- 1College of Geography and Environmental Sciences, Zhejiang Normal University, Jinhua, China
- 2College of Teacher Education, Zhejiang Normal University, Jinhua, China
- 3School of Geography and Environment, Jiangxi Normal University, Nanchang, China
Background: The COVID-19 pandemic has led to public health problems, including depression. There has been a significant increase in research on depression during the COVID-19 pandemic. However, little attention has been paid to the overall trend in this field based on bibliometric analyses.
Methods: Co-Occurrence (COOC) and VOSviewer bibliometric methods were utilized to analyze depression in COVID-19 literature in the core collection of the Web of Science (WOS). The overall characteristics of depression during COVID-19 were summarized by analyzing the number of published studies, keywords, institutions, and countries.
Results: A total of 9,694 English original research articles and reviews on depression during COVID-19 were included in this study. The United States, China, and the United Kingdom were the countries with the largest number of publications and had close cooperation with each other. Research institutions in each country were dominated by universities, with the University of Toronto being the most productive institution in the world. The most frequently published author was Ligang Zhang. Visualization analysis showed that influencing factors, adverse effects, and coping strategies were hotspots for research.
Conclusion: The results shed light on the burgeoning research on depression during COVID-19, particularly the relationship between depression and public health. In addition, future research on depression during COVID-19 should focus more on special groups and those at potential risk of depression in the general population, use more quantitative and qualitative studies combined with more attention to scale updates, and conduct longitudinal follow-ups of the outcomes of interventions. In conclusion, this study contributes to a more comprehensive view of the development of depression during COVID-19 and suggests a theoretical basis for future research on public health.
Introduction
The COVID-19 pandemic had a tremendous impact on humans, crippling daily life activities and posing a serious threat to human health, particularly regarding public mental health. The outbreak of the COVID-19 pandemic caused widespread mass panic. Meanwhile, the lockdown brought about by the COVID-19 outbreak has further triggered psychological stress among the public, including symptoms of depression, anxiety, and posttraumatic stress. For example, Wu et al. found that depression and anxiety rates were significantly higher among college students during the pandemic than before, due to factors such as being isolated at home, online learning stress, and conflict between parents and children (1). Socioeconomic instability, increased burden of living, social isolation, and unemployment were suicidal behavior triggers during the pandemic (2–4). Furthermore, fear of infection, unpredictability, and uncertainty of the COVID-19 pandemic were major stressors that triggered various mental health problems (5, 6). Thus, studying the public's mental state under the impact of a pandemic has become necessary.
The study of depression was an important area of research, even before the pandemic, focusing on depression measurement tools, influencing factors, and treatments. First, in its assessment, many researchers have developed appropriate scales, such as the Beck Depression Inventory and Montgomery Depression Test Scale. Second, regarding factors influencing the development of depression, psychosocial stress (7), patient status (8, 9), physical health status (10, 11), obesity (12), cross-cultural factors (13), and others play a role. Third, many scholars are still exploring treatments for depression, which can be divided into psychotherapy, pharmacotherapy, and other treatments (14, 15).
The relationship between depression and COVID-19 has received considerable attention in the face of sudden outbreaks. There are many theoretical and practical studies on depression during COVID-19, focusing on four aspects: the causes of depression during COVID-19, influencing factors, effects on people, and methods of alleviation. First, regarding its causes, several studies have concluded that the public's social activities were restricted due to pandemic prevention and control measures and that the masses were faced with a lack of exercise and unstable economic resources, in addition to the fear of infection (16, 17). For example, an online survey of 1,258 Italian residents revealed that social isolation during the pandemic had a significant psychosocial impact on people, especially those in vulnerable groups within the population (18). Second, various factors influenced depression during the COVID-19 pandemic. These factors can be divided into several categories: sex, age, occupation, and environmental factors, such as daily exercise. In a study involving 2,992 adults in China, depression rates were higher among men than women and higher among young adults than older adults (19). In addition to sex and age, several other factors contribute to depression. Some researchers have linked the emergence of psychological problems, such as depression, to professions (20–22). Third, depression during COVID-19 also affects public behaviors, such as insomnia (23, 24), alcohol abuse (25, 26) and irregular eating behaviors (27). Fourth, many scholars are currently seeking better ways to cope with the current trend of a high prevalence of psychological disorders, allowing for alleviation. Healthcare workers, for example, face heavy work pressure during the pandemic and usually have higher psychological stress and a higher prevalence of depression than the general population. In response, the mental burden on healthcare workers can be reduced by providing high-quality and transparent communication and accurate information updates to all staff, complete and high-quality personal protective equipment, and supplies to prevent infection (28).
This study applies an innovative approach to conducting literature reviews through systematic reviews with the support of COOC (29) and VOSviewer software, commonly used for bibliometric analysis. COOC is the most powerful bibliometrics and knowledge mapping software available, which eliminates duplication, clears multiple databases, and constructs multidimensional relationship matrices simply and efficiently (29–31). Similarly, VOSviewer is a scientific tool for creating web-based maps, visualizing and navigating them, and presenting large amounts of data in the form of knowledge maps (32). As a powerful tool for quantitatively assessing various parameters related to scientific literature published in a specific field, bibliometric analysis provides insights into popular research topics, trends, key researchers, and scientific institutions (33, 34). Several studies using bibliometric methods have been conducted in areas related to the COVID-19 pandemic. For example, Fan et al. (35) compared English and Chinese COVID-19 literature using bibliometric methods to summarize their differences and characteristics. Another study used a bibliometric approach to analyze literature related to the pediatric field during COVID-19 (36). During the last 3 years of the COVID-19 pandemic, while research in the depression-related field has evolved, the use of bibliometric methods to study this field remains incomplete (37–39).
This study provides a broad understanding of depression during COVID-19 and highlights key research topics to provide ideas for future research. It focuses on a systematic review of depression during COVID-19 using the bibliometric software COOC and VOSviewer, while considering and addressing the following questions: What are the research trends and evolutionary paths of depression during COVID-19? Which countries, authors, and institutions contributed the most to this research area? What are the research hotspots? What are the implications and limitations of this research? Considering the above, this study not only provides a deeper analysis of the literature in the field of depression during COVID-19 but also broadens the ideas for future research and provides a basis and reference for innovation in this field of research.
Data sources and research methods
Data sources
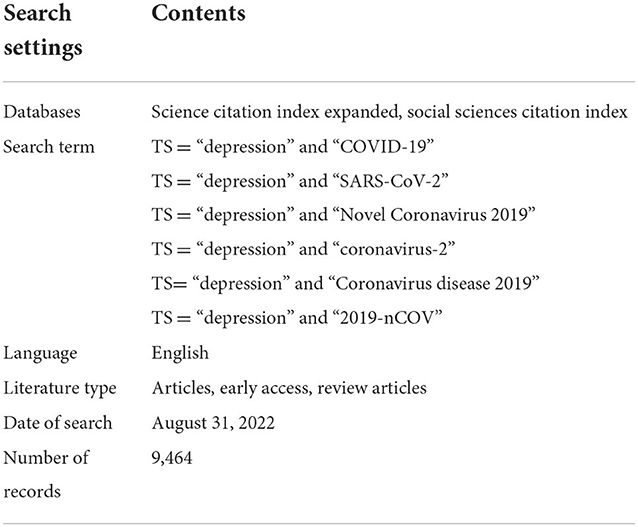
In this study, WOS was used as the literature information acquisition platform, and SSCI and SCIE in the core collection of WOS were used as data sources. A general search was selected, and the search conditions are shown in Table 1, with Articles, Early Access, and Review Articles selected as the literature types, and the search time range started in 2020 and ended on August 31, 2022, yielding 12,331 records. In addition, to ensure the integrity of literature retrieval, we extracted the corresponding terms from Medical Subject Headings (http://www.ncbi.nlm.nih.gov/mesh/). After merging the retrieved data with synonyms and removing duplicate and missing keyword documents, 9,464 valid records were obtained.
Research methods
Through the quantitative data analysis, bibliometrics summarizes and presents the developmental history and research hotspots of a given field. Correspondingly, based on bibliometrics, the analysis of scientific knowledge maps transforms complex knowledge from data mining and information processing into a visual knowledge map that assists scholars in scientifically obtaining the laws of dynamic development in relevant fields. Available software includes COOC, VOSviewer, CiteSpace, Bibexcel, and Bicomb. In this study, COOC and VOSviewer were mainly used, which were jointly developed by Academic Drip and the bibliometric team and are the most complete and relatively simple to operate in the bibliometric field. In addition, COOC can quickly construct relationship matrices and instantly derive matrix results such as word-part and dissimilarity matrices. More importantly, it can also pre-process data, such as batch merging synonyms and removing unnecessary words.
COOC does not currently allow for citation analysis; therefore, this study combined it with VOSviewer, developed in collaboration with Nees Jan van Eck and Ludo Waltman at Leiden University in the Netherlands, as a bibliometric analysis, and visualization tool based on a Java environment to further analyze the field of research on depression during COVID-19 (40). This is a powerful tool for “co-occurrence” network clustering and density analysis. In addition, while VOSviewer lacks data pre-processing and fast matrix generation functions compared to the COOC software, its powerful graphical presentation capabilities allow for better visualization of bibliographic relationships and provide an excellent operating environment for this study (40, 41).
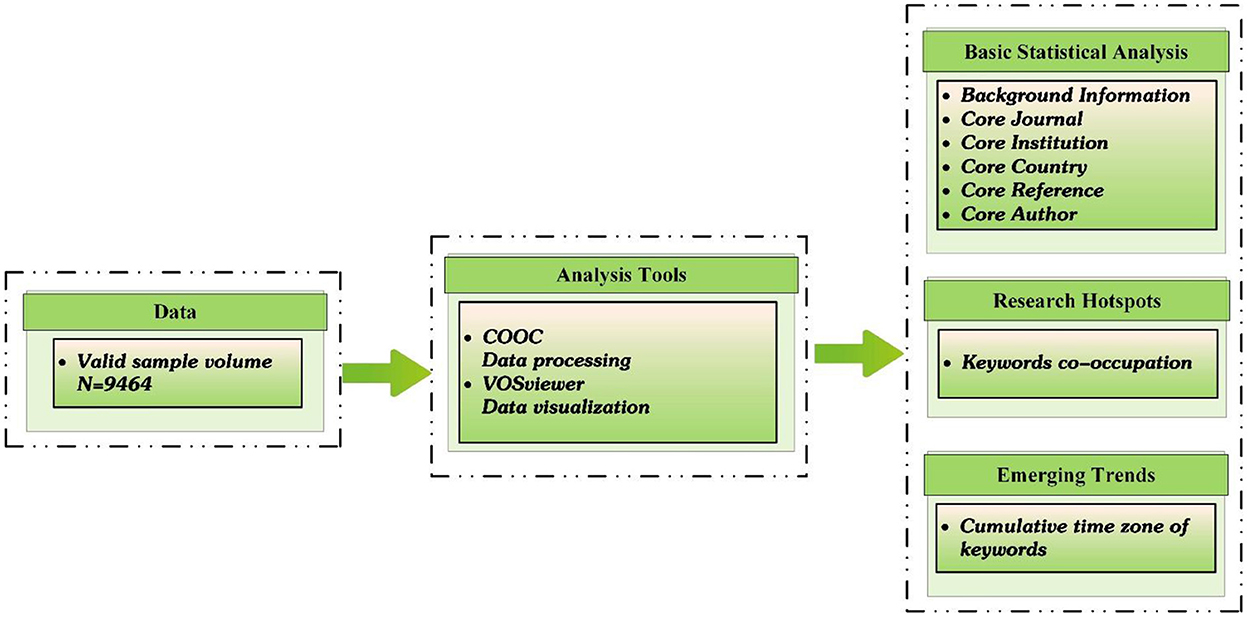
This study was based on the retrieved literature and utilized tools including COOC and VOSviewer for statistical analysis, information processing, and visual knowledge mapping to comprehensively grasp the research hotspots and dynamic change patterns of “depression during COVID-19.” COOC was used to create a cumulative time-zone map, while VOSviewer was used to create a co-occurrence map, as shown in Figure 1.
Results
Background information
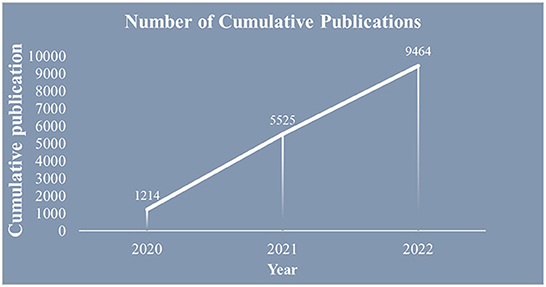
The statistics of the temporal distribution of the literature partially reflect the level of research and development in the field, as shown in Figure 2. Overall, the relevant research literature in this field started late; however, the number of publications is increasing. The COVID-19 pandemic started to spread at the end of 2019, and the number of related publications was 1,214 at the end of 2020. The cumulative number of publications reached 5,525 by 2021, with a rapid upward trend in annual publications. As of August 31, 2022, 9,464 articles had been published.
Importing the processed literature data in the COOC software yielded the top 10 countries with the highest number of publications from 2020 to 2022, as shown in Figure 3. Since 2020, there has been a gradual increase in research on depression during the COVID-19 pandemic. Articles published in 2020 were mainly from countries such as the United States, China, and Italy. As the COVID-19 epidemic continued to spread and worsen, the year 2021 witnessed a steady spurt of relevant literature, with 4,311 publications. Articles published in 2021 were mainly from the United States, China, the United Kingdom, Italy, Canada, and Spain. As of August 31, there were 3,939 articles published for 2022, mainly from the United States, China, and the United Kingdom.
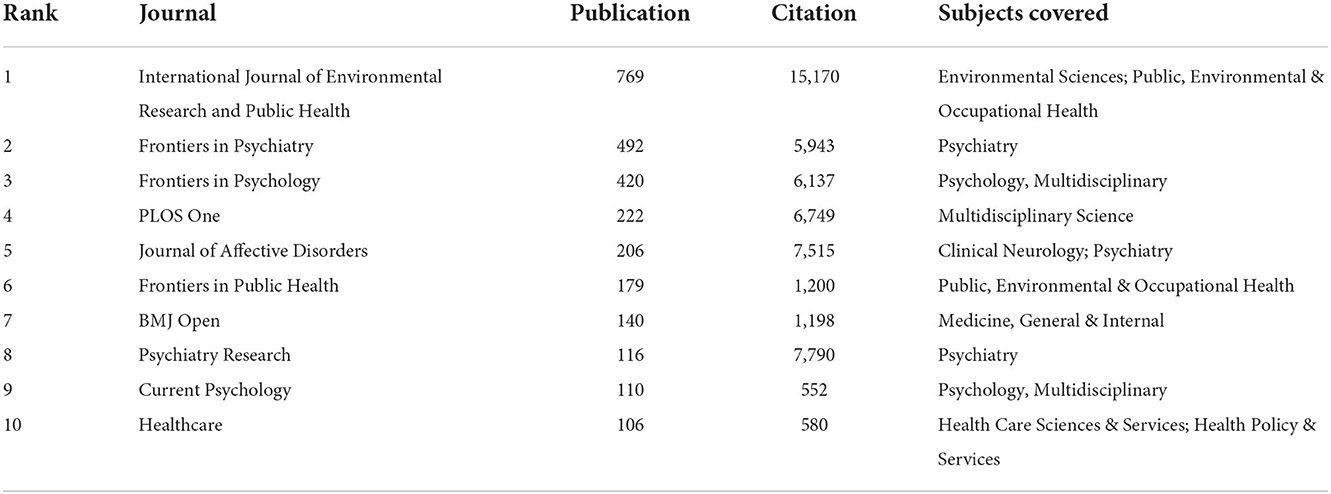
Core journal analysis
According to statistics, 1,727 journals are involved in depression during COVID-19 research publications at WOS, and the top 10 journals in terms of the number of articles published are shown in Table 2, accounting for 29.17% of the total literature volume. Journals with citations ≥2,924 are considered among the top 10 journals in terms of citations, while in Table 2, the International Journal of Environmental Research and Public Health, Frontiers in Psychiatry, Frontiers in Psychology, PLOS One, Journal of Affective Disorders, and Psychiatry Research are among the top 10 cited journals. These six journals can shed light specifically on research hotspots and evolutionary trends in the field of research on depression during COVID-19, which can provide direction and ideas for future research.
Statistics show that journals in the field of depression research during the COVID-19 pandemic focus on psychology, clinical practice, psychiatry, and others.
Core institution analysis
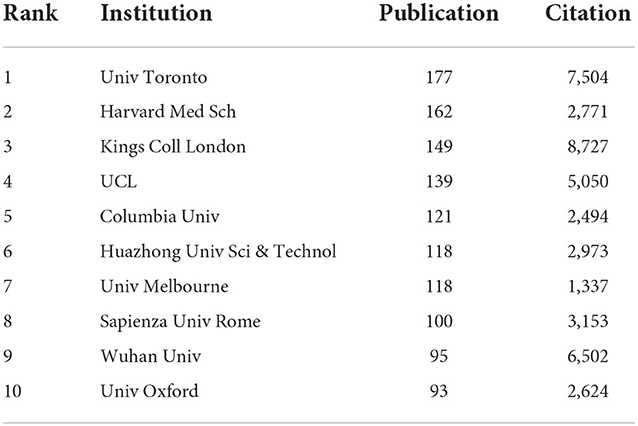
To further understand the cooperation relationship between institutions, the data were imported into VOSviewer by setting the frequency to be ≥40, and the remaining parameters to default, resulting in 83 institutional cooperation networks, as shown in Figure 4. As can be seen from the inter-institutional cooperation network diagram, cooperation between institutions is relatively close. Kings College London, University of Toronto, and Harvard Med School are at the center of the network.
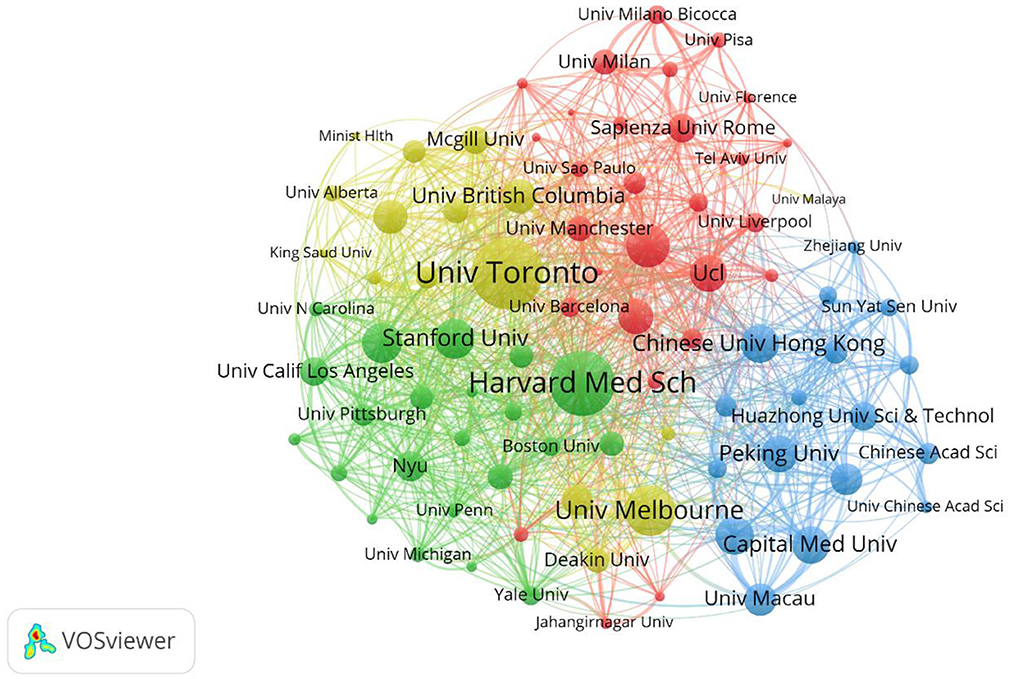
Figure 4. Map of institution network. The nodes represent institutions. The lines represent cooperation relationships.
Table 3 shows the top 10 institutions by number of publications, and the top 10 institutions had ≥3,880 citations. Statistics show that Kings College London, University of Toronto, Wuhan University, and University College London (UCL) are among the top 10 institutions regarding the number of published articles and citations. This shows that these four institutions are in a highly significant position in the field of depression during COVID-19 research and can lead future trends and hotspots in the field. From the institutional cooperation chart and the top 10 institutions ranking table, clearly the main force in research on depression during COVID-19 is major universities. Most of these universities are from the United States, China, and the United Kingdom, where universities are more active in the research field and the connections between universities from different countries are stronger.
Core country analysis
The number of publications in a country reflects the level of research and impact of the country in the relevant field. Table 4 lists the top 10 countries in terms of the number of publications on depression during COVID-19. As can be seen from Table 4, the United States had the highest number of publications (2,557 times), followed by China (1,535 times), the United Kingdom (1,289 times), Italy (806 times), Canada (636 times), Spain (588 times), Australia (523 times), Germany (480 times), Turkey (412 times), and Brazil (325 times). The United States, China, and the United Kingdom have accounted for more than 50% of the publications in this field and have made major contributions to research in this area.
The retrieved literature from 144 countries was imported into VOSviewer with the frequency set to 40, and the remaining parameters defaulted to obtain the cooperation network graph from 52 countries, as shown in Figure 5. The major research forces in this field are concentrated in the United States, China, the United Kingdom, Canada, Australia, Italy, and Spain. There are cooperative relationships among various countries, particularly the United States, with China and the United Kingdom having strong ties. Analyzing cooperative exchange relations between countries is conducive to further in-depth research on depression during the COVID-19 pandemic, which is an inevitable trend in research and development in this field.
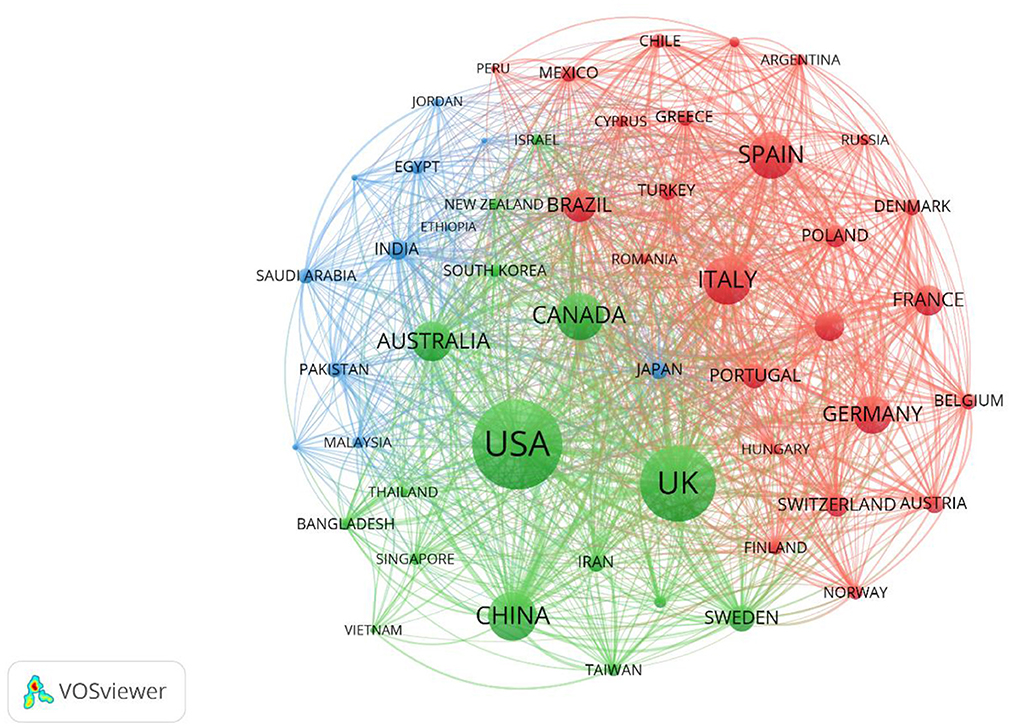
Figure 5. Map of countries network. The nodes represent countries. The lines represent cooperation relationships.
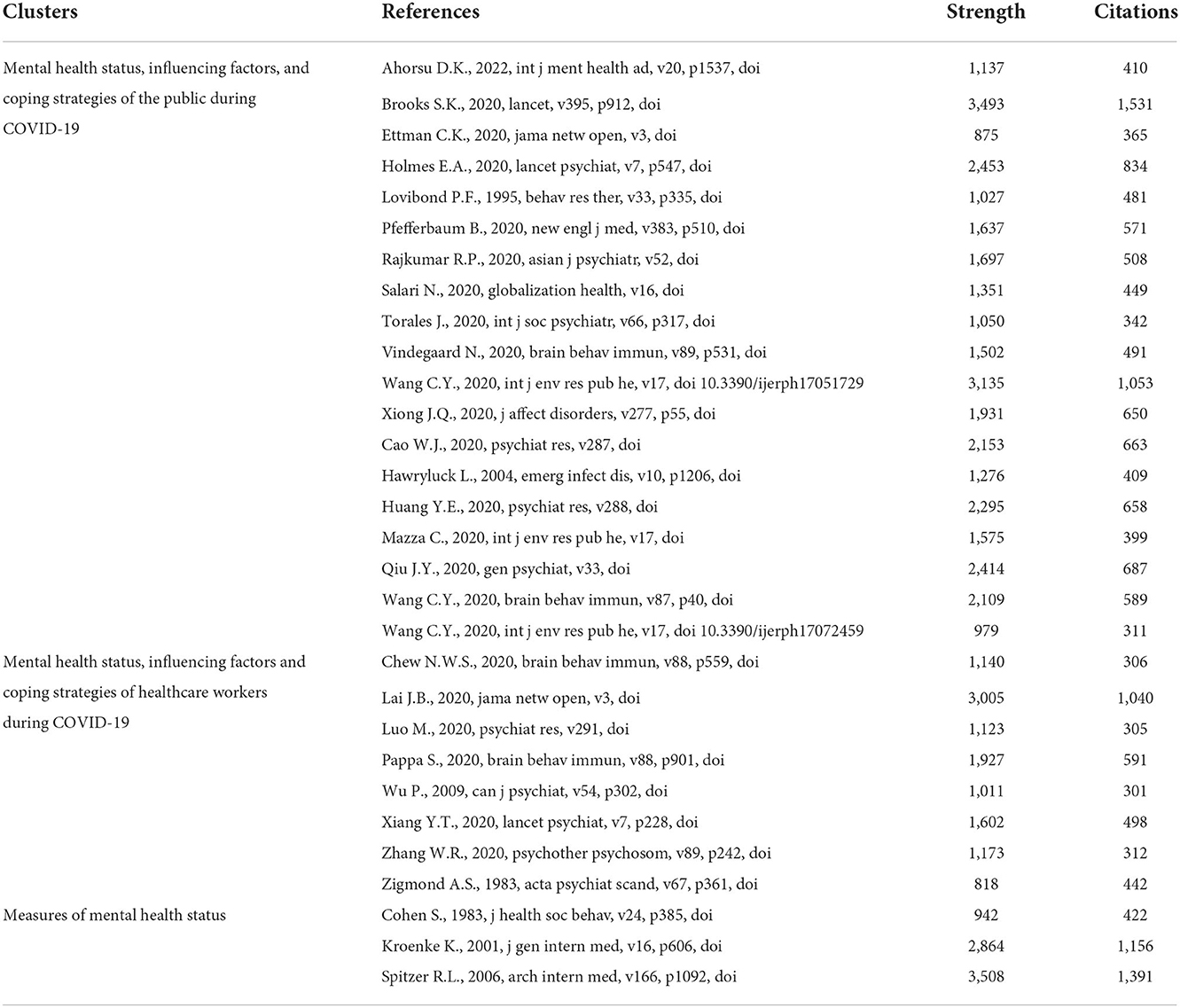
Core reference analysis
Citation analysis can reflect the structure of research and important literature in the field. To further understand the citation structure of the depression research field during COVID-19, this study analyzed the cited literature with critical reading and obtained three clusters. The required data were imported into VOSviewer, and the frequency was set to 300 to obtain the top 30 cited studies, as shown in Table 5. The most frequently cited references were Spitzer R. L. (published in 2006; cited 1391 times), Brooks S. K. (published in 2020; cited 1351 times), Kroenke K. (published in 2001; cited 1156 times), Wang C. Y. (published in 2020; cited 1053 times), Lai J.B. (published in 2020; cited 1040 times), and Holmes E.A. (published in 2020; cited 834 times).
In Figure 6, the 30 references were grouped into three categories, with each color representing a category. The references with high strength values in Table 5 represent important milestones in the field of depression research during COVID-19. The first milestone was to summarize the broad psychological impact of isolation measures and to consider how to reduce this impact (42). The second milestone was to study the mental health status of healthcare workers and its associated factors during COVID-19 (43). The third milestone was to develop a validated tool to screen for generalized anxiety disorder and assess its severity (44).
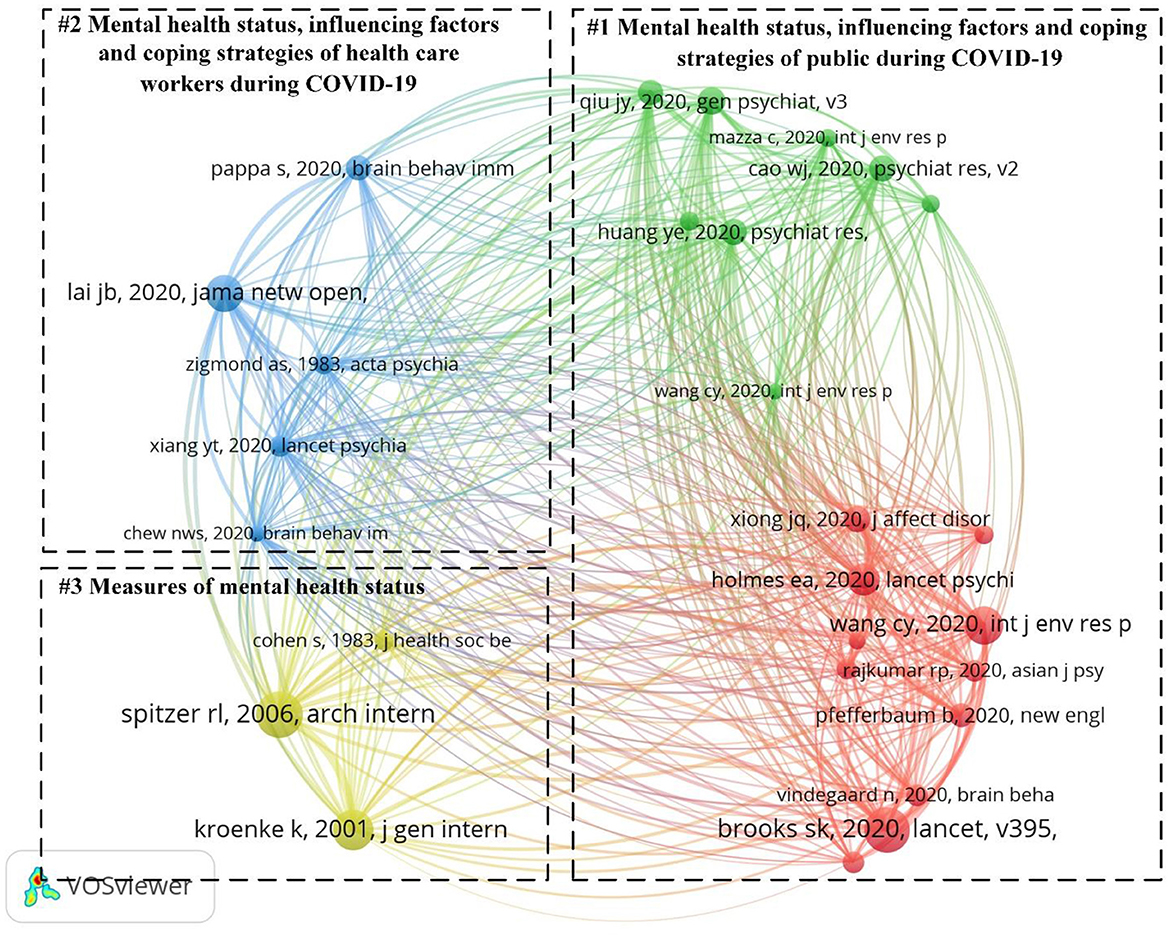
Figure 6. Map of references network. The nodes represent cited literature. The lines represent co-citation relationships. The green and red represent “Mental health status, influencing factors, and coping strategies of the public during COVID-19.” The blue represents “Mental health status, influencing factors and coping strategies of health care workers during COVID-19.” The yellow represents “Measures of mental health status.”
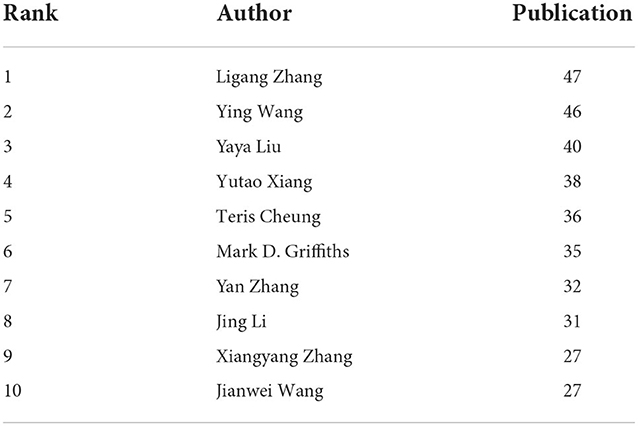
Core author analysis
The number of publications by an author reflects the author's degree of influence in the relevant field. Table 6 lists the top 10 authors who published articles on depression during the COVID-19 pandemic. The statistical analysis of the authors who published articles in the field of research on depression during COVID-19 was performed using VOSviewer, with the frequency set to 10 and other parameters defaulted, to generate an author collaboration network graph, as shown in Figure 7. The nodes in the graph represent the authors, the number of articles published by the author determines the size of the nodes and fonts, and the connecting lines between the nodes represent the existence of cooperative relationships between the nodes. Overall, author collaborations in this field show a cluster-like distribution. The largest number of authors was the author collaboration network formed by Jing Li, Ying Wang, and 55 other individuals.
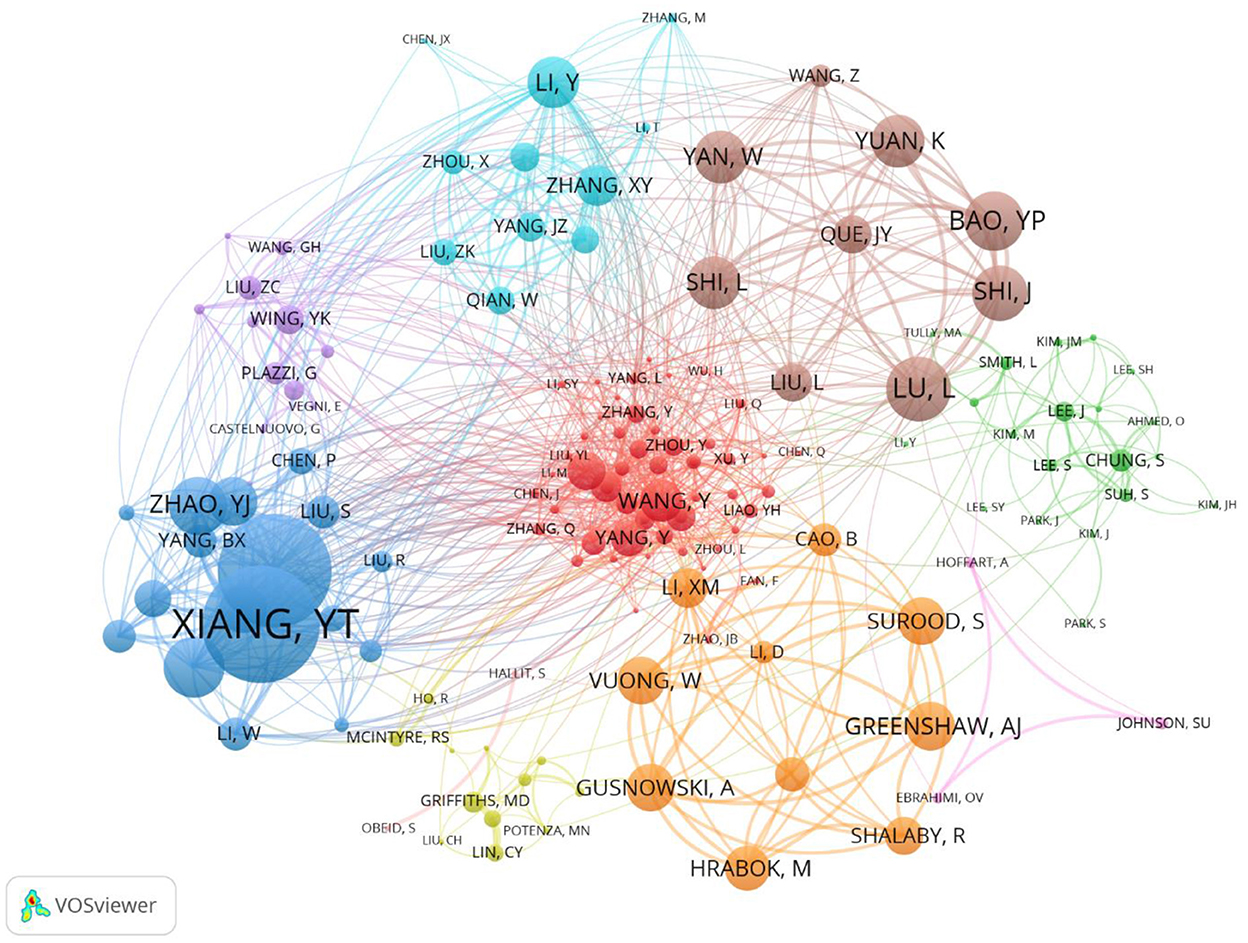
Figure 7. Map of co-authors network. The nodes represent authors. Node size indicates the number of articles produced. The lines represent cooperation relationships.
Research hotspots
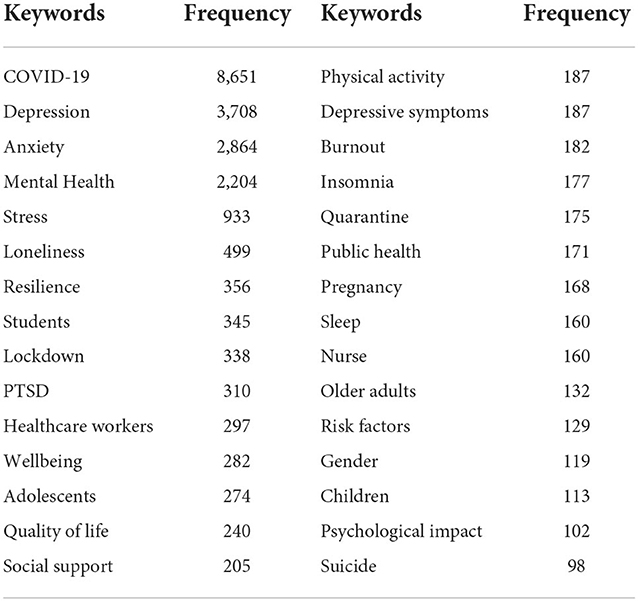
Keywords are the essence and distillation of the article's content, which can effectively reflect the research content, purpose, method, object, and results of the article and link them together to reveal the general lineage of the article. If a keyword appears frequently and repeatedly in a research field during a certain period, the research topic characterized by that keyword is considered the research hotspot of that research field. Table 7 lists the top 30 keywords related to the depression research field during the COVID-19 period, and the co-occurrence graph of keywords was obtained by importing the data into VOSviewer, as shown in Figure 8, the larger the corresponding font and node, the greater the weight of its keywords. The keywords “mental health,” “anxiety,” “lockdown,” and “adolescents” are important hotspots in depression-related fields during COVID-19. Through the analysis, the following three main categories of research hotspots on depression during COVID-19 were obtained.
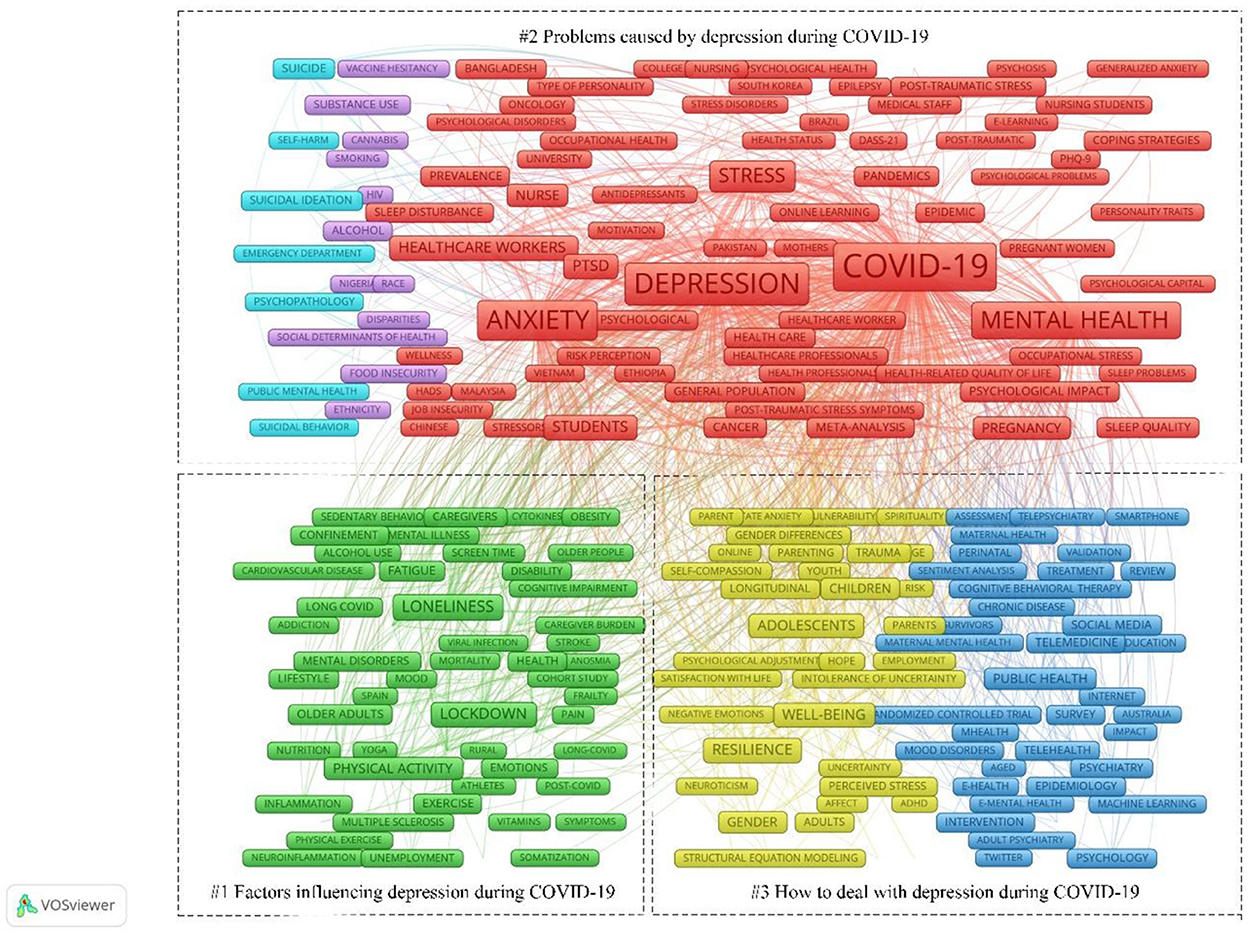
Figure 8. Map of keywords. The nodes represent keywords. The lines represent co-occurrence relationships. Green represents “Factors influencing depression during COVID-19.” Light blue, purple, and red represent “Problems caused by depression during COVID-19.” Dark blue and yellow represent “How to deal with depression during COVID-19.”
Factors influencing depression during COVID-19
High-frequency keywords included in the study's hotspots were lockdown (338 times), healthcare workers (297 times), physical Activity (187 times), burnout (182 times), older adults (132 times), gender (119 times), and unemployment (25 times). During the COVID-19 pandemic, the prevalence of mental illness was significantly higher than before the pandemic. Studies on the prevalence of depression during the pandemic have focused on factors that influence mental illness. Various analytical methods have been used to investigate this issue, and the following factors have been identified:
1. Quarantine policies enacted by governments during the COVID-19 pandemic reduced exercise time and social activities for the population in each country, and the lack of both activities was a significant factor in the elevated prevalence of mental illness in the population (45).
2. During the COVID-19 pandemic, most productive social activities were halted, and the country's population was left with unemployment and job insecurity (46, 47).
3. The sex, age, occupation, and social media use of residents influenced the development of mental illness (47–49).
Problems caused by depression during COVID-19
High-frequency keywords included in this research hotspot were PTSD (310 times), quality of life (240 times), insomnia (177 times), sleep (160 times), suicide (98 times), and alcohol (47 times). During the pandemic, mental illness has also caused problems such as insomnia, alcoholism, suicide, and smartphone addiction (50–52). These seriously affect the quality of life of people, especially adolescents (53); teenagers, college students, older adults (54); health care workers (55–57); and pregnant women (58, 59).
How to deal with depression during COVID-19
The high-frequency keywords included in this research hotspot were resilience (356 times), well-being (282 times), and social support (205 times). The increase in the prevalence of mental health problems, particularly depression, during the COVID-19 pandemic, cannot be ignored; therefore, how should this phenomenon be faced and what measures should be taken to prevent or alleviate it? Some scholars suggest that the phenomenon of “social isolation” caused by home isolation can be alleviated through digital media (60). Additionally, frontline healthcare workers should improve their subjective wellbeing and pay attention to their mental health status (61). For those who are already depressed, interventions to promote resilience should be provided whenever possible (62–64). In addition, authorities should provide adequate supplies to the population during the quarantine period and promote the benefits of public isolation to society.
Emerging trends
The cumulative time zones of the keywords were mapped using COOC, and Figure 9 shows the top 15 high-frequency keywords for 2020–2022. The graph provides an overall picture of changes in the study path (65–68). The size of the circles next to the keywords represents the number of keyword occurrences. The 2020 study concluded that the outbreak and prolonged isolation caused by the COVID-19 pandemic would affect public mental health, particularly the wellbeing of adolescents and healthcare workers, and emphasized that negative emotions should be alleviated through social support and improving psychological resilience. The 2021 study concluded that the duration of the COVID-19 pandemic was long. The 2022 study focused on the harm caused by depression during COVID-19, such as economic collapse, loss of fixed housing, brain fog, neuropsychiatric disorders, and collective trauma, as well as on coping strategies, including social interaction, social engagement, and good mood regulation strategies.
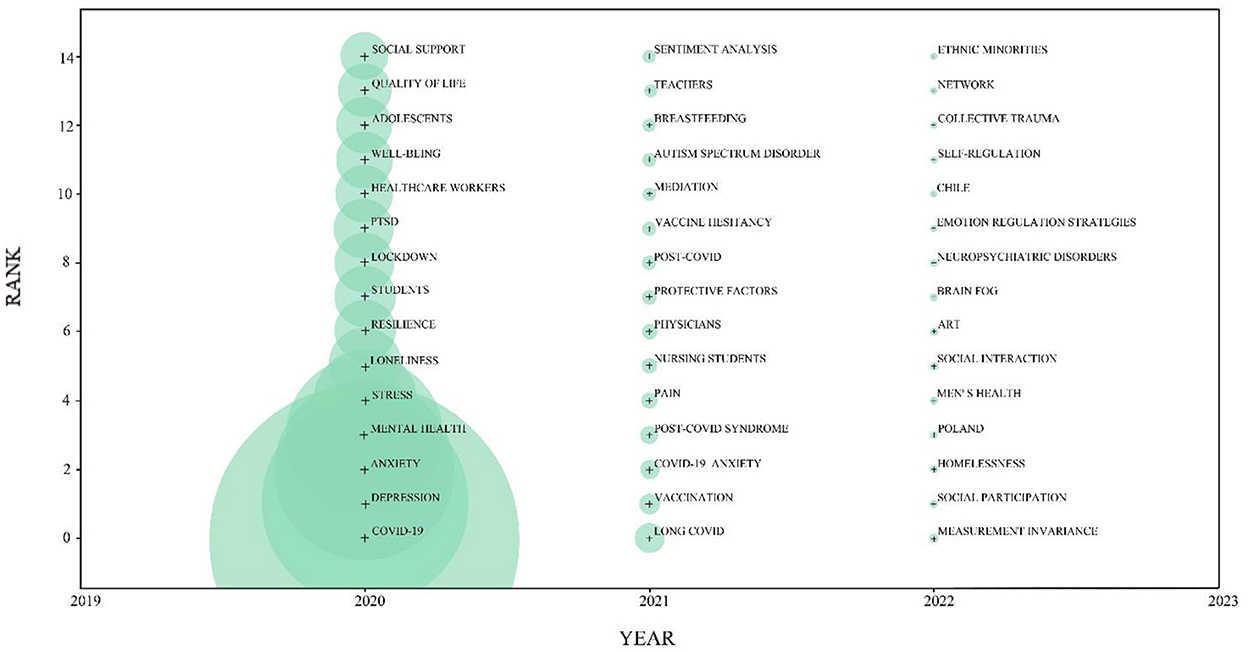
Figure 9. Emerging trends of research on depression during COVID-19. The nodes represent keywords. The node size indicates the number of keyword occurrences. The year corresponding to the node is the year in which the keyword first appeared.
Discussion
Discussion of the results
In this study, WOS was selected as a search platform for bibliometric analysis of publications, countries, institutions, and keyword counts in the field of depression during COVID-19 and for the presentation of scientific knowledge maps. Statistics show that the literature in this field peaked in 2021. In total, 144 countries, 48,103 authors, and 10,853 research institutions worldwide participated in this study. Of these, the United States, China, and the United Kingdom had the highest total number of publications and strong collaborative relationships, and the main research institutions in each country are universities. In addition, this study specifically focused on exploring the evolution of knowledge structures and research themes. Regarding the development of this study and its hotspot tracking, the important findings are as follows:
First, a general upward trend in research on depression during COVID-19 is evident in terms of research progress. Although this area has been studied for <3 years, it has received widespread attention worldwide due to its specificity. The number of publications in the field of depression during COVID-19 peaked in 2021, and related research in this field entered a period of rapid development. This may be because several studies have found significant changes in the frequency of public psychological problems arising at two time points, before the pandemic and during the embargo. In particular, the prevalence of depression was greatly increased during the embargo (1, 69–74). Moreover, according to the World Health Organization, the pandemic has led to a significant increase in the global prevalence of depression and anxiety disorders by 28 and 26%, respectively (75). COVID-19 has significantly impacted global healthcare, and new research hotspots are gradually shifting from COVID-19 and related clinical studies to studies on its psychological and social impact on humanity (36). Therefore, the shift in research hotspots and the societal impact of COVID-19 have been influenced by COVID-19's significant impact on global healthcare. As a result, an increasing number of scholars have started to conduct research on depression during the COVID-19 pandemic, influenced by the shift in research hotspots and social concerns.
Second, the hotspots of depression research during COVID-19 were significantly concentrated in regions such as the Americas, Western Europe, and South Asia. This may be related to the severity of the COVID-19 pandemic in each region. For example, India, which is in South Asia and had the second-highest total number of people diagnosed with COVID-19 worldwide, had a high prevalence of psychological problems among the population during the COVID-19 pandemic (76). In addition, a study on adults from several countries showed that participants living in Brazil had the most severe symptoms of anxiety and depression (77). This may be related to the severe COVID-19 pandemic experienced in Brazil. Furthermore, several Western European countries have paid considerable attention to the impact of the COVID-19 pandemic on public mental health and have conducted corresponding studies. For example, Bäuerle et al. found that the public mental health burden in Germany significantly increased during the COVID-19 pandemic (78). Notably, panic after infection, social isolation during treatment, and implicit discrimination after recovery were important causes of depression during COVID-19 in confirmed individuals (79, 80).
Finally, the hotspots of depression research during the pandemic could be summarized into three areas: factors influencing depression during COVID-19, consequences of depression during COVID-19, and coping strategies for depression during COVID-19.
Factors influencing depression during COVID-19
To better explain the relationship between depression and COVID-19, the factors influencing the formation of depression during COVID-19 were examined. Regarding social factors, the pressure from rising house prices (81), negative news spread on social media (82), the anxiety caused by social isolation (83, 84), and others are contributing factors to the poor mental health of residents during the pandemic. First, the ecosystem theory proposed by Bronfenbrenner mainly studies the interrelationship between human behavior and the social environment, which treats the social environment in which humans grow up as a kind of social ecosystem, emphasizes the importance of the ecosystem for analyzing and understanding human behavior, and focuses on the interaction between humans and environmental systems and their influence on individual development. Social factors that lead to depression during COVID-19, such as rising housing prices, negative news, and social isolation, change the social environment on which human growth depends. Changes in the social environment inevitably affect individual development and, consequently, have an impact on public mental health.
Regarding characteristic factors, gender, age, and occupation of the residents are conditions for the occurrence of depression during COVID-19 (85). For example, several meta-analytic studies on the prevalence of depression during COVID-19 among frontline healthcare workers have shown that they exhibit higher levels of depression than the general population (86, 87). During the pandemic, healthcare workers not only face a heavy workload but also the risk of contracting COVID-19, and their negative emotions need to be attended to. Additionally, a meta-analytic study by Li et al. found that the prevalence of depression and anxiety disorders among college students has greatly increased (88). According to Erikson's theory of psychological development, college students are still in the sameness-to-role confusion stage, and their psychological development is still in a transitional stage, immature, and vulnerable to disturbance by negative external events. Moreover, during the pandemic, college students are forced to be isolated at home, which interrupts their social activities. They have to also manage their online studies, and all of these contribute to their depressive symptoms.
Problems caused by depression during COVID-19
Brailovskaia et al. found a significant increase in suicidal ideation and suicide rates among the public during the COVID-19 pandemic (89). The American clinical psychologist Beck (90) proposed a cognitive model of depression that argues that the underlying cognitive schema and cognitive theoretical assumptions of depressed individuals are at the root of patients' negative attitudes. Some individuals with depression may be less depressed; however, sudden negative events in their lives give them a heavy blow, leading to further despair and helplessness. Despair and helplessness are important factors influencing suicide. Therefore, the COVID-19 pandemic, as a sudden negative life event, may be the root cause of helplessness and negative attitudes in depressed patients. Furthermore, several studies have pointed out that the probability of abnormal behaviors, such as insomnia and irregular diet, has increased significantly during the pandemic (91, 92). These studies are consistent with the Theory of Planned Behavior, which suggests that people's intentions or behaviors can be manipulated by attitudes, subjective norms, and perceived behavioral control to target behaviors (93). The negative, desperate, and helpless attitude of depressed individuals can lead to changes in their behavior, which may include loss of appetite, overeating, insomnia, and other abnormal behaviors. The rise in the probability of alcoholism and Internet addictive behavior is also a prevalent feature of COVID-19 (94, 95). Learned helplessness theory suggests that uncontrollable negative events are an important cause of depression. If such negative events are frequent and prolonged, they can lead to an uncontrollable perception that, no matter what one does, one cannot change the outcome. Because of the prolonged preventive and control measures and socioeconomic impacts during the COVID-19 pandemic, people's normal social activities are restricted, and their physical and mental health are damaged, making them prone to psychological burdens and causing them to develop learned helplessness. Alcoholism and Internet addiction are among the behaviors that make patients give up on their efforts and paralyze them.
How to deal with depression during COVID-19
To mitigate the increased prevalence of depression during COVID-19, treatment interventions should be improved (96, 97). Previous studies found that digital socialization, social support, and welfare measures are important in alleviating depression during the COVID-19 pandemic (98). Rose and Rudolph reconstructed the interpersonal context theory based on the interpersonal theory (99), arguing that negative early family experiences can cause individuals to develop negative interpersonal relationship evaluation tendencies and social behavior disorders, which adversely affect subsequent interpersonal skills and thus deepen public depression. Therefore, residents can reduce the incidence of depression during COVID-19 by constructing good interpersonal relationships. House (100) considers social support as an interpersonal transaction involving emotional care (liking, love, empathy), instrumental assistance (goods or services), information (environment), and assessment (information related to self-assessment). In sociological theory, Virginia (101) states that social support is a reciprocal relationship between individuals and networks that provide psychological, social, and substantive help through social networks. Therefore, to some extent, social support can alleviate the development of depression during COVID-19.
In addition, residents can prevent depression by exercising regularly and actively adjusting their mindset (102, 103). The embodied cognition theory emphasizes the interaction between cognitive processes and the anatomical structure of the body, body movements, and the external environment of the body (104). It is believed that cognition is not only related to the brain, but also to the body, which is the carrier of cognition and cognitive functions. The body can also directly participate in mental processes such as emotion and thinking. Lack of physical exercise, as mentioned earlier, is one of the factors contributing to depression during COVID-19. However, regular exercise can influence the mental health of the public by improving their mood.
Implications
The significance of this study is reflected in the following two aspects: First, this study used COOC (29) and VOSviewer (40) software as tools to conduct a literature econometric analysis and scientific knowledge mapping in the field of depression research during COVID-19, aiming to systematically summarize the trends and research hotspots in this field. Second, as an emerging topic, depression during COVID-19 has not been developed for a long time; however, it has been widely noticed worldwide owing to its specificity (43, 105). In addition, this study adopted a visualization method to quickly locate the key research results in this field. A review of the literature in this area will assist future researchers in further analyzing the causes of depression and finding measures to alleviate depression during COVID-19. It also assists the government in improving the current trend of frequent public psychological problems and provides ideas and references for solving public psychological problems caused by global issues in the future (106, 107).
Limitations and directions for future research
This study has some limitations. First, as an emerging hot topic, the earliest literature on depression during COVID-19 was published in 2020, which was <3 years ago, and scholars' research in this field is limited to the initial stage, which does not perfectly reflect the development and evolutionary trends of this field. Future research should continue to track the literature in this field over the next few years to enrich the research trends and hotspots. Second, the search platform of this study was limited by the WOS platform, the type of literature is specified, and the amount of literature obtained is incomplete. Future research should attempt to join other search platforms, such as PubMed, and compare and analyze the literature retrieved by WOS and PubMed to summarize the patterns.
Through bibliometric analysis and scientific knowledge mapping of the field of depression research during COVID-19, the following aspects may also be of interest in the future. First, most articles in the field of depression research during COVID-19 have been studied using quantitative research methods, and few have been studied using a mixture of qualitative and quantitative research methods (108, 109). Second, by reading the articles, it was established that most of the scales used to assess depression in the field articles were developed before the pandemic. Future research could thus update the depression assessment scales (110). Third, there is a lack of research on the differences in depression during COVID-19 caused by the cross-cultural context (13). Fourth, regarding factors that shape depression during COVID-19, future research should consider multi-layer linear modeling. Feinberg et al. (111) used HLM methods to study effects of public health interventions on families and individuals; in terms of causing problems, there could be a sustained focus on the specific impact of depression on special groups during COVID-19 (112); in terms of coping strategies, longitudinal studies of interventions (113) are warranted, while government (114) and society should also pay sustained attention to those with low levels of depression but are potentially at risk.
Conclusion
This study used COOC and VOSviewer tools for a comprehensive follow-up and visual analysis of the literature in the field of depression during COVID-19. The goal of this study was to systematically review the literature in this area and draw the following conclusions. First, regarding research progress, the field of depression during COVID-19 has been studied for <3 years but has entered a rapid development period. Second, the number of regional publications in the area is related to the severity and importance of the pandemic in each region. Among these, the strongest collaboration is between the United States, China, and the United Kingdom. Finally, regarding research hotspots, the field of depression during COVID-19 is particularly concerned with “factors influencing depression during COVID-19,” “consequences of depression during COVID-19,” and “coping strategies for depression during COVID-19.” The three areas of “depression during COVID-19” are discussed. Finally, this series of studies on COVID-19 provides a reference for future exploration of public mental health in the context of a global pandemic, as well as helps to forge new pathways for addressing the legacy of human psychological problems after the end of the COVID-19 pandemic and setting a research agenda for future investigations.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
JZ, QF, JG, and YX designed the study. QF, JG, and YX performed the analysis and interpreted the data. JZ, XL, YY, YM, and SS reviewed the article and provided comments or suggestions. JZ had primary responsibility for final content. All authors contributed to manuscript and approved the submitted version.
Funding
This study was supported by National Office for Education Sciences Planning, Grant Number BAA180017.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wu S, Zhang K, Parks-Stamm EJ, Hu Z, Ji Y, Cui X. Increases in anxiety and depression during COVID-19: a large longitudinal study from China. Front Psychol. (2021) 12:706601. doi: 10.3389/fpsyg.2021.706601
2. Gratz KL, Tull MT, Richmond JR, Edmonds KA, Scamaldo KM, Rose JP. Thwarted belongingness and perceived burdensomeness explain the associations of COVID-19 social and economic consequences to suicide risk. Suicide Life Threat Behav. (2020) 50:1140–8. doi: 10.1111/sltb.12654
3. Iob E, Steptoe A, Fancourt D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br J Psychiatry. (2020) 217:543–6. doi: 10.1192/bjp.2020.130
4. Kramer A, Kramer KZ. The potential impact of the Covid-19 pandemic on occupational status, work from home, and occupational mobility. J Vocat Behav. (2020) 119:103442. doi: 10.1016/j.jvb.2020.103442
5. Shi L, Que JY, Lu ZA, Gong YM, Liu L, Wang YH, et al. Prevalence and correlates of suicidal ideation among the general population in China during the COVID-19 pandemic. Eur Psychiatry. (2021) 64:e18. doi: 10.1192/j.eurpsy.2021.5
6. Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q, et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. (2020) 323:1915. doi: 10.1001/jama.2020.6130
7. Bonde JPE. Psychosocial factors at work and risk of depression: a systematic review of the epidemiological evidence. Occup Environ Med. (2008) 65:438–45. doi: 10.1136/oem.2007.038430
8. Field T. Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behav Dev. (2010) 33:1–6. doi: 10.1016/j.infbeh.2009.10.005
9. Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res. (2013) 47:391–400. doi: 10.1016/j.jpsychires.2012.11.015
10. Reijnders JSAM, Ehrt U, Weber WEJ, Aarsland D, Leentjens AFG. A systematic review of prevalence studies of depression in Parkinson's disease: the prevalence of depression in PD. Mov Disord. (2008) 23:183–9. doi: 10.1002/mds.21803
11. Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord. (2012) 142:S8–21. doi: 10.1016/S0165-0327(12)70004-6
12. Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BWJH, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. (2010) 67:220. doi: 10.1001/archgenpsychiatry.2010.2
13. Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. (2013) 34:119–38. doi: 10.1146/annurev-publhealth-031912-114409
14. Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol. (2006) 74:658–70. doi: 10.1037/0022-006X.74.4.658
15. Semkovska M, McLoughlin DM. Objective cognitive performance associated with electroconvulsive therapy for depression: a systematic review and meta-analysis. Biol Psychiatry. (2010) 68:568–77. doi: 10.1016/j.biopsych.2010.06.009
16. Cindrich SL, Lansing JE, Brower CS, McDowell CP, Herring MP, Meyer JD. Associations between change in outside time pre- and post-COVID-19 public health restrictions and mental health: brief research report. Front Public Health. (2021) 9:619129. doi: 10.3389/fpubh.2021.619129
17. Slemon A, McAuliffe C, Goodyear T, McGuinness L, Shaffer E, Jenkins EK. Reddit users' experiences of suicidal thoughts during the COVID-19 pandemic: a qualitative analysis of r/Covid19_support posts. Front Public Health. (2021) 9:693153. doi: 10.3389/fpubh.2021.693153
18. Cerami C, Canevelli M, Santi GC, Galandra C, Dodich A, Cappa SF, et al. Identifying frail populations for disease risk prediction and intervention planning in the COVID-19 era: a focus on social isolation and vulnerability. Front Psychiatry. (2021) 12:626682. doi: 10.3389/fpsyt.2021.626682
19. Liu C, Liu D, Huang N, Fu M, Ahmed JF, Zhang Y, et al. The combined impact of gender and age on post-traumatic stress symptoms, depression, and insomnia during COVID-19 outbreak in China. Front Public Health. (2021) 8:620023. doi: 10.3389/fpubh.2020.620023
20. Hayat K, Arshed M, Fiaz I, Afreen U, Khan FU, Khan TA, et al. Impact of COVID-19 on the mental health of healthcare workers: a cross-sectional study from Pakistan. Front Public Health. (2021) 9:603602. doi: 10.3389/fpubh.2021.603602
21. Khatun MF, Parvin MF, Rashid MM, Alam MS, Kamrunnahar M, Talukder A, et al. Mental health of physicians during COVID-19 outbreak in Bangladesh: a web-based cross-sectional survey. Front Public Health. (2021) 9:592058. doi: 10.3389/fpubh.2021.592058
22. Alhurishi SA, Almutairi KM, Vinluan JM, Aboshaiqah AE, Marie MA. Mental health outcomes of healthcare providers during COVID-19 pandemic in Saudi Arabia: a cross-sectional study. Front Public Health. (2021) 9:625523. doi: 10.3389/fpubh.2021.625523
23. Folayan MO, Ibigbami O, Brown B, El Tantawi M, Aly NM, Ezechi OC, et al. Factors associated with experiences of fear, anxiety, depression, and changes in sleep pattern during the COVID-19 pandemic among adults in Nigeria: a cross-sectional study. Front Public Health. (2022) 10:779498. doi: 10.3389/fpubh.2022.779498
24. Eleftheriou A, Rokou A, Arvaniti A, Nena E, Steiropoulos P. Sleep quality and mental health of medical students in Greece during the COVID-19 pandemic. Front Public Health. (2021) 9:775374. doi: 10.3389/fpubh.2021.775374
25. Bonsaksen T, Ekeberg Ø, Schou-Bredal I, Skogstad L, Heir T, Grimholt TK. Use of alcohol and addictive drugs during the COVID-19 outbreak in Norway: associations with mental health and pandemic-related problems. Front Public Health. (2021) 9:667729. doi: 10.3389/fpubh.2021.667729
26. Miller ER, Olver IN, Wilson CJ, Lunnay B, Meyer SB, Foley K, et al. COVID-19, Alcohol consumption and stockpiling practises in midlife women: repeat surveys during lockdown in Australia and the United Kingdom. Front Public Health. (2021) 9:642950. doi: 10.3389/fpubh.2021.642950
27. De Pasquale C, Sciacca F, Conti D, Pistorio ML, Hichy Z, Cardullo RL, et al. Relations between mood states and eating behavior during COVID-19 pandemic in a sample of Italian College Students. Front Psychol. (2021) 12:684195. doi: 10.3389/fpsyg.2021.684195
28. Halms T, Strasser M, Kunz M, Hasan A. How to reduce mental health burden in health care workers during COVID-19?–A scoping review of guideline recommendations. Front Psychiatry. (2022) 12:770193. doi: 10.3389/fpsyt.2021.770193
29. XueShuDianDi. COOC is a software for bibliometrics and knowledge graph drawing. GitHub. Available online at: https://github.com/2088904822 (accessed November 10, 2022).
30. Qin F, Li J, Zhang C, Zeng G, Huang D, Tan X, et al. Biochar in the 21st century: a data-driven visualization of collaboration, frontier identification, and future trend. Sci Total Environ. (2022) 818:151774. doi: 10.1016/j.scitotenv.2021.151774
31. Tan H, Li J, He M, Li J, Zhi D, Qin F, et al. Global evolution of research on green energy and environmental technologies: a bibliometric study. J Environ Manage. (2021) 297:113382. doi: 10.1016/j.jenvman.2021.113382
32. You Y, Li W, Liu J, Li X, Fu Y, Ma X. Bibliometric review to explore emerging high-intensity interval training in health promotion: a new century picture. Front Public Health. (2021) 9:697633. doi: 10.3389/fpubh.2021.697633
33. Ke L, Lu C, Shen R, Lu T, Ma B, Hua Y. Knowledge mapping of drug-induced liver injury: a scientometric investigation (2010–2019). Front Pharmacol. (2020) 11:842. doi: 10.3389/fphar.2020.00842
34. Yeung AWK, Kletecka-Pulker M, Eibensteiner F, Plunger P, Völkl-Kernstock S, Willschke H, et al. Implications of twitter in health-related research: a landscape analysis of the scientific literature. Front Public Health. (2021) 9:654481. doi: 10.3389/fpubh.2021.654481
35. Fan J, Gao Y, Zhao N, Dai R, Zhang H, Feng X, et al. Bibliometric analysis on COVID-19: a comparison of research between English and Chinese studies. Front Public Health. (2020) 8:477. doi: 10.3389/fpubh.2020.00477
36. Hu S, Wang X, Ma Y, Cheng H. Global research trends in pediatric COVID-19: a bibliometric analysis. Front Public Health. (2022) 10:798005. doi: 10.3389/fpubh.2022.798005
37. Al-Jabi SW. Current global research landscape on COVID-19 and depressive disorders: Bibliometric and visualization analysis. World J Psychiatry. (2021) 11:253–64. doi: 10.5498/wjp.v11.i6.253
38. Nuryana Z, Murshidi GA, Rahman A. Publication trends related to schizophrenia, mental health, and depression during COVID-19. Asian J Psychiatry. (2021) 66:102878. doi: 10.1016/j.ajp.2021.102878
39. Hernández RM, Saavedra-López MA, Calle-Ramírez XM. Latin American authors in the scientific production on depression in times of COVID-19. Asian J Psychiatry. (2021) 65:102856. doi: 10.1016/j.ajp.2021.102856
40. van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. (2010) 84:523–38. doi: 10.1007/s11192-009-0146-3
41. Zhong H, Zhou Y, Mei SY, Tang R, Feng JH, He ZY, et al. Scars of COVID-19: a bibliometric analysis of post-COVID-19 fibrosis. Front Public Health. (2022) 10:967829. doi: 10.3389/fpubh.2022.967829
42. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
43. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
44. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092. doi: 10.1001/archinte.166.10.1092
45. Bohn L, Gomes S, Neto ESQ, Lage ACSS, de Freitas MDDB, Magalhães FP, et al. Predictors of lower depression levels in older adults during COVID-19 lockdown. J Appl Gerontol. (2021) 40:1407–16. doi: 10.1177/07334648211025116
46. Ganson KT, Tsai AC, Weiser SD, Benabou SE, Nagata JM. Job insecurity and symptoms of anxiety and depression among US young adults during COVID-19. J Adolesc Health. (2021) 68:53–6. doi: 10.1016/j.jadohealth.2020.10.008
47. Levy I, Cohen-Louck K. Predicting individual function during COVID-19 lockdown: depression, fear of COVID-19, age, and employment. Front Psychol. (2021) 12:682122. doi: 10.3389/fpsyg.2021.682122
48. Hou F, Bi F, Jiao R, Luo D, Song K. Gender differences of depression and anxiety among social media users during the COVID-19 outbreak in China: a cross-sectional study. BMC Public Health. (2020) 20:1648. doi: 10.1186/s12889-020-09738-7
49. Solomou I, Constantinidou F. Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: age and sex matter. Int J Environ Res Public Health. (2020) 17:4924. doi: 10.3390/ijerph17144924
50. McPhee MD, Keough MT, Rundle S, Heath LM, Wardell JD, Hendershot CS. Depression, environmental reward, coping motives and alcohol consumption during the COVID-19 pandemic. Front Psychiatry. (2020) 11:574676. doi: 10.3389/fpsyt.2020.574676
51. Wardell JD, Kempe T, Rapinda KK, Single A, Bilevicius E, Frohlich JR, et al. Drinking to cope during COVID-19 pandemic: the role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems. Alcohol Clin Exp Res. (2020) 44:2073–83. doi: 10.1111/acer.14425
52. Xu X, Wang W, Chen J, Ai M, Shi L, Wang L, et al. Suicidal and self-harm ideation among Chinese hospital staff during the COVID-19 pandemic: prevalence and correlates. Psychiatry Res. (2021) 296:113654. doi: 10.1016/j.psychres.2020.113654
53. Itani MH, Eltannir E, Tinawi H, Daher D, Eltannir A, Moukarzel AA. Severe social anxiety among adolescents during COVID-19 lockdown. J Patient Exp. (2021) 8:237437352110383. doi: 10.1177/23743735211038386
54. Arpino B, Pasqualini M. Effects of pandemic on feelings of depression in Italy: the role of age, gender, and individual experiences during the first lockdown. Front Psychol. (2021) 12:660628. doi: 10.3389/fpsyg.2021.660628
55. Ahmed MZ, Ahmed O, Aibao Z, Hanbin S, Siyu L, Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatry. (2020) 51:102092. doi: 10.1016/j.ajp.2020.102092
56. Greenberg N, Weston D, Hall C, Caulfield T, Williamson V, Fong K. Mental health of staff working in intensive care during Covid-19. Occup Med. (2021) 71:62–7. doi: 10.1093/occmed/kqaa220
57. Gilleen J, Santaolalla A, Valdearenas L, Salice C, Fusté M. Impact of the COVID-19 pandemic on the mental health and well-being of UK healthcare workers. BJPsych Open. (2021) 7:e88. doi: 10.1192/bjo.2021.42
58. Iyengar U, Jaiprakash B, Haitsuka H, Kim S. One year into the pandemic: a systematic review of perinatal mental health outcomes During COVID-19. Front Psychiatry. (2021) 12:674194. doi: 10.3389/fpsyt.2021.674194
59. Silverio SA, Davies SM, Christiansen P, Aparicio-García ME, Bramante A, Chen P, et al. A validation of the postpartum specific anxiety scale 12-item research short-form for use during global crises with five translations. BMC Pregnancy Childbirth. (2021) 21:112. doi: 10.1186/s12884-021-03597-9
60. Bermejo-Sánchez FR, Peña-Ayudante WR, Espinoza-Portilla E. Depresión perinatal en tiempos del COVID-19: rol de las redes sociales en Internet. Acta Medica Peru. (2020) 37:88–93. doi: 10.35663/amp.2020.371.913
61. Sharif Nia H, Gorgulu O, Naghavi N, Robles-Bello MA, Sánchez-Teruel D, Khoshnavay Fomani F, et al. Spiritual wellbeing, social support, and financial distress in determining depression: the mediating role of impact of event during COVID-19 pandemic in Iran. Front Psychiatry. (2021) 12:754831. doi: 10.3389/fpsyt.2021.754831
62. Lv F, Yu M, Li J, Tan J, Ye Z, Xiao M, et al. Young adults' loneliness and depression during the COVID-19 pandemic: a moderated mediation model. Front Psychol. (2022) 13:842738. doi: 10.3389/fpsyg.2022.842738
63. Servidio R, Scaffidi Abbate C, Costabile A, Boca S. Future orientation and symptoms of anxiety and depression in Italian university students during the COVID-19 pandemic: the role of resilience and the perceived threat of COVID-19. Healthcare. (2022) 10:974. doi: 10.3390/healthcare10060974
64. Yalçin I, Can N, Mançe Çalişir Ö, Yalçin S, Çolak B. Latent profile analysis of COVID-19 fear, depression, anxiety, stress, mindfulness, and resilience. Curr Psychol. (2022) 41:459–69. doi: 10.1007/s12144-021-01667-x
65. Zhang Q, Li J, Weng L. A bibliometric analysis of COVID-19 publications in neurology by using the visual mapping method. Front Public Health. (2022) 10:937008. doi: 10.3389/fpubh.2022.937008
66. Zhang Q, Weng L, Li J. The evolution of intracranial aneurysm research from 2012 to 2021: Global productivity and publication trends. Front Neurol. (2022) 13:953285. doi: 10.3389/fneur.2022.953285
67. Zhang Q, Li S, Liu J, Chen J. Global trends in nursing-related research on COVID-19: a bibliometric analysis. Front Public Health. (2022) 10:933555. doi: 10.3389/fpubh.2022.933555
68. Huang D, Wang J, Fang H, Wang X, Zhang Y, Cao S. Global research trends in the subjective well-being of older adults from 2002 to 2021: a bibliometric analysis. Front Psychol. (2022) 13:972515. doi: 10.3389/fpsyg.2022.972515
69. Alzueta E, Podhajsky S, Zhao Q, Tapert SF, Thompson WK, de Zambotti M, et al. Risk for depression tripled during the COVID-19 pandemic in emerging adults followed for the last 8 years. Psychol Med. (2021) 1–8. doi: 10.1017/S0033291721004062
70. Betancourt-Ocampo D, Toledo-Fernández A, González-González A. Mental health changes in older adults in response to the COVID-19 pandemic: a longitudinal study in Mexico. Front Public Health. (2022) 10:848635. doi: 10.3389/fpubh.2022.848635
71. Cassioli E, Rossi E, Castellini G, Sanfilippo G, Silvestri C, Voller F, et al. Psychopathological consequences and dysfunctional behaviours during the COVID-19 epidemic in Italy: a longitudinal study before and after the lockdown. Eur Psychiatry. (2021) 64:S96–7. doi: 10.1192/j.eurpsy.2021.282
72. Rehman U, Yildirim M, Shahnawaz MG. A longitudinal study of depression, anxiety, and stress among Indians during COVID-19 pandemic. Psychol Health Med. (2022) 1–9. doi: 10.1080/13548506.2021.2023751
73. Saraswathi I, Saikarthik J, Senthil Kumar K, Madhan Srinivasan K, Ardhanaari M, Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. PeerJ. (2020) 8:e10164. doi: 10.7717/peerj.10164
74. Wu J, Wu Y, Tian Y. Temporal associations among loneliness, anxiety, and depression during the COVID-19 pandemic period. Stress Health. (2022) 38:90–101. doi: 10.1002/smi.3076
75. Director-General's report to Member States at the 75th World Health Assembly – 23 May 2022 (2022). Available online at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-address-at-the-75th-world-health-assembly-−23-may-2022 (accessed June 15, 2022).
76. Nagabhirava G, Godi SM, Goel AD. Fear, psychological impact, and coping during the initial phase of COVID-19 pandemic among the general population in India. Cureus. (2021) 13:e20317. doi: 10.7759/cureus.20317
77. Ding K, Yang J, Chin MK, Sullivan L, Demirhan G, Violant-Holz V, et al. Mental health among adults during the COVID-19 pandemic lockdown: a cross-sectional multi-country comparison. Int J Environ Res Public Health. (2021) 18:2686. doi: 10.3390/ijerph18052686
78. Bäuerle A, Teufel M, Musche V, Weismüller B, Kohler H, Hetkamp M, et al. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J Public Health. (2020) 42:672–8. doi: 10.1093/pubmed/fdaa106
79. Bhanot D, Singh T, Verma SK, Sharad S. Stigma and discrimination during COVID-19 pandemic. Front Public Health. (2021) 8:577018. doi: 10.3389/fpubh.2020.577018
80. Piredda M, Fiorini J, Marchetti A, Mastroianni C, Albanesi B, Livigni L, et al. The wounded healer: a phenomenological study on hospital nurses who contracted COVID-19. Front Public Health. (2022) 10:867826. doi: 10.3389/fpubh.2022.867826
81. Bower M, Buckle C, Rugel E, Donohoe-Bales A, McGrath L, Gournay K, et al. “Trapped”, “anxious” and “traumatised”: COVID-19 intensified the impact of housing inequality on Australians' mental health. Int J Hous Policy. (2022) 1–32. doi: 10.1080/19491247.2021.1940686
82. Luo T, Chen W, Liao Y. Social media use in China before and during COVID-19: Preliminary results from an online retrospective survey. J Psychiatr Res. (2021) 140:35–8. doi: 10.1016/j.jpsychires.2021.05.057
83. Daly Z, Slemon A, Richardson CG, Salway T, McAuliffe C, Gadermann AM, et al. Associations between periods of COVID-19 quarantine and mental health in Canada. Psychiatry Res. (2021) 295:113631. doi: 10.1016/j.psychres.2020.113631
84. Kim Y, Kwon HY, Lee S, Kim CB. Depression during COVID-19 quarantine in South Korea: a propensity score-matched analysis. Front Public Health. (2022) 9:743625. doi: 10.3389/fpubh.2021.743625
85. Pieh C, Budimir S, Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J Psychosom Res. (2020) 136:110186. doi: 10.1016/j.jpsychores.2020.110186
86. Muller AE, Hafstad EV, Himmels JPW, Smedslund G, Flottorp S, Stensland SØ, et al. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatry Res. (2020) 293:113441. doi: 10.1016/j.psychres.2020.113441
87. Olaya B, Pérez-Moreno M, Bueno-Notivol J, Gracia-García P, Lasheras I, Santabárbara J. Prevalence of depression among healthcare workers during the COVID-19 outbreak: a systematic review and meta-analysis. J Clin Med. (2021) 10:3406. doi: 10.3390/jcm10153406
88. Li Y, Wang A, Wu Y, Han N, Huang H. Impact of the COVID-19 pandemic on the mental health of college students: a systematic review and meta-analysis. Front Psychol. (2021) 12:669119. doi: 10.3389/fpsyg.2021.669119
89. Brailovskaia J, Truskauskaite-Kuneviciene I, Kazlauskas E, Gelezelyte O, Teismann T, Margraf J. Physical activity, mental and physical health during the Covid-19 outbreak: longitudinal predictors of suicide ideation in Germany. J Public Health. (2022) 1–11. doi: 10.1007/s10389-022-01708-0
90. Beck AT, Steer RA, Brown G. Beck depression inventory–II. American Psychological Association. (2011). Available from: http://doi.apa.org/getdoi.cfm?doi=10.1037/t00742-000 (accessed November 10, 2022).
91. Niu X, Snyder HR. The role of maladaptive emotion regulation in the bidirectional relation between sleep and depression in college students during the COVID-19 pandemic. Anxiety Stress Coping. (2022) 1–14. doi: 10.1080/10615806.2022.2073441
92. Wu H, Li H, Li X, Su W, Tang H, Yang J, et al. Psychological health and sleep quality of medical graduates during the second wave of COVID-19 pandemic in post-epidemic era. Front Public Health. (2022) 10:876298. doi: 10.3389/fpubh.2022.876298
93. Shen L, Gu X, Zhang T, Lee J. Adolescents' physical activity and depressive symptoms: a psychosocial mechanism. Int J Environ Res Public Health. (2022) 19:1276. doi: 10.3390/ijerph19031276
94. Lee S, Mun IB. How does perceived parental rejection influence cyberbullying by children? A serial mediation model of children's depression and smartphone addiction. Soc Sci J. (2022) 1–16. doi: 10.1080/03623319.2022.2070826
95. Sugaya N, Yamamoto T, Suzuki N, Uchiumi C. Alcohol use and its related psychosocial effects during the prolonged COVID-19 pandemic in Japan: a cross-sectional survey. Int J Environ Res Public Health. (2021) 18:13318. doi: 10.3390/ijerph182413318
96. Irfan M, Naeem F, Afridi M, Javed A. Prevention of occupational stress in health-care workers during COVID-19 pandemic. Indian J Psychiatry. (2020) 62:495. doi: 10.4103/psychiatry.IndianJPsychiatry_844_20
97. Rodríguez-Rey R, Garrido-Hernansaiz H, Collado S. Psychological impact and associated factors during the initial stage of the Coronavirus (COVID-19) pandemic among the general population in Spain. Front Psychol. (2020) 11:1540. doi: 10.3389/fpsyg.2020.01540
98. Feng L, Yin R. Social support and hope mediate the relationship between gratitude and depression among front-line medical staff during the pandemic of COVID-19. Front Psychol. (2021) 12:623873. doi: 10.3389/fpsyg.2021.623873
99. Rose AJ, Rudolph KD. A review of sex differences in peer relationship processes: Potential trade-offs for the emotional and behavioral development of girls and boys. Psychol Bull. (2006) 132:98–131. doi: 10.1037/0033-2909.132.1.98
100. House JS. Barriers to work stress: i. social support. In:Gentry WD, Benson H, Wolff CJ, , editors. Behavioral Medicine: Work, Stress and Health. Dordrecht: Springer Netherlands. (1985). p. 157–80.
101. Tilden VP, Weinert C. Social support and the chronically III individual. Nurs Clin North Am. (1987) 22:613–20. doi: 10.1016/S0029-6465(22)01312-3
102. Pieh C, O'Rourke T, Budimir S, Probst T. Relationship quality and mental health during COVID-19 lockdown Montazeri A, editor. PLoS ONE. (2020) 15:e0238906. doi: 10.1371/journal.pone.0238906
103. Zhang Y, Huang L, Luo Y, Ai H. The relationship between state loneliness and depression among youths during COVID-19 lockdown: coping style as mediator. Front Psychol. (2021) 12:701514. doi: 10.3389/fpsyg.2021.701514
104. Barsalou LW. Grounded cognition. Annu Rev Psychol. (2008) 59:617–45. doi: 10.1146/annurev.psych.59.103006.093639
105. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y, et al. nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. (2020) 33:e100213. doi: 10.1136/gpsych-2020-100213
106. Bodrud-Doza Md, Shammi M, Bahlman L, Islam ARMdT, Rahman MdM. Psychosocial and socio-economic crisis in Bangladesh due to COVID-19 pandemic: a perception-based assessment. Front Public Health. (2020) 8:341. doi: 10.3389/fpubh.2020.00341
107. Porat T, Nyrup R, Calvo RA, Paudyal P, Ford E. Public health and risk communication during COVID-19—enhancing psychological needs to promote sustainable behavior change. Front Public Health. (2020) 8:573397. doi: 10.3389/fpubh.2020.573397
108. Stoichitoiu LE, Pinte L, Ceasovschih A, Cernat RC, Vlad ND, Padureanu V, et al. In-hospital antibiotic use for COVID-19: facts and rationales assessed through a mixed-methods study. J Clin Med. (2022) 11:3194. doi: 10.3390/jcm11113194
109. Toran M, Özden B. Are there any changes in mothers' attitudes? Analysis of the impact of the COVID-19 quarantine on child-rearing attitudes. Child Youth Serv Rev. (2022) 134:106372. doi: 10.1016/j.childyouth.2022.106372
110. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. (2022) 20:1537–45. doi: 10.1007/s11469-020-00270-8
111. Feinberg ME, Mogle J, Lee J, Tornello SL, Hostetler ML, Cifelli JA, et al. Impact of the COVID-19 pandemic on parent, child, and family functioning. Fam Process. (2022) 61:361–74. doi: 10.1111/famp.12649
112. Reid G, Ritholtz S. A queer approach to understanding LGBT vulnerability during the COVID-19 pandemic. Polit Gend. (2020) 16:1101–9. doi: 10.1017/S1743923X20000707
113. Yang Z, Ji LJ, Yang Y, Wang Y, Zhu L, Cai H. Meaning making helps cope with COVID-19: a longitudinal study. Personal Individ Differ. (2021) 174:110670. doi: 10.1016/j.paid.2021.110670
Keywords: COOC analysis, VOSviewer, depression during COVID-19, bibliometric analysis, visualization analysis
Citation: Fu Q, Ge J, Xu Y, Liang X, Yu Y, Shen S, Ma Y and Zhang J (2022) The evolution of research on depression during COVID-19: A visual analysis using Co-Occurrence and VOSviewer. Front. Public Health 10:1061486. doi: 10.3389/fpubh.2022.1061486
Received: 04 October 2022; Accepted: 21 November 2022;
Published: 06 December 2022.
Edited by:
Mohammadreza Shalbafan, Iran University of Medical Sciences, IranReviewed by:
Tsz Kit Ng, The University of Hong Kong, Hong Kong SAR, ChinaXue Lan, China Medical University, China
Carlo Lazzari, South West Yorkshire Partnership NHS Foundation Trust, United Kingdom
Qian Zhang, Xiangya Hospital, Central South University, China
Copyright © 2022 Fu, Ge, Xu, Liang, Yu, Shen, Ma and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianzhen Zhang, amlhbnpoZW56aGFuZ2VkdUBmb3htYWlsLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Qiannan Fu1†
Qiannan Fu1† Jiahao Ge
Jiahao Ge Yanhua Xu
Yanhua Xu Xiaoyu Liang
Xiaoyu Liang Suqin Shen
Suqin Shen Yanfang Ma
Yanfang Ma Jianzhen Zhang
Jianzhen Zhang