- 1Management Science and Engineering, Shandong University of Finance and Economics, Jinan, China
- 2School of Labor Relations, Shandong Management University, Jinan, China
- 3School of Information Engineering, Shandong Management University, Jinan, China
- 4Shandong Labor Vocational and Technical College, Jinan, China
- 5College of Traditional Chinese Medicine, Shandong University of Traditional Chinese Medicine, Jinan, China
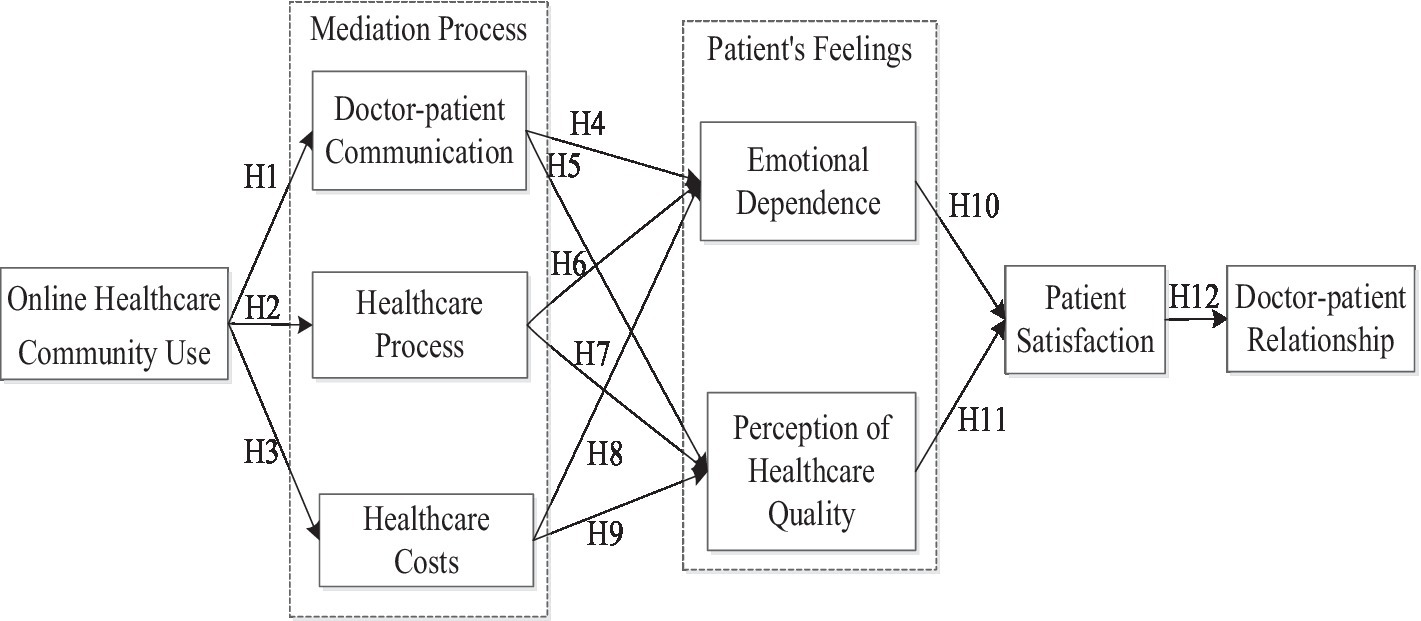
Possible improvements to the doctor-patient relationship are an important subject confronting national healthcare policy and health institutions. In recent years, online healthcare communities have changed the ways in which doctors and patients communicate, especially during the COVID-19 pandemic. However, previous research on how usage of online healthcare communities has affected the doctor-patient relationship is rather limited. This paper proposes a research model to investigate the relationship between online healthcare community usage and the doctor-patient relationship. An analysis of 313 patients’ data using structural equation modeling showed the following. First, the use of an online healthcare community has a positive impact on doctor-patient communication, helps improve the performance of healthcare procedures, and reduces healthcare costs. Second, doctor-patient communication and healthcare costs have a positive impact on patients’ emotional dependence and patients’ perception of healthcare quality, while healthcare procedures do not have this impact. Finally, patients’ emotional dependence and perception of healthcare quality have a positive effect on doctor-patient relationship through the mediator of patients’ satisfaction.
Introduction
The improvement of the doctor-patient relationship in the field of healthcare is an important issue that is currently troubling the country, including both doctors and patients (1). According to the 2020 National Big Data Report on Healthcare Damage Liability Dispute Cases, the total number of healthcare damage liability dispute cases in China was 18,670, up about 3 percent from 2019. At the same time, although China has carried out many healthcare reforms that have had some effect on the quality of healthcare services, the fundamentally tense relationship between doctor and patient remains largely unchanged. Patients complain that they do not receive proper services, and their interests can be harmed (2). For their part, doctors complain of the pressures put on them due to various social and economic aspects of providing healthcare (3). Therefore, means of improving the doctor-patient relationship in healthcare are urgently necessary.
Scholars have made attempts to improve the doctor-patient relationship, as seen in the literature. Studies have focused on patient satisfaction, trust, and communication between doctors (4, 5), the use of information systems, doctors’ caring attitude, interpersonal skills, treatment interpretation (1, 6), technical skills, hospital equipment, clinical ability, and others (5, 7). For example, Chenget al. (8) found that doctors’ caring attitude, interpersonal skills, treatment interpretation, technical skills, hospital equipment, and clinical competence had a significant positive impact on patient satisfaction and the improvement of doctor-patient relationship. Naidu (9) pointed out that patients’ perceptions, especially of doctors’ communication skills, were also important determinants of satisfaction and influenced the improvement of the doctor-patient relationship. Grunloh et al. (10) showed that patient loyalty is an important factor in patients’ willingness to repeatedly seek healthcare treatment. If healthcare and healthcare services can retain patients and make them loyal customers, it will improve the doctor-patient relationship and bring long-term commercial benefits to healthcare institutions.
Although previous studies have produced outstanding contributions to the doctor-patient relationship literature, few have explored how the use of online healthcare communities affects the doctor-patient relationship and how this effect comes about. In recent years, with the rapid development of the Internet, online healthcare communities have gained attention. These communities, which have patients or potential patients as their main service objects, provide health information, online consultations, healthcare consultations, and other services, providing channels for doctor-patient interactions through online community platforms (11). By examining the role that online healthcare communities play in the doctor-patient relationship, this study conducts a novel exploration of how the use of online healthcare communities by patients affects the doctor-patient relationship. Clarifying this issue is of great significance for understanding patients’ use level of online healthcare communities and to develop improvements in the service level of doctors in the online healthcare community.
In the course of this examination, this study constructs a theoretical model for the relationship between online healthcare community usage and the doctor-patient relationship. In this way, this study contributes to the doctor-patient relationship literature and by exploring the mediator role of doctor-patient communication, healthcare procedures, healthcare costs, emotional dependence, and perceptions of healthcare quality for online healthcare community usage and the doctor-patient relationship. Finally, this study provides practical insight for national healthcare and health institutions to improve the doctor-patient relationship.
Research hypotheses and model proposal
Online healthcare community usage and doctor-patient communication
Doctor-patient communication refers to the communication and exchange that patients and their families have with healthcare personnel in healthcare institutions and online healthcare communities regarding diagnosis and treatment, services, and health, psychological, and social factors (12). Wang et al. (11) found that doctor-patient communication includes six main sub-categories: emotional attitude, mode, adequacy, efficiency, content similarity, and communication service quality. The use of online healthcare communities has a positive impact on doctor-patient communication, as it can improve the degree of communication and patient satisfaction, as well as meeting patients’ expectations of consultation (11). Other studies have confirmed parts of these conclusions. For example, prior research finds that online doctor-patient communication can break through time–space limitations of traditional healthcare treatment situations and present new features and trends for doctor-patient communication practice (13). Patients can not only have private conversations with doctors anytime and anywhere to obtain healthcare services and health information with a higher degree of specialization and customization, but they can also have a stronger sense of control and participation in the process of doctor-patient communication with the empowerment of professional healthcare resources and healthcare information (14, 15). Therefore, online healthcare communities provide a platform for doctor-patient communication. When patients use an online healthcare community, the doctor-patient communication can be significantly improved. Based on this discussion, this paper proposes the following hypothesis:
H1: Use of an online healthcare community has a positive impact on doctor-patient communication.
Online health community use, healthcare process, and healthcare costs
The healthcare treatment process refers to the steps and main procedures that patients need to go through to obtain healthcare treatment, falling into two sub-categories: offline healthcare treatment process and online healthcare treatment process (16). The use of an online healthcare community has a positive impact on the healthcare treatment process because online healthcare community provides online registration, which is much more convenient for patients (17). Overall, the use of an online healthcare community can shorten the time required for patients to see a doctor and optimize the healthcare treatment process through online registration and appointment of examination items (18).
Healthcare costs are the comprehensive expenditures of economy, time, energy, and other resources in the process of seeking healthcare treatment, which includes two main sub-categories: providing free consultation services online and reducing the cost of healthcare treatment online (19). In traditional healthcare treatment, patients have higher healthcare costs, especially with respect to transportation, accommodation, registration, waiting for healthcare treatment, payment, and other costs of long-distance healthcare treatment. However, online healthcare communities can alleviate these problems to a certain extent and have greater selectivity than traditional healthcare patients. In particular, the use of an online healthcare community can reduce the time and monetary costs of healthcare treatment (20–22). From this discussion, this paper proposes the following hypotheses:
H2: Use of an online healthcare community has a positive impact on the healthcare process.
H3: Use of an online healthcare community has a negative impact on healthcare costs.
Doctor-patient communication, emotional dependence, and patients’ perception of healthcare quality
Online doctor-patient communication uses computer terminals or mobile devices as media, doctors and patients as interactive parties, and healthcare consultation or health exchange as communication purposes (12). This study examines online healthcare communities in which both doctors and patients participate. A survey has found that online doctor-patient communication often uses graphic consultation (14). Patients may generate emotional dependence and satisfaction while using online healthcare platform communication (2, 23). Emotional dependence refers to an outcome-based emotional evaluation generated by patients in their consumption of healthcare services, which reflects the emotional connections and bonds established among patients, doctors, and the platforms (24). Online healthcare platforms are a novel type of communication channel, allowing patients to feel that their doctor is a bit like themselves, similar to the concept of family doctor or private doctor in Europe and the United States. Online healthcare platforms allow patients to ask questions of their doctor and make it easier to form a relationship of trust and dependence between the patient and the doctor (5).
The doctor’s attitude is very important as well, especially if the doctor has a good attitude. The process of communicating with their doctor may bring psychological comfort to the patient; in such a case, the patient may feel that their condition is not as serious, which gives patients confidence. Doctor-patient communication based on online healthcare platforms have a positive impact on patients’ emotional dependence. Additionally, online healthcare platforms can improve the degree of communication, improve patients’ perception of healthcare quality, and meet patients’ expectations through consultation (8, 9). Taken together, these indicate that doctor-patient communication using an online healthcare platform can have a positive impact on patients’ perception of healthcare quality. From this discussion, the following hypotheses are proposed:
H4: Doctor-patient communication has a positive impact on patients' emotional dependence.
H5: Doctor-patient communication has a positive impact on patients' perception of healthcare quality.
Healthcare process, healthcare costs, emotional dependence, and patients’ perception of healthcare quality
The healthcare process involving an online healthcare community includes online appointments and offline treatments. The healthcare process involving an online healthcare community can save healthcare expenses and have an impact on patients’ emotional dependence and satisfaction. For example, online healthcare community can save patients’ time in making an appointment and save them time in queuing for offline treatment (15). Online healthcare communities can save treatment costs, facilitate patients, influence them, and improve their emotional dependence and perception of healthcare quality (25).
The use of an online healthcare community can reduce the cost of healthcare treatments for patients, which may impact on patients’ emotional dependence and satisfaction. For example: using an online healthcare community is convenient for patients, increasing their emotional dependence (26). In addition, the use of an online healthcare community improves patient experience by reducing patient costs, thus affecting patients’ perception of healthcare quality (27). From this discussion, this paper proposes the following hypotheses:
H6: Improvement of healthcare process has a positive impact on patients' emotional dependence.
H7: Improvement of healthcare process has a positive impact on patients' perception of quality of care.
H8: Improvement of healthcare costs have a positive impact on patients' emotional dependence.
H9: Improvement of healthcare costs have a positive impact on patients' perception of healthcare quality.
Patients’ emotional dependence, perceived healthcare quality, and doctor-patient satisfaction
Emotional dependence refers to outcome-based emotional evaluation that is generated by patients in their interaction with healthcare services and reflects the emotional connection and bond established between patients, doctors, and online healthcare platforms (28). The perception of healthcare quality refers to the quality and effects of healthcare services, largely, the timeliness, effectiveness, and safety of healthcare services (29). Patient satisfaction refers to patients’ satisfaction with the online healthcare community and the service level of their doctors (30). While using online healthcare communities, patients’ emotional dependence and perception of healthcare quality may affect their patient satisfaction (31). The use of an online healthcare community can increase the emotional dependence of patients, and when the patient generates emotional dependence on the doctor, indicating that the patient is satisfied with treatment by that doctor, patient satisfaction improves. On the other hand, as the patient perception of healthcare quality improves, the patient also has increased satisfaction because higher healthcare quality, which includes timeliness, effectiveness, and safety of healthcare services, generates greater patient satisfaction (32). This paper proposes the following hypotheses from this discussion:
H10: Patients' emotional dependence has a positive effect on patient satisfaction.
H11: Patients' perception of healthcare quality has a positive impact on patient satisfaction.
Patient satisfaction and the doctor-patient relationship
Patient satisfaction plays an important role in the relationship between healthcare service quality and the doctor-patient relationship. Studies have shown that when patients are satisfied, they perceive higher healthcare quality and an improved doctor-patient relationship (33). According to Wang et al. (11), in the online healthcare community, patients can find a doctor at any time, and many patients already trust their doctor, who, through online communications, can reply to the patients in a timely fashion, increasing trust even more, ultimately improving the entire doctor-patient relationship. Trust in doctors may be associated with increased trust throughout the entire site of health care, such as a hospital, such that doctors in the hospital and some healthcare services provided by the hospital also become more trusted (34). Thus, patients will trust the hospital more after the experience of using an online healthcare community. In conclusion, the online healthcare community can improve the trust and satisfaction of patients and then improve the doctor-patient relationship as well (1, 23). From this discussion, this paper proposes the following hypothesis:
H12: Patient satisfaction has a positive impact on the doctor-patient relationship.
Theoretical model proposed
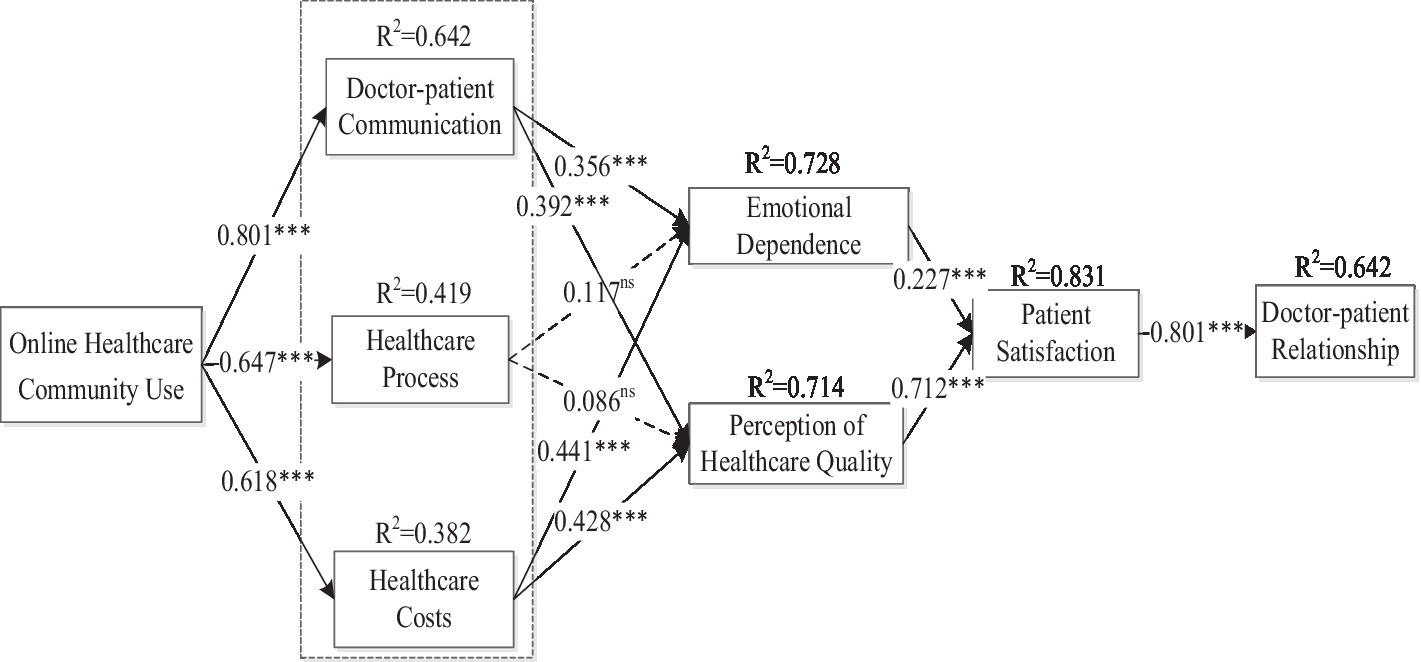
A theoretical model of the research is proposed as shown in Figure 1. The model explains how the use of an online healthcare community affects doctor-patient communication, healthcare treatment, and treatment cost, from this affecting patients’ emotional dependence and patients’ perceptions of healthcare quality, which ultimately has an impact on patient satisfaction and the doctor-patient relationship.
Research design
Measurement of variables
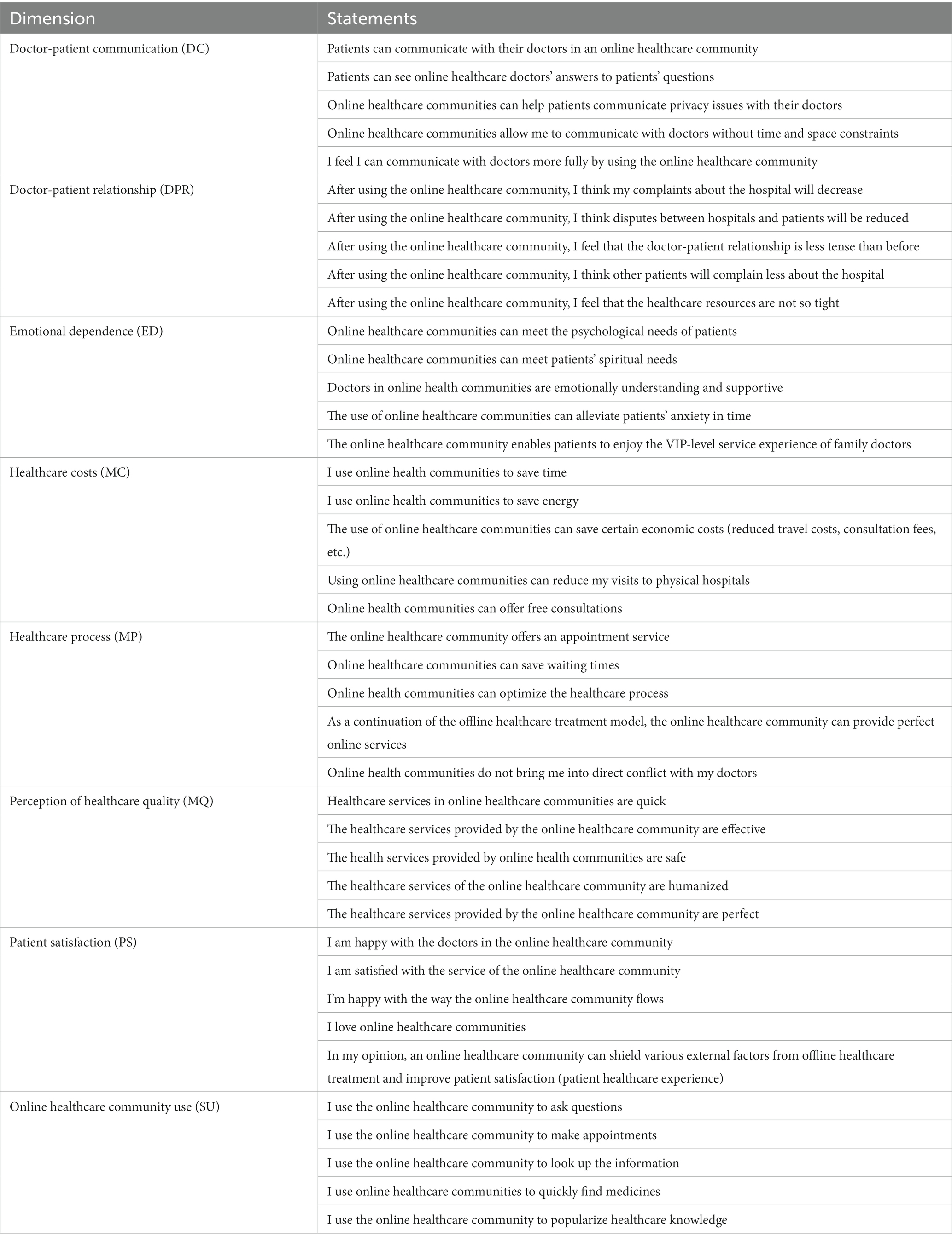
This paper collected data with a questionnaire survey. Question items and measures were drawn from earlier studies. Among these was doctor-patient communication, including five measure items, taken from Ha and Longnecker (13) and Wang et al. (11). The doctor-patient relationship was measured with included five measurement items revised from Zhang et al. (1). The scale of emotional dependence was adopted from Macia et al. (28) and Wang, Zhang, Han, and Ma (11). The measure of healthcare costs was adopted from Wang et al. (11). The measure for the healthcare process was revised from Jin et al. (35). The perception of healthcare quality was revised from Ramadan and Arafeh (36). Patient satisfaction measures were taken from Batbaatar et al. (37) and Chen et al. (23). Finally, online healthcare community use was revised from Goh et al. (38) and Liu et al. (39). The complete measurement items of the scale are shown in Table 1. The questionnaire was presented on a 7-point Likert scale ranging from 1(strongly disagree/very unlikely) to 7(strongly agree/very likely).
Data collection
After the completion of the questionnaire design, this paper invited three associate professors and five graduate students to fill in the questionnaire to ensure its readability. This paper also integrated study instrument piloted among the population. This paper used the snowball sampling method and we distribute questionnaires in the WeChat group to collect the sample data. Each participant was asked about any prior experience using an online healthcare community and filled out a questionnaire to collect their personal information and personal experiences in the use of the online healthcare community platform. The questionnaire begins with a brief description of the purpose of the survey, namely, to explore the use of online healthcare communities. Following this, interviewees were required to provide basic personal information, including gender, age, education level, monthly income, and health status. Finally, interviewees were required to share their experience in using an online healthcare community platform and online healthcare treatment based on their own experience. A total of 315 respondents completed the survey. Among these, 313 were valid, with an effective completion rate of 99.36%.
Data analysis tool
Smart PLS3.0 was used to analyze the data and test the hypotheses. A second-generation multivariate statistical analysis tool, PLS3.0 can evaluate both measurement models and structural models. A PLS model can use a smaller sample size than the structural equation model based on covariance, and PLS is not limited by the normal distribution, so it is more suitable for a study of this kind. Following a two-step analysis (40), the measurement model and the structural model were tested in this paper.
Data analysis and hypothesis testing
Descriptive statistical analysis
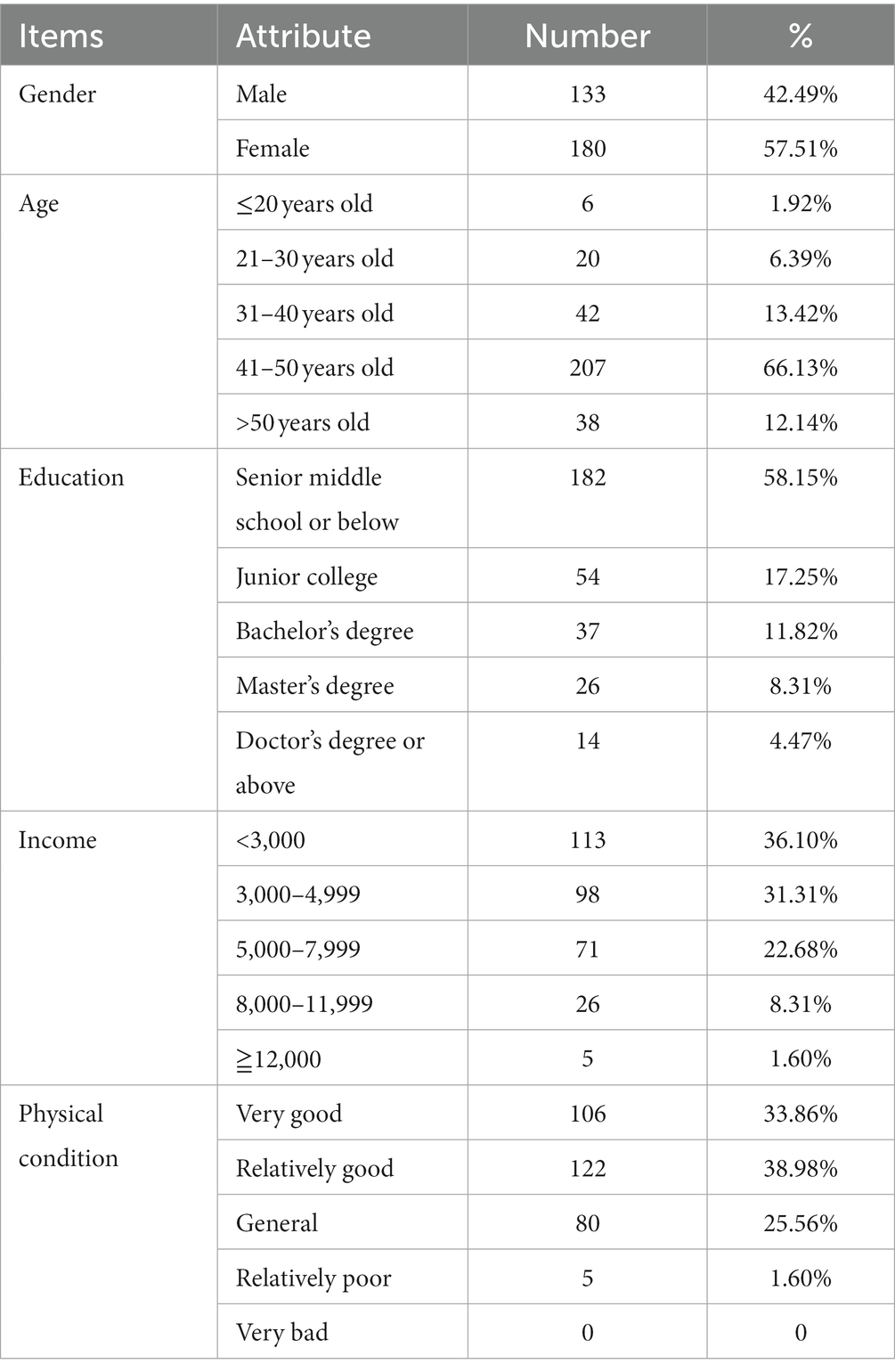
Table 2 lists the sample characteristics of the collected questionnaires. Most respondents were female, 57.51%. Most were between 41 and 50 years old, 66.13%. Most had a high school education or below, 58.15%. Most monthly incomes were less than 5,000 RMB, 67.41, and 36.10% were less than 3,000 RMB, and 31.31% were between 3,000 RMB and 4,999. Most were in good health, accounting for 38.98%.
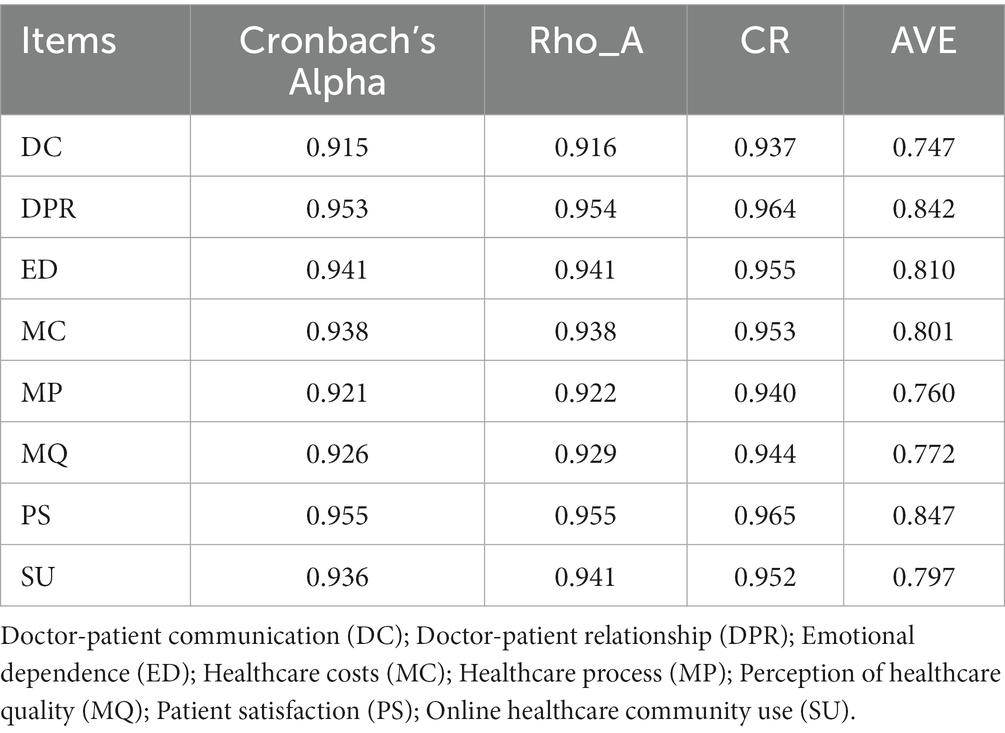
Model of measurement
Cronbach’s alpha coefficient and combined reliability were used in this study to test the consistency of the scale. From Table 3, we can see that the overall Cronbach’s alpha coefficient and combined reliability values were both above 0.7, indicating good internal consistency for each dimension of the scale.
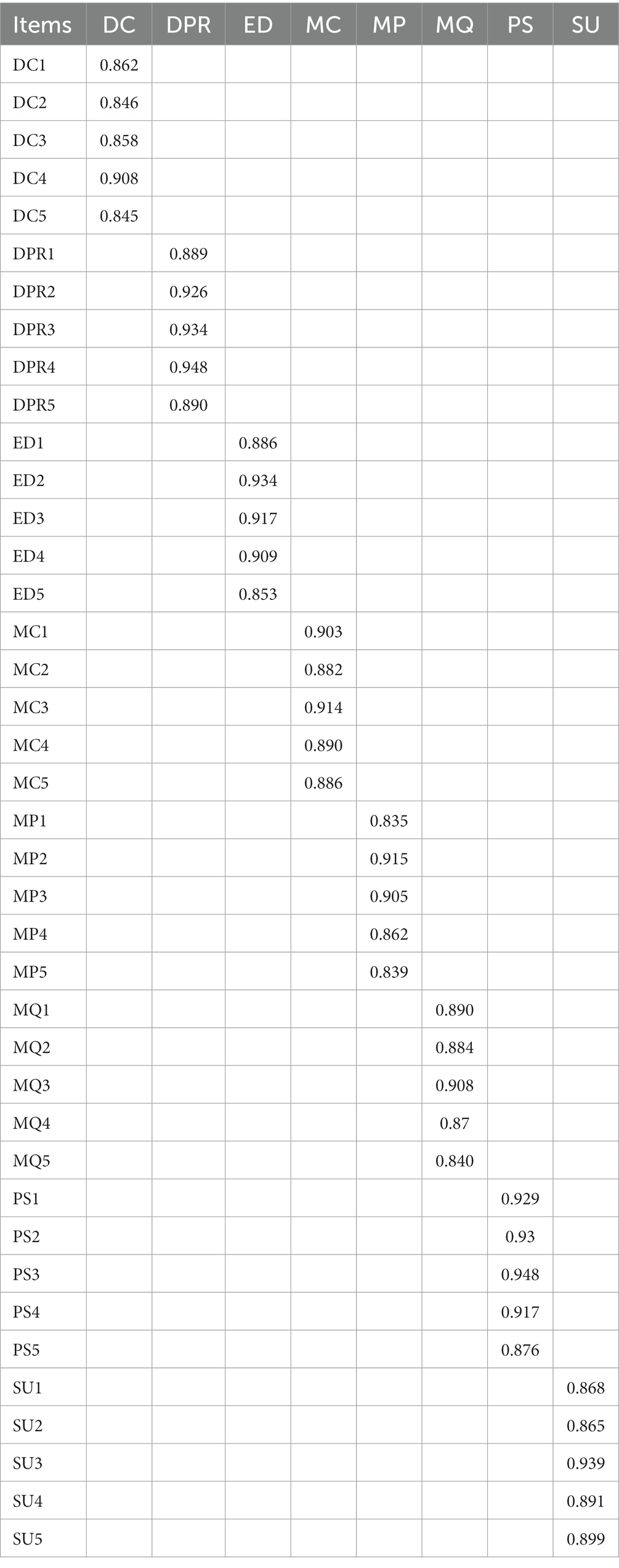
Hair et al. (41) suggested that the following indicators be used to test whether the measurement model has good convergent validity: (1) standardized factor load >0.7; (2) CR (composite reliability) > 0.7; AVE (average variance extracted) > 0.5. As can be seen in Table 4, the standardized factor load of all measurement items was greater than 0.7. Table 3 shows that the variation range of CR was from 0.937 to 0.965, and AVE ranged from 0.747 to 0.847, indicating that the measurement model in this study had high convergent validity.
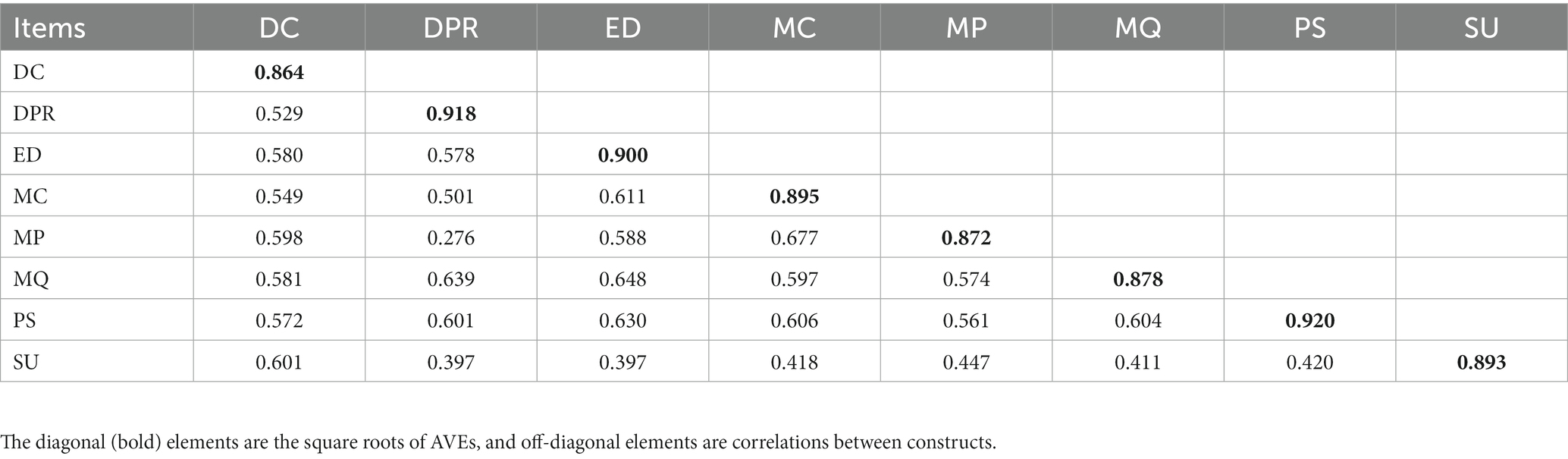
Discriminant validity analysis is used to verify whether there are statistically significant differences between different research dimensions. Theoretically, measurement items at different dimensions should not be highly correlated. If the correlation coefficient is higher than 0.85, the contents measured by these measurement items belong to the same dimension (42). Both Fornell-Larcker criterion and HTMT method were used to test the discriminant validity. The discriminant validity values of Fornell-Larcker criterion are shown in Table 5. The data present Pearson correlation coefficients between variables, where the diagonal line represents the square root value of AVE. When Pearson’s correlation coefficient between two variables is less than the square sum value of the two variables AVE, this indicates that the discriminant validity between two variables is acceptable. All dimensions in this study met these requirements, indicating that the discriminative validity of each dimension was acceptable. On the other hand, this paper also used the HTMT approach for discriminant validity, the HTMT value was 0.791, lower than the suggested value (0.85), indicating good discriminant validity.
Common method bias
Harman’s single-factor test was used to test the data for common method bias (43) and ensure the accuracy and objectivity of the analysis results. SPSS22.0 software was to conduct exploratory factor analysis for all other variables after the control variables were eliminated, and then the unrotated factor variance explanation rate was assessed through principal component analysis. The results showed that the total variance of the first principal component interpretation was 25.029%, which was far less than the critical value of 50% (44), indicating that no excess variance was present, and there was no common method bias.
Model of structure
Structural equation model results
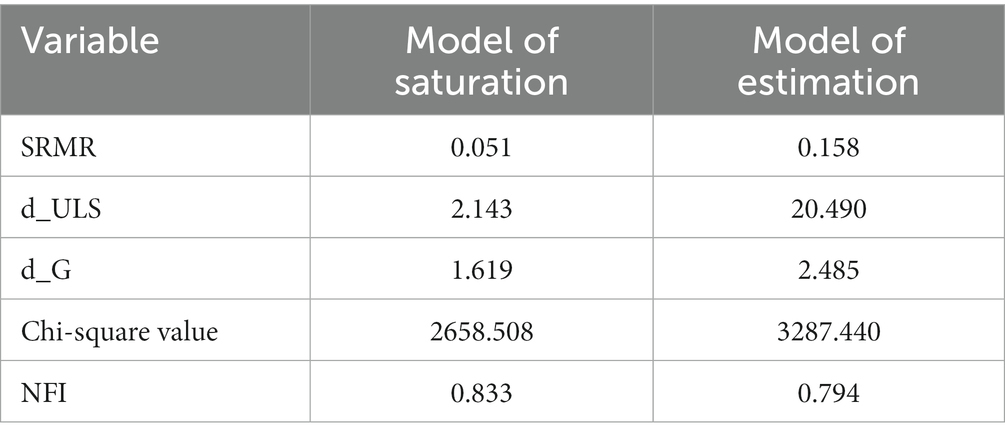
The degree of matching of the research model is shown in Table 6, and the model indicators all meet fitting criteria, indicating that the construction and fitting results of the model were ideal.
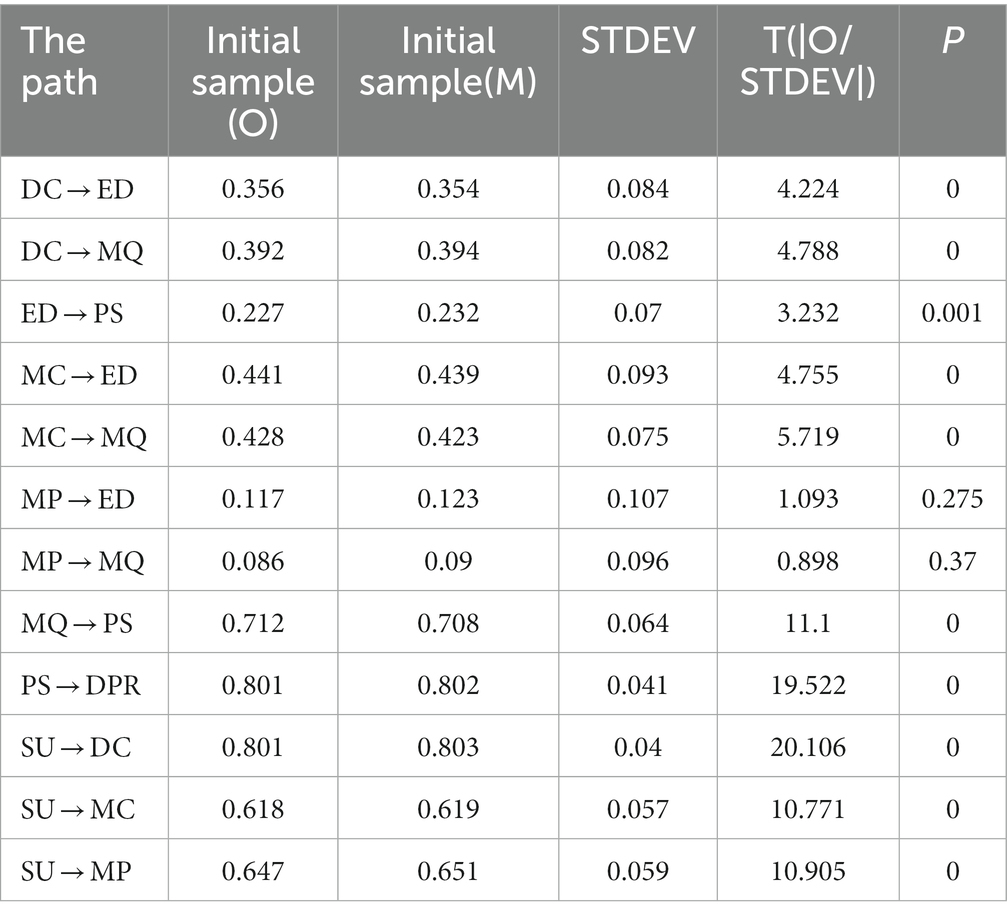
The structural equation model results for this study are shown in Figure 2. Online healthcare community had a positive impact on doctor-patient communication (β = 0.801, p < 0.001), healthcare treatment process (β = 0.647, p < 0.001), and healthcare treatment cost (β = 0.618, p < 0.001). Therefore, H1, H2, and H3 are considered to be supported. Second, doctor-patient communication had a positive impact on patients’ emotional dependence (β = 0.356, p < 0.001) and patients’ perception of healthcare quality (β = 0.392, p < 0.001). Therefore, H4 and H5 were supported. Healthcare procedures had no significant effects on patients’ emotional dependence (β = 0.119, p > 0.05) or patients’ perception of healthcare quality (β = 0.086, p > 0.05). Therefore, hypotheses H6 and H7 were not supported.
Healthcare costs had a positive impact on patients’ emotional dependence (β = 0.441, p < 0.001) and patients’ perception of healthcare quality (β = 0.428, p < 0.001). Therefore, H8 and H9 were supported. Finally, affective dependence had a positive effect on patient satisfaction (β = 0.227, p < 0.001), so H10 was supported. Patients’ perceptions of healthcare quality had a positive impact on patients’ satisfaction (β = 0.712, p < 0.001). Therefore, H11 was supported. Finally, patient satisfaction had a positive effect on the doctor-patient relationship (β = 0.801, p < 0.001). Therefore, H12 was supported (see Table 7).
Mediation effect
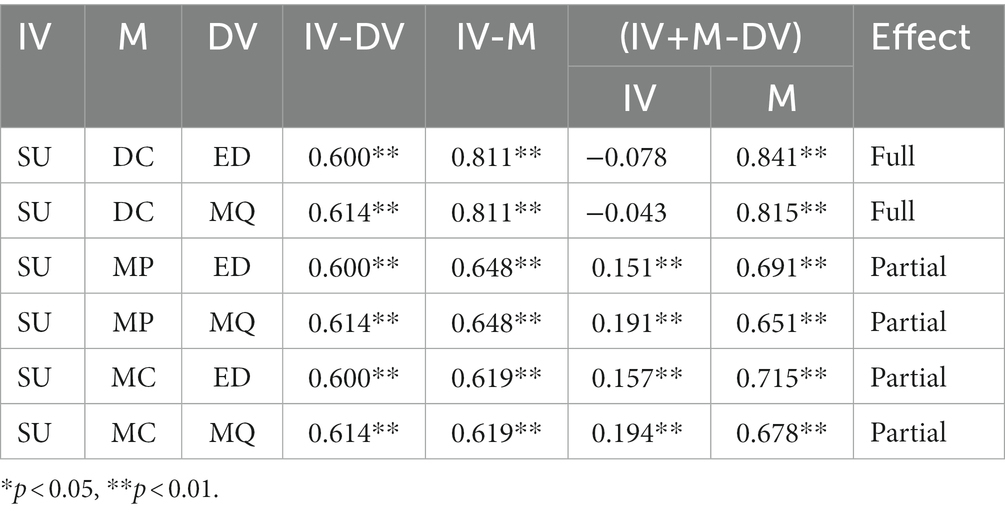
Mediating effects of doctor-patient communication, healthcare process, and healthcare cost
Bootstrapping was used to test for mediating effects (45), in particular for doctor-patient communication, healthcare process, and healthcare cost. As shown in Table 8, first, doctor-patient communication has a full mediating effect between the use of online healthcare community and emotional dependence. This indicates that the use of online healthcare communities completely mediated patients’ emotional dependence through doctor-patient communication. Doctor-patient communication had a fully mediating effect between the use of online healthcare community and patients’ perception of healthcare quality. This suggests that the use of online healthcare communities affects patients’ perception of healthcare quality completely through doctor-patient communication.
Second, the healthcare process has a partial mediating effect between the use of the online healthcare community and emotional dependence. On the one hand, the use of online healthcare community affects patients’ emotional dependence; On the other hand, it also affects patients’ emotional dependence by affecting the healthcare process. The healthcare process has a partially mediating effect between the use of online healthcare community and patients’ perception of healthcare quality. On the one hand, the use of online healthcare community affects patients’ perception of healthcare quality, but on the other, the use of online healthcare communities affects patients’ perceptions of healthcare quality by affecting the healthcare process.
Third, healthcare cost has a partial mediating effect between the use of online healthcare community and emotional dependence. On the one hand, the use of online healthcare community affects patients’ emotional dependence; on the other hand, it also affects patients’ emotional dependence by affecting healthcare costs. Healthcare costs have a partially mediating effect between the use of online healthcare community and patients’ perception of healthcare quality. On the one hand, the use of online healthcare community affects patients’ perception of healthcare quality, but on the other, the use of online healthcare communities affects patients’ perception of healthcare quality by affecting healthcare costs.
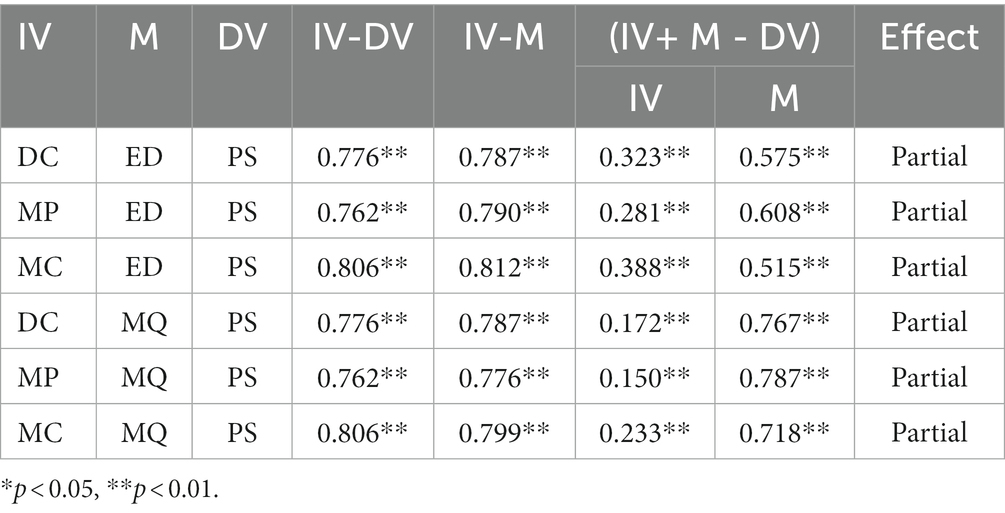
Mediating effects of emotional dependence and patients’ perception of healthcare quality
Bootstrapping was used to test the mediating effects of emotional dependence and patients’ perception of healthcare quality. As shown in Table 9, studies show that, first, emotional dependence has a partially mediating effect between doctor-patient communication and patient satisfaction. This indicates that on the one hand, doctor-patient communication affects patient satisfaction; on the other hand, doctor-patient communication affects patient satisfaction by influencing emotional dependence. Second, emotional dependence has a partially mediating effect between the healthcare process and patient satisfaction. This indicates that on the one hand, the healthcare process affects patient satisfaction; on the other hand, the healthcare process affects patient satisfaction by affecting emotional dependence. Third, emotional dependence has a partially mediating effect between healthcare cost and patient satisfaction. This indicates that on the one hand, healthcare costs affect patient satisfaction; on the other hand, healthcare cost affects patient satisfaction by influencing emotional dependence.
On the other hand, patients’ perception of healthcare quality has a partial mediating effect between doctor-patient communication and patient satisfaction. This indicates that, on the one hand, doctor-patient communication affects patient satisfaction; on the other hand, doctor-patient communication affects patient satisfaction by affecting the perception of healthcare quality. Second, the perception of healthcare quality has a partial mediating effect between the healthcare treatment process and patient satisfaction. This indicates that on the one hand, the healthcare process affects patient satisfaction; on the other hand, the healthcare process affects patient satisfaction by affecting the perception of healthcare quality. Third, the perception of healthcare quality has a partially mediating effect between healthcare cost and patient satisfaction. This indicates that on the one hand, healthcare cost affects patient satisfaction; on the other hand, healthcare cost affects patient satisfaction by affecting the perception of healthcare quality.
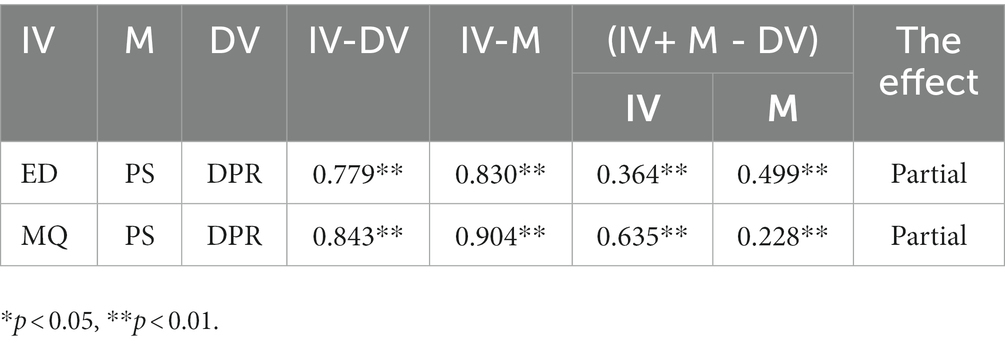
Mediating effect of patient satisfaction
Bootstrapping was also used to test the mediating effects of patient satisfaction (40). As can be seen from Table 10, first, patient satisfaction has a partially mediating effect between emotional dependence and the doctor-patient relationship. This indicates that emotional dependence affects the doctor-patient relationship; on the other hand, emotional dependence affects the doctor-patient relationship by affecting patient satisfaction. Second, patient satisfaction has a partially mediating effect between the perception of healthcare quality and doctor-patient relationship. On the one hand, the perception of healthcare quality affects the doctor-patient relationship; on the other hand, perceived healthcare quality affects the doctor-patient relationship by influencing patient satisfaction.
Conclusion
Key findings
The results of hypothesis testing are summarized in Table 11 below. The results show that the use of an online healthcare community has a positive impact on doctor-patient communication, improvement of healthcare procedures, and reduction of healthcare costs. In addition, doctor-patient communication has a positive impact on patients’ emotional dependence and patients’ perception of healthcare quality. However, no significant positive effect was seen on patients’ emotional dependence and perceived healthcare quality. The cost of healthcare treatment has a positive effect on patients’ emotional dependence and perception of healthcare quality. Patients’ emotional dependence has a positive effect on patients’ satisfaction. Patients’ perception of healthcare quality has a positive impact on patients’ satisfaction. Finally, patient satisfaction has a positive impact on the doctor-patient relationship.
This part discusses the process and mechanisms of the influence of online healthcare community on the doctor-patient relationship. The findings of this study, drawing on a large-sample survey in China, are as follows:
First, the use of online healthcare community has a positive impact on doctor-patient communication, healthcare process, and healthcare costs. Previous studies mainly focused on the influencing factors of patients’ healthcare choice behaviors in online healthcare communities (46), the influencing factors of user acceptance and use behavior in online health community, the influencing factors of user satisfaction in an online health community, doctor-patient participation in online healthcare community and influencing factors (15, 26). This study added the further findings that the use of online healthcare community can affect doctor-patient communication, healthcare process, and healthcare cost.
Second, the study found that doctor-patient communication had a positive impact on patients’ emotional dependence and perceptions of healthcare quality. This indicates that doctor-patient communication through an online healthcare community has a significant impact on improving patients’ emotional dependence and perception of healthcare quality. Previous studies largely focused on the impact of healthcare service quality, negative emotions (47), patient perceptions and other factors on the perception of healthcare quality (48). From existing studies, this study further found that the use of the online healthcare community would affect patients’ emotional dependence and perception of healthcare quality. Second, the effect of the healthcare process on patients’ emotional dependence and perception of healthcare quality was not significant. One of the possible reasons may be that emotional dependence and perception of healthcare quality mainly depend on the interaction between doctors and patients (3, 9), healthcare process mainly focused on the improvement of the medical process, such as reducing the cost of queuing time. Therefore, the healthcare process has no significant influence on them. Finally, the cost of healthcare has a positive impact on patients’ emotional dependence and perception of healthcare quality. This indicates that with the reduction of healthcare costs, patients’ emotional dependence and perception of healthcare quality will gradually improve.
Third, emotional dependence has a positive effect on patient satisfaction. This indicates that with the increase in patients’ emotional dependence, their perception of healthcare quality level will gradually improve, and their satisfaction will be significantly improved. Previous studies focused on social capital (49), network media communication (13, 33) and so on. This study additionally showed that emotional dependence has a positive impact on patient satisfaction. Second, patients’ perception of healthcare quality has a positive impact on patient satisfaction. This indicates that with the increase in patients’ perception of healthcare quality, their perception of healthcare quality is significantly improved, and their satisfaction is also significantly improved. Finally, studies have shown that patient satisfaction has a positive impact on the doctor-patient relationship. This indicates that with the improvement of patient satisfaction, the doctor-patient relationship can be improved.
Theoretical implications
First, this paper forms a contribution to the doctor-patient relationship literature by investigating the relationship between online healthcare community use and the doctor-patient relationship. Most prior research has focused on patients’ behavior, such as their willingness to engage in a community (18), their informational and emotional support (48), social support (50), their knowledge sharing (51) and information seeking (52), their information disclosure intention (53); physicians’ behavior, such as group joining behavior (54), and physicians’ teams’ performance (55); differences in demographic characteristics (56), and value co-creation behaviors in online health communities (47). However, few studies have focused on the relationship between online healthcare community use and the doctor-patient relationship. To fill this gap in the research, this paper investigates the relationship between the use of an online healthcare community and the doctor-patient relationship. The conclusions of this research enrich the understanding of the use of the online healthcare community and the relationship between doctors and patients.
Second, this paper contributes to the literature on the doctor-patient relationship by revealing the mediation process between online healthcare community use and the doctor-patient relationship. In the limited range of literature, Bernardi and Wu (46), drawing on 44 semi-structured interviews with members of an online health community for people with diabetes, find that patients exercise a great deal of agency in evaluating healthcare options not only by activating the logic of personal choice but also by appropriating the logic of medical professionalism. However, their study is limited in the types of results it can generate, as collects qualitative data, without relevant empirical tests, and does not reveal the intermediary process of the impact of the online healthcare community on the doctor-patient relationship. Unlike previous studies, this study found that online healthcare community usage affects the doctor-patient relationship by improving doctor-patient communication, improving healthcare procedures, and reducing healthcare costs, all of which further affect patients’ emotional dependence and patients’ perception of healthcare quality, finally affecting doctor-patient relationship through the mediator of patients’ satisfaction. This study clarifies the process mechanism of the impact of online healthcare community use on the doctor-patient relationship.
Practical implications
This paper has practical and guiding significance for doctors, patients, and administrators of the online healthcare community. First, this paper provides guidance and suggestions to enable doctors and patients to use online healthcare communities more actively and to platform operators to promote doctors and patients in this type of effective use. Drawing on online and offline aspects, this paper studies the influencing factors of patients’ use of online healthcare community, putting forward strategies to promote patients’ active use of online healthcare community and providing corresponding suggestions for doctors to make better use of online healthcare community to relieve shortages of offline healthcare resources and guide patients to use online healthcare communities. This paper also puts forward suggestions for the online healthcare community platform operators to improve the platform operation mechanism and attract more doctors and patients.
Second, doctors should strengthen doctor-patient communication, patiently listening to patients’ views on their own health, supporting and encouraging patients to participate in the healthcare decision-making process and adapting to the transformation of the healthcare service mode from a doctor-led mode to a patient-centered one. At the same time, clinicians should also pay attention to the evaluation of patients throughout the network, carry forward the advantages, improve the shortcomings, and establish an all-around personal brand, stimulating the participation of doctors. On the other hand, through an online healthcare community, patients can carry out health self-examination and real-time monitoring of their own health status, to reach healthcare services in good time. After seeing a doctor, patients can use the online platform to reflect on their own recovery, pose questions, and effectively carry out post-service activities. Thus, a smooth communication channel can be formed between doctors and patients, and the doctor-patient contradictions and disputes caused by information asymmetry can be effectively avoided, thus promoting the healthy development of the doctor-patient relationship.
Third, the Chinese government has proposed to promote the “Internet + healthcare” consultation model to meet growing healthcare and health needs in the country. Therefore, it will be necessary to analyze the factors influencing the use of the online healthcare community and the use effect of the platform, to support Chinese government organs, healthcare organizations at all levels, and operators of online healthcare community platforms to continually improve the specific implementation suggestions on the standardized use of “Internet + healthcare.” This study focuses on the use of online healthcare communities and emphasizes the importance of online healthcare communities in relieving the shortage of healthcare resources and improving the doctor-patient relationship. This will help Chinese governmental organizations, healthcare organizations at all levels, and online healthcare community platforms formulate detailed guidelines for promoting the use of online healthcare communities.
Finally, for government organizations, administrative departments should strengthen the supervision of healthcare and health websites in the system, and crack down on and rectify websites that spread false health information and malicious healthcare products. Relevant laws and regulations are constantly being supplemented and improved to ensure the scientific nature and accuracy of Internet healthcare and healthcare information, promoting the healthy and orderly development of online healthcare and online healthcare information services. On the other hand, industry organizations such as the Chinese Healthcare Association and Healthcare Doctor Association regularly have healthcare experts review and evaluate various online healthcare platforms, publishing these reviews to the public, to allow patients to correctly identify healthcare network information and identify high-quality Internet healthcare services. In addition, all healthcare units, especially public hospitals, should take the initiative to fulfill the social responsibility of popularizing healthcare knowledge and improving residents’ healthcare literacy, developing apps specifically for popularizing healthcare knowledge among patients, equipped with functions such as self-detection of health status, introducing common disease symptoms, conditions, diagnoses, and treatments, as well as guidance for rehabilitation programs. To help patients clarify their subjective cognition about the disease and reduce the large gap between the expected diagnosis and treatment effect and the actual diagnosis and treatment effect of patients, not only to promote the promotion and application of online healthcare community but also to help ease the tense doctor-patient relationship.
Limitations and directions for future research
Although the findings of this study are valid and valuable, they should be approached with caution for several reasons. First and most importantly, the sample may not represent the whole population of patients in China. Due to time and data constraints, 313 patients’ data were used for analysis. Future studies can test the generalizability of this study by collecting additional patient data. Second, online healthcare community use is a subjective factor across patients, which makes it inevitable that there will be some self-report bias in the measurement. In addition, respondents’ external environment, other interference, and respondents own emotions naturally had an impact on the quality of the questionnaire results. Therefore, future research can combine text mining, emotion analysis, and other methods to collect information related to patients’ healthcare search and consultation in an online healthcare community, to enrich research data sources, and analyze the impact of the use of online healthcare communities on the doctor-patient relationship through the combination of subjective and objective data. Finally, this article only explores the mechanism of its effect on the doctor-patient relationship from the perspective of the online healthcare community, although the doctor-patient relationship may also be affected by other external factors, such as relevant national healthcare and social security policies, laws and regulations, patient disease types, healthcare staff income, and treatments (20). Future research should fully consider the impact of external factors on the doctor-patient relationship to conduct a more scientific and thorough systematic analysis and in-depth assessment of the doctor-patient relationship.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XZ and YZ: conceptualization. ZW: writing—original draft. DH: investigation. FH: writing—review and editing. LM: model analysis. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Social Science Planning Project of Shandong Province (19CDNJ06 and 20CJJJ21), Development plan of the Youth Innovation Team in colleges and universities of Shandong Province (2021RW029), and Shandong Institute of Management 2021 Scientific Research Launch Plan Project (Project No. QH2021R15).
Acknowledgments
We would like to thank the editors and reviewers for their comments.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.Zhang, X, Ma, L, Ma, YB, and Yang, X. Mobile information systems usage and doctor-patient relationships: an empirical study in China. Mob Inf Syst. (2021) 2021:1–11. doi: 10.1155/2021/6684448
2.Hussain, A, Sial, MS, Usman, SM, Hwang, J, Jiang, YS, and Shafiq, A. What factors affect patient satisfaction in public sector hospitals: evidence from an emerging economy. Int J Environ Res Public Health. (2019) 16:994. doi: 10.3390/ijerph16060994
3.Molina-Mula, J, and Gallo-Estrada, J. Impact of nurse-patient relationship on quality of care and patient autonomy in decision-making. Int J Environ Res Public Health. (2020) 17:835. doi: 10.3390/ijerph17030835
4.Liang, CY, Gu, DX, Tao, FJ, Jain, HK, Zhao, Y, and Ding, B. Influence of mechanism of patient-accessible hospital information system implementation on doctor-patient relationships: a service fairness perspective. Inf Manag. (2017) 54:57–72. doi: 10.1016/j.im.2016.03.010 WOS:000392889100005
5.Peng, YX, Yin, PP, Deng, ZH, and Wang, RX. Patient-physician interaction and Trust in Online Health Community: the role of perceived usefulness of health information and services. Int J Environ Res Public Health. (2020) 17:139. doi: 10.3390/ijerph17010139 WOS:000509391500139
6.Hsu, YT, Duan, R, Chiu, YL, and Wang, JN. Understanding the inequality of web traffic and engagement in online healthcare communities. Front Public Health. (2022) 10:917522. doi: 10.3389/fpubh.2022.917522
7.Wu, H, Deng, ZH, Wang, B, and Wang, H. How online health community participation affects physicians' performance in hospitals: empirical evidence from China. Inf Manag. (2021) 58:103443. doi: 10.1016/j.im.2021.103443 WOS:000683463200007
8.Cheng, SH, Yang, MC, and Chiang, TL. Patient satisfaction with and recommendation of a hospital: effects of interpersonal and technical aspects of hospital care. Int J Qual Health Care. (2003) 15:345–55. doi: 10.1093/intqhc/mzg045
9.Naidu, A. Factors affecting patient satisfaction and healthcare quality. Int J Health Care Qual Assur. (2009) 22:366–81. doi: 10.1108/09526860910964834 WOS:000212476900019
10.Grunloh, C, Myreteg, G, Cajander, A, and Rexhepi, H. "why do they need to check me?" patient participation through eHealth and the doctor-patient relationship: qualitative study. J Med Internet Res. (2018) 20:e11. doi: 10.2196/jmir.8444.
11.Wang, ZY, Zhang, X, Han, DM, and Ma, L. Antecedents and consequences of online healthcare community usage: a grounded theory approach. Healthcare. (2022) 10:1749. doi: 10.3390/healthcare10091749
12.Wu, B. Patient continued use of online health care communities: web Mining of Patient-Doctor Communication. J Med Internet Res. (2018) 20:e126. doi: 10.2196/jmir.9127
13.Ha, JF, and Longnecker, N. Doctor-patient communication: a review. J Am Board Fam Med. (2022) 35:38–43.
14.Luo, AJ, Qin, L, Yuan, YF, Yang, ZZJ, Liu, F, Huang, PH, et al. The effect of online health information seeking on physician-patient relationships: systematic review. J Med Internet Res. (2022) 24:e23354. doi: 10.2196/23354
15.Mirzaei, T, and Esmaeilzadeh, P. Engagement in online health communities: channel expansion and social exchanges. Inf Manag. (2021) 58:103404. doi: 10.1016/j.im.2020.103404 WOS:000602792600008
16.Li, YF, Song, YY, Zhao, W, Guo, XT, Ju, XF, and Vogel, D. Exploring the role of online health community information in Patients' decisions to switch from online to offline medical services. Int J Med Inform. (2019) 130:103951. doi: 10.1016/j.ijmedinf.2019.08.011
17.Wu, H, and Lu, NJ. Online written consultation, telephone consultation and offline appointment: an examination of the channel effect in online health communities. Int J Med Inform. (2017) 107:107–s9. doi: 10.1016/j.ijmedinf.2017.08.009
18.Tseng, HT, Ibrahim, F, Hajli, N, Nisar, TM, and Shabbir, H. Effect of privacy concerns and engagement on social support behaviour in online health community platforms. Technol Forecast Soc Chang. (2022) 178:121592. doi: 10.1016/j.techfore.2022.121592 WOS:000778411300027
19.Nomura, Y, Ishii, Y, Chiba, Y, Suzuki, S, Suzuki, A, Suzuki, S, et al. Does last Year's cost predict the present cost? An application of machine leaning for the Japanese area-basis public health insurance database. Int J Environ Res Public Health. (2021) 18:565. doi: 10.3390/ijerph18020565
20.Wang, ZY, Zhang, X, and Ma, L. How to maintain a sustainable doctor-patient relationship in healthcare in China: a structural equation modeling approach. Journal of healthcare. Engineering. (2022) 2022:8251220. doi: 10.1155/2022/8251220
21.Guo, SS, Guo, XT, Zhang, XF, and Vogel, D. Doctor-patient relationship strength's impact in an online healthcare community. Inf Technol Dev. (2018) 24:279–s0. doi: 10.1080/02681102.2017.1283287 WOS:000428580400005
22.Zhou, YS, Zhu, L, Wu, CH, Huang, SJ, and Wang, Q. Do the rich grow richer? An empirical analysis of the Matthew effect in an online healthcare community. Electron Commer Res Appl. (2022) 52:101125. doi: 10.1016/j.elerap.2022.101125 WOS:000783884900005
23.Chen, SQ, Guo, XT, Wu, TS, and Ju, XF. Exploring the online doctor-patient interaction on patient satisfaction based on text mining and empirical analysis. Inf Process Manag. (2020) 57:102253. doi: 10.1016/j.ipm.2020.102253 WOS:000542996300006
24.Xiaofei, Z, Guo, XT, Ho, SY, Lai, KH, and Vogel, D. Effects of emotional attachment on mobile health-monitoring service usage: an affect transfer perspective. Inf Manag. (2021) 58:103312. doi: 10.1016/j.im.2020.103312 WOS:000620291500012
25.Liu, C, Li, HL, Zhang, SP, Cheng, L, and Zeng, QT. Cross-department collaborative healthcare process model discovery from event logs. IEEE Trans Autom Sci Eng. (2022):1–11. doi: 10.1109/tase.2022.3194312
26.Rhoden, PA, Bonilha, H, and Harvey, J. Patient satisfaction of telemedicine remote patient monitoring: a systematic review. Telemed E-Health. (2022) 28:1332–41. doi: 10.1089/tmj.2021.0434
27.Kamalasanan, A, Sathiyamurthi, G, and Subbarayalu, AV. A tool to assess the quality perception of healthcare employees. Int J Health Care Qual Assur. (2020) 33:291–307. doi: 10.1108/IJHCQA-01-2020-0008 WOS:000541529100001
28.Macia, P, Estevez, A, Iruarrizaga, I, Olave, L, Chavez, MD, and Momene, J. Mediating role of intimate partner violence between emotional dependence and addictive behaviours in adolescents. Front Psychol. (2022) 13:873247. doi: 10.3389/fpsyg.2022.873247
29.Carayon, P, Wetterneck, TB, Rivera-Rodriguez, AJ, Hundt, AS, Hoonakker, P, Holden, R, et al. Human factors systems approach to healthcare quality and patient safety. Appl Ergon. (2014) 45:14–25. doi: 10.1016/j.apergo.2013.04.023
30.Pettegrew, LS, Clements, ML, Scacco, JM, and Miller, R. Assessing patient satisfaction: using the radiation oncology patient satisfaction ROPS questionnaire in a private practice setting. Health Serv Insights. (2022) 15:117863292211182–11. doi: 10.1177/11786329221118241
31.Sun, SW, Zhang, J, Zhu, YW, Jiang, M, and Chen, SH. Exploring users' willingness to disclose personal information in online healthcare communities: the role of satisfaction. Technol Forecast Soc Chang. (2022) 178:121596. doi: 10.1016/j.techfore.2022.121596 WOS:000778411300030
32.Abdullah, MZ, Othman, AK, Hamzah, MI, Anuar, A, Tobi, SNM, and Solat, N. The influence of healthcare service quality on public university Students' satisfaction and behavioural intention: moderating role of trust. J Health Manag. (2022):097206342210768. doi: 10.1177/09720634221076886
33.Katsaliaki, K. Evaluating patient and medical staff satisfaction from doctor-patient communication. Int J Health Care Qual Assur. (2022) 35:38–55. doi: 10.1108/IJHCQA-03-2022-0033
34.Yang, JX, Luo, BA, and Tsai, FS. Continuance intention of online healthcare communities: the mediation mechanism of social interaction ties. J Organ End User Comput. (2022) 34:1–25. doi: 10.4018/JOEUC.302892 WOS:000861774300005
35.Jin, JH, Yan, XB, Li, YJ, and Li, YM. How users adopt healthcare information: an empirical study of an online Q&a community. Int J Med Inform. (2016) 86:91–3. doi: 10.1016/j.ijmedinf.2015.11.002
36.Ramadan, N, and Arafeh, M. Healthcare quality maturity assessment model based on quality drivers. Int J Health Care Qual Assur. (2016) 29:337–13. doi: 10.1108/IJHCQA-08-2015-0100
37.Batbaatar, E, Dorjdagva, J, Luvsannyam, A, Savino, MM, and Amenta, P. Determinants of patient satisfaction: a systematic review. Perspect Public Health. (2017) 137:89–1. doi: 10.1177/1757913916634136 WOS:000397472100011
38.Goh, JM, Gao, GD, and Agarwal, R. The creation of social value: can an online health community reduce rural-urban health disparities? MIS Q. (2016) 40:247–3. doi: 10.25300/MISQ/2016/40.1.11 WOS:000370447400011
39.Liu, S, Wang, H, Gao, BJ, and Deng, ZH. Doctors' provision of online health consultation service and patient review valence: evidence from a quasi-experiment. Inf Manag. (2022) 59:103360. doi: 10.1016/j.im.2020.103360 WOS:000814203000002
40.Ma, L, Zhang, X, Ding, XY, and Wang, GS. Bike sharing and users' subjective well-being: an empirical study in China. Transport Res Part Pract. (2018) 118:14–24. doi: 10.1016/j.tra.2018.08.040 WOS:000452941000002
41.Hair, JF, Black, WC, Babin, BJ, and Anderson, RE. Multivariate Data Analysis. 7th ed. New Jersey: Prentice Hall (2009).
42.Ma, L, Zhang, X, and Ding, XY. Social media users' share intention and subjective well-being: an empirical study based on WeChat. Online Inf Rev. (2018) 42:784–1. doi: 10.1108/OIR-02-2017-0058 WOS:000444477500004
43.Ma, L, Zhang, X, Ding, XY, and Wang, GS. Risk perception and intention to discontinue use of ride-hailing services in China: taking the example of DiDi Chuxing. Transport Res Part F Traffic Psychol Behav. (2019) 66:459–13. doi: 10.1016/j.trf.2019.09.021 WOS:000496865700034
44.Ma, L, Zhang, X, Wang, GS, and Zhang, G. How to build employees' relationship capital through different enterprise social media platform use: the moderating role of innovation culture. Internet Res. (2021) 31:1823–48. doi: 10.1108/INTR-01-2020-0022 WOS:000646302000001
45.Ma, L, Zhang, X, and Ding, XY. Enterprise social media usage and knowledge hiding: a motivation theory perspective. J Knowl Manag. (2020) 24:2149–69. doi: 10.1108/JKM-03-2020-0234 WOS:000574696000001
46.Bernardi, R, and Wu, PF. Online health communities and the patient-doctor relationship: an institutional logics perspective. Soc Sci Med. (2022) 314:115494. doi: 10.1016/j.socscimed.2022.115494
47.Liu, S, Xiao, WY, Fang, C, Zhang, X, and Lin, JB. Social support, belongingness, and value co-creation behaviors in online health communities. Telematics Inform. (2020) 50:101398. doi: 10.1016/j.tele.2020.101398 WOS:000525320000009
48.Chen, LT, Baird, A, and Straub, D. A linguistic signaling model of social support exchange in online health communities. Decis Support Syst. (2020) 130:113233. doi: 10.1016/j.dss.2019.113233 WOS:000515215800009
49.Guo, SS, Guo, XT, Fang, YL, and Vogel, D. How doctors gain social and economic returns in online health-care communities: a professional capital perspective. J Manag Inf Syst. (2017) 34:487–9. doi: 10.1080/07421222.2017.1334480 WOS:000407928400009
50.James, TL, Villacis Calderon, ED, Bélanger, F, and Lowry, PB. The mediating role of group dynamics in shaping received social support from active and passive use in online health communities. Inf Manag. (2022) 59:103606. doi: 10.1016/j.im.2022.103606
51.Meng, FB, Zhang, XF, Liu, LB, and Ren, CC. Converting readers to patients? From free to paid knowledge-sharing in online health communities. Inf Process Manag. (2021) 58:102490. doi: 10.1016/j.ipm.2021.102490 WOS:000633035800012
52.Ma, D, Zuo, M, and Liu, L. The information needs of Chinese family members of cancer patients in the online health community: what and why? Inf Process Manag. (2021) 58:102517. doi: 10.1016/j.ipm.2021.102517
53.Zhang, X, Liu, S, Chen, X, Wang, L, Gao, BJ, and Zhu, Q. Health information privacy concerns, antecedents, and information disclosure intention in online health communities. Inf Manag. (2018) 55:482–3. doi: 10.1016/j.im.2017.11.003 WOS:000431748100008
54.Qiao, WX, Yan, ZJ, and Wang, XH. Join or not: the impact of physicians' group joining behavior on their online demand and reputation in online health communities. Inf Process Manag. (2021) 58:102634. doi: 10.1016/j.ipm.2021.102634 WOS:000681134700001
55.Yang, H, Yan, Z, Jia, L, and Liang, HG. The impact of team diversity on physician teams' performance in online health communities. Inf Process Manag. (2021) 58:102421. doi: 10.1016/j.ipm.2020.102421 WOS:000598920600013
Keywords: online healthcare community, doctor–patient relationship, patients’ satisfaction, patients communicate, healthcare costs
Citation: Wang Z, Zhang X, Han D, Zhao Y, Ma L and Hao F (2023) How the use of an online healthcare community affects the doctor-patient relationship: An empirical study in China. Front. Public Health. 11:1145749. doi: 10.3389/fpubh.2023.1145749
Edited by:
Shixuan Fu, University of Science and Technology Beijing, ChinaCopyright © 2023 Wang, Zhang, Han, Zhao, Ma and Hao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feifei Hao, YWlmZWlmZWkwMjEwQDEyNi5jb20=
 Zhanyou Wang1,2
Zhanyou Wang1,2 Liang Ma
Liang Ma Feifei Hao
Feifei Hao