- 1Social Determinants of Health Research Center, Gonabad University of Medical Sciences, Gonabad, Iran
- 2Asadabad School of Medical Sciences, Asadabad, Iran
- 3Health Metrics Research Centre, Iranian Institute for Health Sciences Research, ACECR, Tehran, Iran
- 4Social Determinants of Health Research Center, Research Institute for Health Development, Kurdistan University of Medical Sciences, Sanandaj, Iran
- 5Center for Research on Occupational Disease, Tehran University of Medical Sciences, Tehran, Iran
- 6Department of Environmental Engineering, Mehralborz University (MAU), Tehran, Iran
- 7Department of Public Health, School of Public Health, Research Center for Evidence-Based Health Management, Maragheh University of Medical Sciences, Maragheh, Iran
- 8Department of Public Health, School of Health and Safety, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Introduction: Suicide is a major issue of concern for public health. It is estimated that suicide accounts for 700,000 deaths every year. A personal history of one or more suicide attempts is the most important determinant of suicide among the general population. This study aimed to assess the major risk factors associated with suicidal behaviors among Iranian employees in a medical setting.
Methods: In this study, 3,913 employees of Tehran University of Medical Sciences who participated in the employees' cohort study conducted by the university were recruited. Suicidal behaviors (SBs) and their associated risk factors were evaluated using the World Mental Health Composite International Diagnostic Interview (CIDI) Version 3.0. Univariate and multivariate logistic regressions were performed to identify the determinants of SBs among the participants, and crude and adjusted odds ratios (ORs) with corresponding 95% confidence intervals (95% CIs) were calculated.
Results: Overall, 49.6% of respondents (n = 1,939) reported that they were tired of life and thinking about death. The lifetime prevalence rate of suicidal ideation (SI) was 8.1% (n = 317), that of suicide planning (SP) was 7.3% (n = 287), and that of suicide attempts (SA) was 3.1% (n = 122). Being female (OR: 1.87, CI: 1.64–2.12), being divorced (OR: 3.13, CI: 1.88–5.22), having a low level of education (OR: 1.57, CI: 1.15–2.14), and working in clinical and medical services (OR: 1.25, CI: 1.09–1.43) were associated with being tired of life and thinking about death. These factors were also associated with SI, SP, and SA.
Discussion: These findings highlight the need to prioritize mental health for suicide prevention, especially for high-risk groups, in workplace mental health promotion programs and policies.
Introduction
Suicide is a major issue of concern for public health; globally, it is considered to be among the 20 most common causes of death. Every year, ~700,000 people die by suicide (1), although these deaths are preventable. The majority of suicide cases (~79%) are reported to occur in low- and middle-income countries, where financial and professional resources to help those in need are limited (2). Suicide is not an independent event; rather, it is a process that begins with suicidal ideation (SI); continues with disappointment, momentary SI, and precise plans; and finally ends with a suicide attempt (SA) (3).
Some studies suggest that total rates of SA are up to four times higher than the rate fatal SA (4–9). A study that investigated the prevalence of SI, suicide plans, and attempts among 84,850 adults from 17 countries reported that 9.2% of adults had experienced lifelong SI, but only 3.1% reported lifelong suicide planning (SP), and 2.7% reported at least one SA (10). However, the study also reported that 60% of people attempt suicide in the first year after SI. Among people with SI, there was a 33% probability of ever having planned suicide and a 29% probability of ever having attempted suicide. In addition, among the individuals who had experienced both SI and SP, ~56% had attempted suicide, as compared to the 15.4% rate of suicide attempts among those who had experienced only SI (10). Therefore, it is clear that SI increases the risk of suicide, and having an SP increases this risk even more (11). Most fatal SAs happen after one or two previous SAs (8, 12). The risk of recurrence of SA is at its highest in the first 6 months after an episode (13), during which period the rate of recurrence can be up to 9% (14). Within 1–2 years after an episode, ~60% of individuals experience recurrence of SA (15). In comparison, the rate of fatal SA during 1–4 years of follow-up is ~3% (16).
Studies have identified several potential determinants of or influencing factors for suicide and fatal SA, including social, biological, genetic, psychological, environmental, and local factors (17). For example, a history of mental illness, substance or alcohol abuse, chronic illness, emotional problems, violence, sudden major changes in a person's life (such as job loss or separation), lack of a source of income or insufficient income to make ends meet, and a history of suicide among immediate family members are the major determinants of suicide. A multiplicity of these factors in a particular individual will increase the chance of a fatal SA (10, 18–20). Suicide attempters are often diagnosed with other psychiatric disorders, including major depressive disorder, anxiety disorder, post-traumatic stress disorder, and substance abuse disorder. Most attempters also often report SI (21, 22). Fatal SAs are reportedly associated to a greater extent with severe clinical conditions (23, 24), as well as being influenced by gender and age (25). Statistics show that the rate of suicide is three to four times lower in males than in females (26, 27), but hospitalization due to SA is more common among females (28). However, the mortality rate of SA is three times higher in males than in females (26, 29). These differences are attributed to the higher prevalence of depression in females and the use of more lethal methods by men during SA (30).
Suicide is not easy to predict, as it is a complex multifactorial phenomenon that depends on the dynamics of various factors over time (4–9). In addition, the effects of risk factors may vary among different individuals based on their demographic characteristics, which are subject to change over time. For example, the effect of being single and unemployed and having a low income on the incidence of suicide is greater in men (31). Unpleasant psychosocial conditions in the workplace, known as social determinants of health (SDH) (32), such as low job control and high job demand (28), as well as reward imbalances, lead to poor mental health, which is a major predictor of suicide (33).
Mental health in the workplace is a crucial aspect of workplace health, as it influences both the health and the productivity of employees (33). According to a systematic review of suicide risk among healthcare workers, SI is a significant problem among these workers. The review found that healthcare workers have a higher risk of suicide than the general population. The authors also found that there is a lack of research on the topic of SI among healthcare workers (34). Hence, a key initial step for any effective and tailored workplace health promotion program is to identify the important mental health risk factors and high-risk groups within the environmental context of employees in terms of living and working. This article presents one component of a major workplace health cohort project conducted in Iran by the Tehran University of Medical Sciences (TUMS). This study aimed to assess the major risk factors associated with suicidal behavior (SB) among Iranian employees in medical settings.
Materials and methods
Study design and population
Data were extracted from the TUMS employees' cohort (TEC) study. Specifically, 3,913 employees who participated in the TEC study, which was undertaken by the university between January 2018 and August 2019, were included. The participants (employees of TUMS) were interviewed at the TEC center of the university, and a questionnaire was used to collect data on their mental and physical health. Participants were included if they were employed by TUMS under any type of employment status during the study period and provided informed consent. Job title, employment status, and occupational group (including office and administrative services, clinical and medical services, public services, technical services, diagnostic and chemical laboratory staff, and security guards) were recorded for all participants (35).
Data collection
Data related to the different aspects of SB were collected using the third version of the World Mental Health Composite International Diagnostic Interview (CIDI) (36). The CIDI assesses participants' lifetime occurrence, age of onset, and recency of suicidal ideation (“Have you ever seriously thought about attempting suicide?”), suicide planning (“Have you ever made a plan for attempting suicide?”), and suicide attempts (“Have you ever attempted suicide?”). The questionnaires were completed through interviews, which were conducted by trained personnel.
Independent variables assessed in this study included personal and social determinants of health. These were age, gender, marital status, educational level, childhood socioeconomic status (SES), current SES, degree of fluctuation in SES, occupational group, employment status, job position, number of people in the household, number of books read in the past year (except for textbooks, business books, religious books, and holy books), work experience, social capital, and household assets.
Household assets assessed included a car (not for commercial purposes), a dishwasher, a microwave oven, a personal computer, a washing machine, a color television, or a video system (VHS, VCD, or DVD), as well as Internet access at home. Number of rooms and per capita area of the building; frequency of concert, theater, and movie attendance; frequency of eating a restaurant meal with the cost covered by the respondent; frequency of taking a flight; and monthly Internet cost were combined using categorical principal components analysis (CATPCA). The SES of the participants was selected as the first factor, and this was divided into five categories (percentiles) (37, 38). The respondents were thus classified into five groups based on their SES category, from high SES (richest) to low SES (poorest).
Data analysis
Descriptive analyses were conducted to assess the distribution of sociodemographic variables and SBs among the participants. Data on continuous variables are reported in the form of means and standard deviations, and categorical data are reported as frequencies and percentages. Differences in SBs among different subgroups were explored using Chi-square analysis.
Univariate and multivariate logistic regressions were performed to identify the risk factors for SBs. Each independent variable was first entered separately into a univariate logistic regression analysis, and variables displaying an association with p < 0.2 were entered into a multiple logistic regression model. Crude and adjusted odds ratios (ORs) with their corresponding 95% confidence interval (95% CI) were recorded. All statistical analyses were conducted using SPSS 24. The threshold for statistical significance was defined as a p-value < 0.05.
Results
Among the 3,913 participants enrolled in this study, 2,371 (60.6%) were women, and 3,166 (80.9%) were married. The mean age of the participants was 41.73 years (SD: 8.83, range: 20–75). Overall, 49.6% of respondents (n = 1,939) reported that they were sometimes tired of life and thought about death. The lifetime prevalence rates of SI (n = 317), SP (n = 287), and SA (n = 122) were 8.1%, 7.3%, and 3.1%, respectively. Table 1 presents the incidence of suicidal behaviors among different sociodemographic groups.
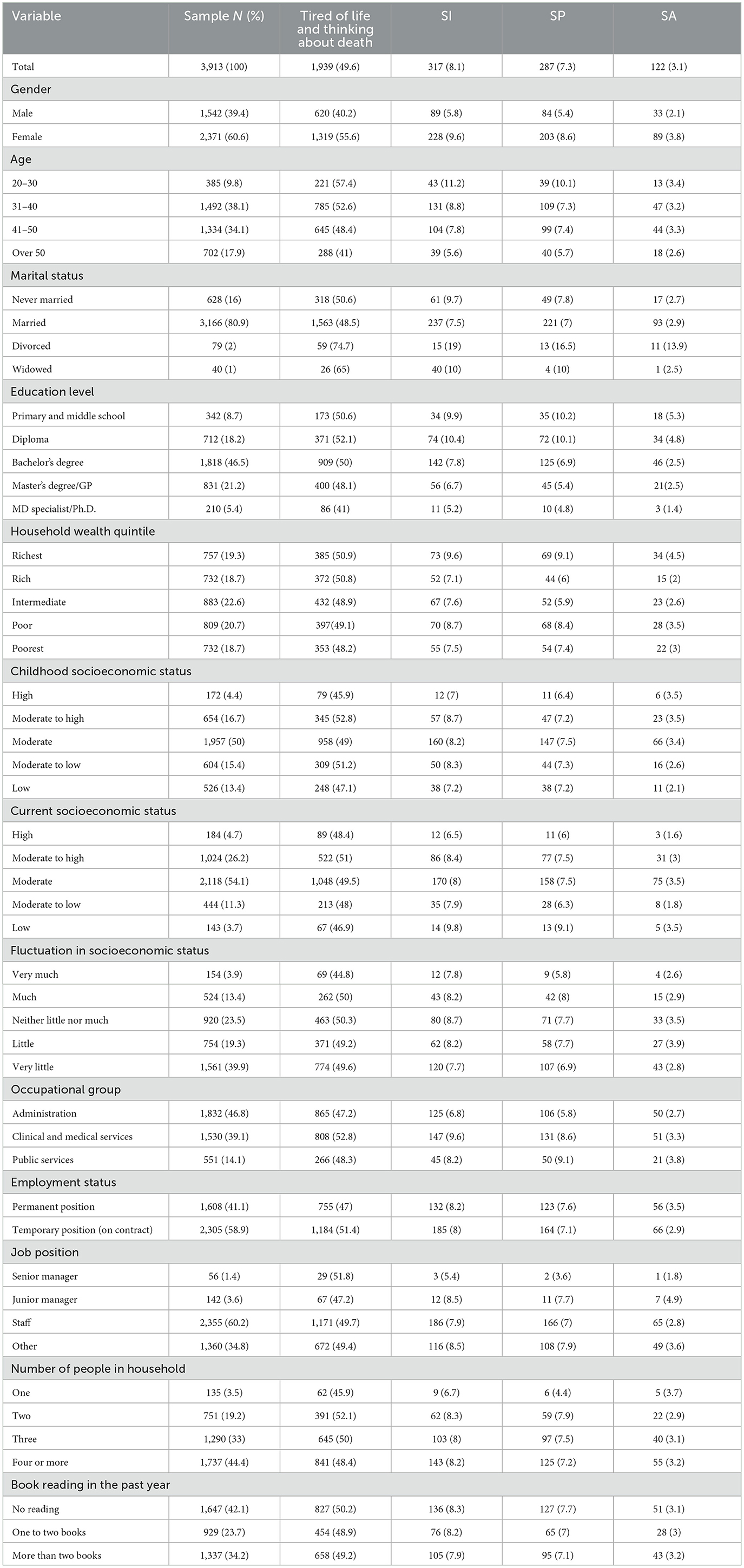
Table 1. The distribution of being tired of life and thinking about death and of suicidal behaviors according to participant characteristics.
Crude and adjusted odds ratios calculated to explore the associations of suicidal feelings, thoughts, and behaviors with various sociodemographic characteristics are shown in Tables 2, 3. In the crude model, female gender was associated with being tired of life and thinking about death [crude odds ratio (cOR) = 1.87, 95% CI: 1.64–2.12], as well as with all three types of SB: SI (cOR = 1.74, 95% CI: 1.35–2.24), SP (cOR = 1.62, 95% CI: 1.25–2.11), and SA (cOR = 1.78, 95% CI: 1.19–2.67). In the crude model, the odds of being tired of life and thinking about death, as well as the odds of experiencing SI and SP, decreased with increasing age. However, SA had no significant relationship with age in the crude model.
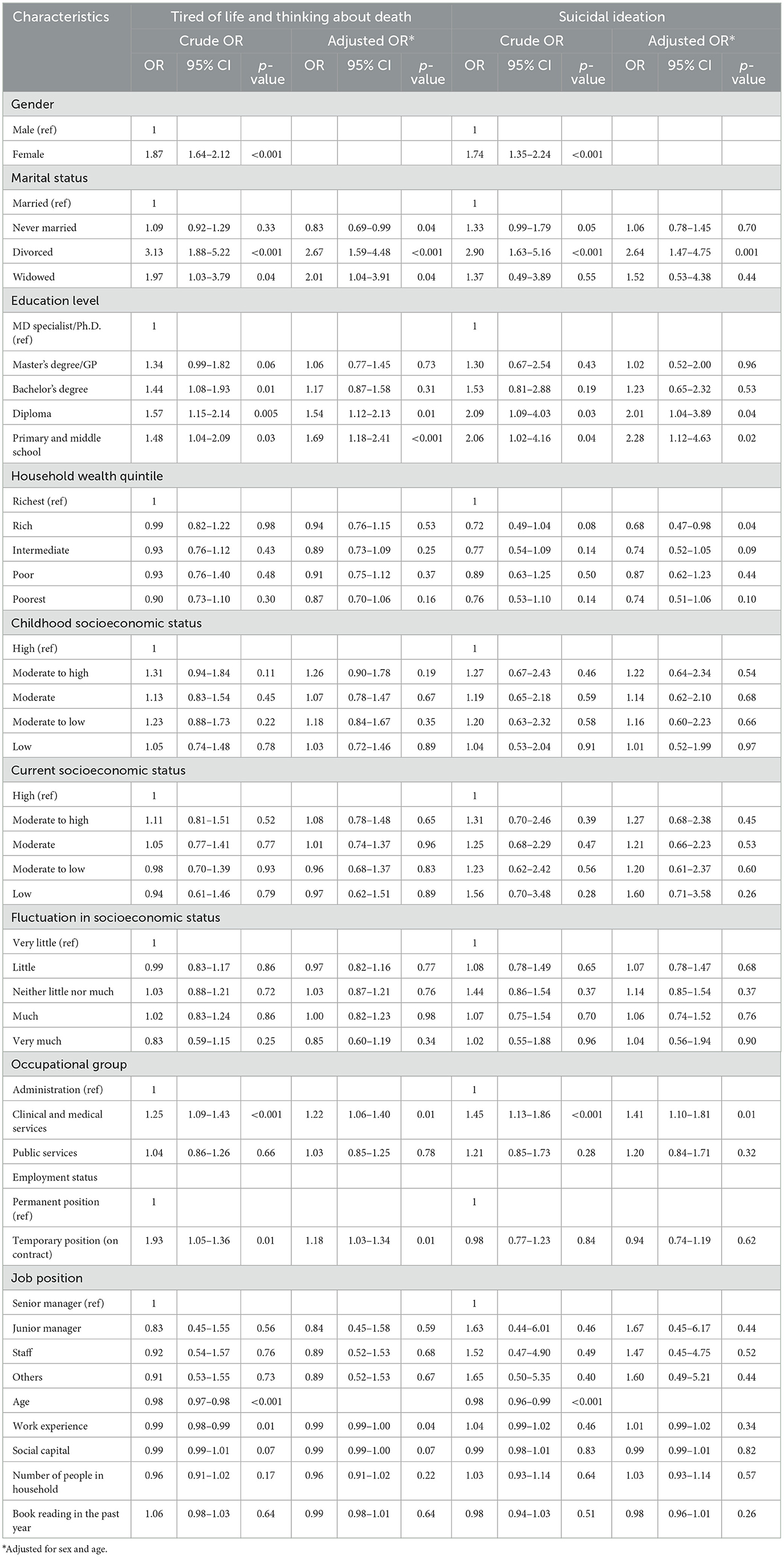
Table 2. Logistic regression models for being tired of life and thinking about death and for suicidal ideation according to sociodemographic characteristics.
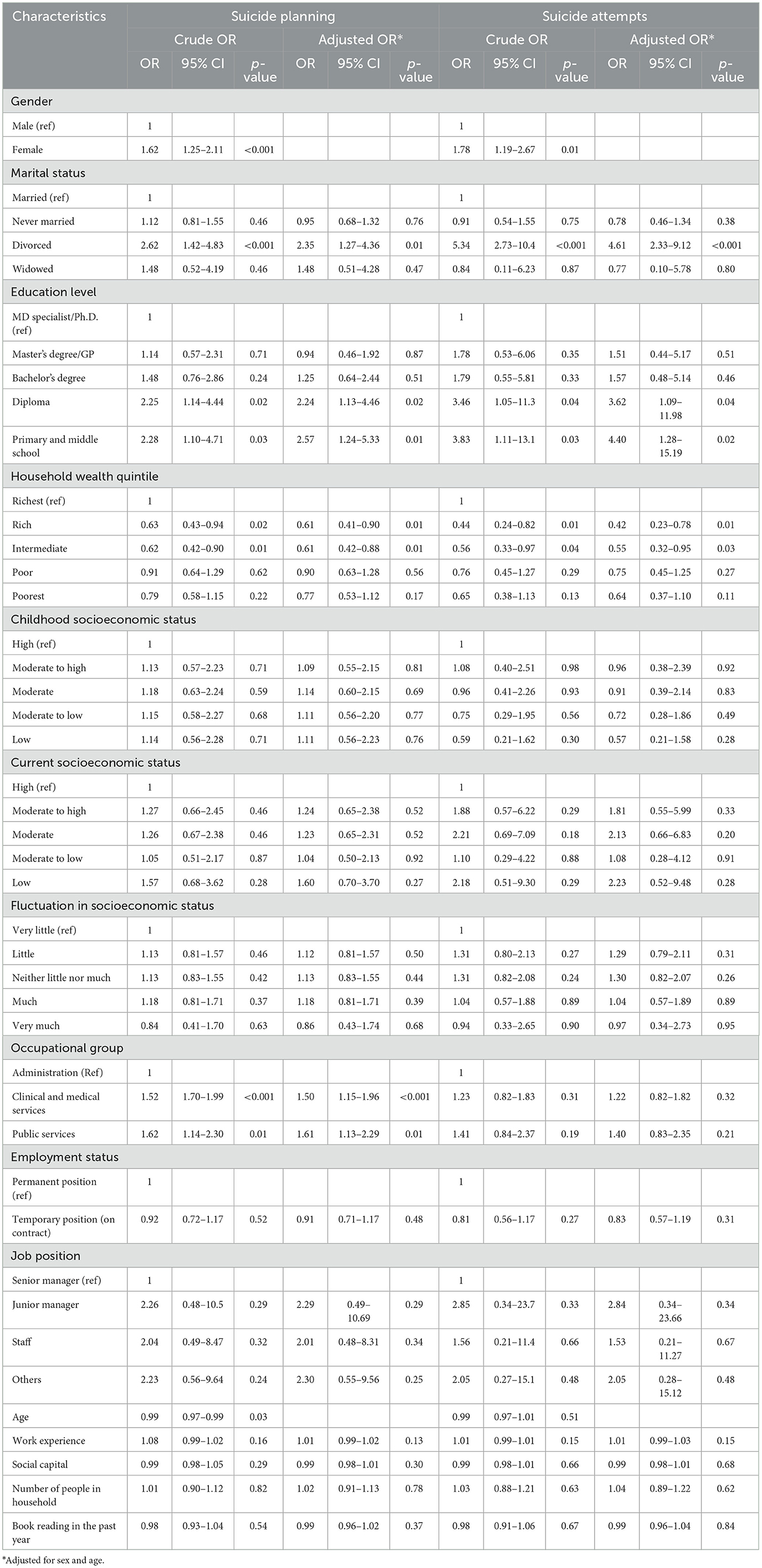
Table 3. Logistic regression models for suicide planning and suicide attempts according to sociodemographic characteristics.
Compared with married employees, divorced employees were much more likely to report feeling tired of life and thinking about death [adjusted odds ratio (aOR) = 2.67, 95% CI: 1.59–4.48], and to report having engaged in all three types of suicidal behavior (SI: aOR = 2.64, 95% CI 1.47–4.75; SP: aOR = 2.35, 95% CI 1.27–4.36; and SA: aOR = 4.61, 95% CI 2.33–9.12). In terms of employment group, compared with the administrative services group, people working in clinical and medical services and those directly involved in providing medical and therapeutic services to patients were at a higher risk of SI (aOR = 1.41, 95% CI: 1.10–1.81) and SP (aOR = 1.50, 95%CI: 1.15–1.96), as well as a higher risk of feeling tired of life and thinking about death (aOR = 1.22, 95% CI: 1.06–1.40). In the crude and adjusted analyses, respondents with education levels no higher than a diploma had significantly increased odds of reporting being tired of life and thinking about death, and of reporting suicidal behaviors. Employment status was only significantly associated with feeling tired of life and thinking about death. Compared with permanent employees, employees working under temporary contracts had increased odds of reporting feeling tired of life and thinking about death (aOR = −1.18, 95% CI: 1.03–1.34). Generally, in both the crude and the adjusted model, household wealth quintile was significantly associated with risk of SP and SI. In comparison with the richest quintile, the odds of SP in the rich and intermediate-wealth quintiles were 39% lower. In addition, the odds of SA in the rich and intermediate-wealth quintiles were 58 and 45% lower, respectively.
Discussion
Employee mental health is a key resource for good quality of life, wellbeing, and work. Therefore, monitoring employee mental health should be an element of workplace health promotion and development plans and programs. This study showed that approximately half of the employees studied reported that they felt tired of life and had thought about death.
These characteristics may fall within the concept of “demoralization.” Demoralization is experienced as existential despair, hopelessness, helplessness, and loss of meaning and purpose in life. Hopelessness, the hallmark of demoralization, is associated with poor outcomes in physical and psychiatric illness and, importantly, with SI and the wish to die (39). A previous systematic review showed that demoralization could be associated with SI/SB and with a significant increase in suicide risk (40). The results of this study showed that almost 10% of healthcare professionals reported having experienced SI (8.1%), SP (7.3%), or SA (3.1%). According to a WHO report, Iran's crude suicide rate for all ages (per 100,000) in 2019 was 5.2 (41). A study conducted in the USA showed that 5% of suicide deaths from 2003 to 2016 occurred among healthcare professionals (42).
Similar to other studies, this study showed that thinking about death, SI, SP, and SA were more prevalent in women than in men (but less than twice as prevalent) (43, 44). A previous systematic review and meta-analysis indicated that women were at approximately twice as great a risk of SA and men approximately three times as great a risk of suicide death (45). In addition, similar to previous studies (including a European cross-national study of 5,212 participants), this study showed that SAs by men appeared to be more serious than SAs by women (46–51). Men are less likely to seek social support, indicating that the goal of suicide attempts by men is more likely to be to die rather than to seek help (52–54). Since patterns of suicidal behavior differ by gender, these differences should be considered carefully in the design of preventive intervention programs to address suicide.
The data analysis also showed that an increase in age protects individuals against feeling tired of life, thinking about death, and SI. A similar effect has been reported in a nationally representative survey conducted in the USA, which reported that individuals younger than 26 years were more likely to report having major depressive disorder and suicidal thoughts, and were more likely to attempt suicide and/or to die by suicide as compared to adults aged 26 years or older (51). These results strongly indicate that adolescents are a high-risk group for suicide-related behaviors.
Marital status was also found to influence the risk of suicide in this study, as divorced employees were more likely to feel tired of life, think about death, and engage in each of the three types of suicidal behavior (SI, SP, and SA). Similar associations between marital status and suicide have been reported in other studies (52, 53): specifically, divorcees are more likely to report having thoughts of “life not worth living,” major depression, panic and anxiety disorders, and low self-esteem, which are known risk factors for suicide (53). However, there are also contradictory findings. For example, one study in the USA showed that healthcare professionals who were married were at a higher risk of suicide than those who were not married (42). This is probably because of issues related to the quality of married life, as observed in a study conducted in China, where a significant relationship with suicide or SA was found for marital conflicts and quarreling with a partner within the past month (54).
Studies that have measured rates of suicide in different occupational groups have shown that suicide rates vary across these groups (55, 56). The present study also showed that type of job influences risk of suicide. People working in clinical and medical services were more likely to be at risk for suicidal behaviors than those working in administration. A study conducted in the United States showed that the suicide rate of medical professionals is noticeably higher than that of the general population. For example, the risk of dying by suicide is three times higher for surgeons than it is for the general population (57). Another study in Denmark reported that medicine and nursing are the occupations with the highest suicide rate (58). The effect of job type on suicide may be due to high levels of stress in some occupations (59). Furthermore, burnout is also a risk factor in healthcare professions (60), and this is reportedly associated with SI (61). Other potential reasons might be that health professionals are more aware of suicide methods (for example, different kinds of drugs, lethal doses, and their effects) and have better access to these methods (62).
This study also indicated that lower income, lower education levels, and lower occupation levels might be risk factors for feeling tired of life and thinking about death, and for suicidal behaviors. A study conducted among Korean employees showed that workers with fewer years of education experienced more SI (63). Similar to certain other studies (64), the present study identified a significant association between employment status and having a sense of being tired of life and thinking about death. Socioeconomic factors, such as level of education, income, and employment, are interrelated variables, the most important of which can be level of education. People with higher levels of education are more likely to have better jobs, and consequently, they are more likely to have higher incomes. Exposure to poor working conditions is associated with poor mental health, which can be a predictor of suicide (33). Therefore, level of education can function as a fundamental factor in suicide. According to the findings, the top priority groups for suicide prevention programs in the workplaces studied should be women, especially divorced women with low levels of education.
In conclusion, this study has identified social determinants of employees' mental health, such as being female, being divorced, and having a low level of education, which were found to significantly affect both thoughts and behaviors even after adjusting for socioeconomic variables. The results also confirmed that most suicide risk factors present in the general population also applied to the employees of the medical university studied. This finding highlights the need to prioritize mental health and to focus on high-risk groups (women, divorced individuals, and those with a low level of education) for suicide prevention in workplace programs and policies promoting mental health, as well as in research and clinical practice. For example, divorced female employees with limited education should be considered a priority group to utilize mental health consultation and treatment provided by mental health practitioners and clinicians.
Strengths and limitations
The study partially reported in this article is a major workplace health cohort project with a relatively large and highly diverse representative sample consisting of individuals from different socioeconomic backgrounds. Another notable strength of the study is the investigation of suicide-related feelings, in addition to SI, SP, and SA. However, the findings of this cross-sectional study are limited in terms of the possibility of making any causal interpretation. Therefore, the results must be interpreted with caution.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Tehran University of Medical Sciences. The patients/participants provided their written informed consent to participate in this study.
Author contributions
ZR, AA, NK-M, and AL contributed to the study conception and design, drafting of the manuscript, and critical revision of the manuscript for important intellectual content. SM and HP participated in the acquisition of data, drafting of the manuscript, and critical revision of the manuscript for important intellectual content. All authors agreed on the final manuscript prior to submission and agreed to be accountable for all aspects of this work.
Funding
This study was conducted with the cooperation and support of the Tehran University of Medical Sciences (TUMS) employees' cohort (TEC) study (Grant no: 36600).
Acknowledgments
The researchers would like to thank all the participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
Abbreviations: SDH, social determinants of health; TUMS, Tehran University of Medical Sciences; SES, socioeconomic status; SI, suicidal ideation; SP, suicide planning; SA, suicide attempt.
References
1. World Health Organization. Suicide Worldwide in 2019: Global Health Estimates. Geneva: WHO (2021).
2. World Health Organization. National Suicide Prevention Strategies: Progress, Examples and Indicators. Geneva: World Health Organization (2018).
3. Van Heeringen K, Hawton K, Williams JMG. Pathways to suicide: an integrative approach. In:van Heeringen K, Hawton K, , editors. The International Handbook of Suicide and Attempted Suicide. Hoboken, NJ: Wiley (2000), p. 223–34. doi: 10.1002/9780470698976.ch14
4. Dhingra K, Boduszek D, O'Connor RC. Differentiating suicide attempters from suicide ideators using the Integrated Motivational–Volitional model of suicidal behaviour. J Affect Disord. (2015) 186:211–8. doi: 10.1016/j.jad.2015.07.007
5. Klonsky ED, May AM, Saffer BY. Suicide, suicide attempts, and suicidal ideation. Annu Rev Clin Psychol. (2016) 12:307–30. doi: 10.1146/annurev-clinpsy-021815-093204
6. Choi KH, Wang S-M, Yeon B, Suh S-Y, Oh Y, Lee H-K, et al. Risk and protective factors predicting multiple suicide attempts. Psychiatry Res. (2013) 210:957–61. doi: 10.1016/j.psychres.2013.09.026
7. Baca-Garcia E, Perez-Rodriguez MM, Oquendo MA, Keyes KM, Hasin DS, Grant BF, et al. Estimating risk for suicide attempt: are we asking the right questions?: passive suicidal ideation as a marker for suicidal behavior. J Affect Disord. (2011) 134:327–32. doi: 10.1016/j.jad.2011.06.026
8. Parra-Uribe I, Blasco-Fontecilla H, Garcia-Parés G, Martínez-Naval L, Valero-Coppin O, Cebrià-Meca A, et al. Risk of re-attempts and suicide death after a suicide attempt: a survival analysis. BMC Psychiatry. (2017) 17:1–11. doi: 10.1186/s12888-017-1317-z
9. Bryan CJ, Rudd MD. The importance of temporal dynamics in the transition from suicidal thought to behavior. Clin Psychol: Sci Pract. (2016) 23:21–5. doi: 10.1111/cpsp.12135
10. Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. (2008) 192:98–105. doi: 10.1192/bjp.bp.107.040113
11. LeFevre ML. Screening for suicide risk in adolescents, adults, and older adults in primary care: US Preventive Services Task Force recommendation statement. Ann Intern Med. (2014) 160:719–26. doi: 10.7326/M14-0589
12. Allen MH, Abar BW, McCormick M, Barnes DH, Haukoos J, Garmel GM, et al. Screening for suicidal ideation and attempts among emergency department medical patients: instrument and results from the P sychiatric E mergency R esearch C ollaboration. Suicide Life Threat Behav. (2013) 43:313–23. doi: 10.1111/sltb.12018
13. Beghi M, Rosenbaum JF, Cerri C, Cornaggia CM. Risk factors for fatal and nonfatal repetition of suicide attempts: a literature review. Neuropsychiatr Dis Treat. (2013) 9:1725–36. doi: 10.2147/NDT.S40213
14. Bhaskaran J, Wang Y, Roos L, Sareen J, Skakum K, Bolton JM. Method of suicide attempt and reaction to survival as predictors of repeat suicide attempts: a longitudinal analysis. J Clin Psychiatry. (2014) 75:802–8. doi: 10.4088/JCP.13m08879
15. Daigle MS, Pouliot L, Chagnon F, Greenfield B, Mishara B. Suicide attempts: prevention of repetition. Can J Psychiatry. (2011) 56:621–9. doi: 10.1177/070674371105601008
16. Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm: systematic review. Br J Psychiatry. (2002) 181:193–9. doi: 10.1192/bjp.181.3.193
17. Wasserman D, Carli V, Wasserman C, Apter A, Balazs J, Bobes J, et al. Saving and empowering young lives in Europe (SEYLE): a randomized controlled trial. BMC Public Health. (2010) 10:1–14. doi: 10.1186/1471-2458-10-192
18. Fountoulakis KN, Koupidis SA, Siamouli M, Grammatikopoulos IA, Theodorakis PN. Suicide, recession, and unemployment. Lancet. (2013) 381:721–2. doi: 10.1016/S0140-6736(13)60573-5
19. Amiri B, Pourreza A, Rahimi Foroushani A, Hosseini SM, Poorolajal J. Suicide and associated risk factors in Hamadan province, west of Iran, in 2008 and 2009. J Res Health Sci. (2012) 12:88–92.
20. Esang M, Ahmed S. A closer look at substance use and suicide. Am J Psychiatry Resid J. (2018) 13:6–8. doi: 10.1176/appi.ajp-rj.2018.130603
21. Brezo J, Paris J, Tremblay R, Vitaro F, Hébert M, Turecki G. Identifying correlates of suicide attempts in suicidal ideators: a population-based study. Psychol Med. (2007) 37:1551. doi: 10.1017/S0033291707000803
22. Klonsky ED, May A. Rethinking impulsivity in suicide. Suicide Life Threat Behav. (2010) 40:612–9. doi: 10.1521/suli.2010.40.6.612
23. Forman EM, Berk MS, Henriques GR, Brown GK, Beck AT. History of multiple suicide attempts as a behavioral marker of severe psychopathology. Am J Psychiatry. (2004) 161:437–43. doi: 10.1176/appi.ajp.161.3.437
24. Park CHK, Lee JW, Lee SY, Moon J, Jeon D-W, Shim S-H, et al. Suicide risk factors across suicidal ideators, single suicide attempters, and multiple suicide attempters. J Psychiatr Res. (2020) 131:1–8. doi: 10.1016/j.jpsychires.2020.08.018
25. Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L. Age-and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry. (1999) 38:1497–505. doi: 10.1097/00004583-199912000-00010
26. Bachmann S. Epidemiology of suicide and the psychiatric perspective. Int J Environ Res. (2018) 15:1425. doi: 10.3390/ijerph15071425
27. Chang B, Gitlin D, Patel R. The depressed patient and suicidal patient in the emergency department: evidence-based management and treatment strategies. Emerg Med Pract. (2011) 13:1–23. Available online at: https://pubmed.ncbi.nlm.nih.gov/22164363/
28. Skinner R, McFaull S, Draca J, Frechette M, Kaur J, Pearson C, et al. Suicide and self-inflicted injury hospitalizations in Canada (1979 to 2014/15). HPCDP. (2016) 36:243–51. doi: 10.24095/hpcdp.36.11.02
29. Gbd 2015 Mortality and Cause of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the global burden of disease study 2015. Lancet. (2016) 388:1459–544. doi: 10.1016/S0140-6736(16)31012-1
30. Kuehner C. Gender differences in unipolar depression: an update of epidemiological findings and possible explanations. Acta Psychiatr Scand. (2003) 108:163–74. doi: 10.1034/j.1600-0447.2003.00204.x
31. Qin P, Agerbo E, Mortensen P. Suicide risk in relation to socioecomonic, demographic, psychiatric and familial factors. Eur Psychiatry. (2002) 17(S1):138s–s. doi: 10.1016/S0924-9338(02)80606-X
32. World Health Organization. Social Determinants of Health. Geneva: WHO Regional Office for South-East Asia (2008).
33. Bonde JPE. Psychosocial factors at work and risk of depression: a systematic review of the epidemiological evidence. Occup Environ Med. (2008) 65:438–45. doi: 10.1136/oem.2007.038430
34. Dutheil F, Aubert C, Pereira B, Dambrun M, Moustafa F, Mermillod M, et al. Suicide among physicians and health-care workers: a systematic review and meta-analysis. PLoS ONE. (2019) 14:e0226361. doi: 10.1371/journal.pone.0226361
35. Nedjat S, Mehrdad R, Yunesian M, Pouragha H, Biagi V, Monazzam-Esmaeelpour MR. Prospective cohort study on the social determinants of health: Tehran University of Medical Sciences employeescohort (TEC) study protocol. BMC Public Health. (2020) 20:1–7. doi: 10.1186/s12889-020-09798-9
36. Kessler RC, Üstün TB. The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI). Int J Methods Psychiatr Res. (2004) 13:93–121. doi: 10.1002/mpr.168
37. Sartipi M, Nedjat S, Mansournia MA, Baigi V, Fotouhi A. Assets as a socioeconomic status index: categorical principal components analysis vs. latent class analysis. Arch Iran Med. (2016) 19: 791–6. Available online at: https://pubmed.ncbi.nlm.nih.gov/27845549/
38. Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. (2006) 21:459–68. doi: 10.1093/heapol/czl029
39. Clarke DM, Kissane DW. Demoralization: its phenomenology and importance. Aust N Z J Psychiatry. (2002) 36:733–42. doi: 10.1046/j.1440-1614.2002.01086.x
40. Costanza A, Vasileios C, Ambrosetti J, Shah S, Amerio A, Aguglia A, et al. Demoralization in suicide: a systematic review. J Psychosom Res. (2022) 157:110788. doi: 10.1016/j.jpsychores.2022.110788
41. Ji YD, Robertson FC, Patel NA, Peacock ZS, Resnick CM. Assessment of risk factors for suicide among US health care professionals. JAMA Surg. (2020) 155:713–21. doi: 10.1001/jamasurg.2020.1338
42. World Health Organization. Suicide in the World: Global Health Estimates. Geneva: World Health Organization (2019). Available online at: https://apps.who.int/iris/handle/10665/326948 (accesed August 3, 2023).
43. Harriss L, Hawton K, Zahl D. Value of measuring suicidal intent in the assessment of people attending hospital following self-poisoning or self-injury. Br J Psychiatry. (2005) 186:60–6. doi: 10.1192/bjp.186.1.60
44. Denning DG, Conwell Y, King D, Cox C. Method choice, intent, and gender in completed suicide. Suicide Life Threat Behav. (2000) 30:282–8. Available online at: https://pubmed.ncbi.nlm.nih.gov/11079640/
45. Haw C, Casey D, Holmes J, Hawton K. Suicidal intent and method of self-harm: a large-scale study of self-harm patients presenting to a general hospital. Suicide Life Threat Behav. (2015) 45:732–46. doi: 10.1111/sltb.12168
46. Schrijvers DL, Bollen J, Sabbe BG. The gender paradox in suicidal behavior and its impact on the suicidal process. J Affect Disord. (2012) 138:19–26. doi: 10.1016/j.jad.2011.03.050
47. Freeman A, Mergl R, Kohls E, Székely A, Gusmao R, Arensman E, et al. A cross-national study on gender differences in suicide intent. BMC Psychiatry. (2017) 17:1–1. doi: 10.1186/s12888-017-1398-8
48. Scourfield J, Evans R. Why might men be more at risk of suicide after a relationship breakdown? Sociological insights. Am J Mens Health. (2015) 9:380–4. doi: 10.1177/1557988314546395
49. Cleary A. Suicidal action, emotional expression, and the performance of masculinities. Soc Sci Med. (2012) 74:498–505. doi: 10.1016/j.socscimed.2011.08.002
50. Rhodes AE, Boyle MH, Bridge JA, Sinyor M, Links PS, Tonmyr L, et al. Antecedents and sex/gender differences in youth suicidal behavior. World J Psychiatry. (2014) 4:120. doi: 10.5498/wjp.v4.i4.120
51. Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J Abnorm Psychol. (2019) 128:185. doi: 10.1037/abn0000410
52. Palhares-Alves HN, Palhares DM, Laranjeira R, Nogueira-Martins LA, Sanchez ZM. Suicide among physicians in the state of São Paulo, Brazil, across one decade. Braz J Psychiatry. (2015) 37:146–9. doi: 10.1590/1516-4446-2014-1534
53. Kposowa AJ. Divorce and suicide risk. J Epidemiol Community Health. (2003) 57:993. doi: 10.1136/jech.57.12.993
54. Liu B-P, Zhang J, Chu J, Qiu H-M, Jia C-X, Hennessy DA. Negative life events as triggers on suicide attempt in rural China: a case-crossover study. Psychiatry Res. (2019) 276:100–6. doi: 10.1016/j.psychres.2019.04.008
55. Miranda-Mendizabal A, Castellví P, Parés-Badell O, Alayo I, Almenara J, Alonso I, et al. Gender differences in suicidal behavior in adolescents and young adults: systematic review and meta-analysis of longitudinal studies. Int J Public Health. (2019) 64:265–83. doi: 10.1007/s00038-018-1196-1
56. Nordentoft M, Branner J. Gender differences in suicidal intent and choice of method among suicide attempters. Crisis. (2008) 29:209–12. doi: 10.1027/0227-5910.29.4.209
57. Sullivan S, Germain ML. Psychosocial risks of healthcare professionals and occupational suicide. Ind Commer Train. (2019) 52:1–14. doi: 10.1108/ICT-08-2019-0081
58. Agerbo E, Gunnell D, Bonde JP, Mortensen PB, Nordentoft M. Suicide and occupation: the impact of socio-economic, demographic and psychiatric differences. Psychol Med. (2007) 37:1131–40. doi: 10.1017/S0033291707000487
60. Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. (2016) 387:1227–39. doi: 10.1016/S0140-6736(15)00234-2
61. Dyrbye LN, Thomas MR, Massie FS, Power DV, Eacker A, Harper W, et al. Burnout and suicidal ideation among US medical students. Ann Intern Med. (2008) 149:334–41. doi: 10.7326/0003-4819-149-5-200809020-00008
62. Windsor-Shellard B, Gunnell D. Occupation-specific suicide risk in England: 2011–2015. Br J Psychiatry. (2019) 1–6. doi: 10.1192/bjp.2019.69. [Epub ahead of print].
63. Kim S-Y, Shin D-W, Oh K-S, Kim E-J, Park Y-R, Shin Y-C, et al. Gender differences of occupational stress associated with suicidal ideation among South Korean employees: the Kangbuk Samsung Health Study. Psychiatry Investig. (2018) 15:156. doi: 10.30773/pi.2017.05.31.1
Keywords: suicide, suicidal behavioral, employed in the medical area, demoralization, suicide ideation and behavior
Citation: Rezaei Z, Mohammadi S, Aghaei A, Pouragha H, Latifi A and Keshavarz-Mohammadi N (2023) Assessment of risk factors for suicidal behavior: results from the Tehran University of Medical Sciences Employees' Cohort study. Front. Public Health 11:1180250. doi: 10.3389/fpubh.2023.1180250
Received: 05 March 2023; Accepted: 19 July 2023;
Published: 22 August 2023.
Edited by:
Michal Grivna, United Arab Emirates University, United Arab EmiratesReviewed by:
Aurelio Luna, University of Murcia, SpainAlessandra Costanza, University of Geneva, Switzerland
Copyright © 2023 Rezaei, Mohammadi, Aghaei, Pouragha, Latifi and Keshavarz-Mohammadi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Arman Latifi, bGF0aWZpYXJtYW5AZ21haWwuY29t; Nastaran Keshavarz-Mohammadi, bl9rZXNoYXZhcnNAeWFob28uY29t
†ORCID: Zahed Rezaei orcid.org/0000-0001-7331-4500
Samira Mohammadi orcid.org/0000-0001-8921-4045
Abbas Aghaei orcid.org/0000-0001-9612-1250
Hamidreza Pouragha orcid.org/0000-0002-9748-2864
Arman Latifi orcid.org/0000-0002-6823-0561
Nastaran Keshavarz-Mohammadi orcid.org/0000-0001-6475-3587
 Zahed Rezaei1,2†
Zahed Rezaei1,2† Abbas Aghaei
Abbas Aghaei Hamidreza Pouragha
Hamidreza Pouragha Arman Latifi
Arman Latifi Nastaran Keshavarz-Mohammadi
Nastaran Keshavarz-Mohammadi