- 1Department of Cardiology, The Second People’s Hospital of Chengdu, Chengdu, Sichuan, China
- 2Department of Neurology, The Second People’s Hospital of Chengdu, Chengdu, Sichuan, China
- 3Department of Endocrinology and Metabolism, Second People’s Hospital of Chengdu, Chengdu, Sichuan, China
- 4School of Health Policy and Management, Nanjing Medical University, Nanjing, Jiangsu, China
- 5Jiangsu Provincial Institute of Health, Nanjing Medical University, Nanjing, Jiangsu, China
- 6Center for Global Health, Nanjing Medical University, Nanjing, Jiangsu, China
- 7Department of Internal Medicine, Cardiovascular Center and Division of Cardiology, National Taiwan University Hospital, Taipei City, Taiwan, China
Objectives: This study aimed to investigate the prevalence and related factors of abdominal obesity among urban adults aged 35 to 79 years in southwest China.
Methods: From September 2013 to March 2014, a multi-stage sampling was conducted, and a total of 10,981 people aged 35–79 years living in Chengdu and Chongqing were included. More than 30 investigators were trained in data collection, including questionnaire, anthropometric measurements and blood biomarkers testing. Abdominal obesity was defined as waist circumference ≥ 90 cm for men and ≥ 85 cm for women.
Results: The prevalence of abdominal obesity was 30.7%, 24.8% in males and 33.9% in females (p < 0.001). The prevalence of abdominal obesity increased with BMI. The prevalence of abdominal obesity was positively correlated with age, sex, marriage, alcohol consumption, hypertension and diabetes, and negatively correlated with high education level, smoking and Physical activity.
Conclusion: The prevalence of abdominal obesity among adults aged 35–79 in urban communities in southwest China is high, which is close to that of adults in urban communities in China. We should strengthen health education among the population, adopt healthy diet, maintain moderate physical activity and other measures to curb the prevalence of abdominal obesity in urban communities in southwest China.
Introduction
Overweight and obesity are important risk factors for coronary heart disease, diabetes, stroke and chronic kidney disease (1–3). About 4 million deaths worldwide are directly attributed to high BMI, which accounts for 7.1 percent of all deaths (4). With the rapid development of China’s economy and society, the prevalence of overweight and obesity is rising (5, 6). In southwest China, 200 million people live in an area of more than 2.3 million square kilometers, accounting for one quarter of China’s land area (7). The implementation of China’s western development strategy since 2000 has led to significant economic and infrastructure growth in southwest China. At the same time, the prevalence of overweight and obesity is also increasing, which may change with economic development and lifestyle changes. Current obesity epidemic data are based on BMI analysis. While BMI is the most commonly used tool for measuring obesity, it mainly reflects body fat, not visceral fat (8–10). Previous research has shown that abdominal obesity is a key factor in cardiovascular disease risk (9, 10). In order to effectively control the obesity epidemic, it is necessary to understand the prevalence of abdominal obesity. However, large-scale epidemiological investigations of abdominal obesity have been lacking in the region. Therefore, from 2013 to 2014, we conducted an epidemiological investigation of abdominal obesity in Chengdu and Chongqing and analyzed the related factors, which provided a certain theoretical basis for the prevention and treatment of obesity and cardiovascular and cerebrovascular diseases in this region.
Methods
Study population
From September 2013 to March 2014, a cross-sectional survey was conducted among urban community population over 35 years old in Chengdu and Chongqing by means of multi-stage stratified sampling. The first step was to randomly sample Jinjiang District, Longquanyi District and Chenghua District as the urban areas of Chengdu, Yubei district and Jiangbei District as the urban areas of Chongqing. The second step was to randomly sample a subdistrict from each district. In the third step, a community was randomly sampled from each subdistrict, and a total of 5 communities were sampled. In each community according to the inclusion and exclusion criteria of this study, the survey team selected community residents with buildings as the basic unit, registered a total of 14,061 eligible participants, and finally 13,378 adults aged 35 to 79 were included in the survey. Due to the lack of demographic information and blood pressure, weight, lipid measurements, or waist circumference, and body mass index (BMI) data, 10,981 participants were included in the final analysis.
In 2004, Data from CCDRFS indicate that the prevalence of abdominal obesity among adults in China was 25.9%, to achieve a margin of error (ε) of 2%, so, according to the sample size calculate formula, which would require the sample size to reach 1844. Giving a 10% missing rate, it would require us to survey 2029 individuals for each community. Total 5 communities from Chengdu and Chongqing, so the sample size has least to reach 10,145.
This study has been reviewed by the Ethics Committee of Chengdu Second People’s Hospital (no 2013015). All respondents signed written informed consent forms.
Inclusion and exclusion criteria
Adults between the ages of 35 and 79 who had lived in selected communities for more than five years were included in the study from September 2013 to March 2014. People with malignancy, mental illness, secondary hypertension, kidney failure requiring dialysis, or refusal to participate were excluded.
Data collection
More than 30 medical staffs had been uniformly trained and qualified before taking up their works. The project team carried out field investigation with a unified questionnaire design. The questionnaire included general demographic information, lifestyle, personal and family history (family history of overweight and obesity), height, weight and other physical examinations. Measurement of height and weight requires participants to take off shoes, hat and trousers. Body mass index (BMI) = weight/height (2) (Kg/m2). Waist circumference (WC) was measured as the minimum circumference between the inferior margin of the ribcage and the iliac crest (11). The blood pressure was measured with an Omron arm electronic sphygmomanometer after 15 min rest. The blood pressure of the right upper arm was measured twice in the sitting position, and the mean value was taken. Blood sample collection and laboratory examination: after fasting for at least 12 h, fasting venous blood of patients from morning onwards and 75 g glucose 2 h postprandial venous blood were extracted, and blood glucose, lipid and uric acid were detected. Total cholesterol (TC), triglycerides (TG) and blood glucose were measured by oxidase method. The levels of high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C) were determined by homogeneous method. Serum uric acid was determined by phosphotungstic acid method on automatic biochemical analyzer. All anthropometric measurements and blood biomarkers testing were carried out in accordance with relevant guidelines and regulations.
Diagnostic standards
According to Health Industry Standards of the People’s Republic of China classifications (12), overweight is defined as a BMI between 24 kg/m2 and 28 kg/m2, while obesity is defined as a BMI greater than 28 kg/m2. Abdominal obesity was defined as waist circumference ≥ 90 cm for men and ≥ 85 cm for women (12). Smoking history was defined as having smoked at least once a day, smoked for more than a year, currently smoking or had quit for less than three years. A history of alcohol consumption was defined as drinking at least once a week, drinking for more than a year, and currently drinking or being sober for less than three years. Hypertension was defined as the self-reported history of hypertension or systolic blood pressure ≥ 140 mmHg and (or) diastolic blood pressure ≥ 90 mmHg (13). Diabetes was defined as the self-reported history of diabetes or fasting blood glucose ≥7.0 mmol/L and (or) OGTT 2-h post-load glucose ≥11.1 mmol/L (14). In our study, we analyzed physical intensity at work and leisure-time exercise. Referring to the Handbook of Cardiovascular Epidemiological Investigation Methods (15), we classify physical intensity at work as (1) very light: sitting (2) light: standing or walking back and forth, driving, housework (3) moderate: general indoor and outdoor activities, yard operation, carrying or lifting light objects, etc. (4) high: heavy industry or agriculture, outdoor construction, field construction, carrying or lifting heavy objects, strenuous sports activities, etc. We classified leisure-time exercise as yes or no, i.e., at least once a week. This definition is relatively simple and is a limitation of our study. In future studies, we will further subdivide the exercise situation based on the WHO definition by frequency and time.
Statistical analysis
Absolute number (percentage, %) was used to describe the categorical data, and a Chi-Square test was used to compare the difference between different groups. The quantitative data subject to or approximately subject to normal distribution were described by mean ± SD, and the differences between different groups were compared by T-test or analysis of variance. Chi-square trend test was used for the trend analysis of the rate. The multivariable analyses of obesity were conducted by using the non-conditional logistic regression model, and variable screening was conducted by using the forward stepwise selection method. The likelihood ratio (LR), and OR value and its 95% confidence interval were calculated. All statistical analyses were performed with SPSS 23.0 software, and p < 0.05 was statistically significant.
Results
Demographic and clinical characteristics of the study participants
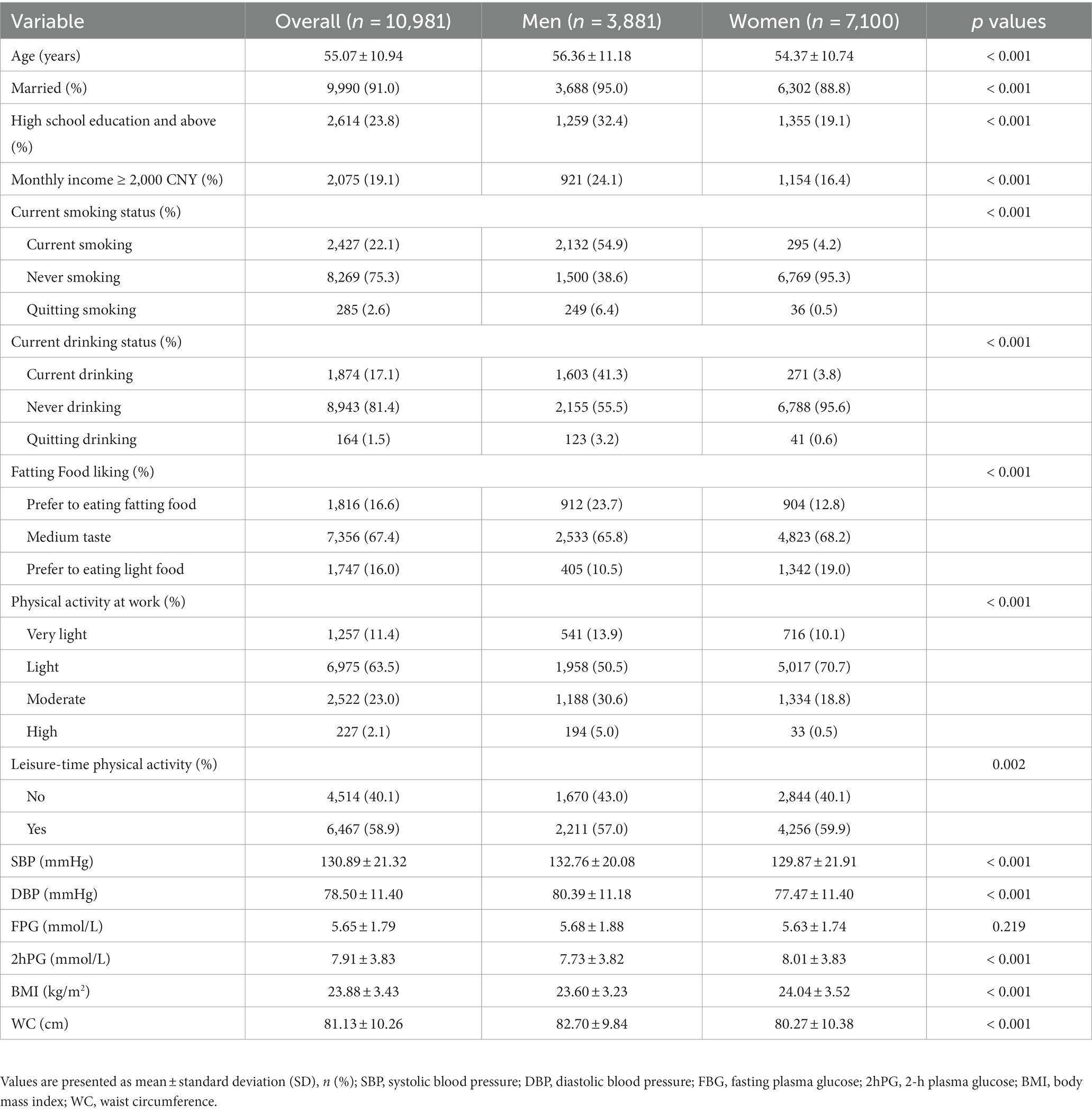
Among the 10,981 participants (Table 1), 3,881 were men and 7,100 were women. The mean age was 55.07 ± 10.94 years, and men had a higher average age. Men had higher prevalence of marriage, education level above high school degree, smoking, drinking, physical exercise intensity, systolic blood pressure, diastolic blood pressure, and WC (all p < 0.001). Women had higher BMI and 2hPG and were more likely to engage in leisure-time physical activity (p < 0.05). There was no significant difference in FPG.
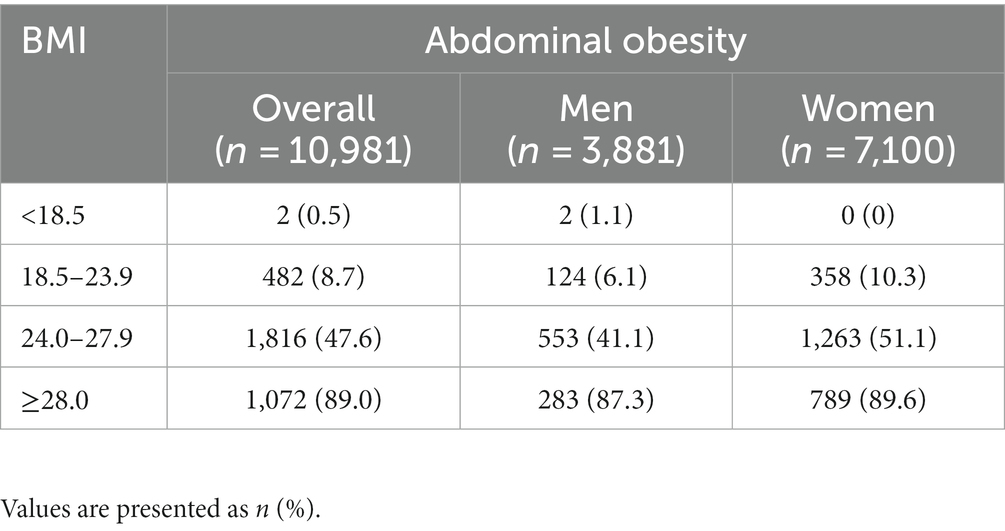
Relationship between BMI and abdominal obesity
The prevalence of abdominal obesity increased with BMI (Table 2). The prevalence of abdominal obesity in individuals with a normal BMI was 8.7%. Of note, 0.5% individuals with a BMI less than 18.5 were still abdominal obesity while 11% of those with a BMI greater than 28 were not.
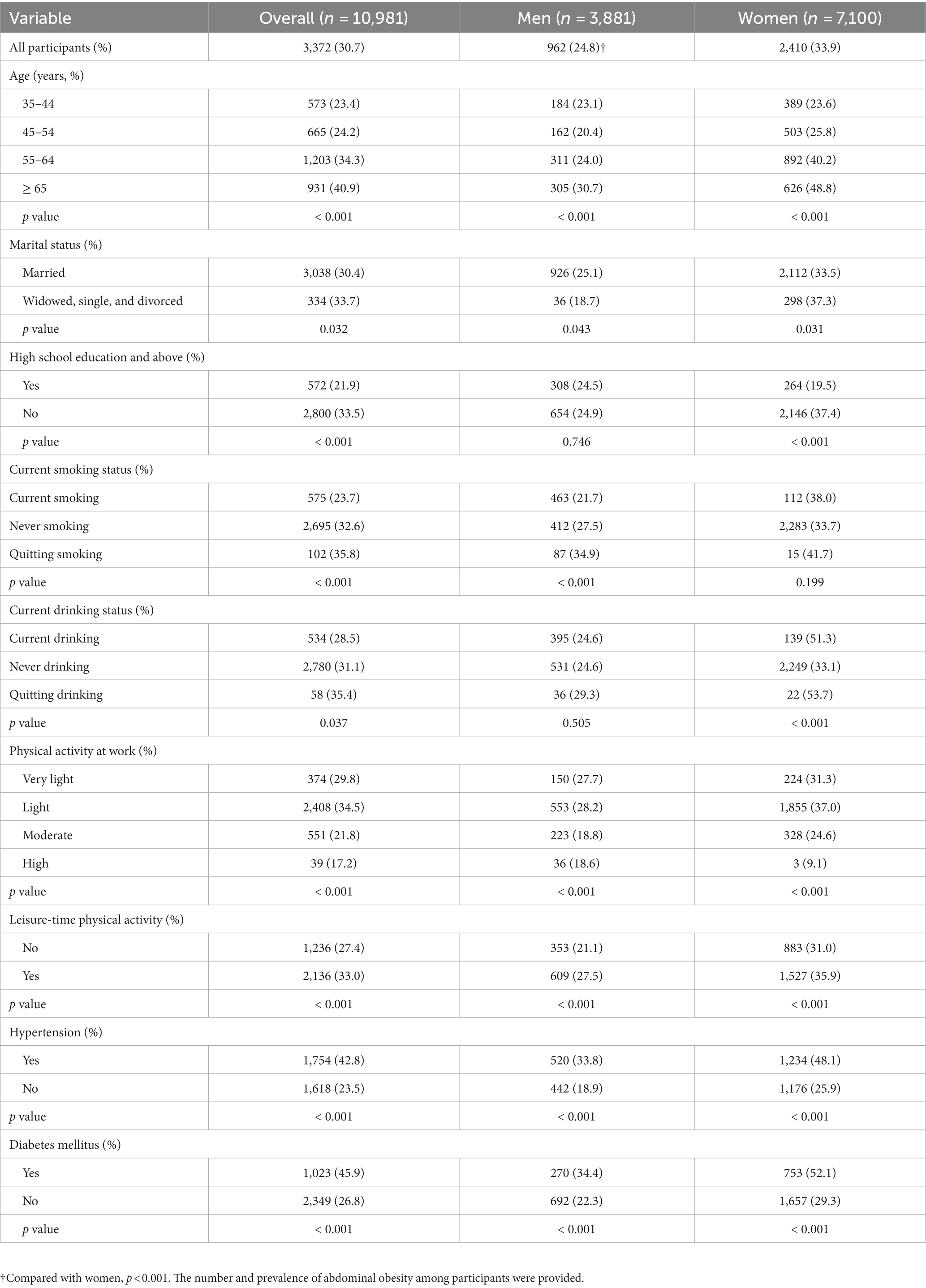
Prevalence of abdominal obesity
Table 3 shows the prevalence of abdominal obesity in different populations. The overall prevalence of abdominal obesity was 30.7%(3372/10981). The prevalence of abdominal obesity in women was higher than that in men (33.9% vs. 24.8%, p < 0.001). The overall prevalence of abdominal obesity increased with age, but the prevalence was lowest in men aged 45–54 years, while the prevalence was positively correlated with age in women. The overall prevalence of abdominal obesity in married people was lower than that in single, divorced or widowed people (p = 0.032). Whereas the prevalence was higher among married men (25.1% vs. 18.7%, p = 0.043) and lower among married women (33.5% vs. 37.3%, p = 0.031). The overall prevalence was lower among the highly educated, among women and no statistically significant difference among men. The prevalence of abdominal obesity was higher in people engaged in light physical labor and lower in people engaged in moderate to high intensity physical labor. The prevalence of abdominal obesity in hypertensive and diabetic patients was significantly increased.
Multivariable-adjusted ORs and 95% CI for abdominal obesity
Table 4 shows the results of multivariate logistic regression. Abdominal obesity was positively correlated with female, age, marriage, alcohol consumption, hypertension, and diabetes, but negatively correlated with high school education and above, smoking, moderate and high physical activity at work.
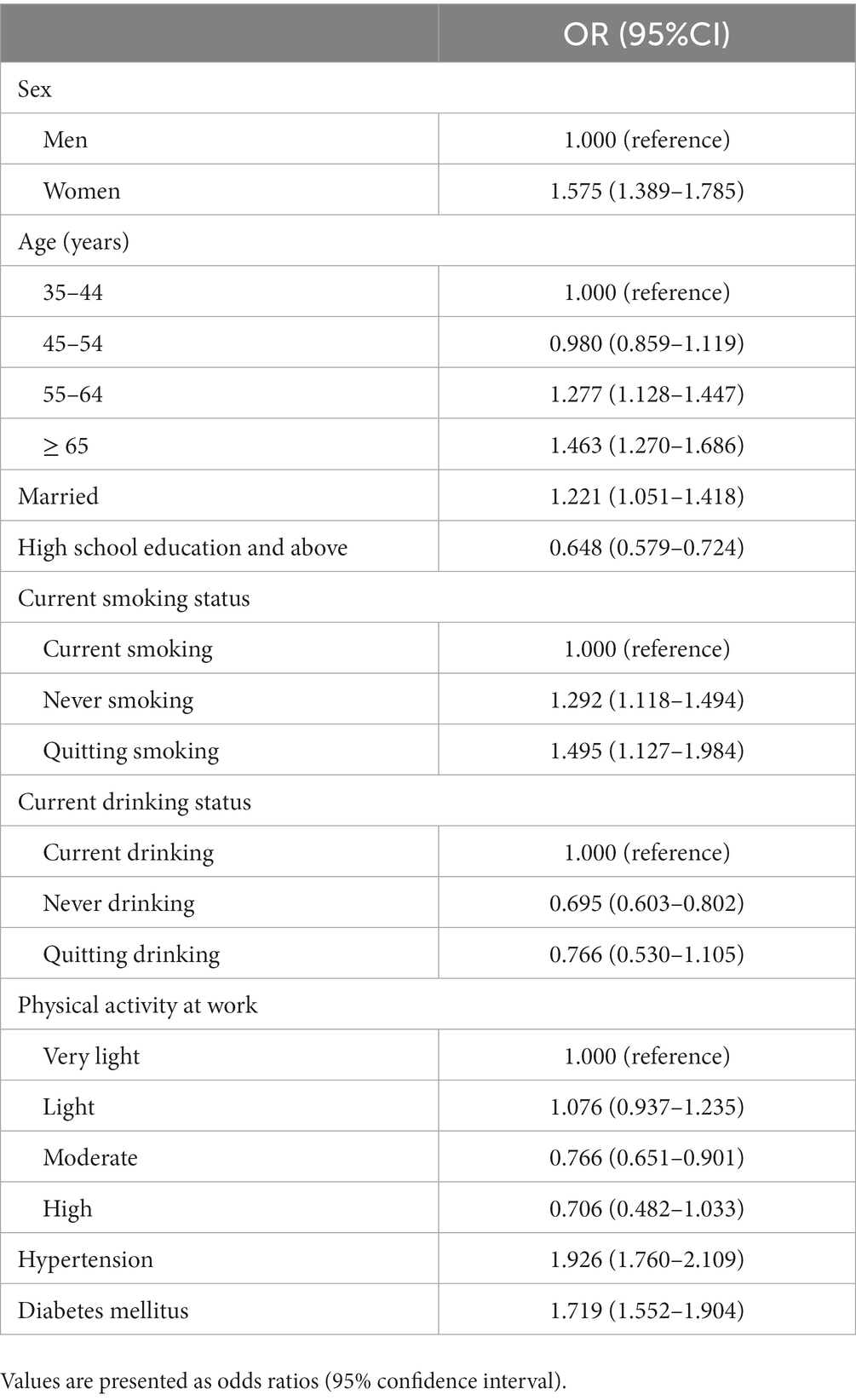
Table 4. Multivariable logistic regression analysis of abdominal obesity and the associated factors.
Discussion
This study assessed the prevalence and related factors of abdominal obesity in adults aged 35–79 years in Chengdu and Chongqing from September 2013 to March 2014. Overall, the prevalence of abdominal obesity was 30.7%. Previous data on the prevalence of abdominal obesity in the region was scant. A previous survey of 1,061 middle-aged and older adults in Chengdu suggested that the prevalence of abdominal obesity increased significantly (23.7% vs. 50%) 15 years ago from 1992 to 2007 (16). However, in this study, waist circumference ≥ 85 cm for men and waist circumference ≥ 80 cm for women were selected as the diagnostic criteria for abdominal obesity, so the prevalence was relatively high. It has to be mentioned that many years ago, the definition of abdominal obesity among middle-aged and older adults in urban communities in Chengdu adopted the 2004 Guidelines for the Prevention and Control of overweight and obesity among adults in China, while the definition of abdominal obesity in this study adopted the Health Industry Standards of the People’s Republic of China classifications in 2013. The comparison of prevalence calculated by different standards is not accurate. In another study, the prevalence of abdominal obesity in 4,551 Han people aged 20–80 years in Guizhou in 2012 was 26.8% (17). However, there is no separate data of urban community population for the prevalence of Han population in Guizhou. Our study to some extent filled the lack of data in this area, which is one of the important reasons for our research. Collectively, abdominal obesity is common among adults in southwest China, and with the rapid economic development of southwest China in recent years, overeating, lack of exercise and other unhealthy lifestyles, the prevalence of abdominal obesity has also increased significantly.
A national study of 441,306 participants aged 18 and older between October 2012 and December 2015 showed a prevalence of 29.1% (6). This study indicates that the prevalence of abdominal obesity in southwest China is close to the national level. Compared with other regions in China, abdominal obesity has obvious regional differences (18–20). Overall, the prevalence of abdominal obesity is higher in the North than in the South, which may be due to the cold climate in the North and the difference in eating habits between the north and the South (21, 22). The prevalence of abdominal obesity in Beijing and Guangzhou was higher than that in surrounding areas (6, 23), and the prevalence of abdominal obesity has increased with economic development in recent years, indicating that abdominal obesity may also be related to economic development.
This study further analyzed the factors associated with abdominal obesity, and the results showed that women, age, marriage, alcohol consumption, hypertension and diabetes were positively correlated with abdominal obesity, consistent with previous studies (6, 19, 20). However, the education level above high school, smoking, moderate and heavy physical labor were negatively correlated with abdominal obesity. The prevalence of abdominal obesity in females was higher than that in males (33.9% vs. 24.8%, p < 0.001), and this difference increases from the age group over 45 years. Possible explanation is that middle-aged and older women are less concerned with body image management than men, such as waist circumference, and changes in estrogen levels, particularly after menopause (24), also contribute to this difference. For the gender difference in the prevalence of abdominal obesity in different marital status, married men are more likely to be abdominal obesity, while this situation is opposite in women. The possible reason is that the diet status of unmarried men in most cases is often simple, that is, dietary intake is low. After marriage, men tend to eat more because their wives usually prepare rich meals for their families. In addition, after marriage, men’s work pressure and life pressure become greater, which affects the hormone levels of men, may lead to weight gain. For women, after marriage, in addition to working, they also need to complete housework, take care of children, and take care of their spouse, etc., and their physical activity increases significantly, which may lead to weight loss and a decrease in waist circumference. Several factors may contribute to obesity in married women but may be largely offset by increased physical activity. In this study, abdominal obesity was more common in people over 55 years of age, possibly due to decreased physical activity, decreased limb muscle mass, and changes in postmenopausal hormone levels (25). The older adults are at high risk of cardiovascular diseases. In addition to the prevention and treatment of hypertension and glycolipid abnormalities, the prevention and management of abdominal obesity are also very important. As a Chinese saying goes a thin body for an old man is beyond all money value. Drinking alcohol is quite common in China. While it has been widely recognized that alcohol consumption increases the risk of obesity, previous studies have reported inconsistent results on the relationship between alcohol consumption and obesity (26, 27). A study of abdominal obesity and drinking patterns in normal-weight middle-aged adults in South Korea found that in normal-weight middle-aged adults, the amount of alcohol consumed per drink affected abdominal obesity (28). The possible explanation is that high alcohol intake increases energy intake, leading to fat accumulation, and the endocrine changes caused by alcohol intake seem to be important (26). Alcohol alters steroid metabolism in the liver, leading to fat accumulation (29). Reducing alcohol consumption may help reduce the prevalence of abdominal obesity, thereby reducing cardiovascular disease, metabolic syndrome and other related diseases. In addition, our study showed that hypertension and diabetes were positively correlated with the prevalence of abdominal obesity. Previous studies have discussed the important impact of obesity on cardiovascular disease (30, 31). So we should actively control these underlying diseases that are associated with obesity. Interestingly, the prevalence of abdominal obesity was lower in people with higher levels of education, consistent with previous national studies (6). People with higher levels of education usually have more stable jobs and incomes and a higher standard of living. This could be due to greater health awareness, a better diet, as well as a more regular lifestyle and physical activity. In our study, current smokers were associated with a reduced prevalence of abdominal obesity, while former smokers were associated with an increased prevalence of abdominal obesity. The results are consistent with previous studies (6, 32), including a national study of a Chinese population (6). But the link between smoking and abdominal obesity remains controversial. Many previous studies (33–37) have observed an increased prevalence of abdominal obesity in people who smoke, such as adolescents (33, 34), women (35, 36), people with type 2 diabetes (37), heavy smokers (37), and former smokers (38). The possible mechanisms in the association between smoking and abdominal obesity are as follows. Some studies have suggested that nicotine causes insulin resistance (39, 40) and increases cortisol levels (41), factors that may be linked to belly fat accumulation. In addition, smokers are more likely to have unhealthy lifestyle habits, such as increased alcohol intake and lack of physical activity, which may contribute to abdominal obesity (42). Smokers gain weight after quitting, which may contribute to abdominal obesity in people who give up smoking (43, 44). Female smokers have a higher prevalence of abdominal obesity, and this sex difference may be explained by the anti-estrogen effects of nicotine (45). Results on the prevalence of abdominal obesity in current smokers are inconsistent (6, 32, 35–37). Smokers are more likely to have cardiovascular disease, diabetes, and metabolic syndrome (46, 47), although they may have a lower BMI than nonsmokers (48). So smoking is not recommended as a way to control weight.
The current situation of abdominal obesity in southwest China is not optimistic, which will further lead to diabetes and cardiovascular diseases, and thus could contribute to heavier medical burden. As is demonstrated in this study, more preventive measures should be taken to reduce the prevalence of abdominal obesity. For example, a healthy lifestyle, lower alcohol consumption, strict control of blood pressure and blood glucose, and active participation in physical exercise are of great significance for controlling abdominal obesity.
This study has several limitations. In this study, approximately 18% of participants were excluded due to the lack of important information, such as demographic information, anthropometry, and obesity measurements, which could lead to potential selection bias. This study selected five communities in Chengdu and Chongqing, the most developed cities in southwest China. However, these communities may not fully represent the urban areas in southwest China. This study is a cardiovascular metabolism study carried out in urban communities in southwest China. The original target population of this study is middle-aged and older adults, mainly including people over 40-years-old, but also some people between 35 and 40 years old. People aged 18–34 were not included. This is also a limitation of this study. Finally, other alternative measures of obesity such as waist-to-height ratio are of great significance. In future study, we expect to make a comprehensive comparison between these measures of obesity (e.g., waist circumference, waist-to-hip circumference, waist-to-height ratio) and yield a more accurate indicator for abdominal obesity.
Our study confirms the prevalence of abdominal obesity in southwest China is approximate to the national level. The prevalence of abdominal obesity was positively correlated with age, sex, marriage, alcohol consumption, hypertension and diabetes, and negatively correlated with high education level, smoking and Physical activity. The current situation of abdominal obesity in southwest China is not optimistic, our study provides evidence for the active prevention and control of abdominal obesity and the promotion of public health. Last but not least, this study collected socioeconomic and lifestyle variables such as monthly household income and eating habits of the research subjects in the last year, which were not reported in this study because the results were not significant. These variables have been reported with the results of previous studies on hypertension and diabetes (49–51). Otherwise, this study also has certain limitations, the cross-sectional nature of the survey cannot show a causal relationship between relevant influencing factors and the prevalence of abdominal obesity. In addition, the potential for recall bias or self-reporting errors in data collection may bring some bias to the study results.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Chengdu Second People's Hospital (no 2013015). The patients/participants provided their written informed consent to participate in this study.
Author contributions
CH and X-bH conceived and designed the study. CH, YZ, W-WT, J-XL, Y-MH, and YL analysed the data, drafted, and revised the manuscript. W-WT, T-DW, and X-bH advised on the interpretation of results and were responsible for the research. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by the Szechwan Province Science and Technology Agency Fund Project (2009FZ0027), Chengdu, China and Population and health project of Chengdu Municipal Science and Technology Bureau (10YTYB272SF-182), Chengdu, China. The Excellent Innovation Team of the Philosophy and Social Sciences in the Universities and Colleges of Jiangsu Province “The Public Health Policy and Management Innovation Research Team”.
Acknowledgments
We sincerely thank all the field staff and participants for their contributions, and the Excellent Innovation Team of the Philosophy and Social Sciences in the Universities and Colleges of Jiangsu Province “The Public Health Policy and Management Innovation Research Team” funded for this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Prospective Studies CollaborationWhitlock, G, Lewington, S, Sherliker, P, Clarke, R, Emberson, J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. (2009) 373:1083–96. doi: 10.1016/S0140-6736(09)60318-4
2. Berrington de Gonzalez, A, Hartge, P, Cerhan, JR, Flint, AJ, Hannan, L, MacInnis, RJ, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. (2010) 363:2211–9. doi: 10.1056/NEJMoa1000367
3. Haffner, SM. Relationship of metabolic risk factors and development of cardiovascular disease and diabetes. Obesity (Silver Spring). (2006) 14:121S–7S. doi: 10.1038/oby.2006.291
4. Reilly, JJ. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. (2017) 377:1496. doi: 10.1056/NEJMc1710026
5. Gu, D, Reynolds, K, Wu, X, Chen, J, Duan, X, Reynolds, RF, et al. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet. (2005) 365:1398–405. doi: 10.1016/S0140-6736(05)66375-1
6. Zhang, L, Wang, Z, Wang, X, Chen, Z, Shao, L, Tian, Y, et al. Prevalence of abdominal obesity in China: results from a cross-sectional study of nearly half a million participants. Obesity (Silver Spring). (2019) 27:1898–905. doi: 10.1002/oby.22620
7. Zhang, ZB, Yang, Y, Zhang, XP, and Chen, ZJ. Wind speed changes and its influencing factors in southwestern China. Acta Ecol Sin. (2014) 34:471–81. doi: 10.5846/stxb201305141051
8. Einstein, FH, Atzmon, G, Yang, XM, Ma, XH, Rincon, M, Rudin, E, et al. Differential responses of visceral and subcutaneous fat depots to nutrients. Diabetes. (2005) 54:672–8. doi: 10.2337/diabetes.54.3.672
9. Yusuf, S, Hawken, S, Ounpuu, S, Bautista, L, Franzosi, MG, Commerford, P, et al. INTERHEART study investigators. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. (2005) 366:1640–9. doi: 10.1016/S0140-6736(05)67663-5
10. Zhang, C, Rexrode, KM, van Dam, RM, Li, TY, and Hu, FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation. (2008) 117:1658–67. doi: 10.1161/CIRCULATIONAHA.107.739714
11. Zhang, S, Liu, X, Yu, Y, Hong, X, Christoffel, KK, Wang, B, et al. Genetic and environmental contributions to phenotypic components of metabolic syndrome: a population-based twin study. Obesity (Silver Spring). (2009) 17:1581–7. doi: 10.1038/oby.2009.125
12. National Health and Family Planning Commission of PRC. WS/T 428–2013. Health industry standards of the People’s republic of China: adult weight determination [in Chinese]. Beijing, China: China Standards Publishing House (2013)
13. Chinese hypertension prevention and treatment guidelines revision committee, hypertension Alliance (China), Chinese Society of Cardiovascular Diseases. Chinese hypertension prevention and treatment guidelines (2018 revised edition). Chinese J Cardiovasc. (2019) 24:24–56. doi: 10.3969/j.issn.1007-5410.2019.01.002
14. Chinese diabetes society. National Offic for primary diabetes care. [national guidelines for the prevention and control of diabetes in primary care (2018)]. Zhonghua Nei Ke Za Zhi. (2018) 57:885–93. doi: 10.3760/cma.j.issn.0578-1426.2018.12.003
15. Zhou, B, and WU, X. Handbook of cardiovascular epidemiological investigation methods. Beijing: Beijing Medical University and China Union Medical University Press (1997).
16. Wu, K, Chen, XP, Gong, L, Luo, XJ, Chen, XN, and Huang, DJ. Changes in the prevalence of obesity and abdominal obesity in middle-aged Chengdu residents during 1992 and 2007. Sichuan Da Xue Xue Bao Yi Xue Ban. (2011) 42:401–12. doi: 10.1007/s00216-011-5245-3
17. Wang, K, Wang, D, Pan, L, Yu, Y, Dong, F, Li, L, et al. Prevalence of obesity and related factors among Bouyei and Han peoples in Guizhou Province, Southwest China. PLoS One. (2015) 10:e0129230. doi: 10.1371/journal.pone.0129230
18. Song, N, Liu, F, Han, M, Zhao, Q, Zhao, Q, Zhai, H, et al. Prevalence of overweight and obesity and associated risk factors among adult residents of Northwest China: a cross-sectional study. BMJ Open. (2019) 9:e028131. doi: 10.1136/bmjopen-2018-028131
19. Liu, X, Wu, W, Mao, Z, Huo, W, Tu, R, Qian, X, et al. Prevalence and influencing factors of overweight and obesity in a Chinese rural population: the Henan rural cohort study. Sci Rep. (2018) 8:13101. doi: 10.1038/s41598-018-31336-2
20. Hu, L, Huang, X, You, C, Li, J, Hong, K, Li, P, et al. Prevalence of overweight, obesity, abdominal obesity and obesity-related risk factors in southern China. PLoS One. (2017) 12:e0183934. doi: 10.1371/journal.pone.0183934
21. Cardona, A, Pagani, L, Antao, T, Lawson, DJ, Eichstaedt, CA, Yngvadottir, B, et al. Genome-wide analysis of cold adaptation in indigenous Siberian populations. PLoS One. (2014) 9:e98076. doi: 10.1371/journal.pone.0098076
22. Fumagalli, M, Moltke, I, Grarup, N, Racimo, F, Bjerregaard, P, Jørgensen, ME, et al. Greenlandic Inuit show genetic signatures of diet and climate adaptation. Science. (2015) 349:1343–7. doi: 10.1126/science.aab2319
23. Ji, T, Zhang, L, Tang, Z, Sun, F, Li, Y, and Ma, L. Prevalence of Normal-weight obesity in community-dwelling Chinese older adults: results from the Beijing longitudinal study of aging. Diabetes Metab Syndr Obes. (2020) 13:1611–7. doi: 10.2147/DMSO.S246884
24. Sternfeld, B, Bhat, AK, Wang, H, Sharp, T, and Quesenberry, CP Jr. Menopause, physical activity, and body composition/fat distribution in midlife women. Med Sci Sports Exerc. (2005) 37:1195–202. doi: 10.1249/01.mss.0000170083.41186.b1
25. Visser, M, Pahor, M, Tylavsky, F, Kritchevsky, SB, Cauley, JA, Newman, AB, et al. One-and two-year change in body composition as measured by DXA in a population-based cohort of older men and women. J Appl Physiol. (1985) 94:2368–74. doi: 10.1152/japplphysiol.00124.2002
26. Schröder, H, Morales-Molina, JA, Bermejo, S, Barral, D, Mándoli, ES, Grau, M, et al. Relationship of abdominal obesity with alcohol consumption at population scale. Eur J Nutr. (2007) 46:369–76. doi: 10.1007/s00394-007-0674-7
27. Risérus, U, and Ingelsson, E. Alcohol intake, insulin resistance, and abdominal obesity in elderly men. Obesity (Silver Spring). (2007) 15:1766–73. doi: 10.1038/oby.2007.210
28. Park, KY, Park, HK, and Hwang, HS. Relationship between abdominal obesity and alcohol drinking pattern in normal-weight, middle-aged adults: the Korea National Health and nutrition examination survey 2008–2013. Public Health Nutr. (2017) 20:2192–200. doi: 10.1017/S1368980017001045
29. Bjorntorp, P. Endocrine abnormalities of obesity. Metabolism. (1995) 44:21–3. doi: 10.1016/0026-0495(95)90315-1
30. Global BMI Mortality CollaborationDi Angelantonio, E, Bhupathiraju, S, Wormser, D, Gao, P, Kaptoge, S, et al. Body-mass index and all-cause mortality: individual- participant-data meta-analysis of 239 prospective studies in four continents. Lancet. (2016) 388:776–86. doi: 10.1016/S0140-6736(16)30175-1
31. Fan, J, Song, Y, Chen, Y, Hui, R, and Zhang, W. Combined effect of obesity and cardiometabolic abnormality on the risk of cardiovascular disease: a meta-analysis of prospective cohort studies. Int J Cardiol. (2013) 168:4761–8. doi: 10.1016/j.ijcard.2013.07.230
32. Rezaei, S, Hajizadeh, M, Pasdar, Y, Hamzeh, B, Moradinazar, M, and Najafi, F. Association of Smoking with general and abdominal obesity: evidence from a cohort study in west of Iran. J Res Health Sci. (2017) 18:e00401
33. Bertoni, N, de Almeida, LM, Szklo, M, Figueiredo, VC, and Szklo, AS. Assessing the relationship between smoking and abdominal obesity in a National Survey of adolescents in Brazil. Prev Med. (2018) 111:1–5. doi: 10.1016/j.ypmed.2018.02.017
34. Saarni, SE, Pietiläinen, K, Kantonen, S, Rissanen, A, and Kaprio, J. Association of smoking in adolescence with abdominal obesity in adulthood: a follow-up study of 5 birth cohorts of Finnish twins. Am J Public Health. (2009) 99:348–54. doi: 10.2105/AJPH.2007.123851
35. Tuovinen, EL, Saarni, SE, Männistö, S, Borodulin, K, Patja, K, Kinnunen, TH, et al. Smoking status and abdominal obesity among normal and overweight/obese adults: population-based FINRISK study. Prev Med Rep. (2016) 4:324–30. doi: 10.1016/j.pmedr.2016.07.003
36. Clair, C, Chiolero, A, Faeh, D, Cornuz, J, Marques-Vidal, P, Paccaud, F, et al. Dose-dependent positive association between cigarette smoking, abdominal obesity and body fat: cross-sectional data from a population-based survey. BMC Public Health. (2011) 11:23. doi: 10.1186/1471-2458-11-23
37. Yun, JE, Kimm, H, Choi, YJ, Jee, SH, and Huh, KB. Smoking is associated with abdominal obesity, not overall obesity, in men with type 2 diabetes. J Prev Med Public Health. (2012) 45:316–22. doi: 10.3961/jpmph.2012.45.5.316
38. Fujiyoshi, A, Miura, K, Kadowaki, S, Azuma, K, Tanaka, S, Hisamatsu, T, et al. Lifetime cigarette smoking is associated with abdominal obesity in a community-based sample of Japanese men: the Shiga epidemiological study of subclinical atherosclerosis (SESSA). Prev Med Rep. (2016) 4:225–32. Published 2016 Jun 16. doi: 10.1016/j.pmedr.2016.06.013
39. Facchini, FS, Hollenbeck, CB, Jeppesen, J, Chen, YD, and Reaven, GM. Insulin resistance and cigarette smoking. Lancet. (1992) 339:1128–30. doi: 10.1016/0140-6736(92)90730-Q
40. Attvall, S, Fowelin, J, Lager, I, Von Schenck, H, and Smith, U. Smoking induces insulin resistance–a potential link with the insulin resistance syndrome. J Intern Med. (1993) 233:327–32. doi: 10.1111/j.1365-2796.1993.tb00680.x
41. Cryer, PE, Haymond, MW, Santiago, JV, and Shah, SD. Norepinephrine and epinephrine release and adrenergic mediation of smoking-associated hemodynamic and metabolic events. N Engl J Med. (1976) 295:573–7. doi: 10.1056/NEJM197609092951101
42. Chiolero, A, Wietlisbach, V, Ruffieux, C, Paccaud, F, and Cornuz, J. Clustering of risk behaviors with cigarette consumption: a population-based survey. Prev Med. (2006) 42:348–53. doi: 10.1016/j.ypmed.2006.01.011
43. Pisinger, C, and Jorgensen, T. Waist circumference and weight following smoking cessation in a general population: the Inter99 study. Prev Med. (2007) 44:290–5. doi: 10.1016/j.ypmed.2006.11.015
44. Tian, J, Venn, A, Otahal, P, and Gall, S. The association between quitting smoking and weight gain: a systemic review and meta-analysis of prospective cohort studies. Obes Rev. (2016) 17:1014. doi: 10.1111/obr.12448
45. Tanko, LB, and Christiansen, C. An update on the antiestrogenic effect of smoking: a literature review with implications for researchers and practitioners. Menopause. (2004) 11:104–9. doi: 10.1097/01.GME.0000079740.18541.DB
46. Manson, JE, Ajani, UA, Liu, S, Nathan, DM, and Hennekens, CH. A prospective study of cigarette smoking and the incidence of diabetes mellitus among US male physicians. Am J Med. (2000) 109:538–42. doi: 10.1016/S0002-9343(00)00568-4
47. Wannamethee, SG, Shaper, AG, and Perry, IJ, British Regional Heart Study. Smoking as a modifiable risk factor for type 2 diabetes in middle-aged men. Diabetes Care. (2001) 24:1590–5. doi: 10.2337/diacare.24.9.1590
48. Audrain-Mcgovern, J, and Benowitz, NL. Cigarette smoking, nicotine, and body weight. Clin Pharmacol Ther. (2011) 90:164–8. doi: 10.1038/clpt.2011.105
49. Cao, X, Yang, M, Huang, XB, Tan, XL, Liu, Y, Huo, N, et al. Prevalence and rates of new diagnosis and missed diagnosis of diabetes mellitus among 35-74-year-old residents in urban communities in Southwest China. Biomed Environ Sci. (2019) 9:704–09. doi: 10.3967/bes2019.089
50. Zhang, Y, Nie, FQ, Huang, XB, Tang, W, Hu, R, Zhang, WQ, et al. High prevalence and low awareness of hyperuricemia in hypertensive patients among adults aged 50-79 years in Southwest China. BMC Cardiovasc Disord. (2022) 22:2. doi: 10.1186/s12872-021-02427-2
Keywords: prevalence, related factor, abdominal obesity, urban adults, southwest China
Citation: Huang C, Zhang Y, Liu Y, Liu J-X, Hu Y-M, Tang W-W, Wang T-D and Huang X-b (2023) Prevalence and related factors of abdominal obesity among urban adults aged 35 to 79 years in southwest China. Front. Public Health. 11:1117897. doi: 10.3389/fpubh.2023.1117897
Edited by:
Karolina Skonieczna-Żydecka, Pomeranian Medical University, PolandReviewed by:
Shelly R. McFarlane, University of the West Indies, JamaicaBing Han, Shanghai Jiao Tong University, China
Copyright © 2023 Huang, Zhang, Liu, Liu, Hu, Tang, Wang and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei-Wei Tang, aG9tZXJ0YW5nQG5qbXUuZWR1LmNu; Tzung-Dau Wang, dGR3YW5nQG50dS5lZHUudHc=; Xiao-bo Huang, ZHJ4aWFvYm9odWFuZ0AxMjYuY29t
†These authors have contributed equally to this work
 Chuan Huang
Chuan Huang Ying Zhang2†
Ying Zhang2† Wei-Wei Tang
Wei-Wei Tang Tzung-Dau Wang
Tzung-Dau Wang