- 1Nursing Education Department, Nursing College, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
- 2Public Health Nursing Department, Faculty of Nursing, King Abdul-Aziz University, Jeddah, Saudi Arabia
- 3Nursing Department, College of Applied Medical Sciences, University of Hafr Al Batin, Hafar Al Batin, Saudi Arabia
- 4College of Nursing, University of Hail, Hail, Saudi Arabia
- 5Department of Nursing Education, Nursing College, Qassim University, Buraydah, Saudi Arabia
- 6Medical and Surgical Department, Nursing College, Taibah University, Medina, Saudi Arabia
- 7Nursing Department, College of Applied Medical Sciences, Majmaah University, Al Majma'ah, Saudi Arabia
- 8Nursing Administration and Education Department, College of Nursing, King Saud University, Riyadh, Saudi Arabia
- 9Community Health Nursing Department, College of Nursing, Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia
- 10Community Health Nursing Department, Nursing College, Taibah University, Medina, Saudi Arabia
- 11Nursing Department, College of Applied Medical Sciences, University of Hafr Albatin, Hafar Al Batin, Saudi Arabia
- 12Medicine Department, Nazarbayev University School of Medicine, Nazarbayev University, Astana, Kazakhstan
During this pandemic, it is crucial to implement early interventions to help nurses manage their mental wellbeing by providing them with information regarding coping skills, preventive risk assessment approaches (such as hospital preparedness and rapid risk assessment), and the ability to respond. This study evaluated the effect of fear and risk assessment management on nurses' mental wellbeing during the COVID-19 pandemic in Saudi Arabia. A total of 507 nurses who worked in tertiary public hospitals were asked to take a descriptive design survey. Three survey scales were used to assess the survey: the Risk Assessment Scale, the Fear of COVID-19 Scale, and the Warwick-Edinburgh Mental Wellbeing Scale. Independent t-tests and a one-way ANOVA were used to examine the association between fear of COVID-19 and nurses' demographic characteristics on their mental wellbeing. A multiple regression analysis was performed to examine the predictors associated with mental wellbeing. Findings revealed that almost half of the participants showed moderate positive mental wellbeing, 49.7%, while only 14% had low levels of fear on the Warwick-Edinburgh Mental Well being Scale. Most of the respondents had low levels of fear on the Fear of COVID-19 Scale, 45%, while only 15% had high levels of fear on the scale. Then, some demographic variables, such as “age,” “nationality,” “total years of experience in the current hospital,” and “region you work at” had statistically significant differences with p < 0.5. Meanwhile, risk assessment is also associated with mental wellbeing scores. All items on the Fear of COVID-19 Scale showed no significant difference with a P > 0.05. In conclusion, most nurses providing direct patient care to a patient with COVID-19 emphasized the importance of wearing PPE and performing hand hygiene before and after any clean or aseptic procedure. Meanwhile, although almost all nurses were vaccinated, they were still afraid of a COVID-19 infection. Additionally, the results reported that the older the nurses are, the better their mental wellbeing scores. Non-Saudi nurses had higher perceived mental wellbeing scores than Saudi nurses, and different working environments corresponded to different mental wellbeing scores. Finally, nurses' risk assessment was associated with mental wellbeing scores.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has unsympathetically put the health of healthcare professionals (HCPs) and the public at unprecedented health risks. This has prompted immediate action from medical facilities around the world. Two years after the COVID-19 outbreak, as of 2 May 2022, data showed that 66.2% of the world population has already received the vaccine, which is more than 5.08 billion people around the world (1). According to the World Health Organization's (1) epidemiological update regarding COVID-19, there was a 16% decline in newly reported cases from 28 March 2022 to 3 April 2022, and both new weekly cases and deaths have been declining globally (1). However, although the data speak positively on a macro-level scale, individuals are nevertheless confronted with challenges at the micro level. For instance, in some countries, HCPs were assigned as one of the priority healthcare groups for vaccination (2, 3). A recent Centers for Disease Control and Prevention study published in 2021 (4) reported that vaccination has a greater protection rate than those previously infected with COVID-19. There was high anticipation from the HCPs for these vaccines. Nurses make up one of the largest groups of HCPs and have the most direct patient contact, so vaccination is crucial for them because it reduces their risk of infection (5).
By the end of 2021, over 50% of healthcare professionals (including nurses) worldwide were neither fully vaccinated nor had no plans to do so (6). For instance, vaccination hesitancy has been one of the determinants of under-vaccination in some nurses (7). According to Reses et al. (3), the reason for the high hesitancy status of getting vaccinated can be attributed to people's political views and a lack of confidence and trust in vaccine manufacturers. Moreover, people were hesitant to get the COVID-19 vaccination due to their concerns regarding its side effects, which stemmed from the vaccine's quick development and the conspiracy theory that it is employed for population control (8–10). The rapid pace of vaccine development and rollout may have caused doubts regarding vaccine safety. Meanwhile, another study found the cause of greater reluctance to vaccination to be the vaccine development process and a lack of knowledge about the vaccine's long-term effects (11).
Similar to vaccination reluctance, the physical and mental wellbeing of HCPs, particularly frontline nurses, is becoming a significant concern over the pandemic's larger impact due to the unknown number of COVID-19-related excess deaths among HCPs (12). COVID-19 also impacted the workforce in the healthcare sector. Undoubtedly, nurses were most severely affected by the pandemic, as they faced multiple hazards that affected their physical as well as mental wellbeing (13). In addition, Al-Dossary et al. (14) explained that nurses experienced moderate to severe symptoms of burnout, distress, anxiety, fear, and trauma during the COVID-19 pandemic. Another study from Bangladesh about the challenges faced by HCPs reported that nurses experienced greater workloads, scarce incentives, psychological distress, personal protective equipment (PPE) shortages, and social exclusion/stigmatization (15).
In addition, the disproportionate impact of the COVID-19 pandemic on hospitals has resulted in nursing staff shortages and increased workload (16), which could lead to stress and exhaustion for nurses. This heavy workload negatively affects patient safety, causes greater stress, reduces job satisfaction, and increases occupational burnout. Increased demands on nurses' time and energy lead to a decline in their quality of life (17) and can have negative consequences for patient care in the form of staffing shortages and high turnover rates.
When the pandemic hit Saudi Arabia, it exacerbated an already problematic situation for nursing professionals. A recent study revealed that nurses dreaded the disease for a variety of reasons, including the abrupt increase in COVID-19-related morbidity and mortality in the country (18, 19). Moreover, nurses reported being directly involved in the treatment of patients diagnosed positive for COVID-19. Thus, they were apprehensive about contracting the infection and passing it on to their families. Furthermore, nurses, like any human being, fear the unknown. During the first few months of the pandemic, the lack of adequate disease knowledge and no specific treatment caused the nurses to be exposed to transmission risk and emotional distress (14, 20). Nurses' anxiety about COVID-19 may have been influenced by any number of factors, many of which have been the subject of prior research. As reported by recent studies, assessing the nurses' fear and mental wellbeing during the outbreak of COVID-19 has been seen as a crucial matter. For example, the investigation by Albaqawi et al. (21) regarding the nurses' risk for COVID-19 infection revealed that nurses who do not practice proper hand hygiene after physical contact with patients with COVID-19 and who do not replace PPE are at a higher risk of contracting the infection. Additionally, nurses' inadequate understanding of COVID-19, inadequate PPE, lack of access to tests, and the presence of psychological stress were the major factors for infection among healthcare professionals (22, 23), thus highlighting the importance of COVID-19 preparedness in managing its risks to HCPs. A study conducted in the Najran Region, KSA, revealed that nurses are well-versed in preventive measures and reported attending orientation about the COVID-19 guidelines (24). This is probably why early interventions help the nurses manage their mental wellbeing by providing them with information regarding coping skills and, at the same time, the preventive risk assessment approach (e.g., hospital preparedness and rapid risk assessment) and the ability to respond during this pandemic is greatly important (25).
Previous studies examined how they manage the emotional distress brought on by the pandemic, and it was revealed that nurses' use of COVID-19 protective measures such as PPE, psychological and management support, avoidance strategies, faith-based practices, and social support from their families during the COVID-19 outbreak improved nurses' coping response (26, 27).
A study identified informational support, such as training and clear preventative programs, as one of the factors that may treat mental health issues. It has been demonstrated that instrumental support is particularly effective in providing adequate PPE and other protection protocols. Emotional and psychological support, such as counseling and therapy for nurses experiencing emotional distress, and organizational support, such as manpower allocation and redistribution of workloads and working hours, were themes that were revealed to be helpful not only to nurses but also to policymakers in each healthcare institution (28). The strain on mental health can cause dysfunction at work and other disorders that could be more serious if left untreated. Actions such as risk management and risk reduction for all staff can be taken to mitigate this risk.
The interventions, such as spreading awareness through public health education, helped the HCPs manage their fear and psychological wellbeing throughout the pandemic. A study has shown that public health education decreased the fear of an individual toward COVID-19 since the awareness of the disease helped nursing professionals understand that preventive measures can work effectively (29). Time management training for the nurses was also found to be helpful for their mental health during the COVID-19 pandemic. Sun (30) conducted a 16-week intervention for the nurses, and the results suggested that the training significantly increased the mental health level of the nurses. Mental health interventions, such as emotional management, were given to the HCPs and could enhance the ability of the nurses to regulate their emotions and help them prevent mental disorders (31). Previous studies proved that interventions had positive effects on nurses. Ali et al. (22) discussed that the number of HCPs getting infected with COVID-19 is increasing and that one of the major risk factors is the lack of understanding of the disease. Thus, they suggested that governing bodies should focus on providing education and training to increase the readiness of their staff. The same suggestion was also made in the study by d'Ettorre et al. (32), where they advised a need for interventions to protect against the mental health effects brought by the pandemic and management strategies for posttraumatic stress symptoms. A risk assessment strategy can successfully decrease the occurrence of risk events in nursing practice (33).
Therefore, it is also safe to presume that the risk assessment and management of the HCPs could also influence their undue fear and mental wellbeing during the COVID-19 pandemic. While there are studies investigating the risk assessment of the HCPs, particularly the nurses, to the best of the researchers' ability, there has been no study conducted in Saudi Arabia exploring the direct relationship of risk assessment management to the fear and mental wellbeing of nurses. Mental wellbeing is an integral and essential component of nurses' health, impacting patient safety and the quality of care provided. Evaluating the effect of risk assessment management on nurses' mental wellbeing and fear is significant, particularly in the nursing profession, since it helps healthcare institution policymakers better combat nurses' fear and mental wellbeing. In this study, the information on how healthcare professionals fear COVID-19, which, in turn, will support further designing of appropriate programs to take care of their fear and mental wellbeing, could also ensure that they deliver quality care, thereby maintaining the safety of the patients. Maintaining the good mental health conditions of the HCWs would mean that they are fit to perform the task at their optimum level. When the nurses work at their best, they become efficient. In addition, better mental health increases HCP satisfaction and decreases voluntary turnover, which is a cost-saving move for hospital administration due to the reduction or elimination of a number of charges and losses that would otherwise be incurred (34).
Finally, the result could provide baseline information on risk assessment on reducing the transmission rate of COVID-19 and promoting positive mental wellbeing. Having established the impact of COVID-19 on the fear and mental health of nurses providing direct patient care in Saudi Arabia, this study is crucial for advancement not only in nursing research but also for the nursing profession in Saudi Arabia. This study evaluated the effect of risk assessment management on nurses' mental wellbeing and fear during the COVID-19 pandemic in Saudi Arabia. It is currently relevant that a new study will be conducted, especially since the COVID-19 pandemic is ongoing. The mere presence of the pandemic simply means that the challenges for nurses remain. Thus, the study seeks to determine how HCPs manage the risks posed by the pandemic, as well as its effect on nurses' fear and mental health.
Materials and methods
This study is cross-sectional in design. We used online survey questionnaires to gather data from the selected tertiary public hospitals in Saudi Arabia. The nurses were eligible to become participants in the study if they had a license and had at least 1 year of hospital experience. We are presently working in a Saudi Arabian public or private hospital that has provided care to patients with COVID-19 and gave consent to participate in the study.
Data collection
This study was approved by the Ministry of Health Ethical Review Board (Institutional Review Board–Hafr Albatin committee (KACST No. H-05-FT-083). Each survey questionnaire was accompanied by a cover letter describing the study's goal, the participant's right to decline participation, and the fact that participation implies consent. Confidentiality was ascertained as the survey questionnaire did not ask for any data that could expose the identity of the participants. After ethical approval was obtained, the researcher sent a copy of the survey questionnaire to each department in the selected tertiary hospitals for approval. Permission to use the tools was sent to each author of the tool, and approval letters from the authors were received. After the participants were identified, the questionnaires were distributed. Participants were asked to complete the questionnaire during their respective free time to avoid disturbing their work. Data were collected from February to May 2022.
Sample size
The sample size was decided using the online Sample Size Calculator (https://www.calculator.net/sample-size-calculator.html). This means 385 or more surveys were needed to have a 95% confidence level in which the real value was within ±5% of the surveyed value. In this study, a total of 507 nurses answered the survey, which is above the minimum sample requirements.
Survey questionnaire
The tool is a four-part questionnaire:
Demographic data
This section describes respondents' demographic and work-related characteristics.
Risk assessment scale
This scale is a modified version of the WHO's COVID-19 Virus Exposure Risk Assessment Form for HCPs. This tool contains three subparts that assess the risk category of nurses after exposure to a patient with COVID-19 (25). The first part contains the five items on nurses' intervention conducted on patients with COVID-19 in clinical settings. The second part contains the 7-item adherence to IPC procedures during healthcare interactions. Finally, the third part contains 5-item questions regarding the COVID-19 vaccine. In this study, this tool's reliability was 0.91 (Cronbach's alpha).
Warwick–Edinburgh mental wellbeing scale
The tool was composed of 14 items that assessed the mental state of the nurses during the COVID-19 outbreak (35). The participants' responses were measured on a 5-point scale (1 = none of the time to 5 = all of the time), with higher mean scores meaning greater positive mental wellbeing. The minimum score on the scale is 14, while the maximum score that can be attained is 70. A higher score means improved mental wellbeing. Several studies performed in various countries on the psychometric properties of the tools found that they have acceptable reliability and validity for assessing an individual's mental wellbeing (13, 36, 37). This study has a reliability of 0.95 (Cronbach's alpha).
Fear of COVID-19 scale
The tool measures anxiety and fear of COVID-19 (38). This tool comprises a 7-item self-administered questionnaire and has been psychometrically validated in several countries (39–42). Nurses indicated their level of agreement with the statements using a five-item Likert-type scale. Answers included “strongly disagree,” “disagree,” “neutral,” “agree,” and “strongly agree.” The minimum score possible for each question was 1, and the maximum was 5. A total score could be calculated by adding up each item's score (ranging from 7 to 35). A higher overall score attained indicated severe fear of COVID-19. This study's computed Cronbach's alpha was 0.92, indicating high reliability.
Data analysis
Demographic variables, risk assessment, fear of COVID-19, and mental wellbeing were frequently counted, and percentages, mean scores, and standard deviations were calculated. The Shapiro–Wilk test was applied to check the normality or distribution of data. It found that if the value of the Shapiro–Wilk and Kolmogorov-Smirnova tests is >0.05, the data are normal. Pairwise deletion of cases was used with missing data. Independent t-tests and one-way ANOVA were used to examine the association between fear of COVID-19 and nurses' demographic characteristics on their mental wellbeing. Multiple regression analysis examined the predictors associated with mental wellbeing. The dependent variable used is the Warwick–Edinburgh Mental Well-Being Scale, and the independent variables are the nurses' demographic characteristics and fear of COVID-19. A p-value of 0.05 is considered significant.
Results
Table 1 shows that the total number of participants was equal to 507. Most of the participants were women (86.2%), and the age of most participants ranged between 31 and 40 years (47.3%), while the participants aged 61 years and above had the lowest percentage (0.2%). More than half of the participants were married, with a percentage of 66.1%, while only 3.4% of them were separated. The participants' education level had 66.7% bachelor's degrees, while only 0.2% had doctorate degrees. The participants with non-Saudi nationality represented 57.8%, while those with Saudi nationality represented 42.2% of the participants. One-third of the participants (32.3%) had an experience of 1–5 years, and only 6.5% had an experience of 21 years or more. The central region (Riyadh, Qassim) represented the majority region where 46.7% of participants worked, followed by the Eastern Region (39.6%), the Northern Region (3.2%), the Southern Region (4.7%), and the Western Region (5.7%). Most of the participants were assigned to ICUs (15.4%), emergency departments (15.2%), and obstetric departments (15.6%), comprising almost half of the participants.
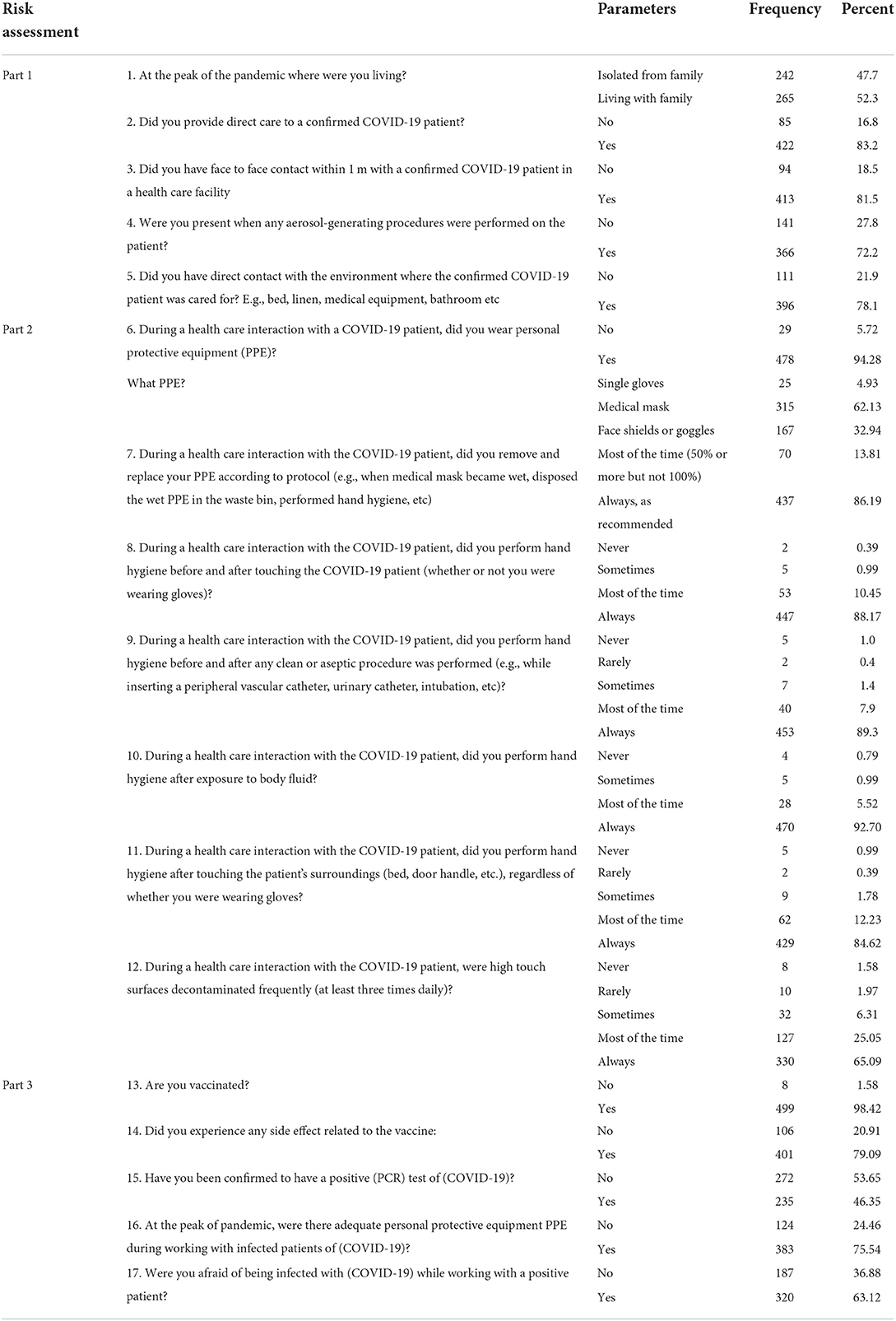
The perceived risk assessment of the respondents is shown in Table 2. The first part of the risk assessment tool consists of five questions reflecting the following: 52.3% of the participants lived with their families at the pandemic's peak. In contrast, the remaining lived in an isolated room, where 83.2% of participants provided direct care to a confirmed COVID-19 patient, 81.5% had face-to-face contact within 1 m with a patient confirmed with COVID-19 in a health care facility, 72.2% were present when any aerosol-generating procedures were performed on the patient, and 78.1% had direct contact with the environment where the patient was confirmed for COVID-19. The second part of the risk assessment tool consisted of seven questions, which reflects the following: 94.28% of the participants wore PPE (62.13% medical masks, 32.94% face shields or goggles, and 4.93% single gloves), 86.19% followed the protocols by removing and replacing their PPE, 88.17% “always practice hand hygiene before and after touching the COVID-19 patient,” 89.3% “always practice hand hygiene before and after any clean or aseptic procedure was performed,” 92.70% “always practice hand hygiene after exposure to body fluid, 84.62% perform hand hygiene after touching the patient's surroundings,” and 65.09% of them “always have high touch surfaces decontaminated frequently.” The third part of the risk assessment tool consisted of five questions, which reflects the following: 98.42% of the participant were vaccinated, 79.09% of them had experienced side effects related to the vaccine, 53.65% had negative PCR test, 75.54% had adequate personal protective equipment (PPE) when working with patients infected with COVID-19, and 63.12% of the participants were afraid of becoming infected while working with patients tested positive for COVID-19 (Table 2).
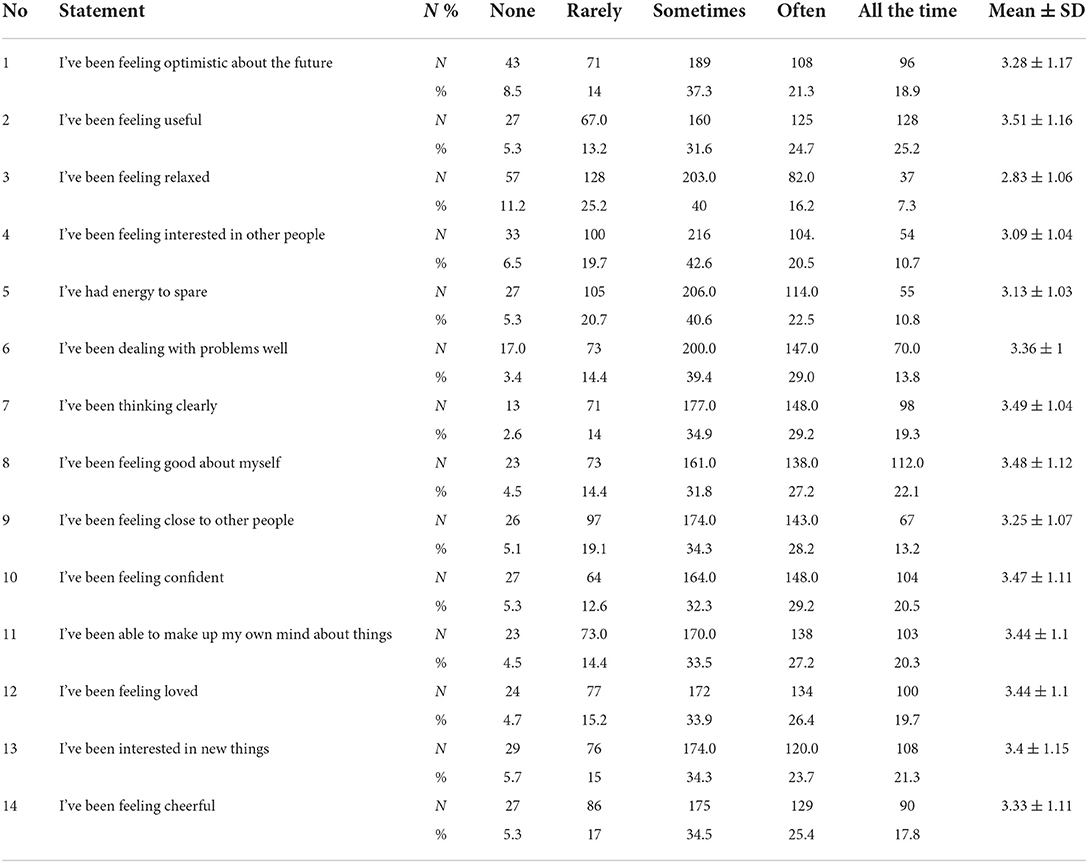
Table 3 shows the respondent's perceived mental wellbeing using the WEMWBS.
Items 1, 3, 4, 5, 6, 9, and 14 had a moderate mean ranging between 3.09 and 3.36, while items 2, 7, 8, 10, 11, 12, 13, and 14 had a high mean ranging between 3.4–3.51. The WEMWBS was converted into three categories, which are low, moderate, and high. Most of the participants had moderate levels, with a percentage of 49.7%, while only 14% had low levels of mental scale. This result implies a perceived moderate positive mental wellbeing among nurses.
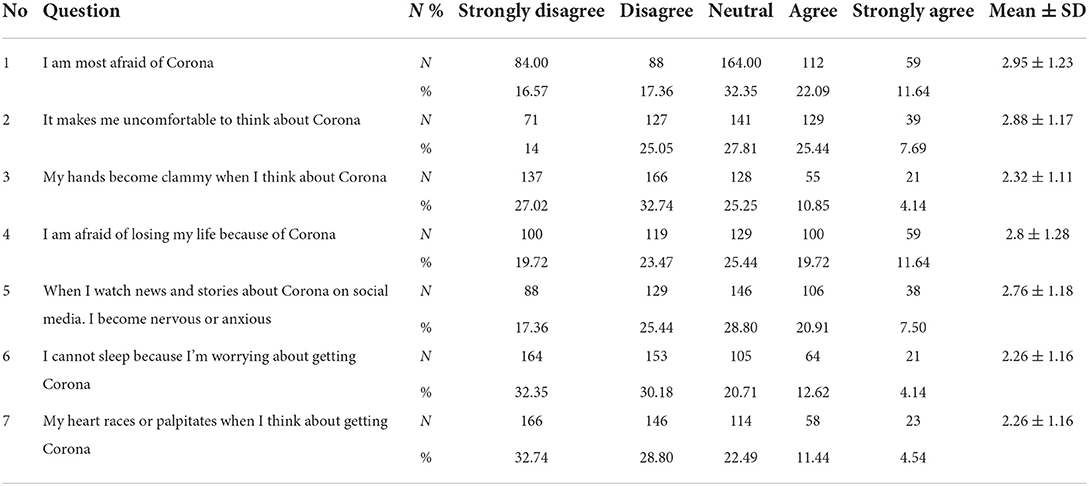
The association between respondents' demographic profile and perceived risk assessment about their mental wellbeing scores is shown in Table 4. Items 1, 2, 4, and 5 have results of “neutral” with a mean range between 2.76–2.95, while items 3, 6, and 7 have results of “disagree” with a mean range between 2.26–2.32. The Fear of the COVID-19 Scale was converted into three categories, which are low, moderate, and high levels. Most of the respondents had a low level of fear, 45%, while only 15% had high levels of fear on the scale. This implies that respondents had a low fear of COVID-19.
Table 5 shows the relationship between respondents' demographic profile and their perceived risk assessment of their mental wellbeing scores. As shown in the Table 5, “age,” “nationality,” “total years of experience in the current hospital,” and “region you work at” had statistically significant differences with P-values less than 0.5 as follows 0.048, 0.008, 0.036, and 0.004, respectively. In contrast, “gender,” “marital status,” “educational attainment,” and “area of practice” had no significant difference with a P > 0.05. Meanwhile, risk assessment is also associated with mental wellbeing scores with a statistical significance difference with a P < 0.5.
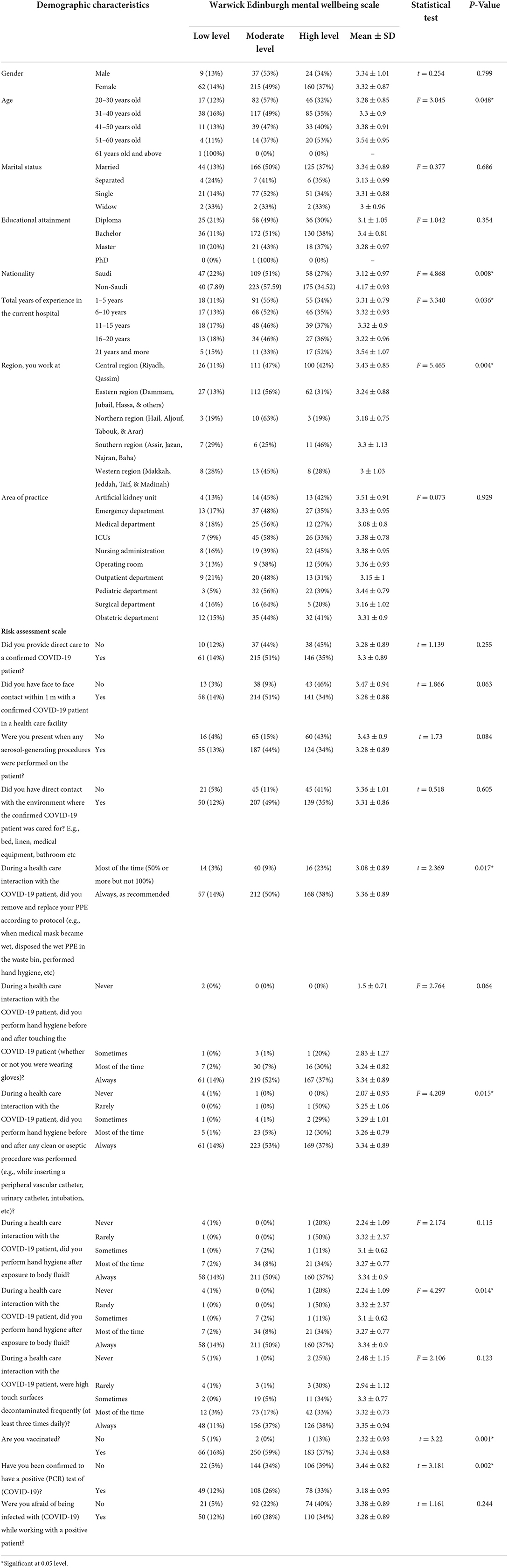
Table 5. Association between respondents' demographic profile and perceived risk assessment in relation to their mental wellbeing scores.
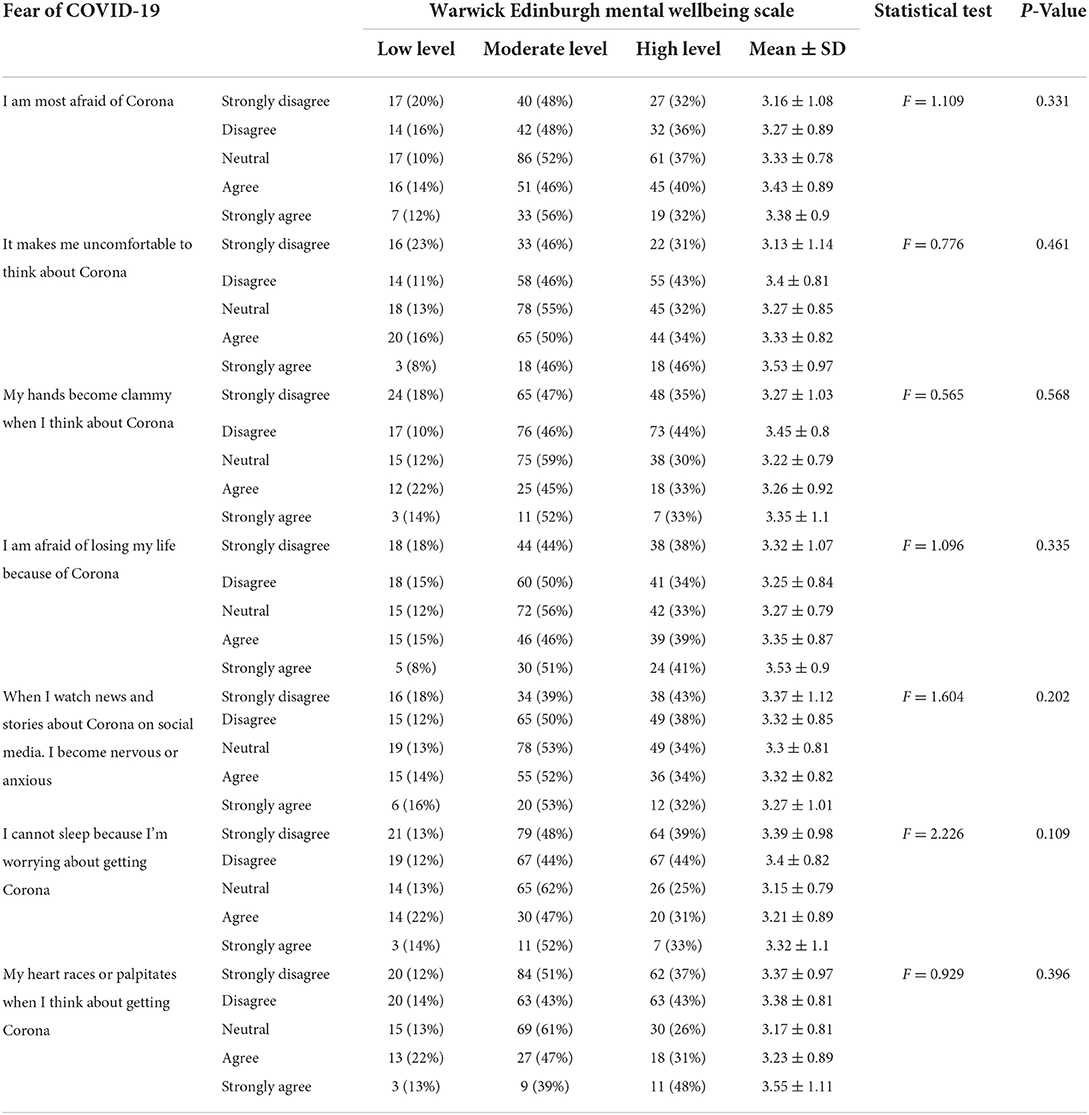
Table 6 depicts the relationship between fear of COVID-19 and nurses' mental wellbeing scores. An ANOVA test was applied according to the data type. As shown in the table, all items on the Fear of COVID-19 Scale had a non-significant difference with a P-value of more than 0.05.
Discussion
This study assessed the relationship between nurses' risk assessment and management, fear perception, and mental wellbeing during the COVID-19 pandemic in Saudi Arabia.
Findings in the risk assessment part 1 reported that most nurses (83.2%) provide direct patient care to patients infected with COVID-19. Previous literature showed that frontline workers, such as the HCPs who provide direct care to patients with COVID-19, are at risk of getting infected, as was the case in the study conducted in Saudi Arabia (43, 44). The results are congruent with other recent research on the high-risk perception among nurses during Saudi Arabia's COVID-19 pandemic (45).
Nurses are particularly at risk for contracting COVID-19 because they have to come in direct contact with suspected COVID-19 patients and treat multiple infections simultaneously (45). The nurses' work during this pandemic made them more vulnerable to risks such as infection. In fact, this is confirmed in the results of a phenomenological study in which the participants expressed that they were at a high risk of COVID-19 infection and that this type of vulnerability is unavoidable (46). As of November 30, 2020, the number of nurses infected with COVID-19 in the Kingdom of Saudi Arabia was already 57,159 HCPs (47). This is most likely because COVID-19 infection is higher among HCWs than in the general community, with 2747 cases per 100,000 frontline HCWs compared to 242 cases per 100,000 people in the general population (48, 49). Given the fact that nurses provide direct contact with the patient, it is indeed logical that they commonly contract the infection. This possibility could explain the increased risk of COVID-19 among the HCP, particularly the nurses.
In the Part 2 risk assessment, most of the respondents wear PPE and practice hand hygiene before and after any clean or aseptic procedure. The occurrence of pandemic affected the usage of PPE and its perceived importance by the HCPs. In a previous study, HCWs reported that PPE was frequently used and perceived as more important than the reports before the pandemic (50). Medical-ward nurses, in particular, are quite conscientious about following standard precautions like wearing masks and washing their hands before and after handling PPE (1). This might be because the HCPs recognize the additional protection in wearing PPE and practicing hand hygiene throughout this pandemic, especially for those directly caring for COVID-19 patients. The infection modes of COVID-19 were airborne, droplets, and close contact with an infected individual. Thus, wearing appropriate PPE can protect against infectious microorganisms that help in the transmission of COVID-19 infection (12). This could be why most of the nurses in this study reported wearing PPE and practicing hand hygiene before and after procedures. Despite the benefit and the additional protection, it can pose problems such as the low adherence of nurses to using PPE and not practicing hand hygiene; these problems remain a challenge for healthcare institutions. A study by Keleb et al. (51) revealed that the Northeastern Ethiopian HCP's compliance with PPE, equipment utilization, and hand hygiene was low. HCPs in the UK also reported suboptimal adherence to personal protective measures (52). The discrepancy in the results may be attributed to the difference in the setting where the nurses reportedly work. Smith et al. (54) discussed in their study that the nurses' adherence to PPE was associated with the training received by the HCWs regarding safety and health in the workplace. In Saudi Arabia, nurses reported receiving sufficient training on the preventive measures for COVID-19 (24). This could be why nurses frequently use the gear because they are aware of the protection they can get against COVID-19.
In Part 3, risk assessment, although almost all nurses are vaccinated, they are still afraid of being infected while working with a positive patient. These findings are supported by the study by Zhang et al. (53); they revealed that nurses did not change their protective behavior even after getting vaccinated. While COVID-19 vaccines are effective for immunizing people, they do not guarantee 100% complete protection (12). Even if a person is fully vaccinated, there is still a possibility that they will contract the virus. This could be why the respondents still feared being infected even after vaccination. Although this might be the case for the nurses, additional protection against COVID-19, such as getting vaccinated and adhering to protective behavior, is much better than working with no protection against the virus. Thus, it is essential to address the vaccine hesitancy of HCPs and the general population for an additional layer of protection.
Other findings of the study reported that nurses have moderate positive mental wellbeing, indicating good mental health during the pandemic. The result is congruent with the study by Abo-Ali et al. (54), in which the majority of the HCPs in Saudi Arabia had positive mental wellbeing scores during the COVID-19 pandemic. One of the probable reasons nurses felt positive mental wellbeing despite the COVID-19 pandemic is that the situation as of 2022, when this study was conducted, is under control. As of June 2022, over 71.5% of people in Saudi Arabia are vaccinated, and the newly reported cases of COVID-19 in the last seven days were only 3,830, which is lower than at the onset of the pandemic (55). This indicates that COVID-19 cases relatively decreased, which made the nurses' work more relaxed. Furthermore, nurses might have already been used to the protocol and the procedures that are necessary to perform for COVID patients, which allowed them to work more smoothly. Therefore, regular drills and training for disaster management are suggested to help HCWs adjust and use the routine.
The current study found that nurses reported a low fear of COVID-19 scores. This level of fear is lower compared to the study of Mohsin et al. (56), which revealed that Saudi nurses have an overall low or moderate level of fear of COVID-19. The low fear of nurses toward COVID-19 may be attributed to the policies that were clearly established to mitigate the negative situation brought on by the pandemic. For instance, aside from the vaccine rollouts in Saudi Arabia, the Ministry of Health developed COVID-19 guidelines based on recent COVID-19 research to help HCPs deal with COVID-19 patients. The MOH protocol for patients who tested or were thought to be positive for COVID-19, airway management, and mechanical ventilation protocols was detailed in instruction manuals (57). Nurses, as human beings, fear the unknown. However, due to the continuous publication of guidelines and materials to guide the HCPs, the facts and other important information became known, which might be why they are no longer afraid of dealing with it. Considering this, healthcare institutions may review their COVID-19 policies and protocols to clarify implementation.
There is a significant association between some demographic profile variables and perceived risk assessment of nurses' mental wellbeing scores. Specifically, nurses' age is significantly associated with mental wellbeing. It implies that the older the nurses are, the better their mental wellbeing. This result agrees with the results in a study by Cheung and Yip (58), which revealed that age and years of experience negatively correlate with poor mental health. Specifically, younger nurses with less experience had lower mental health. This is worth noting since older nurses might have acquired more extensive experience in nursing practice, which allowed them to adjust well to the situation and become well-versed with the routine and procedures. Although some studies identified specific age brackets of nurses with better mental wellbeing, there is no consensus among the researchers regarding the specific age of nurses with better mental wellbeing. The only common denominator in their findings was that they all agreed on the result that older nurses have better mental wellbeing. Healthcare institutions may help younger nurses to achieve stable and better mental wellbeing by providing opportunities for them to acquire more experience through various training programs and life coaching to support their journey and help them to manage their time while balancing their career and family life.
The nationality of nurses is associated with mental wellbeing scores. Specifically, non-Saudi nurses have higher perceived mental-wellbeing scores than Saudi nurses. This finding is backed by recent research (7), which revealed that nationality was a significant predictor of nurses' psychological burden. In their study, Filipino and Indian nurses achieved lower mean scores for depression, anxiety, and stress than Saudi nurses. This may be attributed to the support system that non-Saudi nurses received from their families and friends. As expatriate nurses in Saudi Arabia, Filipino nurses were known to have close familial ties (59). Consistent and close communication with families might be one of the reasons why non-Saudi nurses are provided with adequate social support. Having social support from friends had an indirect effect on the resilience of the nurses (59). This might be the reason why better mental wellbeing is observed among expatriates. With this in mind, it is recommended that healthcare institutions provide a good support system for all the HCPs to rely on amidst the pandemic.
Next, the region where nurses currently work has been significantly associated with mental wellbeing. This is worth noting since different regions might have different hospital policies, human resource management policies, providing care policies, administrative policies, and a diversity of healthcare professionals' compliance with several policies and procedures of each organization. Considering the complex nature of the healthcare industry's structure, this may affect their mental wellbeing. According to WHO (1), workplace environments also have different health and safety issues, communication, management practices, employee support, and organizational tasks and objectives, all affecting their mental health. Although the current study included the area of practice, findings have shown that it has no significant association with the perceived risk in relation to their mental wellbeing. Nonetheless, it negates the study by Cruz et al. (17), in which they discussed that emergency nurses have a higher infection risk, higher workload, fatigue, and helplessness, which could be associated with a high depression level in ED nurses. A recent study in China conducted by Chen et al. (60) revealed that ICU nurses and those assigned to COVID-19-designated hospitals and departments have a higher developing symptoms risk, the same with posttraumatic stress disorder (PSTD). This could indicate that the workplace where nurses are assigned might have brought risks that could affect their mental wellbeing. However, the method did not include risk factors for mental health that may be present in the working environment. Thus, further research determining risk factors for mental health and relationships between work environments is warranted.
Finally, nurses' risk assessment is associated with mental wellbeing scores. This result agrees with the results of the previous studies that the risks encountered by the nurses as frontline workers during the COVID-19 pandemic increase their mental health issues (13, 14). This is worth noting since nurses, as health care professionals, render direct care to patients with COVID-19, which indicates that they are more exposed to the risks affecting their mental wellbeing. A study showed that HCPs working in direct contact with patients who tested positive for COVID-19 experienced two times the risk of depression and anxiety compared to HCWs with less exposure to COVID-19 (61). Since the newly reported cases are constantly decreasing, the possibility of the risks that nurses might experience decreases as well, thereby maintaining their mental health. Continuous support on vaccine rollouts, adherence to wearing protective gear, and hand hygiene behaviors among frontline workers may enable them to fully control adverse events that currently occur during the pandemic.
Conclusion
The findings indicate that the risks posed by the COVID-19 pandemic affect nurses' mental wellbeing. Due to their frequent and close interaction with patients with COVID-19, nurses are at an increased risk for mental health issues. The results revealed that most nurses provide direct patient care to patients with COVID-19, state the importance of wearing PPE, and perform hand hygiene before and after any clean or aseptic procedure. Meanwhile, although almost all nurses are vaccinated, they are still afraid of being infected with COVID-19 while working with a patient tested positive for COVID-19 and reported low fear of COVID-19 scores. Additionally, the results reported that the older the nurses, the better their mental wellbeing scores; non-Saudi nurses have higher perceived mental wellbeing scores than Saudi nurses, and different working environments correspond to different mental wellbeing scores. Finally, nurses' risk assessment is associated with mental wellbeing scores. Therefore, the study's findings proved that despite getting vaccinated and the nurses' adherence to hand hygiene behaviors, they are still susceptible to fear of COVID-19, which will impact their mental wellbeing.
Limitations of the study
Some limitations should be considered in the findings. This study used a cross-sectional design with online survey questionnaires. Hence, causality cannot be conclusively inferred. Also, convenient sampling was used, which led to an inability to generalize the findings. The study was conducted after the COVID-19 vaccine was introduced and after 2 years of pandemic experience. Further interventional studies' management assessment of nurses' mental wellbeing and various coping mechanisms for nurses' mental health during and after the pandemic are warranted.
Implications
These findings may help us understand the implications of healthcare institutions' policies, which are relevant to improving healthcare workers' mental health during the COVID-19 pandemic. The result of the study could provide information as a benchmark for promoting positive mental health while reducing the risk and fear perception of COVID-19. The results improved our understanding of the links between the described variables and nurses' mental wellbeing, contributing to effective prevention programs and therapeutic intervention development methods. At a nursing practice level, the results may be useful for nursing management in identifying and supporting nurses' COVID-19 anxiety levels and risk perception to mitigate risks. Interventions focused on improving mental wellbeing coping strategies might increase nurses' confidence and resilience in the face of unpredictable adverse events on psychological wellbeing that seek to reduce the anxiety and fear induced by the pandemic to promote both the implementation of preventive behaviors against COVID-19 and wellbeing in the evaluated Latin American and Caribbean countries. The authorities in the healthcare sector must first recognize that nurses are most susceptible to poor mental health during the COVID-19 pandemic. Creating an awareness program and life coaching may help nursing professionals to be mindful of their mental health during the pandemic. A comprehensive review of the local COVID-19 policies and protocol may be essential to ensure it is implemented. Enabling support systems for nursing professionals is also important to address adequate support for the protective measures against COVID-19. They must be physically and mentally supported to maintain healthy mental wellbeing during the COVID-19 pandemic.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Board—Hafr Albatin committee (KACST No. H-05-FT-083). The patients/participants provided their written informed consent to participate in this study.
Author contributions
RA-D, SA, MB, MA, HA, KA, MSA, BA, RF, NA, KA, JA, and JUA contributed from the data collection, data analysis and interpretation, drafting of the article, and critical revision of the article. All authors contributed to the article and approved the submitted version.
Acknowledgments
The author would like to thank all nurses who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Saudi Arabia: WHO Coronavirus Disease (COVID-19) Dashboard With Vaccination Data. World Health Organization (2020). Available online at: https://covid19.who.int/region/emro/country/sa/ (accessed June 16, 2022).
2. Centers for Disease Control Prevention. Real-World COVID-19 Vaccine Effectiveness in Healthcare Workers. Centers for Disease Control and Prevention (2022). Available online at: https://www.cdc.gov/vaccines/covid-19/effectiveness-research/vaccine-effectiveness-hcp.html (accessed June 17, 2022).
3. Reses HE, Jones ES, Richardson DB, Cate KM, Walker DW, Shapiro CN. COVID-19 vaccination coverage among hospital-based healthcare personnel reported through the department of health and human services unified hospital data surveillance system, United States. Am J Infect Control. (2021) 49:1554–7. doi: 10.1016/j.ajic.2021.10.008
4. Centers for Disease Control Prevention. New CDC Study: Vaccination Offers Higher Protection Than Previous COVID-19 Infection CDC. Centers for Disease Control and Prevention (2016). Available online at: https://www.cdc.gov/media/releases/2021/s1029-Vaccination-Offers-Higher-Protection.html (accessed June 16, 2022).
5. Thazha SK, Cruz JP, Alquwez N, Scaria B, Rengan SS, Almazan JU. Infection prevention and control awareness, attitudes, and practices among healthcare professionals in South India. J Infect Dev Ctries. (2022) 16:659–67. doi: 10.3855/jidc.14746
6. National Health Services Statistics. Statistics-COVID-19 Vaccinations. National Health Services Statistics (2021). Available online at: https://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-vaccinations/ (accessed June 15, 2022).
7. Alshehry AS, Cruz JP, Alquwez N, Alsharari AF, Tork HMM, Almazan JU, et al. Predictors of nursing students' intention to receive COVID-19 vaccination: a multi-university study in Saudi Arabia. J Adv Nurs. (2021) 78:446–57. doi: 10.1111/jan.15002
8. Alsolais A, Alquwez N, Alotaibi KA, Alqarni AS, Almalki M, Alsolami F, et al. Risk perceptions, fear, depression, anxiety, stress and coping among Saudi nursing students during the COVID-19 pandemic. J Ment Health. (2021) 30:194–201. doi: 10.1080/09638237.2021.1922636
9. Jennings W, Stoker G, Bunting H, Valgarð*sson VO, Gaskell J, Devine D, et al. Lack of trust, conspiracy beliefs, and social media use predict COVID-19 vaccine hesitancy. Vaccines. (2021) 9:593. doi: 10.3390/vaccines9060593
10. Kuter BJ, Offit PA, Poland GA. The development of COVID-19 vaccines in the United States: why and how so fast? Vaccine. (2021) 39:2491–5. doi: 10.1016/j.vaccine.2021.03.077
11. Bullock J, Lane JE, Shults FL. What causes COVID-19 vaccine hesitancy? Ignorance and the lack of bliss in the United Kingdom. Hum Soc Sci Commun. (2022) 9:87. doi: 10.1057/s41599-022-01092-w
12. World Health Organization. The Impact of COVID-19 on Health and Care Workers: A Closer Look at Death. World Health Organization. Available online: https://apps.who.int/iris/bitstream/handle/10665/345300/WHO-HWF-WorkingPaper-2021.1-eng.pdf (accessed June 12, 2022).
13. Aruta JJBR, Almazan JU, Alamri MS, Adolfo CS, Gonzales F. Measuring mental well-being among frontline nurses during the COVID-19 crisis: evidence from Saudi Arabia. Curr Psychol. (2022) 4:1–11. doi: 10.1007/s12144-022-02828-2
14. Al-Dossary R, Alamri M, Albaqawi H, Al Hosis K, Aljeldah M, Aljohan M, et al. Awareness, attitudes, prevention, and perceptions of COVID-19 outbreak among nurses in Saudi Arabia. Int J Environ Res Public Health. (2020) 17:8269. doi: 10.3390/ijerph17218269
15. Razu SR, Yasmin T, Arif TB, Islam MdS, Islam SMS, Gesesew HA, et al. Challenges faced by healthcare professionals during the COVID-19 pandemic: a qualitative inquiry from Bangladesh. Front Public Health. (2021) 9:647315. doi: 10.3389/fpubh.2021.647315
16. Zhang M, Zhang P, Liu Y, Wang H, Hu K, Du M. Influence of perceived stress and workload on work engagement in front-line nurses during COVID-19 pandemic. J Clin Nurs. (2021) 30:1584–95. doi: 10.1111/jocn.15707
17. Cruz JP, Cabrera DNC, Hufana OD, Alquwez N, Almazan J. Optimism, proactive coping and quality of life among nurses: a cross-sectional study. J Clin Nurs. (2018) 27:2098–108. doi: 10.1111/jocn.14363
18. AL-Dossary R. Investigating the feasibility of applying the gig economy framework in the nursing profession towards the Saudi Arabian vision 2030. Inform Med Unlock. (2022) 30:100921. doi: 10.1016/j.imu.2022.100921
19. Mekonen E, Shetie B, Muluneh N. The psychological impact of COVID-19 outbreak on nurses working in the northwest of Amhara regional state referral hospitals, northwest Ethiopia. Psychol Res Behav Manage. (2021) 13:1353–64. doi: 10.2147/PRBM.S291446
20. Moussa ML, Moussa FL, Alharbi HA, Omer T, Khallaf SA, Al Harbi HS, et al. Fear of nurses during COVID-19 pandemic in Saudi Arabia: a cross-sectional assessment. Front Psychol. (2021) 30:736103. doi: 10.3389/fpsyg.2021.736103
21. Albaqawi HM, Pasay-an E, Mostoles R, Villareal S. Risk assessment and management among frontline nurses in the context of the COVID-19 virus in the northern region of the Kingdom of Saudi Arabia. Appl Nurs Res. (2021) 58:1–6. doi: 10.1016/j.apnr.2021.151410
22. Ali S, Noreen S, Farooq I, Bugshan A, Vohra F. Risk assessment of healthcare workers at the frontline against COVID-19. Pak J Med Sci. (2020) 36:99–103. doi: 10.12669/pjms.36.COVID19-S4.2790
23. Nabe-Nielsen K, Nilsson CJ, Juul-Madsen M, Bredal C, Hansen LOP, Hansen AM. COVID-19 risk management at the workplace, fear of infection and fear of transmission of infection among frontline employees. Occup Environ Med. (2021) 78:248–54. doi: 10.1136/oemed-2020-106831
24. Al Baalharith IM, Pappiya EM. Nurses' preparedness and response to COVID-19. Int J Afr Nurs Sci. (2021) 14:1–6. doi: 10.1016/j.ijans.2021.100302
25. World Health Organization. Workers Exposure Risk Assessment and Management in the Context of COVID-19. World Health Organization (2021). Available online at: virus.https://apps.who.int/iris/bitstream/handle/10665/331340/WHO-2019-nCov-HCW_risk_assessment-2020.1-eng.pdf (accessed June 11, 2022).
26. Sehularo LA, Molato BJ, Mokgaola IO, Gause, G. Coping strategies used by nurses during the COVID-19 pandemic: a narrative literature review. Health SA Gesondheid. (2021) 26:1–8. doi: 10.4102/hsag.v26i0.1652
27. Htay MNN, Marz RR, Bahari R, AlRifai A, Kamberi, F, et al. How healthcare workers are coping with mental health challenges during COVID-19 pandemic? A cross-sectional multi-countries study. Clin Epidemiol Glob Health. (2022) 11:100759. doi: 10.1016/j.cegh.2021.100759
28. Zaçe D, Hoxhaj I, Orfino A, Viteritti AM, Janiri L, Di Pietro ML. Interventions to address mental health issues in healthcare workers during infectious disease outbreaks: a systematic review. J Psychiatr Res. (2021) 136:319–33. doi: 10.1016/j.jpsychires.2021.02.019
29. Mubarak N, Safdar S, Faiz S, Khan J, Jaafar M. Impact of public health education on undue fear of COVID-19 among nurses: the mediating role of psychological capital. Int J Ment Health Nurs. (2020) 30:544–52. doi: 10.1111/inm.12819
30. Sun L. Intervention effect of time management training on nurses' mental health during the COVID-19 epidemic. Psychiatr Danub. (2021) 33:626–33. doi: 10.24869/psyd.2021.626
31. Priede A, Lopez-Alvarez I, Carracedo-Sanchidrian D, Gnzalez-Blanch. Mental health interventions for healthcare workers during the first wave of COVID-19 pandemic in Spain. Rev Psiquiatr Salud Ment. (2021) 14: 83–9. doi: 10.1016/j.rpsm.2021.01.005
32. d'Ettorre G, Ceccarelli G, Santinelli L, Vassalini P, Innocenti GP, Alessandri F, et al. Post-Traumatic stress symptoms in healthcare workers dealing with the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. (2021) 18:601. doi: 10.3390/ijerph18020601
33. Qiao H, Yang J, Wang C. Effect of cluster nursing based on risk management strategy on urinary tract infection in patients with severe craniocerebral. Injury Front Surg. (2022) 8:826835. doi: 10.3389/fsurg.2021.826835
34. Albougami AS, Almazan JU, Cruz JP, Alquwez N, Alamri MS, Adolfo CA, et al. Factors affecting nurses' intention to leave their current jobs in Saudi Arabia. Int J Health Sci. (2020) 14:33–40.
35. Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental well-being scale (WEMWBS): development and UK validation. Health Qual Life Outcomes. (2007) 5:63. doi: 10.1186/1477-7525-5-63
36. Cilar L, Pajnkihar M, Štiglic, G. Validation of the Warwick-Edinburgh mental well-being scale among nursing students in Slovenia. J Nurs Manage. (2020) 28:1335–46. doi: 10.1111/jonm.13087
37. Marmara J, Zarate D, Vassallo J, Patten R, Stavropoulos, V. Warwick Edinburgh Mental well-being scale (WEMWBS): measurement invariance across genders and item response theory examination. BMC Psychol. (2020) 28:1335–46. doi: 10.21203/rs.3.rs-857946/v1
38. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. (2020) 3:1–9. doi: 10.1037/t78404-000
39. Mahmood QK, Jafree SR, Qureshi WA. The psychometric validation of FCV19S in urdu and socio-demographic association with fear in the people of the Khyber Pakhtunkhwa (KPK) province in Pakistan. Int J Ment Health Addict. (2020) 20:426–36. doi: 10.1007/s11469-020-00371-4
40. Soraci P, Ferrari A, Abbiati FA, Del Fante E, De Pace R, Urso A, et al. Validation and psychometric evaluation of the Italian version of the fear of COVID-19 scale. Int J Ment Health Addict. (2020) 20:1913–22. doi: 10.1007/s11469-020-00277-1
41. Martínez-Lorca M, Martínez-Lorca A, Criado-Álvarez JJ, Armesilla, M, Latorre J. The fear of COVID-19 scale: validation in Spanish university students. Psychiatry Res. (2020) 293:1–6. doi: 10.1016/j.psychres.2020.113350
42. Elemo AS, Satici SA, Griffiths MD. The fear of COVID-19 scale: psychometric properties of the Ethiopian Amharic version. Int J Ment Health Addict. (2020) 3:1–12. doi: 10.1007/s11469-020-00448-0
43. Sultan S, Bashar A, Nomani I, Tabassum A, Iqbal MS, Fallata E, et al. Impact of COVID-19 pandemic on psychological health of a sample of the health care workers in the western region of Kingdom of Saudi Arabia. Middle East Curr Psychiatry. (2020) 29:5. doi: 10.1186/s43045-022-00174-4
44. Alkhamees AA, Alrashed SA, Alzunaydi AA, Almohimeed AS, Aljohani MS. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Compr Psychiatry. (2020) 102:1–9. doi: 10.1016/j.comppsych.2020.152192
45. Alfaifi A, Darraj A, El-Setouhy M. The psychological impact of quarantine during the COVID-19 pandemic on quarantined non-healthcare workers, quarantined healthcare workers, and medical staff at the quarantine facility in Saudi Arabia. Psychol Res Behav Manage. (2022) 15:1259–70. doi: 10.2147/PRBM.S362712
46. Rathnayake S, Dasanayake D, Maithreepala SD, Ekanayake R, Basnayake PL. Nurses ‘perspectives of taking care of patients with Coronavirus disease 2019: a phenomenological study. PLoS ONE. (2021) 16:e0257064. doi: 10.1371/journal.pone.0257064
47. Al Bujayr AA, Aljohar BA, Bin Saleh GM, Alanazi KH, Assiri AM. Incidence and epidemiological characteristics of COVID-19 among health care workers in Saudi Arabia: a retrospective cohort study. J Infect Public Health. (2021) 14:1174–8. doi: 10.1016/j.jiph.2021.08.005
48. Nguyen LH, Drew DA, Graham, MS, Joshi, AD, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. (2020) 5:E475–83. doi: 10.1016/S2468-2667(20)30164-X
49. Sabetian G, Moghadami M, Haghighi L, Shahriarirad R, Fallahi MJ, Asmarian, et al. COVID-19 infection among healthcare workers: a cross-sectional study in Southwest Iran. Virol J. (2021) 18:58. doi: 10.1186/s12985-021-01532-0
50. Shwe S, Sharma AA, Lee P. Personal protective equipment: attitudes and behaviors among nurses at a single university medical center. Cureus. (2021) 13:e20265. doi: 10.7759/cureus.20265
51. Keleb A, Ademas A, Lingerew M, Sisay T, Berihun G, Adane M. Prevention practice of COVID-19 using personal protective equipment and hand hygiene among healthcare workers in public hospitals of South Wollo Zone, Ethiopia. Front Public Health. (2021) 2:782705. doi: 10.3389/fpubh.2021.782705
52. Smith L, Serfioti D, Westonn D, Greenberg N, James Rubin G. Adherence to protective measures among healthcare workers in the UK: a cross-sectional study. Emerg Med J. (2022) 39:100–5. doi: 10.1136/emermed-2021-211454
53. Zhang N, Lei H, Li L, Jin T, Liu X, Miao D, et al. COVID-19 vaccination did not change the personal protective behaviors of healthcare workers in China. Front Public Health. (2021) 21:777426. doi: 10.3389/fpubh.2021.777426
54. Abo-Ali EA, Al-Rubaki S, Lubbad S, Nchoukati M, Alqahtani R, Albraim S, et al. Mental well-being and self-efficacy of healthcare workers in Saudi Arabia during the COVID-19 pandemic. Risk Manage Healthc Policy. (2021) 14:3167–77. doi: 10.2147/RMHP.S320421
55. World Health Organization. Weekly Epidemiological Update on COVID-19-−5 April 2022 Edition 86. World Health Organization (2022). Available online at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19-−5-april-2022 (accessed June 1, 2022).
56. Mohsin SF, Agwan MA, Shaikh S, Alsuwaydani ZA, AlSuwaydani SA. COVID-19: fear and anxiety among healthcare workers in Saudi Arabia. A cross-sectional study. SAGE J. (2021) 58:469580211025225. doi: 10.1177/00469580211025225
57. Ministry of Health. MOH Publications COVID-19 Guidelines. Ministry of Health (2022). Available online at: https://www.moh.gov.sa/en/Ministry/MediaCenter/Publications/Pages/covid19.aspx (accessed June 1, 2022).
58. Cheung T, Yip PS. Depression, anxiety and symptoms of stress among Hong Kong nurses: a cross-sectional study. Int J Environ Res Public Health. (2015) 12:11072–100. doi: 10.3390/ijerph120911072
59. Almazan JU, Albougami AS, Alamri MS. Exploring nurses' work-related stress in an acute care hospital in KSA. J Taibah Univer Med Sci. (2019) 14:376–82. doi: 10.1016/j.jtumed.2019.04.006
60. Chen R, Sun C, Chen JJ, Jen HJ, Kang XL, Kao CC, et al. A large-scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID-19 pandemic. Int J Ment Health Nurs. (2021) 30:102–16. doi: 10.1111/inm.12796
Keywords: COVID-19, fear perception, risk assessment and management, mental wellbeing, pandemic
Citation: Al-Dossary RN, AlMahmoud S, Banakhar MA, Alamri M, Albaqawi H, Al Hosis K, Aljohani MS, Alrasheadi B, Falatah R, Almadani N, Aljohani K, Alharbi J and Almazan JU (2022) The relationship between nurses' risk assessment and management, fear perception, and mental wellbeing during the COVID-19 pandemic in Saudi Arabia. Front. Public Health 10:992466. doi: 10.3389/fpubh.2022.992466
Received: 12 July 2022; Accepted: 03 October 2022;
Published: 10 November 2022.
Edited by:
Oriol Yuguero, Lleida Institute for Biomedical Research (IRBLleida), SpainReviewed by:
Fatih Sekercioglu, Ryerson University, CanadaBushra Elhusein, London Health Sciences Centre, Canada
Copyright © 2022 Al-Dossary, AlMahmoud, Banakhar, Alamri, Albaqawi, Al Hosis, Aljohani, Alrasheadi, Falatah, Almadani, Aljohani, Alharbi and Almazan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joseph U. Almazan, Sm9hbG1hemFuMDMwQGdtYWlsLmNvbQ==; am9zZXBoLmFsbWF6YW5AbnUuZWR1Lmt6
 Reem N. Al-Dossary
Reem N. Al-Dossary Sana AlMahmoud
Sana AlMahmoud Maram Ahmed Banakhar
Maram Ahmed Banakhar Majed Alamri
Majed Alamri Hamdan Albaqawi
Hamdan Albaqawi Khaled Al Hosis5
Khaled Al Hosis5 Mohammed S. Aljohani
Mohammed S. Aljohani Bader Alrasheadi
Bader Alrasheadi Rawaih Falatah
Rawaih Falatah Noura Almadani
Noura Almadani Khalid Aljohani
Khalid Aljohani Jalal Alharbi
Jalal Alharbi Joseph U. Almazan
Joseph U. Almazan