- 1Department of Science and Education, RuiJin Hospital LuWan Branch, School of Medicine, Shanghai Jiaotong University, Shanghai, China
- 2Department of Psychiatry, Xuhui Mental Health Center, Shanghai, China
- 3Department of Biostatistics, School of Public Health, Fudan University, Shanghai, China
- 4NHC Key Laboratory of Health Technology Assessment, Fudan University, Shanghai, China
- 5Key Laboratory of Public Health Safety of Ministry of Education, Fudan University, Shanghai, China
- 6Nursing Department, RuiJin Hospital LuWan Branch, School of Medicine, Shanghai Jiaotong University, Shanghai, China
- 7Graduate Medical Education Office, Shanghai Pudong New Area Gongli Hospital, Shanghai, China
- 8Teaching Affairs Office, Shanghai Seventh People's Hospital, Shanghai, China
- 9Department of Orthopedic Surgery, Zhongshan Hospital, Fudan University, Shanghai, China
Background: The COVID-19 pandemic may have increased the prevalence of psychiatric disorders, such as anxiety, depressive disorders, and post-traumatic stress disorder (PTSD), among healthcare workers.
Purpose: This study aims to investigate the prevalence of PTSD and its risk factors among residents in the standardized residency training programs (SRTPs) in Shanghai during the COVID-19 outbreak.
Participants and methods: An online cross-sectional survey was conducted between December 17, 2021, and January 7, 2022, among SRPT residents from 15 hospitals in Shanghai, China. Questionnaires comprising general information, medical-related traumatic event experiences, the PTSD Checklist (PCL-5), and the perceived social support scale (PSSS) were distributed to the participants using the online Questionnaire Star electronic system.
Results: We included 835 valid responses for the analysis. In total, 654 residents (78.3%) had experienced at least one traumatic event, and 278 residents (33.3%) were found to have PTSD symptoms. The age 26–30 years old, female sex, and increased resident working hours were identified as the risk factors for PTSD (p < 0.05), and perceived social support had a significant negative association with PTSD (p < 0.05).
Conclusion: During the COVID-19 pandemic, there was a high prevalence of PTSD among SRTPs residents in Shanghai. The age 26–30 years old, female sex, and increased resident working hours were identified as risk factors for PTSD, while perceived social support was identified as a protective factor against PTSD. The present findings can be applied in STRPs management and provide useful information for designing special interventions and protocols for SRTPs residents.
1. Introduction
On 11 March 2020, the World Health Organization (WHO) reported severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) as the causative agent of coronavirus disease-2019 (COVID-19) and declared the pandemic status of COVID-19 (1). The pandemic prompted an assertive public health response worldwide, including social isolation as well as the closure of schools, businesses, and other establishments, all of which contributed to a rise in various mental health problems among citizens (2). Healthcare workers (HCWs) working at the frontline of this pandemic experienced high stress levels and were particularly at risk for persistent mental health problems, such as depression, chronic psychological stress, anxiety, insomnia, and posttraumatic stress disorder (PTSD) (2). Importantly, these mental health problems, in turn, could result in hazards exceeding the consequences of the COVID-19 pandemic itself (3).
PTSD is a significant economic burden while a highly prevalent condition. The prevalence of probable PTSD in HCWs is about three times than observed in the general population. This pattern is due to the long-term work-related stressors HCWs must endure (4). Studies have suggested a high risk for PTSD development among HCWs who have been involved in the three major recent coronavirus disease-related outbreaks: severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), and COVID-19 (5). More specifically, it has consistently been shown that a high proportion of HCWs is at a high risk of developing PTSD due to the COVID-19 pandemic (6, 7), and the individual-level risk factors for this phenomenon include pre-existing mental-health concerns (8), being in the nursing profession (9), being female (10), and young age (11).
In China, standardized residency training programs (SRTPs) were first implemented in Shanghai in 2010 to set quality standards for residency training (12). Since then, all hospitals in Shanghai have hired physicians only with certifications from SRTPs. SRTPs are considered an important resource for continuing education and receiving system-based clinical training (13). In general, the importance of SRTPs has been demonstrated because they provide residents with more standardized training and ensure that the residents are highly qualified. However, the transition to a SRTP leads to challenges, such as the uncertainty of employment and less personal attachment to the workplace for SRTP residents. Moreover, entering an SRTP adds 3 years of highly stressful training and relatively low-paid work for young physicians (14). Given the work-related stressors, pressures elicited by patients, and challenging daily work routines, SRTP residents may be at an increased risk of psychopathological stress-related disorders. Zhang and colleagues reported that the prevalence of depression disorder was 28.3% among SRTP residents (15). Thus, it would not be surprising if the prevalence of PTSD among SRTP residents was much higher than that in the general population.
Studies have found that young age, low work experience, heavy workload, working in unsafe settings, as well as a lack of training and social support are predictors of stress-related symptoms (16). SRTP residents are more likely than other HCWs to experience traumatic events and develop PTSD due to their high-pressure roles, and this is especially pertinent in relation to the COVID-19 pandemic. Therefore, given that SRTP residents are one of the populations most vulnerable to PTSD among HCWs, we investigated the prevalence of PTSD and its risk factors among SRTP residents during the COVID-19 outbreak from 2019 to 2021.
2. Materials and methods
2.1. Study design and participants
The Department of Ethics Commission of Ruijin Hospital/Lu Wan Branch within the School of Medicine of Shanghai Jiaotong University (Shanghai, China) provided ethical approval (LWEC2020031) for our study protocol.
Online informed consent for participation was obtained upon completion of the questionnaire. Fifteen hospitals providing SRTPs in Shanghai were selected as research units using a multistage method based on stratified random-cluster sampling. The online Questionnaire Star electronic system (www.wjx.cn/) was used, and questionnaires were distributed to participants as a link via the WeChat (www.wechat.com/), with the help of the education departments of selected hospitals. The inclusion criterion for participants was residents enrolled in an SRTP from 2019 to 2021.
2.2. Screening questionnaire
The screening questionnaire was written in Chinese and comprised four main components: general information, medical-related traumatic experiences, PTSD Checklist for the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5, PCL-5), and the perceived social support scale (PSSS).
2.2.1. General information
The general data of participants collected were hospital level, sex, age, education, medical specialty, training grade, marital status, average number of hours worked per week, and salary.
2.2.2. Medical-related traumatic events
The checklist for medical-related traumatic events in the questionnaire comprised nine common traumatic events: “criticism/bullying by senior doctors,” “criticism/bullying by other SRTP residents,” “failing an important examination,” “iatrogenic exposure/infection,” “conflict with patients/family members, being threatened or attacked,” “medical negligence and malpractice,” “patients died/deteriorated,” “medical isolation/separation,” and “yourself or hospital colleague fell seriously ill.” If participants had experienced traumatic events that were not included in this checklist, they could describe it as “other.” Furthermore, those who reported at least one traumatic experience were required to select the most affecting traumatic event and continue to PCL-5 and the PSSS. If they had not suffered a traumatic experience, the survey was terminated, and participants were excluded from the diagnosis of PTSD.
2.2.3. PCL-5
PCL-5 is a self-reported screening measurement with 20 items to assess PTSD symptoms. The responses on PCL-5 are given using a Likert scale, and the severity of each symptom is divided into five levels: 0 = “not at all”; 1 = “a little bit”; 2 = “moderately,” 3 = “quite a bit”; 3 = “extremely.” The maximum score is 80. We used a cutoff score of 33 points (7) to determine a diagnosis of PTSD, and this scale had satisfactory reliability and validity (Cronbach’s α = 0.94).
2.2.4. PSSS
The PSSS consists of 12 items, with four items measuring “family support,” four items measuring “friend support,” and four items measuring “significant other support.” The responses for each item are ranked on a seven-point Likert scale (1 = “strongly disagree”; 7 = “strongly agree”). The total score of perceived social support is the sum of all items, with a high score indicating a high level of perceived support.
In the present study, social support was categorized into three levels according to the total score: “low” (PSSS score < 37), “moderate” (37 ≤ PSSS score ≤ 60), and “high” (PSSS score > 60) (17). The Chinese version of the PSSS was found to have adequate internal consistency (Cronbach’s α = 0.94) among undergraduate students during the early phases of the COVID-19 pandemic (18). In the present study, Cronbach’s alpha of the total scale was 0.93.
2.3. Data collection
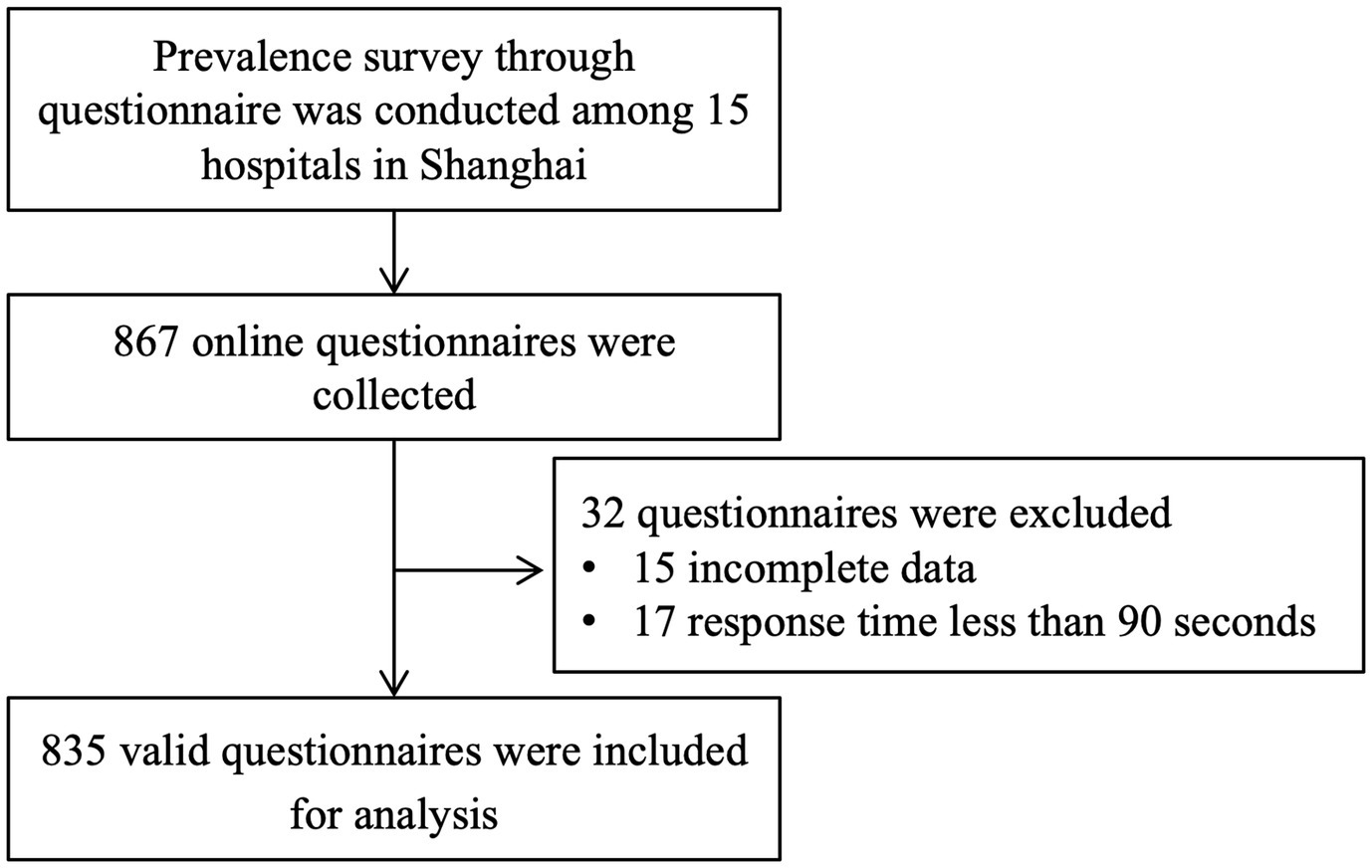
A total of 867 online questionnaires from 15 hospitals were collected, and 32 questionnaires were excluded because of incomplete data (15 questionnaires) or response times of less than 90 s (17 questionnaires). Finally, 835 valid responses were included valid for analysis, the response rate was 96.3%, as shown in Figure 1.
2.4. Data analysis
Statistical analyses were undertaken using SPSS 25.0 (IBM, Armonk, NY, United States). Categorical variables are expressed as absolute values (percentages). The internal consistency of the total scores of PCL-5 and the PSSS was evaluated using Cronbach’s alpha. Analyses of descriptive statistics were conducted to examine the demographic and other selected characteristics of participants. Pearson’s chi-square test or Fisher’s exact test were used to compare differences among subgroups. Multivariate logistic regression was employed to assess the risk factors for PTSD variables that were significant in the univariate analysis at p ≤ 0.10. p < 0.05 was considered significant unless stated otherwise.
3. Results
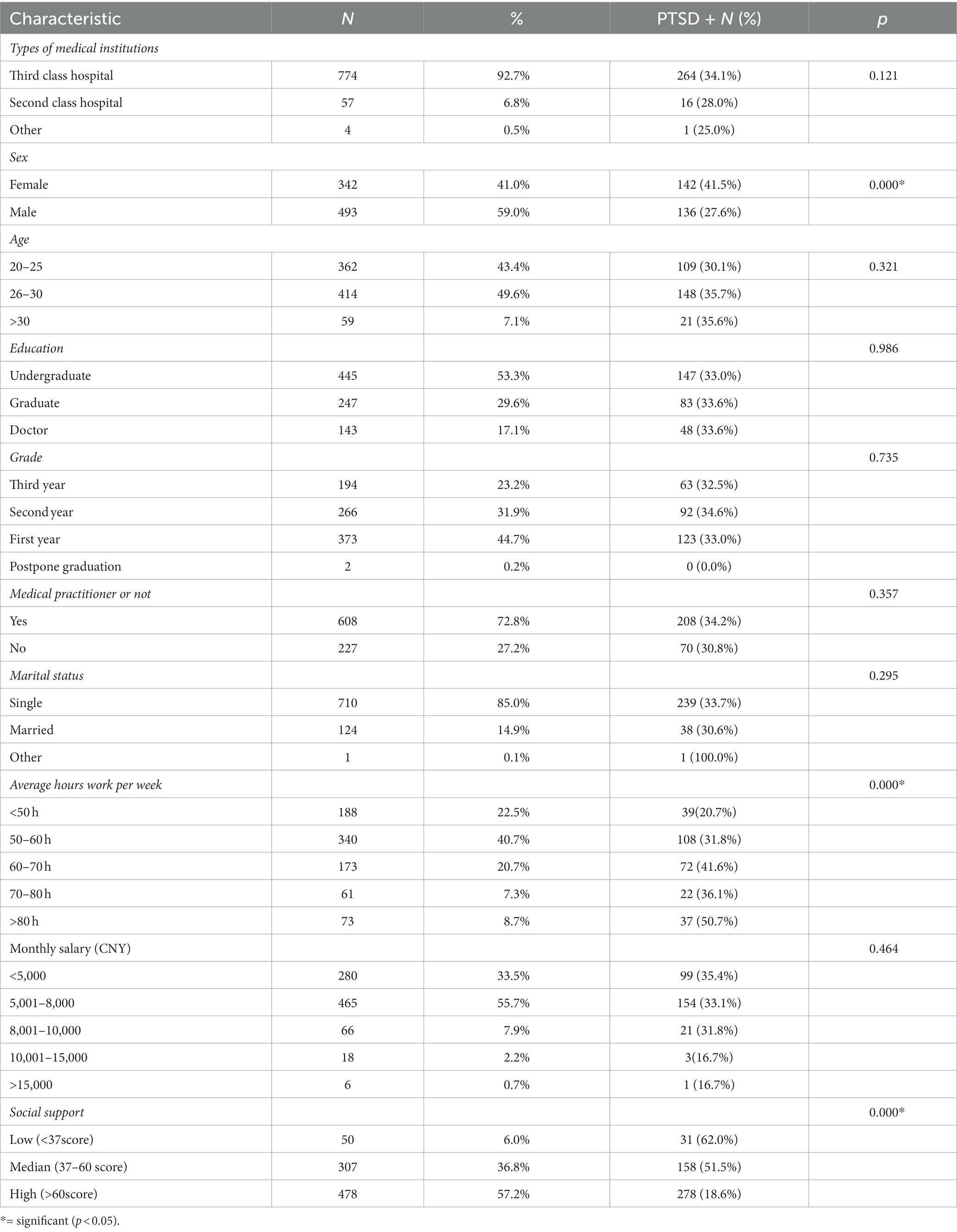
Table 1 summarizes the sociodemographic characteristics and PTSD prevalence of respondents. Most (92.7%) respondents were from a third-class hospital. Most respondents were male (n = 493, 59.0%). The prevalence of PTSD was higher in women (41.5%) than in men (27.6%). Respondents were between 20 and 30 years of age (n = 776). Respondents were mainly undergraduates (n = 445, 53.3%). Specifically, 194 respondents were in their third year, 266 were in their second year, and the largest number of respondents were in their first year (n = 373, 44.7%) of training. Most respondents: were medical practitioners (n = 608, 72.8%); were unmarried (n = 710, 85.0%); worked 50–60 h per week (n = 340, 40.7%); had a monthly salary of 5,001–8,000 yuan (n = 465, 55.7%).
Overall, 50 residents (6%) had a low level of social support (PSSS score < 37), 307 residents (36.8%) had a moderate level of social support (PSSS score ≥ 37 and ≤ 60), and 478 residents (57.2%) had a high level of social support (PSSS score > 60). Social support was negatively associated with PTSD. The prevalence of PTSD in respondents with a high level of social support (n = 278, 18.6%) was lower than that for respondents with a low level of social support (n = 31, 62%) or moderate level of social support (n = 158, 51.5%; p < 0.05) (Table 1).
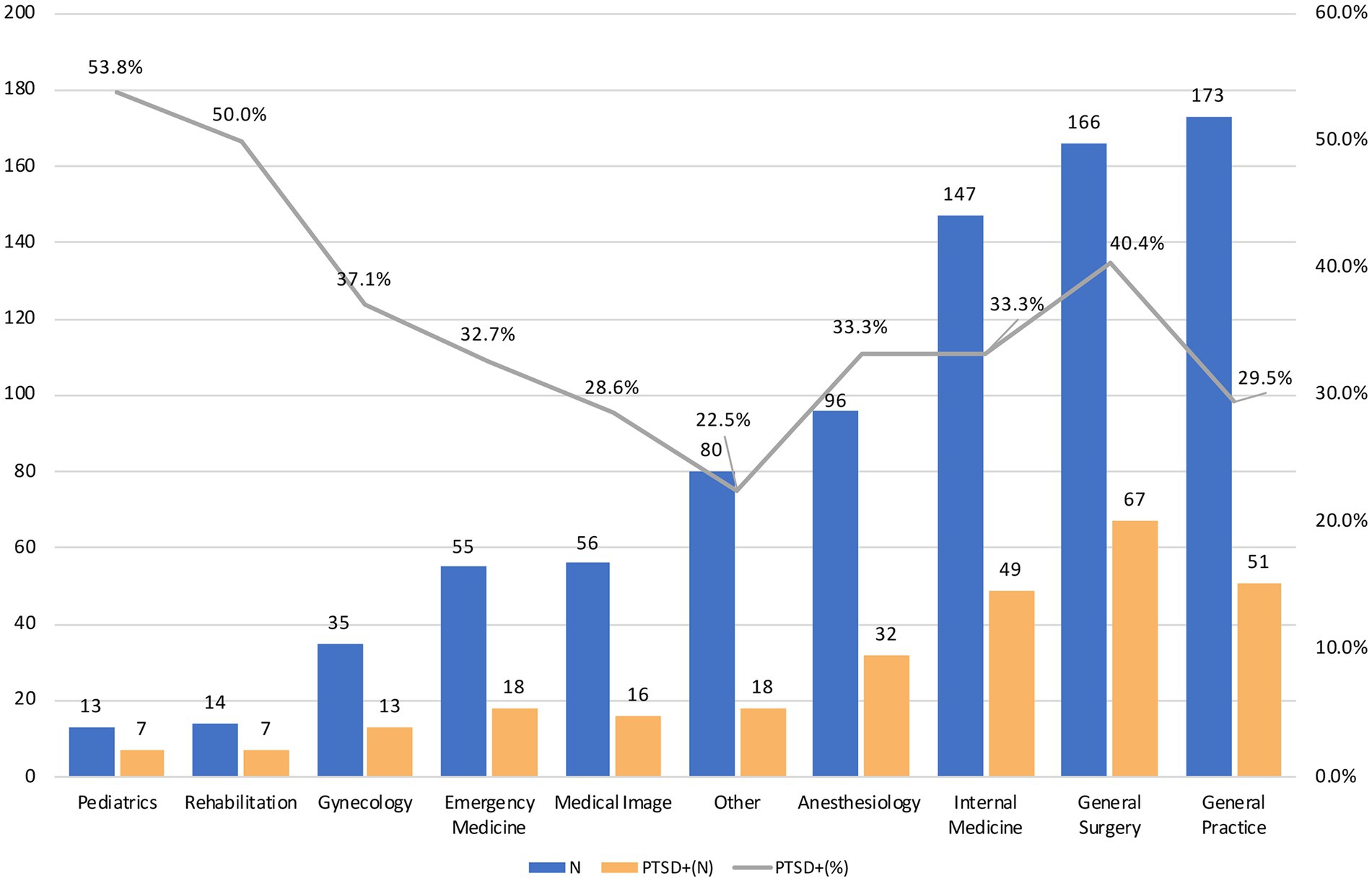
Figure 2 shows the prevalence of PTSD among different specialties. The specialties represented in the cohort were internal medicine (n = 147, 17.6%), surgery (n = 166, 19.9%), gynecology (n = 35, 4.2%), pediatrics (n = 13, 1.6%), general practice (n = 173, 20.7%), emergency medicine (n = 55, 6.6%), anesthesiology (n = 96, 11.5%), medical imaging (n = 56, 6.7%), rehabilitation (n = 14, 1.7%), and other (n = 80, 9.6%). The specialties with the lowest prevalence of PTSD were general practice (20.7%), surgery (19.91%), and internal medicine (17.6%). Except for the specialties of pediatrics and rehabilitation, which had a small number of respondents, the medical specialties with the highest proportion of individuals screening positive for PTSD were surgery (40.4%), gynecology (37.1%), internal medicine (33.3%), and anesthesiology (33.3%). Overall, 33.3% of the sample (n = 278) screened positive for PTSD.
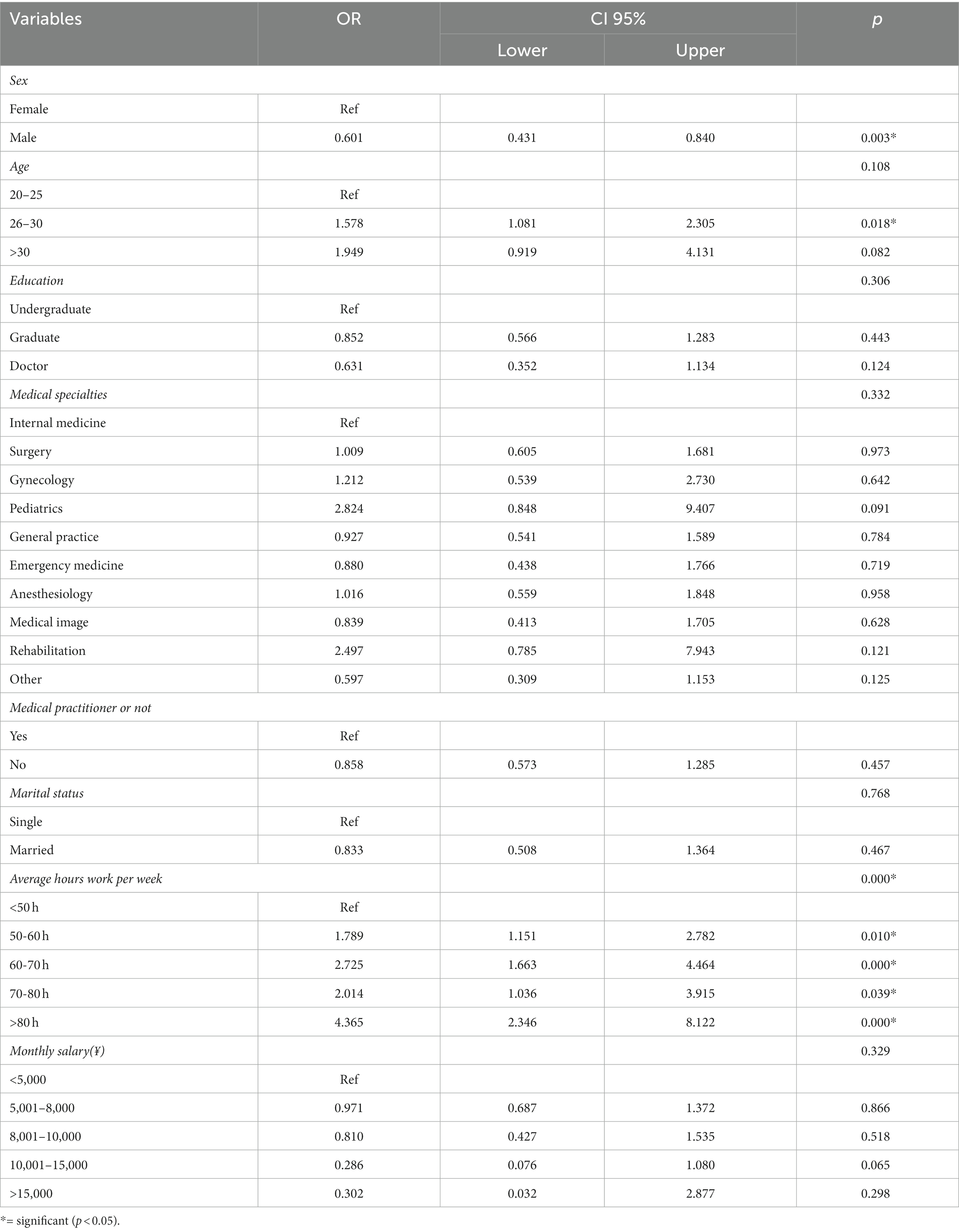
Table 2 shows the multivariate analysis of potential modifiable and nonmodifiable risk factors for PTSD among all specialties. Of the surveyed demographic and occupational characteristics, being female (odds ratio (OR) = 0.601, p = 0.003), being aged 26–30 years (OR = 1.578, p = 0.018), and working an average of 50–60 h per week (OR = 1.789, p = 0.010), 60–70 h per week (OR = 2.725, p < 0.001), 70–80 h per week (OR = 2.014, p = 0.039), and > 80 h per week (OR = 4.365, p < 0.001) were significantly associated with a greater probability of having PTSD symptoms. There were no significant differences (p > 0.05) in the prevalence of PTSD among residents based on their education, medical specialty, marriage status, or monthly salary.
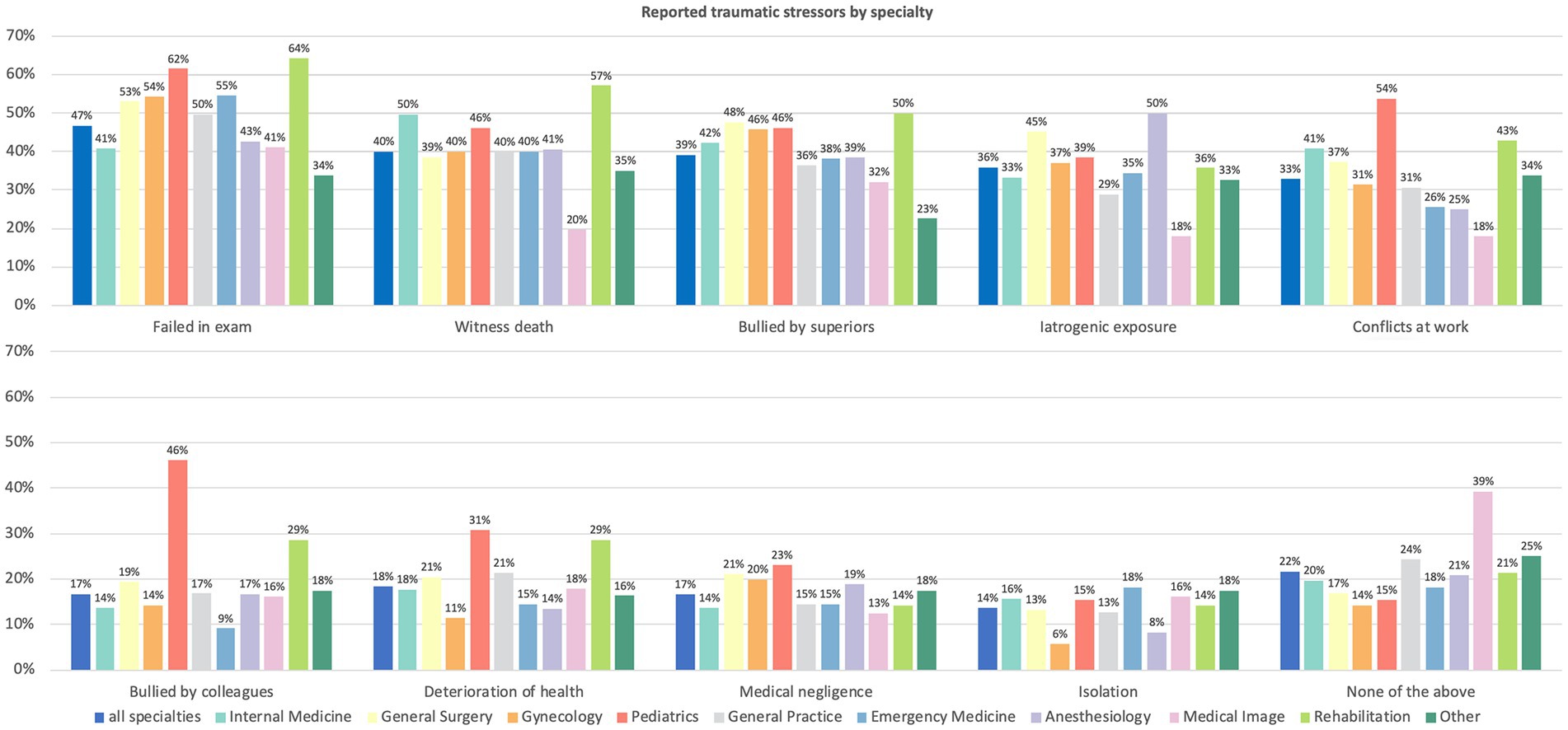
Overall, 654 (78%) residents reported experiencing at least one traumatic event. The most common traumatic stressors were “failing an examination” (47%), “witnessing death” (40%), and “bullying by superiors” (39%) (Figure 3). Traumatic stressors among specialties were compared and, in general, there were similar trends among them. In addition, traumatic stressors were related to the work content and context of the specialism. For example, the number of events of “witnessing death,” “conflicts at work,” and “iatrogenic exposure” in the specialty of medical imaging was lower than that for other specialties.
Multivariate analysis with adjustment for potential confounders showed that the medical profession-related traumatic events of “criticism/bullying by senior doctors” (OR = 2.269,p < 0.001), “criticism/bullying by other SRTP residents (disharmonious relationship)” (OR = 2.366,p < 0.001), “failing an important examination” (OR = 2.666, p < 0.001), and “medical isolation/separation” (OR = 2.105, p = 0.003) were risk factors for PTSD (Table 3).
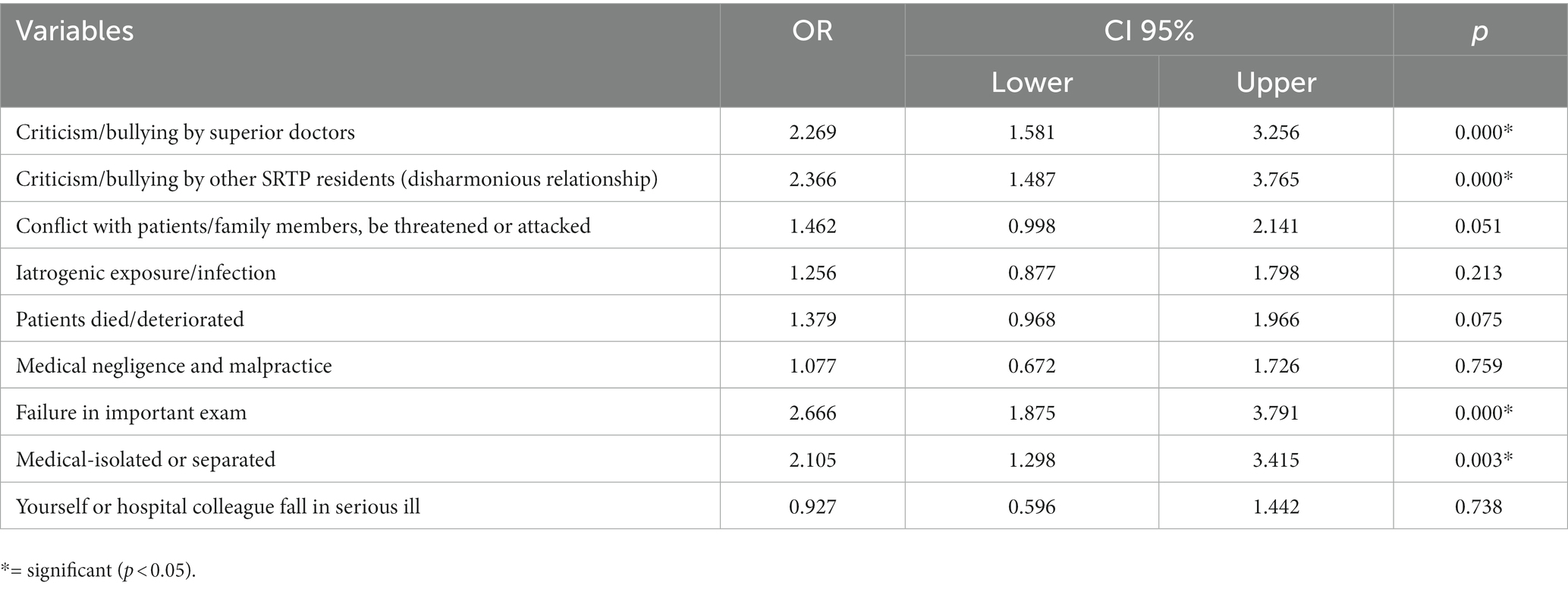
Table 3. The multivariate analysis of PTSD screening positive respondents and medical-relevant traumatic events experiences.
4. Discussion
A number of studies have confirmed the negative psychological impact of experiencing a disaster, suggesting that the subsequent risk of suffering from PTSD is substantial (19). The continuous tussle with unfavorable conditions related to the COVID-19 pandemic has increased the risk of HCWs suffering from PTSD and its symptoms. To clarify the characteristics of medical-related PTSD among SRTP residents in Shanghai during the COVID-19 pandemic, we conducted a cross-sectional survey and included 835 valid responses for analyses. We found that 654 residents (78.3%) had experienced at least one traumatic event, and that 278 residents (33.3%) had PTSD symptoms. Being 26–30 years of age, female, and having long working hours were identified as risk factors for PTSD, and perceived social support had a significant negative association with PTSD.
Overall, 33.3% of SRTP residents were found to have PTSD symptoms. This prevalence is significantly higher compared with that in research on PTSD among HCWs in the three previous outbreaks of coronavirus-related diseases (5). For example, Lin et al. (20) reported a PTSD prevalence of 21.7% among emergency-department staff after SARS 2003, whereas Zhang et al. (21) reported a PTSD prevalence of 12.4% among HCWs in high-risk areas during the COVID-19 pandemic. Studies have reported an increased risk of psychiatric disease and stress-related disorders among HCWs during the COVID-19 pandemic, as well as a high prevalence of PTSD symptomatology (22–24). Kheirallah et al. (25) reported a significant proportion of medical students from Jordan self-reporting an increased level of anxiety (49.2%) and depression (23.1%). Exposure to medical-related stressful events outside the range of normal human experience is part of the job for all HCWs, and the increased prevalence of PTSD in this group is not a new concept (especially during severe pandemics). However, what is an acceptable prevalence of PTSD for SRTP residents?
Among the demographic characteristics of SRTP residents, age, sex, and long working hours were associated with PTSD prevalence. Studies have demonstrated a higher level of work-related stress and “burnout” among female physicians compared with that experienced by male physicians (26, 27). In addition, the high prevalence of PTSD among HCWs is due to long working hours and work-related stress. We found the long working hours of residents to be associated with PTSD prevalence. Therefore, interventions to reduce working hours and, thus, improve physician wellbeing, are needed urgently.
Social support has been proposed to be the most efficacious way to alleviate the physical and emotional impacts of stressors (28). Social support has a critical role in the emotional, cognitive, and behavioral aspects of PTSD (29). Zalta and colleagues identified a lack of social support after trauma as a risk factor for PTSD, with a perceived lack of social support leading to a higher level of PTSD symptoms (30). A significant negative correlation between PTSD prevalence and perceived social support was demonstrated in the present study. Advice from friends, family, and significant others may enable subsequent behavioral changes that make everyday tasks more efficient or positive. Therefore, understanding, respecting, supporting, and empathizing with SRTP residents is fundamental in promoting their mental health in their medical careers.
Failing an examination, witnessing death, and bullying by superiors were the most commonly reported traumatic stressors among all SRTP residents. In general, there were similar trends of reported traumatic stressors between SRTP specialties. In addition, traumatic stressors were related to the work content and context of the specialism. For example, the prevalence of “witnessing death,” “conflicts at work,” and “iatrogenic exposure” in the specialty of medical imaging was lower than that in the other medical specialties. More than 45% of SRTP residents specializing in pediatrics answered “yes” to experiencing five traumatic stressors, indicating the high pressure and workload of pediatric medicine in China (31).It is not surprising that “failing an examination” was listed as the most common stressor among all SRTP residents. To ensure training quality, residents must complete the entire SRTP course and pass all examinations before they can apply for the exit examination (13). The latter is critically important, and those who do not pass it cannot graduate from the STRP and practice medicine in Shanghai. In addition, they receive only one more opportunity to take the examination after ≥6 months of training.
Isolation is an effective form of public-health management to prevent the spread of infectious diseases. However, isolation is associated with negative psychosocial effects, including depression, anxiety, anger, and PTSD. Samrah et al. (32) reported on isolated patients suffering from COVID-19 in Jordan; 44% reported symptoms of depression, and 21% were at high risk of major depressive disorder. HCWs (especially SRTP residents) may also develop PTSD as a result of isolation.
The present study had two main limitations. First, we focused on the occurrence of and risk factors for PTSD among STRP residents instead of clinical diagnoses and therapy. Therefore, the self-reported screening measures of PTSD and social support were applied in our study, but clinician-administered measures may have led to different results. Second, our cross-sectional research showed a strong bidirectional relationship between PTSD and social support, but we could not determine the direction of causality between social support and PTSD symptoms. Further research may be needed to ascertain if our findings can be replicated using longitudinal data.
5. Conclusion
The present findings demonstrate that there was a high prevalence of PTSD among SRTPs residents in Shanghai during the COVID-19 pandemic. The age 26–30 years old, female sex, and increased resident working hours were identified as risk factors for PTSD, while perceived social support was identified as a protective factor against PTSD. The present findings can be applied in SRTPs management for designing special interventions and protocols to protect the mental health of SRTPs residents.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: the datasets presented in this article are not readily available because the data includes sensitive and private information. According to the ethical approval we cannot share it with the third party.
Ethics statement
The studies involving humans were approved by the Department of Ethics Commission of Ruijin Hospital/Lu Wan Branch, School of Medicine, Shanghai Jiaotong University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
RH participated in conception, design of the work, data interpretation and analysis, drafting, and revision of the manuscript. CT, TL, LW, and CL participated in the acquisition and interpretation of data. JL and LC participated in the data analysis and revision of the draft. LC and SW made contributions to the concept and design of the study, acquisition of data, manuscript revision, and supervision. All authors approved the publication of this final version.
Funding
This study was supported by grants from the Science and Technology Commission of Huangpu District, Shanghai (HLY202101); Young Physician Training Project of Huangpu District Health Commission, Shanghai (2021QN02); “Science and Technology Innovation Action Program” Natural Science Foundation of Shanghai supported by Shanghai Science and Technology Commission (21ZR1412100 and 23ZR1480300).
Acknowledgments
The authors would like to thank all participants and cooperating authors in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kang, L, Li, Y, Hu, S, Chen, M, Yang, C, Yang, BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. (2020) 7:e14. doi: 10.1016/S2215-0366(20)30047-X
2. Shultz, JM, Baingana, F, and Neria, Y. The 2014 ebola outbreak and mental health: current status and recommended response. JAMA. (2015) 313:567–8. doi: 10.1001/jama.2014.17934
3. Bao, Y, Sun, Y, Meng, S, Shi, J, and Lu, L. 2019-ncov epidemic: address mental health care to empower society. Lancet. (2020) 395:e37–8. doi: 10.1016/S0140-6736(20)30309-3
4. Jackson, TN, Morgan, JP, Jackson, DL, Cook, TR, McLean, K, Agrawal, V, et al. The crossroads of posttraumatic stress disorder and physician burnout: a national review of United States trauma and nontrauma surgeons. Am Surg. (2019) 85:127–5. doi: 10.1177/000313481908500217
5. Carmassi, C, Foghi, C, Dell'Oste, V, Cordone, A, Bertelloni, CA, Bui, E, et al. Ptsd symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the covid-19 pandemic. Psychiatry Res. (2020) 292:113312. doi: 10.1016/j.psychres.2020.113312
6. Liu, P, Wang, L, Cao, C, Wang, R, Zhang, J, Zhang, B, et al. The underlying dimensions of dsm-5 posttraumatic stress disorder symptoms in an epidemiological sample of Chinese earthquake survivors. J Anxiety Disord. (2014) 28:345–1. doi: 10.1016/j.janxdis.2014.03.008
7. Krüger-Gottschalk, A, Knaevelsrud, C, Rau, H, Dyer, A, Schäfer, I, Schellong, J, et al. The German version of the posttraumatic stress disorder checklist for dsm-5 (pcl-5): psychometric properties and diagnostic utility. BMC Psychiatry. (2017) 17:379. doi: 10.1186/s12888-017-1541-6
8. Chatterjee, SS, Barikar, CM, and Mukherjee, A. Impact of covid-19 pandemic on pre-existing mental health problems. Asian J Psychiatry. (2020) 51:102071. doi: 10.1016/j.ajp.2020.102071
9. Lai, J, Ma, S, Wang, Y, Cai, Z, Hu, J, Wei, N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
10. Zhu, Z, Xu, S, Wang, H, Liu, Z, Wu, J, Li, G, et al. Covid-19 in Wuhan: sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. Eclin Med. (2020) 24:100443. doi: 10.1016/j.eclinm.2020.100443
11. Vizheh, M, Qorbani, M, Arzaghi, SM, Muhidin, S, Javanmard, Z, and Esmaeili, M. The mental health of healthcare workers in the covid-19 pandemic: a systematic review. J Diabetes Metab Disord. (2020) 19:1967–78. doi: 10.1007/s40200-020-00643-9
12. Yang-Huang, J, Qian, W, Zhang, K, Shi, L, and Huang, J. The influence of standardized residency training on trainees’ willingness to become a doctor: a comparison between traditional chinese medicine and western medicine. Int J Environ Res Public Health. (2019) 16:3017. doi: 10.3390/ijerph16173017
13. He, Y, Qian, W, Shi, L, Zhang, K, and Huang, J. Standardized residency training: an equalizer for residents at different hospitals in shanghai, China? Int J Health Plan Manag. (2020) 35:592–5. doi: 10.1002/hpm.2970
14. Zhu, J, Li, W, and Chen, L. Doctors in China: improving quality through modernisation of residency education. Lancet. (2016) 388:1922–9. doi: 10.1016/S0140-6736(16)00582-1
15. Zhang, Y, Chu, X, Sha, Y, Zeng, X, and Shen, T. Survey of job burnout and depression in standardized residency training programs in China. Medicine (Baltimore). (2019) 98:e16890. doi: 10.1097/MD.0000000000016890
16. Dettorre, G, Ceccarelli, G, Santinelli, L, Vassalini, P, Innocenti, GP, Alessandri, F, et al. Post-traumatic stress symptoms in healthcare workers dealing with the covid-19 pandemic: a systematic review. Int J Environ Res Public Health. (2021) 18:601. doi: 10.3390/ijerph18020601
17. Gao, L, Qu, J, and Wang, AY. Anxiety, depression and social support in pregnant women with a history of recurrent miscarriage: a cross-sectional study. J Reprod Infant Psychol. (2020) 38:497–8. doi: 10.1080/02646838.2019.1652730
18. Huang, Y, Su, X, Si, M, Xiao, W, Wang, H, Wang, W, et al. The impacts of coping style and perceived social support on the mental health of undergraduate students during the early phases of the covid-19 pandemic in China: a multicenter survey. BMC Psychiatry. (2021) 21:530. doi: 10.1186/s12888-021-03546-y
19. Neria, Y, Nandi, A, and Galea, S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. (2008) 38:467–09. doi: 10.1017/S0033291707001353
20. Lin, C, Peng, Y, Wu, Y, Chang, J, Chan, C, and Yang, D. The psychological effect of severe acute respiratory syndrome on emergency department staff. Emerg Med J. (2007) 24:12–7. doi: 10.1136/emj.2006.035089
21. Zhang, R, Hou, T, Kong, X, Wang, G, Wang, H, Xu, S, et al. Ptsd among healthcare workers during the covid-19 outbreak: a study raises concern for non-medical staff in low-risk areas. Front Psych. (2021) 12:12. doi: 10.3389/fpsyt.2021.696200
22. Sarapultseva, M, Zolotareva, A, Kritsky, I, Nasretdinova, NY, and Sarapultsev, A. Psychological distress and post-traumatic symptomatology among dental healthcare workers in Russia: results of a pilot study. Int J Environ Res Public Health. (2021) 18:708. doi: 10.3390/ijerph18020708
23. Forte, G, Favieri, F, Tambelli, R, and Casagrande, M. Covid-19 pandemic in the Italian population: validation of a post-traumatic stress disorder questionnaire and prevalence of ptsd symptomatology. Int J Environ Res Public Health. (2020) 17:4151. doi: 10.3390/ijerph17114151
24. Chew, NWS, Lee, GKH, Tan, BYQ, Jing, M, Goh, Y, Ngiam, NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during covid-19 outbreak. Brain Behav Immun. (2020) 88:559–5. doi: 10.1016/j.bbi.2020.04.049
25. Kheirallah, K, Bloukh, S, Khasawneh, W, Alsulaiman, J, Khassawneh, A, Al-Mistarehi, AH, et al. Medical students' relative immunity, or lack thereof, against covid-19 emotional distress and psychological challenges; a descriptive study from Jordan. F1000Res. (2021) 10:297. doi: 10.12688/f1000research.52051.2
26. Dyrbye, LN, Shanafelt, TD, Balch, CM, Satele, D, Sloan, J, and Freischlag, J. Relationship between work-home conflicts and burnout among American surgeons: a comparison by sex. Arch Surg. (2011) 146:211–7. doi: 10.1001/archsurg.2010.310
27. Spiliopoulos, K, Gansera, L, Weiland, HC, Schuster, T, Eichinger, W, and Gansera, B. Chronic stress and coping among cardiac surgeons: a single center study. Rev Bras Cir Cardiovasc. (2014) 29:308–5. doi: 10.5935/1678-9741.20140083
28. Thoits, PA . Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. (2011) 52:145–1. doi: 10.1177/0022146510395592
29. Guay, S, Billette, V, and Marchand, A. Exploring the links between posttraumatic stress disorder and social support: processes and potential research avenues. J Trauma Stress. (2006) 19:327–8. doi: 10.1002/jts.20124
30. Zalta, AK, Tirone, V, Orlowska, D, Blais, RK, Lofgreen, A, Klassen, B, et al. Examining moderators of the relationship between social support and self-reported ptsd symptoms: a meta-analysis. Psychol Bull. (2021) 147:33–54. doi: 10.1037/bul0000316
31. Zhang, Y, Huang, L, Zhou, X, Zhang, X, Ke, Z, Wang, Z, et al. Characteristics and workload of pediatricians in China. Pediatrics. (2019) 144:1. doi: 10.1542/peds.2018-3532
Keywords: post-traumatic stress disorder, COVID-19, residents, standardized residency training program, perceived social support
Citation: Huang R, Tang C, Luo J, Li T, Wang L, Li C, Cao L and Wu S (2023) Prevalence of post-traumatic stress disorder among residents of Shanghai standardized training programs during the COVID-19 outbreak: a cross-sectional study. Front. Public Health. 11:1203333. doi: 10.3389/fpubh.2023.1203333
Edited by:
Juan Jesús García-Iglesias, University of Huelva, SpainReviewed by:
Abdel-Hameed Al-Mistarehi, Johns Hopkins Medicine, United StatesShen Liu, Anhui Agricultural University, China
Richa Tripathi, All India Institute of Medical Sciences Gorakhpur, India
Copyright © 2023 Huang, Tang, Luo, Li, Wang, Li, Cao and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lu Cao, Y2FvLmx1QHpzLWhvc3BpdGFsLnNoLmNu; Shiyu Wu, d3VzaGl5dTMxN0AxNjMuY29t
 Ruiwen Huang
Ruiwen Huang Chao Tang2
Chao Tang2 Jianfeng Luo
Jianfeng Luo Lu Cao
Lu Cao