- 1Shifa College of Nursing, Shifa Tameer-e-Millat University, Islamabad, Pakistan
- 2Department of Physiological Nursing, School of Nursing and Department of Epidemiology & Biostatistics, School of Medicine, University of California, San Francisco, San Francisco, CA, United States
Background: Patient-centered care in diabetes self-management might be a significant factor in improving health outcomes of adults with type 2 diabetes, yet the supporting evidence is inadequate. This review aimed at assessing the effectiveness of patient-centered self-management care interventions on glycemic control (HbA1c) and self-care behaviors compared with usual care.
Methods: CINAHL, PubMed, Cochrane Library, Google Scholar, and the HEC Digital Library were searched for studies in English language that assessed patient-centered self-management educational and/or behavioral interventions in adults aged 18 years or older with type 2 diabetes from 2005 to 2020. Interventional studies with at least 3 months of follow-up and reporting on self-care outcomes such as glycemic control (HbA1c) and self-care behaviors including diet control, physical activity, foot care, and medication adherence were included.
Results: Of 168 identified records, 24 were found eligible comprising 20 RCTs and four QESs with total 4,083 participants. The meta-analysis involved 19 RCTs that provided enough information for a pooled estimate of HbA1c. Compared with the control group, patient-centered self-management interventions significantly lowered HbA1c, −0.56 (95% CI −0.79, −0.32). Stratified analysis for HbA1c with respect to various aspects of intervention showed larger effects in interventions employing both educational and behavioral components, −0.66 (95% CI −0.97, −0.34); spanned over shorter (<03 months) duration, −0.85 (95% CI −1.28, −0.43); administered by nurses, −0.80 (95% CI −1.44, −0.16); and delivered in community settings −0.70 (95% CI −1.14, −0.26).
Conclusion: This systematic review provided evidence supporting the effectiveness of patient-centered self-management care interventions in improving glycemic control and self-care behaviors in adults with type 2 diabetes and identified key features of intervention contributing toward success.
Introduction
Diabetes mellitus (DM) is one of the major health problems of the 21st century due to its growing prevalence and the risk of increased morbidity and mortality (1, 2). In 2021, the International Diabetes Federation (IDF) estimated that one in 10 adults aged 20–79 years have DM, equivalent to 537 million people worldwide (3). The IDF report showed a higher prevalence in the Middle East and North Africa, especially in low- and middle-income countries where three in four adults are affected. (4) More than 90% of patients with DM have type 2, simply known as type 2 diabetes. Micro- and macrovascular complications resulting from hyperglycemia in type 2 diabetes affect individuals' functional capacity, quality of life, and demand for healthcare services, with a significant economic impact on healthcare system and national economies (5, 6). The rise in type 2 diabetes is driven by socioeconomic, demographic, environmental, and genetic factors (7, 8). Age, sedentary lifestyle, metabolic syndrome, systematic low-grade inflammation, and insulin resistance are all well-known risk factors for type 2 diabetes. Type 2 diabetes is also linked with obesity, and there is a strong immune-metabolic connection between the two diseases (9). Furthermore, in low- to middle-income countries, a poor healthcare system, inaccessibility to healthcare centers, inequality in the provision of healthcare services, gender disparity, and poor socioeconomic conditions, as well as low level of education, are all contributing factors (10).
The growing prevalence of type 2 diabetes and the associated health and economic burden must be addressed on an urgent basis. The only pillar is delaying disease progression and avoiding diabetes-related complications, which may lead to better health and economic outcomes for patients, families, society, and the healthcare system as a whole. Evidence based guidelines suggest that progression of type 2 diabetes can be delayed and serious complications might be avoided by adopting a healthy lifestyle through improvement in self-care behaviors with medication as required (11). Therefore, type 2 diabetes is also known as a self-managed condition because the majority of the care is provided by patients themselves (12).
However, self-management requires patients' full commitment and capability to perform self-care activities, including healthy dietary habits, physical activity, blood glucose monitoring, and regular intake of medicines. Patients need to make a concerted and self-motivated effort toward adoption of a healthy life style as pharmacotherapy alone cannot achieve these goals (13). Also, type 2 diabetes is associated with complexity because there are multiple risk factors mostly involving a behavioral or social component that the individuals, their family, or society must struggle hard to implement. Therefore, a patient-centered behavioral or social approach would make a long-lasting impact toward effective disease management. Patient-centered care (PCC) has been recognized as a desirable attribute of healthcare since the late 1980s when the concept ‘patient-centeredness' was introduced. Patient-centeredness is characterized by utilization of a bio-psycho-social perspective, which means focusing on patients and honoring their preferences as a holistic being, rather than adopting a biomedical perspective that focuses on the disease (14). The shift from a biomedical model to a patient-centered care model may necessitate more effective patient engagement, collaboration on an individual care plan, and motivation of patients to adopt self-management behaviors (15). Therefore, PCC is characterized as a care that is tailored to the patients' specific needs, values, and preferences (16). PCC is an important factor in the self-management of type 2 diabetes and is associated with improved health outcomes such as quality of life and self-care behaviors in this population (17). The American Diabetes Association (ADA), in their consensus report, also advocated PCC to enhance patient engagement in self-care activities for type 2 diabetes self-management (18). Moreover, PCC improved patient activation in terms of knowledge, motivation, confidence, and skills, as well as better illness perception and a lower level of distress, in people with type 2 diabetes (19).
PCC in type 2 diabetes is defined as a purposefully designed holistic care intervention that provides information and skills needed for effective self-management of the disease based on patients' preferences to achieve optimum glycemic control by improving self-care behaviors in addition to medication (20). Self-management education is the major component of PCC that, according to the WHO, provides the basis for management of the disease (21). The literature supports that up to 8% of DM-associated complications can be reduced through proper self-management education (22). Behavioral intervention is another major component of PCC in type 2 diabetes self-management. The American Association of Diabetes Educators (AADE) suggests to prepare patients for behavior modification by equipping them with the necessary skills to improve their self-care behaviors. According to the AADE, seven parameters of self-care behaviors are healthy diet, regular physical activity, regular blood sugar monitoring, medication adherence, effective problem-solving approach, resilient coping skills, and risk reduction behaviors (23). Studies have shown behavioral interventions aimed at self-care activities significantly improved glycemic control, reduced diabetes-associated complications, and contributed to enhanced quality of life of patients with diabetes (24). A meta-analysis published in 2003 has demonstrated the effectiveness of behavioral interventions in improving self-care outcomes and the overall health status in patients with type 2 diabetes (25).
Given the increasing prevalence of type 2 diabetes worldwide and the risk of increased morbidity and mortality, PCC can play a crucial role in effective self-management of the disease. Therefore, an updated systematic review of PCC would give a better understanding of whether this care approach is associated with better clinical outcomes. This review aimed at assessing the effectiveness of PCC employing educational and behavioral interventions on glycemic control and self-care behaviors in adults with type 2 diabetes compared with usual care.
Methods
Search strategy
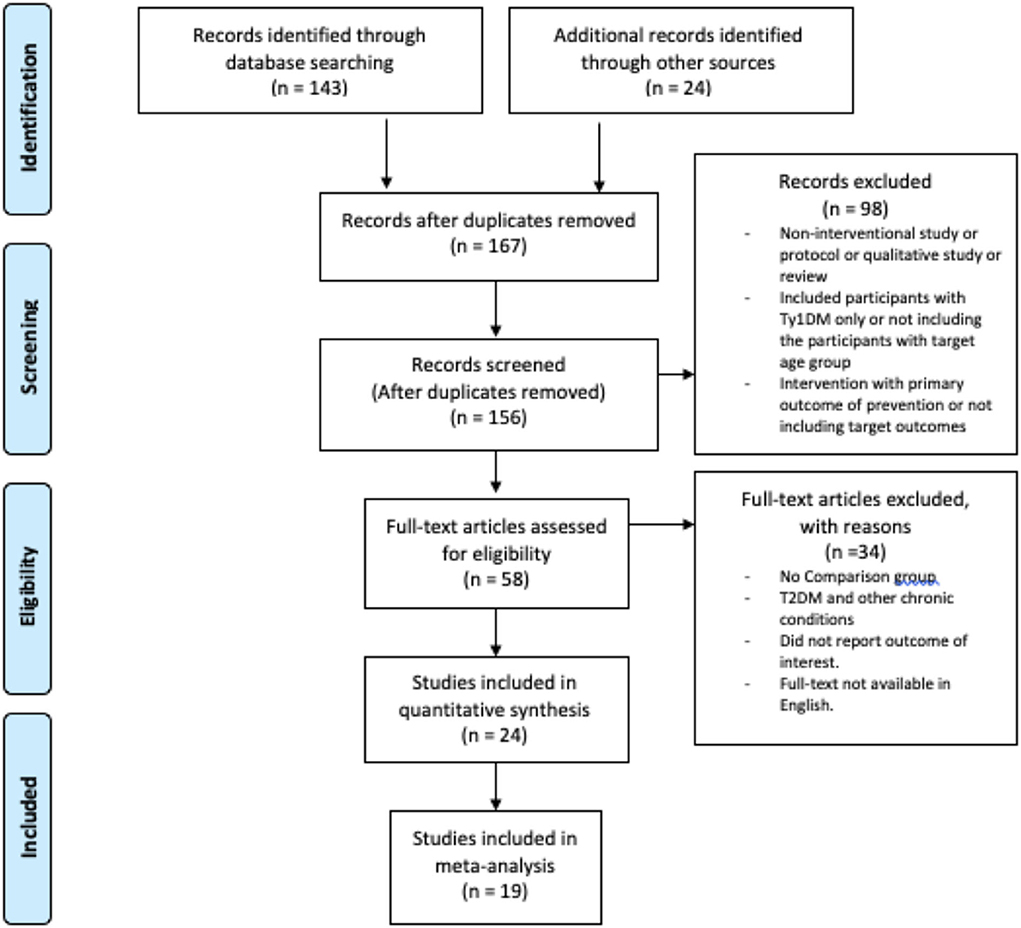
The literature search was performed in CINAHL, PubMed, Cochrane Library, Google Scholar, and the HEC Digital Library for studies in English language published between 1 January 1990 and 30 October 2020. 1 January 1990 has been selected as the search initiation date because the term patient-centered care/patient centeredness have been introduced in the literature in the late 1980s (26). The Medical Subject Headings (MeSH) terms and TIAB terms used were “Diabetes Mellitis, Type 2” OR “Type 2 Diabetes,” OR “Type II Diabetes,” AND “Patient-Centered-Care,” OR “Person-Oriented-Care,” OR “Holistic Care,” AND “Self-Management,” OR “Self-Care” AND “Glycated Hemoglobin A” OR Glycemic Control” or “HbA1c” AND “Self-Care Behaviours” OR Self-Care Activities”. The retrieved titles and abstracts were evaluated for relevance. Articles found relevant were reviewed as full text for consideration of inclusion in this review by completing the eligibility form based on inclusion criteria. In addition to systematic database searches, a manual search was performed to find studies in reference lists of relevant articles and reviews. Duplicates were removed with the help of Mendeley Reference Manager. With the exception of one study conducted in 1998 (27), the initial search in the databases retrieved records between 2005 and 2020. Because a study carried out in the 1990s would offer a limited scope due to changes in lifestyle, the search duration was reduced to 2005–2020. This review was planned, conducted, and reported in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (28). The PRISMA flowchart for selection of the studies and reasons for exclusion are presented in Figure 1.
Inclusion and exclusion criteria
Studies were found eligible if they meet the following inclusion criteria: (1) type of studies as interventional studies including randomized controlled trials (RCTs) and quasi-experimental studies (QESs); (2) type of participants as adults (≥ 18 years) diagnosed with type 2 diabetes for at least last 6 months; (3) type of intervention as patient-centered care intervention for diabetes self-management with educational and/or behavioral component provided in any setting, by any method, by any provider, for any contact time, and with at least 3 months of follow-up; (4) comparison intervention as usual care or standard care; and last, (5) type of outcomes involving glycemic control (HbA1c) as the primary outcome, and self-care behaviors including diet control, physical activity, foot care, and medication adherence as secondary outcomes.
The following studies were excluded: (1) review, (2) non-intervention study, (3) qualitative study, (4) protocol, (5) patients with type 1 diabetes only, (6) adult patients with type 2 diabetes and with other chronic conditions, and (7) patients younger than 18 years targeted exclusively at prevention of type 2 diabetes.
Data extraction
Data from the eligible studies were extracted and entered into an Excel sheet. Entered data were verified two times for accuracy and completeness. Discrepancies in the extracted data were discussed, and disagreements were adjudicated by reaching consensus.
Quality assessment of individual studies
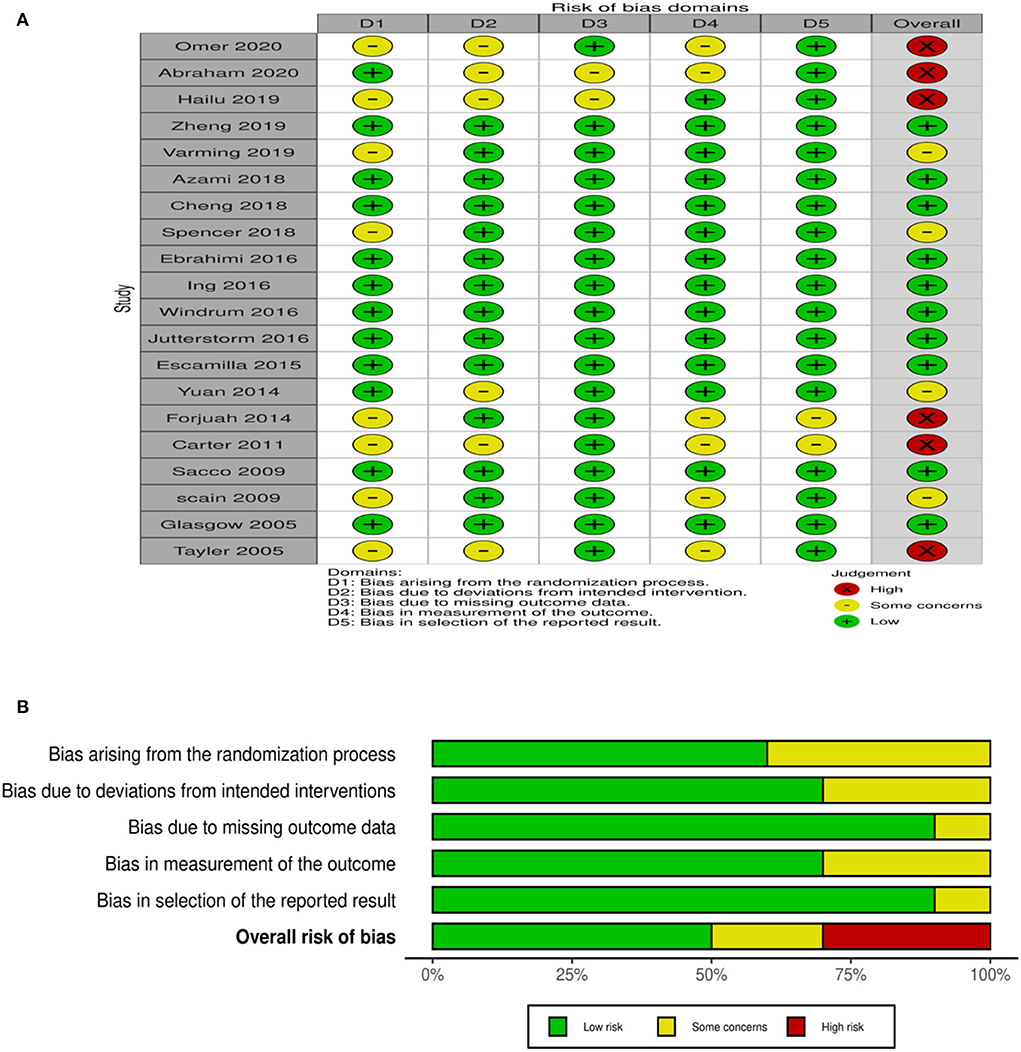
Individual studies were assessed for methodological quality by using the Cochrane Collaboration risk-of-bias assessment tool that yields a judgment for low, high, or unclear risk (expressing some concerns). Authors of the studies were contacted to request additional information. Rob 2 (version 2 of the Cochrane risk-of-bias tool for randomized trials) was used for RCTs (29). Quality of included RCTs was assessed on five domains of risk of bias in the randomization process, deviation in intended intervention, missing outcome data, measurement of outcome, and selection of the reported result, as shown in Figure 2 with a summary plot.
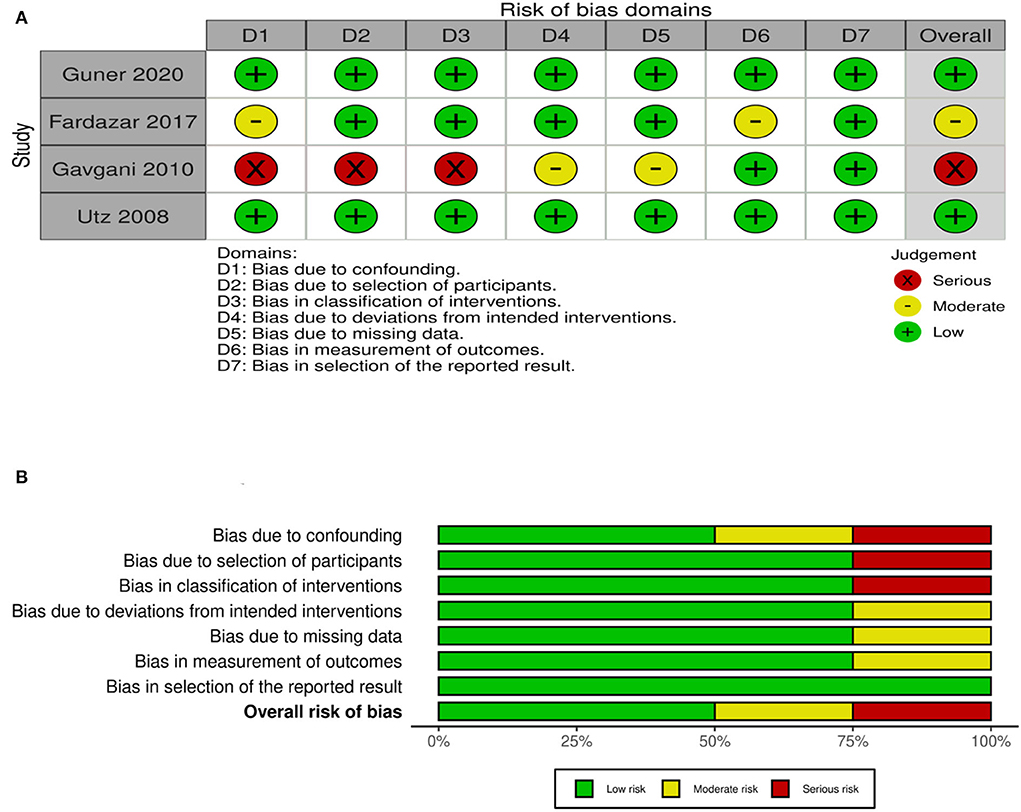
For quality assessment of QESs, Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I) was used (30). Quality of QESs assessed by using ROBINS-1 on seven domains is given in Figure 3 with a summary plot.
Statistical analysis
A meta-analysis was performed using REVMAN 5.4.1 to calculate the magnitude of pooled effect size for change in HbA1c, the primary outcome (31). Of 24 included studies, 22 reported on HbA1c, which included 19 RCTs and three QESs. However, only RCTs were included in the meta-analysis due to their optimal validity and causal inference. Data entered in REVMAN involved final values of mean and standard deviation of HbA1c for the experimental group and control group, and the number of participants in each group. Standardized mean difference of HbA1c between experimental and control groups and 95% confidence intervals were calculated for estimation of effect size. I2 statistics were used to estimate statistical heterogeneity among studies. The random effect model was applied on more than 50% heterogeneity (32). To further explore sources of heterogeneity, stratified analysis was performed based on key aspects of intervention, including (a) component of intervention (educational vs. educational and behavioral), (b) duration of intervention (<3 months vs. 3–6 months vs. > 6 months), (c) provider of intervention (nurse vs. other professional vs. ≥ 2 disciplines), and (d) setting of intervention (hospital vs. community vs. combined hospital and community).
Results
Characteristics of studies
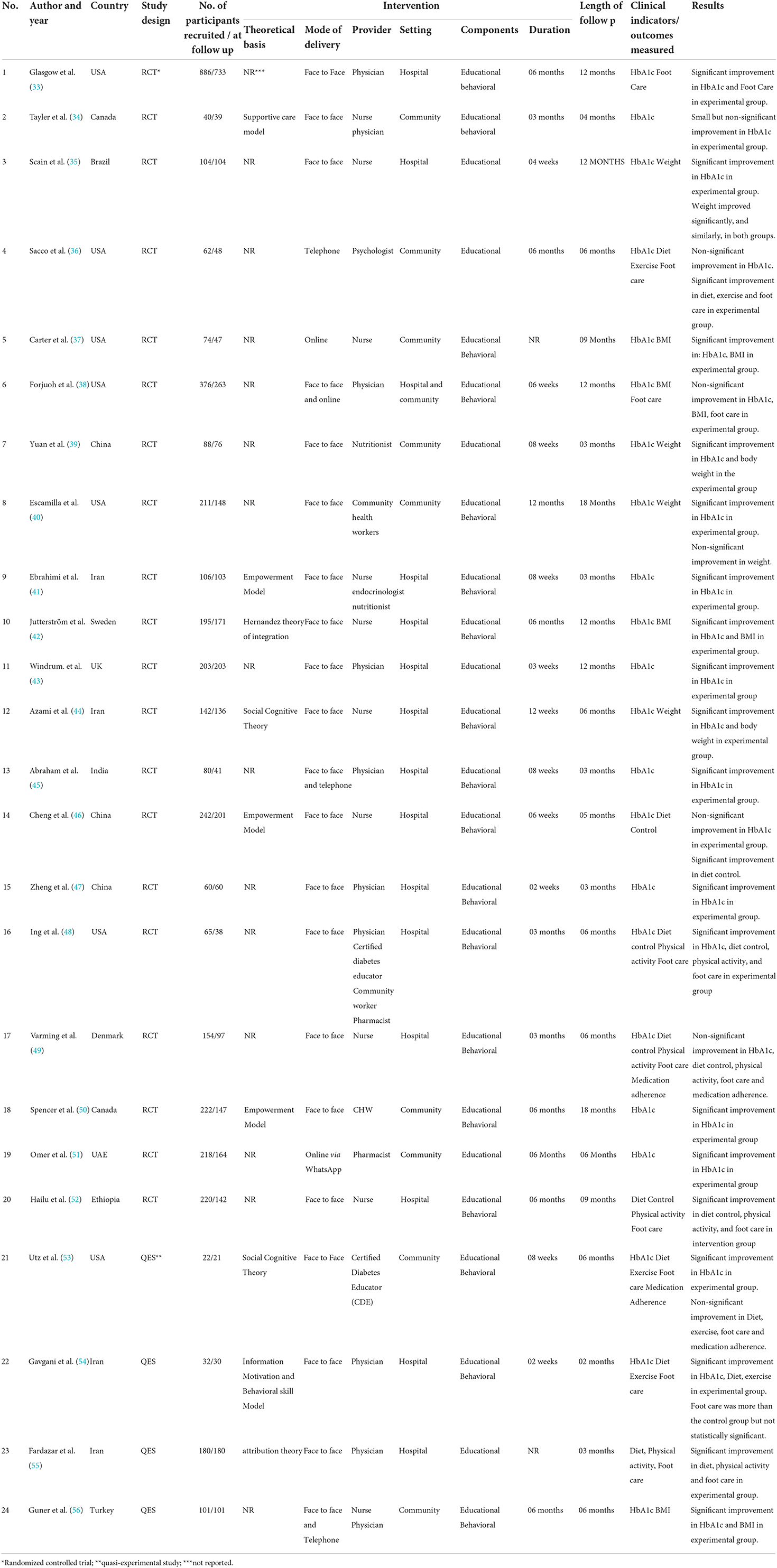
For this review, 24 studies met the eligibility criteria. The included studies were published between 2005 and 2020 where the majority was published between 2015 and 2020. A majority of the studies were RCTs, accounting for 83%. In total, 4,083 participants were involved, with the mean age of 56.1 years (range 18–69 years). The study population involved patients with type 2 diabetes, with a mean duration of disease of 7.5 years (range 06–12.9 years). The sample size of a single study ranged from 22 to 886 involving both male and female patients. The characteristics of included studies are presented in Table 1.
Characteristics of intervention
Interventions of all studies were compared with usual care. Usual care majorly involved consultation with the physician; having blood sugar, blood pressure, and weight checked; and getting scheduled for the next appointment, which sometimes included verbal or written guidance on lifestyle changes. Overall, 37.5% of (nine of 24) studies reported on the theoretical model used for design and implementation of DM self-management intervention (34, 41, 42, 44, 46, 50, 53–55). In total, two studies (44, 53) based their intervention on the social cognitive theory; three studies (41, 46, 50) on the empowerment model; one study based on the supportive care model (34), one based on information motivation and behavioral skill model (54), one based on the Hernandez theory of integration (42), and one based on the attribution theory (55). The mean duration of intervention was 12 weeks, ranging from 2 weeks (54) to 12 months (40). A wide range of intensity of intervention was reported ranging from 15 to 20 min over a day to 1,530 min over 12 months. The majority of the (18 of 24) studies administered both educational and behavioral components of intervention. The follow-up duration ranged from 2 months (54) to 18 months (40). A few (four of 24) studies used the multidisciplinary care approach involving two or more than two different members of the healthcare team delivering the intervention. The majority of studies involved interventions delivered at hospitals and some in community settings, whereas only one study reported administration of intervention both in hospitals and in community settings (38).
Study outcomes
Primary outcome (glycemic control HbA1c)
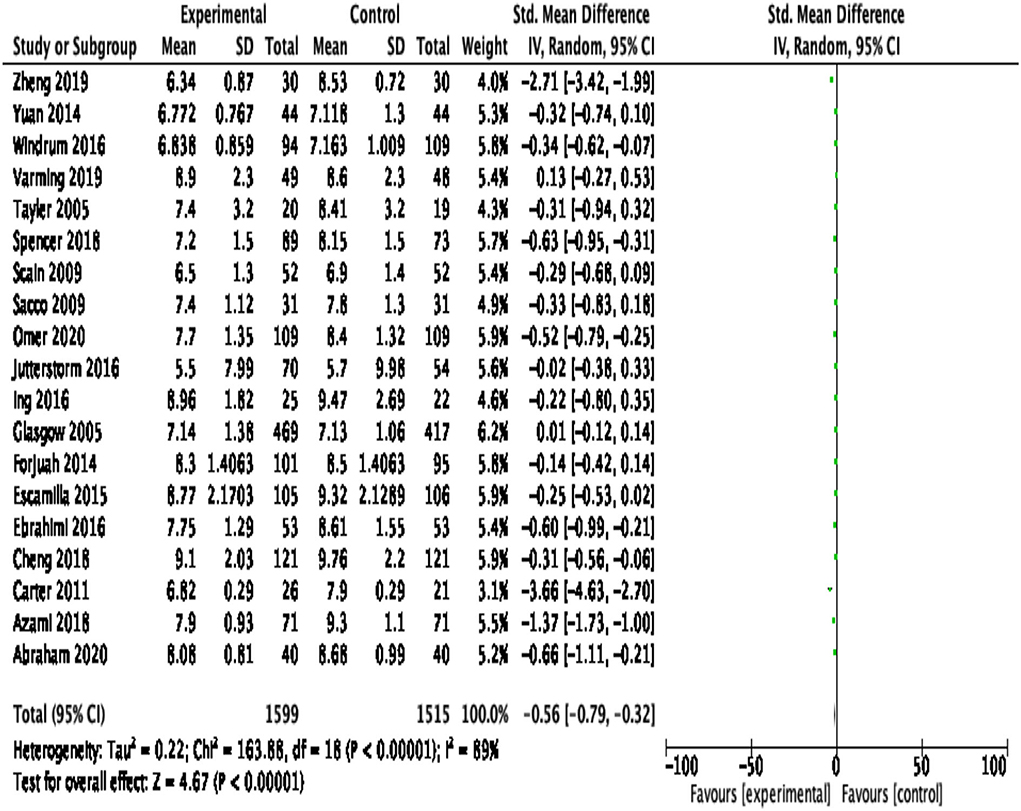
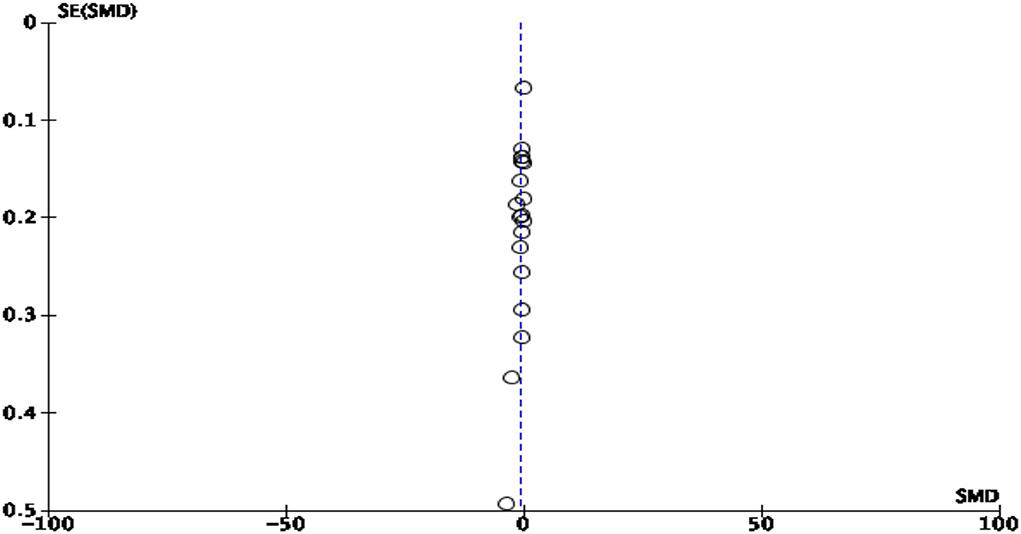
HbA1c was reported as an outcome measure in 22 studies. The majority of the studies reported statistically significant reduction in HbA1c. Because of the significant heterogeneity (>50%) among studies, the random effect model was applied. At 95% CI with 3,114 participants in 19 RCTs, the magnitude of effect, −0.56 (95% CI −0.79, −0.32), was statistically significant (p < 0.00001), showing a substantial reduction in HbA1c in the experimental group compared with the control group. The pooled effect size of HbA1c is shown in Figure 4. The likelihood of publication bias among studies was measured using a Funnel plot, as illustrated in Figure 5. When there is no suspicion of publication bias, the observed studies are scattered symmetrically around the pooled effect size. Visual inspection of the funnel plot shows that the observed studies are clustered around the mean, displaying an equal distribution. However, there are gaps with no scattered points to the left and right of the mean, signifying some publication bias.
Stratified analysis based on components of intervention
Earlier, Gary TL et al. in their meta-analysis concluded that studies with the behavioral component of intervention were found more effective in reducing HbA1c than studies involving the educational component only (25). In this analysis, studies were sub-grouped into two components of intervention: (1) educational only and (2) combined educational and behavioral intervention. Pooled effect size indicated that studies with combined educational and behavioral components yielded larger effect size (−0.66; 95% CI −0.97, −0.34) than studies with the educational component only (−0.39; 95% CI −0.54, −0.24). Overall heterogeneity (I2) was 89%; therefore, the random effect model was applied (see Figure 6A).
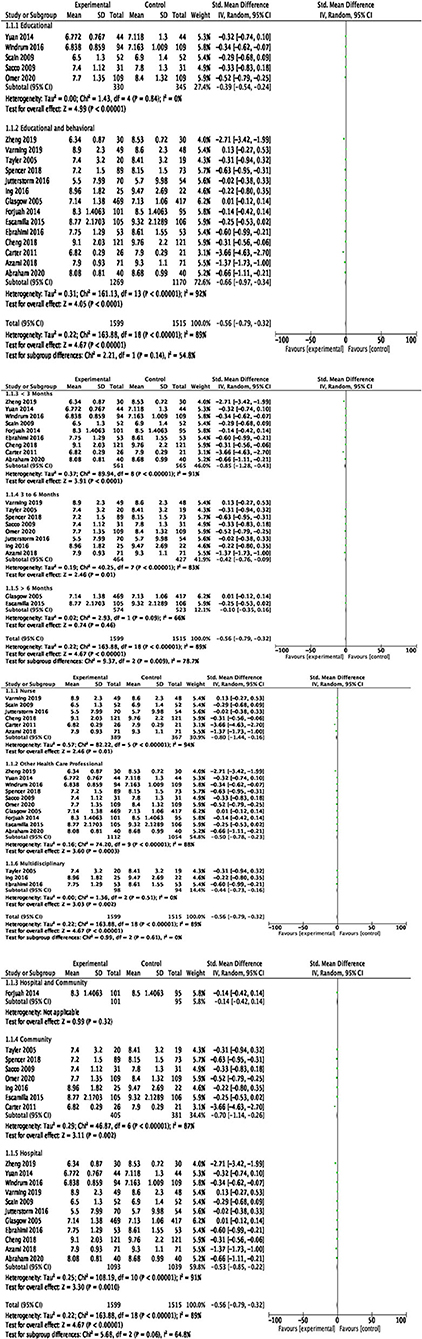
Figure 6. (A) Pooled effect size of HbA1c in studies sub-grouped by components of intervention; (B) pooled effect size of HbA1c in studies sub-grouped by duration of intervention; (C) pooled effect size of HbA1c in studies sub-grouped by provider of intervention; (D) pooled effect size of HbA1c in studies sub-grouped by setting of intervention.
Stratified analysis based on duration of intervention
Existing evidence suggested that a longer duration of intervention (> 6 months) showed significant reduction in HbA1c compared with a shorter duration (< 6 months) (25) Considering the span of intervention, studies were sub-grouped into (1) studies with a duration of intervention < 3 months, (2) 3–6 months, and (3) > 6 months. Pooled effect size indicated that studies with a shorter duration (< 3 months) produced larger effect size (−0.85; 95% CI −1.28, −0.43) than studies with a duration of intervention of 3–6 months (−0.42; 95% CI −0.76, −0.09) and studies with a longer duration of intervention of > 6 months (−0.10; 95% CI −0.35, −0.16). Overall heterogeneity (I2) was 89%; therefore, the random effect model was applied (see Figure 6B).
Stratified analysis based on provider of intervention
Evidence suggests that a multidisciplinary team approach is more effective in improving HbA1c (57). Given this, a stratified analysis was performed by dividing studies into three groups based on the provider of intervention: (1) a nurse, (2) other healthcare professional such as a physician, nutritionist, pharmacist, or community health worker; and (3) multidisciplinary team members (≥ 2 disciplines). Pooled effect size indicated that studies involved a nurse as a provider of intervention produced larger effect size (−0.80; 95% CI −1.44, −0.16) than studies with other professional as s provider (−0.50; 95% CI −0.78, −0.23) and studies involving ≥ 2 disciplines (−0.44; 95% CI −0.73, −0.16). Overall heterogeneity (I2) was 89%; therefore, the random effect model was applied (see Figure 6C).
Stratified analysis based on setting of intervention
To see the effect of setting, a stratified analysis was performed by grouping studies into three categories: (1) hospital, (2) community, and (3) combined setting including both hospital and community. Studies with intervention delivered in community settings produced larger effect size (−0.70; 95% CI −1.14, −0.26) than those in hospitals (−0.53; 95% CI −0.85, −0.22) and combined settings (−0.14; 95% CI −0.42, −0.14). Overall heterogeneity was 89%; therefore, a random effect model was applied (see Figure 6D).
Secondary outcomes
Secondary outcomes included diet control, physical activity, foot care, and medication adherence. A total of 16 (35–40, 42, 44, 46, 48, 49, 52–56) studies reported on dietary outcomes including body mass index (BMI) and weight, where the majority (69%; 11 of 16) showed statistically significant improvement in diet control in the experimental group receiving PCC; seven studies (36, 48, 49, 52–55) reported on physical activity or exercise outcomes, where the majority (71%; five of seven) showed significant improvement in physical activity in the experimental group receiving PCC; nine studies (33, 36, 38, 48, 49, 52–55) reported on foot care outcome, where more than half (55%; five of nine) showed statistically significant improvement in foot care in the experimental group receiving PCC; and two studies (49, 53) reported on this outcome that showed non-significant improvement in medication adherence in the experimental group receiving PCC.
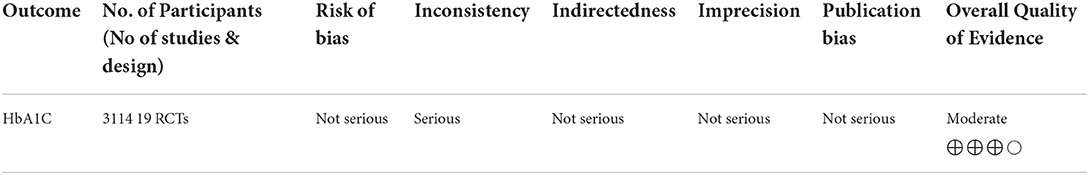
Summary of findings
Table 2 shows a summary of findings including the sum of available data on primary outcomes (HbA1c), magnitude of the intervention effect, and certainty of evidence utilizing the Group Reading Assessment and Diagnostic Evaluation (GRADE) approach (58).
Table 2 illustrates that in terms of risk of bias, none of the RCTs demonstrated a high risk in any of the five domains. Of the 19 RCTs, 10 had a low risk of bias; four had some concerns in one domain, indicating an unclear risk of bias; and five RCTs had high risk of bias, showing some concerns in multiple domains. There is inconsistency found in the results of HbA1c indicated by substantial heterogeneity. Variability in the social environment and conditions of delivery of intervention, which may not be discernible from published results, may be the reasons for this unexplained heterogeneity. With regard to indirectness, the patients, interventions, and comparison in the included studies provided direct evidence to the clinical question. However, the authors examined some variations in the mode and delivery of intervention. In terms of imprecision, the authors judged to have no serious imprecision. The included trials enrolled 4,113 patients, with some trials reporting significant results and others reporting non-significant results, most likely due to the small number of participants enrolled, which resulted in wide confidence intervals and no effects. Last, the authors did not find strong suspicion of publication bias since both the positive and negative results of trials were reported. Summarizing all, the authors judged the overall quality of the evidence as moderate. Future research focusing on PCC social and situational factors will likely have a significant impact on the confidence in effect estimate.
Discussion
This review aimed at evaluating the effectiveness of patient-centered self-management care interventions on self-care outcomes of adults with type 2 diabetes compared with usual care. The most important indicator of optimum management of DM is glycemic control (HbA1c). Therefore, the primary outcome of this review was glycemic control (HbA1c), whereas changes in diet control, physical activity, foot care, and medication adherence were the secondary outcomes.
To estimate the overall effect of intervention, a meta-analysis was performed to calculate the magnitude of effect size for change in HbA1c. Pooled effect size indicated a statistically significant difference in HbA1c between experimental and control groups, −0.56 (95% CI −0.79, −0.32). The findings of this review are similar to the findings of previous meta-analysis by Gray et al. in 2003, which reported statistically significant reduction in HbA1c, −0.43 (95% CI −0.71, −0.15) (25). This review confirmed that the patient-centered self-management interventions are accompanied with a significant decrease in HbA1c. Since HbA1c is one of the important predictors of DM-associated complications and a key therapeutic goal toward its effective self-management, findings of this review have some important implications for contemporary practice. Evidence suggests that 21% of risk is reduced for any DM-associated complication and its related deaths with a 1% decline in HbA1c (59). Thus, reduction in HbA1c has clinical significance. However, unexplained heterogeneity due to variations in the social environment and conditions of intervention administration may hamper meta-analysis results. Moreover, patient-centered self-management care interventions are influenced by multiple situational factors, such as marital status, socioeconomic conditions, and cultural norms. There is a need to explore such situational and sociocultural factors affecting patient-centered care provision.
To explore heterogeneity further, a stratified analysis for change in HbA1c was performed with regard to various key aspects of intervention to ascertain key elements that might contribute toward effective self-management of type 2 DM. In this review, interventions involving educational and behavioral components, spanned over a shorter (< 3 months) duration, provided by nurses, and delivered in community settings were found more effective as indicated by larger effect sizes. Some findings of this review are contrary to those of the previous meta-analysis by Gary et al., where interventions that involved a longer duration (>3 months) and provided by physicians were found more effective. It appears that interventions with a longer duration may carry out an element of fatigue due to long contact times, which may produce lesser effect. A previous systematic review by Norris et al. (60) also found inconsistencies in the duration of intervention and its beneficial effects. There is a need to further explore the factors associated with the intervention duration demonstrating an area of research. Moreover, the finding of this review showing larger effects with nurses as providers of intervention emphasizes the importance that nurses are uniquely positioned to bring their expertise and knowledge toward effective self-management of type 2 diabetes. This again demonstrates an area of research to further investigate the clinical effectiveness of nurse-led interventions. The findings are consistent with those of a previous meta-analysis with regard to the setting of intervention confirming that interventions delivered in community settings are more effective. This confirms that community settings are the best place for patients living in neighborhood to form peer groups in order to gain diabetes knowledge, reinforce each other, and receive support for change in behavior.
With regard to secondary outcomes, this review indicated that patient-centered self-management care interventions are effective in improving patients' diet control, physical activity, and foot care. Diet control improved significantly in the majority of included studies, confirming the findings of a previous systematic review by Norris et al. (60) These findings are also consistent with Williams et al. stating that PCC improves dietary behaviors in patients with type 2 DM (17). The change in physical activity was also found effective, confirming the results of previous studies (61, 62). However, the effect on medication adherence was not found significant, which may be due to the reason that only two studies reported this outcome. These findings are not consistent with the study by Williams et al., which reported a significant association of PCC with medication adherence (17). This may necessitate an area of further exploration, which could help identify the key components of PCC interventions targeting medication adherence. Overall, this review provided with the evidence that PCC for self-management is effective in improving glycemic control and self-care behaviors in adults with type 2 diabetes.
Limitations and strengths
The limitations of this review are as follows: including only studies in English language; selective reporting of the outcomes, which might have affected the findings; frequent methodological biases found in included studies; insufficient description of intervention in the included studies; and failure in reporting medications or any drug prescription information because medication intake may act as a confounder between the interventions and outcomes.
However, this review has several strengths: rigorous reviewing methods, a thorough search to capture all relevant information, explicit and reproducible eligibility criteria, and stratified analysis with answers to clinically relevant and important questions.
Conclusion
Overall, this review provided with the evidence that PCC for self-management is effective in improving glycemic control and self-care behaviors in adults with type 2 diabetes. Some gaps were found that are needed to be addressed: (1) only few studies provided a thorough description with regard to the intervention including intensity, duration, length of follow-up, and theoretical background; (2) the behavioral component was not described in adequate detail with regard to the methods applied, and (3) medication adherence was reported only by a few studies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
KA: study conception and design, literature retrieval, and drafting of the manuscript. KD: data analysis and interpretation and critical revision of the manuscript. RG: study conception, critical revision, and final approval of the manuscript. EF: conceptualizing the review process, data analysis and interpretation, critical revision, and final approval of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AADE, American Association of Diabetes Educators; ADA, American Diabetes Association; CINAHL, Cumulative Index to Nursing and Allied Health; DM, diabetes mellitus; GRADE, Grading of Recommendations, Assessment, Development, and Evaluation; IDF, International Diabetes Federation; PCC, patient-centered care; QES, quasi-experimental study; RCT, randomized controlled trial; WHO, World Health Organization.
References
1. Glovaci D, Fan W, Wong ND. Epidemiology of diabetes mellitus and cardiovascular disease. Curr Cardiol Rep. (2019) 21:1–8. doi: 10.1007/s11886-019-1107-y
2. Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: a review of current evidence. Diabetologia. (2019) 62:3–16. doi: 10.1007/s00125-018-4711-2
3. Federation ID. IDF Diabetes Atlas 10th Edition. International Diabetes Federation. (2021) p. 905–11.
4. Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF diabetes atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for (2045). Diabetes Res Clini Pract. (2022) 183:109119. doi: 10.1016/j.diabres.2021.109119
5. Khan MA, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes–global burden of disease and forecasted trends. J Epidemiol Glob Health. (2020) 10:107. doi: 10.2991/jegh.k.191028.001
6. Williams R, Karuranga S, Malanda B, Saeedi P, Basit A, Besançon Besançon S, et al. Global and regional estimates and projections of diabetes-related health expenditure: results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clini Pract. (2020) 162:108072. doi: 10.1016/j.diabres.2020.108072
7. Hills AP, Arena R, Khunti K, Yajnik CS, Jayawardena R, Henry CJ, et al. Epidemiology and determinants of type 2 diabetes in south Asia. Lancet Diabetes Endocrinol. (2018). 6:966–78. doi: 10.1016/S2213-8587(18)30204-3
8. Kyrou I, Tsigos C, Mavrogianni C, Cardon G, Van Stappen V, Latomme J, et al. Sociodemographic and lifestyle-related risk factors for identifying vulnerable groups for type 2 diabetes: a narrative review with emphasis on data from Europe. BMC Endocr Disord. (2020) 20:1–3. doi: 10.1186/s12902-019-0463-3
9. Eldakhakhny BM, Al Sadoun H, Choudhry H, Mobashir M. In-silico study of immune system associated genes in case of type-2 diabetes with insulin action and resistance, and/or obesity. Front Endocrinol. (2021) 12:641888. doi: 10.3389/fendo.2021.641888
10. Basit A, Fawwad A, Baqa K. Pakistan and diabetes—a country on the edge. Diabetes Res Clini Pract. (2019) 147:166–8. doi: 10.1016/j.diabres.2018.11.001
11. American Diabetes Association. 4. Lifestyle management: standards of medical care in diabetes-−2018. Diabetes Care. (2018) 41:S38–50. doi: 10.2337/dc18-S004
12. Powers MA, Bardsley JK, Cypress M, Funnell MM, Harms D, Hess-Fischl A, et al. Diabetes self-management education and support in adults with type 2 diabetes: a consensus report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care. (2020) 43:1636–49 doi: 10.2337/dci20-0023
13. Rutten GE. Person-centred type 2 diabetes care: time for a paradigm shift. Lancet Diabetes Endocrinol. (2018) 6:264–6. doi: 10.1016/S2213-8587(17)30193-6
14. Kalra S, Megallaa MH, Jawad F. Perspectives on patient-centered care in diabetology. J Midlife Health. (2012) 3:93. doi: 10.4103/0976-7800.104471
15. Al Mahrouqi AS, Mallinson RK, Oh KM, Weinstein AA. Patients' and nurses' perceptions of diabetes self-management in oman: a qualitative study. Int J Environ Res Public Health. (2022) 19:6929. doi: 10.3390/ijerph19116929
16. Delaney LJ. Patient-centred care as an approach to improving health care in Australia. Collegian. (2018) 25:119–23. doi: 10.1016/j.colegn.2017.02.005
17. Williams JS, Walker RJ, Smalls BL, Hill R, Egede LE. Patient-centered care, glycemic control, diabetes self-care, and quality of life in adults with type 2 diabetes. Diabetes Technol Ther. (2016) 18:644–9. doi: 10.1089/dia.2016.0079
18. Davies MJ, D'Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. (2018) 41:2669–701. doi: 10.2337/dci18-0033
19. Rutten GE, Van Vugt H, de Koning E. Person-centered diabetes care and patient activation in people with type 2 diabetes. BMJ Open Diabetes Res Care. (2020) 8:e001926. doi: 10.1136/bmjdrc-2020-001926
20. Ford RT. Teaching comprehensive treatment planning within a patient-centered care model. J Dent Educ. (1988) 52:114–7. doi: 10.1002/j.0022-0337.1988.52.2.tb02173.x
21. Davis K, Schoenbaum SC, Audet AM, A. 2020 vision of patient-centered primary care. J Gen Intern Med. (2005) 20:953–7. doi: 10.1111/j.1525-1497.2005.0178.x
22. Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, et al. 2017 National standards for diabetes self-management education and support. Diabetes Care. (2017). 40:1409–19. doi: 10.2337/dci17-0025
23. World Health Organization. Diabetes action now: an initiative of the World Health Organization and the International Diabetes Federation Organization. (2004).
24. Mehravar F, Mansournia MA, Holakouie-Naieni K, Nasli-Esfahani E, Mansournia N, Almasi-Hashiani A. Associations between diabetes self-management and microvascular complications in patients with type 2 diabetes. Epidemiol Health. (2016) 38. doi: 10.4178/epih.e2016004
25. Gary TL, Genkinger JM, Guallar E, Peyrot M, Brancati FL. Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educ. (2003) 29:488–501. doi: 10.1177/014572170302900313
26. Laine C, Davidoff F. Patient-centered medicine: a professional evolution. Jama. (1996) 275:152–6. doi: 10.1001/jama.1996.03530260066035
27. Kinmonth AL, Woodcock A, Griffin S, Spiegal N, Campbell MJ. Randomised controlled trial of patient centred care of diabetes in general practice: impact on current wellbeing and future disease risk. BMJ. (1998) 317:1202–8. doi: 10.1136/bmj.317.7167.1202
28. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. (2009) 62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006
29. Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. bmj. (2019) 28:366. doi: 10.1136/bmj.l4898
30. Sterne JAC, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. (2016) 355:i4919. doi: 10.1136/bmj.i4919
31. Cochrane Collaboration. Review manager (RevMan)[computer program]. Copenhagen Nord Cochrane Cent. (2014).
32. Baker KA, Weeks SM. An overview of systematic review. J Perianesth Nurs. (2014) 29:454–8. doi: 10.1016/j.jopan.2014.07.002
33. Williams GC, Lynch M, Glasgow RE. Computer-assisted intervention improves patient-centered diabetes care by increasing autonomy support. Health Psychology. (2007) 26:728. doi: 10.1037/0278-6133.26.6.728
34. Taylor KI, Oberle KM, Crutcher RA, Norton PG. Promoting health in type 2 diabetes: nurse-physician collaboration in primary care. Biol Res Nurs. (2005) 6:207–15. doi: 10.1177/1099800404272223
35. Scain SF, Friedman R, Gross JL, A. structured educational program improves metabolic control in patients with type 2 diabetes. Diabetes Educ. (2009) 35:603–11. doi: 10.1177/0145721709336299
36. Sacco WP, Malone JI, Morrison AD, Friedman A, Wells K. Effect of a brief, regular telephone intervention by paraprofessionals for type 2 diabetes. J Behav Med. (2009) 32:349–59. doi: 10.1007/s10865-009-9209-4
37. Carter EL, Nunlee-Bland G, Callender C. A patient-centric, provider-assisted diabetes telehealth self-management intervention for urban minorities. Perspectives in health information management/AHIMA, American health information management association. (2011) p. 8.
38. Forjuoh SN, Bolin JN, Huber Jr JC, Vuong AM, Adepoju OE, Helduser JW, et al. Behavioral and technological interventions targeting glycemic control in a racially/ethnically diverse population: a randomized controlled trial. BMC Public Health. (2014) 14:1–2. doi: 10.1186/1471-2458-14-71
39. Yuan C, Lai CW, Chan LW, Chow M, Law HK, Ying M. The effect of diabetes self-management education on body weight, glycemic control, and other metabolic markers in patients with type 2 diabetes mellitus. J Diabetes Res. (2014) 1:2014. doi: 10.1155/2014/789761
40. Pérez-Escamilla R, Damio G, Chhabra J, et al. Impact of a community health workers-led structured program on blood glucose control among Latinos with type 2 diabetes: the DIALBEST trial. Diabetes Care. (2015) 38:197–205. doi: 10.2337/dc14-0327
41. Ebrahimi H, Sadeghi M, Amanpour F, Vahedi H. Evaluation of empowerment model on indicators of metabolic control in patients with type 2 diabetes, a randomized clinical trial study. Primary Care Diabetes. (2016) 10:129–35. doi: 10.1016/j.pcd.2015.09.003
42. Jutterström L, Hörnsten Å, Sandström H, Stenlund H, Isaksson U. Nurse-led patient-centered self-management support improves HbA1c in patients with type 2 diabetes—a randomized study. Patient Educ Couns. (2016). 99:1821–9. doi: 10.1016/j.pec.2016.06.016
43. Windrum P, García-Goñi M, Coad H. The impact of patient-centered versus didactic education programs in chronic patients by severity: the case of type 2 diabetes mellitus. Value Health. (2016) 19:353–62. doi: 10.1016/j.jval.2016.01.014
44. Azami G, Soh KL, Sazlina SG, Salmiah M, Aazami S, Mozafari M, et al. Effect of a nurse-led diabetes self-management education program on glycosylated hemoglobin among adults with type 2 diabetes. J Diabetes Res. (2018) 8:2018. doi: 10.1155/2018/4930157
45. Abraham AM, Sudhir PM, Philip M, Bantwal G. Efficacy of a brief self-management intervention in type 2 diabetes mellitus: a randomized controlled trial from India. Indian J Psychol Med. (2020) 42:540–8. doi: 10.1177/0253717620932250
46. Cheng L, Sit JW, Choi KC, Chair SY, Li X, Wu Y, et al. Effectiveness of a patient-centred, empowerment-based intervention programme among patients with poorly controlled type 2 diabetes: a randomised controlled trial. Int J Nurs Studies. (2018) 79:43–51. doi: 10.1016/j.ijnurstu.2017.10.021
47. Zheng F, Liu S, Liu Y, Deng L. Effects of an outpatient diabetes self-management education on patients with type 2 diabetes in China: a randomized controlled trial. J Diabetes Res. (2019) 17:2019. doi: 10.1155/2019/1073131
48. Ing CT, Zhang G, Dillard A, Yoshimura SR, Hughes C, Palakiko DM. Social support groups in the maintenance of glycemic control after community-based intervention. J Diabetes Res. (2016) 2016:7913258. doi: 10.1155/2016/7913258
49. Varming AR, Rasmussen LB, Husted GR, Olesen K, Grønnegaard C, Willaing I. Improving empowerment, motivation, and medical adherence in patients with poorly controlled type 2 diabetes: a randomized controlled trial of a patient-centered intervention. Patient Educ Couns. (2019). 102:2238–45. doi: 10.1016/j.pec.2019.06.014
50. Spencer MS, Kieffer EC, Sinco B, Piatt G, Palmisano G, Hawkins J, et al. Outcomes at 18 months from a community health worker and peer leader diabetes self-management program for Latino adults. Diabetes Care. (2018). 41:1414–22. doi: 10.2337/dc17-0978
51. Al Omar M, Hasan S, Palaian S, Mahameed S. The impact of a self-management educational program coordinated through WhatsApp on diabetes control. Pharmacy Practice (Granada). (2020) 18. doi: 10.18549/PharmPract.2020.2.1841
52. Hailu FB, Moen A, Hjortdahl P. Diabetes self-management education (DSME)–Effect on knowledge, self-care behavior, and self-efficacy among type 2 diabetes patients in Ethiopia: a controlled clinical trial. Diabetes Metab Syndr Obes. (2019) 12:2489. doi: 10.2147/DMSO.S223123
53. Utz SW, Williams IC, Jones R, Hinton I, Alexander G, Yan G, et al. Culturally tailored intervention for rural African Americans with type 2 diabetes. Diabetes Educ. (2008) 34:854–65. doi: 10.1177/0145721708323642
54. Gavgani RM, Poursharifi H, Aliasgarzadeh A. Effectiveness of Information-Motivation and Behavioral skill (IMB) model in improving self-care behaviors & Hba1c measure in adults with type2 diabetes in Iran-Tabriz. Procedia Soc Behav Sci. (2010) 5:1868–73. doi: 10.1016/j.sbspro.2010.07.380
55. Fardaza FE, Heidari H, Solhi M. Effect of educational intervention based on locus of control structure of attribution theory on self-care behavior of patients with type II diabetes. Med J Islam Repub Iran. (2017) 31:116. doi: 10.14196/mjiri.31.116
56. Güner TA, Coşansu G. The effect of diabetes education and short message service reminders on metabolic control and disease management in patients with type 2 diabetes mellitus. Primary Care Diabetes. (2020) 14:482–7. doi: 10.1016/j.pcd.2020.04.007
57. Jeong S, Lee M, Ji E. Effect of pharmaceutical care interventions on glycemic control in patients with diabetes: a systematic review and meta-analysis. Ther Clin Risk Manag. (2018) 14:1813. doi: 10.2147/TCRM.S169748
58. Schünemann HJ. Using Systematic Reviews in Guideline Development: The GRADE Approach. Systematic Reviews in Health Research: Meta-Analysis in Context. Res Synth Methods. (2022) 22:424–48. doi: 10.1002/9781119099369.ch22
59. Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. (2000) 321:405–12. doi: 10.1136/bmj.321.7258.405
60. Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. (2002) 25:1159–71. doi: 10.2337/diacare.25.7.1159
61. De Greef K, Deforche B, Tudor-Locke C, De Bourdeaudhuij I. Increasing physical activity in Belgian type 2 diabetes patients: a three-arm randomized controlled trial. Int J Behav Med. (2011) 18:188–98. doi: 10.1007/s12529-010-9124-7
62. Kirk AF, Higgins LA, Hughes AR, Fisher BM, Mutrie N, Hillis S, et al. A randomized, controlled trial to study the effect of exercise consultation on the promotion of physical activity in people with Type 2 diabetes: a pilot study. Diabetic Medicine. (2001) 18:877–82. doi: 10.1046/j.0742-3071.2001.00570.x
Keywords: education and counseling, HbA1c, meta-analysis, type 2 diabetes, self-management, patient-centered care
Citation: Asmat K, Dhamani K, Gul R and Froelicher ES (2022) The effectiveness of patient-centered care vs. usual care in type 2 diabetes self-management: A systematic review and meta-analysis. Front. Public Health 10:994766. doi: 10.3389/fpubh.2022.994766
Received: 15 July 2022; Accepted: 03 October 2022;
Published: 28 October 2022.
Edited by:
Mohd Imtiaz Nawaz, King Saud University, Saudi ArabiaReviewed by:
Dubravka Jurišić ErŽen, University of Rijeka, CroatiaMohammad Mobashir, Karolinska Institutet (KI), Sweden
Copyright © 2022 Asmat, Dhamani, Gul and Froelicher. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kainat Asmat, a2FpbmF0YXdhbjI3QGdtYWlsLmNvbQ==
 Kainat Asmat
Kainat Asmat Khairunnisa Dhamani
Khairunnisa Dhamani Raisa Gul1
Raisa Gul1 Erika Sivarajan Froelicher
Erika Sivarajan Froelicher