- 1School of Public Health and Research, Somali National University, Mogadishu, Somalia
- 2Somali Institute for Health Research (SIHR), Garoowe, Somalia
- 3Norwegian Institute of Public Health, Garoowe, Somalia
Background: Diabetes mellitus (DM) causes significant morbidity and mortality in sub-Saharan Africa (SSA), including Somalia. Among diabetic patients, diabetic foot ulcers (DFUs) constitute the largest proportion of admissions, amputations, and mortality. The aim of this study is to assess the prevalence of diabetic foot ulcers and subsequently determine factors associated with it among diabetic patients at three major hospitals in Somalia.
Methods: An institutional-based cross-sectional study was conducted among 193 diabetic patients between August and November 2022. All eligible diabetes patients who were attending De Martini Hospital, Madina General Hospital, and Deynile General Hospital during the study period were included in the study. Patients were interviewed using a structured questionnaire. We collected demographic, clinical, and behavioral variables from all participants. A bivariate and multivariable logistic regression model was fitted to identify factors associated with diabetic foot ulcer. An odds ratio with a 95% confidence interval was computed to determine the level of significance.
Result: The mean age of the study’s participants was 50.9 ± 13.6 years. The prevalence of diabetic foot ulcer was 15%. Patients who were either overweight or obese (OR 4.63, CI: 2.08–10.30), had a lack of family support in managing diabetes (OR 3.33, CI: 1.74–6.36), and did not check their feet regularly were more likely to develop DFU (OR 1.99, CI:1.08–3.66).
Conclusion: Increased body mass index, lack of family support, and not checking feet regularly were associated with DFUs. The high prevalence of DFUs and the plethora of needs of people with DFUs pose challenges for health care. A coordinated health care system is necessary to meet the needs of diabetic patients and prevent DFUs.
Background
The rising prevalence of diabetes mellitus (DM) worldwide, with an estimated 642 million people with diabetes globally by 2040, is a global public health concern (1). In 2019, it was estimated that there were 19 million persons with diabetes in SSA, and the projected prevalence of DM to be 29 million in 2030 and 47 million by 2045 (2, 3). DM is associated with many systematic complications, including diabetic foot ulcers (DFU), which is an infection, ulceration, or destruction of the deep tissues of the foot. It is a devastating component of progression of diabetes with estimated 15% of patients with diabetes may develop DFUs, leading to more than 80,000 amputations per year in the United States (4). Diabetic foot ulcer (DFU) are defined as a “foot affected by ulceration that is associated with neuropathy and/or peripheral arterial disease of the lower limb in a patient with diabetes.” It is often caused by loss of glycemic control, peripheral neuropathy, peripheral vascular disease, and immunosuppression. A previous systematic review of the risk stratification systems for diabetic foot ulceration identified: previous lower extremity amputation, history of a foot ulcer, anatomic foot deformity, peripheral vascular disease, poor glycemic control and smoking (5). The lifetime risk of DFUs for patients with diabetes may reach up to 68 per 1,000 persons as reported by some studies (6). In Africa, the overall prevalence of foot ulcers was 13% and has increased over time, especially since 2001. Approximately 15% of patients with foot lesions underwent major amputation and 14.2% died during hospitalization. In patients with diabetic ulcers, neuropathy was the most common predisposing factor (7).
Somalia is a sub-Saharan African country that has experienced decades of armed conflict that have rendered the national public health care system dysfunctional. As a result, the health care system in the country is dominated by the private system, which is unaffordable for a large segment of the population (8–10). Although there is no representative data about diabetes in Somalia, the World Health Organization has estimated it at 5% in 2016, with 22% of the people in Somalia being overweight or obese (11). The 2021 data by the World Bank shows that the diabetes prevalence of the population between the ages of 20 and 79 in Somalia is 6.5% (12). The number of diabetes patients with foot ulcer is not yet known in Somalia due to the absence of both regular diabetes screening, and strict management for the known diabetes patients. The current study is the first of its kind investigating the prevalence of diabetes foot ulcers and associated risk factors among diabetes patients in Somalia.
Methods
A hospital-based cross-sectional study was performed with 193 diabetic patients who attended the De Martini Hospital, Madina General Hospital, and Deynile General Hospital from August to November 2022. The first and second hospitals are referral public hospitals, while the third is a community hospital that provides free health services to a large catchment area in the northern part of Mogadishu. All are located in Mogadishu, the capital city of Somalia. The study population is composed of diabetic adult patients who come to the clinic for check-ups or are admitted to one of the three hospitals for diabetes related problems during the study period. The aim of this study was to assess the prevalence of diabetic foot ulcers and factors associated with them among diabetic patients in the three hospitals. All eligible diabetes patients who were attending the three hospitals during the study period were included in the study. Patients were interviewed using a structured questionnaire. DFUs were determined by reports of the history of a breach on the normal skin occurring as indurations, ulcerations, or changes of colors on the foot. Patients who were critically ill with a traumatic ulcer, patients admitted with diabetic ketoacidosis, patients with clinical suspicion of having Charcot foot, and diabetic patients who refused participation in the study were excluded. A validated, pretested, and structured questionnaire was used to gather information from the participants. The questionnaire was validated prior to application with three patients, and it was reviewed by two public health experts. The questionnaire included questions about sociodemographic characteristics, clinical variables, and behavioral factors.
The data were entered into Microsoft Excel version 16 and then exported into SPSS version 23.0 for analysis. Descriptive analyses were performed to summarize the characteristics of the study participants. To determine factors associated with diabetic foot ulcers, bivariable logistic regression was performed. Variables with a value of p < 0.25, in the bivariable analysis, were taken further to the multivariable logistic regression analysis. A p-value < 0.05 and a 95% confidence interval were considered statistically significant. Ethical clearance was obtained from the Institutional Review Board of the School of Public Health and Research, Somali National University. Written permission was obtained from hospital managers. Since most of the study participants could not write, verbal informed consent was obtained from them.
Result
Socio-demographic characteristics of respondents
A total of 193 adult diabetic patients were enrolled in the study. Of them, 76 (39.4%) were males, while 117 (60.6%) were females. The mean age of the study participants was 50.9 ± 13.6 years, and most of the study participants were in the age group 40–59 years. Regarding their educational status, 104 (53.9%) had no formal education, while 89 (46.1%) had formal education. More than half (50.2%) were unemployed, and the majority (75.6%) were urban residents. Of the total sample, 29 (15%, CI: 0.01–0.06) had diabetes foot ulcer during the study.
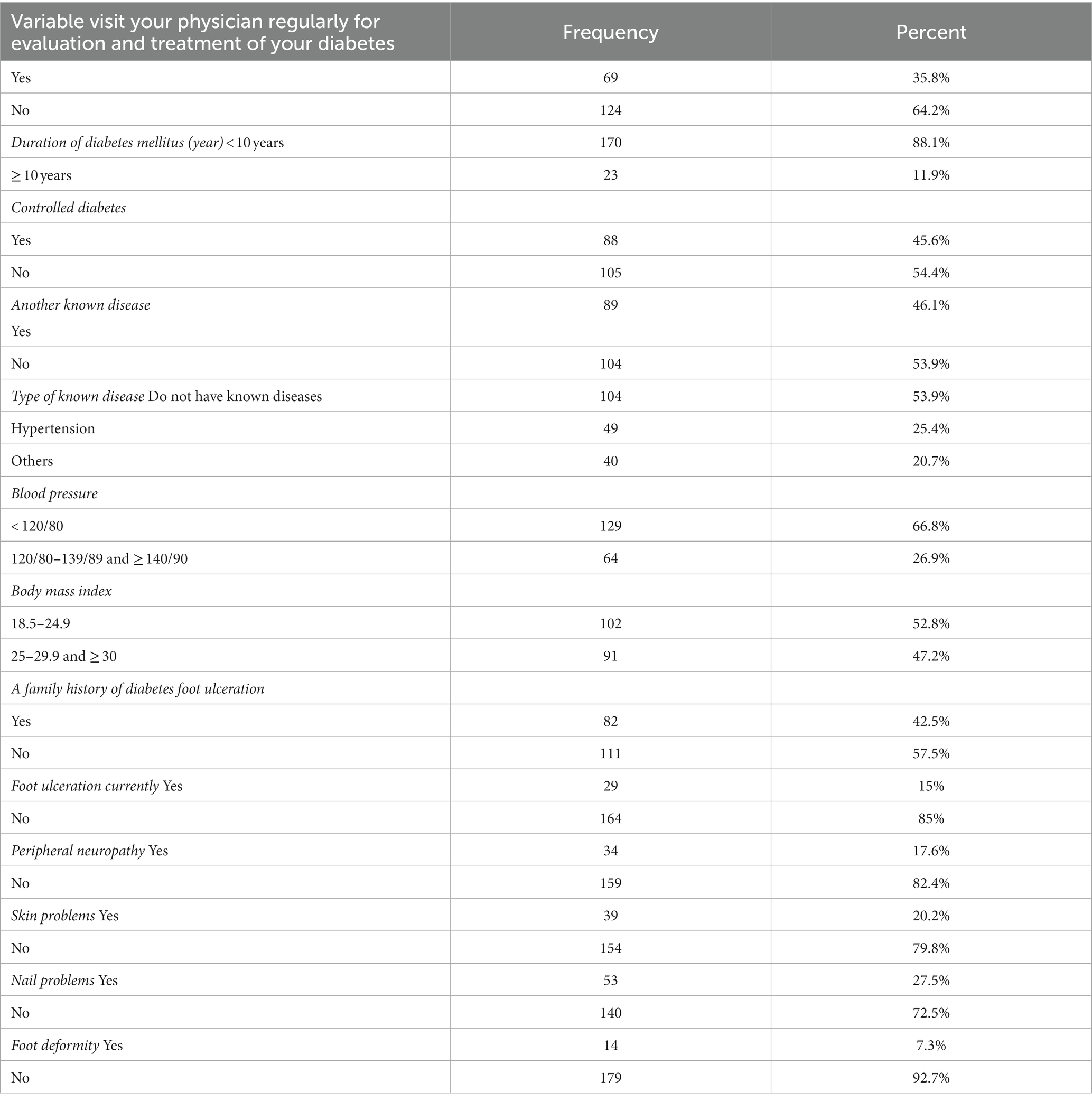
Of the total 193 study respondents, 69 (35.8%) had regular evaluation and treatment for diabetes mellitus. The majority, 170 (88.1%), had lived with diabetes for more than 10 years, and 54.4% had poorly controlled diabetes mellitus. Nearly half of the study respondents, 91 (46.2%), were either overweight or obese. Eighty-two (42.5%) participants had a family history of diabetes foot ulceration while 17.6% had Peripheral neuropathy (Table 1).
Behavioral factors of respondents
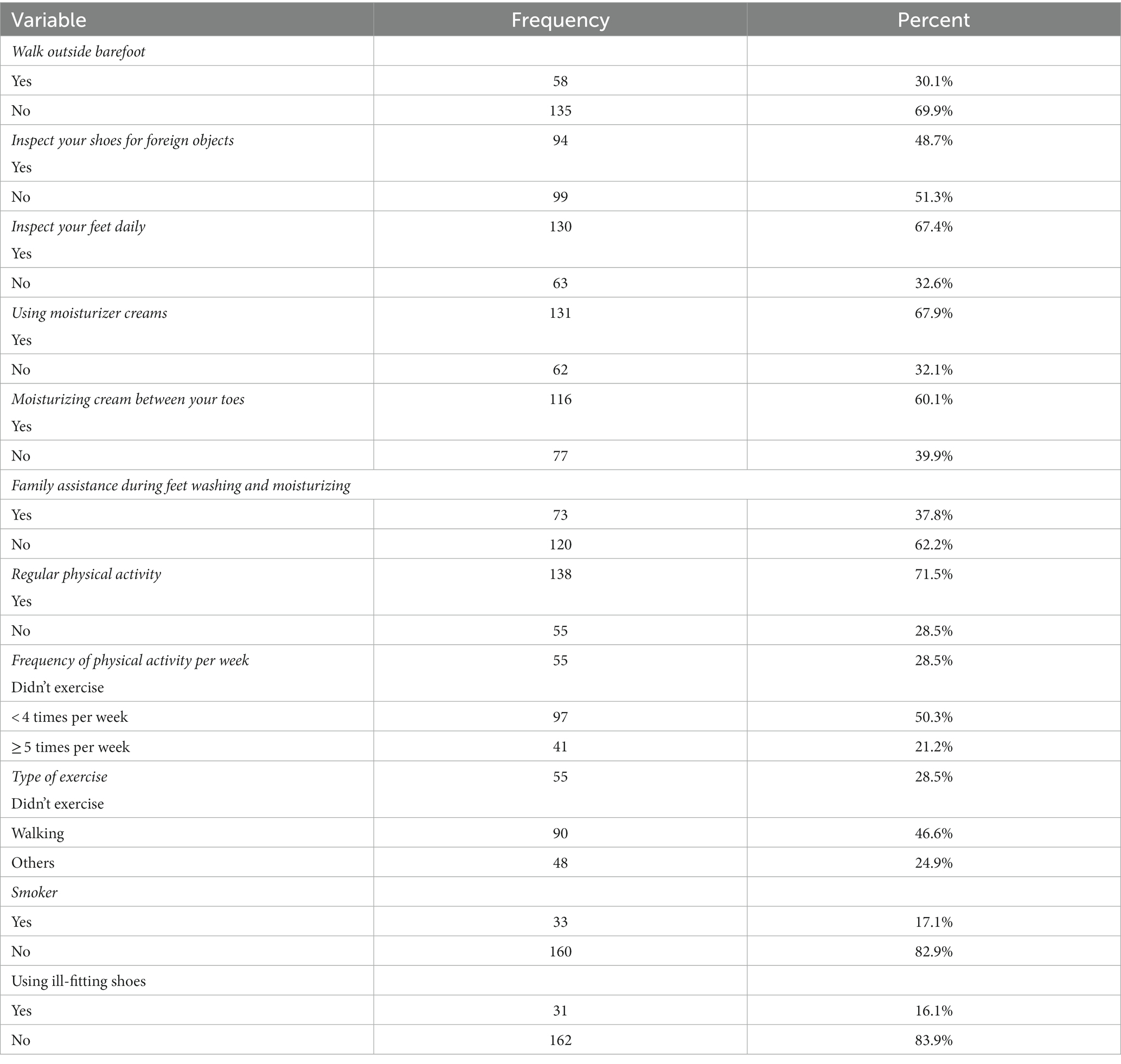
The majority of participants (62.2%) did not receive family assistance during diabetes care, while nearly half (48.7%) reported that they always inspected their shoes for foreign objects. 30.1% of the respondents reported having walked outside barefoot.
Thirty-three (17.1%) respondents were smokers, while 138 (71.5%) of the participants stated that they engaged in physical exercise. Nearly half (46.6%) reported the type of exercise they engage in as walking, and more than half (50.3%) engage in physical activities fewer than four times per week. The behavioral factors of the respondents are shown in Table 2.
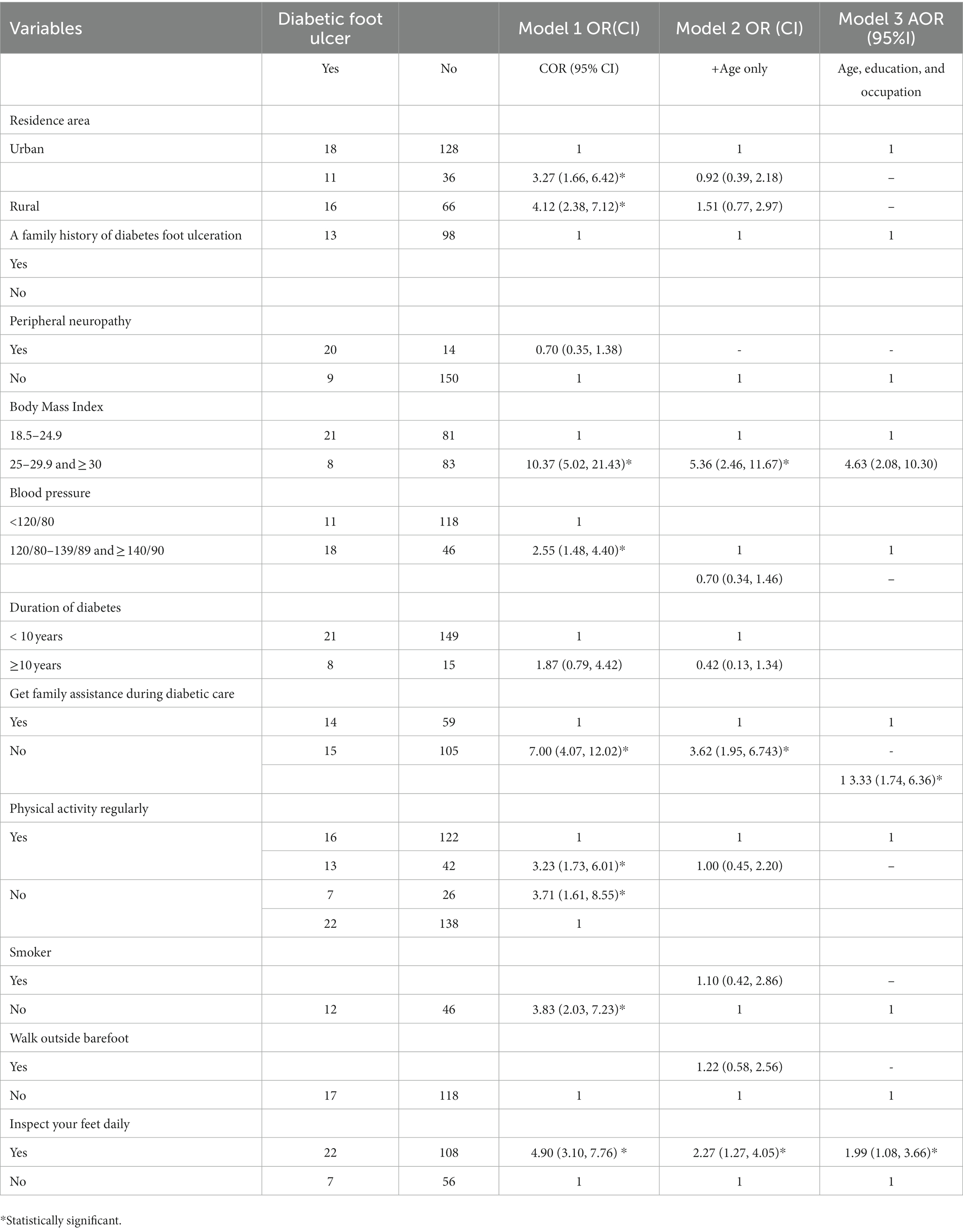
Table 3 shows variables that are associated with diabetic foot ulcer after adjusting age, education, and employment. Overweight or obese people had almost five times higher odds of developing diabetic foot ulcer compared to diabetic patients who had a normal body mass index (OR 4.63, CI: 2.08–10.30). Similarly, people who do not receive family support in managing diabetes had over three times higher odds of developing DFUs (OR 3.33, CI: 1.74–6.36). Further, people who do not check their feet regularly were more likely to develop DFUs compared to those who did it (OR 1.99, CI:1.08–3.66).
Discussion
The study shows that the prevalence of diabetes foot ulcers (DFUs) is 15% among study participants. A prior review of data from 19 African countries found that 13% of diabetes patients had foot ulcers (7). Despite the fact that the prevalence of DFUs in our sample is slightly higher than that observed in other parts of the world, Somalia is facing a formidable challenge in the management of DFUs, given that the country has one of the poorest health care systems in Africa. Therefore, like many other countries in Africa, the DFUs in Somalia may frequently progress to sepsis or gangrene, resulting in prolonged hospital stays and significant mortality (13, 14). A study shows that in the Africa continent, with poor resources, how to prevent and manage successfully DFUs is a major challenge (14). Large segments of the Somali people live in rural, while 26% are nomadic pastoralists that travel with their livestock often with barefoot. In this situation, it is not unexpected that the prevalence of DFUs in Somalia is 15%. Evidence shows that the diabetic foot complications resulting in amputation begin overwhelmingly with the formation of skin ulcers (15). Early detection and appropriate treatment of these ulcers may prevent up to 85% of amputation (15).
Factors that are associated with the DFUs in our sample include increased BMI, with people who are either overweight or obese having almost five times higher odds of developing DFUs. Literature documented a link between increased body mass index (BMI) and chronic DFUs (16–18). As high BMI drives number of functional impairments that are related to obesity and type 2 diabetes mellitus (19), the BMI > 25 may alter biological processes that are important in wound healing. For example, increased BMI is associated with impaired circulation which may compromise ulcer healing process (20), and impair oxygen delivery, thereby encouraging the growth of anaerobic microbes and fungi (21). Since Somalia does not have laboratory capacity to culture and conduct sensitivity tests these cases are often treated traditionally or not treated at all, thus eventually leading to amputation. A study in Tanzania, a country with much better health system than Somalia, shown that among patients admitted with DFUs, 33% had amputations, and 54% of those, with advanced pathology (Wagner Score ≥ 4), died within 1 year (22). Although there is no available data about overweight and obesity in Somalia, research on the Somali diaspora showed extremely high rates of obesity among Somalis, and a higher risk of DM (23). Combined with poor diabetes management, the DFUs may contribute to high rates of morbidity and mortality among people with DM in Somalia.
Variables such as long duration of diabetes, having high blood pressure, and walking barefoot have shown significantly higher odds of having DFUs in our sample, but this significance attenuated after we controlled the age, education, and occupation. However, people who do not receive family assistance for diabetes care have over three times the odds of having DFUs than those who do. A prior review of the literature stated that family support is an integral part of sustaining self-management behaviors and improving the health outcomes of diabetes patients (24). In Somalia, professional support services, such as nurse visits or disease education programs, are supposed to provide invaluable support for patients with diabetes are often unavailable. As a result, family members are recognized as a viable option in the care of DFU patients in conflict settings such as Somalia. There is empirical evidence about the association between insufficient social support from family members and poor diabetes self-management (25) and the fact that family support has a positive effect on patients’ self-management behaviors (25, 26). In Somalia, where professional support services are scarce, family shapes the environment in which self-care takes place and frequently plays an active role in managing the patient’s chronic illness. Family members are often the first to notice new symptoms, and most health problems are handled by patients and family members without consulting a health care professional (27). It is known that family support is linked with improved self-reported health and general well-being (28) as well as improved coping, quality of life, and glycemic outcomes (29). Our finding suggests that family support for diabetic patients, particularly those with DFUs, should be fostered in Somalia to prevent the adverse effects of diabetes, including DFUs.
Moreover, patients who do not inspect their feet daily had twice the odds of having DFUs as those who inspect their feet daily. According to the CDC, people who check their feet every day, can catch problems early and get them treated right away, thus reducing their risk of amputation (30). Adequate self-care can reduce the risk of lesions, infections, and amputation in people at risk of foot ulcer. The aforesaid self-care may include, but is not limited to, daily foot control, adequate hygiene, not walking barefoot, using appropriate footwear, cutting nails, early professional care for open foot wounds and lesions, and routine foot examinations by a trained professional to identify diabetic foot complications. However, these types of self-care require a high level of health literacy by the patients, which is a level of health literacy that Somali patients may not have (31). Further, there is no health education about self-care measures for foot ulcers among diabetes patients in Somalia. The lack of health literacy on foot care and/or clear daily foot care plans increases the risk of developing ulcers and amputations (32), while foot ulcers and amputations were found to increase in patients who did not adopt self-care measures (33). In this case, foot care knowledge and foot care practices are highly associated (34), which implies that when patients receive appropriate foot care guidelines and education, they will carry out the corresponding practices (35). Therefore, it is imperative for diabetes patients in Somalia to receive health education and self-care guidelines to prevent the adverse consequences of diabetic foot ulcers.
The important limitation of this study is its cross-sectional design, which makes it difficult to establish the causes. Moreover, most of the variables were self-reported, with a distinct possibility of both under- and/or over-reporting. However, this is the first study of its kind ever conducted in Somalia, thereby providing highly needed information for health providers and policymakers in Somalia to improve healthcare for diabetic patients and strengthen the national prevention strategy for diabetes foot ulcers. The study was performed with all diabetic patients who were attending the three major hospitals in the country from August to November 2022; thus, the study may be generalized to diabetic patients in Mogadishu.
Conclusion
The prevalence of foot ulcers in Somalia is higher than that of many countries in the region. Lack of foot care among patients and the absence of family support were associated with the development of DFUs. Therefore, more intensive health education about footcare directed at diabetes patients and their families might improve the DFUs among diabetes patients in Somalia. Further, regular physical activity for diabetes patients may help them maintain a normal body weight, which may prevent DFUs and subsequent amputations.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Somali National University School of Public Health and Research Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tolossa, T, Mengist, B, Mulisa, D, Fetensa, G, Turi, E, and Abajobi, A. Prevalence and associated factors of foot ulcer among diabetic patients in Ethiopia: a systematic review and meta-analysis. BMC Public Health. (2020) 20:41. doi: 10.1186/s12889-019-8133-y
2. IDF Diabetes Atlas. International diabetes federation, diabetes atlas, (2019). Available at: https://www.diabetesatlas.org/en/resources/
3. Atun, R, Davies, JI, Gale, EAM, Bärnighausen, T, Beran, D, Kengne, AP, et al. Diabetes in sub-Saharan Africa: from clinical care to health policy. Lancet Diabetes Endocrinol. (2017) 5:622–67. doi: 10.1016/S2213-8587(17)30181-X
4. Boulton, AJ, Vileikyte, L, Ragnarson-Tennvall, G, and Apelqvist, J. The global burden of diabetic foot disease. Lancet. (2005) 366:1719–24. doi: 10.1016/S0140-6736(05)67698-2
5. Lipsky, BA, Berendt, AR, Cornia, PB, Pile, JC, Peters, EJ, Armstrong, DG, et al. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. (2012) 54:e132–73. doi: 10.1093/cid/cis346
6. Lavery, LA, Armstrong, DG, Wunderlich, RP, Tredwell, J, and Boulton, AJM. Diabetic foot syndrome: evaluating the prevalence and incidence of foot pathology in Mexican Americans and non-hispanic whites from a diabetes disease management cohort. Diabetes Care. (2003) 26:1435–8. doi: 10.2337/diacare.26.5.1435
7. Rigato, M, Pizzol, D, Tiago, A, Putoto, G, Avogaro, A, and Fadini, GP. Characteristics, prevalence, and outcomes of diabetic foot ulcers in Africa. A systemic review and meta-analysis. Diabetes Res Clin Pract. (2018) 142:63–73. doi: 10.1016/j.diabres.2018.05.016
8. Ministry of health and human services. The Ministry of Health, Somalia health sector strategic plan January 2013. (2016). Available at: http://www.nationalplanningcycles.org/sites/default/files/country_docs/Somalia/the_federal_government_of_somali_republic_health_sector_strategic_plan_2013-2016.pdf.
9. Gele, AA, Ahmed, MY, Kour, P, Moallim, SA, Salad, AM, and Kumar, B. Beneficiaries of conflict: a qualitative study of people's trust in the private health care system in Mogadishu. Somalia Risk Manag Health Policy. (2017) 10:127–35. doi: 10.2147/RMHP.S136170
10. The World Health Organization. Health Systems Profile–Somalia. Geneva: WHO (2006) Regional Health Systems Observatory (EMRO).
12. The World Bank. Diabetes Prevalence (% of population ages 20 to 79). Somalia: The World Bank (2021).
13. Abbas, ZG. Diabetic-foot complications in African and Antarctica continents, chapter 2 In: M Zubair, J Ahmad, A Malik, and MR Talluri, editors. Diabetic Foot Ulcer. Singapore: Springer (2021). 29–40.
14. Abbas, ZG. The diabetic foot worldwide: sub-Saharan Africa In: AJM Boulton, G Rayman, and D Wukich, editors. The Foot in Diabetes. Chichester, UK: John Wiley & Sons Ltd (2020). 379–85.
15. Abbas, ZG, and Bal, A eds. Pocket Guideline of Diabetic Foot 2019; 2nd Edition. Gujarat, India: Jaypee Brothers Medical Publishers (P) Ltd (2019).
16. Sohn, M-W, Budiman-Mak, E, Lee, TA, Oh, E, and Stuck, RM. Significant J-shaped association between body mass index (BMI) and diabetic foot ulcers. Diabetes Metab Res Rev. (2011) 27:402–9. doi: 10.1002/dmrr.1193
17. Assaad-Khalil, SH, Zaki, A, Rehim, AA, Megallaa, MH, Gaber, N, Gamal, H, et al. Prevalence of diabetic foot disorders and related risk factors among Egyptian subjects with diabetes. Prim Care Diabetes. (2015) 9:297–303. doi: 10.1016/j.pcd.2014.10.010
18. Tanamas, SK, Wluka, AE, Berry, P, Menz, HB, Strauss, BJ, Davies-Tuck, M, et al. Relationship between obesity and foot pain and its association with fat mass, fat distribution, and muscle mass. Arthritis Care Res. (2012) 64:262–8. doi: 10.1002/acr.20663
19. Algoblan, A, Alalfi, M, and Khan, M. Mechanism linking diabetes mellitus and obesity. DMSO. (2014) 7:587–91. doi: 10.2147/DMSO.S67400
20. Pierpont, YN, Dinh, TP, Salas, RE, Johnson, EL, Wright, TG, Robson, MC, et al. Obesity and surgical wound healing: a current review. ISRN Obes. (2014) 2014:1–13. doi: 10.1155/2014/638936
21. Kalan, L, Loesche, M, Hodkinson, BP, Heilmann, K, Ruthel, G, Gardner, SE, et al. Redefining the chronic-wound microbiome: fungal communities are prevalent, dynamic, and associated with delayed healing. MBio. (2016) 7:e01058–16. doi: 10.1128/mBio.01058-16
22. Gulam-Abbas, Z, Lutale, JK, Morbach, S, and Archibald, LK. Clinical outcome of diabetes patients hospitalized with foot ulcers, Dar ES salaam. Tanzania Diabet Med. (2002) 19:575–9. doi: 10.1046/j.1464-5491.2002.00740.x
23. Gele, AA, Pettersen, KS, Kumar, B, and Torheim, LE. Diabetes risk by length of residence among Somali women in Oslo area. J Diabetes Res. (2016) 2016:5423405. doi: 10.1155/2016/5423405
24. Mashili, F, Joachim, A, Aboud, S, Mchembe, M, Chiwanga, F, Addo, J, et al. Prospective exploration of the effect of adiposity and associated microbial factors on healing and progression of diabetic foot ulcers in Tanzania: study protocol of a longitudinal cohort study. BMJ Open. (2019) 9:e031896. doi: 10.1136/bmjopen-2019-031896
25. Miller, TA, and Dimatteo, MR. Importance of family/social support and impact on adherence to diabetic therapy. Diabetes Metab Syndr Obes Targets Ther. (2013) 6:421–6. doi: 10.2147/DMSO.S36368
26. Wong-Rieger, D, and Rieger, FP. Health coaching in diabetes: empowering patients to self-manage. Can J Diabetes. (2013) 37:41–4. doi: 10.1016/j.jcjd.2013.01.001
27. Gleeson-Kreig, J, Bernal, H, and Woolley, S. The role of social support in the self-management of diabetes mellitus among a Hispanic population. Public Health Nurs. (2002) 19:215–22. doi: 10.1046/j.0737-1209.2002.19310.x
28. Nicklett, EJ, Heisler, ME, Spencer, MS, and Rosland, AM. Direct social support and long-term health among middle-aged and older adults with type 2 diabetes mellitus. J Gerontol B Psychol Sci Soc Sci. (2013) 68:933–43. doi: 10.1093/geronb/gbt100
29. Mayberry, LS, and Osborn, CY. Family support, medication adherence, and glycemic control among adults with type 2 diabetes. Diabetes Care. (2012) 35:1239–45. doi: 10.2337/dc11-2103
30. Center For Disease Control and Prevention (CDC). Diabetes and your feet. (2022). Available at: https://www.cdc.gov/diabetes/library/features/healthy-feet.html.
31. Gele, AA, Pettersen, KS, Torheim, LE, and Kumar, B. Health literacy: the missing link in improving the health of Somali immigrant women in Oslo. BMC Public Health. (2016) 16:1134. doi: 10.1186/s12889-016-3790-6
32. Bohorquez Robles, R, Compeán Ortiz, LG, González Quirarte, NH, Berry, DC, Aguilera Pérez, P, and Piñones, MS. Knowledge and practices of diabetes foot care and risk of developing foot ulcers in México may have implications for patients of Mexican heritage living in the US. Diabetes Educ. (2017) 43:297–303. doi: 10.1177/0145721717706417
33. Bonner, T, Foster, M, and Spears-Lanoix, E. Type 2 diabetes–related foot care knowledge and foot self-care practice interventions in the United States: a systematic review of the literature. Diabet Foot Ankle. (2016) 7:29758. doi: 10.3402/dfa.v7.29758
34. Dündar, C, and Akinci, GE. Knowledge and practice of foot care in diabetic inpatients: a descriptive cross-sectional study. Erciyes Med J. (2017) 39:160–4. doi: 10.5152/etd.2017.17023
Keywords: diabetes, ulcers, prevalence, hospital, Somalia
Citation: Salad AM, Duale HA, Sheikh IM, Hassan GD, Farah AA and Gele A (2023) Prevalence of diabetes foot ulcers and associated factors among adult diabetic patients in three referral hospitals in Mogadishu, Somalia. Front. Public Health. 11:1195483. doi: 10.3389/fpubh.2023.1195483
Edited by:
Mohammad Zubair, University of Tabuk, Saudi ArabiaReviewed by:
Farha Fatima, Aligarh Muslim University, IndiaLeila Yazdanpanah, Ahvaz Jundishapur University of Medical Sciences, Iran
Copyright © 2023 Salad, Duale, Sheikh, Hassan, Farah and Gele. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abdulwahab M. Salad, YWJkaXNhbGFkMjBAZ21haWwuY29t
 Abdulwahab M. Salad
Abdulwahab M. Salad Hodan A. Duale
Hodan A. Duale Ismael M. Sheikh
Ismael M. Sheikh Gallad Dahir Hassan
Gallad Dahir Hassan Abdiqani A. Farah
Abdiqani A. Farah Abdi Gele
Abdi Gele