- 1Experimental Management Center, Shanxi University of Chinese Medicine, Jinzhong, China
- 2Respiration Department, Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 3Department of Chinese Medicine, Shanxi Provincial People's Hospital, Taiyuan, China
Background: Transcutaneous electrical nerve stimulation over an acupoint (acu-TENS), a new technique applied in pulmonary rehabilitation programs, has been gradually used in the management of chronic obstructive pulmonary disease (COPD). However, the effects of acu-TENS have not been fully evaluated. Therefore, this review was conducted to assess the effects of acu-TENS on COPD.
Methods: A total of seven electronic databases were searched from their inception to September 2021 for randomized controlled trials of acu-TENS for COPD. Two investigators independently performed data extraction and methodological quality assessment. Heterogeneity was examined by Cochrane χ2 and I2 tests. The source of heterogeneity was investigated by subgroup analysis or sensitivity analysis.
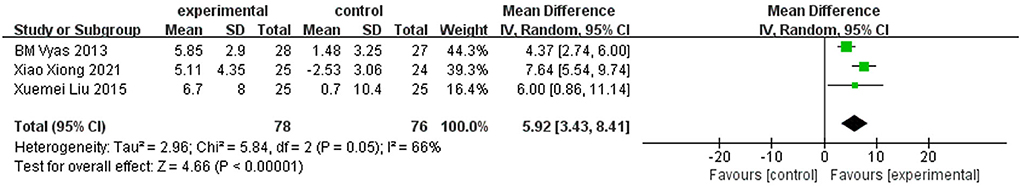
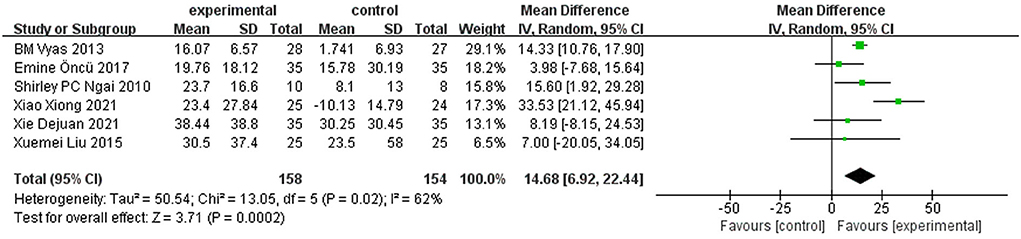
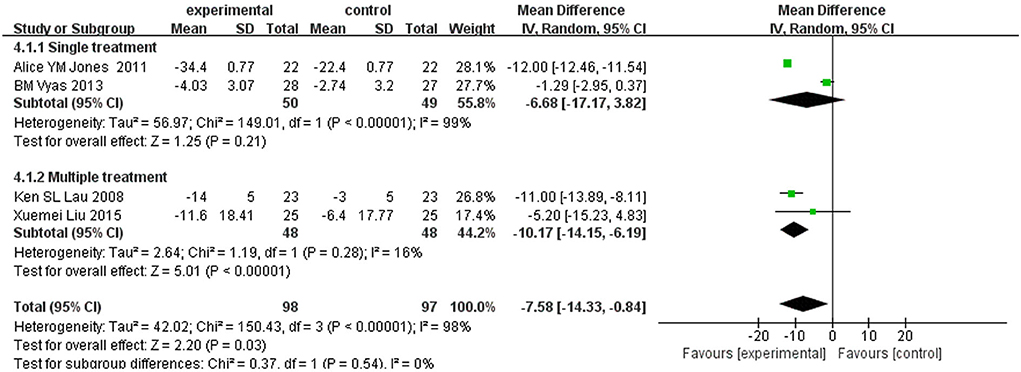
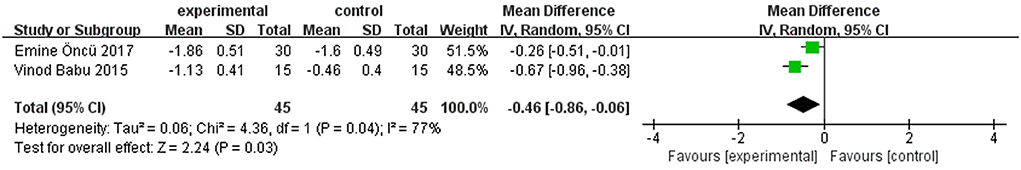
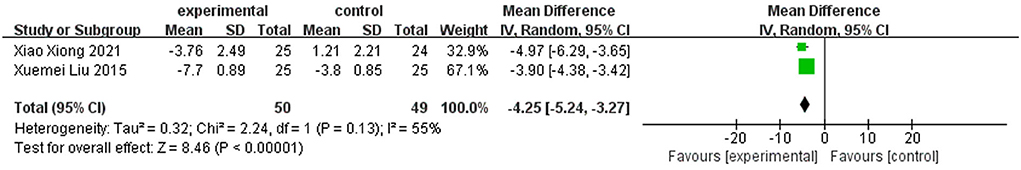
Results: In our review, ten studies between 2008 and 2021 were included. The aggregated results indicated that acu-TENS showed positive effects in forced expiratory volume in 1 s (FEV1) [MD = 0.13 L, 95% CI (0.11–0.16), P < 0.00001], FEV1% predicted [MD = 5.92%, 95% CI (3.43–8.41), P < 0.00001], 6-min walk distance (6MWD) [MD = 14.68m, 95% CI (6.92–22.44), P = 0.0002], dyspnea visual analog scale (DVAS) [MD = −7.58, 95%CI (−14.33 to −0.84), P = 0.03], modified Borg scale (MBS) [MD = −0.46, 95% CI (−0.86 to −0.06), P = 0.03], and COPD assessment test (CAT) [MD = −4.25, 95% CI (−5.24 to −3.27), P < 0.00001]. Although six studies reported adverse effects, only one patient had shoulder pain after acu-TENS.
Conclusion: Acu-TENS seems to be effective in improving pulmonary function and health status in patients with COPD, with little effect on exercise capacity and dyspnea. However, this result should be interpreted with caution, and high-quality RCTs were needed for further verification.
Introduction
Chronic obstructive pulmonary disease (COPD) is a debilitating chronic illness characterized by sustained airflow obstruction and recurrent respiratory symptoms. Statistically, 3.2 million people died of COPD in 2015, making it the third leading cause of death worldwide (1). Therefore, effective prevention, management, and treatment of COPD remain one of the major tasks for public health worldwide. In the therapy of COPD, a pulmonary rehabilitation program is regarded as a hallmark of treatment for all patients (2). Evidence suggests that it can improve exercise capacity and reduce both fatigue and dyspnea in patients with COPD (3, 4).
Transcutaneous electrical nerve stimulation over acupoints (acu-TENS) is a new technique used in pulmonary rehabilitation programs (5). It combines acupoint stimulation therapy with transcutaneous electrical nerve stimulation (TENS), which has similar analgesic effects and peripheral and central effects as acupuncture (6). Unlike traditional acupuncture, acu-TENS is a noninvasive, easy-to-apply intervention that induces therapeutic effects through the application of surface electrodes over the specific acupoints instead of needles (5).
In recent years, acu-TENS has been gradually applied to the treatment of patients with COPD. Limited evidence suggests that acu-TENS can improve the dyspnea of patients with COPD during walking, especially those with more severe dyspnea during peak exercise (7). In addition, Shirley et al. (8) found that acu-TENS can improve the expiratory flow rates after exercise in healthy subjects. However, most of the reports on the intervention effect of acu-TENS on COPD are clinical trials with small sample sizes, which make it difficult to draw reliable conclusions. Considering that the evidence for acu-TENS in patients with COPD has not been systematically reviewed, this meta-analysis aims to analyze the clinical efficacy of acu-TENS and provide certain guidance for clinical application and further research.
Methods
This systematic review and meta-analysis were performed following the guidelines of PRISMA (9).
Search strategy
Literature retrieval was performed by two researchers independently. To capture as many studies as possible, the following electronic databases were searched: PubMed, Cochrane Library, Embase, Web of Science, China Network Knowledge Infrastructure (CNKI), Wanfang Database, and VIP Database. All databases were searched from inception to September 2021. Literature references were also checked for the existence of eligible studies. In terms of retrieval strategy, we adopted a combination of medical subject heading (MeSH) terms and free words. There were no restrictions on language or publication status.
Study selection
The selection of studies was performed independently by two researchers, and any disagreements arising were resolved through discussion. In this review, the included studies met the following criteria: (a) randomized controlled trials (RCTs). (b) Participants were diagnosed with COPD, and there were no restrictions on COPD type, GOLD grade, age, gender, or nationality. (c) Acu-TENS was used as an intervention. Thus, the control interventions included conventional treatment for COPD, placebo TENS (i.e., transcutaneous electrical nerve stimulation over an acupoint without current output), or sham TENS (i.e., transcutaneous electrical nerve stimulation over a non-acupoint). In the treatment group, a combination of acu-TENS and control interventions, or acu-TENS alone, were allowed. (d) The outcome indicators included pulmonary function index assessed by the forced expiratory volume in 1 s (FEV1) and FEV1% predicted; exercise capacity assessed by 6MWD; health status assessed by CAT; and dyspnea assessed by MBS and DVAS. Literature retrieved from databases was imported into Endnote X7. By assessing the titles, abstracts, and full texts, eligible studies were included.
Data extraction
Data extraction was performed independently by two researchers based on a pre-formulated data extraction form, and any discrepancies were resolved by discussion. The following information was extracted: first author, publication date, and country; the number of participants; duration of disease; COPD type; GOLD grade; interventions of the treatment group; interventions of the control group; acupoint; parameters of TENS; course of treatment; outcome indicators; safety; and funding. If necessary, the authors were contacted by email for relevant information.
Quality assessment
The methodological quality of the included studies was assessed by two researchers independently using the revised Cochrane risk of bias tool (RoB 2) (10). Any objections raised by the two reviewers were solved through discussion. The risk of bias was evaluated via process randomization, deviations from intended interventions, missing outcome data, measurement of outcome, and selection of reported results. The study was considered “low risk of bias” only if all five aspects were assessed as low risk. However, the study was considered to have “some concerns of bias” if at least one item was judged to have some concerns. The study was considered to be a “high risk of bias” if at least one item was judged as high risk.
Data synthesis and analysis
Data were analyzed using Review Manager 5.3. There are two methods for meta-analysis of continuous variables: inverse-variance fixed effect method and inverse-variance random-effect method. The effect estimation of continuous variables was represented by mean difference (MD) and 95% confidence interval (CI). Heterogeneity was examined by Cochrane X2 and I2 tests. A fixed effect model was adopted if the heterogeneity was not significant; otherwise, a random-effect model was adopted (11). The source of heterogeneity was investigated by subgroup analysis or sensitivity analysis. In addition, if there were 10 or more RCTs, publication bias was tested by funnel plots and Egger's tests.
Results
Search results and study characteristics
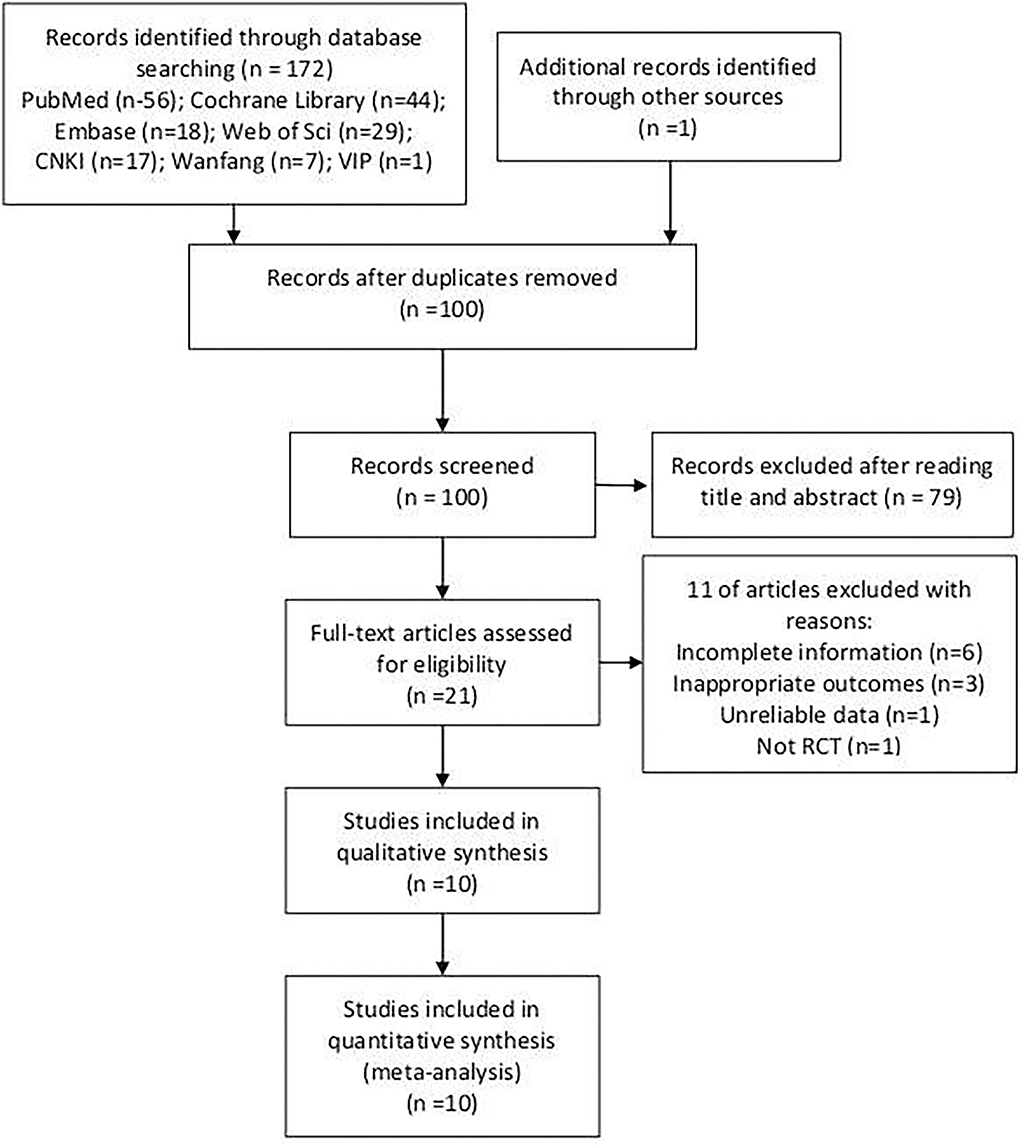
A total of 172 studies have been searched from seven databases, and 1 eligible study was found in the literature references. After removing replicates, 100 potentially relevant studies were identified. A total of 79 studies were deleted after reading the titles and abstracts. The full text of the remaining 21 studies was assessed, and 11 studies were excluded according to the inclusion criteria or the exclusion criteria. Finally, 10 studies were included in this meta-analysis (12–21). The detailed process is depicted in Figure 1.
Characteristics of the included studies
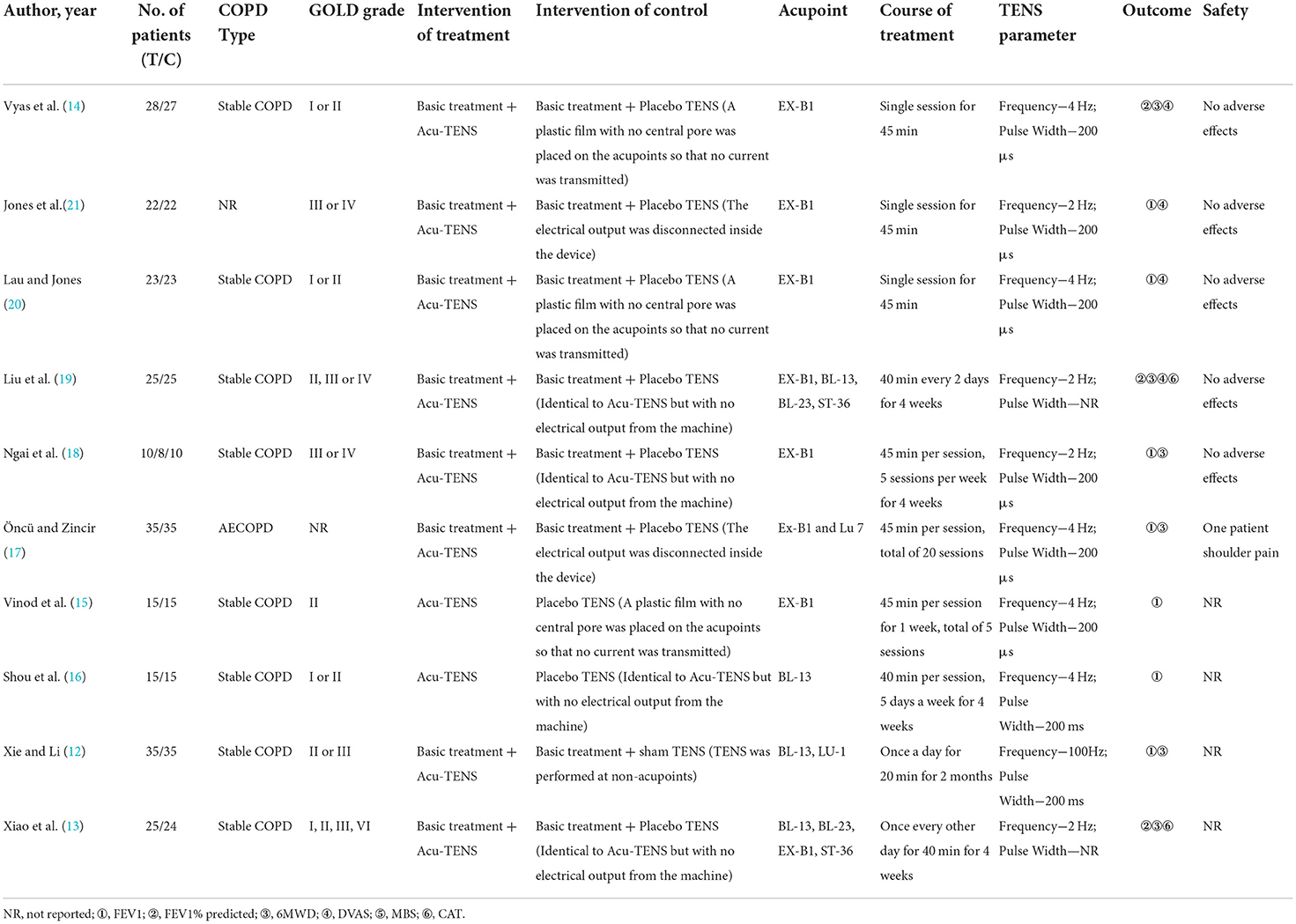
A total of 472 patients were included, including 233 in the treatment group and 239 in the control group. The studies, published between 2008 and 2021, were conducted mainly in China, India, and Turkey. The age of patients with COPD ranged from 42 to 85 years, with an average course of 5–42 years. Among the studies, eight included patients with stable COPD, one included patients with acute exacerbation of COPD, and one did not mention the stage of COPD. In terms of acupoints, five studies applied TENS over EX-B1, one applied over BL-13, and four applied over multiple acupoints. In terms of the course of treatment, three studies received a single session of acu-TENS, and the remaining studies received multiple sessions of acu-TENS. The specific characteristics of included studies are presented in Table 1.
Methodological quality
As shown in Figure 2, three studies had a high risk of bias (12, 16, 17), and seven showed some concern about bias (13–15, 18–21). Except for two studies (12, 16), the remaining studies reported the method of random sequence generation and the process of assigning concealment in detail. Since the vast majority of subjects completed the intervention, two studies (13, 17) showed deviations from the intended interventions and were judged to be of “some concerns”. In terms of missing outcome data, only one study (17) had < 90% of available outcome data. For the selective report, the judgment could not be made since none of the included trials were publicly registered or published their protocols. In summary, the missing outcome data, deviations from the intended intervention, and the selection of reported results were the main factors that limited the quality of studies.
Synthesis of the results
FEV1
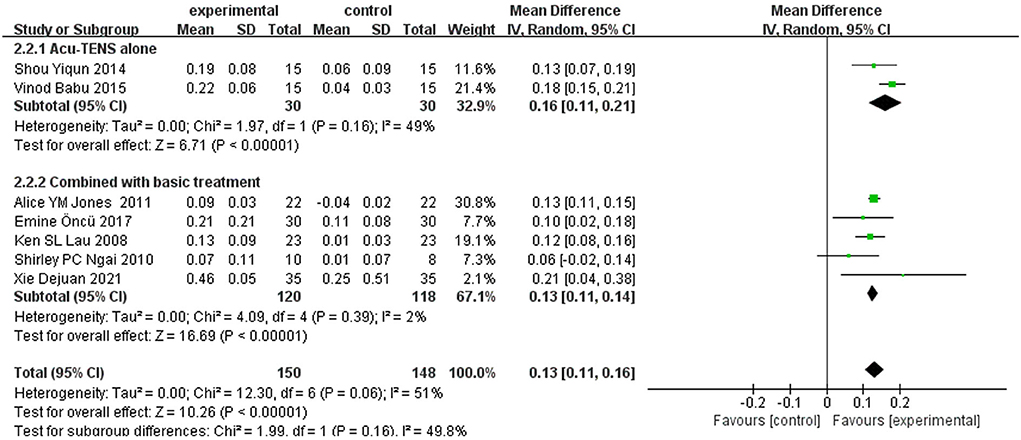
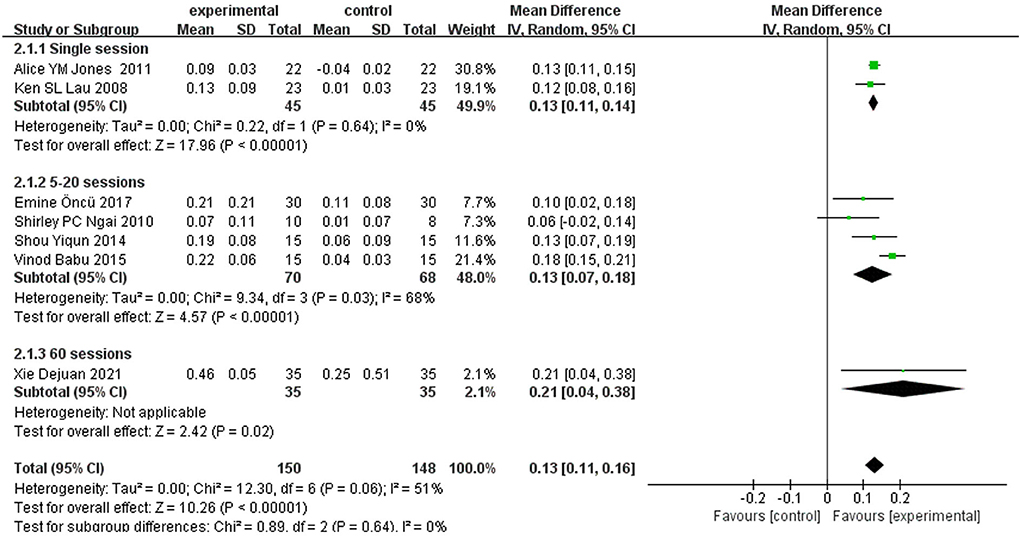
A total of seven (12, 15–18, 20, 21) studies reported FEV1 as an outcome. Due to the results of heterogeneity test (I2 = 51%, P = 0.06), a random-effect model was adopted. Meta-analysis showed that the experimental group can significantly increase FEV1 in patients with COPD [MD = 0.13 L, 95% CI (0.11–0.16), P < 0.00001]. As a rule of thumb, tests of funnel plot asymmetry should not be performed when fewer than 10 studies were included, because the power of tests was too low to distinguish chance from real asymmetry. To explore the possible sources of heterogeneity, subgroup analyses were conducted according to different intervention strategies (acu-TENS alone or combined with basic treatment, Figure 3) and the courses of treatment (single session, 5–20 sessions, or 60 sessions, Figure 4). Results showed that the therapeutic effect of acu-TENS on FEV1 may not be influenced by the intervention strategies and courses of intervention (test for subgroup differences: P all > 0.05).
However, subgroup analysis was not effective in reducing heterogeneity. Therefore, sensitivity analysis was performed by eliminating studies one by one to investigate the possible sources of heterogeneity. The sensitivity analysis of FEV1 showed that the heterogeneity was reduced (I2 = 0%, P = 0.54) after removing the article by Vinod et al. (15). A fixed-effect model was used to analyze the other six studies, and the result for FEV1 showed an improvement of 0.13 L in the experimental group compared with the control group [MD = 0.13 L, 95% CI (0.11–0.14), P < 0.00001].
FEV1% predicted
Among the included RCTs, three (13, 14, 19) reported FEV1% predicted as an outcome. Due to the obvious heterogeneous (I2 = 66%, P = 0.05), a random-effect model was used. Meta-analysis revealed that the treatment group can significantly increase FEV1% predicted in patients with COPD [MD = 5.92%, 95% CI (3.43–8.41), P < 0.00001] (Figure 5). The sensitivity analysis of FEV1% predicted showed that the heterogeneity was reduced (I2 = 0%, P = 0.56) after removing the article by Vyas et al. (14). A fixed-effect model was used to analyze the other two studies, and the result for FEV1% predicted showed an improvement of 7.41% in the experimental group compared with the control group [MD = 7.41, 95% CI (5.46–9.35), P < 0.00001].
6-min walk distance
A total of six trials (12–14, 17–19) reported 6-min walk distance (6MWD) as an outcome. The random-effect model was adopted according to the results of heterogeneity test (I2 = 62%, P = 0.02). Meta-analysis showed that the treatment group can significantly increase 6WMD in patients with COPD [MD = 14.68 m, 95% CI (6.92–22.44), P = 0.0002] (Figure 6). The sensitivity analysis of 6MWD showed that the heterogeneity was reduced (I2 = 0%, P = 0.48) after removing the article by Xiao et al. (13). A fixed-effect model was used to analyze the other five studies, and the result for 6MWD showed an improvement of 13.27 m in the experimental group compared with the control group [MD = 13.27 m, 95% CI (10.04–16.49), P < 0.00001].
Dyspnea visual analog scale
Among the included studies, four (14, 19–21) reported dyspnea visual analog scale (DVAS) as an outcome. Because of the significant heterogeneity (I2 = 98%, P < 0.00001), a random-effect model was chosen. Meta-analysis showed that the treatment group can significantly decrease the scores of DVAS in patients with COPD [MD = −7.58, 95% CI (−14.33 to −0.84), P = 0.03] (Figure 7). Subgroup analysis of different courses suggested that there was no significant difference between subgroups (test for subgroup differences: P = 0.54).
However, subgroup analysis was not effective in reducing heterogeneity. Therefore, sensitivity analysis was performed, and the heterogeneity was reduced (I2 = 9%, P = 0.33) after removing the article by Vyas et al. (14). A fixed-effect model was used to analyze the other three studies, and the result for DVAS showed a statistical reduction of 11.96 points in the experimental group compared with the control group [MD = −11.96, 95% CI (−12.41 to −11.51), P < 0.00001].
Modified borg scale
Among the included studies, two (15, 17) reported the modified Borg scale (MBS) as an outcome. Due to the significant heterogeneity between studies (I2 = 77%, P = 0.04) and the inability to exclude individual studies for sensitivity analysis, a random-effect model was chosen. Meta-analysis showed that the experimental group can statistically decrease the scores of MBS in patients with COPD [MD = −0.46, 95% CI (−0.86 to −0.06), P = 0.03] (Figure 8).
COPD assessment test
The results of acu-TENS on COPD assessment test (CAT) were reported in two studies (13, 19). Due to the high heterogeneity between studies (I2 = 55%, P = 0.13) and the inability to exclude individual studies for sensitivity analysis, a random-effect model was adopted. Meta-analysis showed that the experimental group can significantly decrease the scores of CAT in patients with COPD [MD = −4.25, 95% CI (−5.24 to −3.27), P < 0.00001] (Figure 9).
Adverse effects
Among the included studies, five reported that no adverse events occurred (14, 18–21); one study reported that one patient had shoulder pain after acu-TENS (17); and the remaining studies did not mention adverse events (12, 13, 15, 16).
Discussion
As we all know, systematic reviews and meta-analyses supply the highest levels of clinical evidence (22). In this review, the clinical evidence of acu-TENS in the treatment of COPD was systemically collected and evaluated for the first time to provide better guidance for clinical treatment. The main results indicated that acu-TENS was associated with a statistical improvement in pulmonary function, 6MWD, dyspnea, and the scores of the CAT in COPD patients. However, not all statistically significant differences are clinically relevant (23). The minimal clinically important difference (MCID) is the bridge between statistics and the clinical establishment and is the latest standard for determining the effectiveness of clinical trial interventions (24). Any amount of change that exceeds the MCID threshold is considered significant or important (25).
The pulmonary function test (PFT) is a common examination method in the respiratory department, which is crucial for diagnosis, evaluating therapeutic effects, and predicting perioperative risk and prognosis of COPD (26–28). One study reported that loss of lung function in older adults may lead to ventilation restriction during exercise, which reduces the accumulation of health benefits from physical activity (29). In this review, the level of changes in FEV1 exceeded the MCID of 100 ml (30), which suggested that these changes were clinically significant. Due to the lack of reported studies on the MCID value of FEV1% predicted, it was difficult to judge whether the statistical improvement of FEV1% predicted by acu-TENS is clinically significant. As a submaximal exercise test, the 6-min walk distance (6MWD) is mainly used to assess the physical performance of daily activities in patients with COPD (31). Studies have suggested that a 6MWD of less than 350 m or a decrease of 30 m or more within 1 year was significantly associated with higher mortality in patients with COPD (32, 33). Our results showed that the changes in 6MWD did not reach the MCID of 26 m (34), which indicated that these improvements in patients with COPD were insufficient evidence to support acu-TENS benefiting exercise capacity.
The COPD assessment test (CAT) is designed to evaluate the general health status of COPD patients and is widely used in clinical practice due to its excellent measurement properties (35). The meta-analysis showed that acu-TENS was associated with a statistically significant reduction in the score of CAT. Furthermore, the overall effect size of CAT exceeded the MCID by 2 points (36), which suggested that acu-TENS therapy has clinical benefits on the health status of patients with COPD. Dyspnea is one of the most common and distressing symptoms of various pulmonary diseases. Research has found that the severity of dyspnea is significantly related to decreased quality of life and survival rate (37). In this review, acu-TENS showed statistically significant improvement in dyspnea assessed by the MBS and DVAS. However, it is important to note that Ekstrom et al. (38) pointed out that an improvement of about 10 mm in a 100 mm VAS was clinically significant for chronic dyspnea, and the overall effect size of DVAS in this analysis was lower than the MCID of 10 mm. As for the MCID of MBS, there is still a lack of relevant research reports. In this context, we concluded that acu-TENS has little effect on the improvement of dyspnea in patients with COPD.
The TENS device is a hand-held, battery-powered machine that delivers pulsed currents by using electrode pads (39). Based on the acupuncture-like efficacy of TENS (40), researchers placed TENS electrodes on acupoints, known as acu-TENS. As a noninvasive and cost-efficient option, acu-TENS has become a common alternative therapy to acupuncture (41). Our meta-analysis showed that acu-TENS treatment can improve the pulmonary function indicators and health status in COPD patients with minimal benefit on exercise capacity and dyspnea. Acupuncture and acu-TENS are two different forms of acupoint stimulation therapy, but the results of studies on their efficacy in patients with COPD are not completely consistent. According to the review by Wang et al. (42), acupuncture can not only improve the pulmonary function index of patients with COPD but also improve their exercise ability and alleviate breathlessness. However, the degree of improvement in dyspnea and exercise capacity in our meta-analysis was not clinically significant, thus further confirmation is still needed. Ngai et al. (18) found that β-endorphin levels increased significantly in the acu-TENS group after treatment but not in the placebo-TENS and sham-TENS groups, suggesting that the release of opioids induced by TENS may depend on acupoint stimulation. Furthermore, research has found that stimulation of opioid receptors could enhance the relaxation of canine airway smooth muscle mediated by beta-adrenal receptors (43). This may be one of the mechanisms of acu-TENS in the treatment of COPD. However, the mechanisms of acu-TENS still need further study.
Limitations and implications
In this review, some deficiencies should not be ignored. First, only a small number of RCTs were included, and they were all single-center and small-sample studies. Second, due to the incomplete information reported by studies and the deficiencies in study design, the methodological quality of included studies was generally low. Third, since few studies were included, no publication bias was tested. However, the possibility of publication bias cannot be excluded since none of the trials were publicly registered. Fourth, it is important to ensure that the acu-TENS is safe. However, about half of the studies did not report adverse reactions, which affected the judgment of safety. Fifth, since no studies have reported follow-up, the long-term efficacy of acu-TENS is unclear.
This meta-analysis found several typical problems in this study, and addressing these problems will be of great help to enhance the quality of TCM research. First, although RCTs are the best method to evaluate the efficacy of interventions, low-quality RCTs can lead to incorrect assessments. Thus, future research on acu-TENS should focus on the registration of clinical trials, which can make research information more transparent, reduce publication bias, and improve the credibility of TCM research. Second, as the incomplete research report is one of the reasons for the waste of TCM research, we suggest that future research on acu-TENS should be reported in accordance with the statement of CONSORT (44). Finally, the occurrence of adverse reactions is related to the lack of enough attention to safety. Therefore, more attention should be paid to the safety of acu-TENS in future studies.
Conclusion
Considering the available data, this meta-analysis concluded that acu-TENS seems to be effective in improving pulmonary function and health status in patients with COPD, with little effect on exercise capacity and dyspnea. However, the results should be interpreted with caution, limited by the number and methodological quality of the included studies, and high-quality RCTs are needed in the future to investigate the efficacy and safety of acu-TENS.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
YW and YD: design, investigation, manuscript writing, and supervision. LW and JD: methodology, verification, and analysis. NY: verification, writing, and editing. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Soriano JB, Abajobir AA, Abate KH, Abera SF, Agrawal A, Ahmed MB, et al. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet Resp Med. (2017) 5:691–706. doi: 10.1016/s2213-2600(17)30293-x
2. Zhang H, Hu D, Xu Y, Wu L, Lou L. Effect of pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis of randomized controlled trials. Ann Med. (2022) 54:262–73. doi: 10.1080/07853890.2021.1999494
3. Ries AL, Bauldoff GS, Carlin BW, Casaburi R, Emery CF, Mahler DA, et al. Pulmonary rehabilitation: joint ACCP/AACVPR evidence-based clinical practice guidelines. Chest. (2007) 131:4s−42s. doi: 10.1378/chest.06-2418
4. Altenburg WA, de Greef MH, Ten Hacken NH, Wempe JB. A better response in exercise capacity after pulmonary rehabilitation in more severe COPD patients. Respir Med. (2012) 106:694–700. doi: 10.1016/j.rmed.2011.11.008
5. Elnaggar RK, Moawd SA, Ali SE, Yousef AM, Azab AR. Potential impacts of Acu-TENS in the treatment of adolescents with moderate to severe bronchial asthma: a randomized clinical study. Compl Ther Med. (2021) 57:102673. doi: 10.1016/j.ctim.2021.102673
6. Mingyang W, Chengwei Y, Mingming H, Tao H, Fang K, Juan L. Effect of transcutaneous electric acupoint stimulation on prognosis in patients at high risk of postop-erative pulmonary complications. Chin J Anesthesiol. (2017) 37:1287–90. doi: 10.3760/cma.j.issn.0254-1416.2017.11.002
7. Ngai SP, Spencer LM, Jones AY, Alison JA. Acu-TENS reduces breathlessness during exercise in people with chronic obstructive pulmonary disease. Evid Based Compl Alternat Med eCAM. (2017) 2017:3649257. doi: 10.1155/2017/3649257
8. Ngai SP, Jones AY, Hui-Chan CW. Acu-TENS and postexercise expiratory flow volume in healthy subjects. Evid Based Compl Alternat Med eCAM. (2011) 2011:726510. doi: 10.1155/2011/726510
9. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
10. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ (Clin Res Ed). (2019) 366:l4898. doi: 10.1136/bmj.l4898
11. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
12. Xie D, Li X. Clinical effect of TENS at Shu-and Mu-acupoints in the treatment of COPD. China Pract. Med. (2021) 16:175–7.
13. Xiao X, Li S, Wang Y, Lei DM, Zhang X, Zhao FR, et al. Effect of transcutaneous electrical acupoint stimulationon lung function and risks of exacerbation for patients with chronic obstructive pulmonary disease. Acupunct Res. (2021) 46:598–604. doi: 10.13702/j.1000-0607.200646
14. Vyas BM, Shah S, Tiwari H, Singh A. The effect of Acu-TENS on FEV1, 6 min walk distance and dyspnoea in patients with chronic obstructive pulmonary disease: a randomised trial. Int J Biomed Adv Res. (2013) 4:448. doi: 10.7439/ijbar.v4i7.392
15. Vinod BK, Akalwadi A, Sai KN, Brahmbhatt MD. Short term effect of acupuncture-tens on lung functions and dyspnea for subjects with moderate COPD. Int J Physiother. (2015) 2:868–75. doi: 10.15621/ijphy/2015/v2i5/78246
16. Shou Y, Ge H, Dai Z, Yan T, Chen W. The effects of transcutaneous electrical nerve stimulation on pulmonary function, airflow, dyspnea, exercise capacity and TNF-α levels in patients with pulmonary obstruction. Chin J Phys Med Rehabil. (2014) 36:705–8.
17. Öncü E, Zincir H. The effect of transcutaneous electrical nerve stimulation in patients with acute exacerbation of chronic obstructive pulmonary disease: randomised controlled trial. J Clin Nurs. (2017) 26:1834–44. doi: 10.1111/jocn.13450
18. Ngai SP, Jones AY, Hui-Chan CW, Ko FW, Hui DS. Effect of 4 weeks of Acu-TENS on functional capacity and beta-endorphin level in subjects with chronic obstructive pulmonary disease: a randomized controlled trial. Respir Physiol Neurobiol. (2010) 173:29–36. doi: 10.1016/j.resp.2010.06.005
19. Liu X, Fan T, Lan Y, Dong S, Fu J, Mao B. Effects of transcutaneous electrical acupoint stimulation on patients with stable chronic obstructive pulmonary disease: a prospective, single-blind, randomized, placebo-controlled study. J Alternat Compl Med. (2015) 21:610–6. doi: 10.1089/acm.2014.0284
20. Lau KS, Jones AY. A single session of Acu-TENS increases FEV1 and reduces dyspnoea in patients with chronic obstructive pulmonary disease: a randomised, placebo-controlled trial. Aust J Physiother. (2008) 54:179–84. doi: 10.1016/S0004-9514(08)70024-2
21. Jones AY, Ngai SP, Hui-Chan CW, Yu HP. Acute effects of acu-TENS on FEV1 and blood B-endorphin level in chronic obstructive pulmonary disease. Altern Ther Health Med. (2011) 17:8–13.
22. Izzo AA, Hoon-Kim S, Radhakrishnan R, Williamson EM. A critical approach to evaluating clinical efficacy, adverse events and drug interactions of herbal remedies. Phytother Res PTR. (2016) 30:691–700. doi: 10.1002/ptr.5591
23. Beaton DE, Bombardier C, Katz JN, Wright JG, Wells GEORGE, Boers M, et al. Looking for important change/differences in studies of responsiveness. OMERACT MCID working group Outcome measures in rheumatology. Minimal clinically important difference. J Rheumatol. (2001) 28:400–5.
24. Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. (1989) 10:407–15. doi: 10.1016/0197-2456(89)90005-6
25. Kupferberg DH, Kaplan RM, Slymen DJ, Ries AL. Minimal clinically important difference for the UCSD shortness of breath questionnaire. J Cardiopulm Rehabil. (2005) 25:370–7. doi: 10.1097/00008483-200511000-00011
26. Kouri A, Gupta S, Yadollahi A, Ryan CM, Gershon AS, To T, et al. Addressing reduced laboratory-based pulmonary function testing during a pandemic. Chest. (2020) 158:2502–10. doi: 10.1016/j.chest.2020.06.065
27. GOLD. 2021 Global strategy for prevention, diagnosis and management of COPD: global initiative for chronic obstructive lung Disease. Global Initiative for Chronic Obstructive Lung Disease (GOLD) (2021).
28. Gershon AS, Hwee J, Chapman KR, Aaron SD, O'Donnell DE, Stanbrook MB, et al. Factors associated with undiagnosed and overdiagnosed COPD. Eur Respir J. (2016) 48:561–4. doi: 10.1183/13993003.00458-2016
29. Roman MA, Rossiter HB, Casaburi R. Exercise, ageing and the lung. Eur Respir J. (2016) 48:1471–86. doi: 10.1183/13993003.00347-2016
30. Donohue JF. Minimal clinically important differences in COPD lung function. COPD. (2005) 2:111–24. doi: 10.1081/COPD-200053377
31. Borgmann M, Ivanda M, Hadizamani Y, Mohaupt M, Bals R, Lucas R, et al. Does the 6-min walk test in hospitalized COPD patients exclusively correlate with lung function parameters or should psychological factors also be taken into account? PLoS ONE. (2020) 15:e0232587. doi: 10.1371/journal.pone.0232587
32. Polkey MI, Spruit MA, Edwards LD, Watkins ML, Pinto-Plata V, Vestbo J, et al. Six-minute-walk test in chronic obstructive pulmonary disease: minimal clinically important difference for death or hospitalization. Am J Respir Crit Care Med. (2013) 187:382–6. doi: 10.1164/rccm.201209-1596OC
33. Andrianopoulos V, Wouters EF, Pinto-Plata VM, Vanfleteren LE, Bakke PS, Franssen FM, et al. Prognostic value of variables derived from the 6-min walk test in patients with COPD: results from the ECLIPSE study. Respir Med. (2015) 109:1138–46. doi: 10.1016/j.rmed.2015.06.013
34. Holland AE, Hill CJ, Rasekaba T, Lee A, Naughton MT, McDonald CF. Updating the minimal important difference for 6-min walk distance in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. (2010) 91:221–5. doi: 10.1016/j.apmr.2009.10.017
35. Makuch M, Milanowska J, Michnar M, Makuch M, Samardakiewicz M, Milanowski J. The relationship between COPD assessment test (CAT) scores and distress thermometer (DT) results in COPD patients. Ann Agric Environ Med AAEM. (2020) 27:689–94. doi: 10.26444/aaem/114103
36. Kon SS, Canavan JL, Jones SE, Nolan CM, Clark AL, Dickson MJ, et al. Minimum clinically important difference for the COPD assessment test: a prospective analysis. Lancet Resp Med. (2014) 2:195–203. doi: 10.1016/S2213-2600(14)70001-3
37. Anzueto A, Miravitlles M. Pathophysiology of dyspnea in COPD. Postgrad Med. (2017) 129:366–74. doi: 10.1080/00325481.2017.1301190
38. Ekström M, Johnson MJ, Huang C, Currow DC. Minimal clinically important differences in average, best, worst and current intensity and unpleasantness of chronic breathlessness. Eur Respir J. (2020) 56:1902202. doi: 10.1183/13993003.02202-2019
39. Cardinali A, Celini D, Chaplik M, Grasso E, Nemec EC. Efficacy of transcutaneous electrical nerve stimulation for postoperative pain, pulmonary function, and opioid consumption following cardiothoracic procedures: a systematic review. Neuromodul J Int Neuromodul Soc. (2021) 24:1439–50. doi: 10.1111/ner.13302
40. Tang C, Ding Z, Chen C. Effects of transcutaneous electrical stimulation of acupoints combined with task-related training on sub-acute stroke patients with lower limb and ankle dysfunction. Chin J Phys Med Rehabil. (2015) 37:276–9. doi: 10.1097/NPT.0b013e3181fe0ab0
41. Jun MH, Kim YM, Kim JU. Modern acupuncture-like stimulation methods: a literature review. Integ Med Res. (2015) 4:195–219. doi: 10.1016/j.imr.2015.09.005
42. Wang J, Li J, Yu X, Xie Y. Acupuncture therapy for functional effects and quality of life in COPD patients: a systematic review and meta-analysis. Biomed Res Int. (2018) 2018:3026726. doi: 10.1155/2018/3026726
43. Tagaya E, Tamaoki J, Chiyotani A, Konno K. Stimulation of opioid mu-receptors potentiates beta adrenoceptor-mediated relaxation of canine airway smooth muscle. J Pharmacol Exp Ther. (1995) 275:1288–92.
Keywords: transcutaneous electrical nerve stimulation (TENS), acupoint, COPD, efficacy, meta-analysis
Citation: Wei Y, Yuan N, Dong Y, Wang L and Ding J (2022) Transcutaneous electrical nerve stimulation over acupoint for chronic obstructive pulmonary disease: A systematic review and meta-analysis. Front. Public Health 10:937835. doi: 10.3389/fpubh.2022.937835
Received: 06 May 2022; Accepted: 06 September 2022;
Published: 06 October 2022.
Edited by:
Walid Kamal Abdelbasset, Prince Sattam Bin Abdulaziz University, Saudi ArabiaReviewed by:
Wessam Ezzat, Faculty of Medicine Ain Shams University, EgyptAhmed Abdelmoniem Ibrahim, University of Hail, Saudi Arabia
Copyright © 2022 Wei, Yuan, Dong, Wang and Ding. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Dong, ZG9uZ3lhbjYxQDE2My5jb20=
 Ying Wei
Ying Wei Nairong Yuan3
Nairong Yuan3 Yan Dong
Yan Dong Lixia Wang
Lixia Wang