- 1Department of Family Medicine, Taipei and Linkou Main Branches, Chang Gung Memorial Hospital, Taoyuan, Taiwan
- 2Metabolism and Obesity Institute, Taipei and Linkou Main Branches, Chang Gung Memorial Hospital, Taoyuan, Taiwan
- 3Department of Industrial Engineering and Manage-ment, National Taipei University of Technology, Taipei, Taiwan
- 4College of Medicine, Chang Gung University, Taoyuan, Taiwan
- 5School of Medicine, National Tsing Hua University, Hsinchu, Taiwan
- 6Department of Pediatrics, Linkou Main Branch, Chang Gung Memorial Hospital, Taoyuan, Taiwan
- 7Department of Pulmonary and Critical Care Medicine, Linkou Main Branch, Chang Gung Memorial Hospital, Taoyuan, Taiwan
- 8Sleep Center, Linkou Main Branch, Chang Gung Memorial Hospital, Taoyuan, Taiwan
- 9Department of Otorhinolaryngology – Head and Neck Surgery, Linkou Main Branch, Chang Gung Memorial Hospital, Taoyuan, Taiwan
- 10Department of Child Psychiatry, Linkou Main Branch, Chang Gung Memorial Hospital, Taoyuan, Taiwan
- 11Department of Psychiatry, Taipei Veter-ans General Hospital, Taipei, Taiwan
- 12Institute of Brain Science, National Yang Ming Chiao Tung University, Taipei, Taiwan
- 13Faculty of Medicine, National Yang-Ming University, Taipei, Taiwan
- 14Department of Otolaryngology, Ren-Ai Branch, Taipei City Hospital, Taipei, Taiwan
- 15Tsaotun Psychiatric Center, Ministry of Health and Wel-fare, Nantou, Taiwan
- 16Sleep Research Center, National Yang Ming Chiao Tung University, Taipei, Taiwan
Background: Dietary behavior is a main contributing yet modifiable factor to the body weight status of children and may be involved in the pathophysiology of childhood obstructive sleep apnea (OSA). This study aimed to investigate the dietary profile of pediatric OSA patients, effects of educational counseling after adenotonsillectomy, and predictor for disease resolution.
Methods: This observational study included 50 pediatric OSA patients undergoing adenotonsillectomy with routine educational counseling (Group 1), 50 pediatric OSA patients undergoing adenotonsillectomy without formal educational counseling (Group 2), and 303 healthy children without OSA (Control). The three groups were matched by age. The consumption frequency of 25 food items/groups was assessed by the Short Food Frequency Questionnaire. Quality of life was evaluated by the OSA-18 questionnaire. Sleep architecture and OSA severity were measured by standard polysomnography. Between- and within-group comparisons were analyzed by non-parametric approaches and generalized estimating equations. Prediction of disease recovery was performed by multivariable logistic regression models.
Results: Group 1 children consumed fruit drinks with sugar, vegetables, sweets, chocolate, rice, and noodles more frequently than Control Group children. At baseline, the distributions of sex, weight status, OSA-18 scores, and polysomnographic variables were comparable between Group 1 and Group 2. After a 12-month follow-up, Group 1 had better improvements in physical suffering, caregiver concerns, sleep architecture, and mean peripheral oxygen saturation compared to Group 2. Furthermore, Group 1 no longer had excessive consumption of fruit drinks with sugar, chocolate, and noodles; however, food consumption frequencies did not change significantly. Notably, younger age and reduced intake of butter/margarine on bread and noodles were independent predictors of cured OSA in Group 1.
Conclusion: The present study preliminarily characterized an unhealthy dietary profile among pediatric OSA patients and suggested that routine educational counseling in addition to adenotonsillectomy yielded some clinical benefits. Certain items/groups of food frequencies may be associated with disease recovery and further investigations are warranted.
1. Introduction
Obstructive sleep apnea (OSA) is one of the most common sleep disorders in children, with a prevalence of approximately 4% worldwide (1). In addition to snoring and abnormal breathing during sleep, childhood OSA can be comorbid with many diseases, such as obesity (2), metabolic syndrome (3), cardiovascular disease (4), and attention-deficit/hyperactivity disorder (5). Hypertrophy of the adenoid and tonsils and overweight/obesity are frequently encountered in pediatric OSA patients (6–8). Adenotonsillectomy remains the first-line treatment for childhood OSA (6, 9). However, residual OSA after adenotonsillectomy (defined by a postoperative apnea-hypopnea index [AHI] ≥ 1.0 events/h) is not uncommon, accounting for 49% of the overall adenotonsillectomy-treated pediatric OSA patients and 66% of those with obesity (10). Furthermore, age and obesity are two well-recognized risk factors for residual disease after adenotonsillectomy among pediatric OSA patients (8, 11, 12). Although residual OSA does not necessarily represent a treatment failure, efforts are underway to identify successful strategies for curing OSA.
Evidence has indicated negative impacts of inadequate or poor-qualitied sleep on weight status and metabolic prolife (13–15). Preadolescents with longer sleep duration had lower body fat percentage and better insulin sensitivity (16). Sleep restriction increases levels of ghrelin, the “hunger hormone” which promotes appetite and stimulates eating (17). Food intake following sleep restriction contains an average of 328 more calories, primarily from carbohydrates (17). Sleep duration reduction, poor sleep quality, and circadian rhythm dysregulation can all lead to insulin resistance, a cardinal pathway to the development of metabolic syndrome and type 2 diabetes (18). Some study also suggests that lack of sleep has a direct negative effect on physical activity (19). Despite still some knowledge gap in pathophysiology, it has been quite evident that insufficient or bad sleep leads to weight gain and metabolic deterioration.
Intriguingly, albeit a significant improvement in sleep quality, pediatric OSA patients are likely to increase their body mass index (BMI) z-score (20) after adenotonsillectomy. Furthermore, the velocity and amount of weight gain in turn becomes independent risk factors for OSA recurrence in children (21). Some specific foods have been associated with excessive weight gain among children and adolescents, such as butter/margarine spread, potato chips, coated fish, processed meats, desserts and sweets, milk, and savory snacks (22). Increases in caloric and protein intake also have been linked to somatic growth in this population (20). Multidisciplinary weight loss interventions have been shown to improve the severity of OSA in children and adolescents with obesity (23). However, the relationships between OSA and eating behavior remain unclear in adults (24), and data for pediatric OSA patients are even scantier (25). Evidence on the effectiveness of educational counseling is lacking. The associations of baseline characters or changes in dietary behavior with OSA treatment outcomes are unknown.
We hypothesized that pediatric OSA patients were more prone to unhealthy eating, and educational counseling would have positive effects on their dietary behavior and clinical health outcomes; furthermore, changes in eating were causally attributable to changes in subjective and objective sleep parameters after adenotonsillectomy. This study aimed to: (1) delineate the dietary profile of pediatric OSA patients and compare it to children without OSA, (2) investigate the effects of educational counseling on food consumption and sleep outcomes among pediatric OSA patients undergoing adenotonsillectomy, and (3) identify predictors for cured OSA in patients receiving combined treatment.
2. Materials and methods
2.1. Study participants
The retrospective case–controlled study retrieved data from our previously established databank (26), a collection of electronic medical records of 396 children who were referred to the Department of Otorhinolaryngology-Head and Neck Surgery at Chang Gung Memorial Hospital (Linkou Main Branch, Taoyuan, Taiwan) to treat OSA between January 2010 and August 2019. This retrospective study was approved by the Institutional Review Board of Chang Gung Medical Foundation (No. 202000873B0). The requirement for written informed consent had been waived because the subsequent analyses were based on existing data. All procedures complied with the Declaration of Helsinki 1975, and the Strengthening the Reporting of Observational Studies in Epidemiology—Nutritional Epidemiology guidelines were followed (27). Parts of the subjects’ characteristics have also been reported elsewhere (7, 8, 28–31).
The inclusion criteria of this study were: (1) age 5–12 years, (2) available polysomnography confirming the diagnosis of OSA based on the definition of obstructive AHI ≥ 2.0 events/h or obstructive apnea index ≥1.0 event/h (8, 32), and (3) a history of adenotonsillectomy at our department during the study period. The exclusion criteria were: (1) patients with craniofacial, neuromuscular, or chronic inflammatory disorders that required multi-modality treatments (28, 33), and (2) those with no available data of item/group-specific food frequencies, quality of life, or polysomnographic data at baseline and 6 months post-adenotonsillectomy.
The subjects were further divided into ‘Group 1’ (adenotonsillectomy with routine educational counseling) and ‘Group 2’ (adenotonsillectomy without formal educational counseling). Furthermore, Group 1 and Group 2 participants were matched by age, sex, BMI z-score, AHI, and follow-up period.
To compare the dietary profiles of the study participants to the general population, we included data from a prospective internet survey investigating item/group-specific food frequencies among healthy Taiwanese children without obvious OSA symptoms. We invited parents and caregivers who had children without habitual snoring to evaluate their children’s food frequencies from November 24, 2022, to November 30, 2022. The inclusion criteria were: (1) age 5–12 years, (2) no obvious OSA symptoms such as habitual snoring, sleep-disturbed breathing, chronic mouth breathing, daytime sleepiness, and attention-deficit/hyperactivity, and (3) total score of the OSA-18 questionnaire <60 (34). The exclusion criteria were: (1) any known history of chronic disorders such as neuromuscular, gastrointestinal, or cardiovascular disorders, and (2) any long-termed usage of medications. All participants filled in the questionnaire voluntarily without any incentive offered. The Institutional Review Board of Chang Gung Medical Foundation approved this internet survey (No. 202201649B0), and the anonymous volunteers (children’s parents/caregivers) agreed to participate after reading the informed consent.
2.2. Measurements
2.2.1. Clinical information
Age, sex, tonsil size, adenoidal-nasopharyngeal ratio (ANR), and BMI z-score were recorded. Obesity was defined by a BMI z-score ≥ 1.645 (35). Radical adenotonsillectomy procedures, including extracapsular tonsillectomy and adenoidectomy, were performed by the principal investigators in a single stage under general anesthesia (36). All the children received inpatient care with an average hospitalization of 3 days and ate a regular diet within 2 weeks.
2.2.2. Food frequency
All caregivers recorded the consumption frequency of 23 food items in their children using the Short Food Frequency Questionnaire (SFFQ) (37). Nine questions of the SFFQ pertain to drinks, including full-fat milk, low-fat milk (1.5% fat), semi-skimmed milk (0.7% fat), skimmed milk, orange juice, fruit drinks and soft drinks with or without sugar. The SFFQ also contains questions on each of the following food items or food groups: potatoes, vegetables, fruit/berries, potato chips, whole meal bread, fish for dinner (not including bread spread), pizza, hamburgers/hot dogs/kebabs, sweets, chocolate, savory snacks, peanuts and cod liver oil/vitamin supplements, and an additional question on the use of butter/margarine on bread. In addition, two Chinese food items (rice and noodles) were also investigated in the present study. The participants and their caregivers were asked to recall their food habits in the past 1 month and filled in the questionnaire together. The frequency scale used for drinks was 0 (never-seldom), 1 (1–3 glasses per month), 2 (1–3 glasses per week), 3 (4–6 glasses per week), 4 (1–3 glasses per day), 5 (4–6 glasses per day), and 6 (7 glasses or more per day). Half a liter was defined as being equal to 3 glasses. For other foods, the frequency scales were 0 (never-seldom), 1 (1–3 times per month), 2 (1–3 times per week), 3 (4–6 times per week), 4 (1 time per day), 5 (2 times per day), 6 (3 times per day), and 7 (4 or more times per day). The question about the use of butter/margarine on bread was answered with 1 (yes) or 0 (no). The reproducibility of the 23 food items/groups of the SFFQ ranged from moderate to almost perfect (intraclass correlation coefficients: 0.58–0.84) (38) with moderate test–retest reliability (39). It has been validated to rank children according to food item/group intake (38), dietary behaviors (40, 41), and adherence to dietary guidelines (42).
2.2.3. Quality of life
All caregivers evaluated their children’s OSA-related quality of life using the Chinese version of the OSA-18 questionnaire (43), which includes 18 items scored using a 7-point ordinal scale (overall range, 18–126) and has been shown to have excellent test–retest reliability (34). This questionnaire collected information about five domains that are considered to be elements in the quality of life: sleep disturbance (4 items), physical suffering (4 items), emotional distress (3 items), daytime problems (3 items), and caregiver concerns (4 items).
2.2.4. Polysomnography
All participants underwent full-night, in-laboratory polysomnography (Nicolet Biomedical Inc., Madison, WI, United States) to document objective sleep characteristics (33). Total sleep time, sleep stages, AHI, apnea index, arousal index, mean peripheral oxygen saturation (SpO2), and minimal SpO2 were scored and manually verified by the study investigators, according to the 2012 American Academy of Sleep Medicine Scoring Manual (44). An apnea episode was defined as a ≥ 90% decrease in airflow for a duration of ≥2 consecutive breaths, and a hypopnea episode was defined as a ≥ 30% decrease in airflow in association with electroencephalographic arousal or a ≥ 3% reduction in SpO2 for a duration of ≥2 consecutive breaths. The AHI was calculated by dividing the sum of all apneas and hypopneas by the hours of total sleep time. Herein, ‘cured OSA’ was defined as a reduction in both obstructive AHI < 2.0 events/h and obstructive apnea index <1.0 event/h after adenotonsillectomy and/or educational counseling (32).
2.3. Routine educational counseling
Each child of Group 1, who had been enrolled in our previous study [CMRPG3F1091-3, approved by the Institutional Review Board of Chang Gung Medical Foundation (No. 201507279A3), study period 2016–2019] (8, 28), received three sessions of age-appropriate educational counseling within 3 months after adenotonsillectomy. The children and their caregivers were given verbal recommendations for sleep hygiene (adequate sleep, early sleep, avoid caffeine after lunchtime, avoid large meals or vigorous physical activity before bedtime), healthy eating [limit sweetened beverages, eat less fast food, recommend the Daily Dietary Guidelines of Taiwan for children as a reference material (45)], regular exercise (increase outdoor/after-school exercise, exercise training), and nasal saline irrigation (46). Each session of educational counseling was conducted face-to-face for 10–15 min by the research investigators and assistants.
2.4. Statistical analysis
Data were analyzed using G*Power 3.1.9.2 (Heinrich-Heine University, Dusseldorf, Germany), SPSS version 25.0 (IBM Corp., Armonk, NY, United States), and GraphPad Prism 9.0 for Windows (Graph Pad Software Inc., San Diego, CA, United States). The Shapiro–Wilk test was used to examine normality, which showed that most of the continuous variables of interest were non-parametric. Therefore, descriptive statistics were expressed as median (interquartile range [IQR]) for continuous and skewed variables and number (proportion) for categorical variables.
Based on a previous study (47), we applied fruit frequency to estimate the sample size. The modal scores of fruit consumption in healthy children without OSA (n = 177), pediatric OSA patients without obesity (n = 25), and pediatric OSA patients with obesity (n = 43) were 3–5 times/week, 3–5 times/week, and 1–2 times/week, respectively (Kruskal-Wallis test of variance by ranks, H(2245) = 7.0, p = 0.03). To compare the difference between healthy children without OSA and pediatric OSA patients, we estimated the weighted modal score of pediatric OSA patients. To reach 95% power with a type I error of 0.05, the total sample size would be 38. However, the investigation was powered to detect item/group-specific food frequencies as low as 0% reliably; we estimated the absence of item/group-specific food frequencies among 300 children would generate a one-sided 97.5% confidence interval between 0 and 0.99% (48).
For continuous and skewed variables, the Mann–Whitney U test was used to assess between-group differences and changes, and the Wilcoxon signed-rank test was used to assess within-group changes, as appropriate. Differences in independent categorical variables between two subgroups were analyzed using Fisher’s exact test, and differences in related categorical variables within groups were assessed using the McNemar test. Relationships between variables of interest were assessed using Spearman and point-biserial correlation tests, as appropriate.
Multivariable logistic regression models, including variables with a p-value < 0.200 (49), with manual selection based on a probability of F < 0.05 were used to identify independent variables for predicting cured OSA using a parsimonious approach. The variance inflation factor (VIF) of each predictor was calculated to adjust for intervariable relationships within the model. The regression model was repeated after removing all variables with a VIF ≥ 5 to reduce multicollinearity (50).
To compare differences in the changes of outcome variables by post-intervention OSA status, generalized estimating equations with adjustments for pre-intervention age, sex, and obesity were used. Specifically, each subgroup variable was entered into separate generalized estimating equations that included the main effects of time (post-intervention vs. pre-intervention) and subgroup variable (e.g., boy vs. girl), a two-way interaction term of time × subgroup variable, and the main effects of baseline characteristics. A two-sided p-value of <0.05 was considered statistically significant.
3. Results
3.1. Groups of the study and between-group comparisons
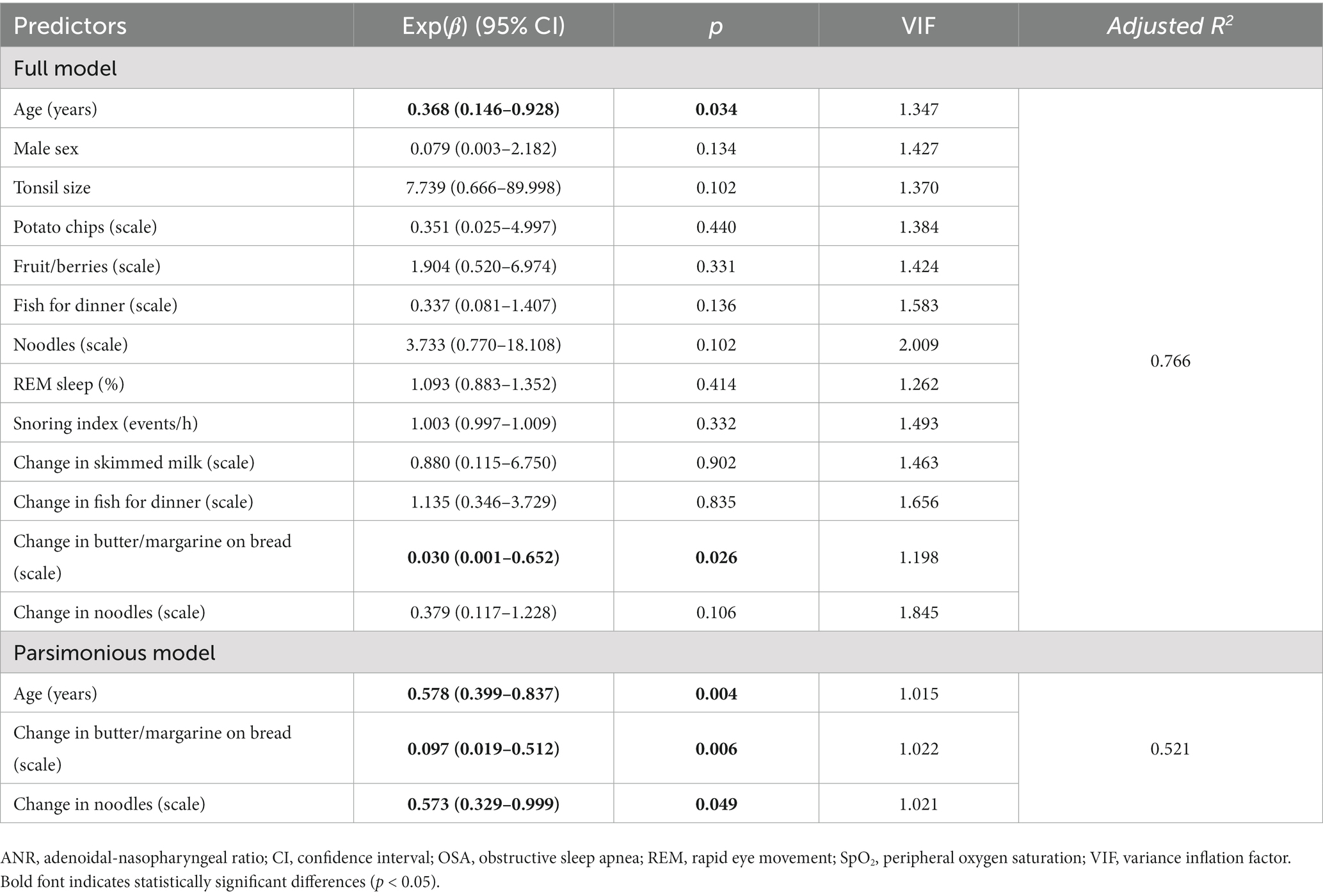
Figure 1 demonstrates the flowchart of the present study. Fifty pediatric OSA patients (38 [76%] boys and 12 [24%] girls) with a median (IQR) age of 7.0 (5.8–10.0) years undergoing adenotonsillectomy with routine educational counseling (Group 1), 50 pediatric OSA patients (40 [80%] boys and 10 [20%] girls) with a median age of 7.4 (5.9–10.3) years undergoing adenotonsillectomy without formal educational counseling (Group 2), and 303 healthy children without obvious OSA symptoms (Control Group) were included for further analysis.
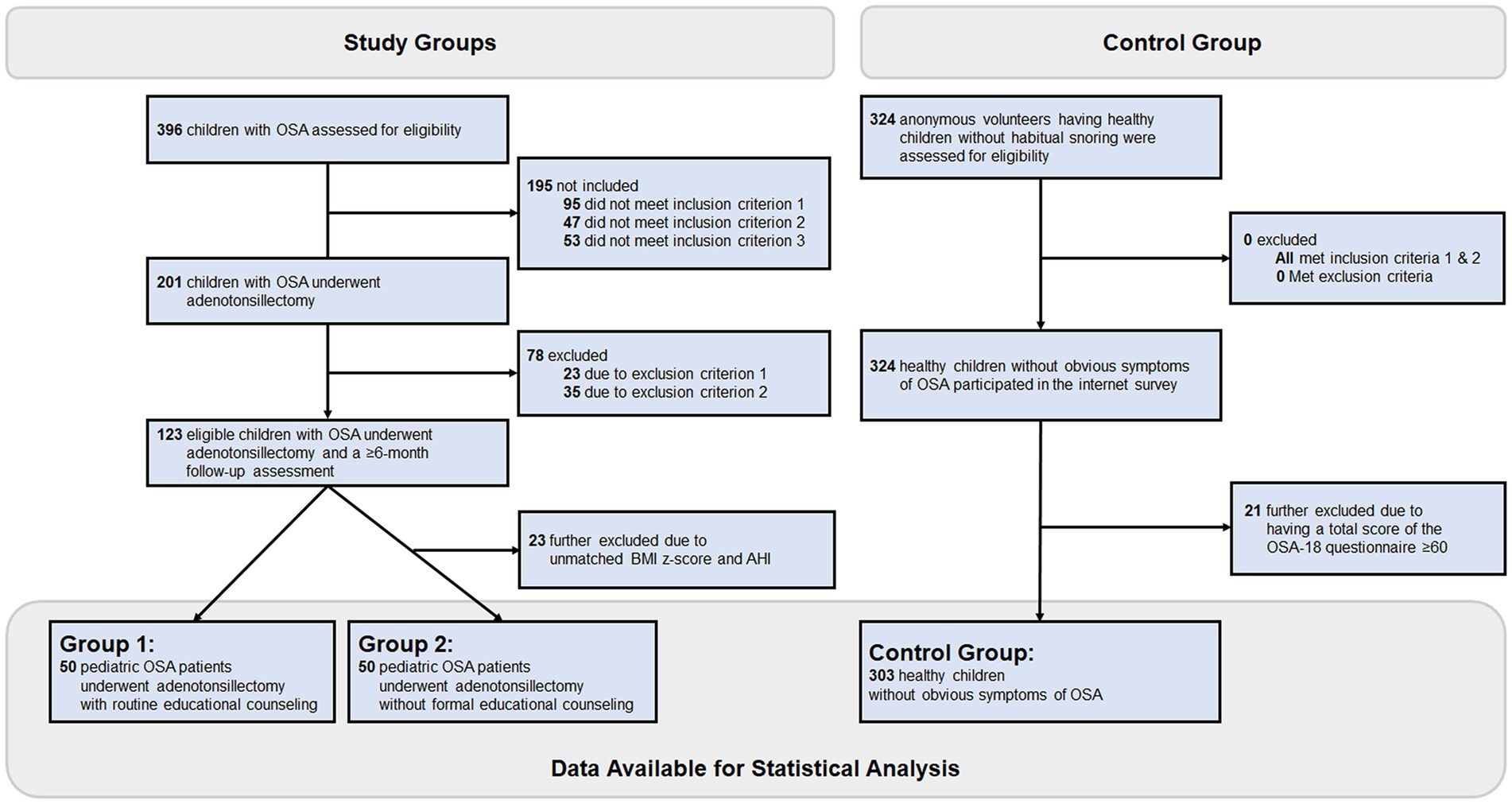
Figure 1. Flowchart of this observation study. Two-hundred one of 396 eligible children with OSA met the inclusion criteria of the study groups. Among them, 78 were excluded due to the exclusion criteria, and 23 were further excluded due to being unmatched by the AHI and BMI z-score between Group 1 (adenotonsillectomy with routine educational counseling) and Group 2 (adenotonsillectomy without formal educational counseling). Besides, 324 anonymous volunteers having healthy children without habitual snoring met the inclusion and exclusion criteria of the control group, and 21 were further excluded due to having a total score of the OSA-18 questionnaire ≥60. After that, the Control Group included 303 children without obvious OSA symptoms. AHI, apnea-hypopnea index; BMI, body mass index; OSA, obstructive sleep apnea.
The Control Group in total had 303 healthy children (159 [52%] boys and 144 [48%] girls; median total OSA-18 score of 35 [28–43]), consisting of 45 (14.9%) 5-year-old, 44 (14.5%) 6-year-old, 39 (12.9%) 7-year-old, 43 (14.2%) 8-year-old, 38 (12.5%) 9-year-old, 45 (14.9%) 10-year-old, and 49 (16.2%) 11-year-old children. The median scores of sleep disturbance, physical suffering, emotional distress, daytime problems, and caregiver concerns of the OSA-18 questionnaire of the Control Group were 6 (5–8), 8 (5–11), 7 (4–9), 6 (4–9), and 7 (4–9), respectively. The difference in age between Group 1 and the Control Group was not significant (p = 0.161); however, the proportion of boys in Group 1 was significantly higher than that of the Control Group (p = 0.002). Because scores of the OSA-18 questionnaire and scales of the SFFQ questionnaire between boys and girls were comparable in Group 1 and Control Group, we did not perform further weighting procedures in the following statistical analyses.
Table 1 shows item/group-specific food frequencies in Group 1 (at baseline and post-adenotonsillectomy) and Control Group (at base line). In Group 1, the most consumed drinks in descending order of frequency were full-fat milk, orange juice and fruit drinks with sugar. The main consumed foods in descending order of frequency included vegetables, rice, fruit/berries, noodles, fish for dinner, and sweets. In the Control Group, all item/group-specific food frequencies between boys and girls were comparable. The most consumed drinks were full-fat milk, fruit drinks with sugar and soft drinks with sugar. The main items/groups of other foods included vegetables, rice, fruit/berries, fish for dinner, savory snacks, and noodles. In addition, Group 1 children ate fruit drinks with sugar, vegetables, sweets, chocolate, rice, and noodles more frequently than the Control Group children did. However, Group 1 children’s daily consumption of vegetables and fruit/berries were significantly lower than those of Taiwanese children aged 7–12 years (vegetables: 1.8 times/day; fruits: 1.0 time/day) (p = 0.013 and < 0.001, respectively) (51).
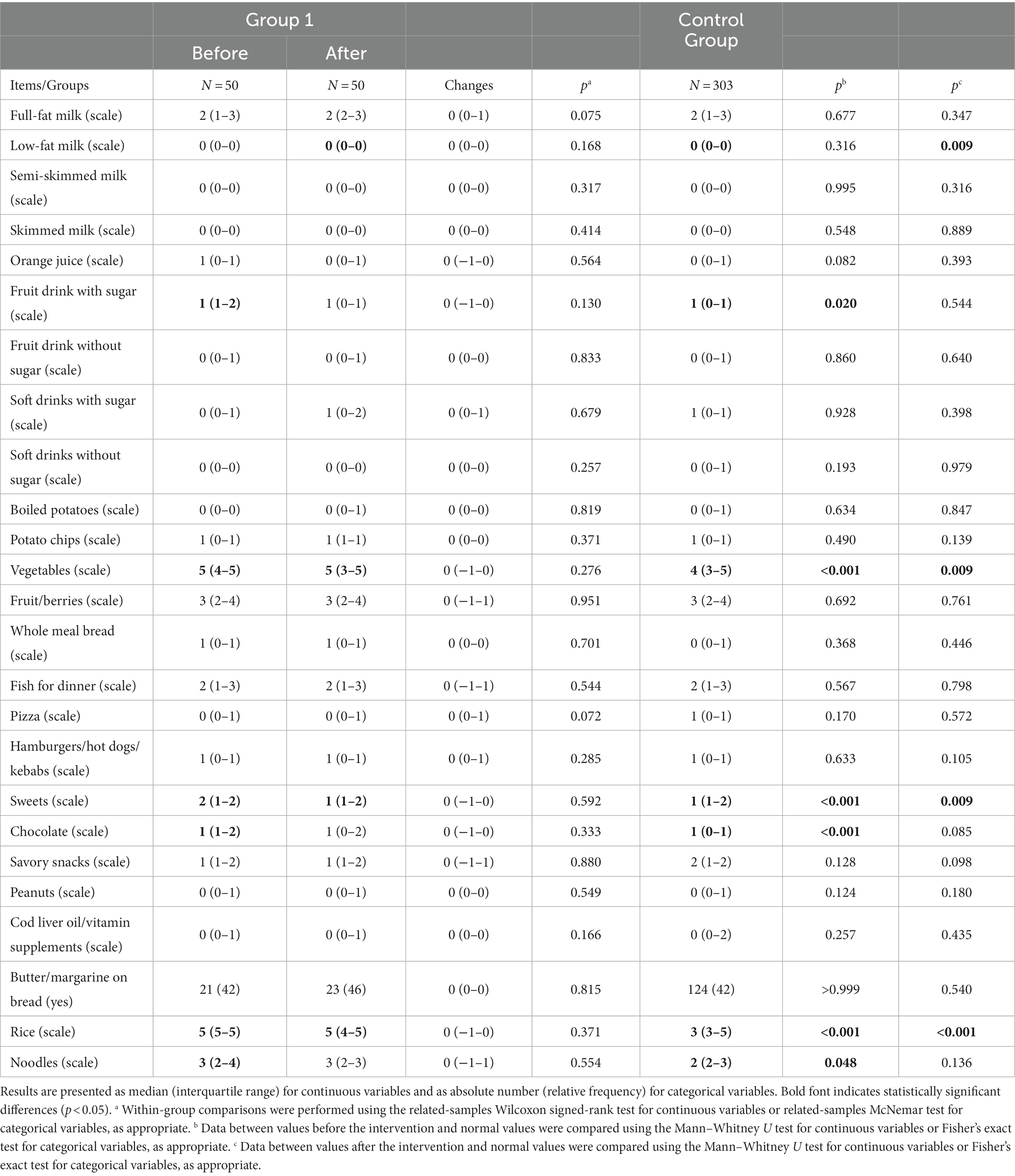
Table 1. Item/group-specific food frequencies in Group 1 (at baseline and post-intervention) and Control Group (baseline).
Table 2 shows patient characteristics, scores of the OSA-18 questionnaire, and polysomnographic variables of Group 1 and Group 2 at baseline and post-adenotonsillectomy ≥6 months. At baseline, all variables were comparable between the two groups. The median scores of sleep disturbance, physical suffering, emotional distress, daytime problems, caregiver concerns, and total scores of the OSA-18 questionnaire of Group 1 and Group 2 (Table 2) were significantly higher than those of the Control Group.
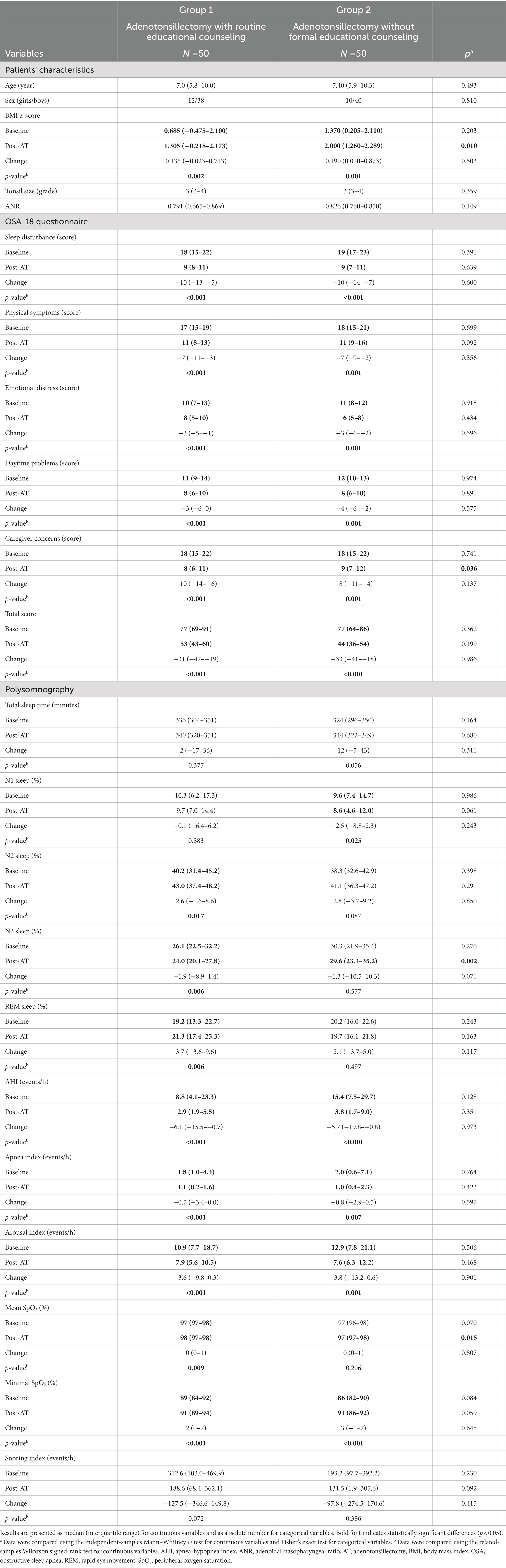
Table 2. Demographic metrics and sleep variables of Group 1 and Group 2 at baseline and post-intervention ≥6 months.
The median follow-up time of Group 1 (12 [IQR, 12–15] months) and Group 2 (15 [IQR, 8–17] months) were comparable (p = 0.950).
After adenotonsillectomy, BMI z-scores of both Groups 1 and 2 significantly increased. The follow-up BMI z-score of Group 1 was significantly lower than that of Group 2. Both Group 1 and Group 2 had significantly reduced scores in five domains and total scores on the OSA-18 questionnaire (Table 2). The follow-up score of caregiver concerns of Group 1 was significantly lower than that of Group 2. Follow-up scores of physical suffering (p = 0.057), emotional distress (p = 0.569), and caregiver concerns (p = 0.219) of Group 1 were comparable to those of the Control Group; however, scores of sleep disturbance (p < 0.001) and daytime problems (p = 0.007), and total scores (p < 0.001) of Group 1 were still significantly higher than those of the Control Group. Follow-up scores of sleep disturbance (p < 0.001), physical suffering (p = 0.001), daytime problems (p = 0.016), and caregiver concerns (p = 0.001), and total scores (p = 0.001) were significantly higher in Group 2 than in the Control Group, while follow-up scores of emotional distress were comparable between Group 2 and Control Group (p = 0.575).
After adenotonsillectomy, Group 1 patients had significantly higher proportions of N2 sleep and rapid eye movement (REM) sleep, mean SpO2 and minimal SpO2, and significantly lower proportion of N3 sleep, AHI, apnea index, and arousal index. Group 2 had significantly higher mean SpO2 and minimal SpO2, and significantly lower proportion of N1 sleep, AHI, apnea index, and arousal index. Group 1 had a significantly lower follow-up proportion of N3 sleep and a higher mean SpO2 than Group 2.
3.2. Within-group analysis and outcome prediction models in the Group 1
Figure 2 demonstrates several significant relationships between variables of interest in Group 1 at baseline. Notably, AHI was inversely related to chocolate, whereas the apnea index was inversely associated with noodles.
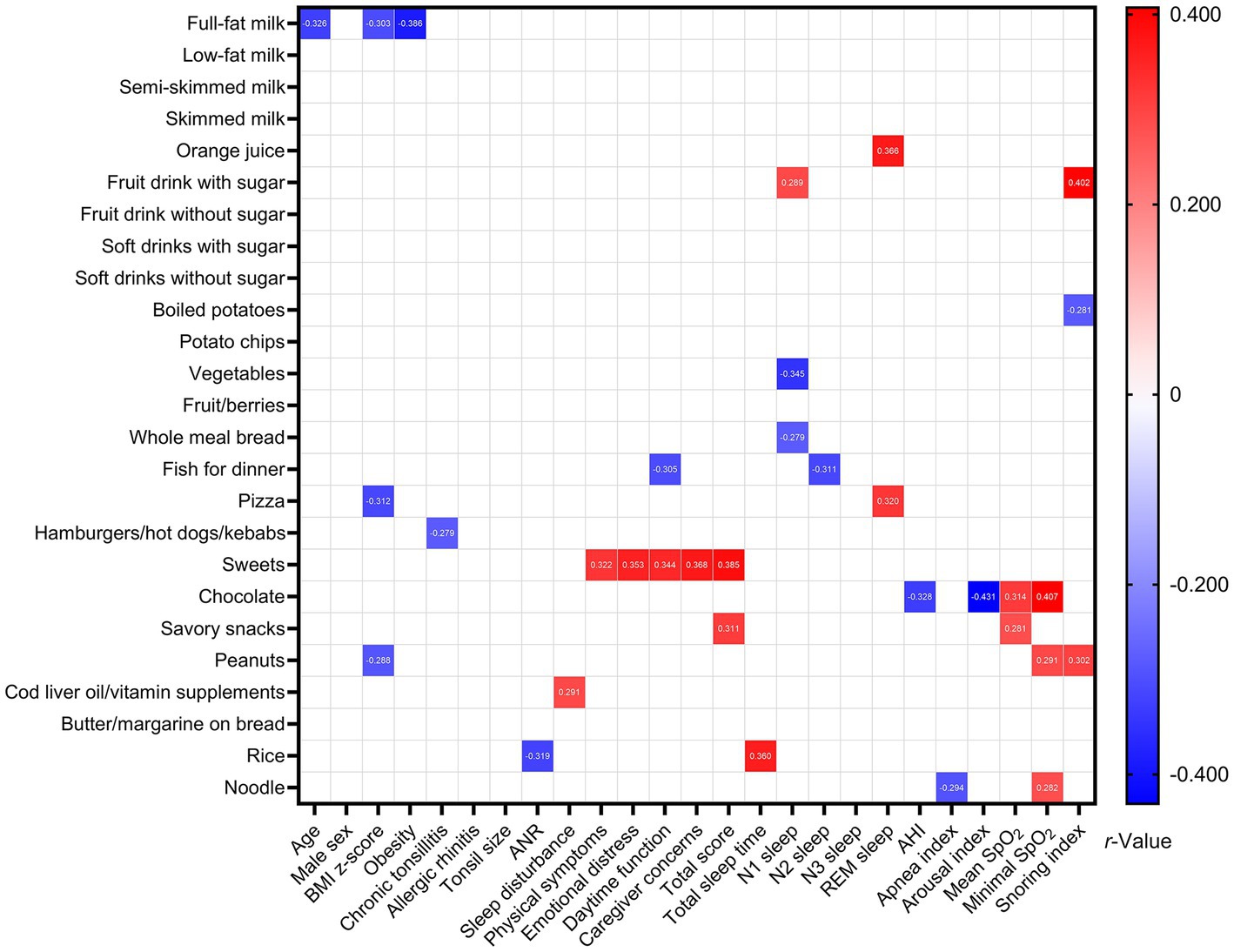
Figure 2. Associations between variables of interest among Group 1 at baseline. Data are summarized as Spearman’s or point-biserial rho, as appropriate. Blank spaces mean two-sided p-values ≥0.05.
Although post-adenotonsillectomy changes in item/group-specific food frequencies were not significant in Group 1, excessive consumption of fruit drinks with sugar, chocolate, and noodles no longer persisted (Table 1). However, Group 1 children drank low-fat milk and still ate vegetables, sweets, and rice more frequently than the Control Group children.
Twenty-five (50%) children had cured OSA, and 25 (50%) had residual OSA. The baseline characteristics of the two outcome subgroups are shown in Table 3. Notably, those with cured OSA were significantly younger than those who had residual OSA. The ANR of those with cured OSA was significantly higher than those who had residual OSA. Furthermore, the proportions of REM stage sleep, mean SpO2, and snoring index of those with cured OSA were significantly higher than those who had residual OSA. The rest of the variables of interest were comparable between the two outcome subgroups.
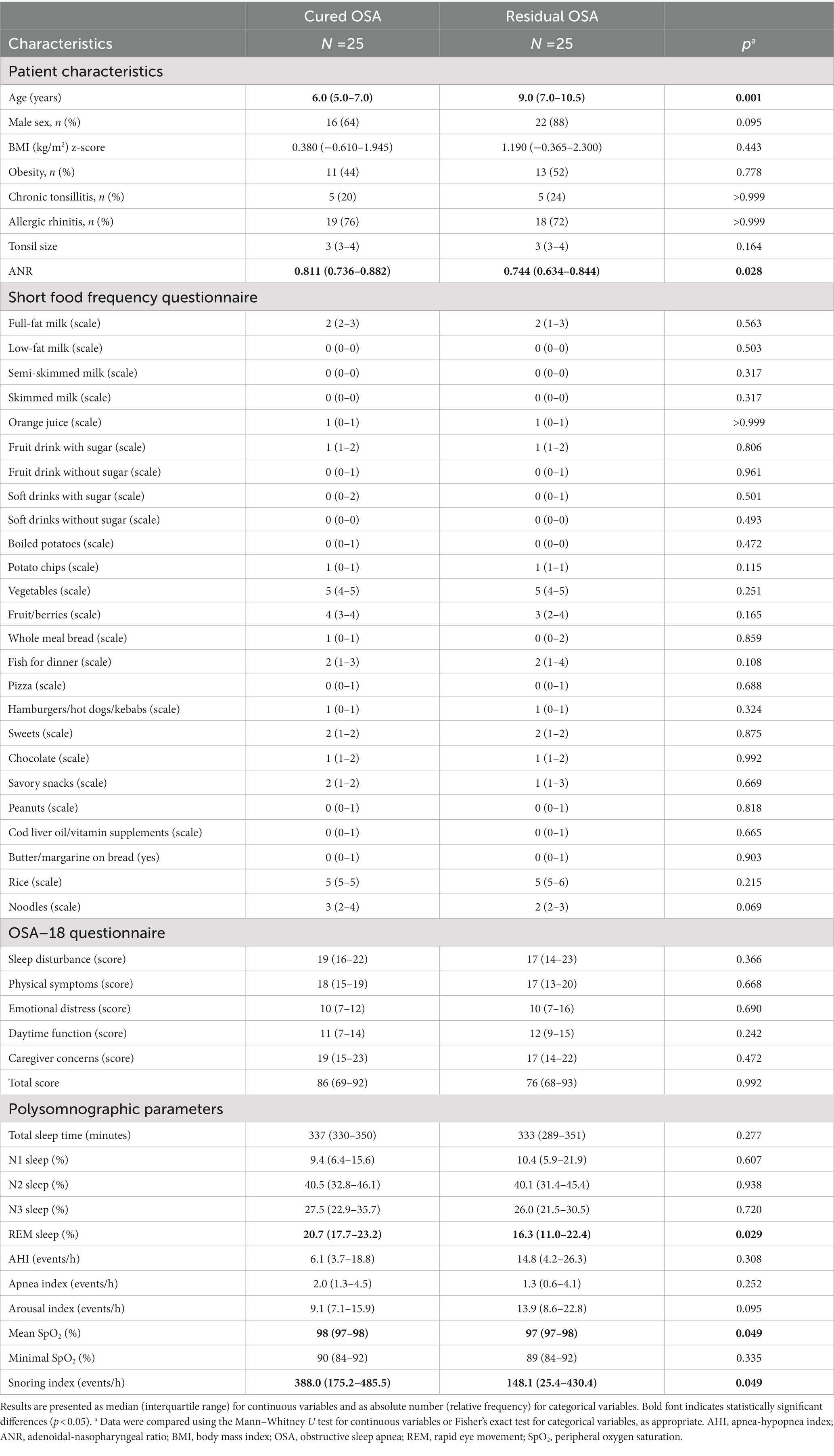
Table 3. Baseline characteristics of the children with cured OSA and those had residual OSA after intervention in Group 1.
After adjustments for baseline age, sex, and obesity (Table 4), the change in fish for dinner for those with cured OSA was significantly higher than for those with residual OSA. In addition, changes in noodles and REM sleep for those with cured OSA were significantly lower than those with residual OSA. The changes in butter/margarine on bread and snoring index between the two subgroups were no longer significant after adjustment. Furthermore, changes in other variables of interest were comparable between the two subgroups before and after adjustment.
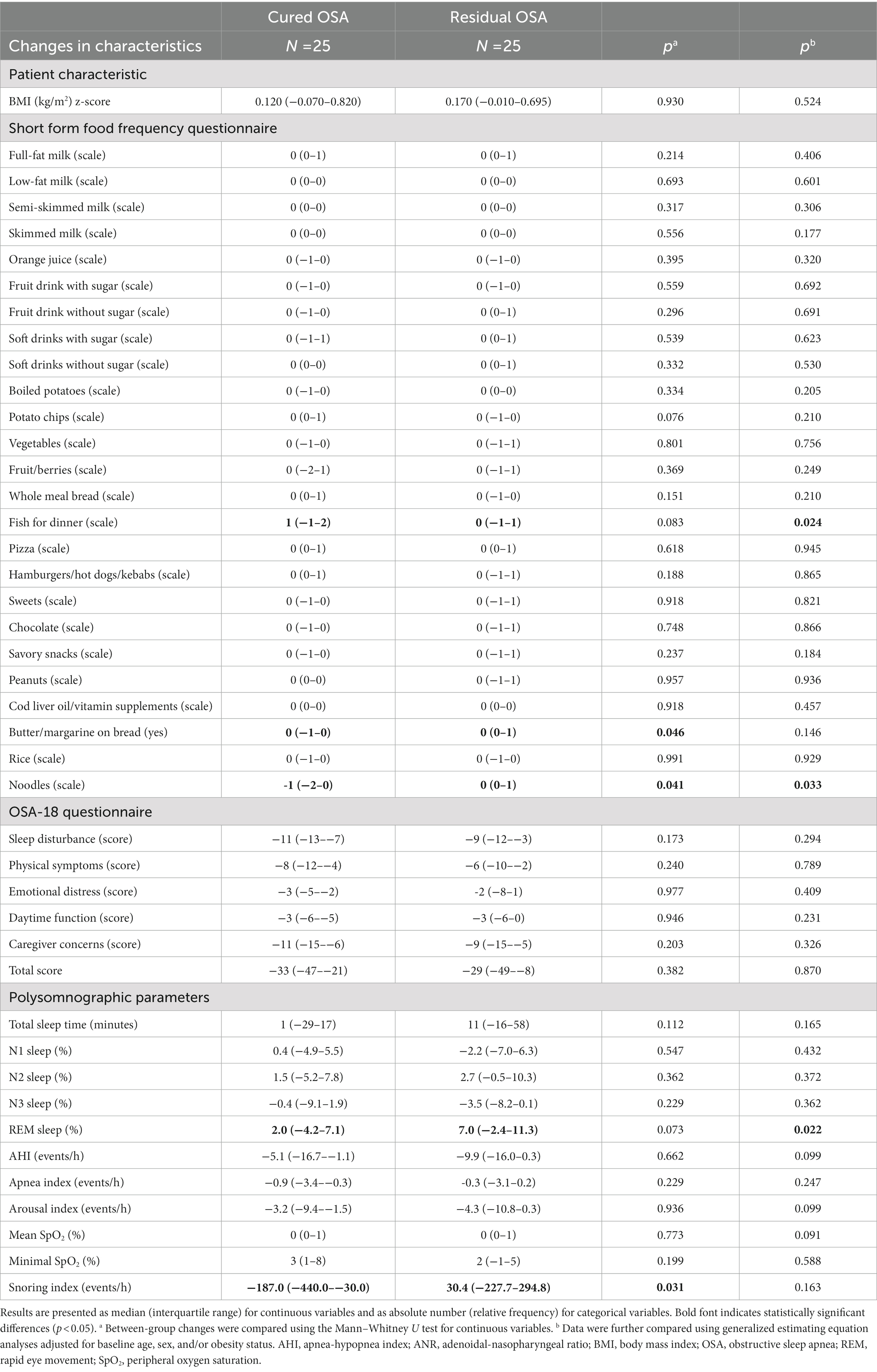
Table 4. Changes in the characteristics of the children with cured OSA and those had residual OSA after intervention in Group 1.
Significant associations were found between changes in SFFQ item/group scores and changes in BMI z-score, OSA-18 domain scores, and changes in polysomnographic parameters (Figure 3). Notably, change in AHI was inversely related to change in cod liver oil/vitamin supplements. Change in apnea index was inversely correlated with changes in fish for dinner and cod liver oil/vitamin supplements.
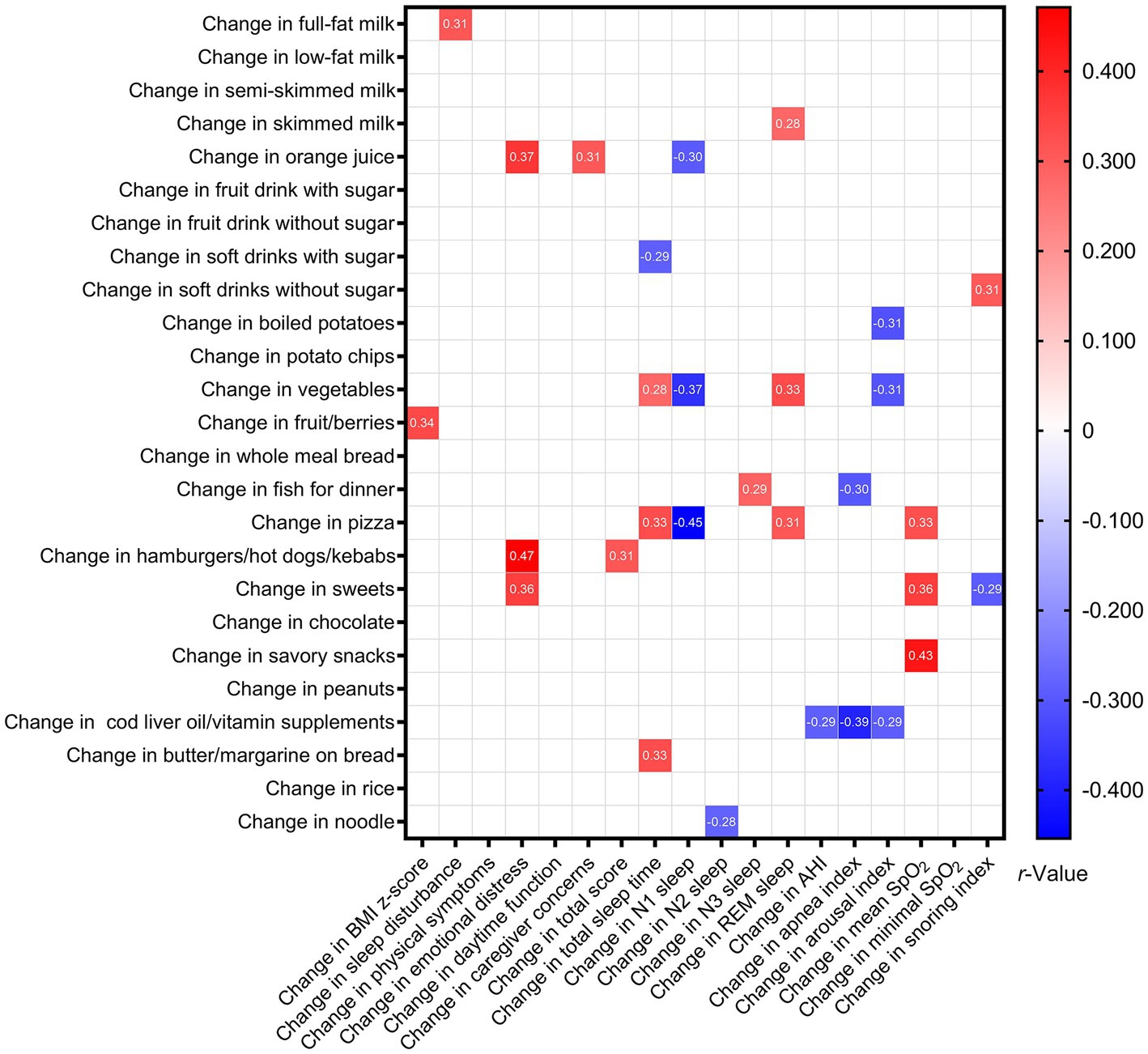
Figure 3. Associations between changes in variables of interest among Group 1 after intervention. Data are summarized as Spearman’s or point-biserial rho, as appropriate. Blank spaces mean two-sided p-values ≥0.05.
To construct prediction models for cured OSA, we included baseline variables with a p-value <0.200 (Tables 3, 4; not including changes in polysomnographic parameters), including age, male sex, tonsil size, ANR, potato chips, fruit/berries, fish for dinner, noodles, REM sleep, arousal index, mean SpO2, snoring index, change in skimmed milk, change in fish for dinner, change in butter/margarine on bread, and change in noodles in multivariable logistic regression analyses.
Table 5 summarizes the full model and the final parsimonious model to predict cured OSA. After removing variables with a VIF ≥ 5 (ANR, arousal index, mean SpO2), the full model identified age and change in butter/margarine on bread as independent predictors under the control of male sex, tonsil size, potato chips, fruit/berries, fish for dinner, noodles, REM sleep, snoring index, change in skimmed milk, change in fish for dinner, and change in noodles. The parsimonious model (including baseline clinical variables and changes in food items/groups) identified age, change in butter/margarine on bread, and change in noodles as the best predictors of cured OSA.
4. Discussion
The current study demonstrated several novel and interesting findings on the dietary profiles of pediatric OSA patients, their differences compared to healthy children without OSA, the effectiveness of routine educational counseling, and predictors for cured OSA among patients receiving combined treatment.
The most commonly consumed food items/groups among pediatric OSA patients were full-fat milk, vegetables, rice, fruit/berries, noodles, fish for dinner, and sweets, and they had fruit drinks with sugar, vegetables, sweets, chocolate, rice, and noodles more frequently than the healthy control did. Daily fruit/berry consumptions in Group 1 and the Control Group were lower than the Taiwanese recommendation (3.5 servings per day) (37, 45). This is not uncommon in Taiwan; although healthy Taiwanese children have a higher median daily vegetable consumption than that of normal Norwegian children (37), the value is still lower than the recommendation (4–5 servings per day) from the Daily Dietary Guidelines of Taiwan for children aged 7–12 years (45). Likewise, Taiwanese children in general drink less full-fat milk than the recommended (1.5 glasses of milk/day) (45). Some child caregivers of our subjects reported that they reduced full-fat milk consumption and replaced it with low-fat milk to lower the risk of childhood obesity. The impacts of dairy foods and their low-fat products on cardio-metabolic health are still controversial, called the “dairy fat paradox” (52). Vanderhout et al. demonstrated that higher cow milk fat intake was related to lower childhood adiposity in a meta-analysis (53). However, most previous research focused on cardiovascular diseases, metabolic syndrome, or weight status as study outcomes; the role of full-fat milk consumption in pediatric OSA is still unclear and needs further investigation.
Consistent with Spruyt’s study (47), the pediatric OSA patients with obesity in the present study ate more fast food and less healthy food, such as vegetables and fruits, than the children without OSA. Elevated ghrelin levels are positively associated with OSA, increased appetite and caloric intake in children with obesity (47). On the contrary, more frequent fruit consumption has been correlated with healthy sleep, including shorter nap duration (54) and long sleep duration in children (55). Our data combined with the literature indicated that education on healthy eating, such as more vegetable/fruit intake and less fast food, needs to be addressed more intensively among children in Taiwan, especially for pediatric OSA patients. The literature indicates that longer, better, and more regular sleep links to lower adiposity and better metabolic health (16). The educational counseling delivered in this study focused firstly on sleep hygiene, which was not only meant to directly improve the sleep and circadian rhythm of participants, but also the efforts in theory would have positive impacts on weight status and body composition. Moreover, the counseling promoted healthy eating and regular exercise, which were both well-documented effective methods to weight management (56).
Our data suggested that pediatric OSA patients receiving combined intervention might have additional treatment benefits other than solitary adenotonsillectomy. First, they had significantly increased N2 and REM sleep proportions and reduced N3 sleep proportion, which suggested a restoration of sleep architecture from disruption toward normal (57). Second, they had a significantly higher mean SpO2 meant, which suggested that the sleep hypoxemia status could be improved by not only surgical treatment but also approaches to lifestyle modification such as sleep hygiene, healthy eating, and regular exercise. However, as current evidence supports that weight reduction through lifestyle and dietary interventions can improve OSA severity in adults, our routine educational counseling did not show effectiveness on significant changes in dietary behavior, weight status, or OSA severity, indicating that more intensive lifestyle interventions are needed to yield more substantial clinical outcomes.
The full multivariable logistic regression model showed that younger age and decreased use of butter/margarine on bread were significant predictors of cured OSA under the control of possible confounding factors in the full model. Older age is a well-recognized risk factor for residual OSA after adenotonsillectomy in children, together with obesity and neurological/developmental/craniofacial comorbidities (8, 11, 12). Butter and margarine are used as spreads on bread and for cooking and baking. Butter is a dairy product generated from milk, containing approximately 80% milk fat and 16% water, and is rich in saturated fats, proteins, calcium, phosphorus, and some essential fat-soluble vitamins (A, D, E) (58). Among children and adolescents, butter/margarine spread is significantly related to excessive weight gain (22). Similar to patients with adulthood OSA, improper dietary habits (such as the frequent use of butter/margarine spread or as a source of fat for cooking) has been associated with body weight gain and OSA (59). Consistent with the literature, our results suggest that a reduction in butter/margarine on bread may help weight control and decrease the severity of childhood OSA.
Interestingly, the parsimonious model further included reduced noodle consumption in addition to younger age and reduced butter/margarine on bread for predicting cured OSA. Noodles are a staple food in Asian countries, and they are made from wheat flour, water, starch, and salt. One hundred grams of noodles have approximately 138 kcal, 2.07 g fat, 25.2 g carbohydrate, 4.54 g protein, 1.2 g fiber, 67.7 g water, and 5 mg sodium (60). Excessive consumption of noodles has been linked to overweight and obesity among school-aged children and adolescents (61), and a higher intake of instant noodles may increase the risk of short sleep duration and poor sleep quality in adolescents (62). To our best knowledge, this study was the first to reveal a significant association between the consumption of noodles and OSA in children. However, since the change in noodle consumption was not related to the change in AHI, we postulated that a reduction in noodle consumption might connect to cured OSA via indirect pathways such as weight reduction.
Somatic growth and weight gain are frequently observed after adenotonsillectomy in children with or without OSA (36, 63, 64). These observations may be explained by the improved retro-nasal olfactory function and consequently increased appetite after tonsil and adenoid removal (65). We conducted routine educational counseling for pediatric OSA patients in Group 1 to promote a healthy lifestyle. Some positive impacts were observed on sleep architecture, oxygenation, and undesirable eating habits. However, item/group-specific food frequencies did not change significantly after a 12-month follow-up, suggesting more intensive educational counseling was needed to yield profound change in food literacy. A multidisciplinary team, including family physicians, nurses, clinical dietitians, social workers, and administrative employees from schools, with a longer interventional duration, may be more effective (66). Besides, like multidisciplinary weight loss interventions in youth (10–19 years old) with obesity, educational counseling with more sessions (10–20 times) for a more extended period (4–12 months) may be more likely to result in improvement of clinical outcomes such as weight status and disease severity.
The greatest strength of this investigation was the inclusion of both a sample of representative and well-characterized pediatric OSA patients and a large sample of healthy children as the control. Furthermore, a long-term follow-up after adenotonsillectomy was completed for pediatric OSA patients. This design allowed a detailed description of diet behaviors across several factors, which we co-adjusted to identify independent associations with cured OSA. Nevertheless, these results need to be interpreted in consideration of some limitations. First, the completeness rate of Group 1 was lower than anticipated (76%), which might be attributed to the outbreak of COVID-19 in Taiwan during the study period. Second, a high degree of heterogeneity in the study groups might lead to increased type II errors due to a lack of statistical power (range: 36–99%), especially in comparing the intervention success group and the residual disorder group in Group 1. Third, the number of routine educational sessions conducted in our study was limited. As previously acknowledged, a larger number of sessions with an extended duration may be more effective in inducing substantial dietary modifications. Forth, although the SFFQ has been reported comparable to the four-day recoded food diary (regarding consumption frequencies and mean intake of food) and the 24-h dietary recall (regarding nutrients intake) (67), this western-country developed questionnaire may not be able to fully reflect the food literacy of Asian children. The lack of change in food frequencies could be a result of the ineffectiveness of the educational counseling, but it could also be due to methodological limitations. Furthermore, tastes/interests in young children vary frequently; other food frequency questionnaires with shorter intervals may reflect more recent diet habits without recall bias. Lastly, the role of sleep hygiene in food preferences, weight status, and OSA severity are not well-established and needs to be further delineated. Nevertheless, our preliminary findings warrant future investigations; a more intricate case–controlled study or a randomized controlled trial with a larger sample will be of interest.
In conclusion, the present study preliminarily characterized a relatively unhealthy dietary profile in pediatric OSA patients compared with the healthy control or the domestic daily dietary recommendations. The results showed that educational counseling in routine workups led to subjective and objective improvements in sleep outcomes after adenotonsillectomy; however, food consumption frequency was not changed substantially. Consumption frequently of certain food items/groups, including butter/margarine on bread and noodles, may be involved in the resolution of OSA after intervention. Given the potential beneficial effects of nutritional interventions on weight control and OSA amelioration, approaches including these item/group-specific foods could be a strategy for the comprehensive management of childhood OSA.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The study involving human participants was reviewed and approved by the Institutional Review Board of the Chang Gung Medical Foundation, Taoyuan, Taiwan (202000873B0 and 202201649B0). Written informed consent from the patients/participants legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
H-HC, R-HL, J-FH, and L-AL conceived and planned the study. H-HC, J-FH, L-PC, H-YL, Y-SH, and L-AL enrolled the patients. H-HC, R-HL, J-FH, Y-SH, AY, G-SL, TK, CY, and L-AL designed the study, analyzed the data, made the statistics, and interpreted the results. H-HC, R-HL, J-FH, L-PC, and L-AL participated in manuscript drafting. H-YL, T-JF, AY, G-SL, TK, and CY supervised the study. All authors read and approved the final manuscript.
Funding
This study was supported by the National Science and Technology Council, Taiwan (grant number 109-2314-B-182-083-MY3) and the Chang Gung Medical Foundation, Taiwan (grant numbers CMRPG3F1091-3 and CMRPG3L0811-2).
Acknowledgments
The authors would like to thank Ruo-Chi Wang and Chung-Fang Hsiao (Department of Otorhinolaryngology, Head and Neck Surgery, Linkou Chang Gung Memorial Hospital, Taoyuan City, Taiwan) for their technical assistance and the authors would like to thank I-An Jen (Department of Public Health, National Yang Ming Chiao Tung University, Taipei, Taiwan) for his kind help in improving the statistical analysis of this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Senaratna, CV, Perret, JL, Lodge, CJ, Lowe, AJ, Campbell, BE, Matheson, MC, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. (2017) 34:70–81. doi: 10.1016/j.smrv.2016.07.002
2. Verhulst, SL, Van Gaal, L, De Backer, W, and Desager, K. The prevalence, anatomical correlates and treatment of sleep-disordered breathing in obese children and adolescents. Sleep Med Rev. (2008) 12:339–46. doi: 10.1016/j.smrv.2007.11.002
3. Patinkin, ZW, Feinn, R, and Santos, M. Metabolic consequences of obstructive sleep apnea in adolescents with obesity: a systematic literature review and meta-analysis. Child Obes. (2017) 13:102–10. doi: 10.1089/chi.2016.0248
4. Gallucci, M, Gessaroli, M, Bronzetti, G, di Palmo, E, Bertelli, L, Giannetti, A, et al. Cardiovascular issues in obstructive sleep apnoea in children: a brief review. Paediatr Respir Rev. (2021) 38:45–50. doi: 10.1016/j.prrv.2020.05.007
5. Urbano, GL, Tablizo, BJ, Moufarrej, Y, Tablizo, MA, Chen, ML, and Witmans, M. The link between pediatric obstructive sleep apnea (OSA) and attention deficit hyperactivity disorder (ADHD). Children. (2021) 8:824. doi: 10.3390/children8090824
7. Chuang, HH, Hsu, JF, Chuang, LP, Chen, NH, Huang, YS, Li, HY, et al. Differences in anthropometric and clinical features among preschoolers, school-age children, and adolescents with obstructive sleep apnea-a hospital-based study in Taiwan. Int J Environ Res Public Health. (2020) 17:4663. doi: 10.3390/ijerph17134663
8. Chuang, HH, Huang, CG, Chuang, LP, Huang, YS, Chen, NH, Li, HY, et al. Relationships among and predictive values of obesity, inflammation markers, and disease severity in pediatric patients with obstructive sleep apnea before and after adenotonsillectomy. J Clin Med. (2020) 9:579. doi: 10.3390/jcm9020579
9. Marcus, CL, Brooks, LJ, Draper, KA, Gozal, D, Halbower, AC, Jones, J, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. (2012) 130:e714–55. doi: 10.1542/peds.2012-1672
10. Lee, CH, Hsu, WC, Chang, WH, Lin, MT, and Kang, KT. Polysomnographic findings after adenotonsillectomy for obstructive sleep apnoea in obese and non-obese children: a systematic review and meta-analysis. Clin Otolaryngol. (2016) 41:498–510. doi: 10.1111/coa.12549
11. Imanguli, M, and Ulualp, SO. Risk factors for residual obstructive sleep apnea after adenotonsillectomy in children. Laryngoscope. (2016) 126:2624–9. doi: 10.1002/lary.25979
12. Bhattacharjee, R, Kheirandish-Gozal, L, Spruyt, K, Mitchell, RB, Promchiarak, J, Simakajornboon, N, et al. Adenotonsillectomy outcomes in treatment of obstructive sleep apnea in children: a multicenter retrospective study. Am J Respir Crit Care Med. (2010) 182:676–83. doi: 10.1164/rccm.200912-1930OC
13. Felso, R, Lohner, S, Hollody, K, Erhardt, E, and Molnar, D. Relationship between sleep duration and childhood obesity: systematic review including the potential underlying mechanisms. Nutr Metab Cardiovasc Dis. (2017) 27:751–61. doi: 10.1016/j.numecd.2017.07.008
14. Liu, S, Wang, X, Zheng, Q, Gao, L, and Sun, Q. Sleep deprivation and central appetite regulation. Nutrients. (2022) 14:5196. doi: 10.3390/nu14245196
15. Cespedes Feliciano, EM, Quante, M, Rifas-Shiman, SL, Redline, S, Oken, E, and Taveras, EM. Objective sleep characteristics and cardiometabolic health in young adolescents. Pediatrics. (2018) 142:e20174085. doi: 10.1542/peds.2017-4085
16. Alves, JM, Chow, T, Nguyen-Rodriguez, S, Angelo, B, Defendis, A, Luo, S, et al. Associations between sleep and metabolic outcomes in preadolescent children. J Endocr Soc. (2022) 6:bvac137. doi: 10.1210/jendso/bvac137
17. Broussard, JL, Kilkus, JM, Delebecque, F, Abraham, V, Day, A, Whitmore, HR, et al. Elevated ghrelin predicts food intake during experimental sleep restriction. Obesity. (2016) 24:132–8. doi: 10.1002/oby.21321
18. Sondrup, N, Termannsen, AD, Eriksen, JN, Hjorth, MF, Faerch, K, Klingenberg, L, et al. Effects of sleep manipulation on markers of insulin sensitivity: a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. (2022) 62:101594. doi: 10.1016/j.smrv.2022.101594
19. Atar, M, Pirgon, O, and Buyukgebiz, A. Sleep disorders and obesity in childhood: a new component in solving obesity. Pediatr Endocrinol Rev. (2019) 16:441–51. doi: 10.17458/per.vol16.2019.apb.sleepdisordersobesitychildhood
20. Nachalon, Y, Lowenthal, N, Greenberg-Dotan, S, and Goldbart, AD. Inflammation and growth in young children with obstructive sleep apnea syndrome before and after adenotonsillectomy. Mediat Inflamm. (2014) 2014:146893. doi: 10.1155/2014/146893
21. Amin, R, Anthony, L, Somers, V, Fenchel, M, McConnell, K, Jefferies, J, et al. Growth velocity predicts recurrence of sleep-disordered breathing 1 year after adenotonsillectomy. Am J Respir Crit Care Med. (2008) 177:654–9. doi: 10.1164/rccm.200710-1610OC
22. Dong, D, Bilger, M, van Dam, RM, and Finkelstein, EA. Consumption of specific foods and beverages and excess weight gain among children and adolescents. Health Aff. (2015) 34:1940–8. doi: 10.1377/hlthaff.2015.0434
23. Roche, J, Isacco, L, Masurier, J, Pereira, B, Mougin, F, Chaput, JP, et al. Are obstructive sleep apnea and sleep improved in response to multidisciplinary weight loss interventions in youth with obesity? A systematic review and meta-analysis. Int J Obes. (2020) 44:753–70. doi: 10.1038/s41366-019-0497-7
24. Cassidy, S, Harvey, L, and Smyth, S. Examining the relationship between obstructive sleep apnoea and eating behaviours and attitudes: a systematic review. Appetite. (2023) 181:106390. doi: 10.1016/j.appet.2022.106390
25. Gohil, A, and Hannon, TS. Poor sleep and obesity: concurrent epidemics in adolescent youth. Front Endocrinol. (2018) 9:364. doi: 10.3389/fendo.2018.00364
26. Chuang, HH, Hsu, JF, Wang, CY, Chuang, LP, Chen, MC, Chen, NH, et al. Hypertension in children with obstructive sleep apnea syndrome-age, weight status, and disease severity. Int J Environ Res Public Health. (2021) 18:9602. doi: 10.3390/ijerph18189602
27. Lachat, C, Hawwash, D, Ocke, MC, Berg, C, Forsum, E, Hornell, A, et al. Strengthening the reporting of observational studies in epidemiology-nutritional epidemiology (STROBE-nut): an extension of the STROBE statement. PLoS Med. (2016) 13:e1002036. doi: 10.1371/journal.pmed.1002036
28. Chuang, HH, Hsu, JF, Chuang, LP, Chiu, CH, Huang, YL, Li, HY, et al. Different associations between tonsil microbiome, chronic tonsillitis, and intermittent hypoxemia among obstructive sleep apnea children of different weight status: a pilot case-control study. J Pers Med. (2021) 11:486. doi: 10.3390/jpm11060486
29. Chuang, HH, Wang, CY, Chuang, LP, Huang, YS, Li, HY, Fang, TJ, et al. The 3% oxygen desaturation index is an independent risk factor for hypertension among children with obstructive sleep apnea. Nat Sci Sleep. (2022) 14:1149–64. doi: 10.2147/NSS.S362557
30. Hsieh, HS, Chuang, HH, Hsin, LJ, Lin, WN, Kang, CJ, Zhuo, MY, et al. Effect of preoperative weight status and disease presentation on postoperative elevated blood pressure after childhood adenotonsillectomy. Otolaryngol Head Neck Surg. (2023) 168:1197–208. doi: 10.1002/ohn.184
31. Huang, CG, Hsu, JF, Chuang, LP, Li, HY, Fang, TJ, Huang, YS, et al. Adenotonsillectomy-related changes in systemic inflammation among children with obstructive sleep apnea. J Chin Med Assoc. (2023). doi: 10.1097/JCMA.0000000000000921. [Epub ahead of print]
32. Marcus, CL, Moore, RH, Rosen, CL, Giordani, B, Garetz, SL, Taylor, HG, et al. A randomized trial of adenotonsillectomy for childhood sleep apnea. N Engl J Med. (2013) 368:2366–76. doi: 10.1056/NEJMoa1215881
33. Huang, YS, Guilleminault, C, Lee, LA, Lin, CH, and Hwang, FM. Treatment outcomes of adenotonsillectomy for children with obstructive sleep apnea: a prospective longitudinal study. Sleep. (2014) 37:71–6. doi: 10.5665/sleep.3310
34. Franco, RA Jr, Rosenfeld, RM, and Rao, M. Quality of life for children with obstructive sleep apnea. Otolaryngol Head Neck Surg. (2000) 123:9–16. doi: 10.1067/mhn.2000.105254
35. Kuczmarski, RJ, Ogden, CL, Guo, SS, Grummer-Strawn, LM, Flegal, KM, Mei, Z, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. (2002) 11:1–190.
36. Lee, LA, Li, HY, Lin, YS, Fang, TJ, Huang, YS, Hsu, JF, et al. Severity of childhood obstructive sleep apnea and hypertension improved after adenotonsillectomy. Otolaryngol Head Neck Surg. (2015) 152:553–60. doi: 10.1177/0194599814561203
37. Lillegaard, IT, Overby, NC, and Andersen, LF. Evaluation of a short food frequency questionnaire used among Norwegian children. Food Nutr Res. (2012) 56:6399. doi: 10.3402/fnr.v56i0.6399
38. Saeedi, P, Skeaff, SA, Wong, JE, and Skidmore, PM. Reproducibility and relative validity of a short food frequency questionnaire in 9−10 year-old children. Nutrients. (2016) 8:271. doi: 10.3390/nu8050271
39. Lien, N, Bjelland, M, Bergh, IH, Grydeland, M, Anderssen, SA, Ommundsen, Y, et al. Design of a 20-month comprehensive, multicomponent school-based randomised trial to promote healthy weight development among 11-13 year olds: the HEalth in adolescents study. Scand J Public Health. (2010) 38:38–51. doi: 10.1177/1403494810379894
40. Gebremariam, MK, Henjum, S, Terragni, L, and Torheim, LE. Correlates of fruit, vegetable, soft drink, and snack intake among adolescents: the ESSENS study. Food Nutr Res. (2016) 60:32512. doi: 10.3402/fnr.v60.32512
41. Amato, A, Proia, P, Caldara, GF, Alongi, A, Ferrantelli, V, and Baldassano, S. Analysis of body perception, preworkout meal habits and bone resorption in child gymnasts. Int J Environ Res Public Health. (2021) 18:2184. doi: 10.3390/ijerph18042184
42. Henriksen, HB, Carlsen, MH, Paur, I, Berntsen, S, Bohn, SK, Skjetne, AJ, et al. Relative validity of a short food frequency questionnaire assessing adherence to the Norwegian dietary guidelines among colorectal cancer patients. Food Nutr Res. (2018) 62:1306. doi: 10.29219/fnr.v62.1306
43. Huang, Y-S, Hwang, F-M, Lin, C-H, Lee, L-A, Huang, P-Y, and Chiu, S-T. Clinical manifestations of pediatric obstructive sleep apnea syndrome: clinical utility of the Chinese-version obstructive sleep apnea questionaire-18. Psychiatry Clin Neurosci. (2015) 69:752–62. doi: 10.1111/pcn.12331
44. Berry, RB, Budhiraja, R, Gottlieb, DJ, Gozal, D, Iber, C, Kapur, VK, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American Academy of sleep medicine. J Clin Sleep Med. (2012) 08:597–619. doi: 10.5664/jcsm.2172
45. Health Promotion Administration. Daily dietary guidelines of Taiwan. (2018). Available at: https://www.hpa.gov.tw/File/Attach/6712/File_6253.pdf (Accessed August 26, 2022).
46. Chuang, HH, Lin, RH, Chen, JY, Yeh, WC, Lin, HF, Ueng, SW, et al. Effectiveness of a multi-faceted intervention among elementary school children. Medicine. (2019) 98:e15079. doi: 10.1097/MD.0000000000015079
47. Spruyt, K, Sans Capdevila, O, Serpero, LD, Kheirandish-Gozal, L, and Gozal, D. Dietary and physical activity patterns in children with obstructive sleep apnea. J Pediatr. (2010) 156:724–730.e3. doi: 10.1016/j.jpeds.2009.11.010
48. Pan, X. Calculation of sampling size for non-zero tolerance level. Glob Ecol Conserv. (2020) 22:e00982. doi: 10.1016/j.gecco.2020.e00982
49. Lu, CT, Li, HY, Lee, GS, Huang, YS, Huang, CG, Chen, NH, et al. Snoring sound energy as a potential biomarker for disease severity and surgical response in childhood obstructive sleep apnoea: a pilot study. Clin Otolaryngol. (2019) 44:47–52. doi: 10.1111/coa.13231
50. Dormann, CF, Elith, J, Bacher, S, Buchmann, C, Carl, G, Carré, G, et al. Collinearity: a review of methods to deal with it and a simulation study evaluating their performance. Ecography. (2013) 36:27–46. doi: 10.1111/j.1600-0587.2012.07348.x
51. Health Promotion Administration. Nutrition and health survey in Taiwan, 2017-2020. (2022). Available at: https://www.hpa.gov.tw/File/Attach/15562/File_18775.pdf (Accessed August 26, 2022).
52. Giosue, A, Calabrese, I, Vitale, M, Riccardi, G, and Vaccaro, O. Consumption of dairy foods and cardiovascular disease: a systematic review. Nutrients. (2022) 14:831. doi: 10.3390/nu14040831
53. Vanderhout, SM, Aglipay, M, Torabi, N, Juni, P, da Costa, BR, Birken, CS, et al. Whole milk compared with reduced-fat milk and childhood overweight: a systematic review and meta-analysis. Am J Clin Nutr. (2020) 111:266–79. doi: 10.1093/ajcn/nqz276
54. Holmes, JF, St Laurent, CW, and Spencer, RMC. Unhealthy diet is associated with poor sleep in preschool-aged children. J Genet Psychol. (2021) 182:289–303. doi: 10.1080/00221325.2021.1905598
55. Cao, M, Zhu, Y, Sun, F, Luo, J, and Jing, J. Short sleep duration is associated with specific food intake increase among school-aged children in China: a national cross-sectional study. BMC Public Health. (2019) 19:558. doi: 10.1186/s12889-019-6739-8
56. Araghi, MH, Chen, YF, Jagielski, A, Choudhury, S, Banerjee, D, Hussain, S, et al. Effectiveness of lifestyle interventions on obstructive sleep apnea (OSA): systematic review and meta-analysis. Sleep. (2013) 36:1562A–E. doi: 10.5665/sleep.3056
57. Kahn, A, Dan, B, Groswasser, J, Franco, P, and Sottiaux, M. Normal sleep architecture in infants and children. J Clin Neurophysiol. (1996) 13:184–97. doi: 10.1097/00004691-199605000-00002
58. Lee, CL, Liao, HL, Lee, WC, Hsu, CK, Hsueh, FC, Pan, JQ, et al. Standards and labeling of milk fat and spread products in different countries. J Food Drug Anal. (2018) 26:469–80. doi: 10.1016/j.jfda.2017.10.006
59. Jeznach-Steinhagen, A, Okreglicka, K, Nitsch-Osuch, A, Czerwonogrodzka-Senczyna, A, and Barnas, M. Nutritional status and dietary patterns in adults with severe obstructive sleep apnea. Adv Exp Med Biol. (2020) 1279:71–9. doi: 10.1007/5584_2020_507
60. Agricultural Research Service U.S. Department of Agriculture. Noodles, egg, enriched, cooked. Washington, DC: U.S. Department of Agriculture (2018).
61. Shin, SM. Association of meat intake with overweight and obesity among school-aged children and adolescents. J Obes Metab Syndr. (2017) 26:217–26. doi: 10.7570/jomes.2017.26.3.217
62. Min, C, Kim, HJ, Park, IS, Park, B, Kim, JH, Sim, S, et al. The association between sleep duration, sleep quality, and food consumption in adolescents: a cross-sectional study using the Korea youth risk behavior web-based survey. BMJ Open. (2018) 8:e022848. doi: 10.1136/bmjopen-2018-022848
63. Ersoy, B, Yuceturk, AV, Taneli, F, Urk, V, and Uyanik, BS. Changes in growth pattern, body composition and biochemical markers of growth after adenotonsillectomy in prepubertal children. Int J Pediatr Otorhinolaryngol. (2005) 69:1175–81. doi: 10.1016/j.ijporl.2005.02.020
64. Hashemian, F, Farahani, F, and Sanatkar, M. Changes in growth pattern after adenotonsillectomy in children under 12 years old. Acta Med Iran. (2010) 48:316–9.
65. Altundag, A, Salihoglu, M, Cayonu, M, and Tekeli, H. Clinical assessment of olfactory functions in children who underwent adenotonsillectomy during pre- and post-operative period. Int J Pediatr Otorhinolaryngol. (2014) 78:1138–42. doi: 10.1016/j.ijporl.2014.04.032
66. Wadolowska, L, Hamulka, J, Kowalkowska, J, Ulewicz, N, Hoffmann, M, Gornicka, M, et al. Changes in sedentary and active lifestyle, diet quality and body composition nine months after an education program in Polish students aged 11-12 years: report from the ABC of healthy eating study. Nutrients. (2019) 11:331. doi: 10.3390/nu11020331
Keywords: adenotonsillectomy, children, dietary profile, dietary educational counseling, food frequency, food literacy, obstructive sleep apnea, outcome assessment
Citation: Chuang H-H, Lin R-H, Hsu J-F, Chuang L-P, Li H-Y, Fang T-J, Huang Y-S, Yang AC, Lee G-S, Kuo TBJ, Yang CCH and Lee L-A (2023) Dietary profile of pediatric obstructive sleep apnea patients, effects of routine educational counseling, and predictors for outcomes. Front. Public Health. 11:1160647. doi: 10.3389/fpubh.2023.1160647
Edited by:
Radwan Qasrawi, Al-Quds University, PalestineReviewed by:
Dominique R. Williams, The Ohio State University, United StatesHazem Agha, Al-Quds University, Palestine
Copyright © 2023 Chuang, Lin, Hsu, Chuang, Li, Fang, Huang, Yang, Lee, Kuo, Yang and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li-Ang Lee, NTczOEBjZ21oLm9yZy50dw==
 Hai-Hua Chuang
Hai-Hua Chuang Rong-Ho Lin3
Rong-Ho Lin3 Jen-Fu Hsu
Jen-Fu Hsu Hsueh-Yu Li
Hsueh-Yu Li Albert C. Yang
Albert C. Yang Guo-She Lee
Guo-She Lee Cheryl C. H. Yang
Cheryl C. H. Yang Li-Ang Lee
Li-Ang Lee