- 1College of Medicine and Health Sciences, Mizan-Tepi University, Mizan-Aman, Ethiopia
- 2Department of Epidemiology and Biostatistics, School of Public Health, Addis Ababa University, Addis Ababa, Ethiopia
Background: Adopting contraception on time is a critical intervention for postpartum women, but violence exposure around pregnancy may interfere with postpartum contraceptive use behaviors. Hence, this study aimed to investigate the time duration of the first modern contraceptive adoption and its individual-and community-level predictors among postpartum women in the Wolaita zone, South Ethiopia.
Methods: A community-based prospective follow-up study was conducted among 1,292 postpartum women nested in 38 “Kebles” (clusters) using multistage-clustered sampling techniques. A multilevel Weibull regression model was employed to investigate predictors of time-to-method initiation after childbirth using STATA Version 14. Kaplan-Meier curve and Wilcoxon log-rank test were used to estimate time-to-modern contraceptive use across different variables. All variables with p-values <0.05 were considered for multivariate analysis. Adjusted time ratios (ATR) with 95 % CI were computed using Weibull accelerated failure time models.
Results: Of the respondents, 62% (95% CI: 59.1–64.5) had started the first modern contraception within a year after childbirth. The restricted mean survival time-to-postpartum modern contraceptive use was 6.28 months. Being a rural dweller (aTR: 1.44; 95% CI: 1.06–1.99) and living in the middle household wealth quintiles (aTR: 1.10; 95% CI: 1.02–1.19) predicted longer time duration to adopt first modern contraception by 44 and 10%, respectively. The women from the community with a high early marriage (aTR: 1.14; 95% CI: 1.01–1.28) took longer time to initiate modern postpartum methods. Furthermore, women who had no history of perinatal abuse took less time than those who had a history of abuse to start postpartum contraception (aTR: 0.71; 95% CI: 0.66–0.78).
Conclusion: Rural residence, poor household wealth status, history of perinatal abuse, and a high rate of early marriage in the community are predicted to lengthen the time duration to start modern postpartum contraception. Thus, community-level women's empowerment, particularly among rural women and integration of intimate partner violence screening into family planning counseling throughout the continuum of care will likely to improve postpartum contraception timing.
Introduction
Intimate partner violence (IPV) is a global public health and human rights crisis that exacts a high burden of suffering on millions of women and families (1, 2). Violence against pregnant or postpartum women is a critical concern because of its pervasive impacts on several psychological and physical outcomes relevant to mother and child (3, 4). Perinatal IPV (P-IPV) refers to violence perpetrated by a partner either in the year before pregnancy, during pregnancy, or/and up to 1 year after childbirth (5, 6). Although perinatal women deserve safety and protection, violence during this critical period is associated with poor physical and psychosocial health, some of which may impact future childbearing and contraceptive use (7, 8). According to literatures, IPV has been linked to many reproductive health problems such as unintended pregnancies, lower contraceptive use, fetal loss, abortions, and a higher incidence of infertility (9–14). In terms of birth control, women in violent relationships have limited decision-making power. Studies have highlighted that women's ability to control their reproductive health choices significantly impacts greater control over pregnancy and pregnancy timing (15, 16).
Adopting contraception on time is a critical intervention for postpartum women who want to avoid unintended pregnancy and closed birth intervals (17, 18), leading to adverse maternal, perinatal and infant outcomes (19). The World Health Organization (WHO) recommends that women start modern methods immediately or within 42 days after childbirth, with the option of continuous contraception or effective switching for two subsequent years, depending on a woman's desire to space or limit future pregnancies (20, 21). Despite more than 90% of women want to avoid or delay pregnancies postpartum, two-thirds are not using contraception (22). Due to limited reproductive health control, women in abusive relationships are at a significantly higher risk of unintended pregnancy (8, 23, 24). Violence around the time of pregnancy may interfere with postpartum contraceptive use behaviors. The existing evidence reveals a variety of results (25). PIPV has been linked to lower or non-postpartum contraceptive use in some studies (13, 26–28), whilst other findings (29, 30) shows that PIPV exposure is associated with increased postpartum contraceptive adoption.
In recognition of its negative consequences, the family planning (FP) agenda 2030 aims to reduce psychosocial barriers that prevent women from using life-saving and life-changing modern contraceptives (31). Ethiopia has made significant progress toward meeting the FP2020 agenda, but the contraceptive prevalence rate remains low (32, 33). According to studies conducted in the country, about 46–66% of women initiated their first methods postpartum (34–36), whilst only 10–30% of them adopted within 2 months post-delivery (35, 36). Apart from this, the median survival time of the first modern contraceptive initiation was 7–11 months, far from the recommended time (35, 36). The timing of postpartum contraceptive adoption varies with an individual, partner, relationship, and community-level characteristics such as age, place of residence (37, 38), maternal education (35, 38), household wealth status (37), appropriate and timely maternal health care utilization (35, 36), breast feeding status (37), menstrual and sexual intercourse resumption and spousal communication (39). However, little is known about the effects of PIPV on time-to-modern contraceptive adoption among currently married women. Moreover, exploring how PIPV exposure affects postpartum women's contraceptive use patterns has important policy and program implications. Also, the finding will be critical in achieving national family planning program targets set in Health Sector Transformation Plan-II (Contraceptive prevalence rate from 41% in 2019 to 50% in 2025) (40). Therefore, this study investigates time duration-to-modern contraceptive adoption between postpartum women who had the experience of perinatal abuse and whom not, and to identify individual-and community-level predictors that influence postpartum women's method initiation in Wolaita zone, South Ethiopia.
Materials and methods
Study design, setting, and period
A community-based prospective follow-up study was conducted in the Wolaita zone located in Ethiopian's South Nations, Nationalities, and People's Regions (SNNPR). The zone is subdivided into sixteen rural districts (woredas) and six town administrations. It is one of the most densely populated zones in the region with an estimated population of 2.5 million people. The estimated number of women in the reproductive age group is 582,500. Of these women, the estimated postpartum population is 86,500. This zone has 310,454 households with an average household size of 4.84 persons (41). There are seven hospitals (five governmental and two private), 68 health centers, and 345 health posts within the zone (42). This study took place in randomly selected rural districts (Damot Woyde, Offa, Kindo Koysha, and Boloso Sore) and three town administrations (Soddo, Boditti, and Areka). The study was conducted between October 2019 and January 2021. The baseline data was collected between October 2019 and January 2020, and the final data was collected between October 2020 and January 2021.
Source and study population with their eligibility criteria
All postpartum women living in the zone during the study period were considered the source population. The study population consisted of postpartum women in the zone's randomly selected districts and towns. The study sample's inclusion criteria were women of reproductive age, who lived with a current male partner for the last year, who were interviewed for baseline survey, and had a current healthy infant. The postpartum women who were divorced and widowed after the baseline survey were excluded from the study. The women who experienced miscarriages were also excluded from the final interview.
Sample size determination
The sample size was computed using STATA Version 16.0. As no similar study was conducted in the country to determine the sample size; study from other developing country, Uganda (43) was used by taking 50% median survival time among groups, 90% power, 5% level of significance, and hazard ratio (1.83). By considering the design effect of 2 and 10% non-response rate, the final sample size was assumed to be 494. The following equations were used to calculate the required sample size. The sample size (n) = [(number of event/probability of event) * deff]/(1-non-response rate). Number of event , where α = Threshold probability for rejecting the null hypothesis (Type I error rate), β = probability of failing to reject the null hypothesis under alternative hypothesis (Type II error rate), p= survival probability rate in group 1 (exposed), q = survival probability rate in group 2 (unexposed), and AHR = Adjusted hazards ratio. The probability of event = Pr (event) = 1 – [P S1 (t) + q S2 (t)]. However, this study was part of a large longitudinal study that designed to investigate the interplay between PIPV and postpartum contraception. The study had four specific objectives, and the alternative sample size for each was calculated. Thus, maximum sample size (1320) was taken for all objectives considering the following assumptions: 95% confidence interval, 4% margin of error, 80% power, proportion of postpartum modern contraceptive use (49%) (38), design effect of 2, and 10% non-response rate. The following single population proportion formula was used to calculate the sample size. N = [{(Zα/2)2*p (1–p)}/d∧2*deff]/ (1-non-response rate), where z = percentile of the standard normal distribution, p = proportion of postpartum modern contraceptive adoption from the other study, d = the desired precision of the estimate, deff = design effect for the multi-stage nature of the sampling procedure. However, to increase the study's power, 1,342 postpartum women who met inclusion criteria were approached at the baseline interview. After excluding non-response cases, 1,292 women had been followed for a year after the baseline survey. As a result, all 1,292 women were included in this study.
Data collection procedure
An interviewer-administered questionnaire was prepared from different literature including WHO and DHS standard tools (44, 45). The pilot study was conducted to test questionnaire's validity and reliability and some modifications were made including frequency and timing of violence occurrence in the perinatal period (before, during and after pregnancy). As this was part of a large longitudinal study, the data were collected in two phases. At the baseline, socio-demographic, economic, psychosocial, and reproductive characteristics were collected. Then, participants had been on follow-up for a year and data on the reproductive events (e.g., breastfeeding, resumption of menses and sexual activity), PIPV exposure status, and contraceptive use dynamics (adoption, switching, continuation, and discontinuation) were collected at the final interview. Thirty-eight data collectors (married, female, diploma holders) with eight supervisors (BSc in Public Health) were trained and deployed after receiving 2 days of intensive training. For administrative purposes, the training was given separately in each district. The main focus of the training was on the purpose of the study, the contents of the instruments, and how to check the nuances of coding, errors, and consistency of each questionnaire.
Sampling procedure
A multistage-clustered sampling technique was used to identify study participants. The zone is divided into sixteen rural districts and six town administrations. As the rule of thumb (>25%), four rural districts and three town administrations were randomly selected. These districts and towns were further clustered by “Kebles,” Ethiopia's lowest administrative unit, and stratified into rural and urban Kebles. In this study, a cluster is a community of people likely to share common values. Then, four rural and two urban Kebles were randomly selected from each rural district. Fourteen Kebles were chosen from town administrations (eight urban and six rural) using a simple random sampling method. With this, thirty-eight (twenty-two rural and sixteen urban) Kebles were drawn from randomly selected districts and towns. The sample size for each Keble was allocated using probability proportional to the size and the expected number of postpartum women per Keble. List of households with eligible women were prepared from a family folder of health extension workers (HEWs) in the respective Kebles. Enumerators compiled the lists with the help of HEWs. When there was more than one eligible woman in a household, only one woman was chosen randomly. Finally, 1,342 eligible women who met the eligibility criteria were included in the baseline survey. However, 1,292 women had been on 1 year follow-up for this study.
Study variables and measurement
The outcome variable was time length-to-modern contraceptive use postpartum. This was recorded in months using a contraceptive calendar (46, 47). The event's occurrence was coded as “1” when women report modern contraception adoption and “0” otherwise. PIPV (psychological, physical, and sexual violence) was the main exposure variable measured using section seven of the WHO standardized questionnaire (44). Overall, the experience of PIPV was classified as a binary variable (yes/no). The women-level predictors included twelve variables that consisted of women's age at childbirth and marriage, education, employment status, number of living children, breastfeeding status, resumption of menses, attitudes toward wife-beating norms, exposure to perinatal violence (before, during pregnancy or either), and women's wealth status. The five husband-level predictors included education and employment status, alcohol and substance abuse history, and wife controlling behavior. The relationship-level predictors incorporated were women's decision-making autonomy, asset ownership, couple's communication about daily life, and income difference. Women's norms and attitudes toward IPV and a man's control over his wife's behaviors and activities were measured using sections six and seven of the WHO multi-country study on women's health and domestic violence questionnaire (44, 45). Participants' decision-making autonomy in household issues was also measured (45) by asking whether women participated in personal health care, daily household purchases, major household purchases, visits family or relatives, husband's and her income.
Community-level variables included were women's residency; classified as urban or rural based on the Ethiopian Central Statistical Authority descriptions of respondent's location (48). Aggregating individual-level characteristics constructed other community-level factors. The aggregates for clusters were computed using means (for normally distributed) or median (not normally distributed) values for each respondent in each category of a given variable. Finally, high-level variables were re-categorized into lower and higher categories.
Data management and analysis
The data were coded, cleaned, and edited using SPSS for Windows version 25.0. Descriptive and summary statistics were computed in number and percentages. Multilevel survival models based on different parametric distributions were fitted because the hierarchical nature of data collected from 1,292 postpartum women nested in 38 clusters (Kebles). The study participants within each cluster ranged from twenty to forty-three. The multilevel survival model is the best model for the right-censored data and yields unbiased estimates of the risk of the occurrence of the target event (49). Consequently, the model handles the cluster-specific random effects on the survival outcomes (50). The effect of covariates on baseline hazards function is measured through two often-used models: the accelerated failure-time (AFT) model and the PH model. The covariate effect is multiplicative on the time scale in the AFT model, while it is multiplicative on the hazard scale in the PH models (50, 51). We preferred AFT to the PH model; hence it accounts for the effect of the covariates directly on the survival times rather than on the hazards rate as in the PH model, and it yields more accurate inference, proper fitting of the model and easy interpretation of the results (52, 53). Then, time ratios rather than hazard ratios were used to report time length-to-postpartum contraceptive use. The intraclass correlation coefficient (ICC) for the intercept only model was calculated to determine whether or not the multilevel survival analysis was required. ICC measures the total variation of postpartum contraceptive use timing between clusters without any covariates (52, 54). The model comparison was made using the log-likelihood ratio test, deviance (-2LL), and Akaike's Information Criterion (AIC) value. The model with the lowest deviance and AIC was selected as the best fitted model and used to describe the data. All variables with a p-value of <0.05 in bivariate analysis were considered candidates for multivariable analysis. In the multivariable multilevel analysis, the adjusted time ratios along with the 95% CI were used to show level of significance and strength of association.
Ethical consideration
The study was reviewed and approved by the Institutional Review Board of the College of Health Sciences, Addis Ababa University, with a protocol number of 006/19/SPH. The interviews were conducted with full respect for WHO ethical and safety recommendation guidelines (55). All the study participants were briefed about the aim and procedures of the research and their right to abstain or withdraw from the study at any time. The informed verbal consent was obtained from each participant separately. The confidentiality of the collected data was maintained by locking it in the file cabinet. All study information was kept secured and confidential with the first author. After the interview, participants were allowed to visit a psychiatric nurse if they experienced any psychological discomfort.
Results
Individual- and community-level characteristics of study participants
A total of 1,252 of the study participants had completed the interview. About 3.1% of them were lost to be reached and censored for survival analysis (Table 1). The majority of the respondents were aged 25–34 years (57.1%), had no formal education (36%), were married to men with no education (30%), unemployed (85%) and had husbands who work in paid jobs (35%). Approximately 64% of the respondents reported resumption of menstruation, and 95% of them resumed sexual activity in the year postpartum. About 57% of the participants had justified IPV favoring norms, and 38% of the participants reported being exposed to violence in the year before pregnancy with 28% of them experienced it during pregnancy. Approximately 40% of women experienced perinatal partner violence either a year before or during pregnancy. Regarding community-level characteristics, the majority of respondents were living in the community with rural residence (56.3%), low early marriage (52.8%), high female literacy (55.7%), high IPV favoring norms (53.2%), and high women's decision-making autonomy (54.3%).
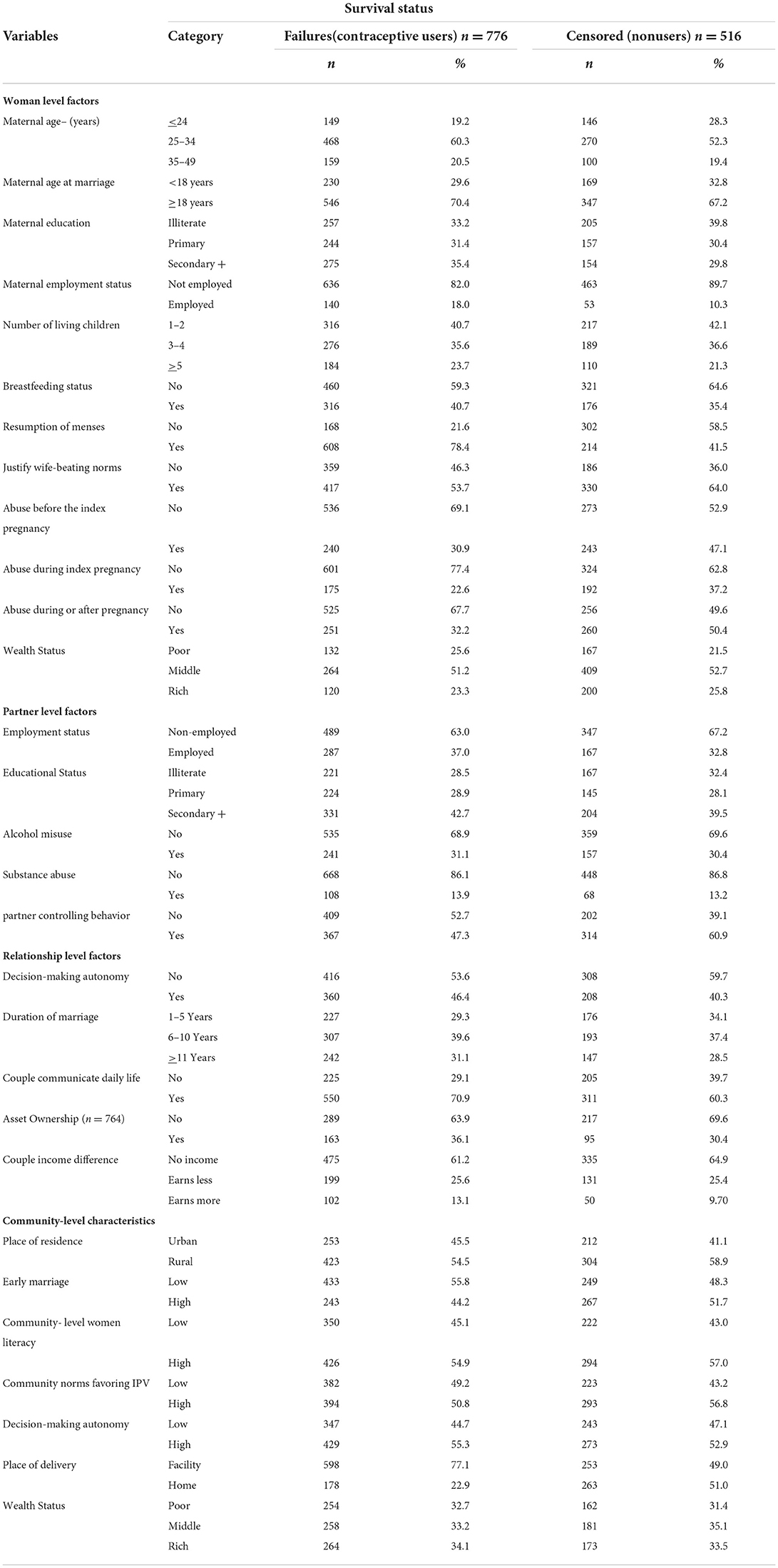
Table 1. Individual (women, partner and relationship) and community-level characteristics of study participants (n = 1292).
Postpartum women's contraceptive use dynamics in the Wolaita zone, Southern Ethiopia
Of the study participants, 62%(95% CI: 59.1%, 64.5%) had started the first postpartum modern contraception in the year postpartum (Table 2). Injectables (44.1%), pills (16.9%), and Implant (15.3%) were the most commonly used modern methods. More than one-third (33.1%) of women discontinued their first modern contraception after childbirth, and 57.6% did not use any methods after discontinuation. At the time of the survey, nearly half of the postpartum women were using contraceptives. Injectable was the most preferred method (47.2%), followed by Implants (25.7%) and IUCD (14.4%), with half (51.3%) reporting side effects from the current method, the majority of respondents (27.0%) stated that they intended to discontinue current methods.
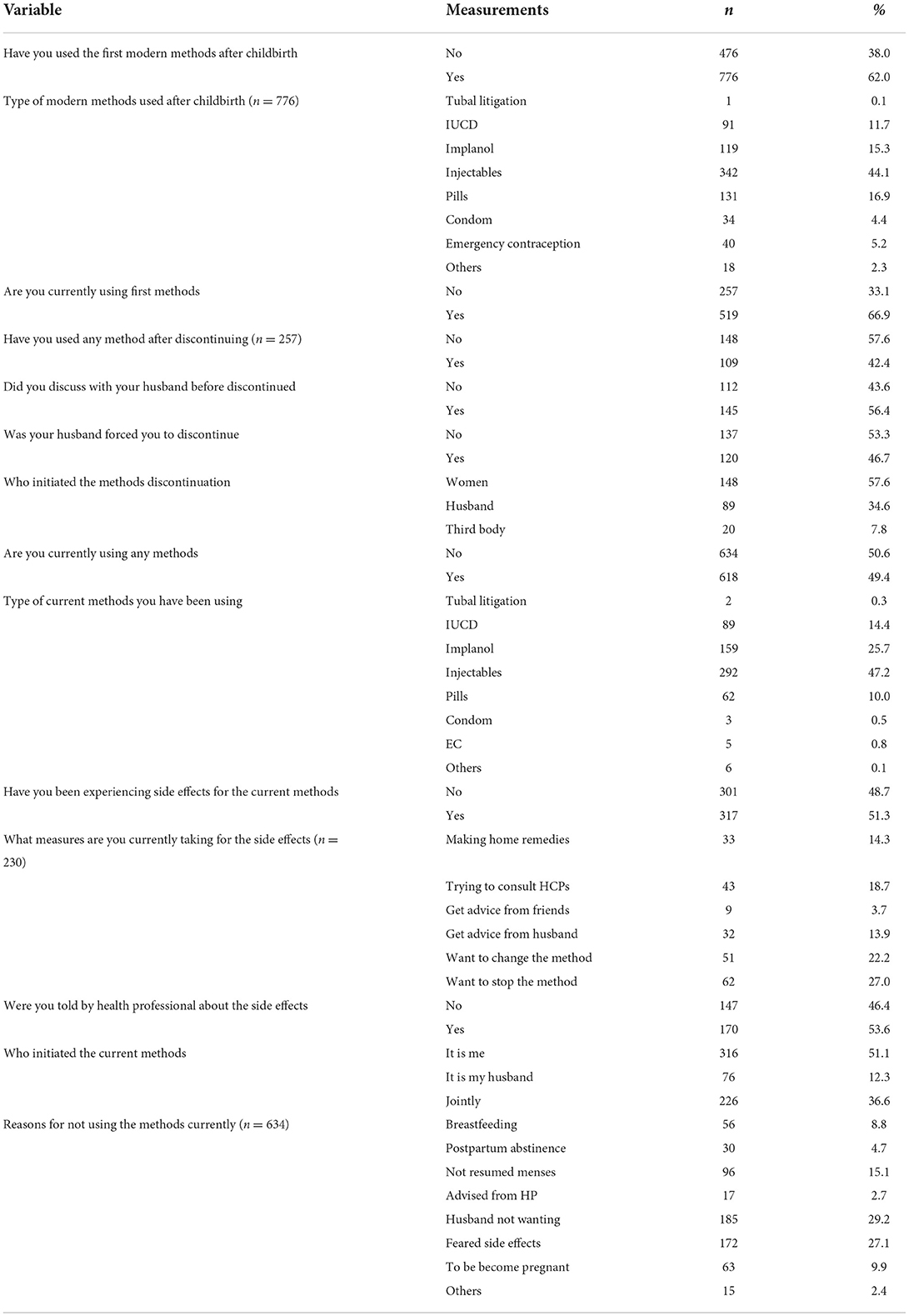
Table 2. Postpartum women's contraceptive use dynamics among currently married women in Wolaita zone, South Ethiopia.
Survival analysis result for time interval-to-modern contraception adoption among postpartum women
A total of 4,879 woman-months (407 women-years) were at risk of initiating modern contraception after index childbirth (Figure 1). The restricted mean survival time-to-first postpartum contraception was 6.28 months (95% CI: 6.07–6.51). At the 3 and 6 months postpartum, about 12.23 and 44.5% of the study participants had started their first modern methods, respectively. The Kaplan-Meier survival curves with large steps for time-to-postpartum contraceptive adoption start at 2 months postpartum. This indicates that many of postpartum women had started their first methods after 2 months.
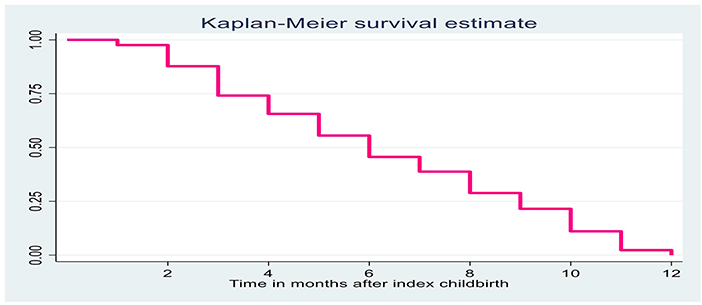
Figure 1. Kaplan Meier survival function curve for postpartum contraception timing after index childbirth among married women.
We examined postpartum modern contraception timing for selected characteristics using the Kaplan-Meier survival estimate (Figure 2). Kaplan-Meir survival curve indicates a substantial difference in postpartum contraceptive method adoption between women who experienced PIPV and women who did not experience PIPV. The Kaplan-Meier survival function for women who experienced perinatal violence is consistently higher than their counterparts revealing that violence exposure before or/and during pregnancy lengthens time duration to modern methods adoption. In addition, Wilcoxon log-rank test has shown a significant difference in the length of survival time-to-postpartum contraceptive use at individual and cluster-level characteristics (Table 3).
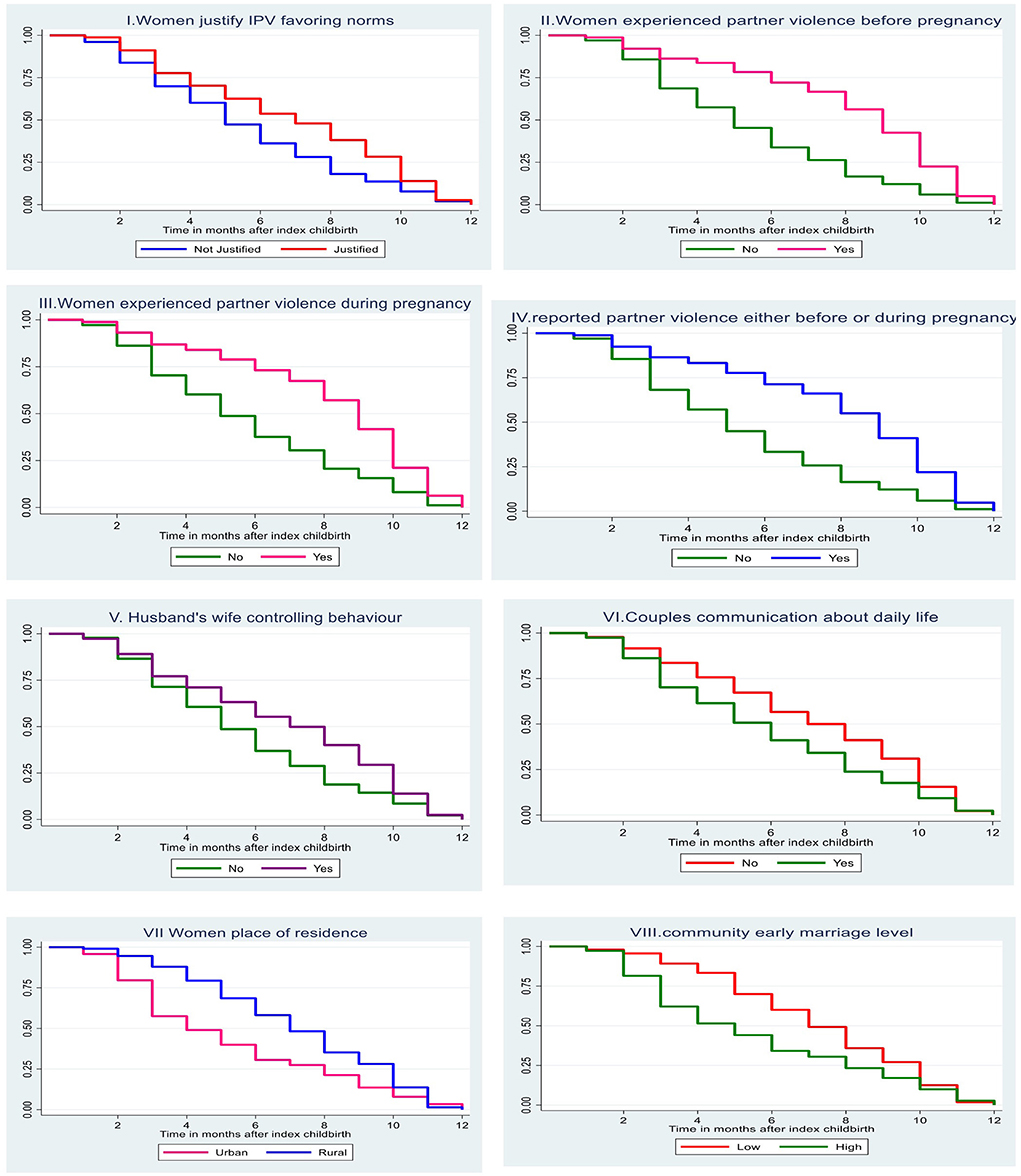
Figure 2. Kaplan-Meier estimate curves for postpartum contraception timing between index childbirth and 12 months by selected characteristics among married women.
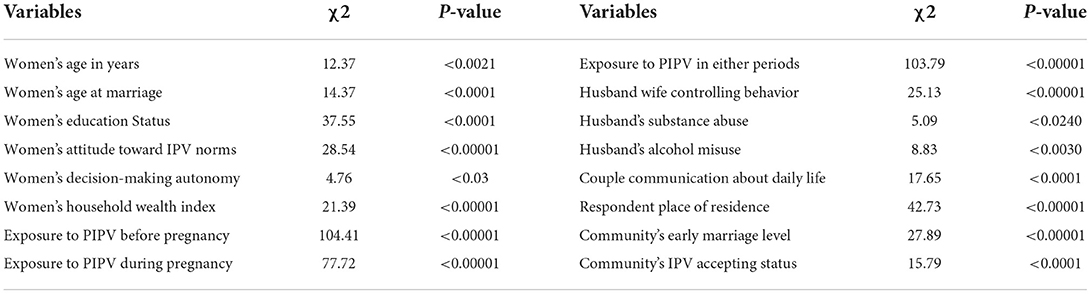
Table 3. Wilcoxon log-rank test for the length of time-to-postpartum contraception use among married women.
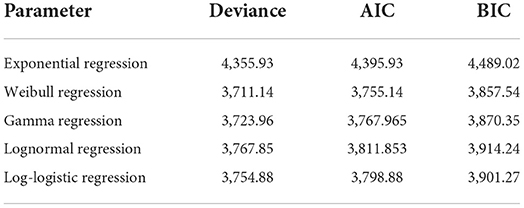
Model comparison for different parametric regression models based on the Akaike information criterion
We fitted different parametric survival models with different survival distribution for model selection: Exponential, Weibull, Gamma, Log-logistic, and lognormal. Weibull regression model was found to be the best-fitted model (Table 4). The ICC for the null model was computed using the variance of level-1 residual and variance of level-2(Keble) to identify the need of multilevel analysis (Table 5). The variance of the level-1(women) residuals is assumed to be independent and identically distributed, and their distributions depend on the model we are fitting. In the case of the Weibull distribution, the error term (residual) follows Gumbell distribution. We calculated residual variance using equation π2/(6 × ρ2), where ρ is the ancillary parameter of the Weibull distribution (52). ICC was found to be 0.805 indicates that 80.5% of the time length-to-postpartum contraceptive use can be explained by at cluster-level variance. In addition, the LR test was significant, which favored the multilevel Weibull regression model than standard Weibull model. Based on Akaike's Information Criterion (AIC), the full model was the most appropriate model that yielded the lowest deviance and AIC value, and selected to describe time-to- first postpartum contraceptive adoption.
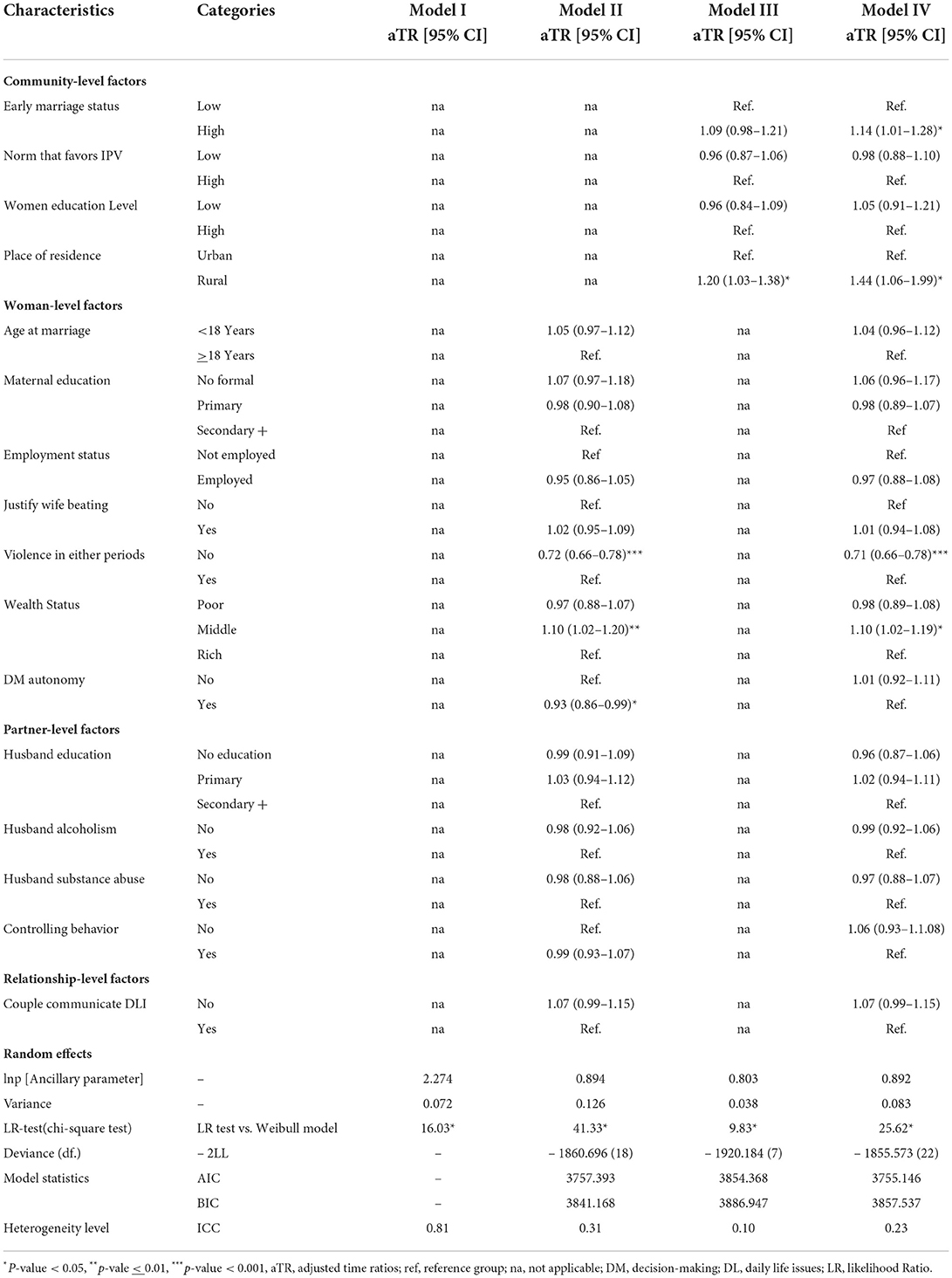
Table 5. Multivariable multilevel survival analysis of the postpartum contraceptive use timing among married women (n = 776).
Multivariate multilevel survival analysis for time duration-to-the first modern contraceptive adoption among postpartum women
After controlling for other covariates, place of residence, community early marriage status, household economic status, and history of perinatal abuse were found to be predictors for the length of time-to-first modern contraceptive adoption (Table 5). Women from the rural community took 44% expected longer time to adopt the first postpartum modern contraception compared to women from the urban community (aTR: 1.44; 95% CI: 1.06–1.99). Similarly, women from the community with high early marriage had a 14% lag time to first postpartum modern contraceptive use compared to women from the community with low early marriage (aTR:1.14; 95% CI: 1.01–1.28). Besides, we have also examined the impact of perinatal partner abuse exposure on the postpartum contraceptive adoption. Women who reported no partner abuse before or/and during pregnancy had 29% expected lesser time to start the first postpartum modern contraceptive method than women who experienced PIPV (aTR: 0.71; 95% CI: 0.66–0.78). Women from the middle wealth quintiles were taken 1.10 times longer time to initiate postpartum contraception compared to women from the richest wealth quintiles (aTR: 1.10; 95% CI: 1.02–1.19).
Discussion
This study has examined the individual- and community-level factors that predict the time duration of the first modern contraceptive adoption after childbirth, considering Keble as a cluster-level effect. The study found statistically significant heterogeneity in time interval-to-start modern methods across clusters. This finding indicates the influence of unobserved community-level characteristics, and is consistent with other studies that identified a woman's environment affects the timing of method use after childbirth (35). This implies the importance of leveraging community-level differences in planning intervention for timely modern contraceptive initiation. In the current study, 62.0% of women started using the first modern contraception in the year postpartum [95% CI: 59.1–64.5%]. This finding is consistent with studies conducted in Ethiopia (59.1%) and Kenya (60.0%) (35, 38). However, this estimate is considerably lower than other study done in Northwest Ethiopia (66.7%) (36) and higher than the nation-wide study done in Tanzania (37) and Ethiopia (56). We speculate that there may be differences in sample population characteristics, study design, and outcome variable measurement. For example, these nation-wide studies measured contraceptive adoption timing from the resumption of sexual intercourse, whereas our study examines the time length from delivery to the uptake of modern contraception. In this study, women's median survival time to start first postpartum modern contraception was found to be 6.3 months. This finding concurs with a study done in Northwest Ethiopia (36), but with at least 5 months' time lag than the WHO recommended time. This imply a sizeable proportion of postpartum women would be at risk of unintended pregnancy as many marks menses return to start contraception and requires community-based intervention during the perinatal and postpartum period.
Women's place of residence and their community early marriage status were predicted time interval-to-contraceptive use after childbirth when other variables were controlled for. As in other studies (56, 57), rural women took a long time to adopt modern methods postpartum than their counterparts. Our findings contrast somewhat with several prior studies (35, 37) that have identified no difference in time to modern contraceptive use among rural and urban residents. This might be correlated with rural women's limited access to media outlets, education, and health facilities infrastructure compared to urban women, which may also be associated with delayed adoption of modern contraception. This study was observed a long lag time to start contraception after childbirth among women from the community with high early marriage. This finding corroborates previous studies (58–60) that have identified early marriage is associated with a lower intention for postpartum contraceptive use. According to this study, women from middle wealth quantiles took longer time to start methods postpartum than women from the wealthiest households. This finding aligns with studies conducted elsewhere (37, 43) that show a shorter time to methods adoption among women in richest quintiles. The fact that low socioeconomic status is a deterrent to postpartum contraception adoption indicates a strengthening of social and community-based health insurance schemes launched by the government of Ethiopia, which increase health-care utilization among the poor (61). Besides, women empowerment could alleviate indirect costs like transportation for contraceptive use among low-in-come mothers even if contraceptive services are provided free of charge. Moreover, a quasi-experimental study by Deborah Sitrin et al. reported that integrating postpartum family planning into a health extension program could increase postpartum adoption of modern contraception (62).
There is inconsistency in the evidence regarding the association between intimate partner violence and the time interval-to-postpartum contraceptive initiations. While our finding confirms that women who had no history of perinatal abuse took less time to adopt modern contraception than those who had a history of abuse. For instance, Marina Plesons' prospective cohort study in Kenya shows a positive correlation between recent partner abuse and time to postpartum contraceptive adoption (63). As such, women's exposure to perinatal abuse may influence postpartum contraception timing in different ways: an abusive partner may restrict access to any form of contraception or prevent from using the most effective methods in an attempt to get the woman pregnant again (64, 65). Moreover, woman's less decisive power and fear of future violence linked with contraceptive initiation could deter timely adoption of the method after childbirth (66). This would imply intimate partner violence should be part of family planning counseling to identify a woman in a violent relationship which could significantly reduce the likelihood of future reproductive coercion.
In this community-based prospective study, applying the Weibull AFT model rather than the PH model to estimate expected survival times between group characteristics in time ratios may be the study's strength because estimated regression parameters in AFT models are robust and easy for interpretation of results. In addition to this significant strength, the finding should be interpreted with caution. The study had a limited follow-up period and frequency of interviews, which could be problematic given the persistence of protective factors like postpartum amenorrhea and abstinence. As this study is based on women's self-reported data collection methods, partner-characteristics and -controlled contraception may be underrepresented. A recent study did not address the timing of the contraceptive method mix. Although traditional methods are an important part of the pathways to avoid unwanted pregnancy, the scope of this study is very limited to identify traditional method users.
Conclusion
In conclusion, rural residence, low household wealth status, and a high rate of early marriage in the community are predicted to lengthen the time to start modern contraception methods. In addition, a woman who had a history of violence either a year before or during pregnancy took a longer time than their counterparts to adopt modern contraception after childbirth. Thus, community-level women's empowerment, particularly among rural women and integration of intimate partner violence screening program into family planning counseling throughout the continuum of care will likely to improve postpartum contraception timing.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Board of College of health sciences, Addis Ababa University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
TA has conceived the study, developed the proposal, conducted data collection and analysis, and drafted the manuscript. FG was involved in proposal development, fieldwork planning, and the result section. ND was involved in the proposal, data analysis and writing up and critical reviewing of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
Addis Ababa University, College of Health Sciences provided financial support for the data collection. It is a public university in Ethiopia and grants small amounts of money to Ph.D. candidates for data collection. Therefore, the university has no conflicts of interest in this study. No other funding was obtained for the current study.
Acknowledgments
The authors would like to thank the Addis Ababa University College of Health Sciences for providing small grants and ethical approval for this study. We are grateful to FG, one of our staff members, mentors, and supervisors, whom we unexpectedly lost during the manuscript preparation process; may his soul rest in perfect peace. We want to thank the Zonal and woreda health department staff for their cooperation and technical support. We are also indebted to HEWs for genuine support in the sampling of participants. We are also grateful to all data collectors, and study participants who participate in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Intimate Partner Violence During Pregnancy: Information Sheet. Geneva: World Health Organization (2011).
2. World Health Organization. Global and Regional Estimates of Violence Against Women: Prevalence And Health Effects of Intimate Partner Violence and Non-Partner Sexual Violence. Geneva: World Health Organization (2013).
3. McPhail W, Toiv H. Violence against women: data on pregnant victims an effectiveness of prevention strategies are limited. GAO Rep Honorable Eleanor Holmes Norton House Representat (GAO-2-530). (2002).
5. Shoffner DH. We don't like to think about it: intimate partner violence during pregnancy and postpartum. J Perinat Neonatal Nurs. (2008) 22:39–48. doi: 10.1097/01.JPN.0000311874.30828.4e
6. Silverman JG, Decker MR, Reed E, Raj A. Intimate partner violence victimization prior to and during pregnancy among women residing in 26 US states: associations with maternal and neonatal health. Am J Obstet Gynecol. (2006) 195:140–8. doi: 10.1016/j.ajog.2005.12.052
7. Hahn CK, Gilmore AK, Aguayo RO, Rheingold AA. Perinatal intimate partner violence. Obstetrics Gynecol Clinics. (2018) 45:535–47. doi: 10.1016/j.ogc.2018.04.008
8. Wadsworth P, Degesie K, Kothari C, Moe A. Intimate partner violence during the perinatal period. J Nurse Practition. (2018) 14:753–9. doi: 10.1016/j.nurpra.2018.08.009
9. Cripe SM, Sanchez SE, Perales MT, Lam N, Garcia P, Williams MA. Association of intimate partner physical and sexual violence with unintended pregnancy among pregnant women in Peru. Int J Gynecol Obstetrics. (2008) 100:104–8. doi: 10.1016/j.ijgo.2007.08.003
10. Gee RE, Mitra N, Wan F, Chavkin DE, Long JA. Power over parity: intimate partner violence and issues of fertility control. Am J Obstetrics Gynecol. (2009) 201:148e1–e7. doi: 10.1016/j.ajog.2009.04.048
11. Cha S, Chapman DA, Wan W, Burton CW, Masho SW. Intimate partner violence and postpartum contraceptive use: the role of race/ethnicity and prenatal birth control counseling. Contraception. (2015) 92:268–75. doi: 10.1016/j.contraception.2015.04.009
12. Kusunoki Y, Barber JS, Gatny HH, Melendez R. Physical intimate partner violence and contraceptive behaviors among young women. J Women's Health. (2018) 27:1016–25. doi: 10.1089/jwh.2016.6246
13. Kabir R, Kordowicz M. Exploring the relationship between intimate partner violence and contraception use by Tanzanian women. Health Care Women Int. (2021) 42:1220–33. doi: 10.1080/07399332.2020.1807552
14. Vinnakota D, Parsa AD, Sivasubramanian M, Mahmud I, Sathian B, Kabir R. Intimate partner violence and pregnancy termination among Tajikistan women: evidence from nationally representative data. Women. (2022) 2:102–14. doi: 10.3390/women2020012
15. Sonfield A, Hasstedt K, Kavanaugh ML, Anderson R. The Social and Economic Benefits of Women's Ability to Determine Whether and When to Have Children. New York: Guttmacher Institute. (2013).
16. Dehne KL, Snow R, O'Reilly KR. Integration of prevention and care of sexually transmitted infections with family planning services: what is the evidence for public health benefits? Bull World Health Organ. (2000) 78:628–39.
17. Gaffield ME, Egan S, Temmerman M. It's about time: WHO and partners release programming strategies for postpartum family planning. Global Health Sci. Practice. (2014) 2:4–9. doi: 10.9745/GHSP-D-13-00156
18. World Health Organization. Programming Strategies for Postpartum Family Planning. Geneva: World Health Organization (2013).
19. Cleland J, Conde-Agudelo A, Peterson H, Ross J, Tsui A. Contraception and health. Lancet. (2012) 380:149–56. doi: 10.1016/S0140-6736(12)60609-6
20. World Health Organization. Reproductive Health, World Health Organization, World Health Organization. Family, Community Health. Selected Practice Recommendations for Contraceptive use. Geneva: World Health Organization (2005).
21. High Impact Practices in Family Planning (HIPs). Immediate Postpartum Family Planning: A Key Component of Childbirth Care. (2017).
22. Moore Z, Pfitzer A, Gubin R, Charurat E, Elliott L, Croft T. Missed opportunities for family planning: an analysis of pregnancy risk and contraceptive method use among postpartum women in 21 low-and middle-income countries. Contraception. (2015) 92:31–9. doi: 10.1016/j.contraception.2015.03.007
23. Coker AL, Sanderson M, Dong B. Partner violence during pregnancy and risk of adverse pregnancy outcomes. Paediatr Perinat Epidemiol. (2004) 18:260–9. doi: 10.1111/j.1365-3016.2004.00569.x
24. Yost NP, Bloom SL, McIntire DD, Leveno KJ, A. prospective observational study of domestic violence during pregnancy. Obstetrics Gynecol. (2005) 106:61–5. doi: 10.1097/01.AOG.0000164468.06070.2a
25. McDougal L, Silverman JG, Singh A, Raj A. Exploring the relationship between spousal violence during pregnancy and subsequent postpartum spacing contraception among first-time mothers in India. EClin Med. (2020) 23:100414. doi: 10.1016/j.eclinm.2020.100414
26. Scribano PV, Stevens J, Kaizar E. The effects of intimate partner violence before, during, and after pregnancy in nurse visited first time mothers. Matern Child Health J. (2013) 17:307–18. doi: 10.1007/s10995-012-0986-y
27. Stevenson AA, Bauman BL, Zapata LB, Ahluwalia IB, Tepper NK. Intimate partner violence around the time of pregnancy and postpartum contraceptive use. Women's Health Issues. (2020) 30:98–105. doi: 10.1016/j.whi.2019.11.006
28. Steinberg JR, Harrison EY, Boudreaux M. Psychosocial factors associated with postpartum contraceptive method use after an unintended birth. Obstet Gynecol. (2020) 135:821. doi: 10.1097/AOG.0000000000003745
29. Mundhra R, Singh N, Kaushik S, Mendiratta A. Intimate partner violence: Associated factors and acceptability of contraception among the women. Indian J Commun Med Official Publ Indian Associat Prevent Soc Med. (2016) 41:203. doi: 10.4103/0970-0218.183589
30. Kuhlmann AS, Shato T, Fu Q, Sierra M. Intimate partner violence, pregnancy intention and contraceptive use in Honduras. Contraception. (2019) 100:137–41. doi: 10.1016/j.contraception.2019.03.050
31. United Nations Department for Economic and Social Affairs. Family Planning and the 2030 Agenda for Sustainable Development (data Booklet). UN (2019).
34. Wakuma B, Mosisa G, Etafa W, Mulisa D, Tolossa T, Fetensa G, et al. Postpartum modern contraception utilization and its determinants in Ethiopia: a systematic review and meta-analysis. PLoS ONE. (2020) 15:e0243776. doi: 10.1371/journal.pone.0243776
35. Emiru AA, Alene GD, Debelew GT. The role of maternal health care services as predictors of time to modern contraceptive use after childbirth in Northwest Ethiopia: application of the shared frailty survival analysis. PLoS ONE. (2020) 15:e0228678. doi: 10.1371/journal.pone.0228678
36. Mekonnen B, Gelagay A, Lakew A. Time to use modern contraceptives and associated factors among women in extended postpartum period in Gondar City, Northwest Ethiopia. Fam Med Med Sci Res. (2020) 9:243. doi: 10.2147/OAJC.S290337
37. Rwabilimbo MM, Elewonibi BR, Yussuf MH, Robert M, Msuya SE, Mahande MJ. Initiation of postpartum modern contraceptive methods: evidence from Tanzania demographic and health survey. PLoS ONE. (2021) 16:e0249017. doi: 10.1371/journal.pone.0249017
38. Mumah JN, Machiyama K, Mutua M, Kabiru CW, Cleland J. Contraceptive adoption, discontinuation, and switching among postpartum women in Nairobi's urban slums. Stud Fam Plann. (2015) 46:369–86. doi: 10.1111/j.1728-4465.2015.00038.x
39. Dona A, Abera M, Alemu T, Hawaria D. Timely initiation of postpartum contraceptive utilization and associated factors among women of child bearing age in Aroressa District, Southern Ethiopia: a community based cross-sectional study. BMC Public Health. (2018) 18:1–9. doi: 10.1186/s12889-018-5981-9
41. Agency CS. Population and Housing Census of Ethiopia: Statistical Report for Southern Nations, Nationalities and Peoples' Region (2007).
42. Cochrane L, Gecho Y. Data on the demographics, education, health and infrastructure: Wolaita zone, Ethiopia. Data in brief. (2018) 21:2095–102. doi: 10.1016/j.dib.2018.11.063
43. Wamala R, Kabagenyi A, Kasasa S. Predictors of time-to-contraceptive use from resumption of sexual intercourse after birth among women in Uganda. Int J Populat Res. (2017) 2017. doi: 10.1155/2017/3875452
44. Organization WH. WHO Multi-Country Study on Women's Health and Domestic Violence Against Women: Initial Results on Prevalence, Health Outcomes and Women's Responses. Geneva: World Health Organization (2005).
45. Central statistical agency (CSA)[Ethiopia] and ICF. Ethiopia Demographic and Health Survey. Addis Ababa, Ethiopia and Calverton, Maryland, USA (2016).
47. Callahan RL, Becker S. The reliability of calendar data for reporting contraceptive use: evidence from rural Bangladesh. Stud Fam Plann. (2012) 43:213–22. doi: 10.1111/j.1728-4465.2012.00319.x
48. Population EOot, Commission HC. Summary and Statistical Report of the 2007 Population and Housing Census: Population Size by Age and Sex: Federal Democratic. Republic of Ethiopia: Population Census Commission (2008).
49. Kim D, Lee Y, Leite WL, Huggins-Manley AC. Exploring student and teacher usage patterns associated with student attrition in an open educational resource-supported online learning platform. Comput Educ. (2020) 156:103961. doi: 10.1016/j.compedu.2020.103961
50. Austin PC. A tutorial on multilevel survival analysis: methods, models and applications. Int. Stat. Rev. (2017) 85:185–203. doi: 10.1111/insr.12214
51. Khanal SP, Sreenivas V, Acharya SK. Accelerated failure time models: an application in the survival of acute liver failure patients in India. Int J Sci Res. (2014) 3:161–66.
52. Canette I. In the spotlight: intraclass correlations after multilevel survival models. Stata News. (2016) 31:31.
53. Faruk A. The comparison of proportional hazards and accelerated failure time models in analyzing the first birth interval survival data. J Phys Conf Ser. (2018) 974:012008. doi: 10.1088/1742-6596/974/1/012008
54. Lam K, Ip D. REML and ML estimation for clustered grouped survival data. Stat Med. (2003) 22:2025–34. doi: 10.1002/sim.1323
55. World Health Organization. Putting Women First: Ethical and Safety Recommendations for Research on Domestic Violence Against Women. Geneva: World Health Organization (2001).
56. Ahmed M, Seid A. Survival time to modern contraceptive uses from the resumption of sexual intercourse among postpartum women in Ethiopia. Int J Women's Health. (2020) 12:641. doi: 10.2147/IJWH.S266748
57. Ekholuenetale M, Olorunju S, Fowobaje KR, Onikan A, Tudeme G, Barrow A. When do nigerian women of reproductive age initiate and what factors influence their contraceptive use? A contextual analysis open access. J Contracept. (2021) 12:133. doi: 10.2147/OAJC.S316009
58. Dingeta T, Oljira L, Worku A, Berhane Y. Low contraceptive utilization among young married women is associated with perceived social norms and belief in contraceptive myths in rural Ethiopia. PLoS ONE. (2021) 16:e0247484. doi: 10.1371/journal.pone.0247484
59. Islam MM, Khan MN, Rahman MM. Factors affecting child marriage and contraceptive use among Rohingya girls in refugee camps. Lancet Regional Health-Western Pacific. (2021) 12:100175. doi: 10.1016/j.lanwpc.2021.100175
60. Costenbader E, Zissette S, Martinez A, LeMasters K, Dagadu NA, Deepan P, et al. Getting to intent: are social norms influencing intentions to use modern contraception in the DRC? PLoS ONE. (2019) 14:e0219617. doi: 10.1371/journal.pone.0219617
61. Atnafu DD, Tilahun H, Alemu YM. Community-based health insurance and healthcare service utilisation, North-West, Ethiopia: a comparative, cross-sectional study. BMJ Open. (2018) 8:e019613. doi: 10.1136/bmjopen-2017-019613
62. Sitrin D, Jima GH, Pfitzer A, Wondimu C, Belete TW, Pleah T, et al. Effect of integrating postpartum family planning into the health extension program in Ethiopia on postpartum adoption of modern contraception. J Global Health Rep. (2020) 4:e2020058. doi: 10.29392/001c.13511
63. Plesons M. Postpartum Contraception Initiation, Discontinuation, and Method Switch in Western Kenya (2017).
64. Thiel d, Bocanegra H, Rostovtseva DP, Khera S, Godhwani N. Birth control sabotage and forced sex: experiences reported by women in domestic violence shelters. Violence Against Women. (2010) 16:601–12. doi: 10.1177/1077801210366965
65. Miller E, Decker MR, McCauley HL, Tancredi DJ, Levenson RR, Waldman J, et al. Pregnancy coercion, intimate partner violence and unintended pregnancy. Contraception. (2010) 81:316–22. doi: 10.1016/j.contraception.2009.12.004
Keywords: perinatal, postpartum, contraception, multilevel, survival, Ethiopia
Citation: Abota TL, Gashe FE and Deyessa N (2022) Perinatal intimate partner violence and postpartum contraception timing among currently married women in Southern Ethiopia: A multilevel Weibull regression modeling. Front. Public Health 10:913546. doi: 10.3389/fpubh.2022.913546
Received: 05 April 2022; Accepted: 30 September 2022;
Published: 19 October 2022.
Edited by:
Ashwani Kumar Mishra, All India Institute of Medical Sciences, IndiaReviewed by:
John Allen Ross, Independent Researcher, New Paltz, United StatesRussell Kabir, Anglia Ruskin University, United Kingdom
Copyright © 2022 Abota, Gashe and Deyessa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tafesse Lamaro Abota, bGFtYXJvLnRhZmVzc2VAeWFob28uY29t
†Deceased
 Tafesse Lamaro Abota
Tafesse Lamaro Abota Fikre Enqueselassie Gashe2†
Fikre Enqueselassie Gashe2† Negussie Deyessa
Negussie Deyessa