- 1Department of Health Management, School of Health Management, Southern Medical University, Guangzhou, Guangdong, China
- 2Department of Health Policy and Management, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, United States
Objective: The aim of this study was to analyze the effectiveness of prevention and control strategies and put forward further measures according to the epidemiological characteristics of Omicron. It summarized the national response during the Omicron epidemic in four countries: China, Israel, South Africa, and the United States.
Methods: This study summarized prevention and control measures in China, Israel, South Africa, and the United States in their response to the Omicron epidemic, and it also evaluated the effectiveness of these measures.
Results: After the Omicron variant emerged, China and Israel adopted containment strategies, using the “dynamic zero” policy and country closure measures. Meanwhile, South Africa and the United States adopted mitigation strategies, which virtually abandoned social interventions and only focused on medical measures and vaccines. From the first day of reported Omicron cases to 28 February 2022, the four countries reported the following cases: China reported 9,670 new confirmed cases and no deaths, with total deaths per million of 3.21; Israel reported 2,293,415 new confirmed cases and 2,016 deaths, with total deaths per million of 1,097.21; South Africa reported 731,384 new confirmed cases and 9,509 deaths, with total deaths per million reaching 1,655.708; the United States reported 3,042,743 new confirmed cases and 1,688,851 deaths, with total deaths per million reaching 2,855.052, which was much higher than the other countries.
Conclusion: Based on this study, it seems that China and Israel adopted containment strategies, while South Africa and the United States adopted mitigation strategies. A rapid response is a powerful weapon against the Omicron epidemic. Vaccines alone will not get any country out of this crisis, and non-pharmacological measures should be used in addition to them. According to the SPO model, future work should consider the strengthening of emergency management capacity, adhering to public health measures, promoting vaccination, and strengthening patient care and close contact management, which are effective measures in coping with Omicron.
Introduction
COVID-19 continues to pose a very high health threat worldwide, and waves of the COVID-19 epidemic are occurring one after another due to mutated variants. After the Alpha, Beta, Gamma, and Delta SARS-CoV-2 variants of concern (VOC), on 24 November 24 2021, South Africa reported to the World Health Organization (WHO) the discovery of a new SARS-CoV-2 variant B.1.1.529, which was named Omicron after 2 days (1). The Omicron variant had an overall global risk assessment of “very high” and spread worldwide (2). By 28 February 2022, there were 4,34,154,739 confirmed cases worldwide and 5,944,342 deaths.
The Omicron variant has important amino acid mutation sites for all previous four VOC variants that spur proteins, including mutation sites that enhance cellular receptor affinity and viral replication ability (3). Omicron spreads faster, and it is roughly 10 times more infectious than the original virus and twice as infectious as the Delta variant (4). Omicron has increased transmissibility, with the ability to evade immunity conferred by past infection or vaccination. Thus, Omicron generally causes less severe disease than infection with prior variants, which could threaten the effectiveness of current vaccination measures (e.g., reducing the effectiveness of current diagnostics, vaccines, and therapies) (3, 5). In addition, immunity duration after infection is about 3–6 months, and the variability of Omicron leads to a low rate of severe illness but increases the risk of re-infection.
From November 2021, the BA.2 subtype began to spread in India, South Africa, and the Philippines. The transmission rate of BA.2 is about 30% higher than BA.1, and more than 90% of infections are asymptomatic infections. There are 20% of latent infections (patients are undetectable by nucleic acid testing), which poses new challenges for detection and traceability (6, 7). In Jan 2022, the proportion of BA.2 sequences even exceeded that of BA.1 in Botswana, Denmark, Sweden, and India.
The spread of Omicron has been met with different responses from different countries. China is an importer of Omicron. Since January 2022, there have been indigenous epidemics caused by Omicron in Tianjin, Anyang, and Baise. The Omicron epidemic was responsible for the largest wave of infections in China after the first wave of COVID-19. Israel, a “vaccination honoree,” entered a violent fifth wave of the epidemic in December 2021, becoming the first closure country under Omicron. South Africa, the first country to report the Omicron variant, adopted a combination of mitigation and containment strategies in response to the previous three waves of COVID-19, but it began to resume work and production prematurely. The United States was severely affected by Omicron, where its rapidly increased, and on 9 January 2022, the Omicron variant accounted for about 98% of total cases, and hospitalizations underwent a 24.5% increase from the previous 7 days (8).
Vaccines are considered the key measure in combating COVID-19, and several studies show that vaccines can prevent severe illness and death. However, in some African countries, vaccination remains a privilege for a minority of the population (9). Omicron led to a dramatic increase in cases not only in countries with low vaccination rates, such as South Africa and Botswana, but also in countries with high vaccination rates, such as Israel and the United Kingdom, where a new COVID-19 wave began. Due to the variability and immune escape of Omicron, vaccination rates have not reached the herd immunity threshold, and with the shortage of vaccines in low-income countries and the time frame for vaccine protection, vaccines alone will not get any country out of this crisis (10). Countries should combine vaccination and non-pharmaceutical interventions, analyze the form of epidemic risk in time, and develop appropriate national response strategies (11, 12). To analyze the effectiveness of prevention and control strategies and put forward further measures according to the epidemiological characteristics of the Omicron variant, this study summarized the national response during Omicron epidemic in four countries: China, Israel, South Africa, and the United States.
Methods
Measures collection
We searched for COVID-19 prevention and control measures from office websites between the day of the first reported Omicron cases and 28 February 2022. The selection criteria and search strategy were as follows: (1) the measures prepared for COVID-19; (2) the measures changed after the discovery of the Omicron variant; (3) the measures were non-pharmaceutical interventions; (4) the measures were issued by the national government or state government.
A systematic literature search was performed in the National Health Commission of the People’s Republic of China,1 Israel’s.
Ministry of Health,2 South Africa’s National Department of Health,3 and the Centers for Disease Control and Prevention of the United States,4 in which literature was collected and screened following defined criteria for analysis. The last search was run on 1 April 2022.
Data collection
The COVID-19 data were extracted from official websites and updated in real time, including the Coronavirus Resource Centre at Johns Hopkins University5 and WHO Coronavirus (COVID-19) Dashboard.6 This study investigated new confirmed cases, total cases, total deaths, and total cases per million, which take country-specific conditions and population bases into account in China, Israel, South Africa, and the United States from the day of the first reported Omicron cases to 28 February 2022.
All in all, this study selected COVID-19 data and the major measures carried out between the day of the first reported Omicron cases and 28 February 2022 and analyzed the effectiveness of the COVID-19 major measures during the Omicron epidemic. It also assessed the effectiveness of controlling COVID-19 cases in four countries by combining total new cases and total new deaths during the Omicron epidemic.
Results
National strategy in response to omicron variant
Containment strategy
Both China and Israel are importers of the Omicron variant, and both countries quickly took border prevention and control measures after the first Omicron case. China has continued its ongoing entry control measures, implemented closed-loop management of arrivals, and issued risk alerts at border crossings. Israel closed its international airport and began a country-wide closure on 26 November 2021 after reporting the first Omicron case, becoming the first country to close the country due to the Omicron variant.
China is not only facing Omicron but also facing the threat of Delta. China adheres to the “guarding against imported cases and preventing a resurgence of epidemics in domestic” strategy and “dynamic zero” policy. Rather than adopting a uniform national strategy for epidemic prevention and control, China has adopted a “targeted management” strategy in different areas. On 8 January 2022, two Omicron cases were reported in Tianjin. As for movement restrictions, Tianjin issued control measures of “not leaving Tianjin unless necessary” and cut off passenger services in some areas; as for social distancing, Tianjin closed educational institutions, adopted closed management, and restricted gathering; and as for public health measures, Tianjin adopted multiple rounds of full staff nucleic acid testing and enhanced virus traceability and early warning of detection at key sites. In the treatment of the Omicron variant, Tianjin’s emphasis has been placed on both Chinese and Western medicine, with Chinese medicine participating in the medical treatment of confirmed cases throughout the whole process. The Omicron transmission period coincided with an important traditional festival, the Chinese New Year. China prepared emergency plans in advance and strengthened the communication and collaborative response mechanism of various departments.
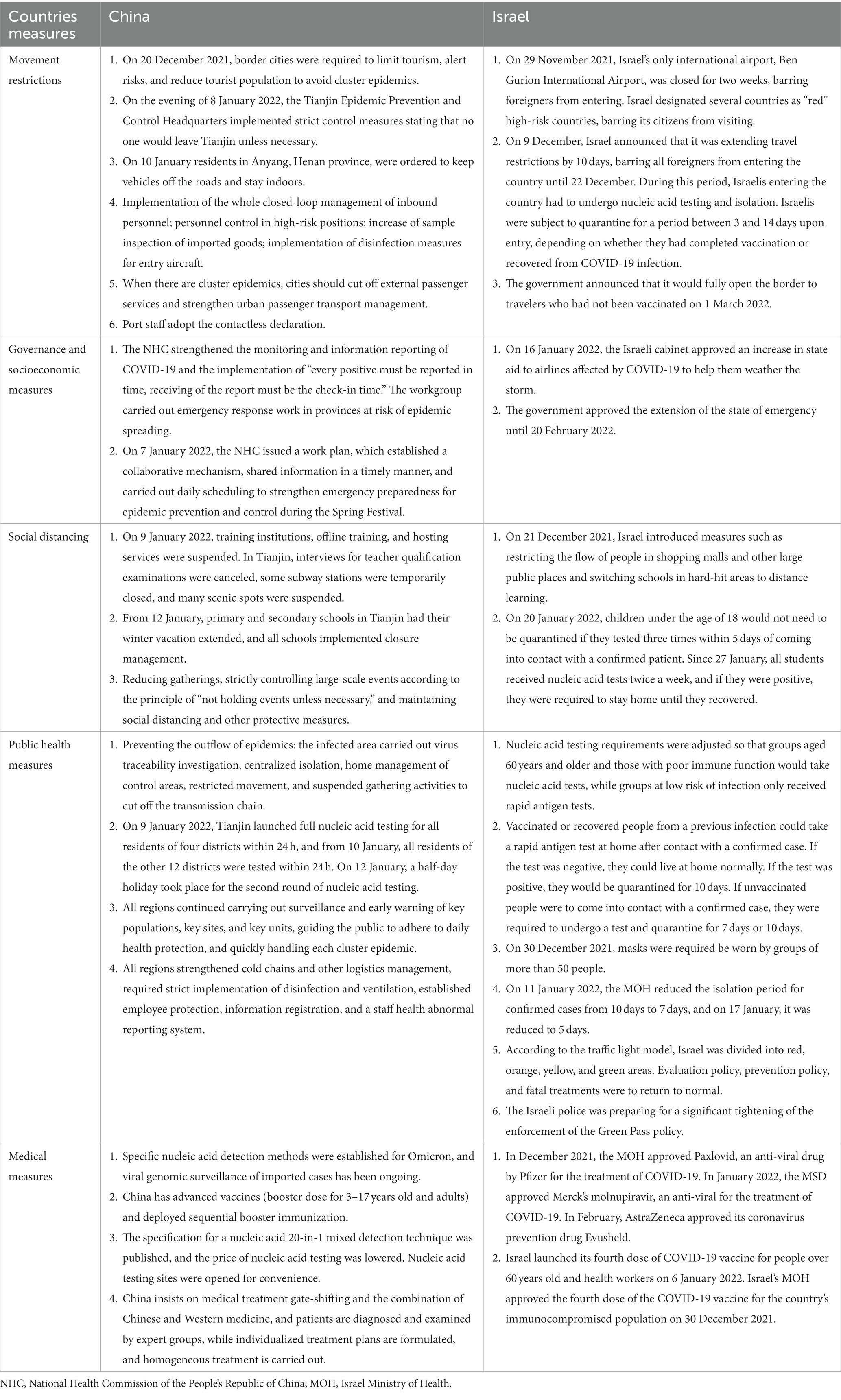
On 26 November 2021, the Israeli Ministry of Health issued a statement saying that the country’s first Omicron case had been identified. The statement said the case came from the African country of Malawi. In addition, two other people entering the country were are also suspected of having been infected with Omicron. Israel quickly closed its borders, switched schools to online teaching, and approved several prevention and treatment drugs. In addition, it used the traffic light model to show the extent of the regional epidemic. According to characteristics of the Omicron variant, it shortened the isolation period and replaced nucleic acid testing with antigen testing. Israel was the first country to introduce a third-dose vaccination and to focus its vaccination efforts on the protection of vulnerable populations. However, on 1 March 2022, Israel lifted almost all social interventions and fully opened its borders to all negative travelers, regardless of their vaccination status. Table 1 summarizes the major measures taken by China and Israel in response to the Omicron variant, including movement restrictions, governance and socioeconomic measures, social distancing, and public health measures.
Mitigation strategy
The Omicron variant was first detected in South Africa on 9 November 2021. By 1 December, for a month-long period, South Africa had little policy response to the Omicron. By mid-December, it began closing schools, adjusting the national statement, and closing nightclubs and some venues. On 30 December, the government said that the COVID-19 data showed that the country had passed the fourth wave peak of the epidemic and would lift curfews and limit gathering. Subsequently, South Africa stepped up vaccine procurement, closed some borders, and resumed classes. It also announced that isolation would be recommended for asymptomatic infections rather than mandatory isolation and allowed participation in social activities, which only required the wearing of masks. From 23 February 2022, South Africa shortened vaccination schedules and allowed different brands of vaccines to promote vaccination.
The United States, which is an importer of the Omicron variant, implemented entry restrictions for southern African countries on 26 November 2021 and added a negative nucleic acid test certificate for international travelers on 6 December; subsequently, international travelers were advised to go into self-isolation upon entry. On 1 December, the United States reported that California had identified its first Omicron case, the carrier of whom had returned to California from South Africa on 22 November and tested positive on 29 November. The United States declared an extended national emergency, introduced indicators for monitoring COVID-19 community levels, and implemented prevention strategies. In the face of the skyrocketing rate of confirmed cases and insufficient medical resources, the United States encouraged people to conduct self-testing at home and shortened the isolation period based on the Omicron incubation period, as well as promoting vaccination, strengthening public health measures such as wearing masks and increasing physical distance in schools, and adopting measures—such as permitting healthcare workers with asymptomatic COVID-19 to return to work after 7 days with a negative test—and other measures to alleviate the shortage of healthcare workers. Table 2 summarizes the major measures taken by South Africa and the United States in response to the Omicron variant, including movement restrictions, governance and socioeconomic measures, social distancing, and public health measures.
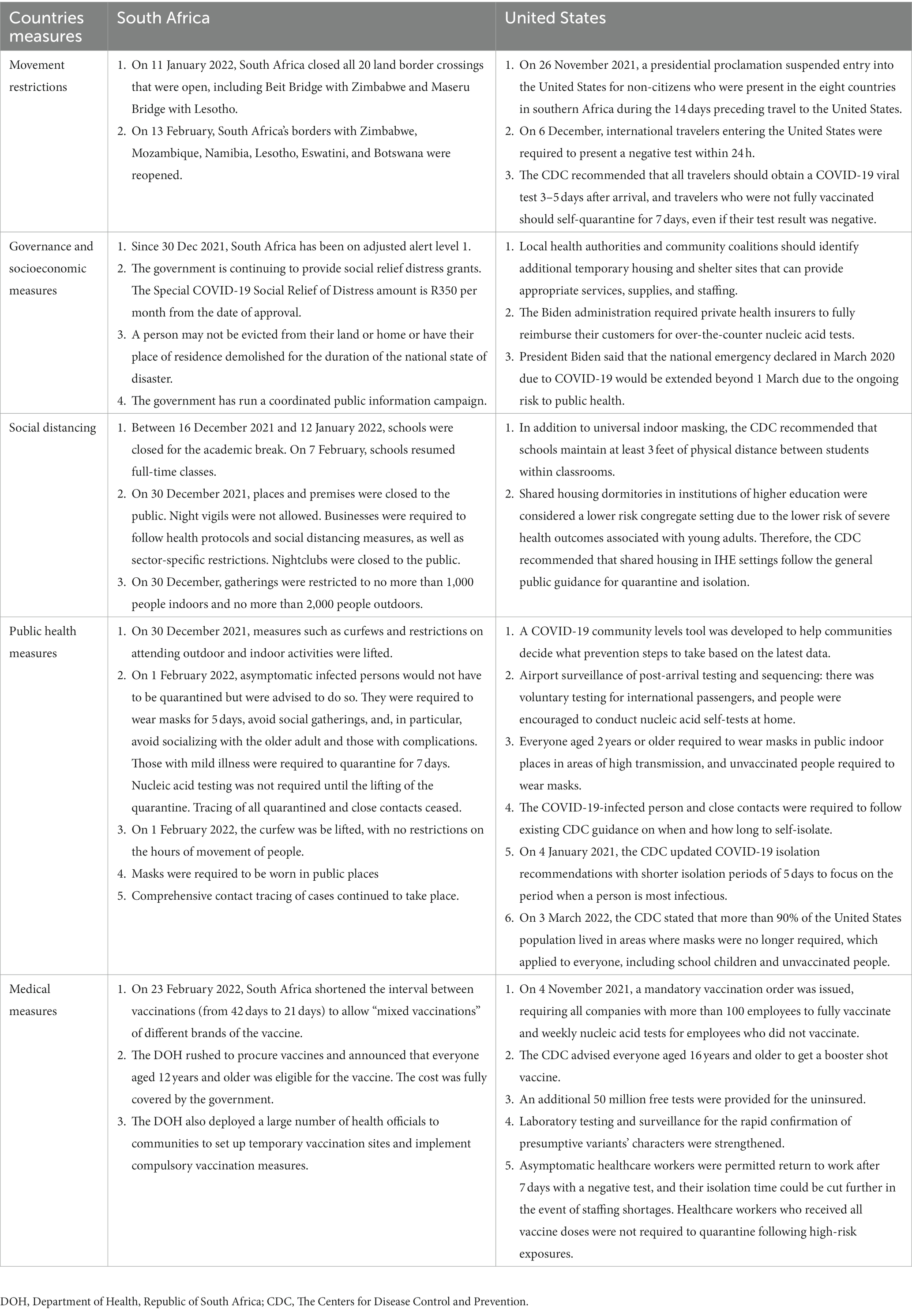
Table 2. The major measures taken by South Africa and the United States in response to the Omicron variant.
Results of national strategies in response to omicron variant
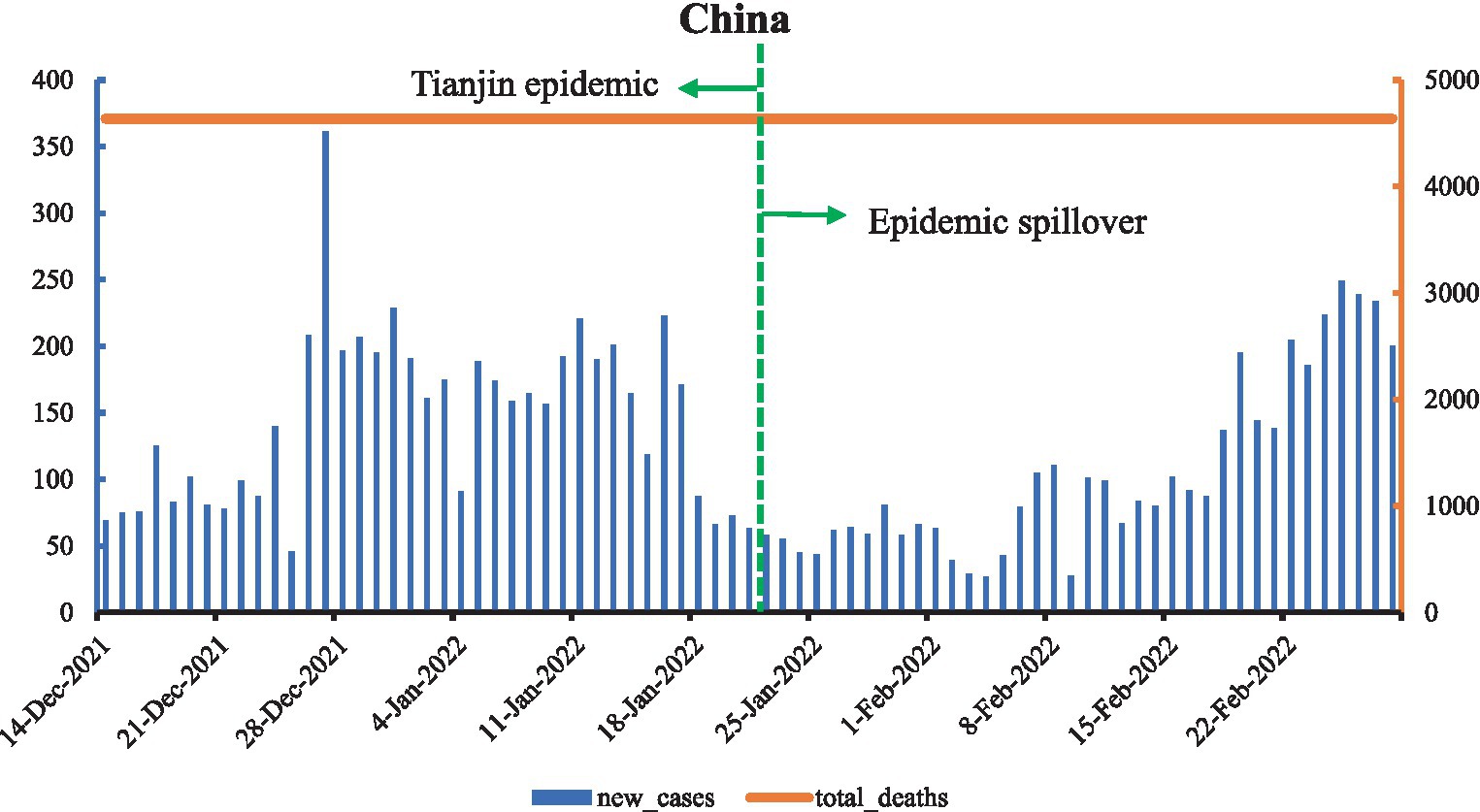
As shown in Figure 1, on 13 December 2021, an Omicron case was reported in Tianjin, which was the first reported Omicron variant case in mainland China. The Omicron variant led to the most confirmed cases in China since the Wuhan epidemic in 2019. Initially, Omicron cases were mainly concentrated in Tianjin, but in January 2022, the Omicron epidemic spilled over to Dalian, Liaoning, and Anyang, Henan, with the second Omicron wave outbreaks. On January 21 2022, Tianjin declared the epidemic to be “socially cleared” as part of the first large-scale battle against Omicron in China. New confirmed cases decreased and remained between 50 and 100 cases. In February, Omicron cases were reported in many places, and new confirmed cases started to grow, with a total of 9,670 new confirmed cases and no deaths during this period and total deaths at 3.21 per million.
As shown in Figure 2, the Omicron epidemic in Israel can be divided into three phases based on new confirmed cases: the containment period, rapid growth period, and decline period. During the containment period, the Omicron variant began to spread as soon as it was reported, with new cases stabilizing to under a thousand. Starting from mid-December 2021, new confirmed cases began to grow rapidly, surpassing 1,000 cases on 20 December 2021, exceeding 10,000 cases on 5 Jan 2022, and peaking on 19 January. Thereafter, new confirmed cases gradually fell back into the decline period. Unlike China, deaths in Israel increased with the new confirmed cases, and by 28 February, there were 2,293,415 new confirmed cases and 2,016 deaths, with total deaths per million reaching 1,097.621.
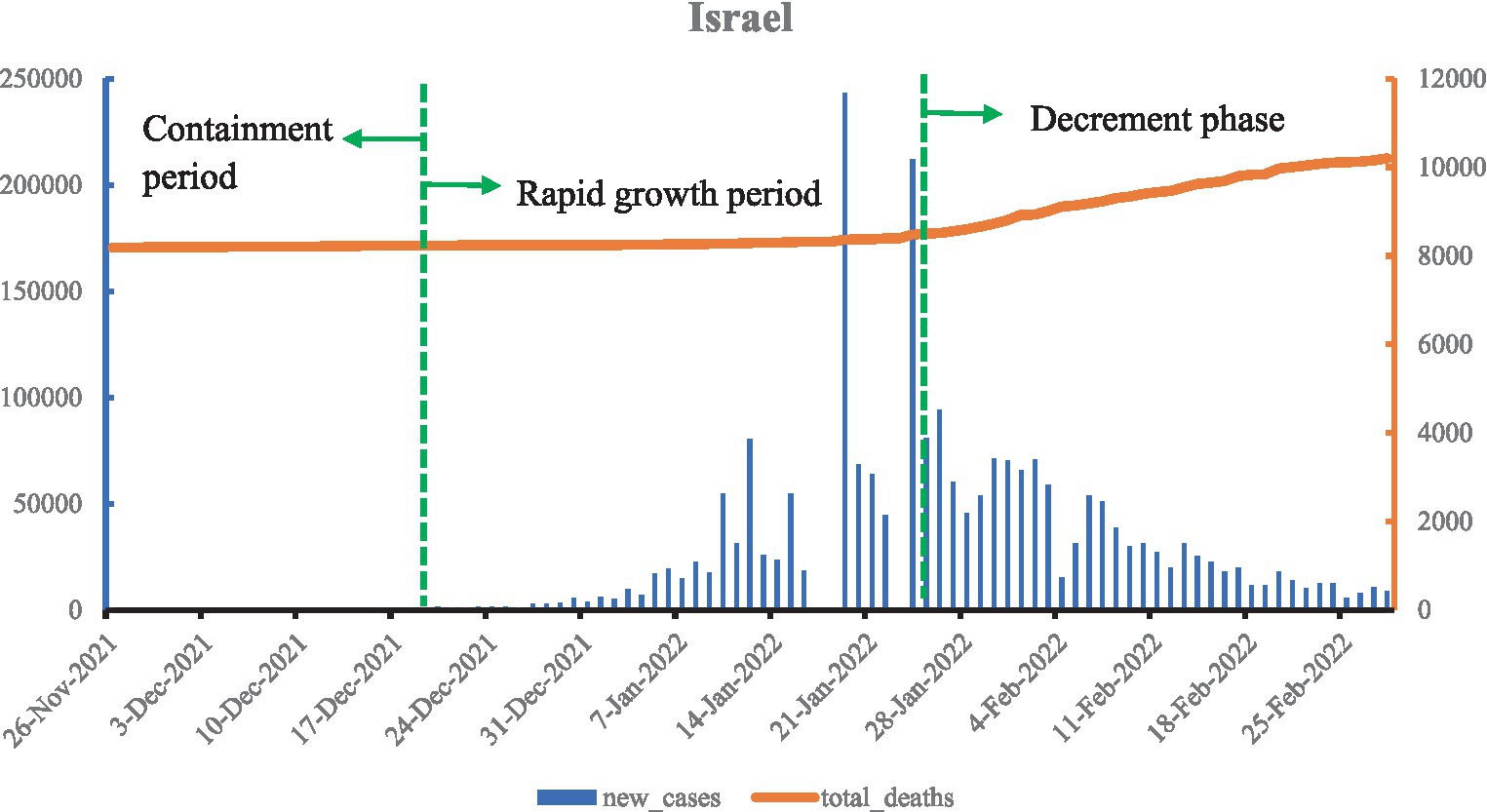
Figure 2. Curve of Omicron variant of COVID-19 epidemic in Israel (data vacancy exists on 17, 18, and 23 January 2022).
As shown in Figure 3, when the Omicron variant was detected in South Africa on 9 November 2021, new confirmed cases remained stable for only half a month. A dramatic increase began on 24 November, and the South African Department of Health announced the official fourth wave of the epidemic peak on 3 December, with the peak reaching more than 37,000 new confirmed cases on 12 December. The new confirmed cases in South Africa show a cyclical trend, with a post-peak period followed by a fall and another peak. In addition, the number of deaths shows a uniform increase. By 28 February 2022, the total confirmed cases were 731,384 and deaths increased by 9,509, with total deaths per million at 1,655.708.
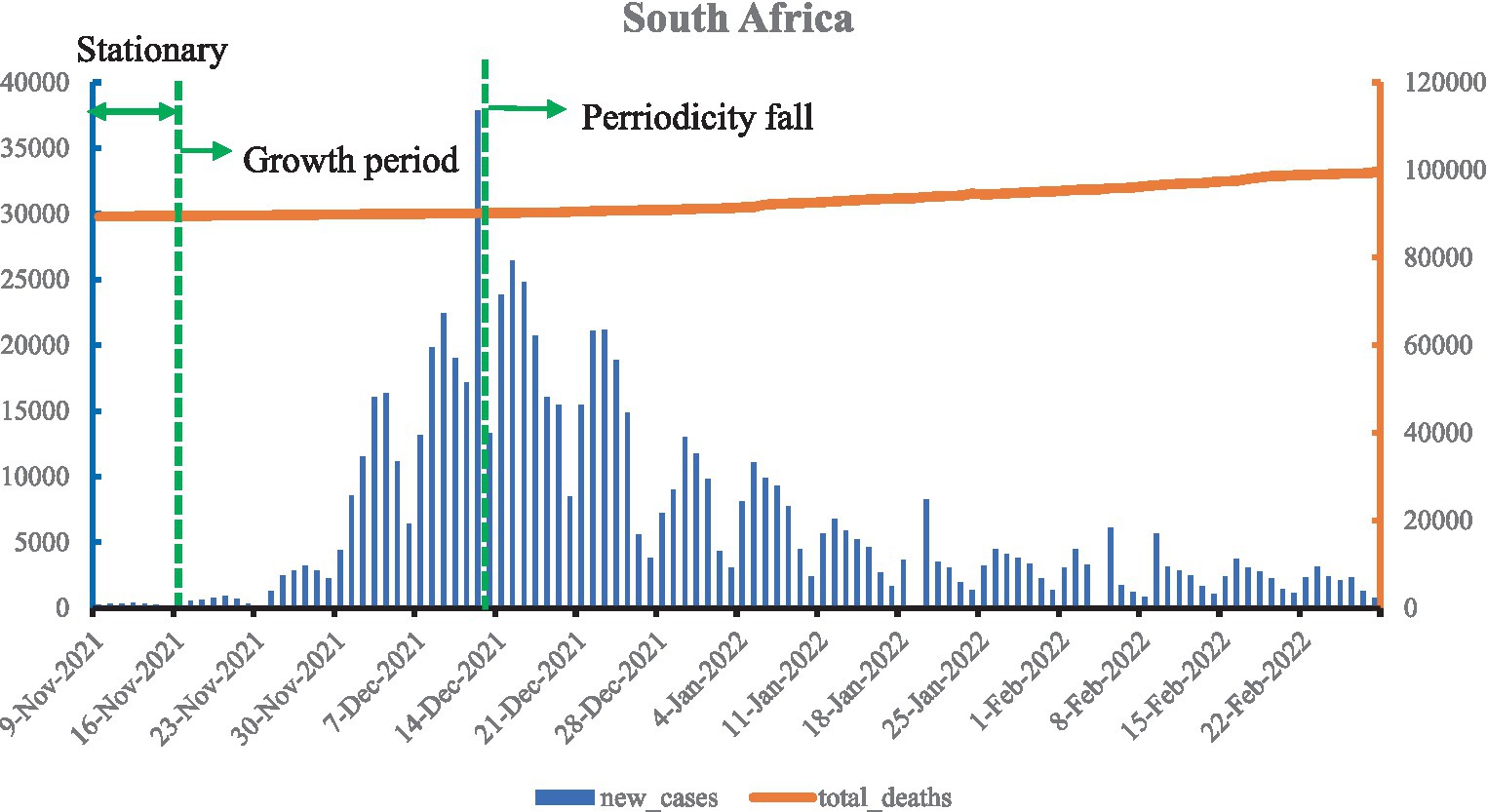
Figure 3. Curve of Omicron variant of COVID-19 epidemic in South Africa (data vacancy exists on 23 November 2021 and 18, 19, and 24 February 2022).
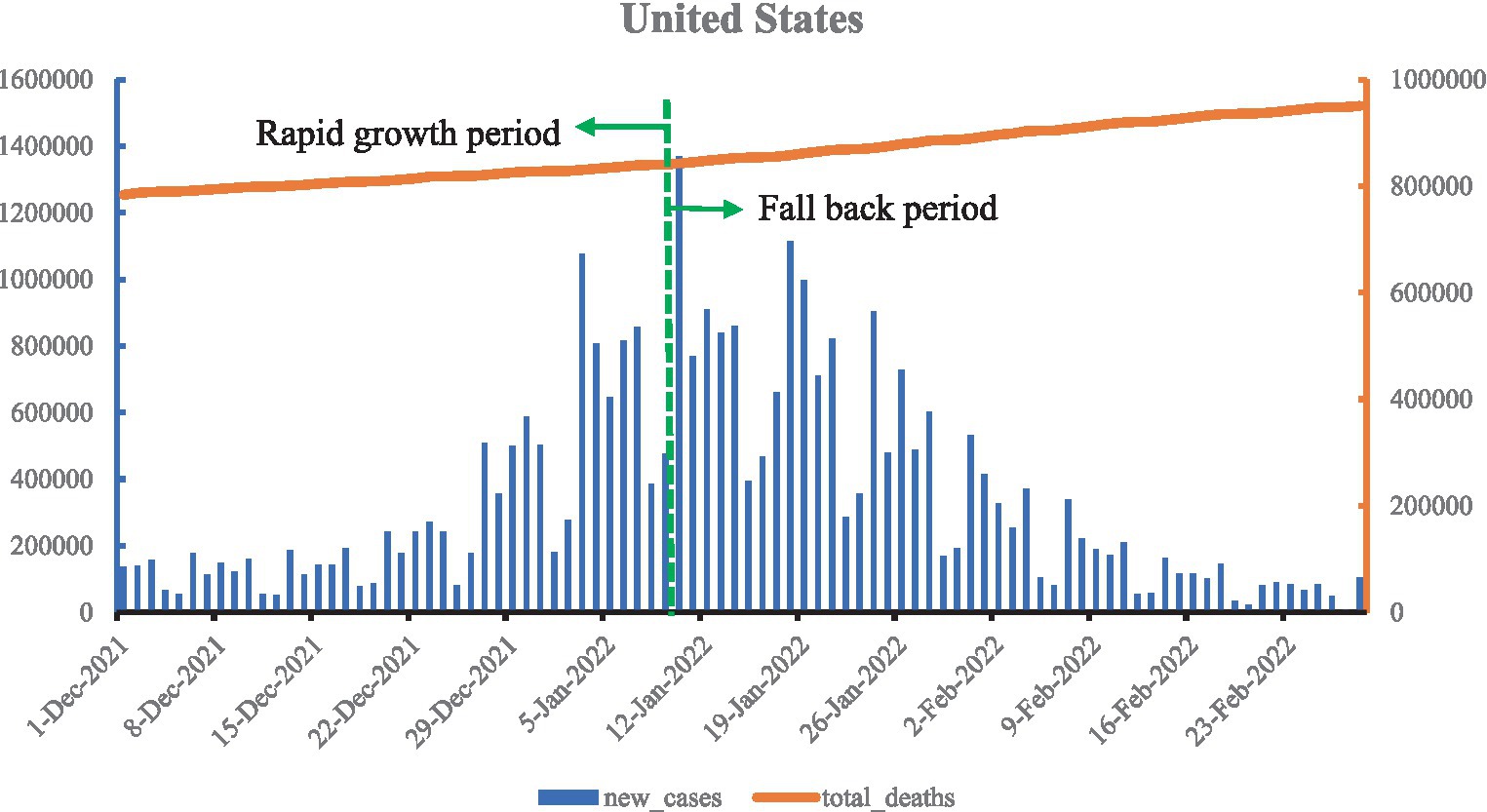
As shown in Figure 4, Omicron spread in the United States, accounting for 92.3% of new confirmed cases in the week of 1 January 2022, and new confirmed cases also increased, slightly higher than previously. In January, the Omicron variant spread more widely across the country. On 10 February, new confirmed cases reached a staggering 1.36 million, a record high, marking the Omicron epidemic peak, after which new confirmed cases fell back. Deaths continued to climb, and by 28 February, the Omicron epidemic had accumulated 30,462,743 new confirmed cases and 168,851 deaths, with total deaths per million at 2,855.052.
The results in Figure 5 comprise the number of COVID-19 cases on 28 February 2022 subtracted from the COVID-19 cases on the day of the first reported Omicron cases. As shown in Figure 5, during the Omicron epidemic, the total new cases and total new deaths in China, Israel, South Africa, and the United States increased in sequence. China increased its total number of new cases by 9,601 and maintained zero new deaths. Israel’s total new cases (2,292,962) were higher than South Africa’s (749,725) but the total new deaths (2,016) remained lower than South Africa’s (10,025). The total new cases and total new deaths in the United States increased exponentially to 730,325,787 and 166,739, respectively.
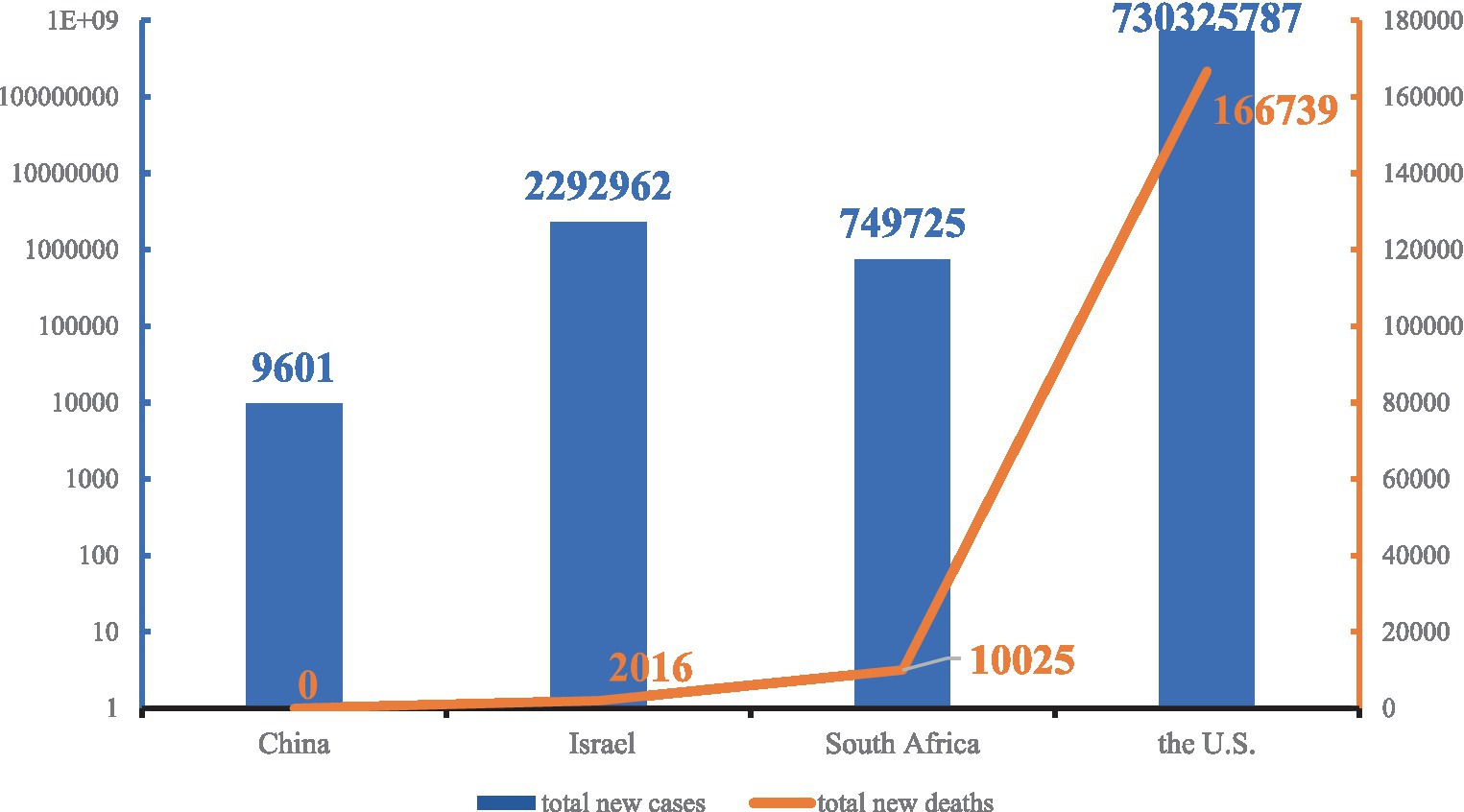
Figure 5. Total new cases and total new deaths in China, Israel, South Africa, and the United States during the Omicron variant of the COVID-19 epidemic.
Discussion
Scholars around the world are debating whether Omicron means that the COVID-19 epidemic is coming to an end or marks the start of a new global pandemic. The WHO Director-General, Dr. Tedros said it was “wrong for people to consider Omicron as mild” (13). According to the WHO, Omicron is more transmissible and has been shown to produce breakthrough infections. In terms of virulence, the death risk caused by Omicron is 69% lower than Delta, but Omicron is 6–9 times more contagious than influenza and is a breakthrough infection, and thus it may cause more infections and deaths (14). All over the world, no health system can withstand the COVID-19 pandemic, and existing vaccines are less effective against Omicron’s neutralizing antibodies, meaning there are higher requirements for the rapid implementation of non-pharmaceutical interventions. Thus, Omicron remains serious (15).
At this point, there are two directions for coping with Omicron. One is the containment strategy, which firmly takes measures to contain the spread of the epidemic, and the other is the mitigation strategy, which abandons epidemic prevention and control measures. Omicron spreads very rapidly, and the current level of epidemic prevention is insufficient. Therefore, there is no chance to regain control once epidemic prevention measures are abandoned, and a government’s judgment and choice of prevention policies will affect the health and lives of people in their country and even the world. This study discusses two response strategies adopted by four countries and makes recommendations for further measures to combat the Omicron pandemic.
Containment strategy
The goal of the containment strategy is to stop the virus from spreading as much as possible and eventually make the epidemic disappear. This is manifested by actively identifying cases and taking action, especially actively tracking and isolating close contacts to cut off the transmission route. Both China and Israel adopted containment strategies, and China has been practicing a dynamic zero policy of detecting one case and containing one case. Israel quickly closed its borders and country.
Omicron in China is characterized by “many points, extensive and frequent,” and the epidemic is very serious. China adhered to the “dynamic zero” policy, which means that when a case or an epidemic emerges, it can be quickly detected, quickly contained, and its transmission process cut off, thus finally achieving the “discover one, extinguish” approach in order to prevent the epidemic from causing community transmission. After discovering an outbreak, the National Health Commission of the People’s Republic of China would immediately send a task force to participate in prevention and control. However, the “zero policy” has been questioned. Some scholars argue that a blockade is not a long-term solution and that the country should be opened. China is the only country that has achieved positive GDP growth and completed poverty eradication in 2020. Confirmed cases in China were only 0.0076% of the country’s population, and the death rate was very low. If intervention measures are lifted, according to China’s population base and population density, infections may grow exponentially, which will easily cause a run on medical resources with unimaginable consequences. At this stage, it is still necessary to adhere to the “zero policy” and gradually open up, exchanging a short period of embargo for a long period of normal life (16).
Israel is known as a “vaccination honoree” and the first country to introduce a third-dose vaccine. Before the Omicron epidemic, Israel was actively preparing for the implementation of a fourth-dose vaccine. When the first Omicron case was reported, over 60% of Israel’s people were fully vaccinated (13). Due to the early vaccinations, the protective effects of the vaccines have decreased, and new confirmed cases remain at a high level (17–20). Israel opened its borders on 1 March 2022, marking the first time since the COVID-19 epidemic that it fully opened its borders. In addition, Israel has adjusted its coronavirus detection requirements of rapid antigen testing for groups at lower risk of infection, replacing the $10.08 PCR test with a $5.70 rapid antigen test, in part to reduce the cost of coronavirus testing (21). The Israeli experience shows that a high rate of vaccination may not prevent the infection and transmission of Omicron, but it can effectively reduce severe illness and mortality and keep the healthcare system from collapsing. Moreover, high vaccine coverage can help control the epidemic and restore normalcy to life.
Mitigation strategy
The mitigation strategy is also used in response to a pandemic, and it is recommended by the WHO for use in phases 5 and 6 of a pandemic, primarily to reduce its impact and contain an epidemic within a certain range. If mitigation strategies are implemented, vaccine promotion and strengthening the carrying capacity of the health system become very important. In response to Omicron, South Africa and the United States did not strengthen their epidemic measures but rather shortened their isolation times, relaxed mandatory isolation, and focused their epidemic prevention on vaccination and severe case management.
By November 2021, after the third wave of COVID-19 in South Africa, seroprevalence was 60% in a rural community and 70% in an urban community (22). The “asymptomatic carriage” rate of Omicron is much higher than prior variants. Significant asymptomatic infections, coupled with the insidious nature and the small amount of viral excretion during the incubation period, make it difficult for detecting the disease, and a single nucleic acid test may show a false negative. During the Omicron epidemic, South Africa reached the peak of the epidemic faster than in the previous three waves, but the disease was milder, and the risk of serious illness was 30% lower than in prior variants (23). On 30 December, the South African government announced that the country had passed the peak of the fourth wave of the epidemic (24). The WHO announced on 18 January 2022 that in South Africa the Omicron epidemic was coming to an end (25). South Africa began to liberalize its borders, resume schooling, lift restrictions, and lift mandatory quarantine of asymptomatic infections, shifting from a blockade to improving population immunity. However, South Africa has a young population and a high early infection rate, which may have contributed to the mild impact of the epidemic. From the global data, the COVID-19 pandemic is still not over, and the BA.2 variant is gradually becoming the dominant virus.
Compared to the death rate in South Africa, daily new deaths in the United States remained at a peak after the previous rounds of confirmed cases and deaths. By February 2022, even with more than 900,000 total deaths, there were still about 2,000 deaths per day (26). The United States COVID-19 response has been called “living with COVID-19,” and no effective prevention policy has even been proposed so far. Rather, it opted to eliminate masks, shorten quarantine times, and slow down prevention policies (27). With the following spike in new confirmed cases, the run on the United States healthcare system was severe. To alleviate the strain on healthcare workers, asymptomatic infected healthcare workers were permitted to return to work after 7 days, and vaccinated healthcare workers do not need to be quarantined even after high-risk exposures. Studies show that United States health workers, especially nurses and advanced practice providers, are experiencing COVID-19-related psychological distress (28). In terms of the healthcare system, it is not enough to ignore epidemic prevention measures and focus solely on vaccination and treatment of serious cases. Healthcare workers and medical equipment are severely overloaded, and nucleic acid testing capacity is insufficient, resulting in confirmed cases not being effectively treated and accelerating transmission, thus creating a vicious cycle (29, 30).
Further measures
As the world enters the third year of the COVID-19 epidemic, after four or five waves of the epidemic, many countries are gradually giving up on prevention. However, the Omicron variant has an average basic and effective reproduction number of 8.2 and 3.6, which means that it has a strong spread (31). Moreover, more and more countries’ epidemic data tell us that vaccines alone will not get any country out of this crisis (10, 32). With the current level of epidemic prevention and capacity of healthcare system, once the epidemic invention measures are abandoned and the optimal period of intervention for Omicron variant is missed, there will be no chance to regain control; thus, countries should take active and effective intervention measures to cope with the Omicron variant.
This study introduces the structure–process–outcome (SPO) model, which was first introduced by the American scholar Avedis Donabedian in the Evaluation of Health Care Quality, which proposes COVID-19 prevention and control measures to cope with the Omicron variant from three dimensions: structure, process, and outcome (33). In the prevention and control of COVID-19, the “structure” dimension includes emergency plans for public health emergencies, governmental epidemic networks, emergency command systems, regulations, and resource allocation, which are mainly reflected in governance and socioeconomic measures. The “process” dimension includes the general protection of the population, mainly reflected in movement restrictions, social distancing, and public health; the “outcome” dimension includes the treatment of confirmed cases and the management of close contacts and experience summaries, covering medical measures and other components (34–36).
Structure
Firstly, countries around the world have to cooperate to fight COVID-19. COVID-19 has become a global pandemic, and no country can stay out of it (37). Secondly, the Omicron variant is always mutating, from the original strain BA.1 to BA.2, and we cannot predict the direction of its mutation. Therefore, countries need to enhance the global surveillance of coronavirus and its variants with data posted on appropriate reporting platforms (38). For many countries, variants are mainly imported through foreign countries. Thus, countries need to strengthen entry management and the related eradication. Finally, countries should develop regulations related to COVID-19, establish work plans and work coordination mechanisms, clarify responsibilities and the division of labor, and prepare for emergencies.
Process
Firstly, countries need to recognize the seriousness of the Omicron variant due to its rapid spread, which requires a faster response (39). In some countries, similar or higher numbers of deaths have been reported when compared to the previous peaks (40). Countries should take an effort to raise awareness and guide people to eliminate fear and cooperate with the implemented measures. Secondly, public health measures such as maintaining social distancing and wearing masks should be adhered to, and restrictive measures such as city closures should be appropriately applied. Public health measures are an effective way of protecting against infection with COVID-19 (41, 42). Thirdly, vaccines are a powerful weapon to prevent COVID-19, and the unvaccinated remain at higher risk of severe disease following infection with Omicron compared to those who have been vaccinated (40). However, vaccine effectiveness decreases over time, and countries should advance sequential immunization, or alternate immunization, to enhance the population’s immune barrier through universal vaccination (20, 43).
Outcome
Firstly, countries should strengthen epidemiological investigations, trace close contacts, and take isolation measures. Secondly, countries should promptly conduct multiple rounds of nucleic acid testing. Omicron spreads faster, has less obvious symptom expression and is more insidious, and it is prone to multi-point dissemination and concentrated outbreaks. Only a rapid response and early screening of positive infections to take control measures can try to contain the spread. Moreover, countries should carry out the treatment of patients, strengthen the service capacity of the healthcare system, and promote telemedicine for other patients as well as drug development.
Conclusion
Based on this study, it seems that China and Israel adopted containment, whereas South Africa and the United States adopted mitigation strategies. A rapid response is a powerful weapon against the Omicron epidemic. To cope with Omicron, we need to recognize its seriousness and firmly take prevention and control measures, especially in terms of immediate collective response in the early stages of the epidemic. Vaccines alone will not get any country out of this crisis, and they should be utilized in coordination non-pharmacological measures (10). According to the SPO model, this is desirable for future work: strengthening emergency management capacity, adhering to public health measures, promoting vaccination, and strengthening patient care and close contact management are the most effective measures in coping with Omicron.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
JJ and GS conceived the manuscript and contributed as the study guarantors. HC, XW, MY, JY, and ML collected the data. JJ drafted the manuscript. LS, HC, and XW revised the manuscript. GS contributed to the critical revision of the manuscript for important intellectual content and approved the final version of the manuscript.
Funding
This study was supported by the Natural Science Foundation of Guangdong Province in 2022: Construction and application of COVID-19 control model PSR-SOR-Haddon in Guangdong Province (No. 2022A1515011112).
Acknowledgments
The authors gratefully acknowledge the study participants who were involved in and contributed to the paper.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
1. ^ http://en.nhc.gov.cn/index.html
2. ^ https://www.gov.il/en/departments/ministry_of_health
3. ^ https://sacoronavirus.co.za/
4. ^ https://www.cdc.gov/coronavirus/2019-ncov/index.html
References
1. Classification of Omicron (B.1.1.529): SARS-CoV-2 Variant of Concern. Available at: (https://www.who.int/news/item/26-11-2021-classification-of-Omicron-(b.1.1.529)-sars-cov-2-variant-of-concern)
2. Enhancing response to Omicron SARS-CoV-2 variant. Available at: (https://www.who.int/publications/m/item/enhancing-readiness-for-Omicron-(b.1.1.529)-technical-brief-and-priority-actions-for-member-states)
3. Kannan, S, Shaik Syed Ali, P, and Sheeza, A. Omicron (B.1.1.529) – variant of concern – molecular profile and epidemiology: a mini review. Eur Rev Med Pharmacol Sci. (2021) 25:8019–22. doi: 10.26355/eurrev_202112_27653
4. Meo, SA, Meo, AS, Al-Jassir, FF, and Klonoff, DC. Omicron SARS-CoV-2 new variant: global prevalence and biological and clinical characteristics. Eur Rev Med Pharmacol Sci. (2021) 25:8012–8. doi: 10.26355/eurrev_202112_27652
5. Kupferschmidt, K, and Vogel, G. How bad is omicron? Some clues are emerging. Science. (2021) 374:1304–5. doi: 10.1126/science.acx9782
6. Bruel, T, Hadjadj, J, Maes, P, Planas, D, Seve, A, Staropoli, I, et al. Serum neutralization of SARS-CoV-2 omicron sublineages BA.1 and BA.2 in patients receiving monoclonal antibodies. Nat Med. (2022) 28:1297–302. doi: 10.1038/s41591-022-01792-5
7. Garrett, N, Tapley, A, Andriesen, J, Seocharan, I, Fisher, LH, Bunts, L, et al. High asymptomatic carriage with the omicron variant in South Africa. Rev Infect Dis. (2022) 75:ciac237:e289–92. doi: 10.1093/cid/ciac237
8. CDC. COVID data tracker weekly review. Centers for Disease Control and Prevention. (2022) Available at: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/past-reports/01142022.html (Accessed February 10, 2022)
9. Key lessons from Africa’s COVID-19 vaccine rollout. WHO | regional Office for Africa. Available at: https://www.afro.who.int/news/key-lessons-africas-covid-19-vaccine-rollout (Accessed December 24, 2021).
10. WHO Director-General’s opening remarks at the media briefing on COVID-19. Available at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---14-december-2021 (Accessed December 14, 2021).
11. Coronavirus disease (COVID-19): How is it transmitted?. Available at: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-how-is-it-transmitted (Accessed December 23, 2021).
12. Morens, DM, Folkers, GK, and Fauci, AS. The concept of classical herd immunity may not apply to COVID-19. J Infect Dis. (2022) 226:195–8. doi: 10.1093/infdis/jiac109
13. COVID-19 Data Explorer. Our world in data. – 23 December 2021. Available at: (https://ourworldindata.org/coronavirus-data-explorer)
14. Nyberg, T, Ferguson, NM, Nash, SG, Webster, HH, Flaxman, S, Andrews, N, et al. Comparative analysis of the risks of hospitalisation and death associated with SARS-CoV-2 omicron (B.1.1.529) and delta (B.1.617.2) variants in England: a cohort study. Lancet Lond Engl. (2022) 399:1303–12. doi: 10.1016/S0140-6736(22)00462-7
15. Islam, MR, and Hossain, MJ. Detection of SARS-CoV-2 omicron (B.1.1.529) variant has created panic among the people across the world: what should we do right now? J Med Virol. (2022) 94:1768–9. doi: 10.1002/jmv.27546
16. Luo, M, Liu, Q, Wang, J, and Gong, Z. From SARS to the omicron variant of COVID-19: China’s policy adjustments and changes to prevent and control infectious diseases. Biosci Trends. (2022) 15:418–23. doi: 10.5582/bst.2021.01535
17. Regev-Yochay, G, Gonen, T, Gilboa, M, Mandelboim, M, Indenbaum, V, Amit, S, et al. Efficacy of a fourth dose of COVID-19 mRNA vaccine against omicron. N Engl J Med. (2022) 386:1377–80. doi: 10.1056/NEJMc2202542
18. Andrews, N, Stowe, J, Kirsebom, F, Toffa, S, Rickeard, T, Gallagher, E, et al. COVID-19 vaccine effectiveness against the omicron (B.1.1.529) variant. N Engl J Med. (2022) 386:1532–46. doi: 10.1056/NEJMoa2119451
19. Haas, EJ, Angulo, FJ, McLaughlin, JM, Anis, E, Singer, SR, Khan, F, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet. (2021) 397:1819–29. doi: 10.1016/S0140-6736(21)00947-8
20. Goldberg, Y, Mandel, M, Bar-On, YM, Bodenheimer, O, Freedman, L, Haas, EJ, et al. Waning immunity after the BNT162b2 vaccine in Israel. N Engl J Med. (2021) 385:NEJMoa2114228. doi: 10.1056/NEJMoa2114228
21. Jakobsen, KK, Jensen, JS, Todsen, T, Tolsgaard, MG, Kirkby, N, Lippert, F, et al. Accuracy and cost description of rapid antigen test compared with reverse transcriptase-polymerase chain reaction for SARS-CoV-2 detection. Dan Med J. (2021) 68:A03210217.
22. Kleynhans, J, Tempia, S, Wolter, N, von Gottberg, A, Bhiman, JN, Buys, A, et al. SARS-CoV-2 Seroprevalence after third wave of infections, South Africa. Emerg Infect Dis. (2022) 28:1055–8. doi: 10.3201/eid2805.220278
23. South African doctors see signs Omicron is milder than delta. AP NEWS. (2021) Available at: https://apnews.com/article/coronavirus-pandemic-health-africa-south-africa-southern-africa-bd7a30e490c407b8d84afef5ac9e203e (Accessed April 11, 2022).
24. South Africa lifts curfew as it says Covid Omicron peak has passed. CNBC. (2021) Available at: https://www.cnbc.com/2021/12/30/south-africa-lifts-curfew-as-it-says-covid-fourth-wave-has-passed-the-peak.html (Accessed April 11, 2022).
25. WHO Director-General’s opening remarks at the media briefing on COVID-19. Available at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-18-january-2022 (Accessed April 11, 2022).
26. CDC. COVID data tracker weekly review. Centers for Disease Control and Prevention. (2022). Available at: (https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/past-reports/02252022.html)
27. Chotpitayasunondh, T, Fischer, TK, Heraud, J, Hurt, AC, Monto, AS, Osterhaus, A, et al. Influenza and COVID-19: what does co-existence mean? Influenza Other Respir Viruses. (2021) 15:407–12. doi: 10.1111/irv.12824
28. Shechter, A, Diaz, F, Moise, N, Anstey, DE, Ye, S, Agarwal, S, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. (2020) 66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007
29. Geyman, J. COVID-19 has revealed America’s broken health care system: what can we learn? Int J Health Serv Plan Adm Eval. (2021) 51:188–94. doi: 10.1177/0020731420985640
30. Ala, A, Wilder, J, Jonassaint, NL, Coffin, CS, Brady, C, Reynolds, A, et al. COVID-19 and the uncovering of health care disparities in the United States, United Kingdom and Canada: call to action. Hepatol Commun. (2021) 5:1791–800. doi: 10.1002/hep4.1790
31. Liu, Y, and Rocklöv, J. The effective reproduction number for the omicron SARS-CoV-2 variant of concern is several times higher than Delta. J Travel Med. (2022) 29:taac037. doi: 10.1093/jtm/taac037
32. Espenhain, L, Funk, T, Overvad, M, Edslev, SM, Fonager, J, Ingham, AC, et al. Epidemiological characterisation of the first 785 SARS-CoV-2 omicron variant cases in Denmark, December 2021. Eur Secur. (2021) 26:2101146. doi: 10.2807/1560-7917.ES.2021.26.50.2101146
33. Duff, P. Structure, process and outcome: quality guru Avedis Donabedian recently presently presented the university of Oxford’s Litchfield lecture on “quality in health care: the Consumer’s role”. Pat Duff reports on his philosophy of health care. Nurs Stand. (1992) 7:4–5. doi: 10.7748/ns.7.11.4.s71
34. Chaves dos Santos, SM, and Pacheco Santos, LM. Evaluation of public policies for food security and hunger control in Brazil, 1995-2002. 1 - methodological framework. Cad Saude Publica. (2007) 23:1029–40. doi: 10.1590/s0102-311x2007000500005
35. Zinn, JS, and Mor, V. Organizational structure and the delivery of primary care to older Americans. Health Serv Res. (1998) 33:354–80.
36. Maurer, NR, Hogan, TH, and Walker, DM. Hospital- and system-wide interventions for health care-associated infections: a systematic review. Med Care Res Rev. (2021) 78:643–59. doi: 10.1177/1077558720952921
37. Aida, T, and Shoji, M. Cross-country evidence on the role of national governance in boosting COVID-19 vaccination. BMC Public Health. (2022) 22:576. doi: 10.1186/s12889-022-12985-5
38. Vogels, CBF, Breban, MI, Ott, IM, Alpert, T, Petrone, ME, Watkins, AE, et al. Multiplex qPCR discriminates variants of concern to enhance global surveillance of SARS-CoV-2. PLoS Biol. (2021) 19:e3001236. doi: 10.1371/journal.pbio.3001236
39. Su, Z, McDonnell, D, Ahmad, J, Cheshmehzangi, A, and Xiang, YT. Mind the “worry fatigue” amid omicron scares. Brain Behav Immun. (2022) 101:60–1. doi: 10.1016/j.bbi.2021.12.023
40. Weekly epidemiological update on COVID-19. Available at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---12-april-2022 (Accessed April 12, 2022).
41. Zhang, J, Feng, T, Kang, J, Li, S, Liu, R, Ma, S, et al. “What should be computed” for supporting post-pandemic recovery policymaking? A life-oriented perspective. Comput Urban Sci. (2021) 1:24. doi: 10.1007/s43762-021-00025-8
42. Karim, SSA, and Karim, QA. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet Lond Engl. (2021) 398:2126–8. doi: 10.1016/S0140-6736(21)02758-6
Keywords: COVID-19, Omicron variant, containment strategy, mitigation strategy, national response
Citation: Jiao J, Shi L, Chen H, Wang X, Yang M, Yang J, Liu M and Sun G (2023) Critical national response in coping with Omicron variant in China, Israel, South Africa, and the United States. Front. Public Health. 11:1157824. doi: 10.3389/fpubh.2023.1157824
Edited by:
Ranjan K. Mohapatra, Government College of Engineering, Keonjhar, IndiaReviewed by:
Dhruv Desai, University of Pennsylvania, United StatesL. V. Simhachalam Kutikuppala, Konaseema Institute of Medical Sciences and Research Foundation (KIMS&RF), India
Copyright © 2023 Jiao, Shi, Chen, Wang, Yang, Yang, Liu and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gang Sun, c3VuaG9uZXkxNjNAMTYzLmNvbQ==; Z3N1bjE1QGpodS5lZHU=
 Jun Jiao
Jun Jiao Leiyu Shi2
Leiyu Shi2 Junyan Yang
Junyan Yang Meiheng Liu
Meiheng Liu Gang Sun
Gang Sun