- 1School of Physical Education and Sport Science, Fujian Normal University, Fuzhou, China
- 2Institute of Physical Education, Huanggang Normal University, Huanggang, China
Objective: This study mainly used network meta-analysis to explore the effect of different types of exercise on hypertension in middle-aged and older adults.
Methods: Several databases (e.g., PubMed, Embase, and the Cochrane Library) were used to search for randomized controlled trials on the effects of different types of exercise on hypertension in middle-aged and older adults.
Results: A total of 19 articles and 2,385 participants were included in the analysis. Aerobic exercise interventions [MD = −9.254, P < 0.05, 95% CI (−14.810, −3.698)] and static exercise interventions [MD = −10.465, P < 0.05, 95% CI (−18.135, −2.794)] had a significant effect on the improvement in systolic blood pressure (SBP). For diastolic blood pressure (DBP), aerobic exercise interventions [MD = −1.4096; P > 0.05, 95% CI (−8.2395, 5.4201)] and static exercise interventions [MD = −4.5206, P > 0.05, 95% CI (−14.0436, 5.0023)] were not statistically significant. The results of the surface under the cumulative ranking curve (SUCRA) showed that static exercise improved hypertension better than aerobic exercise.
Conclusion: Aerobic exercise and static exercise have been shown to have a good effect on the improvement of hypertension, but the effect on DBP is not significant.
1. Introduction
The increasing prevalence of hypertension in modern times is a cause for worry. Hypertension is characterized by higher-than-normal blood pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of Hypertension (2003 guidelines) stated that blood pressure varies throughout the day, and blood pressure measurements that are always higher than normal may indicate hypertension; the higher the blood pressure level, the greater the risk of other health problems, such as heart disease, heart attack, and stroke (1). The American Society of Cardiology/American Heart Association Guidelines for Prevention, Detection, Evaluation, and Management of Adult Hypertension (2017) indicate that normal blood pressure is below 120/80 mmHg; prehypertensive systolic blood pressure is 120–129 mmHg with diastolic blood pressure <80 mmHg; systolic blood pressure for hypertension is 130 mmHg or higher, and diastolic blood pressure is 80 mmHg or higher (2). The growth rate of the population affected by hypertension gradually increases with age, especially in middle-aged people. For adults aged 45 years without hypertension, the risk of hypertension over the next 40 years was 93% in African Americans, 92% in Hispanic individuals, 86% in white individuals, and 84% in Chinese adults (3). In the Framingham Heart Study, ~90% of all adults aged 55 or 65 years without hypertension developed hypertension during their lifetime (4). Hypertension usually develops over time. It may occur due to unhealthy lifestyle choices, such as insufficient physical exercise, excessive alcohol consumption, or an abnormal diet. Non-pharmacological therapy alone is particularly suitable for preventing hypertension and is used to manage the conditions of adults with hypertension or people with mild hypertension (5).
Non-pharmacological interventions can be performed through lifestyle-changing behavioral strategies and the promotion of physical activity, with the goal of modest BP reduction in the general population or more targeted BP reduction in adults at high risk of hypertension (6). The role of increased physical activity in reducing blood pressure has been repeatedly demonstrated in clinical trials, especially due to dynamic aerobic exercise and static isometric exercise (7, 8). Aerobic exercise is mainly fueled by aerobic metabolism, i.e., when the oxygen supply is sufficient. Generally, the exercise time is longer (more than 30 min), and the main muscle groups of the entire body contribute to the increased oxygen consumption during exercise (9). Quiet isometric stretching also has similar effects on functional improvement and therapeutic rehabilitation (10). Most trials were relatively short in duration, but increased physical activity has been a long-term intervention for lowering blood pressure and preventing hypertension (11). However, there is no main overview of the combined intervention of dynamic and static exercise modes, which needs further discussion and research. A meta-analysis revealed that interventions can prevent or improve the effects of hypertension and reported the effects of regular aerobic exercise on blood pressure, with an average reduction of 2–4 mmHg in SBP in adults with normal blood pressure and 5–8 mmHg in hypertensive patients (12). In addition, a meta-analysis showed that isometric exercise also had significant effects on lowering blood pressure (8). An isometric or static contraction is defined as a sustained muscle contraction (i.e., an increase in tension) with no change in the length of the involved muscle group (13). Isometric exercise might be an effective non-drug intervention for preventing and treating hypertension in older adults (14). There are a variety of active and passive stretches that are essential for the flexibility of older adults. This study mainly used network meta-analysis to explore the influence of different exercise types on hypertension in middle-aged and older adults and to explore the best exercise therapy to reduce hypertension in middle-aged and older adults.
2. Materials and methods
2.1. Inclusion criteria and literature search strategies
The literature search used the Boolean logic algorithm to obtain subject words and free words, searching databases including CNKI, Wanfang, Weipu, PubMed, Embase, Cochrane Library, and Web of Science for articles published up to 23 July 2023. The main subject words were “hypertension, blood pressure, high, high blood pressure, middle age, aerobic training, static training, combined training, and randomized controlled trial.” The literature screening applied PICOS strategies, which have been widely used in evidence-based medicine or practice. In the current study, the literature inclusion criteria were as follows: (1) subjects were middle-aged and older adults, with an average age of 45–64 years, without cardiovascular disease or other diseases; (2) randomized controlled experiments; (3) the exercise group only carried out the planned aerobic exercise or static stretching exercise, while the control group received no exercise intervention and no other intervention measures; (4) the intervention lasted more than 4 weeks; and (5) the aim of the study was mainly to compare the mean and standard deviation (SD) of resting blood pressure at baseline and at the end of the study between the control and exercise groups. The studies identified from the literature screening search were mainly those on the effect of exercise on blood pressure in middle-aged and older adults. Once those studies were identified, two investigators independently decided whether they should be included in the analysis. If the two authors disagreed, a third author intervened.
2.2. Data extraction and research quality evaluation
Data extraction was completed with a prespecified data extraction form that extracted relevant data and details related to the study's subject characteristics, interventions, and primary outcomes for systematic analysis. However, the usual PEDro score of two depends on how the study blinded the group and the treatment. In general, it is difficult to blind subjects in studies of exercise interventions. Therefore, these two points were excluded from the study analysis, and the PEDro assessment was based on eight terms, each scoring one point. The authors independently extracted and examined the data and assessed the quality of each study using the PEDro score.
2.3. Statistical analysis
Network meta-analysis was performed using Stata 16 software and RevMan 5.0 software. The outcome indicators selected were continuous variables, and the mean difference (MD) and 95% CI were used as effect size indicators. When P < 0.05, the inconsistent model was significant. These data cannot be directly analyzed by the consistency model; if P > 0.05, there was no significant difference between the direct and indirect comparisons, and the consistency model was used for analysis. A cumulative ranking probability map (SUCRA) was used to rank and compare the types of interventions. When SUCRA = 1, intervention measures are highly effective, while when SUCRA = 0, intervention measures are highly ineffective (15). According to the SUCRA values of the SBP and DBP indices, a stratified cluster analysis was used to explore the optimal treatment intervention.
3. Results
3.1. Literature screening process
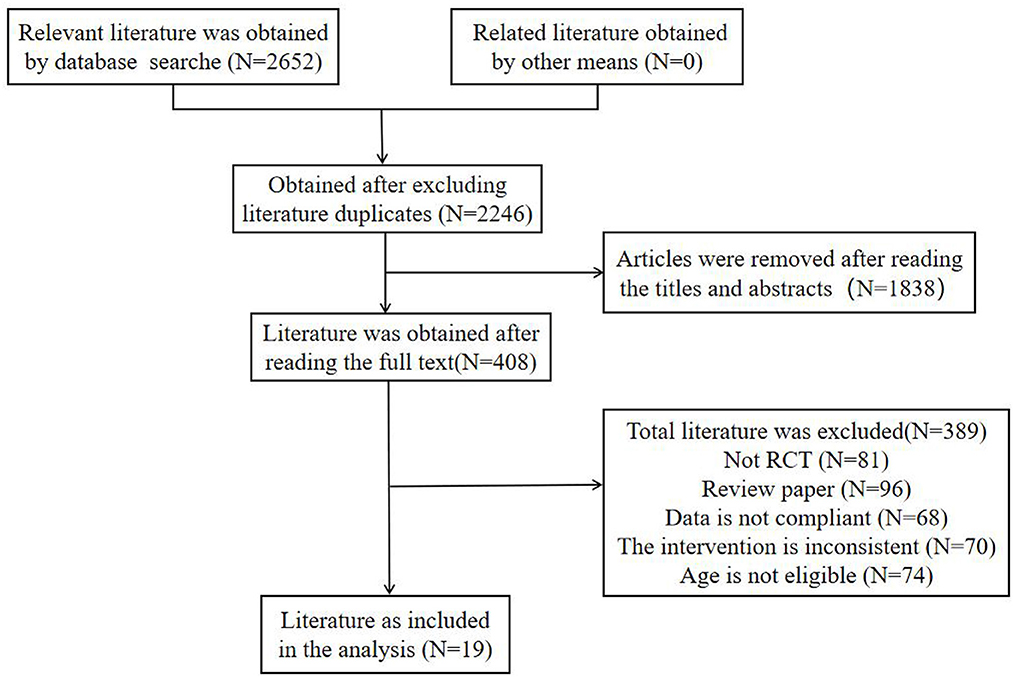
A total of 2,652 relevant articles were screened by a preliminary search of each database, and 19 articles, including 2,385 subjects, were finally included in the preliminary screening of titles and abstracts, as well as the rescreening of the full text. The main flow chart of the literature screening is shown in Figure 1.
3.2. The basic characteristics of the included studies and the evaluation of study quality
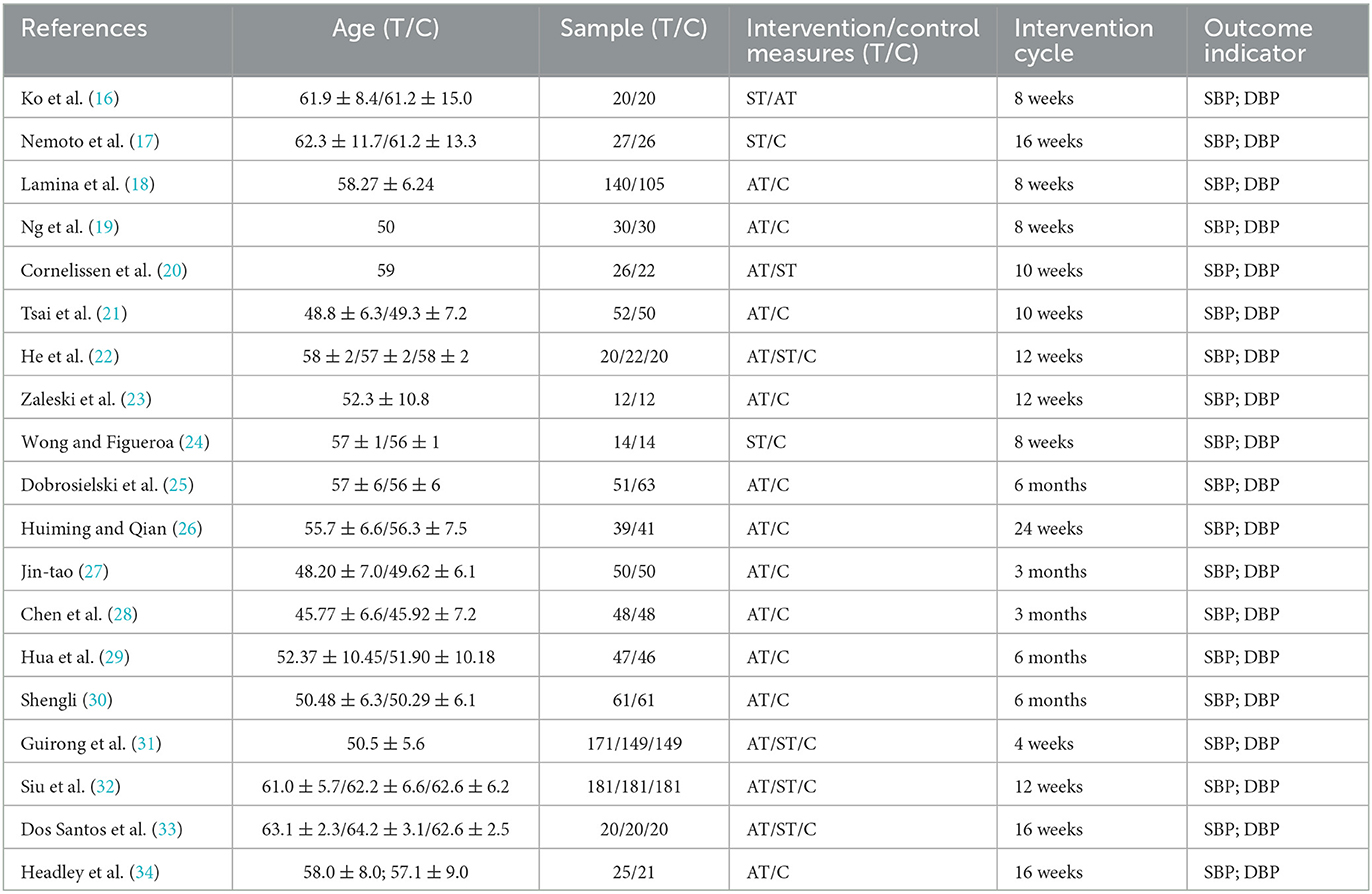
The 19 included studies mainly focused on hypertension in middle-aged and older adults. All subjects were grouped according to the principle of randomized control and the basic characteristics of the included studies (see Table 1).
All 19 included studies achieved “random assignment,” ITT intention-to-treat analysis, “statistical analysis between groups,” and “point measurement and variation measurement.” It is difficult to assess the overall quality of the study by blinding the subjects and therapists; therefore, these two points were excluded. The PEDro assessment is based on eight factors, and each is worth 1 point. Most PEDro scores were between five and six points, with an average score of ~6 points, and only one study reached a score of eight points. Overall, the results of the quality assessment of the literature were good (see Table 2).
3.3. Consistency analysis results
The inconsistency model test of the 19 RCTs included showed that SBP (P = 0.228) and DBP (P = 0.667) were not significant. The results of the local inconsistency test by the node splitting method again resulted in P > 0.05, and the results of indirect comparison and direct comparison of the two indices were shown to be consistent, indicating that the consistency model should be used for analysis.
3.4. Results of network meta-analysis
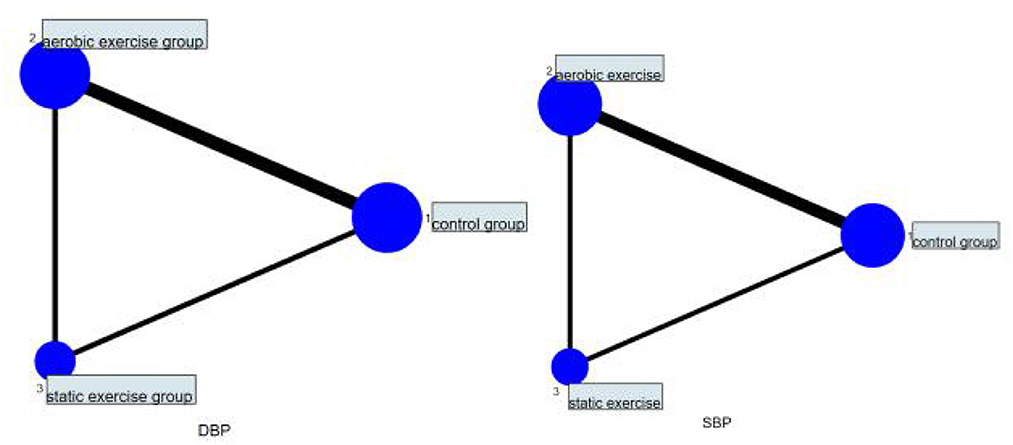
A total of 19 studies were included, including 11 studies comparing aerobic exercise with a control group, two studies comparing static exercise with a control group, and six studies comparing aerobic exercise with static exercise with the control group. For the network relationship between SBP and DBP of different exercise interventions, the circle area of aerobic exercise was the largest. The edge between aerobic exercise and conventional exercise was wider, indicating that studies comparing aerobic exercise with conventional exercise appeared most frequently among the included studies (Figure 2). Therefore, the effect of aerobic exercise on the hypertension of middle-aged and older adults is still supported by many studies, thus indicating a strong theoretical basis for its support.
3.5. Network meta-analysis of the effects of different exercise interventions on SBP
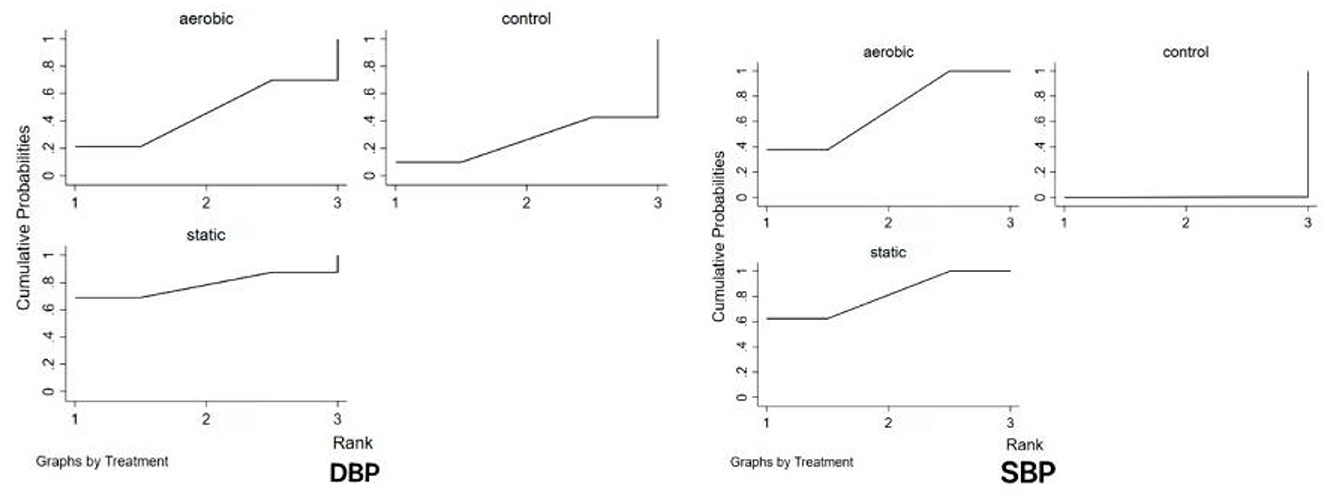
The results of the meta-analysis showed the MD value of aerobic exercise intervention [MD = −9.254, P < 0.05, 95% CI (−14.810, −3.698)] and the MD value of static exercise intervention [MD = −10.465, P < 0.05, 95% CI (−18.135, −18.135); −2.794] were better than those of the control group in improving SBP in hypertension. An indirect comparison between the two exercise modes showed no significant difference in SBP between the two groups (P > 0.05). The results of the SUCRA ranking showed that the effect of static exercise on SBP in hypertension was better than that of aerobic exercise (Figure 3).
3.6. Network meta-analysis of the effects of different exercise interventions on DBP
The results of the meta-analysis showed that the MD value in the aerobic exercise intervention [MD = −1.4096; P > 0.05, 95% CI (−8.2395, 5.4201)] and the MD value in the static exercise intervention [MD = −4.5206, P > 0.05, 95% CI (−14.0436, 5.0023)] had no significant effect on DBP improvement in hypertension (all P > 0.05). An indirect comparison between the two showed no significant difference in exercise mode between the two groups (P > 0.05). The results of the SUCRA ranking showed that static exercise had a better effect on DBP in hypertensive individuals (see Figure 3).
3.7. Detection of publication bias
Compared with the corrected funnel plot, the inverted funnel plot was symmetric, and the scattered points were distributed within the range of the inverted funnel plot (see Figure 4), indicating that there was little possibility of a small-sample effect or publication bias.
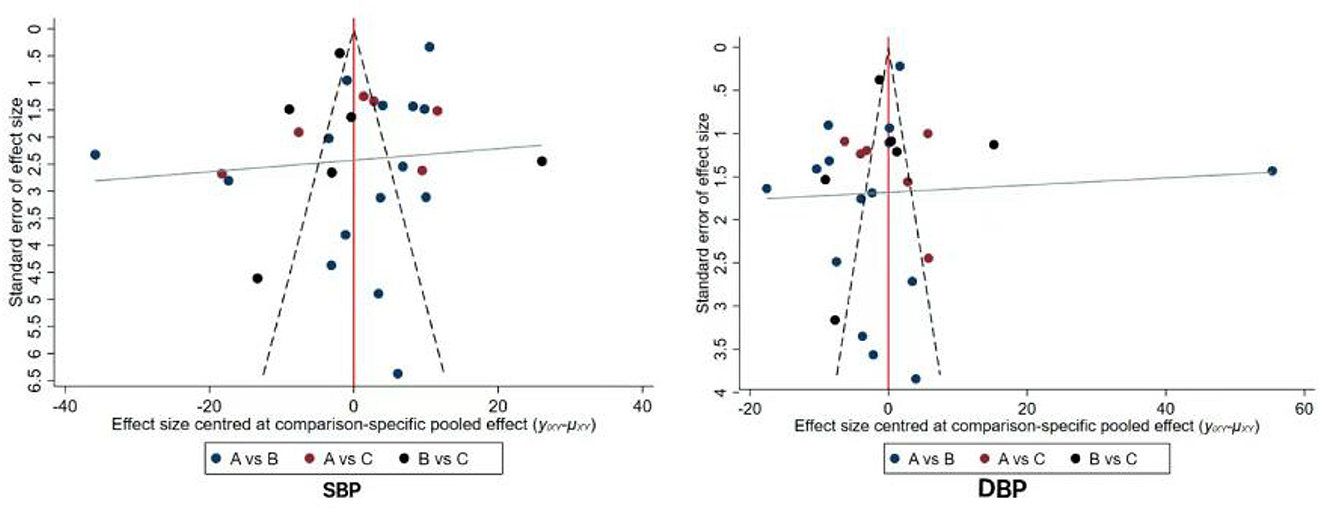
Figure 4. Funnel plots of publication bias for outcome measures of included studies. A: control group; B: aerobic exercise; C: static exercise.
4. Discussion
4.1. Intervention effects of aerobic exercise on hypertension in middle-aged and older adults
Many recent studies have found that exercise modes such as isokinetic resistance training, limb stretching exercises, swimming, and running can reduce blood pressure (12, 35). Some studies have shown that aerobic exercise training can lower blood pressure by 5–7 mmHg (36). In this study, aerobic exercise was also found to have a significant effect on lowering SBP in middle-aged and older adults with hypertension, which can reduce the incidence of hypertension to some extent. Engaging in physical activity can also further prevent cardiopulmonary impairment and lower blood pressure (37). The incidence of hypertension increases with age, and the older the individuals are, the more their exercise ability will be affected, and the exercise mode or intensity will be limited (38). The incidence of many chronic diseases, such as cardiovascular disease and hypertension, further increases with age (39, 40). Many forms of aerobic exercise can lower blood pressure in middle-aged and older adults, such as jogging, square dancing, and aerobics, all of which have good effects. Whelton et al. found that aerobic exercise had an overall net effect of reducing SBP and DBP by 3.84 and 2.58 mmHg, respectively (7). Hagberg et al.'s review showed that in hypertensive adults aged 60 or older, SBP and DBP values were reduced by an average of 7.6/8.8 mmHg (41). In this study, aerobic exercise had a significant effect on SBP but not on DBP. This suggests that in this study, aerobic exercise effectively lowered blood pressure in middle-aged and older adults with hypertension, which has certain clinical significance and value for the health and medical conditions of both middle-aged and older adults.
4.2. Isometric exercise intervention effects on hypertension in middle-aged and older adults
For middle-aged and older individuals, the most common isometric exercises are static stretching exercises, which are primarily defined as sustained muscle contraction (i.e., increased tension) without changes in the length of the involved muscle groups. To date, relatively little attention has been given to the effects of isometric exercise training on resting blood pressure. The results from previous meta-analysis suggest that although the overall sample size is still small, isometric exercise training may produce greater reductions in resting blood pressure (42, 43). The study results also showed that the improvement effect of isometric exercise on the SBP and DBP of middle-aged and older hypertensive individuals was better than that of aerobic exercise on the SBP and DBP of hypertensive individuals, which is similar to the results of the previous meta-analysis. However, middle-aged and older individuals should not excessively perform high-load isometric exercises, as improper training may put pressure on the heart, potentially leading to other diseases. Since isometric exercise is not traditionally recommended for hypertensive subjects, isometric training is generally only applicable to some specific exercise programs. However, small-scale, short-term studies conducted in subjects with normal blood pressure and hypertensive subjects suggest that performing 3–4 short isometric exercises per week can lower systolic and diastolic blood pressure (44). Isometric exercise also has effects on lowering blood pressure in middle-aged and older adults, but its advantages compared to dynamic exercise training (aerobic exercise) may only be limited to blood pressure, and further investigation is still needed regarding other possible aspects. Additionally, middle-aged and older adults need to perform these exercises within their capacity to avoid injuries to the joints and other body parts.
4.3. The impact of different exercise modes on hypertension in middle-aged and older adults
The results of the included literature showed that different exercise intervention modes significantly lower blood pressure in middle-aged and older adults. Aerobic exercise modes such as slow running, hiking, cycling, and brisk walking, as well as static exercises such as stretching, isometric exercises, and combined exercises with low-intensity dynamic and static loading, all have an impact on lowering hypertension in middle-aged and older adults. Currently, international treatment guidelines for primary and secondary prevention of hypertension in China generally recommend lifestyle changes (quitting smoking, weight loss, exercise training, healthy eating, and reducing sodium intake) as the first-line treatment (45). Non-pharmacological treatments can promote the reduction and improvement of blood pressure in middle-aged and older adults, contributing to their physical and mental health development. In daily life, older adults need to engage in reasonable and healthy exercises to cope with the diseases caused by hypertension and provide a suitable and comfortable living environment.
5. Limitations
This study has several limitations. First, it only includes aerobic and static exercise methods, while the effects of other exercise modalities, such as dynamic resistance training, have not been considered. Second, due to the limited number of studies included, there may be a certain degree of selection bias present. Finally, the study incorporates various outcome assessment indicators, and the results of the heterogeneity test suggest that the heterogeneity is relatively high. Therefore, the quality control standards for future clinical trials should be informed by evidence-based medicine standards.
6. Conclusion
Both aerobic exercise and static exercise have significant effects on the reduction of blood pressure in middle-aged and older adults. The effect of both exercise modes on systolic blood pressure, but not diastolic blood pressure, is significant. According to the results of the SUCRA ranking, static exercise is better than aerobic exercise in reducing blood pressure in middle-aged and older adults. Appropriate exercise is effective for middle-aged and older adults with hypertension and has certain benefits in reducing hypertension.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
WG wrote the article. ML was responsible for data collection and analysis. TH checked and revised the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to thank all authors for their encouragement and guidance throughout this project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. (2003) 289:2560–72. doi: 10.1001/jama.289.19.2560
2. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. (2018) 71:e127–248. doi: 10.1161/HYP.0000000000000076
3. Carson AP, Howard G, Burke GL, Shea S, Levitan EB, Muntner P. Ethnic differences in hypertension incidence among middle-aged and older adults: the multi-ethnic study of atherosclerosis. Hypertension. (2011) 57:1101–7. doi: 10.1161/HYPERTENSIONAHA.110.168005
4. Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D'Agostino RB, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: the Framingham Heart Study. J Am Med Assoc. (2002) 287:1003–10. doi: 10.1001/jama.287.8.1003
5. Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger Jr WH, Kostis JB, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in older adults (TONE). J Am Med Assoc. (1998) 279:839–46. doi: 10.1001/jama.279.11.839
6. National High Blood Pressure Education Program Working Group report on primary prevention of hypertension. Arch Intern Med. (1993) 153:186–208.
7. Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. (2002) 136:493–503. doi: 10.7326/0003-4819-136-7-200204020-00006
8. Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc. (2014) 89:327–34. doi: 10.1016/j.mayocp.2013.10.030
9. Liu Y, Tao Z, Yingcui W, Xianglin C. Thoughts on exercise therapy for hypertension. Chin J Hypertension. (2022) 30:118–22. doi: 10.16439/j.issn.1673-7245.2022.02.005
10. Gathright EC, Salmoirago-Blotcher E, DeCosta J, Balletto BL, Donahue ML, Feulner MM, et al. The impact of transcendental meditation on depressive symptoms and blood pressure in adults with cardiovascular disease: a systematic review and meta-analysis. Complement Therapies Med. (2019) 46:172–9. doi: 10.1016/j.ctim.2019.08.009
11. Whelton PK, Appel L, Charleston J, Dalcin AT, Ewart C, Fried L, et al. The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels: results of the Trials of Hypertension Prevention, phase I. J Am Med Assoc. (1992) 267:1213–20. doi: 10.1001/jama.1992.03480090061028
12. Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. (2013) 2:e004473. doi: 10.1161/JAHA.112.004473
13. Mitchell JH, Wildenthal K. Static (isometric) exercise and the heart: physiological and clinical considerations. Annu Rev Med. (1974) 25:369–81. doi: 10.1146/annurev.me.25.020174.002101
14. Ben-Sira D, Oliveira JMF. Hypertension in aging: physical activity as primary prevention. Eur Rev Aging Phys Act. (2007) 4:85–9. doi: 10.1007/s11556-007-0023-0
15. Yuexiong Y, Wei Z, Xiaoyuan L, Juan Z, Ding Jun Z, Qiongying L. Interpretation of graphical results of reticulated meta analysis. Chin J Evid Based Med. (2015) 15:103–9.
16. Ko J, Deprez D, Shaw K, Alcorn J, Hadjistavropoulos T, Tomczak C, et al. Stretching is superior to brisk walking for reducing blood pressure in people with high–normal blood pressure or stage I hypertension. J Phys Act Health. (2020) 18:21–8. doi: 10.1123/jpah.2020-0365
17. Nemoto Y, Satoh T, Takahashi T, Hattori T, Konno S, Suzuki S, et al. Effects of isometric handgrip training on home blood pressure measurements in hypertensive patients: a randomized crossover study. Internal Med. (2021) 60:2181–8. doi: 10.2169/internalmedicine.5865-20
18. Lamina S, Okoye CG, Hanif SM. Randomised controlled trial: effects of aerobic exercise training programme on indices of adiposity and metabolic markers in hypertension. J Pak Med Assoc. (2013) 63:680–7. doi: 10.1186/s12879-014-0697-7
19. Ng CL, Goh SY, Malhotra R, Østbye T, Tai ES. Minimal difference between aerobic and progressive resistance exercise on metabolic profile and fitness in older adults with diabetes mellitus: a randomised trial. J Physiother. (2010) 56:163–70. doi: 10.1016/S1836-9553(10)70021-7
20. Cornelissen VA, Arnout J, Holvoet P, Fagard RH. Influence of exercise at lower and higher intensity on blood pressure and cardiovascular risk factors at older age. J Hypertens. (2009) 27:753–62. doi: 10.1097/HJH.0b013e328322cf60
21. Tsai JC, Yang HY, Wang WH, Hsieh MH, Chen PT, Kao CC, et al. The beneficial effect of regular endurance exercise training on blood pressure and quality of life in patients with hypertension. Clin Exp Hypertension. (2004) 26:255–65. doi: 10.1081/CEH-120030234
22. He LI, Wei WR, Can Z. Effects of 12-week brisk walking training on exercise blood pressure in older adult patients with essential hypertension: a pilot study. Clin Exp Hypertens. (2018) 40:673–9. doi: 10.1080/10641963.2018.1425416
23. Zaleski AL, Taylor BA, Park CL, Santos LP, Panza G, Kramarz M, et al. Using the immediate blood pressure benefits of exercise to improve exercise adherence among adults with hypertension: a randomized clinical trial. J Hypertension. (2019) 37:1877–88. doi: 10.1097/HJH.0000000000002115
24. Wong A, Figueroa A. Eight weeks of stretching training reduces aortic wave reflection magnitude and blood pressure in obese postmenopausal women. J Hum Hypertens. (2014) 28:246–50. doi: 10.1038/jhh.2013.98
25. Dobrosielski DA, Gibbs BB, Ouyang P, Bonekamp S, Clark JM, Wang NY, et al. Effect of exercise on blood pressure in type 2 diabetes: a randomized controlled trial. J General Internal Med. (2012) 27:1453–9. doi: 10.1007/s11606-012-2103-8
26. Huiming Y, Qian A. Effect of moderate-intensity aerobic exercise combined with antihypertensive drugs on blood pressure and cardiorenal function in hypertensive patients. Zhejiang Clin Med. (2017) 19:1274–6.
27. Jin-tao L. Analysis of the effect of intensive aerobic exercise on blood pressure in hypertensive patients. Chin For Med Res. (2017) 15:151–2. doi: 10.14033/j.cnki.cfmr.2017.3.084
28. Yan C, Ying C, Liang L, Jing Q. Analysis of the antihypertensive effect of strength aerobic training in patients with essential hypertension. J Nurse Train. (2016) 31:1835–7. doi: 10.16821/j.cnki.hsjx.2016.20.004
29. Hua L, Yongxin S, Yefei S, Bin L, Li L. Efficacy of aerobic exercise on blood pressure and vasoactive mediators in patients with simple diastolic hypertension. J Cardiovasc Rehabil Med. (2016) 25:122–6. doi: 10.3969/j.issn.1008-0074.2016.02.03
30. Shengli Z. Effects of different exercise patterns on autonomic nerve function and blood pressure in patients with essential hypertension. Henan Med Res. (2019) 13:2363–5. doi: 10.3969/j.issn.1004-437X.2019.13.025
31. Guirong W, Daxiu L. Effect of a comprehensive intervention on blood pressure and heart rate in patients with mild to moderate hypertension. PLA Nursing J. (2006) 23:19–21. doi: 10.3969/j.issn.1008-9993.2006.09.008
32. Siu PM, Yu AP, Chin EC, Yu DS, Hui SS, Woo J, et al. Effects of Tai Chi or conventional exercise on central obesity in middle-aged and older adults: a three-group randomized controlled trial. Ann Internal Med. (2021) 174:1050–7. doi: 10.7326/M20-7014
33. Dos Santos ES, Asano RY, Irênio Filho G, Lopes NL, Panelli P, Nascimento DDC, et al. Acute and chronic cardiovascular response to 16 weeks of combined eccentric or traditional resistance and aerobic training in older adult hypertensive women: a randomized controlled trial. J Strength Condition Res. (2014) 28:3073–84. doi: 10.1519/JSC.0000000000000537
34. Headley S, Germain M, Wood R, Joubert J, Milch C, Evans E, et al. Short-term aerobic exercise and vascular function in CKD stage 3: a randomized controlled trial. Am J Kidney Dis. (2014) 64:222–9. doi: 10.1053/j.ajkd.2014.02.022
35. Pescatello LS, MacDonald HV, Lamberti L, Johnson BT. Exercise for hypertension: a prescription update integrating existing recommendations with emerging research. Curr Hypertens Rep. (2015) 17:87. doi: 10.1007/s11906-015-0600-y
36. Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA, et al. Exercise and hypertension. Med Sci Sports Exercise. (2004) 36:533–53. doi: 10.1249/01.MSS.0000115224.88514.3A
37. Biffi A, Gallo G, Fernando F, Sirico F, Signorello MG, De Martino L, et al. Relationship between cardiorespiratory fitness, baseline blood pressure and hypertensive response to exercise in the ferrari corporate population. High Blood Pressure Cardiovasc Prev. (2022) 5:1–8. doi: 10.1007/s40292-021-00491-5
38. Boutcher YN, Boutcher SH. Exercise intensity and hypertension: what's new? J Hum Hypertension. (2017) 31:157–64. doi: 10.1038/jhh.2016.62
39. Chodzko-Zajko WJ, Proctor DN, Singh MAF, Minson CT, Nigg CR, Salem GJ, et al. Exercise and physical activity for older adults. Med Sci Sports Exerc. (2009) 41:1510–30. doi: 10.1249/MSS.0b013e3181a0c95c
40. Rigaud AS, Forette B. Hypertension in older adults. J Gerontol Ser. (2001) 56:M217–25. doi: 10.1093/gerona/56.4.M217
41. Hagberg JM, Park JJ, Brown MD. The role of exercise training in the treatment of hypertension: an update. Sports Med. (2000) 30:193–206. doi: 10.2165/00007256-200030030-00004
42. Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension. (2011) 58:950–8. doi: 10.1161/HYPERTENSIONAHA.111.177071
43. Owen A, Wiles J, Swaine I. Effect of isometric exercise on resting blood pressure: a meta-analysis. J Hum Hypertens. (2010) 24:796–800. doi: 10.1038/jhh.2010.13
44. Buck C, Donner AP. Isometric occupational exercise and the incidence of hypertension. J Occup Med. (1985) 17:370–2. doi: 10.1097/00043764-198505000-00017
Keywords: hypertension, aerobics, static exercise, middle-aged and older adults, types of exercise
Citation: Gao W, Lv M and Huang T (2023) Effects of different types of exercise on hypertension in middle-aged and older adults: a network meta-analysis. Front. Public Health 11:1194124. doi: 10.3389/fpubh.2023.1194124
Received: 26 March 2023; Accepted: 15 August 2023;
Published: 20 September 2023.
Edited by:
Brijesh Sathian, Hamad Medical Corporation, QatarReviewed by:
Stefano Palermi, University of Naples Federico II, ItalyHeba Abdeen, Cairo University, Egypt
Copyright © 2023 Gao, Lv and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Gao, MjQ5OTk1MjI2MEBxcS5jb20=
 Wei Gao
Wei Gao Moran Lv
Moran Lv Tao Huang
Tao Huang