- 1School of Nursing and Rehabilitation, Shandong University, Jinan, Shandong, China
- 2Department of Nursing, Qilu Hospital of Shandong University, Shandong, Jinan, China
- 3Nursing Theory and Practice Innovation Research Center, Shandong University, Jinan, Shandong, China
- 4Clinical Epidemiology Unit, Qilu Hospital of Shandong University, Jinan, Shandong, China
Background: Even though occupational women have a high incidence of lower urinary tract symptoms (LUTS), which seriously affect their daily work life, few large scale sample studies have provided empirical evidence to support this phenomenon among female nurses in China. Consequently, this article investigated female nurses who was presupposed to have a high prevalence of LUTS, which adversely exposes their health and patient safety to these risks. Additionally, it is considered important to explore the factors associated with LUTS in female nurses for patient care safety and nurse bladder health practice.
Objectives: The purpose of this study was to assess the incidence of LUTS and symptoms-related risk factors among female nurses, to provide evidence for the prevention and control of LUTS.
Methods: An online survey recruiting 23,066 participants was carried out in a multicenter cross-sectional study in 42 hospitals from December 2020 to November 2022. Stepwise multivariate logistic regression analysis and nomogram were used to identify the factors associated with lower urinary tract symptoms. Besides, SPSS version 26.0, R version 4.2.2, and GraphPad Prism Version 8.3 software packages were used for statistical analysis.
Results: Based on the completion rate of the questionnaire which was 84.1% (n = 19,393), it was found that among 19,393 female nurses, the prevalence of LUTS was 67.71% and this rate was influenced by age, Body Mass Index (BMI), marital status, years of working, menstrual status, mode of delivery, history of breastfeeding, history of miscarriage, history of alcohol and coffee or tea consumption (p < 0.05). Interestingly, we also find that in addition to the above mentioned factors, anxiety, depression, and perceived stress were also related to LUTS in female nurses (p < 0.05).
Conclusion: Given the high prevalence of LUTS among female nurses and their potential influencing factors, female nurses should focus on their reproductive health and develop good lifestyle habits. Thus, nursing managers should provide a warm and harmonious work environment and sensitize female nurses to increase their awareness about the importance of drinking clean water and urinating during work in a hygienic environment.
1. Introduction
Lower urinary tract symptoms (LUTS) have been defined by the International Continence Society (ICS) as three primary symptom groups: storage, voiding, and postmicturition symptoms (1). Unambiguously, based on the findings of numerous scientific and empirical studies, women are more susceptible to LUTS than men—due to the anatomy and physiology of the female genitourinary system (2). Similarly, women’s hormonal environmental experiences and gender-centered social experiences during pregnancy and childbirth (3), can be associated with this health issue (4–6). LUTS have greatly and adversely impacted women’s physical, mental, and sexual health (7) and also reducing their quality of life (8). Thus, LUTS unwittingly impact women’s productivity at work (9), as well as lead to social isolation and shame, which concomitantly increases the risk of depression and anxiety (10), in addition to elevating the financial burden caused by treatment (11).
That said, the findings of some previous studies have indicated that there was a bi-directional relationship between LUTS and work (12). On top of that, since nurses comprise the largest proportion of healthcare occupations throughout the world, with women making up at least 90 percent of this occupational group (13, 14), investigating the effect of LUTS on their work patterns is important. Over and beyond, heavy workloads, long shifts, insufficient breaks, delayed voiding, and limited fluid intake are common unhealthy behaviors affecting nurses’ bladders (15), which epitomizes a global nursing occupational problem (16). Correspondingly, this recognizable characteristic of the nurses’ profession is an issue that contributes to their vulnerability to LUTS (17), so it attracts the extensive attention of researchers.
Furthermore, given that the incidence of LUTS in the female nursing workforce is considerably higher than that in the general population (18, 19), it is an issue of great concern to health practitioners globally. The prevalence of at least one type of LUTS is estimated to be 43% (20) to 97% (2) among female nurses. Apart from that, China’s huge population of over 1.4 billion, evokes some critical issues of diversity in the LUTS faced by female nurses generating an unstable development trend, and diseases related factors are complicated and diverse (21). Numerous studies have shown female nurses with LUTS have been diagnosed to often have co-occurring psychological, physical, and social needs (17, 22–27). Analogously, the effect of work-related factors on LUTS has been generally ignored (2), accentuating the impact of years of working, shift patterns, fluid intake during work, etc., on the severity of this scourge on health-related work productivity is vital. Evidentially, LUTS is therefore more common in female nurses when compared to other medical staff populations (18). Consequently, it is essential to study the influence factors in this diseased population to shed more light on the condition of LUTS among female nurses.
Contemporaneously, the identification of individual, behavioral, and environmental associated with LUTS, as well as occupational factors among female nurses might considerably increase the level of awareness of the importance of preventing lower urinary tract symptoms in nurses. Hence, this study aims to assess the prevalence of LUTS and symptom-related risk factors among female nurses in China based on TARGET (28) study, to provide substantial evidence for the prevention and control of LUTS nationwide.
2. Methods and material
2.1. Design, setting, and participants
In this study, the baseline data elicited from the Nurses’ Health Cohort Study of Shandong [registration number: ChiCTR2100043202] conducted between December 2020 to November 2022 was used. In addition, the dataset was organized using a multi-center cross-sectional study technique and data were collected from nurses in 42 hospitals and 16 cities in the Shandong Province of China. The inclusion criteria included all registered nurses with nursing qualification certificates who volunteered to participate in the study within the enumeration areas. More so, the exclusion criteria were comprised of [a] retired, refresher, and student nurses, [b] nurses who suffered from severe mental illness or took psychotropic drugs; [c] nurses who had been working for <6 months; and [d] nurses who were on leave during the investigation.
2.2. Measures
The questionnaire contained socio-demographic information, International Consultation on Incontinence Questionnaire-Female Lower Urinary Tract Symptoms, ICIQ-FLUTS [Chinese version], Generalized Anxiety Disorder-7 [GAD-7], Patient Health Questionnaire-9 [PHQ-9], and Perceived Stress Scale [PSS], which were distributed among Chinese female nurses.
Additionally, demographic variables included: [1] Age, educational background, marital status, and Body Mass Index (BMI);[2] Work-related variables such as professional title, monthly income, working years, shift mode, and shift working years; [3] Living habits variables which encompassed smoking, drinking frequency, drinking coffee or tea during work, fluid intake during work; and [4] Female health variables such as regular menstruation, pregnant times, parturition times, delivery mode, lactation history, as well as abortion history.
The LUTS of female nurses was measured by the Chinese version of the International Consultation on Incontinence Questionnaire-Female Lower Urinary Tract Symptoms, ICIQ-FLUTS, which was translated by Huang et al. (29). The questionnaire included 12 items in 4 dimensions, including urinary storage symptoms, voiding symptoms, incontinence symptoms and the degree of influence of each symptom on daily life. The 5-level scoring method was used: never, occasionally, sometimes, most of the time, and always. The higher the score, the more serious the symptoms. According to the definition of lower urinary tract symptoms by the International Continence Society in 2012 and the specific items of the ICIQ-FLUTS scale, this study classified the symptoms of storage period [nocturia, urinary urgency, bladder discomfort, frequent urination], urination period [urination hesitation, urination difficulty, urinary flow interruption], incontinence symptoms [urgent urinary incontinence, frequent urinary leakage, stress urinary incontinence, enuresis, nocturnal enuresis] as LUTS, that is, the subjects with any one of the above symptoms can be diagnosed as LUTS (30). The LUTS distress score is 0 for no distress, 1–4 for mild distress, 5–7 for moderate distress, and 8–10 for severe distress. If the research object chooses more than 1 point for any symptom, it is necessary to describe the degree of influence of symptoms on their daily life, and the score range is 0–10 [no influence-extreme influence]. The Cronbach’s α for the LUTS score in this study was 0.811, and the Cronbach’s α for the degree of symptom distress was 0.954.
The Generalized Anxiety Disorder 7-Item Scale [GAD-7], designed by Spitzer et al., with a pretest reliability of 0.830 and a Cronbach’s α of 0.920, indicates good reliability and validity, and has been widely used to screen for the presence and severity of anxiety (31). The total GAD-7 score ranges from 0 to 21 points scoring from zero [not at all] to three (nearly every day) such that 0–4, 5–9, 10–14, and 15–21 scores represent normal, mild, moderate, and severe anxiety, respectively (31). He et al. (32) validated the reliability and validity of the Chinese version of the GAD-7, the test–retest reliability was 0.856 and the Cronbach’s α was 0.898. The Cronbach’s α of the GAD-7 was 0.962 in this study.
The Patient Health Questionnaire [PHQ-9] which contains nine items has been widely used to measure depression symptoms (33). Kroenke et al. examined the reliability and validity of the PHQ-9 and found the retest reliability to be 0.840 and the Cronbach’s α of the questionnaire to be 0.890. The total PHQ-9 score ranges from 0 to 27 points, scoring from zero [not at all] to three [nearly every day] such that 0–4, 5–9, 10–14, 15–19, and 20–27 points represent normal, mild, moderate, moderately severe, and severe depression, respectively (34). Wang et al. validated the reliability and validity of the Chinese version of the PHQ-9 (35), the test–retest reliability was 0.860 and the Cronbach’s α was 0.860. The Cronbach’s α of the PHQ-9 was 0.954 in this study.
The perceived stress scale which contains 10 items was used to assess nurses’ perceptions of stress (36). The Chinese version of the perceived pressure scale used in this study has been verified to have good reliability and validity (37). The coefficient alpha values for the positive and negative subscales were 0.83 and 0.76 for PSS-10, respectively. Each item is measured on a 5-point Likert scale from 0 [never] to 4 [always], and the perceived stress level was divided into three categories: low [0–13], medium [14–27], and high [28–40]. The total PSS-10 score ranges from 0–40 points scoring from zero [never] to four [always] such that 0–13, 14–27, and 28–40 points represent low [0–13], medium [14–27], and high [28–40] perceived stress, respectively. The Cronbach’s α of the scale in this study was 0.932.
2.3. Data collection
Nurses who met the inclusion criteria and agreed to volunteer to enroll in the study, after signing an informed consent form, were duly recruited to complete the questionnaire. The recruitment of all the respondents was carried out through a combination of online and on-site recruitment methods. Online recruitment was carried out via the dissemination of recruitment information through the WeChat instant messaging and social media platform, hospital website, and text messaging. However, on-site recruitment was carried out through presentations, seminars, and via the use of recruitment posters in collaboration with the selected hospitals’ senior administrators such as directors and/or chief nurses of the nursing department of the participating hospital (28).
Thanks to the support of the Shandong Provincial Health and Wellness Commission and the National Institute of Health Care Data, the research team signed a research project cooperation agreement with the participating hospitals and obtained informed consent from each participant. In this online questionnaire, participants first registered their personal information using the official WeChat account of the Shandong Nurses Health Cohort Study. Then, they completed an electronic questionnaire sent by the official WeChat account. The survey questionnaire took about 10 to 15 min to complete. During the data collection process, the research team set up a separate cloud server and a MySQL database cluster (28).
Data managers have access to the data platform of the Nurse Health Cohort Study through an authentication mechanism for data interface calls, data maintenance, and data status monitoring. Only professionals who have signed a confidentiality agreement have direct access to this data. To ensure data quality, the questions and data logic control design required for electronic questionnaires were used (28).
2.4. Data analysis
The descriptive statistics were used to assess continuous variables [i.e., mean (M) ± standard deviation (SD)] and categorical variables [such as frequencies and percentages (%)]. One-way analysis of variance (ANOVA) was performed to examine the difference in continuous variables, and the significance of the difference in categorical variables was assessed via chi-squared testing. Furthermore, variables that were statistically significant in the univariate analysis were considered for inclusion in the backward stepwise multivariate logistic regression analysis to identify the main factors associated with LUTS, and to estimate the adjusted odds ratio (AOR) and 95% confidence interval (CI). Thereafter, the final logistic regression model was determined by the Akaike Information Criterion (AIC) minimization, and variables in the final model were indicated as statistically significant differences at p < 0.05.
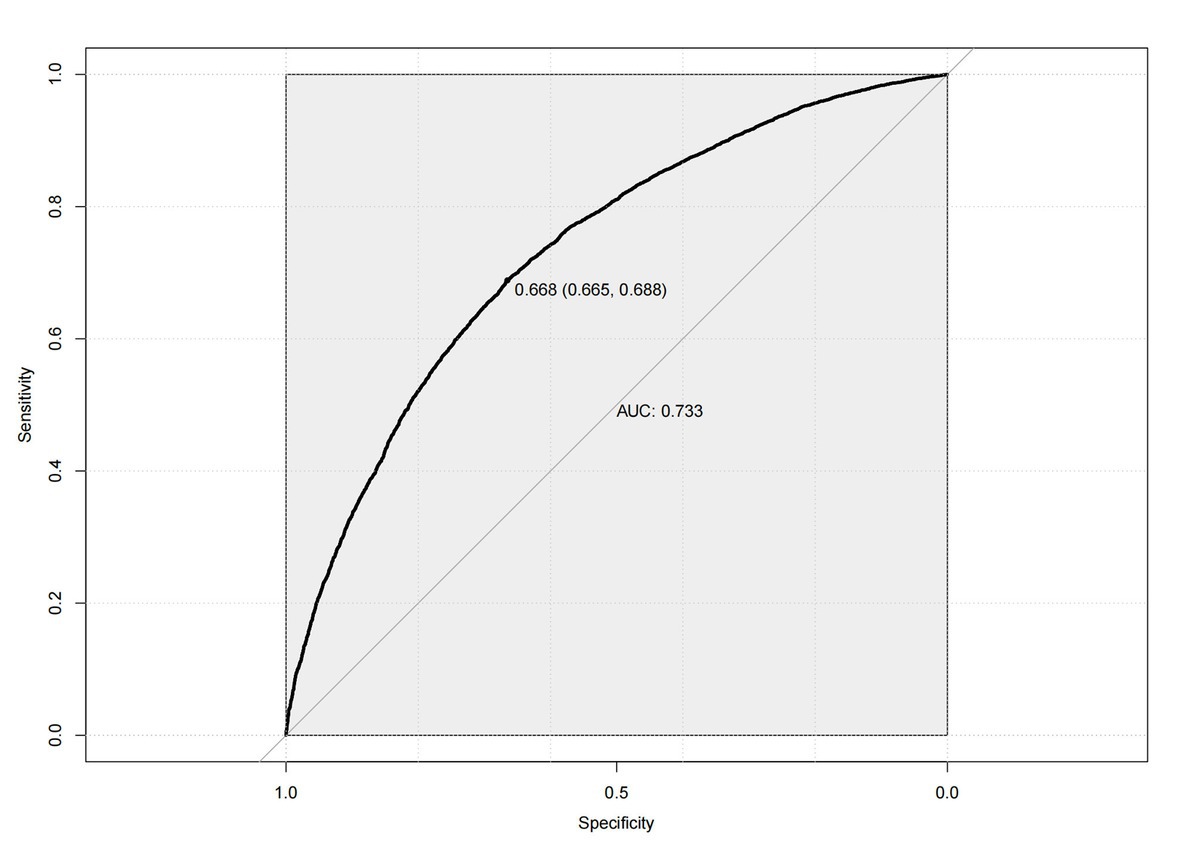
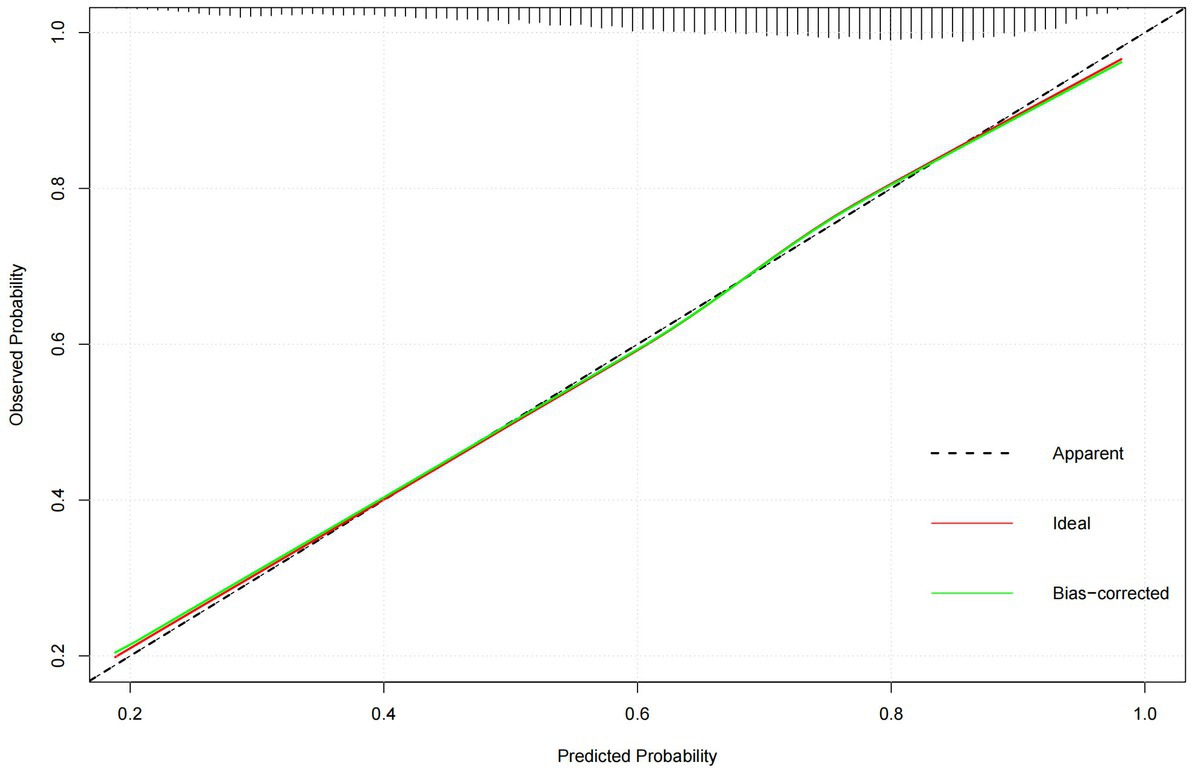
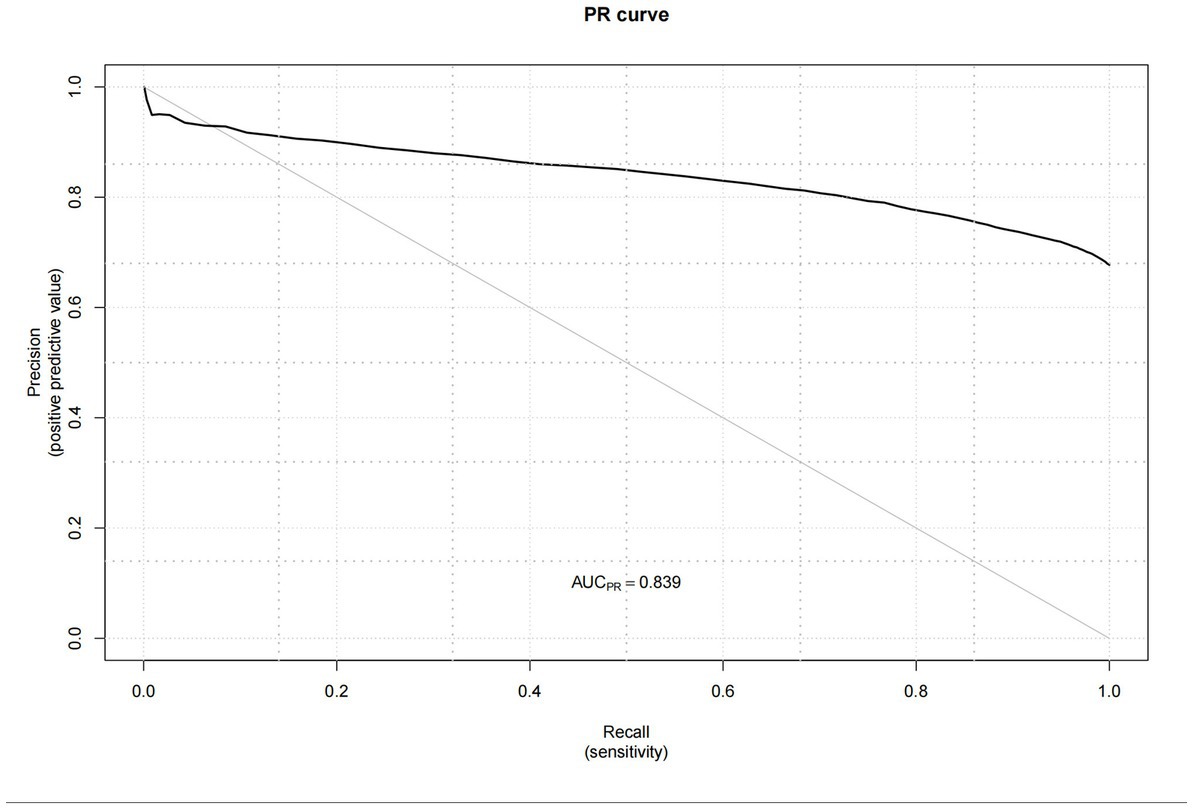
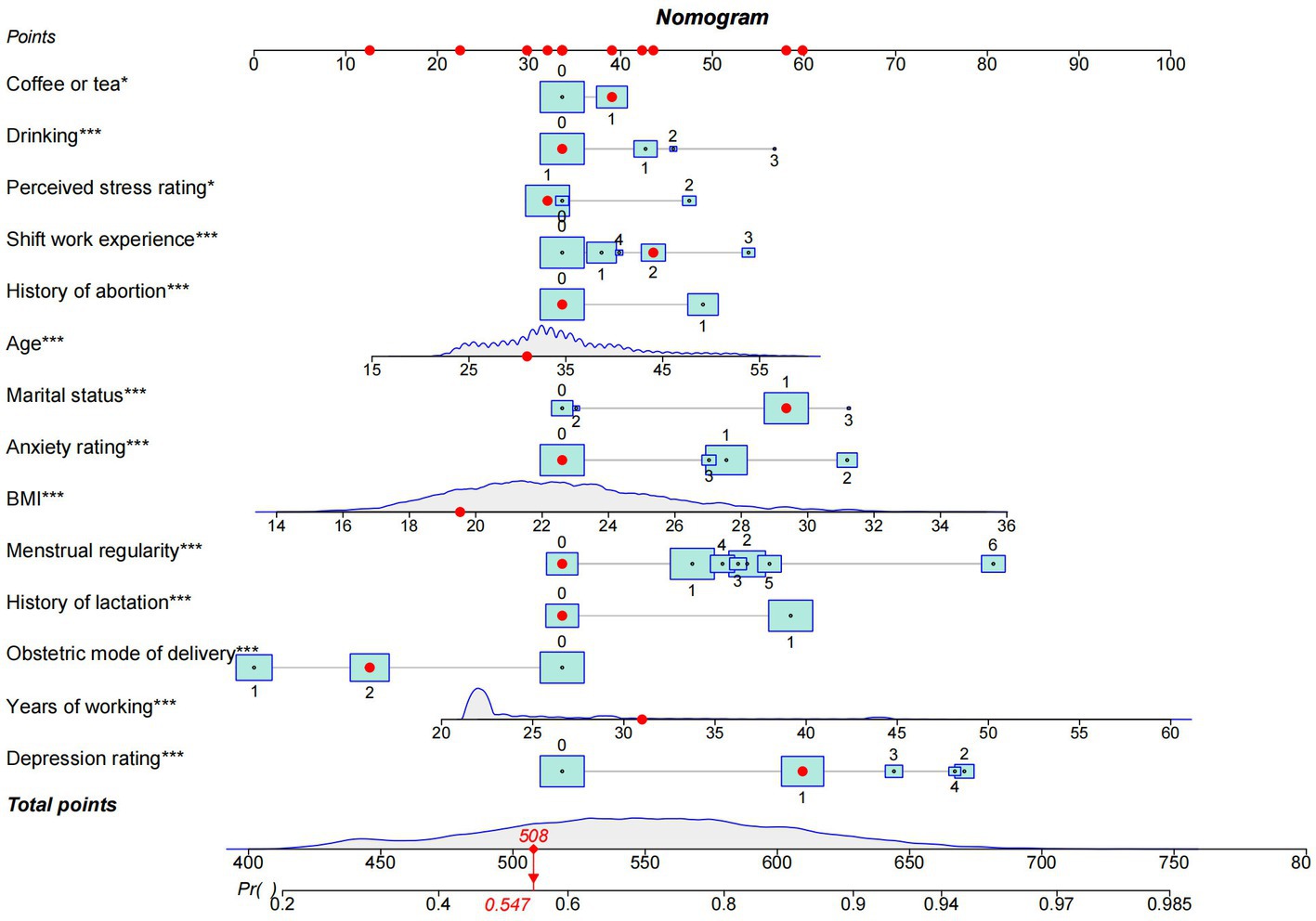
The independent influence variables screened by logistic regression analysis were imported into the software. The “rms package” in R version 4.2.2 was used to build the nomogram model, and the receiver-operating characteristic (ROC) curves, calibration curves and Precision-Recall (Pr) curves were also plotted to evaluate the prediction capability of the model capability. Other data analyses were performed using the SPSS version 26.0. Drawing forest map with GraphPad Prism Version 8.3. The level of significance was set at p < 0.05.
3. Results
3.1. Prevalence and characteristics of LUTS in female nurses
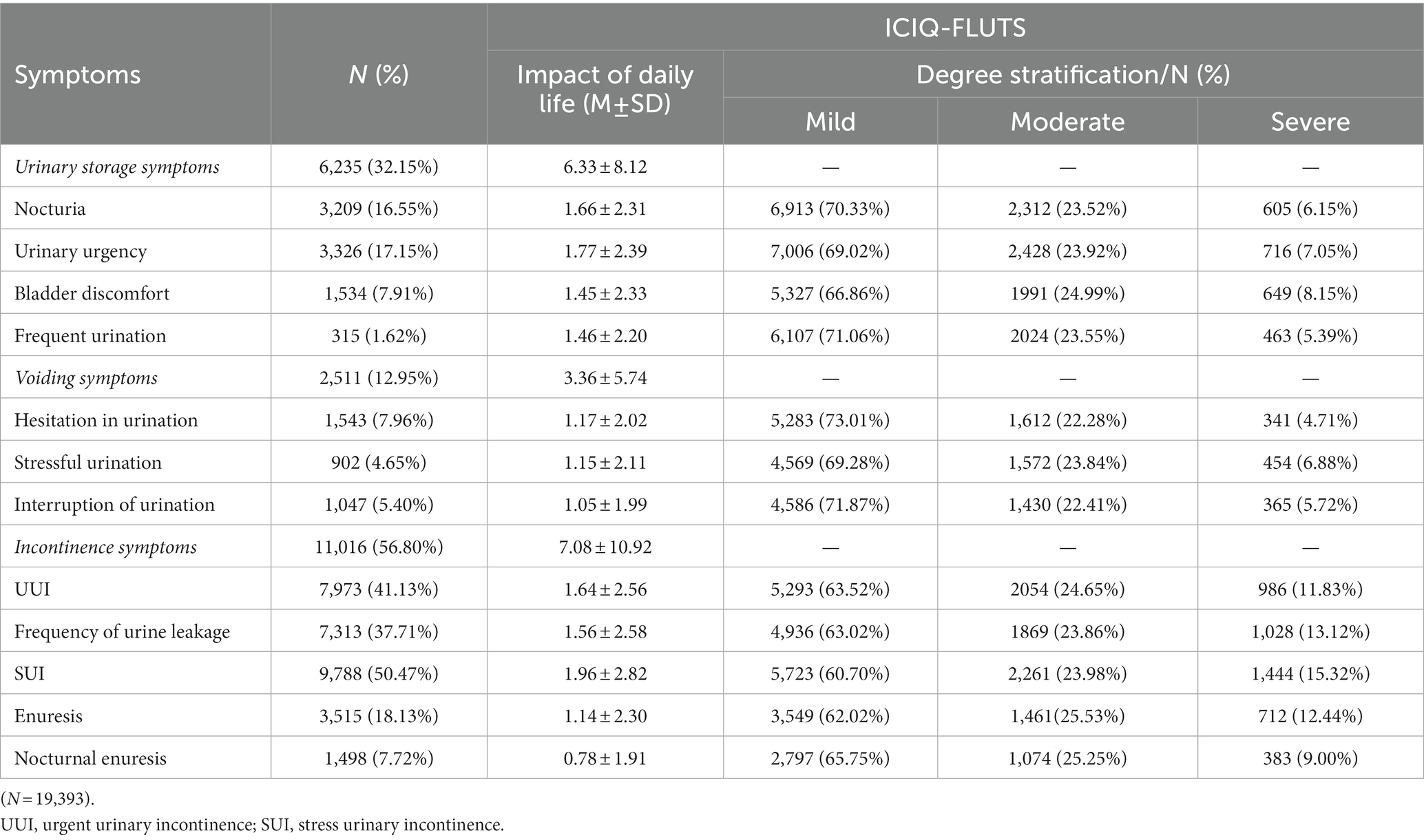
Table 1 shows the distribution of LUTS symptoms among female nurses and the impact on daily life. A total of 23,066 nurses clicked on the questionnaire web link, and 19,393 female nurses completed the questionnaire, indicating an overall response rate of 84.1%. It was observed that the prevalence of LUTS among participating female nurses was high at approximately 67.71%. While, the prevalence of storage symptoms, urination symptoms, and incontinence symptoms were 32.15, 12.95, and 56.80%, respectively. Notably, the prevalence of stress urinary incontinence (SUI) was the highest at 50.47%, just as the probability of frequent urination is lowest at 1.62%. Similarly, incontinence symptoms had the greatest degree of impact on the daily life of female nurses, with 1,444 (i.e., 15.32%) being severely influenced by stress urinary incontinence (SUI) and 1,028 (i.e., 13.12%) being severely affected by leakage of urine (Figure 1).

Figure 1. Symptoms-specific bother and extent of individual lower urinary tract symptoms. (A) Nocturia; (B) Urinary urgency; (C) Discomfort in the bladder area; (D) Frequent urination; (E) hesitation in urination; (F) Stressful urination; (G) Interruption of urination; (H) UUI; (I) Frequency of urine leakage; (J) SUI; (K) Enuresis; (L) Normal enuresis.
Table 2 shows that the mean age of the 19,393 participants was 34.64 (SD = 7.095) years. While the mean working years for nurses was 26.65 (SD = 7.495) years. Likewise, the mean BMI of nurses was 22.59 (SD = 3.152). Approximately 91.4% of participants had bachelor’s degrees, 79.0% were married, and 50.5% had a primary title. Additionally, approximately half of the participants with an average monthly income of less than or equal to 6,000 Chinese Yuan (CNY). Interestingly, over half of the participants (i.e., 63.3%) have been working in shifts, while nearly half (i.e., 46.3%) had worked in shifts for more than 5 years.

Table 2. Descriptive statistics and univariate analysis of variables related to lower urinary tract symptoms in female nurses.
When considering women’s health, it was found that approximately one-third of participants experienced irregular menstruation. Over and above that, about 70% of them have the experience of gravidity, with 68.3% having given birth at least once, 40.7% having a history of vaginal delivery, 65.0% having a history of lactation, and just as 32.0% had a history of abortion. Moreover, it should be noted that 99.7% of participants reported never smoking, 76.6% reported never drinking alcohol, and 32.8% reported drinking coffee or tea, while half of the participants reported consuming less than 500 mL of fluid during work.
Furthermore, with regards to mental health, it was found that nurses with LUTS (n = 13,131), 62.1% (n = 8,150) experienced some level of anxiety (where, mild = 44.2%, moderate = 12.0%, severe = 5.9%), while 65.1% (n = 8,620) experienced some level of depression (where, mild = 42.6%, moderate =10.2%, moderately severe = 8.0%, severe = 4.1%), and 93.2% (n = 12,329) experienced some level of perceived stress (where, medium = 83.2%, high = 9.9%).
3.2. The univariate analysis of factors associated with LUTS
Table 2 also shows all the respondents’ univariate analysis of LUTS from work-related characteristics, female health characteristics, dietary characteristics, and mental health characteristics. It was thereafter established that there were significant differences in distribution patterns between the group with LUTS and the group without it (p < 0.05). It was uncovered that these differences can be grouped by respondents’ age, education, marital status, BMI, professional title, monthly income, years of work, scheduling mode, shift work experience, menstrual regularity, gravidity, production, obstetric mode of delivery, history of lactation, history of abortion, drinking alcohol, consuming coffee or tea, as well as anxiety, depression, and perceived stress rating levels.
3.3. Stepwise multivariate logistic regression analysis of factors associated with LUTS
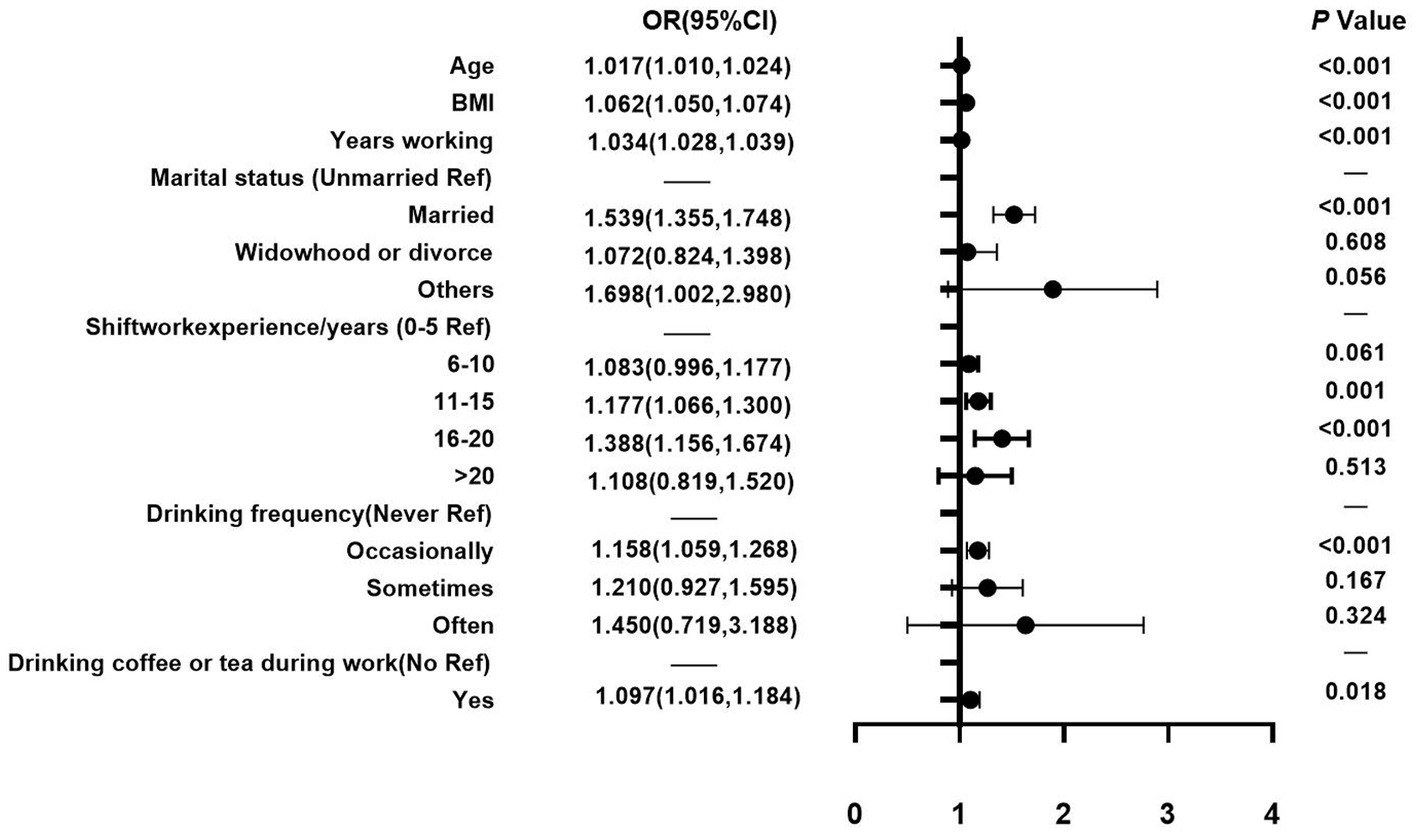
Table 3 shows the results of the backward stepwise multivariate logistic regression model with an adjusted odds ratio (AOR) and 95% CI and the main variables including demographic factors, work-related factors, living habits factors, female health factors, and psychological factors. With regards to demographic and work-related factors (Figure 2), it was found that among female nurses, each 1-unit increase in BMI was associated with a 6.2% increase in the odds of female nurses suffering from LUTS in this study. Relatedly, the odds of having LUTS increased by either 1.7% or 3.4% for every 1-year increase in age or working years among female nurses, respectively. Comparatively, when unmarried nurses were compared to those who were married, nurses who were married were significantly more likely to experience LUTS (AOR = 1.539, 95% CI: 1.355–1.748). Besides, relative to nurses who had 0–5 years of shift work experience, those who had between 11–15 years and 16–20 years were significantly more likely to experience LUTS than those at the early stage of their career (AOR = 1.177, 95% CI: 1.066–1.300; AOR = 1.388, 95% CI: 1.156–1.674). With regards to living habits (Figure 2), it was found that when nurses who never drank alcohol were compared to those who drink occasionally, those who drank alcohol occasionally (AOR =1.158, 95% CI: 1.059–1.268) were significantly more likely to experience LUTS. Nevertheless, drinking coffee or tea was also associated with LUTS among female nurses (AOR = 1.097, 95% CI: 1.016–1.184).
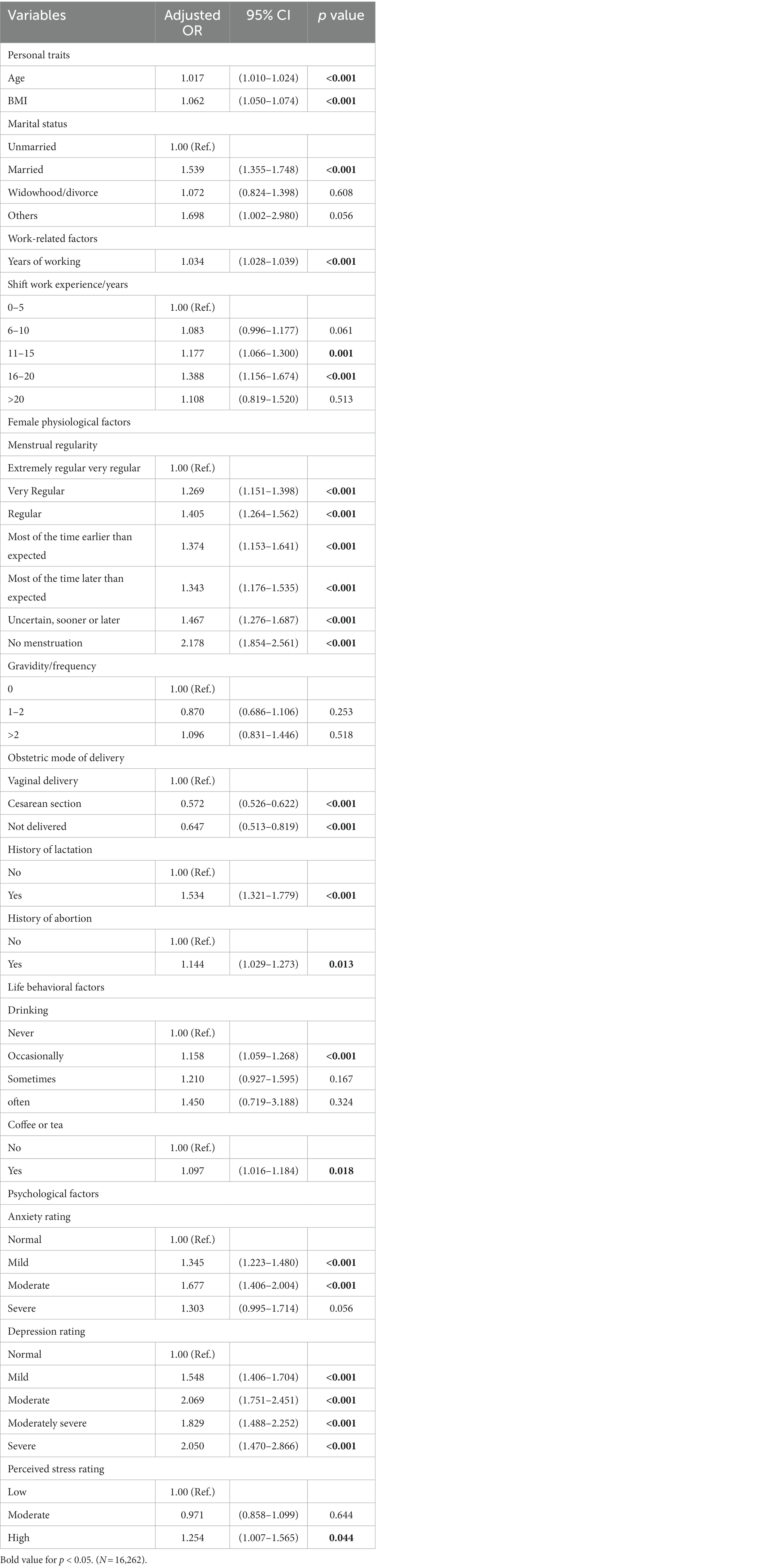
Table 3. Backward stepwise multivariate logistic regression analysis of factors associated with lower urinary tract symptoms in female nurses.
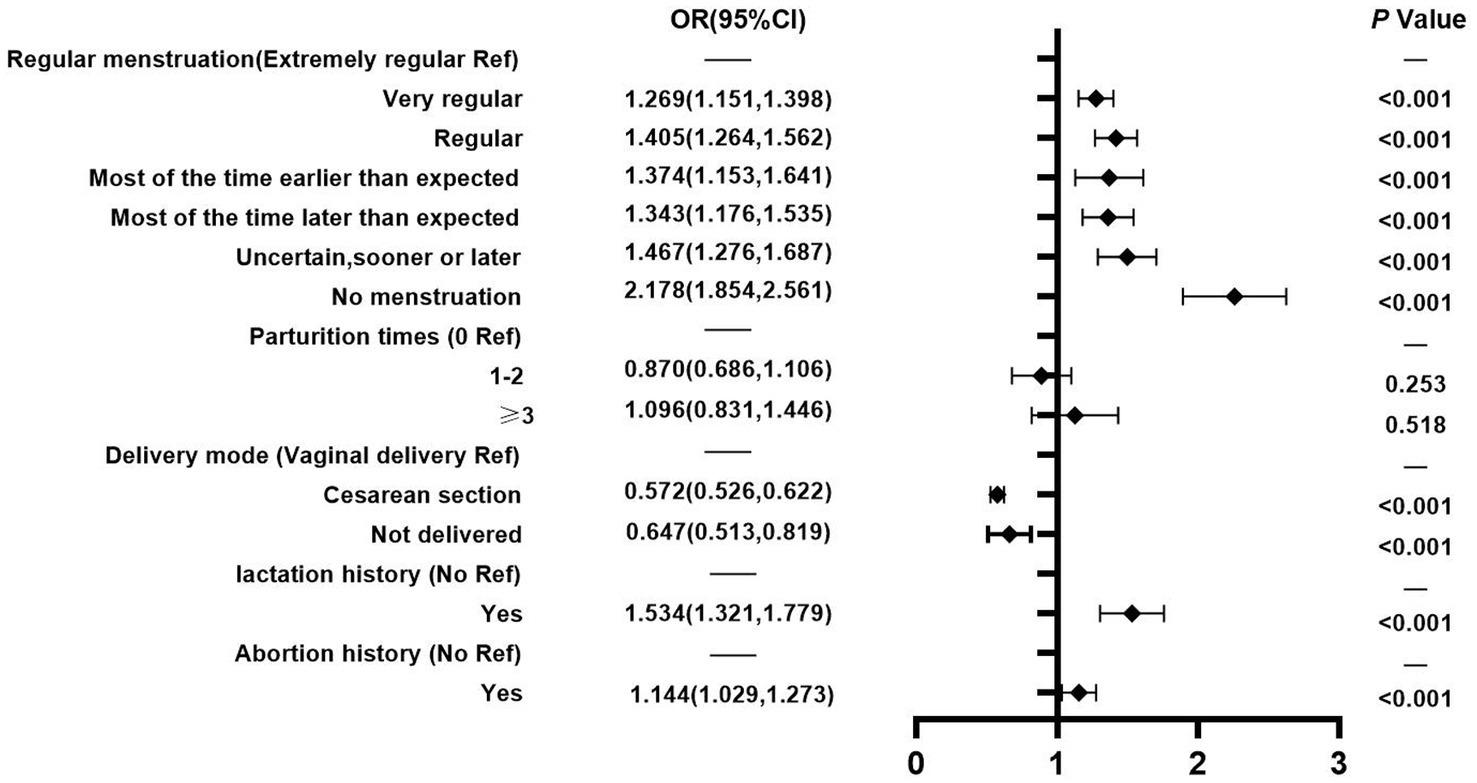
In terms of female health factors (Figure 3), nurses whose menstruation was very regular, regular, and most of the time earlier than expected, as well as those whose menstruation was most of the time later than expected, uncertain, sooner or later, and with no menstruation were significantly more likely to experience LUTS than those who had extremely regular menstruation (AOR = 1.269, 95% CI: 1.151–1.398; AOR = 1.405, 95% CI: 1.264–1.562; AOR = 1.374, 95% CI: 1.153–1.641; AOR = 1.343, 95% CI: 1.176–1.535; AOR = 1.467, 95% CI: 1.276–1.687; and AOR = 2.178, 95% CI:1.854–2.561), respectively. Additionally, female nurses who experienced lactation (AOR =1.534, 95% CI: 1.321–1.779) or experienced abortion (AOR = 1.144, 95% CI: 1.029–1.273) were more likely to develop LUTS than nurses who did not have such experience. Interestingly, nurses who went through cesarean section delivery or have not delivered (AOR = 0.572, 95% CI: 0.526–0.622; AOR = 0.647, 95% CI: 0.513–0.819) were less likely to develop LUTS than those who had a vaginal delivery.
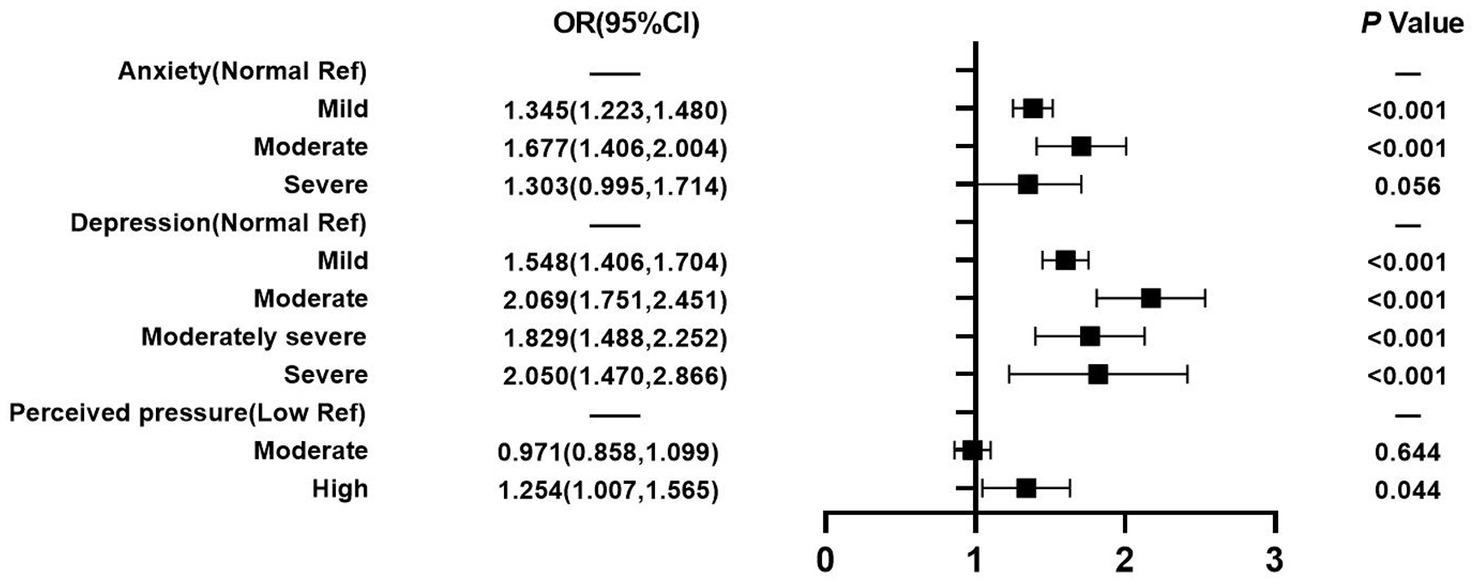
Figure 4 reveals that mental health factors were also found to be associated with LUTS. When nurses who reported a normal level of anxiety were compared to those who reported a mild or moderate level of anxiety, nurses who reported mild or moderate levels of anxiety were significantly more likely to experience LUTS, with an AOR of 1.345 (95% CI: 1.223–1.480) and AOR of 1.677 (95% CI: 1.406–2.004), respectively. Similarly, nurses who reported mild, moderate, moderately severe, or severe levels of depression were significantly more likely to experience LUTS, with AOR of 1.548 (95% CI: 1.406–1.704), 2.069 (95% CI: 1.751–2.451), 1.829 (95% CI: 1.488–2.252), and 2.050 (95% CI: 1.470–2.866), respectively. Likewise, a perceived high-stress level had a statistically significant association with LUTS when compared to a perceived normal-stress level, with an AOR of 1.254 (95% CI: 1.007–1.565).
3.4. Nomogram model of LUTS in female nurses
Next, the performance of the model empirically was evaluated before analyzing its predictors. The results indicated in Figure 5 showed that the predictive efficiency of the logistic regression model was adequate (sensitivity = 0.688, specificity = 0.665, accuracy = 0.681, and area under the receiver operating characteristic curve [AUROC] = 0.733 (95% CI: 0.725–0.740)). The calibration curves (Figure 6) were close to the ideal prediction with a mean absolute error (MAE) of 0.005 after 1,000 bootstrap self-sampling. Furthermore, The Precision-Recall (Pr) curves were depicted in Figure 7. Consequently, the predictive performance of the models that were adopted in this study was guaranteed. The column line graph model (Figure 8) was constructed using 14 risk predictors, which can personalize the calculation of the score corresponding to each independent influencing factor, as well as count the total score and show the predicted value corresponding to the total score which can predict the probability of occurrence of LUTS.
4. Discussion
4.1. Prevalence of LUTS in female nurses
The study was conducted to assess the prevalence and risk factors of LUTS among Chinese female nurses. The result of this study showed that the prevalence of LUTS among 19,393 female nurses from Shandong, China was 67.71%. This estimate is higher than the rate of prevalence of LUTS in Turkey (20), which stands at 44.5%, but lower than the reported 97.36% prevalence rate of LUTS in Iran (2), in comparison to the 89.63% prevalence rate of LUTS among female nurses in Beijing, China (38). An analysis of data obtained from the pilot study carried out by The Taiwan Nurse Bladder Survey (TNBS) revealed that there was a 65% prevalence rate of LUTS among female nurses in Taipei (17), Taiwan which is roughly consistent with the current findings (67.71%). However, this figure is significantly higher than the prevalence rate of LUTS among the adult female population in China, which stands at 55.5% (39). This result indicated that female nurses might considerably suffer from the impact of LUTS in China. Moreover, increased LUTS prevalence could lead to reduced work efficiency or even unemployment, as well as affect their lifelong physical and mental health later in life. Accordingly, the inconsistencies emanating from the different prevalence rates of LUTS in similar studies can be linked to the time frame of prior studies, the research and analysis methods employed, as well as the diverse composition of the studied population, which can be limited to the entire population, age group, and/or ethnicity (40). Therefore, it is hoped that a large scale epidemiological survey of female nurses will be conducted in all countries, using the same questionnaire, to reveal the bladder health status of female nurses worldwide.
4.2. Personal traits and work-related factors
Age and BMI are well-known risk factors influencing the sufferers of LUTS. This assumption is reinforced by the findings of the present study. That said, it has been demonstrated in extant studies carried out across North America (41) and Asia (25, 42). Nonetheless, overweight or obese women with long-term abdominal hypertension may experience an increase in bladder pressure and urethral mobility, which can lead to pelvic organ prolapse, and an increased burden on the pelvic floor muscles (43). In addition, constipation might also increase abdominal pressure during physical activity or defecation, which in turn leads to LUTS (24). Due to a combination of factors and reasons, constipation-related issues were not included in this study. Hence, it was hoped that related studies will include this variable in future research centered on LUTS. In a study by Yuliang et al. in China (44) and a systematic review by Sedighe et al. worldwide (24), bare that excessive BMI is a negative factor in increasing the incidence of LUTS among female nurses. Over and beyond, marriage is also a critical risk factor affecting LUTS among female nurses in China, when this segment of the population is compared to unmarried women, which is consistent with the findings of similar studies (25, 45). Physiologically, married women begin to experience sexual behavior, pregnancies, and even deliveries, and they are easily exposed to LUTS. Psychologically, married women have to take on the burden of a family and deal with complex interpersonal issues, therefore, aggravating stressful conditions may possibly increase the chance of LUTS.
In terms of work-related factors, years of working and long shift working were significantly associated with LUTS among female nurses. Similarly, Zhang’s study (46), revealed that there was a statistically significant difference between work experience and the probability of LUTS among female nurses. The reason for this phenomenon might be the heavy workload, in addition to the high level of work stress experienced over the years by these nurses, which may negatively affect their bladder function. It was also assumed that since the years of work are proportional to age, the relationship between years of work and LUTS is not hard to understand. Additionally, common work environmental factors associated with occupational stress such as high work demand and work overload negatively impacted female nurses’ exposure to LUTS in China (47). As Hyoungseob et al. discovered that unhealthy toileting behaviors to empty their bladders, which mediates the relationship between occupational stress and OAB (48), and the most common behavior was delayed urination. This Phenomenon illustrates the gravity of stress-related issues affecting female nurses in China.
4.3. Life behavioral factors
In this study, drinking alcohol occasionally increased the risk of female nurses contracting LUTS when compared to those that never attempted to do so. However, drinking alcohol sometimes or often drinking alcohol is not associated with LUTS among female nurses. Notably, similar results have been reported in previous studies, although the findings of these studies were controversial (25, 49). Apart from that, light alcohol consumption induces LUTS by increasing sympathetic nervous system activity thereby exerting diuretic effects on the antidiuretic hormone system (50), while moderate to a high level of alcohol consumption appears to reduce the prevalence of LUTS due to enhanced estrogen receptor induction (51). Nevertheless, the frequency of smoking was empirically proven to be unrelated to LUTS, thereby debunking what was put forward by past studies in this area (27, 44). Interestingly, this finding is possibly because the population included in this study was a group of female nurses with relatively healthy lifestyles.
What’s more, it is found that coffee or tea consumption is a risk factor for LUTS among female nurses in China, possibly mediated by caffeine effects such as an increase in diuresis, central nervous stimulation, and increased contractility of the lower urinary tract smooth muscle. Yet, this finding remains disputed, since there is no association between coffee consumption and LUTS found in several cross-sectional studies (52, 53). Interestingly, in Tomlinson’s study, there is an association between a reduction in dietary caffeine intake and a reduction in daytime incontinence, although this was not proven to be statistically significant in this research (54). Additionally, a recent pilot study of 11 women showed an overall reduction in bladder symptoms with caffeine-free beverages when compared to women that ingested caffeine-containing beverages (55). In like manner, the relationship between tea intake and LUTS was substantiated in one study which established a positive association between women who drank two or more cups of tea per day and overactive bladder and nocturia, just as there exists a negative association between tea consumption and stress urinary incontinence (56). The caffeine content of tea is about one-third of that found in coffee (57), suggesting that tea may contain components other than caffeine that may also be related to lower urinary tract dysfunction.
4.4. Female physiological factors
The related analysis of physiological factors revealed that female nurses were prone to risk factors that trigger LUTS such as irregular menstruation, mode of vaginal delivery, history of miscarriage, and history of breastfeeding. Apart from that, it has been scientifically proven that vaginal delivery and the number of deliveries were among the most important risk factors affecting female patients with urinary incontinence (58). However, based on the findings of an Indian study, there was no association between delivery and urinary incontinence, which is inconsistent with the findings of this study (59). Interestingly, hormonal effects and mechanical changes are considered to be the main causes of LUTS during pregnancy (60). In this study, it was found that a dose–response effect of pregnancy was critical, just as multiple pregnancies were an important risk factor for the development of LUTS, which may be the result of repetitive injury to the peripheral pelvic nerves, as well as direct injury to the pelvic supporting tissues (61). Similarly, Zhang et al. reported that women who underwent vaginal delivery were more likely to experience symptoms during the urine storage period (62). It is observed that this may be related to peripheral pelvic nerve injury and direct injury to the intrapelvic fascia. However, cesarean delivery can eliminate damage to either the pelvic floor muscle tissue or the public nerves during delivery, as well as prevent the development of LUTS among female nurses (62).
4.5. Psychological factors
In the current study, it has been proven that negative emotions including anxiety, depression, and perceived pressure contribute to the development of LUTS among female nurses, which has been reinforced by the findings of similar studies (63, 64). It was also envisaged that there is a link between psychological dysfunction and bladder function. Researchers have suggested that the pro-adrenocorticotropic hormone-releasing factor is expressed in areas of the central nervous system that control voiding and stress responses, while the pro-adrenocorticotropic hormone-releasing factor increases in response to anxiety, depression, pain, and dysfunction of the pelvic organs (65). We can therefore decisively submit that LUTS are not fatal but do have a serious impact on women’s mental health. LUTS can largely interfere with an individual’s self-image (66), consequently, the stigma and embarrassment caused by LUTS may lead to feelings of anxiety, depression, and stress among female nurses in China. This can be linked to the fact that patients with LUTS might worry about its development, the possibility of cancer, and their sexuality, which can ultimately create a certain amount of stress among this segment of the population (67).
4.6. Limitations
To the best of our knowledge, this is one of the largest sample studies on the prevalence of LUTS among female nurses in China. The large sample size and wide survey area are the main strengths of this study. Besides, this study involved hospitals at various levels across all the regions of Shandong Province of China which can better reflect the reality of the problems. However, the participants who did not meet the study requirements were excluded to obtain more realistic results. This study also has some limitations. First, the survey of the study gathering phase was carried out only within Shandong province, therefore, the results obtained cannot be extended to the whole country or even a larger area due to regional restrictions and differences. Second, it is a cross-sectional study and cannot verify the causal relationship therein, which implies that a large sample longitudinal study is required to ascertain the causal relationship that exists between factors and LUTS among female nurses in China. Third, due to occupational specificity, fewer male nurses, and the differences in the way LUTS are scored, no male group was included in this study, which is a major limitation when measuring the influence of gender on the infection rates of LUTS patients. Fourth, this study did not use objective indicators to measure LUTS, since the diagnosis we relied upon was based on scales rather than clinical criteria, thus, it shows the existence of recall bias in current dataset.
5. Conclusion
In summary, many of the risk factors associated with LUTS can be offset by a healthy lifestyle, proper urinary habits, frequent physical activity, and weight control (68). Consequently, for female nursing staff, attention needs to be paid to the impact of their work environment on their overall well-being, such as raising awareness among managers to provide educational opportunities for nurses, as well as advocating for the justification of the benefits of nurses’ personal health and bladder health practices in the workplace. Sadly, the habit among nurses of not drinking water or using the toilet in the workplace frequently is a hidden nursing workforce crisis that raises the issue of dignity and human rights in the healthcare industry. Managers, therefore, need to assess nurses’ needs and workplace barriers to healthy practices to ensure their water and toilet use is sufficient, as well as minimize barriers to work and maximize nurses’ bladder health ceteris paribus (69).
Data availability statement
The datasets presented in this article are not readily available because the data from the Nurses’ Health Cohort Study of Shandong needs time for data clearing and the establishment of guidelines. This data will be made public in the future. Requests to access the datasets should be directed to Y2FveWpAc2R1LmVkdS5jbg==.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Scientific Research of Shandong University Qilu Hospital. The patients/participants provided their written informed consent to participate in this study.
Author contributions
XZ and ML: methodology, formal analysis, data curation, software, writing-original draft, and visualization. XZ, WD, and XL: writing-review and editing and project administration. XZ, ML, XL, and LL: investigation. XY: methodology. YC: conceptualization, resources, supervision, project administration, and funding acquisition. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors are grateful to the nurses who participated in the Nurses’ Health Cohort Study of Shandong and also appreciate the Health Commission of Shandong Province for providing assistance in the study design and development. The authors acknowledge TopEdit (www.topeditsci.com) for the linguistic editing and proofreading during the preparation of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Haylen, BT, de Ridder, D, Freeman, RM, Swift, SE, Berghmans, B, Lee, J, et al. An international Urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. (2010) 29:4–20. doi: 10.1002/nau.20798
2. Nasiri, M, Sigaroudi, AE, Moghadamnia, MT, and Leili, EK. Lower urinary tract symptoms and related factors in Iranian female nurses. Iran J Nurs Midwifery Res. (2022) 27:280–6. doi: 10.4103/ijnmr.ijnmr_126_21
3. Brady, SS, Bavendam, TG, Berry, A, Fok, CS, Gahagan, S, Goode, PS, et al. The prevention of lower urinary tract symptoms (PLUS) in girls and women: developing a conceptual framework for a prevention research agenda. Neurourol Urodyn. (2018) 37:2951–64. doi: 10.1002/nau.23787
4. Maserejian, NN, Chen, S, Chiu, GR, Wager, CG, Kupelian, V, Araujo, AB, et al. Incidence of lower urinary tract symptoms in a population-based study of men and women. Urology. (2013) 82:560–4. doi: 10.1016/j.urology.2013.05.009
5. Brady, SS, Berry, A, Camenga, DR, Fitzgerald, CM, Gahagan, S, Hardacker, CT, et al. Applying concepts of life course theory and life course epidemiology to the study of bladder health and lower urinary tract symptoms among girls and women. Neurourol Urodyn. (2020) 39:1185–02. doi: 10.1002/nau.24325
6. Sutcliffe, S, Bavendam, T, Cain, C, Epperson, CN, Fitzgerald, CM, Gahagan, S, et al. The Spectrum of bladder health: the relationship between lower urinary tract symptoms and interference with activities. J Womens Health (Larchmt). (2019) 28:827–1. doi: 10.1089/jwh.2018.7364
7. Coyne, KS, Sexton, CC, Kopp, ZS, Ebel-Bitoun, C, Milsom, I, and Chapple, C. The impact of overactive bladder on mental health, work productivity and health-related quality of life in the UK and Sweden: results from EpiLUTS. BJU Int. (2011) 108:1459–71. doi: 10.1111/j.1464-410X.2010.10013.x
8. Pizzol, D, Demurtas, J, Celotto, S, Maggi, S, Smith, L, Angiolelli, G, et al. Urinary incontinence and quality of life: a systematic review and meta-analysis. Aging Clin Exp Res. (2021) 33:25–35. doi: 10.1007/s40520-020-01712-y
9. Markland, A, Chu, H, Epperson, CN, Nodora, J, Shoham, D, Smith, A, et al. Occupation and lower urinary tract symptoms in women: a rapid review and meta-analysis from the PLUS research consortium. Neurourol Urodyn. (2018) 37:2881–92. doi: 10.1002/nau.23806
10. Choi, EP, Lam, CL, and Chin, WY. Mental health mediating the relationship between symptom severity and health-related quality of life in patients with lower urinary tract symptoms. Low Urin Tract Sympt. (2016) 8:141–9. doi: 10.1111/luts.12086
11. Powell, LC, Szabo, SM, Walker, D, and Gooch, K. The economic burden of overactive bladder in the United States: a systematic literature review. Neurourol Urodyn. (2018) 37:1241–9. doi: 10.1002/nau.23477
12. O'Shea, SD, Pope, R, Freire, K, and Orr, R. Prevalence of lower urinary tract symptoms in a cohort of Australian servicewomen and female veterans. Int Urogynecol J. (2022) 34:885–6. doi: 10.1007/s00192-022-05254-x
13. Australian Institute of Health and Welfare . Health workforce. Australian Institute of Health and Welfare. (2015) Available at: http://www.aihw.gov.au/workforce/ (accessed December 15, 2022).
14. World Health Organization . Health workforce: nursing and mid-wifery personnel (2018). Global Health Observatory data) 2018
15. Pierce, H, Perry, L, Gallagher, R, and Chiarelli, P. Culture, teams, and organizations: a qualitative exploration of female nurses' and midwives' experiences of urinary symptoms at work. J Adv Nurs. (2019) 75:1284–95. doi: 10.1111/jan.13951
16. Wendsche, J, Ghadiri, A, Bengsch, A, and Wegge, J. Antecedents and outcomes of nurses' rest break organization: a scoping review. Int J Nurs Stud. (2017) 75:65–80. doi: 10.1016/j.ijnurstu.2017.07.005
17. Liao, YM, Yang, CY, Kao, CC, Dougherty, MC, Lai, YH, Chang, Y, et al. Prevalence and impact on quality of life of lower urinary tract symptoms among a sample of employed women in Taipei: a questionnaire survey. Int J Nurs Stud. (2009) 46:633–4. doi: 10.1016/j.ijnurstu.2008.12.001
18. Pierce, H, Perry, L, Chiarelli, P, and Gallagher, R. A systematic review of prevalence and impact of symptoms of pelvic floor dysfunction in identified workforce groups. J Adv Nurs. (2016) 72:1718–34. doi: 10.1111/jan.12909
19. Wan, X, Wu, C, Xu, D, Huang, L, and Wang, K. Toileting behaviors and lower urinary tract symptoms among female nurses: a cross-sectional questionnaire survey. Int J Nurs Stud. (2017) 65:1–7. doi: 10.1016/j.ijnurstu.2016.10.005
20. Kaya, Y, Kaya, C, Baseskioglu, B, Ozerdoğan, N, Yenilmez, A, and Demirüstü, C. Effect of work-related factors on lower urinary tract symptoms in nurses and secretaries. Low Urin Tract Sympt. (2016) 8:49–54. doi: 10.1111/luts.12073
21. Qi, M, Hu, X, Liu, J, Wen, J, Hu, X, Wang, Z, et al. The impact of the COVID-19 pandemic on the prevalence and risk factors of workplace violence among healthcare workers in China. Front Public Health. (2022) 10:938423. doi: 10.3389/fpubh.2022.938423
22. Xie, X, Chen, Y, Khan, A, Long, T, Li, S, and Xie, M. Risk factors for urinary incontinence in Chinese women: a cross-sectional survey. Female Pelvic Med Reconstr Surg. (2021) 27:377–1. doi: 10.1097/SPV.0000000000000871
23. Chuang, YC, Liu, SP, Lee, KS, Liao, L, Wang, J, Yoo, TK, et al. Prevalence of overactive bladder in China, Taiwan and South Korea: results from a cross-sectional, population-based study. Low Urin Tract Sympt. (2019) 11:48–55. doi: 10.1111/luts.12193
24. Batmani, S, Jalali, R, Mohammadi, M, and Bokaee, S. Prevalence and factors related to urinary incontinence in older adults women worldwide: a comprehensive systematic review and meta-analysis of observational studies. BMC Geriatr. (2021) 21:212. doi: 10.1186/s12877-021-02135-8
25. Wang, Y, Xu, K, Hu, H, Zhang, X, Wang, X, Na, Y, et al. Prevalence, risk factors, and impact on health related quality of life of overactive bladder in China. Neurourol Urodyn. (2011) 30:1448–55. doi: 10.1002/nau.21072
26. Vaughan, CP, and Markland, AD. Urinary incontinence in women. Ann Intern Med. (2020) 172:ITC17–32. doi: 10.7326/AITC202002040
27. Noh, JW, Yoo, KB, Kim, KB, Kim, JH, and Kwon, YD. Association between lower urinary tract symptoms and cigarette smoking or alcohol drinking. Transl Androl Urol. (2020) 9:312–1. doi: 10.21037/tau.2020.03.07
28. Lv, X, Cao, Y, Li, Y, Liu, Y, Li, R, Guan, X, et al. The TARGET Nurses' health cohort study protocol: towards a revolution in getting nurses' health ticked. J Adv Nurs. (2022) 78:1815–23. doi: 10.1111/jan.15204
29. Huang, L, Zhang, SW, Wu, SL, Ma, L, and Deng, XH. The Chinese version of ICIQ: a useful tool in clinical practice and research on urinary incontinence. Neurourol Urodyn. (2008) 27:522–4. doi: 10.1002/nau.20546
30. Abrams, P, Cardozo, L, Fall, M, Griffiths, D, Rosier, P, Ulmsten, U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the international continence society. Urology. (2003) 61:37–49. doi: 10.1016/S0090-4295(02)02243-4
31. Spitzer, RL, Kroenke, K, Williams, JB, and Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
32. He, XY, Li, CB, Qian, J, Cui, HS, and Wu, WY. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients. Arch Psychiatry. (2010) 22:200–3. doi: 10.3969/j.issn.1002-0829.2010.04.002
33. Levis, B, Benedetti, A, and Thombs, BD. Accuracy of patient health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. (2019) 365:l1476. doi: 10.1136/bmj.l1476
34. Kroenke, K, Spitzer, RL, and Williams, JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–3. doi: 10.1046/j.1525-1497.2001.016009606.x
35. Wang, W, Bian, Q, Zhao, Y, Li, X, Wang, W, Du, J, et al. Reliability and validity of the Chinese version of the patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2014) 36:539–4. doi: 10.1016/j.genhosppsych.2014.05.021
36. Cohen, S, Kamarck, T, and Mermelstein, R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–6. doi: 10.2307/2136404
37. Leung, DY, Lam, TH, and Chan, SS. Three versions of perceived stress scale: validation in a sample of Chinese cardiac patients who smoke. BMC Public Health. (2010) 10:513. doi: 10.1186/1471-2458-10-513
38. Chongjun, H, Chunfang, Z, Ting, H, Luping, Y, Qi, W, Bowen, G, et al. Prevalence of overactive bladder and other lower urinary tract symptoms in female nurses in Beijing and its association with occupational stress. Chin J Urol. (2008) 34:565–71. doi: 10.3760/cma.j.issn.1000-6702.2013.08.001
39. Lei, Z, Lan, Z, Tao, X, Jinghe, L, Zhao, L, Gong, J, et al. A population-based epidemiology survey of the lower urinary tract symptoms in adult Chinese women: cross-sectional study. Beijing: Peking Union Medical College Hospital (PUMCH) (2015).
40. Fan, X, Guo, X, Ren, Z, Li, X, He, M, Shi, H, et al. The prevalence of depressive symptoms and associated factors in middle-aged and elderly Chinese people. J Affect Disord. (2021) 293:222–8. doi: 10.1016/j.jad.2021.06.044
41. Stewart, WF, Van Rooyen, JB, Cundiff, GW, Abrams, P, Herzog, AR, Corey, R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. (2003) 20:327–6. doi: 10.1007/s00345-002-0301-4
42. Homma, Y, Yamaguchi, O, and Hayashi, K. An epidemiological survey of overactive bladder symptoms in Japan. BJU Int. (2005) 96:1314–8. doi: 10.1111/j.1464-410X.2005.05835.x
43. Wu, XH, Liu, XX, Xie, KH, Wang, RM, Wu, YX, and Liu, YG. Prevalence and related factors of urinary incontinence among Hebei women of China. Gynecol Obstet Investig. (2011) 71:262–7. doi: 10.1159/000320333
44. Wang, Y, Hu, H, Xu, K, Wang, X, Na, Y, and Kang, X. Prevalence, risk factors and the bother of lower urinary tract symptoms in China: a population-based survey. Int Urogynecol J. (2015) 26:911–9. doi: 10.1007/s00192-015-2626-8
45. Alshehri, SZ, Abumilha, AK, Amer, KA, Aldosari, AA, Shawkhan, RA, Alasmari, KA, et al. Patterns of urinary incontinence among women in Asir region. Saudi Arabia Cureus. (2022) 14:e21628. doi: 10.7759/cureus.21628
46. Zhang, C, Hai, T, Yu, L, Liu, S, Li, Q, Zhang, X, et al. Association between occupational stress and risk of overactive bladder and other lower urinary tract symptoms: a cross-sectional study of female nurses in China. Neurourol Urodyn. (2013) 32:254–15. doi: 10.1002/nau.22290
47. Chang, EM, Hancock, KM, Johnson, A, Daly, J, and Jackson, D. Role stress in nurses: review of related factors and strategies for moving forward. Nurs Health Sci. (2005) 7:57–65. doi: 10.1111/j.1442-2018.2005.00221.x
48. Yoo, H, Kim, JY, Lee, YM, and Kang, MY. Occupational risk factors associated with lower urinary tract symptoms among female workers: a systematic review. Occup Environ Med. (2023) 80:288–6. doi: 10.1136/oemed-2022-108607
49. Joseph, MA, Harlow, SD, Wei, JT, Sarma, AV, Dunn, RL, Taylor, JM, et al. Risk factors for lower urinary tract symptoms in a population-based sample of African-American men. Am J Epidemiol. (2003) 157:906–4. doi: 10.1093/aje/kwg051
50. Hobson, RM, and Maughan, RJ. Hydration status and the diuretic action of a small dose of alcohol. Alcohol Alcohol. (2010) 45:366–3. doi: 10.1093/alcalc/agq029
51. Schatzl, G, Brössner, C, Schmid, S, Kugler, W, Roehrich, M, Treu, T, et al. Endocrine status in elderly men with lower urinary tract symptoms: correlation of age, hormonal status, and lower urinary tract function. Urology. (2000) 55:397–2. doi: 10.1016/S0090-4295(99)00473-2
52. Rortveit, G, Subak, LL, Thom, DH, Creasman, JM, Vittinghoff, E, Van Den Eeden, SK, et al. Urinary incontinence, fecal incontinence and pelvic organ prolapse in a population-based, racially diverse cohort: prevalence and risk factors. Female Pelvic Med Reconstr Surg. (2010) 16:278–3. doi: 10.1097/SPV.0b013e3181ed3e31
53. Swithinbank, L, Hashim, H, and Abrams, P. The effect of fluid intake on urinary symptoms in women. J Urol. (2005) 174:187–9. doi: 10.1097/01.ju.0000162020.10447.31
54. Tomlinson, BU, Dougherty, MC, Pendergast, JF, Boyington, AR, Coffman, MA, and Pickens, SM. Dietary caffeine, fluid intake and urinary incontinence in older rural women. Int Urogynecol J Pelvic Floor Dysfunct. (1999) 10:22–8. doi: 10.1007/PL00004009
55. Wells, MJ, Jamieson, K, Markham, TC, Green, SM, and Fader, MJ. The effect of caffeinated versus decaffeinated drinks on overactive bladder: a double-blind, randomized, crossover study. J Wound Ostomy Continence Nurs. (2014) 41:371–8. doi: 10.1097/WON.0000000000000040
56. Tettamanti, G, Altman, D, Pedersen, NL, Bellocco, R, Milsom, I, and Iliadou, AN. Effects of coffee and tea consumption on urinary incontinence in female twins. BJOG. (2011) 118:806–3. doi: 10.1111/j.1471-0528.2011.02930.x
57. Arya, LA, Myers, DL, and Jackson, ND. Dietary caffeine intake and the risk for detrusor instability: a case-control study. Obstet Gynecol. (2000) 96:85–9. doi: 10.1016/s0029-7844(00)00808-5
58. Hagan, KA, Erekson, E, Austin, A, Minassian, VA, Townsend, MK, Bynum, JPW, et al. A prospective study of the natural history of urinary incontinence in women. Am J Obstet Gynecol. (2018) 218:502.e1–8. doi: 10.1016/j.ajog.2018.01.045
59. De Nunzio, C, Nacchia, A, Cicione, A, Cindolo, L, Gacci, M, Cancrini, F, et al. Physical activity as a protective factor for lower urinary tract symptoms in male patients: a prospective cohort analysis. Urology. (2019) 125:163–8. doi: 10.1016/j.urology.2018.12.035
60. Chaliha, C, Bland, JM, Monga, A, Stanton, SL, and Sultan, AH. Pregnancy and delivery: a urodynamic viewpoint. BJOG. (2000) 107:1354–9. doi: 10.1111/j.1471-0528.2000.tb11647.x
61. Snooks, SJ, Setchell, M, Swash, M, and Henry, MM. Injury to innervation of pelvic floor sphincter musculature in childbirth. Lancet. (1984) 2:546–15. doi: 10.1016/s0140-6736(84)90766-9
62. Zhang, W, Song, Y, He, X, Xu, B, Huang, H, He, C, et al. Prevalence and risk factors of lower urinary tract symptoms in Fuzhou Chinese women. Eur Urol. (2005) 48:309–3. doi: 10.1016/j.eururo.2005.03.003
63. Vakili, M, Amoqadiri, M, Mohammadi, M, and Modaressi, M. Prevalence and factors associated with stress urinary incontinence after childbirth of Yazd in 2015. J Shahid Sadoughi Univ Med Sci. (2016) 24:716–3.
64. Milsom, I, Altman, D, Cartwright, R, Lapitan, MC, Nelson, R, Sillén, U, et al. Epidemiology of urinary incontinence (UI) and other lower urinary tract symptoms (LUTS), pelvic organ prolapse (POP) and anal incontinence (AI) In: P Abrams, L Cardozo, S Khoury, and AJ Wein, editors. Incontinence: 5th International Consultation on Incontinence. Paris: ICUD-EAU (2013)
65. Klausner, AP, and Steers, WD. Corticotropin releasing factor: a mediator of emotional influences on bladder function. J Urol. (2004) 172:2570–3. doi: 10.1097/01.ju.0000144142.26242.f3
66. Gannon, K, Glover, L, O'Neill, M, and Emberton, M. Men and chronic illness: a qualitative study of LUTS. J Health Psychol. (2004) 9:411–15. doi: 10.1177/1359105304042350
67. Pinnock, C, O'Brien, B, and Marshall, VR. Older men's concerns about their urological health: a qualitative study. Aust N Z J Public Health. (1998) 22:368–3. doi: 10.1111/j.1467-842X.1998.tb01393.x
68. Liu, B, Wang, L, Huang, SS, Wu, Q, and Wu, DL. Prevalence and risk factors of urinary incontinence among Chinese women in Shanghai. Int J Clin Exp Med. (2014) 7:686–6.
Keywords: lower urinary tract symptoms, female nurses, risk factors, prevalence, cross-sectional study
Citation: Zhang XY, Li ML, Dong WS, Lv XY, Li L, Yang XR and Cao YJ (2023) Prevalence and influencing factors of lower urinary tract symptoms in female nurses: a cross-sectional study based on TARGET. Front. Public Health. 11:1201184. doi: 10.3389/fpubh.2023.1201184
Edited by:
Jessica García González, University of Almeria, SpainReviewed by:
Raúl Romero Del Rey, University of Almeria, SpainDavid Lozano-Paniagua, University of Almeria, Spain
Copyright © 2023 Zhang, Li, Dong, Lv, Li, Yang and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yingjuan Cao, Y2FveWpAc2R1LmVkdS5jbg==
 Xinyue Zhang
Xinyue Zhang Mengli Li1
Mengli Li1 Xiaoyan Lv
Xiaoyan Lv Li Li
Li Li Xiaorong Yang
Xiaorong Yang Yingjuan Cao
Yingjuan Cao