- 1SISU Intercultural Institute (SII), Shanghai International Studies University (SISU), Shanghai, China
- 2School of Commerce and Accountancy, University of Management and Technology (UMT), Lahore, Punjab, Pakistan
Objective: The study aims to document sociodemographic features, address the symptoms and levels of depression, anxiety, and stress among frontline doctors in Pakistan, and validate the depression, anxiety, stress scale (DASS-21) on the context of Pakistan.
Method: A cross-sectional survey was conducted throughout the regions of Pakistan on frontline doctors to document their sociodemographic patterns and the levels of depression, anxiety, and stress while dealing with the fifth wave (Omicron-variant) of the coronavirus (SARS-CoV-2) pandemic in Pakistan (December 2021–April 2022). Respondents (N = 319) were recruited through a snowball sampling process.
Results: Though previous literature reported declines in psychological symptoms after earlier waves of COVID-19, these DASS-21 findings show that as the pandemic has worn on, frontline doctors in Pakistan are having considerable personal symptoms of depression (72.7%), anxiety (70.2%), and stress (58.3%). Though specifically related to the COVID-19 pandemic, they rated only moderate levels of depression and stress, however they reported severe levels of anxiety. The results also revealed a positive correlation between depression and anxiety (r = 0.696, p < 0.001), depression and stress (r = 0.761, p < 0.001), and anxiety and stress (r = 0.720, p < 0.001).
Conclusion: Through the application of all required statistical procedures, DASS-21 is validated in the cultural context of Pakistan among this group of frontline doctors. The findings of this study can provide new directions for the policy makers (government and hospitals' administration) of Pakistan to focus on the mental wellbeing of the doctors under similar enduring public health crises and to protect them from short- or long-term disorders.
1. Introduction
The coronavirus (SARS-CoV-2) was reported to have emerged from the city of Wuhan in Hubei province in China and later reported to spread rapidly in different parts of the world within the following months. Its most common symptoms have been equated with flu, high fever, dry cough, sore throat, loss of taste, with frequent impact on the lungs and respiratory system creating breathing difficulties, and with some cases leading to death (1, 2). The speedy transmission, heavy upsurge of infections, and associated deaths have created a sense of panic across the world (3). As the pandemic wave(s) spread, most countries declared the novel corona virus to be a public health emergency and took precautionary measures such as social distancing, isolation, quarantines, and wearing masks (4) to reduce its dispersion (5) aiming to protect their citizens.
Other than physical health, implementation of lockdowns (restricting populations to stay in and work from home) along with inadequate information or uncertain measures to protect themselves or vulnerable loved ones have created varying types of psychological distress among people worldwide (6). Fears of being infected or isolated in quarantines have adversely affected many as they felt compelled to distance themselves from their peers, colleagues, families, and other social contacts (7). Seeking to deal with the uncertainties and possible implications of COVID-19 has impacted human psychology at many levels, including increasing fear, stress, anger (8), depression, anxiety, and in worst case scenarios, suicidal tendencies (9). It has also been reported that pandemic distress coupled with certain extreme preventive measures could trigger other pre-existing mental health diseases and even induce novel symptoms in those who previously did not have any mental health issues (10).
COVID-19 pandemic related studies across various regions have documented different psychological factors that directly and indirectly affect the mental health of almost every segment of the population (11). Special attention has been given to the impacts on medical workers around the world (12–15) as they were both directly exposed to COVID-19 patients and psychologically faced with additional self- and other-care challenges. Studies conducted in diverse cultural contexts such as, Israel, Turkey, Egypt, India, the United States, Saudi Arabia, China, Kuwait, Iran, Poland, and Bangladesh (16–26) have noted and examined the unique issues and implications facing medical staff during the COVID-19 pandemic. However, neither the context nor challenges facing doctors in Pakistan have been widely reported in recent literature especially during the fifth wave of COVID-19.
Pakistan presents an interesting and important case for a national context as a highly populated (220 million) under-developed country and one already facing the multiple challenges of an energy crisis, weak economy, and political instability. A health emergency was declared in Pakistan right after the initial infected COVID-19 cases gained momentum. Partial and smart lockdowns, vaccinations, and improved treatment policies have helped Pakistan to control the transmission of the virus to protect the general citizens of the country (27).
An earlier investigation about the COVID-19 pandemic on seven different Asian countries (including Pakistan) found that the people of Thailand and Pakistan scored very high on the depression anxiety stress scale (DASS-21) as compared to the other countries (28). A study on the Punjab province of Pakistan reported that 21.9% of depression and 21.4% of anxiety symptoms were witnessed among the health care workers (HCW) and that the most affected population was medical doctors (29). It is also found that 79.7% of the HCW in Pakistan were having very high levels of and severe anxiety issues concerning COVID-19 (7). Researchers interviewed thirteen young doctors and found that they were experiencing psychological distress in the form of increased stress, fear, and anxiety after the emergence of the COVID-19 pandemic in Pakistan (30). Another sample reported that 43% of anxiety/depression prevailed among the frontline doctors of Pakistan in 2020 (31). Clearly, HCW in Pakistan have been more exposed to COVID-19 as elsewhere, and as an important health service sector that every country looks to in such distressing pandemic situations, their responses, wellbeing, and mental health cannot be overlooked.
The abovementioned studies provide evidence that HCW and frontline doctors are among the most vulnerable populations at a higher risk who are also more exposed to COVID-19 cases on a frequent and long-term basis as compared to ordinary people (in Pakistan as in other nations). Unfortunately, most of previous studies were completed during the initial waves of COVID-19 and did not adopt a well-established scale (like the DASS-21) to document the levels of depression, anxiety, and stress specifically of doctors. DASS-21 is widely considered to effectively address the symptoms of depression, anxiety, and stress (32) which indicate the mental health of the general populace rather than a clinical population. Research gaps exist in not examining the fifth wave of COVID-19, application of DASS-21, and specifically not yet targeting the frontline doctors in Pakistan. Therefore, the current study aims to address and consider the connections between these previously unexplored areas by incorporating the DASS-21 to apply this instrument to the frontline doctors of Pakistan during fifth wave of COVID-19.
2. Methods
2.1. Respondent and procedures
An online survey (through Google Forms) was created to capture the responses of frontline doctors who were directly dealing with the COVID-19 patients during the fifth wave in Pakistan. In the scenario of this emergency, limited access due to pandemic measures, and seeking broader reach, we resorted to utilizing a snowball sampling technique and approached a couple of doctors that could be accessed to participate in this study and help recruit others. The survey form was shared with them through different social networking platforms. The consent form clearly stated at the top of the survey that their responses and identities would be kept confidential, and if they feel uncomfortable while filling in the survey that they can leave it at any stage. The overall process of data collection took 3 months: starting from February 2022 and ending in April 2022 (at the time that the fifth was considered over).
Considerations regarding the selected sample size include: First, the recommended, calculated minimum sample size was 10 participants for each scale item. Regardless of the number of items on a scale, at least 210–310 participants are recommended for factor analysis (33). The sample size (N = 319) in our study was sufficient according to the ideal ratio of items (10:1). Second, the former relevant studies have considered healthcare workers or professionals (including doctors) as their samples (29–31). Representative size may be questioned, yet the current study has only focused on the frontline doctors compared to the entire medical staff (representation is intentionally limed to this select and important group). Third is the size needed for analysis, whereby structural equation modeling (SEM) requires a minimum of 200 and a maximum of 500 samples for the data analysis regarding the estimation of good results (34). Therefore, the samples (N = 319) of this current research were in between these two thresholds and considered adequately suited for final analysis.
2.2. Survey instrument
The survey form was entirely designed in English with two major sections. The first section elicited standard sociodemographic features such as area, gender, age, etc. and for section two, the DASS-21 instrument (35) was adopted to measure the levels of depression, anxiety, and stress of the doctors. Section one was further classified into ten major sociodemographic questions including area, gender, age, marital status, workplace, job title, current area of practice and work. In addition, two questions about the media preference and the consumption of COVID-19 related news on that specific media channel/portal were also included in this section. To assess psychological states, the DASS-21 instrument contains a total of 21 items with 7 items for each of the three dimensions (depression, anxiety, and stress) respectively. Participating medical doctors were encouraged to rate their responses about the current situation which they were facing in the midst of the fifth wave of COVID-19. A four-point Likert type scale was incorporated to capture their responses ranging from 0 (did not apply to me at all) to 3 (applied to me very much) to avoid mid-point non-meaningful responses. The lower scores represent a normal range; however, the higher scores indicate a more severe emotional situation affecting the doctors. This instrument has previously been shown to exhibit very high reliability and validity and used in a very recent study (32). Furthermore, the validity and reliability of DASS-21 during the COVID-19 period have also been confirmed (36). It has robust validity and reliability values. We therefore employed the original and still widely used version of the scale for the current study.
2.3. Statistical analysis
All statistical procedures were first evaluated using the Statistical Package for Social Sciences (SPSS) version 23.0 and later the reliability and validity of DASS-21 were processed by the Analysis of a Moment Structures (AMOS) version 23.0. In SPSS, the descriptive statistics and one-way ANOVA were performed to report the frequency and percentages of all sociodemographic features of the participants and to document the significant differences among each demographic sub-section. In addition, the individual scores for depression, anxiety, and stress as well as the overall scores of DASS-21 were also evaluated. All essential aspects for testing the reliability and validity of DASS-21 were examined in AMOS.
3. Results
3.1. Respondents' features
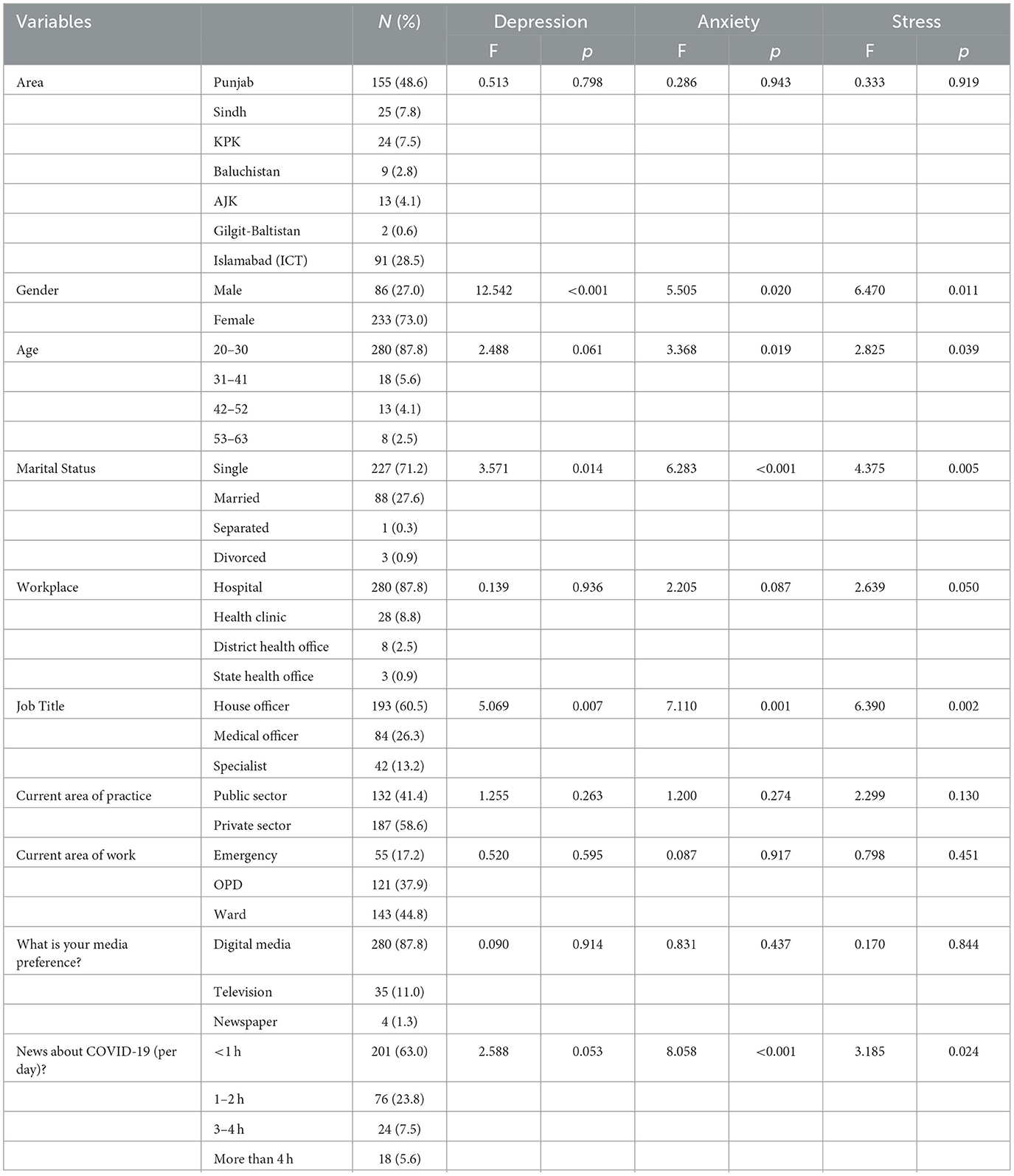
In this study, a total of 319 frontline doctors completed the survey form. The sociodemographic details of the respondents are presented in Table 1 (through SPSS). Many frontline doctors belonged to the Pakistan region of Punjab (N = 155, 48.6%) and 87.8% of the respondents were young with an age range between 20 and 30. Female doctors heavily dominated the sample set with 73%. Regarding marital status, those separated/divorced participants were minimal (only 1.2% of the sample) and most were single (N = 227, 71.2%). In terms of their workplace and job title, 87.8% of the doctors were directly associated with the hospitals and 60.5% were titled as the house officers. Most of them were working in the private sector (N = 176, 55.2%) and performing their duties in wards (N = 143, 44.8%). Regarding media use, a large majority of doctors (N = 280) preferred digital media over newspapers and television. 63% of the frontline doctors reported they consume any form of media for less than an hour daily, mainly to update themselves on news regarding COVID-19, thus can be considered minimal and functional or information-oriented media consumers.
3.2. Levels of depression, anxiety, and stress of frontline doctors
The significant differences regarding the three facets (depression, anxiety, and stress) of DASS-21 among each demographic feature were evaluated based on the one-way ANOVA results. The findings revealed that there were significant differences between the sub-categories of gender (F = 12.542, p < 0.05; F = 5.505, p < 0.05; F = 6.470, p < 0.05), marital status (F = 3.571, p < 0.05; F = 6.283, p < 0.05; F = 4.375, p < 0.05), and job title (F = 5.069, p < 0.05; F = 7.110 p < 0.05; F = 6.390, p < 0.05) of the frontline doctors in reporting depression, anxiety, and stress. In addition, significant differences were also witnessed among the age (F = 3.368, p < 0.05; F = 2.825, p < 0.05) and daily media coverage consumption (F = 8.058, p < 0.05; F = 3.185, p < 0.05) between the doctors concerning the levels of anxiety and stress. However, the other sub-categories of respondents' profile (i.e., area, workplace, area of practice and others) did not have any statistically significant differences regarding the levels of depression, anxiety, and stress. To highlight these findings, the significant values obtained from one-way ANOVA for depression, anxiety, and stress against every sociodemographic feature are stated in Table 1.
The overall trend (Table 2) of the scores revealed that the frontline doctors were having noticeable symptoms of all three: depression (N = 232, 72.7%), anxiety (N = 224, 70.2%), and stress (N = 186, 58.3%). The depression symptoms range among respondents were extremely severe (22.9%), severe (10.7%), moderate (23.8%), and mild (15.4%) respectively. Less intense, the symptoms of anxiety ranged from 8.5% as mild, 14.4% as moderate, 11.6% as severe, and 35.7% as extremely severe in frontline doctors. The participants' reported stress symptoms ranging from 16.3% extremely severe, 17.6% severe, 14.7% moderate, and 9.7% mild. Furthermore, the mean scores for DASS-21 (M = 51.69) and its subscales were also calculated to evaluate the exact level of depression (M = 17.31), anxiety (M = 15.24), and stress (M = 19.14) among the frontline doctors. The mean scores highlighted that the frontline doctors of Pakistan were having severe levels of anxiety and moderate levels of depression and stress.
3.3. Reliability and validity of the DASS-21
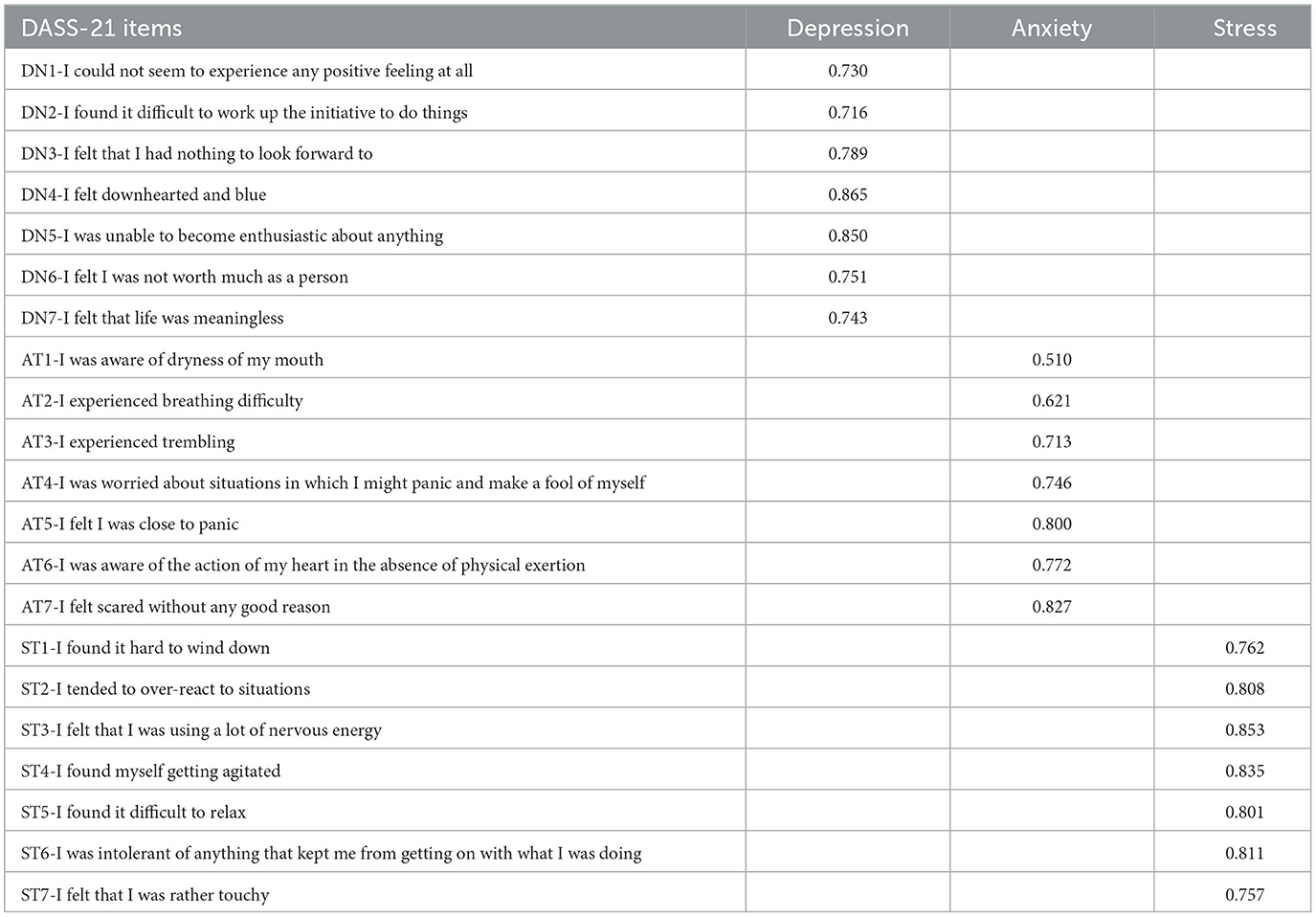
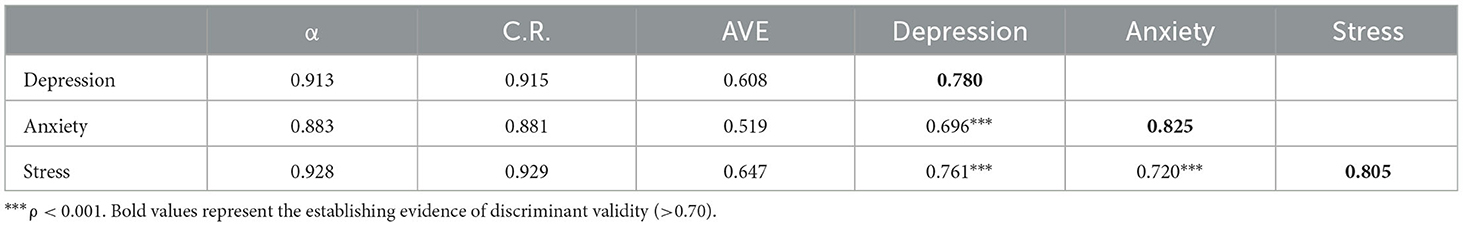
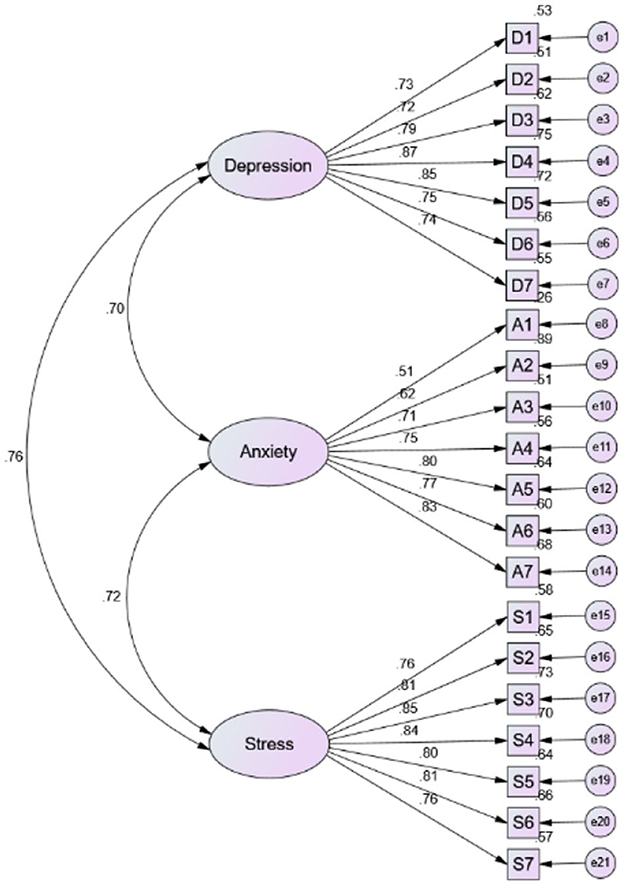
An assessment of DASS-21 was carried out in AMOS, to reconfirm its reliability and validity among the frontline doctors in the context of Pakistan. The process of evaluation was done by considering different approaches such as alpha values, composite reliability (C.R.), confirmatory factor analysis (CFA), construct and convergent validity, and fitness indices in AMOS. The model has fulfilled the minimum required values suggested by the literature (34) regarding CFA (>0.50) and reliability (Table 3). The DASS-21 showed an overall excellent internal consistency reliability (Cronbach's α = 0.953, McDonald's ω = 0.954) as well as for its sub-scales such as, Depression (Cronbach's α = 0.913, McDonald's ω = 0.917), Anxiety (Cronbach's α = 0.883, McDonald's ω = 0.884), and Stress (Cronbach's α = 0.928, McDonald's ω = 0.928). Furthermore, for each factor, all the square roots of average variance extracted (AVE) are highlighted in bold and shown (Table 4) to be greater than the coefficients or off-diagonal elements in the corresponding rows and columns, thus establishing evidence of discriminant validity (>0.70).
Table 4 also indicates that the C.R. values for depression (0.915), anxiety (0.881), and stress (0.926) were relatively higher than the minimum limit of acceptance (>0.70). In addition, the values of AVE for depression, anxiety, and stress were 0.608, 0.519, and 0.617 respectively. It reconfirms that the values have crossed the required minimum threshold (>0.50). Lastly, the fitness indices confirmed that the data were well fitted with the measurement model of DASS-21 which indicates the attainment of construct validity: χ2 = 302.015, χ2/dF = 1.67, SRMR = 0.040, GFI = 0.920, NFI = 0.937, IFI =0.973, TLI 0.969, CFI = 0.973, PNFI 0.803, and RMSEA = 0.046 (37, 38). The measurement model of DASS-21 is presented in Figure 1. Therefore, these procedures of instrument testing confirmed that the use of DASS-21 is validated among the frontline doctors in the cultural context of Pakistan.
3.4. Correlations
The correlations between depression, anxiety, and stress were also examined in the current study (Table 4). The findings revealed that depression was positively and significantly correlated with anxiety (r = 0.696, p < 0.001) and stress (r = 0.761, p < 0.001). Furthermore, a positive and significant association between anxiety and stress (r = 0.720, p < 0.001) was also witnessed from the findings of this present study.
4. Discussion
The study aimed to fill noted gaps to extend pandemic research to document the symptoms and levels of depression, anxiety, and stress among the frontline doctors in Pakistan during the fifth wave of COVID-19, and to validate DASS-21 in the context of Pakistan. Past research in Pakistan tended to focus mainly on HCW but could not be extrapolated to project the special case situation or psychological orientations faced by frontline doctors who had to actively deal with a pandemic that lasted several years and face the unabating needs of COVID-19 patients. Most of the previous research had been carried out during the initial waves of COVID-19 and though contributing much toward general understandings of the psychological effects of a pandemic, had not yet found ways to study the ongoing mental health of frontline doctors, especially during this late stage, in the fifth wave of COVID-19. Most importantly, a well-established scale (DASS-21) had not been previously considered or validated, either in Pakistan or tested for its effectiveness in determining which psychological symptoms arise more prominently in medical or para-medical staff. Therefore, connecting all the above-mentioned limitations, the current study is designed to fill the gaps in the existing literature.
It is evident in this study that 72.7% of doctors were having the symptoms of depression, 70.2% were having anxiety, and 58.3% were dealing with stress arising from the COVID-19 pandemic. The findings revealed that the psychological symptoms reported during the fifth wave of COVID-19 are much higher than the previously documented symptoms had been during the start of pandemic (29). This may be a logical finding from an ongoing pandemic, but has not been studied or confirmed previously, nor the impact expected to this hight degree. In addition, doctors rated moderate levels of depression and stress, but severe levels of anxiety specifically related to COVID-19 issues. The levels are in line with the findings of previous research which reported the severity of anxiety among the HCW in Pakistan (7). It has been reported that the symptoms and levels of depression, anxiety, and stress are more intense over time as compared to the earlier studies (30, 31). In comparison to the normal populace, it seems that mental health of the frontline doctors is seriously affected and considerably worse since the emergence of COVID-19 pandemic, suggesting that their needs may need to be recognized and better dealt with. Even though the treatment system has been improved and multiple vaccines are available and have been administered broadly, medical doctors are still facing psychological challenges.
In terms of the validation of DASS-21, the results of multiple statistical procedures essential for the attainment of reliability and validity of any measurement tool were fulfilled in the current study. There is abundant evidence available in the literature that has confirmed that DASS-21 is a reliable and valid scale for the assessment of depression, anxiety, and stress symptoms among various cultural contexts (32, 35). However, very few studies are available that confirm DASS-21 as a valid measurement tool in the cultural context of Pakistan, and if so, most have been applied to the general public (28) not specifically to the frontline doctors of Pakistan. The findings of this investigation revealed that DASS-21 is a valid and reliable measurement tool to document the depression, anxiety, and stress symptoms of frontline doctors during the fifth wave of COVID-19 on the cultural setting of Pakistan.
Though it has been established that mental health challenges are not limited to ordinary citizens or persons that have already been diagnosed as having mental health diseases, this study shows that those professionals that society relies on most during times of international health crises suffer at higher rates than might be expected. COVID-19 studies have already warned the world that the pandemic will likely have lasting impacts on the masses. The findings of the existing study have reconfirmed their predictions. Continuing in the line of studies that have examined HCW and the medical profession, this study shows even more clearly that even doctors, who are trained to deal with crises and have many such experiences, are not unaffected by its impacts, and in fact, perhaps suffer far more than expected. Pakistan has excellent medical doctor training, and its physicians are expected to perform an important role in the stability of society. Therefore, findings like these on the existence of serious levels of depression, anxiety, and stress among them even (or especially after dealing with several years of this pandemic) cannot be neglected due to the potential adverse effects on the society.
The pandemic may now have subsided, but more research is needed to determine if there are any long-term psychological syndromes that linger among medical professionals. Facing such facts, both policy makers and administrators need to ensure more support and assistance focused on frontline doctors. Their mental health can be improved or maintained primarily through two main bodies: the government and hospitals. The government should focus on providing certain seminars or training sessions for the counseling of their frontline doctors to secure and ensure their mental health. The hospitals and doctors' associations could regularly monitor their mental wellbeing and provide treatments to their HCW. Though effective strategies based on such research findings, Pakistan or other countries with similar conditions might be able to provide better medical conditions and staff support to effectively serve public health needs.
4.1. Limitations
Potential limitations associated with this study include its snowball, cross-sectional design, and inability to explore further effects. The cross-sectional research technique was incorporated as the only viable option under the pandemic conditions and constraints at that time, and the design proved unable to effectively examine the direct cause and effects among different factors. In this study, it was also a limitation that the samples gathered were mostly females (with no clear reasons why fewer male doctors responded), thus gender responses can be explored further, as well as what long-term effects might be noted regarding the mental health of either gender group. The responses are also noted to be time- and situation-sensitive and might change under future conditions, representing a common limitation of survey research. Fourth, the reliability of the participants' answers may be problematic because our study was conducted online. However, online data collection was not just preferable but the only viable option, as the survey was conducted during COVID-19 pandemic measures. Thus, conclusions drawn can only be tentative and generalized to situations like those examined. Future researchers could identify personality and situational factors that might directly be influencing the depression, anxiety, and stress symptoms of the doctors or compare the scores of DASS-21 with other developing or developed countries.
5. Conclusion
The mental wellbeing of the frontline doctors is a necessity for any country or nation during both normal and emergency situations like the COVID-19 pandemic. The current study has shed light on the alarming symptoms and higher-than-expected levels of depression, anxiety, and stress among the frontline doctors who have had to cope with the fifth wave of COVID-19 in Pakistan. Highlighting this issue warrants serious consideration from the government and both public and private hospitals' management. The policy makers in Pakistan or similar countries need to frame new polices to ensure their doctor's wellbeing which can ultimately influence the betterment of health in the society. The present study also validated the established DASS-21 instrument in the cultural context of Pakistan. Future research could seek to identify personality and situational factors that are directly influencing the depression, anxiety, and stress of doctors to consider correlations between factors or moderating variables. More studies targeting the long-term impacts of COVID-19 and the post-pandemic situation on the mental health of doctors or other health care populations will be beneficial for a greater understanding concerning the nature and influences of these past and future pandemics.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Ethics Review Committee of the SISU Intercultural Institute (SII), Shanghai International Studies University (SISU), China (2022-SII/IRB-0103). The patients/participants provided their written informed consent to participate in this study.
Author contributions
MN: investigation, conceptualization, methodology, validation, data collection, formal analysis, and writing—original draft preparation. SK: conceptualization, methodology, resources, and writing—review and editing. IB: conceptualization, formal analysis, and writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
This study was conducted as an extended part of the (Post-Doctoral) Research Program of the SISU Intercultural Institute, Shanghai International Studies University (SISU), Shanghai, China, related to the 2021-2024 SISU University Key Project Number: 2021114007 (Studies on the mechanisms of intercultural communication and interactions in international communication channels).
Acknowledgments
The authors acknowledge the contributions of Miss Meerab A. Harram and her team members in assisting with collecting data from these medical doctor samples during the COVID-19 pandemic. During a time when all were facing both distress and danger, we express our deep appreciation and gratitude for the efforts and help of each.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Uygur OF, Uygur H. Association of post-COVID-19 fatigue with mental health problems and sociodemographic risk factors. Fatigue Biomed Health Behav. (2021) 9:196–208. doi: 10.1080/21641846.2021.2000251
2. Cirrincione L, Plescia F, Ledda C, Rapisarda V, Martorana D, Moldovan RE, et al. COVID-19 pandemic: prevention and protection measures to be adopted at the workplace. Sustainability. (2020) 12:3603. doi: 10.3390/su12093603
3. Elbay RY, Kurtulmuş A, Arpacioglu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in COVID-19 pandemics. Psychi Res. (2020) 290:113130. doi: 10.1016/j.psychres.2020.113130
4. Zhang XY, English AS, Kulich SJ, Chen YX. How mask gap impacts discrimination and anxiety during COVID-19: a study on overseas Chinese during the first outbreak in 2020. Soc Pers Psyc Compass. (2023) e12793. doi: 10.1111/spc3.12793
5. Pedrosa AL, Bitencourt L, Fróes ACF, Cazumbá MLB, Campos RGB, de Brito SBCS, et al. Emotional, behavioral, and psychological impact of the COVID-19 pandemic. Front Psychol. (2020) 11:566212. doi: 10.3389/fpsyg.2020.566212
6. Kulich SJ, Komisarof A, Smith LR, Cushner K. Re-examining intercultural research and relations in the COVID pandemic. Int J of Inter Relations. (2021) 80:A1–6. doi: 10.1016/j.ijintrel.2020.12.003
7. Saleem Z, Majeed MM, Rafique S, Siqqiqui Z, Ghandhi D, Tariq H, et al. COVID-19 pandemic fear and anxiety among healthcare professionals in Pakistan. Res Squ. (2020) 1–16. doi: 10.21203/rs.3.rs-37608/v2
8. Li X, English AS, Kulich SJ. Anger among Chinese migrants amid COVID-19 discrimination: the role of host news coverage, cultural distance, and national identity. PLoS ONE. (2021) 16:866. doi: 10.1371/journal.pone.0259866
9. Torales J, O'Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. (2020) 66:317–20. doi: 10.1177/0020764020915212
10. Cullen W, Gulati G, Kelly BD. Mental health in the COVID-19 pandemic. QJM. (2020) 11:311–2. doi: 10.1093/qjmed/hcaa110
11. Wong LP, Farid NDN, Alias H, Yusop SM, Musa Z, Hu Z, et al. COVID-19 responses and coping in young Malaysians from low-income families. Front Psychiatry. (2023) 14:1165023. doi: 10.3389/fpsyt.2023.1165023
12. Badahdah AM, Khamis F, Al Mahyijari N. The psychological well-being of physicians during COVID-19 outbreak in Oman. Psychiatry Res. (2020) 289:113053. doi: 10.1016/j.psychres.2020.113053
13. Holas P, Wojtkowiak N, Gambin M, Hansen K, Kmita G, Pisula E, et al. Factors associated with burnout in Polish healthcare workers during the COVID-19 pandemic. Front Public Health. (2022) 10:1018612. doi: 10.3389/fpubh.2022.1018612
14. Hummel S, Oetjen N, Du J, Posenato E, Resende de Almeida RM, Losada R, et al. Mental health among medical professionals during the COVID-19 pandemic in eight European countries: cross-sectional survey study. J Med Internet Res. (2021) 23:e24983. doi: 10.2196/24983
15. Nguyen HTH, Hoang AP, Vu LM, Tran DQ, Bui LK, Pham TT, et al. Prevalence of and risk factors associated with depression among nursing students acting on the frontline of COVID-19 pandemic: a cross-sectional study. Front Public Health. (2022) 10:1020419. doi: 10.3389/fpubh.2022.1020419
16. Mosheva M, Hertz-Palmor N, Dorman Ilan S, Matalon N, Pessach IM, Afek A, et al. Anxiety, pandemic-related stress and resilience among physicians during the COVID-19 pandemic. Depress Anxiety. (2020) 37:965–71. doi: 10.1002/da.23085
17. Ceri V, Cicek I. Psychological well-being, depression and stress during COVID-19 pandemic in Turkey: a comparative study of healthcare professionals and non-healthcare professionals. Psychol Health Med. (2021) 26:85–97. doi: 10.1080/13548506.2020.1859566
18. Khalaf OO, Khalil MA, Abdelmaksoud R. Coping with depression and anxiety in Egyptian physicians during COVID-19 pandemic. Middle East Curr Psychiatry. (2020) 27:1–7. doi: 10.1186/s43045-020-00070-9
19. Javadekar A, Javadekar S, Chaudhury S, Saldanha D. Depression, anxiety, stress, and sleep disturbances in doctors and general population during COVID-19 pandemic. Ind Psychiatry J. (2021) 30:20–4. doi: 10.4103/0972-6748.328783
20. Ofei-Dodoo S, Loo-Gross C, Kellerman R. Burnout, depression, anxiety, and stress among family physicians in Kansas responding to the COVID-19 pandemic. J Am Board Fam Med. (2021) 34:522–30. doi: 10.3122/jabfm.2021.03.200523
21. Almalki AH, Alzahrani MS, Alshehri FS, Alharbi A, Alkhudaydi SF, Alshahrani RS, et al. The psychological impact of COVID-19 on healthcare workers in Saudi Arabia: a year later into the pandemic. Front Psychiatry. (2021) 12:797545. doi: 10.3389/fpsyt.2021.797545
22. Zhou Z, Luo D, Yang BX, Liu Z. Machine learning-based prediction models for depression symptoms among Chinese healthcare workers during the early COVID-19 outbreak in 2020: a cross-sectional study. Front Psychiatry. (2022) 13:876995. doi: 10.3389/fpsyt.2022.876995
23. Alnaser MZ, Alotaibi N, Nadar MS, Manee F, Alrowayeh HN. Manifestation of generalized anxiety disorder and its association with somatic symptoms among occupational and physical therapists during the COVID-19 pandemic. Front Public Health. (2022) 10:891276. doi: 10.3389/fpubh.2022.891276
24. Hajebi A, Abbasinejad M, Zafar M, Hajebi A, Taremian F. Mental health, burnout, and job stressors among healthcare workers during the COVID-19 pandemic in Iran: a cross-sectional survey. Front Psychiatry. (2022) 13:891430. doi: 10.3389/fpsyt.2022.891430
25. Babicki M, Kowalski K. Bogudzi'nska B, Mastalerz-Migas A. Alterations in mental health and quality of life among healthcare workers in times of COVID-19: four-stage cross-sectional study during first four pandemic waves in Poland. Front Psychiatry. (2022) 13:1027734. doi: 10.3389/fpsyt.2022.1027734
26. Arefin S, Rashid T, Bhattacharjee M, Habib MD, Islam MA, Rahaman MA. The whole sky has broken down on me. I might die alone: a qualitative study on the lived experiences of COVID-19 positive frontline workers in Bangladesh. Front Sociol. (2022) 7:1054921. doi: 10.3389/fsoc.2022.1054921
27. Kamran K, Ali A. Challenges and strategies for Pakistan in the third wave of covid-19: a mini review. Front Public Health. (2021) 9:690820. doi: 10.3389/fpubh.2021.690820
28. Wang C, Tee M, Roy AE, Fardin MA, Srichokchatchawan W, Habib HA, et al. The impact of COVID-19 pandemic on physical and mental health of Asians: a study of seven middle-income countries in Asia. PloS One. (2021) 16:e0246824. doi: 10.1371/journal.pone.0246824
29. Salman M, Raza MH, Ul Mustafa Z, Khan TM, Asif N, Tahir H. The psychological effects of COVID-19 on frontline healthcare workers and how they are coping: a web-based, cross-sectional study from Pakistan. MedRxiv. (2020) 5:2020–26. doi: 10.1101/2020.06.03.20119867
30. Rashid A, Faisal K. Pandemic anxiety and its correlates among young doctors working frontline in Pakistan. Glo Men Hea. (2020) 7:e27. doi: 10.1017/gmh.2020.22
31. Amin F, Sharif S, Saeed R, Durrani N, Jilani D. COVID-19 pandemic-knowledge, perception, anxiety and depression among frontline doctors of Pakistan. BMC Psychi. (2020) 20:459. doi: 10.1186/s12888-020-02864-x
32. Makara-Studzińska M, Tyburski E, Załuski M, Adamczyk K, Mesterhazy J, Mesterhazy A. Confirmatory factor analysis of three versions of the depression anxiety stress scale (DASS-42, DASS-21, and DASS-12) in Polish adults. Front in Psychi. (2022) 12:2342. doi: 10.3389/fpsyt.2021.770532
33. Uygur OF, Uygur H, Chung S, Ahmed O, Demiroz D, Aydin EF, et al. Validity and reliability of the Turkish version of the glasgow sleep effort scale. Sleep Med. (2022) 98:144–51. doi: 10.1016/j.sleep.2022.06.022
34. Hair JF, Black B, Babin B, Anderson RE, Tatham RL. Multivariate Data Analysis: A Global Perspective. New Jersey, NJ: Pearson Education Inc, USA. (2010).
35. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
36. Uygur FU, Uygur H, Demiroz D, Ahmed O. COVID-19 Worry and related factors: Turkish adaptation and psychometric properties of the COVID-19 Worry Scale. Alpha Psychiatry. (2022) 23:276–83. doi: 10.5152/alphapsychiatry.2022.22926
37. Uygur OF, Ahmed O, Bahar A, Hursitoglu O, Aydin EF, Chung S, et al. Adaptation and validation of the Turkish version of the ford insomnia response to stress test in university students. Nat Sci Sleep. (2023) 15:139–49. doi: 10.2147/NSS.S398489
Keywords: COVID-19, depression, anxiety, stress, doctors, Pakistan
Citation: Nadeem MU, Kulich SJ and Bokhari IH (2023) The assessment and validation of the depression, anxiety, and stress scale (DASS-21) among frontline doctors in Pakistan during fifth wave of COVID-19. Front. Public Health 11:1192733. doi: 10.3389/fpubh.2023.1192733
Received: 24 March 2023; Accepted: 30 May 2023;
Published: 16 June 2023.
Edited by:
Mohammadreza Shalbafan, Iran University of Medical Sciences, IranReviewed by:
Nicholas Pang, Universiti Malaysia Sabah, MalaysiaÖmer Faruk Uygur, Ataturk University, Türkiye
Tao Xiang, The Affiliated Hospital of Southwest Jiaotong University, China
Copyright © 2023 Nadeem, Kulich and Bokhari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Muhammad Umar Nadeem, dW1hcm5hZGVlbUBzaGlzdS5lZHUuY24=
 Muhammad Umar Nadeem
Muhammad Umar Nadeem Steve J. Kulich1
Steve J. Kulich1