cotterill N, Pardoe M, Abrams P. The International Consultation on Incontinence Questionnaires (ICIQ): An update on status and direction. Neurourol Urodyn. (2020) 39:1889–96. doi: 10.1002/nau.24437
24. Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. (2004) 23:322–30. doi: 10.1002/nau.20041
25. Slavin V, Gamble J, Creedy DK, Fenwick J. Perinatal incontinence: psychometric evaluation of the international consultation on incontinence questionnaire-urinary incontinence short form and wexner scale. Neurourol Urodyn. (2019) 38:2209–23. doi: 10.1002/nau.24121
26. Ozturk GZ, Egici MT, Bukhari MH, Toprak D. Association between body mass index and activities of daily living in homecare patients. Pak J Med Sci. (2017) 33:1479–84. doi: 10.12669/pjms.336.13748
27. Palmer MH, Hardin SR, Behrend C, Collins SK, Madigan CK, Carlson JR. Urinary incontinence and overactive bladder in patients with heart failure. J Urol. (2009) 182:196–202. doi: 10.1016/j.juro.2009.02.115
28. Poole K, Kerlin M, Wynne R. Prevalence and characteristics of urinary incontinence in a cohort of patients with chronic heart failure. Heart Lung. (2017) 46:67–73. doi: 10.1016/j.hrtlng.2017.01.002
29. Bardsley A. An overview of urinary incontinence. Br J Nurs. (2016) 25:S14–21. doi: 10.12968/bjon.2016.25.18.S14
30. Jachan DE, Müller-Werdan U, Lahmann NA. Impaired mobility and urinary incontinence in nursing home residents: A multicenter study. J Wound Ostomy Continence Nurs. (2019) 46:524–9. doi: 10.1097/WON.0000000000000580
31. Sackley CM, Rodriguez NA, van den Berg M, Badger F, Wright C, Besemer J, et al. A phase II exploratory cluster randomized controlled trial of a group mobility training and staff education intervention to promote urinary continence in UK care homes. Clin Rehabil. (2008) 22:714–21. doi: 10.1177/0269215508089058
32. Eshkoor SA, Hamid TA, Shahar S, Mun CY. Factors related to urinary incontinence among the Malaysian elderly. J Nutr Health Aging. (2017) 21:220–6. doi: 10.1007/s12603-016-0779-x
33. Lian WQ, Li FJ, Huang HX, Zheng YQ, Chen LH. Constipation and risk of urinary incontinence in women: A meta-analysis. Int Urogynecol J. (2019) 30:1629–34. doi: 10.1007/s00192-019-03941-w
34. Tamanini JTN, Pallone LV, Sartori MGF, Girão MJBC, Dos Santos JLF, de Oliveira Duarte YA, et al. A populational-based survey on the prevalence, incidence, and risk factors of urinary incontinence in older adults – results from the “SABE STUDY”. Neurourol Urodyn. (2018) 37:466–77. doi: 10.1002/nau.23331
35. Smith DB. Urinary incontinence and diabetes: A review. J Wound Ostomy Continence Nurs. (2006) 33:619–23. doi: 10.1097/00152192-200611000-00005
36. Bristow SE, Hilton P. Assessment and investigations for urinary incontinence. Baillieres Best Pract Res Clin Obstet Gynaecol. (2000) 14:227–49. doi: 10.1053/beog.1999.0073
37. Lieberman EG, Radoslovich S, Marshall LM, Yoo JU. Lower urinary tract symptoms and urinary bother are common in patients undergoing elective cervical spine surgery. Clin Orthop Relat Res. (2019) 477:872–8. doi: 10.1097/CORR.0000000000000666
38. Patel D, Steinberg J, Patel P. Insomnia in the elderly: A review. J Clin Sleep Med. (2018) 14:1017–24. doi: 10.5664/jcsm.7172
39. Mega JL, Simon T. Pharmacology of antithrombotic drugs: An assessment of oral antiplatelet and anticoagulant treatments. Lancet. (2015) 386:281–91. doi: 10.1016/S0140-6736(15)60243-4
40. Loll PJ, Picot D, Garavito RM. The structural basis of aspirin activity inferred from the crystal structure of inactivated prostaglandin H2 synthase. Nat Struct Biol. (1995) 2:637–43. doi: 10.1038/nsb0895-637
41. Born G, Patrono C. Antiplatelet drugs. Br J Pharmacol. (2006) 147:S241–51. doi: 10.1038/sj.bjp.0706401
42. Ratchford SM, Lavin KM, Perkins RK, Jemiolo B, Trappe SW, Trappe TA. Aspirin as a COX inhibitor and anti-inflammatory drug in human skeletal muscle. J Appl Physiol. (2017) 123:1610–6. doi: 10.1152/japplphysiol.01119.2016
43. Hou R, Yu Y, Jiang J. PGE2 receptors in detrusor muscle: Drugging the undruggable for urgency. Biochem Pharmacol. (2021) 184:114363. doi: 10.1016/j.bcp.2020.114363
44. Schreiber Pedersen L, Lose G, Høybye MT, Elsner S, Waldmann A, Rudnicki M. Prevalence of urinary incontinence among women and analysis of potential risk factors in Germany and Denmark. Acta Obstet Gynecol Scand. (2017) 96:939–48. doi: 10.1111/aogs.13149
45. Bauer SR, Grimes B, Suskind AM, Cawthon PM, Cummings S, Huang AJ, et al. Urinary incontinence and nocturia in older men: Associations with body mass, composition and strength in the Health ABC Study. J Urol. (2019) 202:1015–21. doi: 10.1097/JU.0000000000000378
Keywords: urinary incontinence, geriatric, older adult, elderly population, prevalence, risk factor, nursing home, subtype
Citation: Tai H, Liu S, Wang H and Tan H (2021) Determinants of Urinary Incontinence and Subtypes Among the Elderly in Nursing Homes. Front. Public Health 9:788642. doi: 10.3389/fpubh.2021.788642
Received: 03 October 2021; Accepted: 15 November 2021;
Published: 06 December 2021.
Edited by:
Miao Liu, Chinese PLA General Hospital, ChinaReviewed by:
Özge Öz Yildirim, Ondokuz Mayis University, TurkeyLin Xu, Sun Yat-sen University, China
Copyright © 2021 Tai, Liu,Wang and Tan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haiqin Wang, d2FuZ2hhaXFpbjc3QGNzdS5lZHUuY24=; Hongzhuan Tan, dGFuaHo5OUBxcS5jb20=
 Hongyan Tai
Hongyan Tai Shunying Liu1
Shunying Liu1 Hongzhuan Tan
Hongzhuan Tan