- 1Department of Sociology, School of Law, Jiangnan University, Wuxi, China
- 2Department of Medical Psychology, The Sixth Medical Center of PLA General Hospital, Beijing, China
- 3Department of Military and Political Training, Army Academy of Armed Forces, Beng Bu, China
- 4Department of Medical Psychology, Air Force Medical University, Xi’an, China
Military personnel encountered multiple stressful events during the COVID-19 lockdown. Reducing non-combat attrition due to mental disorders is crucial for military morale and combat effectiveness. Grounded in stress theory and regulatory focus theory, this study investigates the influence of resilience on military personnel’s mental health; coping style and regulatory focus are considered potential mediators and moderators, respectively. We conducted a routine psychological assessment on 1,110 military personnel in China. The results indicate that: (1) resilience has a negative impact on the psychological symptoms of military groups; (2) mature and mixed coping styles in military personnel mediate the association between resilience and psychological symptoms; and (3) regulatory focus predominance has a negative moderating effect on mature coping styles’ effects on psychological symptoms. Furthermore, this study supports previous findings that resilience and mental health are interrelated; it demonstrates that military personnel can effectively reduce negative psychological symptoms by improving their resilience level and adopting mature coping styles under stressful situations. The current study presents interventional insights regarding coping styles and mental health from a self-regulatory perspective during the COVID-19 pandemic.
1. Introduction
The COVID-19 pandemic has brought about significant economic and health-related challenges, not just in terms of physical health, but also mental health and well-being (1). Several cross-sectional studies have revealed a correlation between the COVID-19 pandemic and higher-than-expected levels of mental distress in some populations, with depression, anxiety, and PTSD being the most frequently reported conditions (2).
During the COVID-19 pandemic, individuals in the military faced more sources of pressure than civilians. In addition to undertaking intensive training, living by strict military standards, and having little free time (3), military personnel may have also faced pressure related to family members falling ill, declining income, and social distancing requirements (4, 5). Due to their occupational characteristics, such as combat exposure and deployment tasks, military personnel already face a relatively high risk of developing mental illness (6). Thus, to reduce non-combat attrition, it is necessary to consider measures to prevent psychological symptoms from becoming psychological disorders (2). In light of the COVID-19 pandemic, scholars are increasingly focusing on the prevention of mental health issues, shifting their focus to the cultivation of psychological resources such as resilience and social support (4, 7). Prior research has shown that resilience and individual coping styles can effectively alleviate adverse psychological symptoms caused by stressors.
We aimed to shed light on the influence of resilience on the mental health of military personnel, taking coping style and regulatory focus as the intermediary and moderating variables, respectively. We further aimed to explore the mechanism by which military personnel reinforce their internal stress resources, providing evidence and support for psychological health interventions during the pandemic.
1.1. The effect of resilience on mental health
The concept of resilience was developed from research on crisis response and stress coping (8). It refers to an individual’s internal resources that enable their successful adaptation when facing adversity, trauma, threats, or other major life pressures (9). Military personnel often face higher mental health risks than do civilians owing to their occupational characteristics of chronic exposure to high-pressure environments (6). In the existing literature, topics related to the mental health of military personnel are often based on clinical outcomes, such as a high incidence of psychiatric problems (e.g., anxiety, depression, and posttraumatic stress disorder) and increased rates of suicide (10–12). Due to the significant increase in military personnel experiencing mental health problems, it is critical to develop strategies to prevent psychological symptoms from developing into more serious psychiatric problems (13).
Extensive research has confirmed that resilience reduces the likelihood of mental health issues (12, 14–17). Psychological resilience is seen as a positive psychological quality that can counteract the adverse effects of stressors, allowing individuals to experience fewer negative emotions, cope better in the face of unexpected events, and have a greater sense of subjective well-being (9, 18). In a study of frontline healthcare workers during the COVID-19 pandemic, resilience was found to be protective against psychological problems such as anxiety, depression, and burnout (19–21). In studies of military populations, resilience has also been found to promote better adjustment to deployment, as well as to reduce the risk of depression, anxiety, substance abuse, and suicide among soldiers (14, 22). Resiliency training improves soldiers’ rational understanding and ability to use more aggressive coping strategies in the face of stressors (23, 24). In studies of veterans, PTSD severity was lower in individuals with high (versus low) resilience; moreover, resilience factors influenced adaptive and coping behaviors and moderated the relationship between adverse experiences and psychiatric disorders (25–27). Thus, there is good reason to believe that resilience positively predicts mental health. In light of this, we formulated the following hypothesis:
Hypothesis 1: Psychological resilience positively predicts mental health in military personnel.
1.2. The mediating role of coping styles
Individuals facing stressful situations tend to employ different cognitive and behavioral skills to manage potential threats and effectively reduce the impact of stress and its accompanying adverse consequences for personal resources (28, 29). A growing number of scholars view mental health phenomena as processes by which resilience comes into play, with the outcomes determined by the interaction between personality traits and coping styles (30–32). Many studies have focused on the positive effects of resilience and coping styles on mental well-being outcomes (24, 33, 34). During the COVID-19 pandemic, scholars found that positive coping was associated with fewer stress symptoms, as well as decreased levels of anxiety, depression, PTSD, and other psychological disorders in healthcare workers, while negative coping was associated with more emotional stress and psychological symptoms (18, 21, 24). Appropriate coping style has a positive relationship with physical and mental health, quality of life, and subjective well-being (29, 35–37), suggesting that coping style may be an essential component in the mechanism by which resilience plays a protective role in mental health outcomes. Past studies have examined coping strategies as mediating factors in the relationship between resilience and adaptive outcomes such as somatic health symptoms and environmental adjustment (9). In studies on student populations, coping responses have been found to influence the impact of resilience on various outcomes, particularly physical health and college adjustment (9). Therefore, we posited the following:
Hypothesis 2: The impact of resilience on mental health is mediated by coping styles.
1.3. The moderating role of regulatory focus
Mental health outcomes under stress or adversity are often due to the interaction of factors in an individual’s complex ecosystem (38, 39). Regulatory focus refers to the specific tendencies that individuals exhibit in the process of self-regulation to achieve their desired end states (40). In response to specific situations, individuals adjust their cognition and behavior through a specific regulatory focus (40). Stress theory suggests that different stressors lead to different coping styles, implying that differences in personality and self-regulation may affect the strategies people use to reduce the discomfort caused by pressures (28, 41). The regulation focus theory suggests that individuals with a promotion-focused predominance are driven to pursue success and profit, pay more attention to positive information and results, view stressful situations as opportunities and challenges, and mobilize all resources available to achieve successful outcomes in their behavioral strategies. By contrast, prevention-focused individuals are risk-averse, sensitive to negative information and outcomes, seek safety and non-failure in their behavioral strategies, perceive stressful situations as threats and obstacles, and consume more of their internal resources in such situations (38–40, 42).
Current empirical studies indicate that different focal conditioning affects individuals’ choice of coping style, leading to different psychological experiences and behavioral outcomes. A promotion focus tends to be associated with positive and well-adapted coping styles, as well as positive emotional experiences with fewer psychological symptoms (29, 38). On the other hand, a prevention focus tends to be associated with passive coping styles, negative emotional experiences, and more maladaptive outcomes (43, 44). Thus, we developed the following hypothesis:
Hypothesis 3: The indirect effect of the degree of resilience on mental health through coping styles is moderated by regulatory focus.
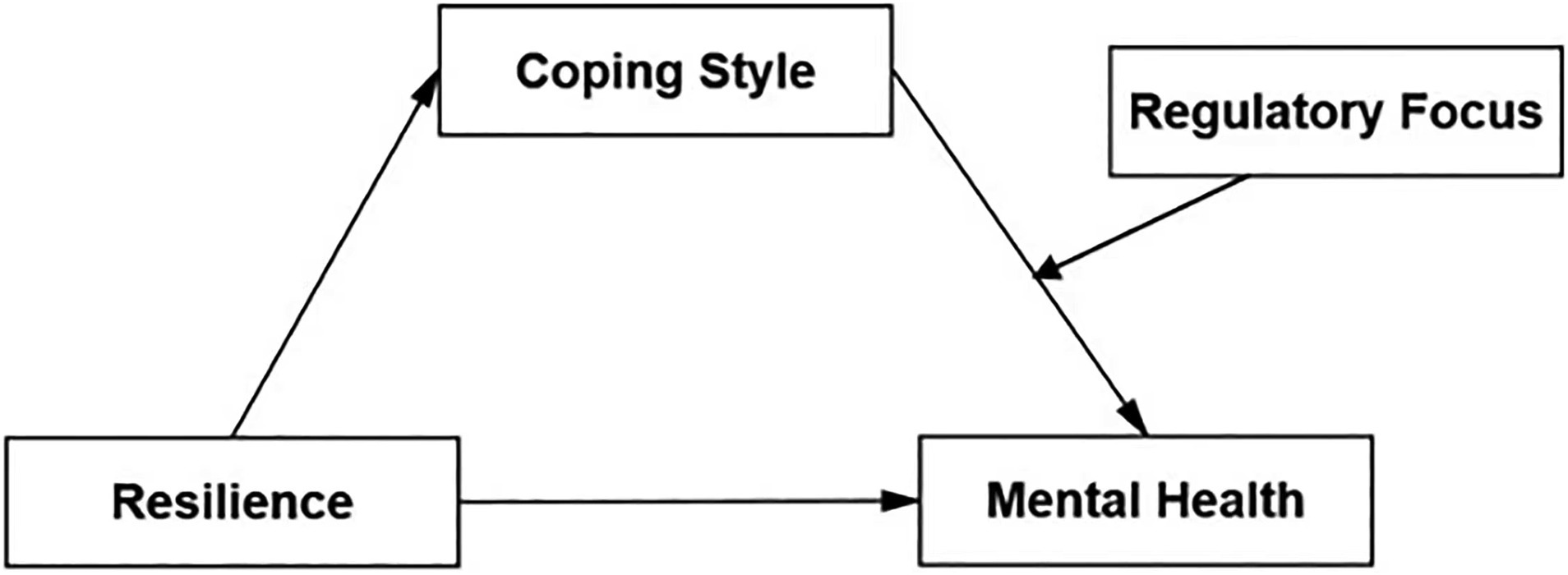
The conceptual model utilized in this study is set out in Figure 1.
2. Methods
2.1. Participants and recruitment
The participants were military officers from grassroots units who took part in a routine psychological assessment to ensure that their psychological status at the time was suitable for the military environment and their job requirements (N = 1,206). These military officers were all on active duty and were stationed in the field. Their main task was to adapt to the field environment and daily military training to improve their field combat effectiveness. All participants were made aware of and consented to the study’s objectives, and 1,110 valid questionnaires were collected. The final sample included 1,110 participants with a 92.04% response rate.
2.2. Measures
2.2.1. Demographics
We used a demographic information questionnaire to collect demographic data, including the following five parameters: (a) gender, (b) age, (c) personnel category, (d) education level, and (e) place of upbringing.
2.2.2. Symptom checklist-90
We used a 90-item checklist, the symptom checklist-90 (SCL-90), to assess the participants’ mental health based on their self-report Likert scale responses (45). Higher scores suggest more severe psychological symptoms and therefore represent poorer mental health. The SCL-90 aims to assess the severity of individuals’ self-perceived symptoms across nine dimensions (i.e., somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism). Participants are asked to respond from 1 (none at all) to 5 (very severe) in terms of their experience of the symptom described by each item. The total score ranges from 90–450, with a higher score denoting more severe symptoms. The nine dimension scores provide insight into the characteristics of the symptom distributions and are a valuable tool for assessing mental health. The Cronbach’s α coefficients for the nine subscales in the current study ranged from 0.811 to 0.904.
2.2.3. The Conner–Davidson resilience scale
We used the Conner–Davidson resilience scale (CD-RISC) to assess participants’ psychological resilience (46). The scale has 25 items, each of which is assessed on a 5-point Likert scale ranging from 0 (completely false) to 4 (almost always true) (1, rarely true; 2, occasionally true; 3, often true). Total scores range from 0 to 100 points, and higher scores indicate better resilience. In the current research, the Cronbach’s α coefficient of this scale was 0.975.
2.2.4. Coping style questionnaire
We employed the coping style questionnaire (CSQ) to evaluate the kinds of coping strategies military personnel used during the pandemic (47). This questionnaire was developed according to Folkman and Bond’s coping and defense questionnaires (48, 49) and has primarily been used to assess coping styles in the context of Chinese linguistic features. The 62-item questionnaire consists of 6 subscales (problem-solving, self-blaming, help-seeking, fantasizing, escaping, and justifying), and each item is scored as either 0 (agree) or 1 (disagree). Problem-solving and help-seeking are recognized as mature coping styles; self-blaming, fantasizing and escaping are recognized as immature coping styles; and justifying is recognized as a mixed coping style. The Cronbach’s α coefficients for the six subscales in the current study ranged from 0.776 to 0.899.
2.2.5. Regulatory focus questionnaire
We used the 11-item regulatory focus questionnaire to measure participants’ regulatory focus predominance (50). The questionnaire consists of a 6-item promotion focus subscale (e.g., “Do you often do well at different things that you try?”) and a 5-item prevention focus subscale (e.g., “Were you prone to getting on your parents’ nerves when you were a child?”) that we reverse scored. Participants rate each item from 1 (rarely) to 5 (always). In this study, the Cronbach’s α coefficients of the two subscales were 0.805 and 0.759. We calculated the predominant regulatory focus in the current study by subtracting the mean rating for prevention-related items from the mean rating for promotion-related items (51). Thus, we acquired an index of regulatory focus predominance, with a higher value indicating a tendency toward promotion predominance.
3. Data analysis and results
We utilized IBM SPSS 23.0 (IBM Corporation, Armonk, NY, United States) for statistical organization and analysis to investigate the connections between psychological symptoms, coping style, and resilience. We also conducted Pearson correlation analyses. We tested the mediating and moderating effects (models 4 and 14) through the SPSS macro program PROCESS 3.5, developed by Hayes (52, 53).
3.1. Descriptive statistics and correlation analysis
Table 1 presents sociodemographic descriptions. The participants were primarily male (94.68% of the total), with an average age of 25.12 ± 5.21 years old. In terms of education level, more than half had a high school degree or above (68.11%), and most grew up in rural areas (65.77%).
Table 2 displays the results of the correlation analysis. Resilience and psychological symptoms had a substantial negative association (p < 0.01), indicating that resilience was an important protective factor for mental health, and a high level of resilience can significantly reduce psychological symptoms. Mixed coping styles were positively correlated with the SCL-90 score (p < 0.01), and mature coping styles were negatively correlated with the SCL-90 score (p < 0.01). The results of correlation analysis between coping styles and psychological symptoms show that different coping styles have different effects on mental health. Compared with justifying, which represents the mixed coping style, individuals’ use of mature coping styles can significantly reduce their psychological symptoms. These findings support Hypothesis 1.
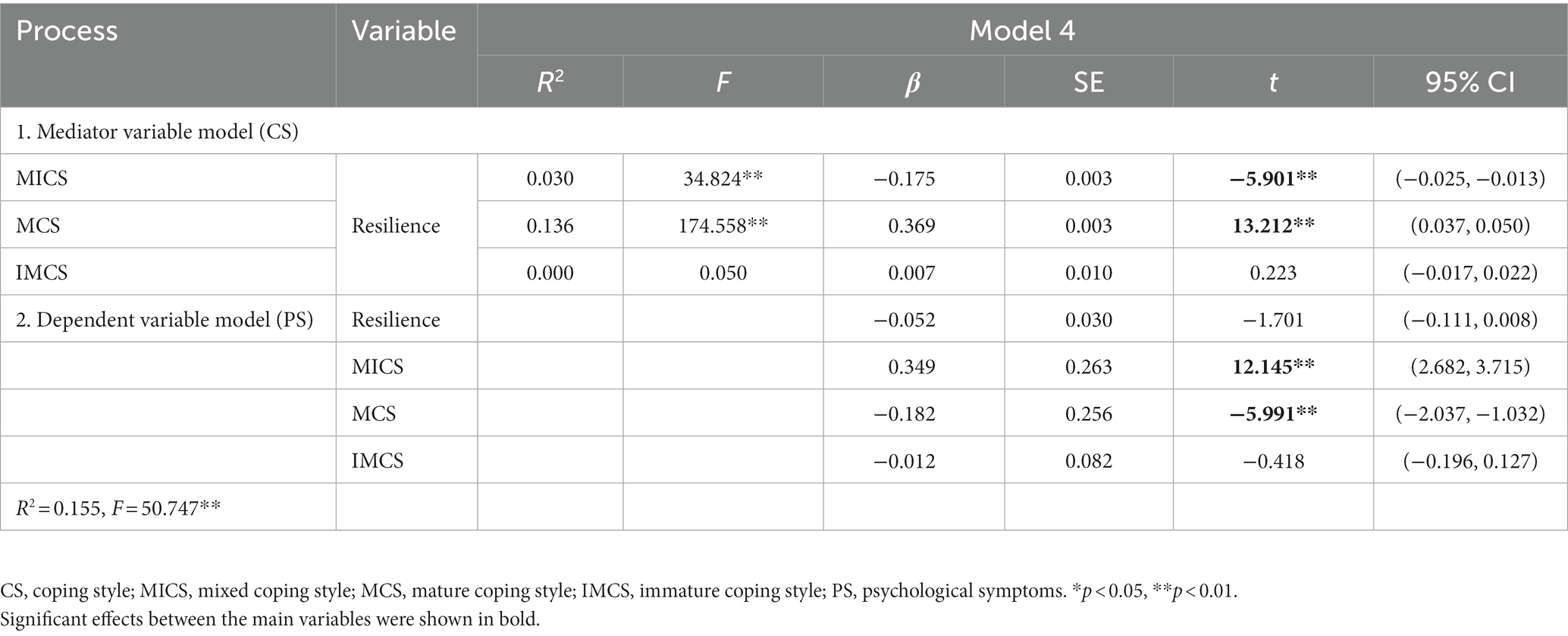
3.2. Test for the mediating effect of coping styles
We conducted a bootstrap analysis with 5,000 resamples to evaluate the mediating effect of coping styles between resilience and psychological symptoms. Table 3 outlines detailed results. Resilience had a significant positive effect on mature coping styles (β = 0.369, p < 0.01) and a significant negative effect on mixed coping styles (β = −0.175, p < 0.01). Mature coping styles (β = −0.182, p < 0.01) and mixed coping styles (β = 0.349, p < 0.01) had a significant influence on psychological symptoms. Therefore, the relationship between resilience and psychological symptoms was mediated by coping styles (mature and mixed coping styles), indicating that coping styles were the mechanism by which resilience affected mental health. These results supported Hypothesis 2.
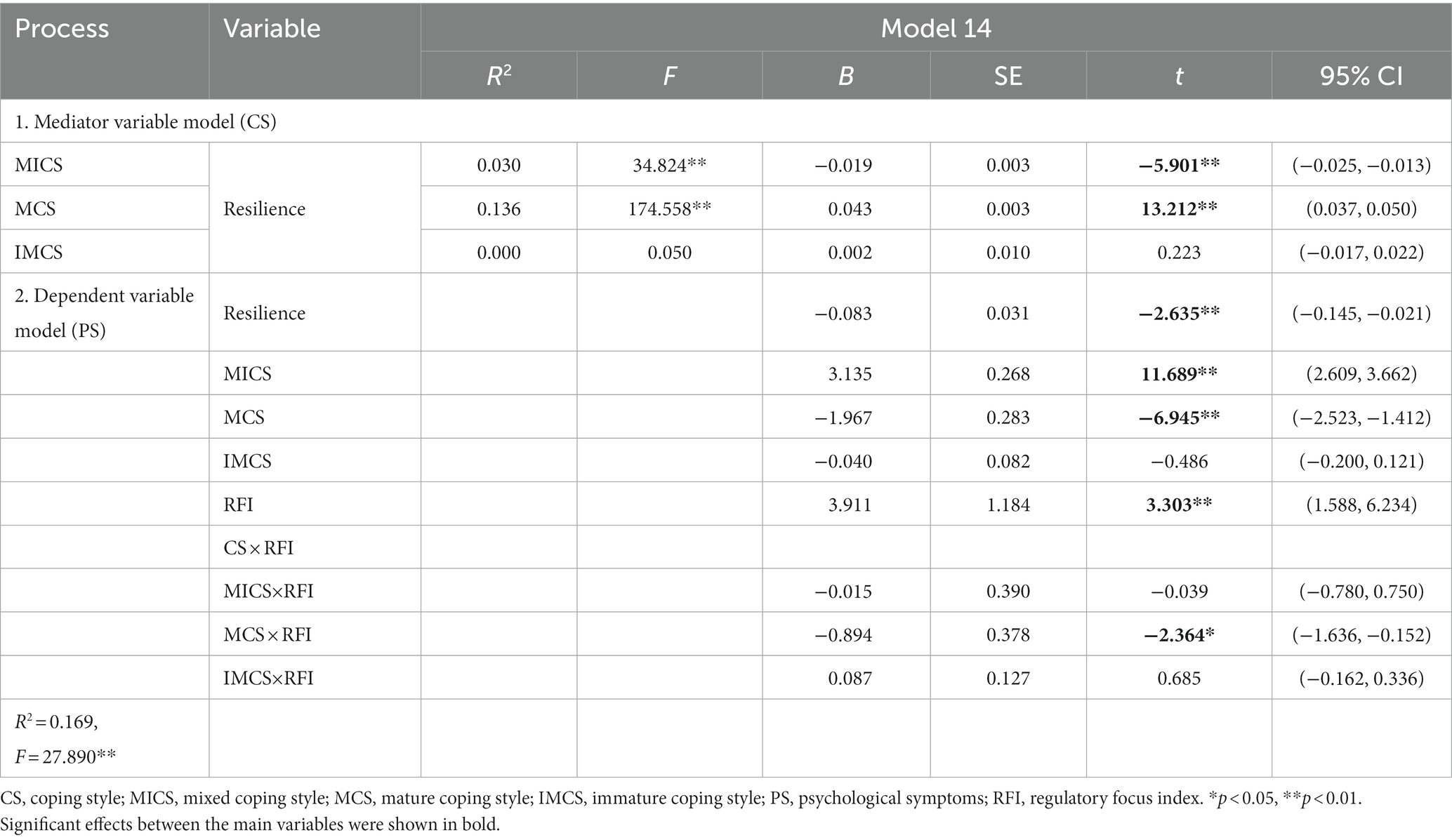
3.3. Test for the moderating effect of regulatory focus predominance
We hypothesized that regulatory focus might moderate the indirect effect (the coping style-mental health pathway) of coping styles on mental health. The findings in Table 4 demonstrate that mature coping styles and regulatory focus were significantly associated with psychological symptoms (B = −0.894, p < 0.01); specifically, regulatory focus moderated the relationship between mature coping styles and mental health. The indirect effects of resilience on mental health through mature coping styles were moderated by regulatory focus. These results support Hypothesis 3.
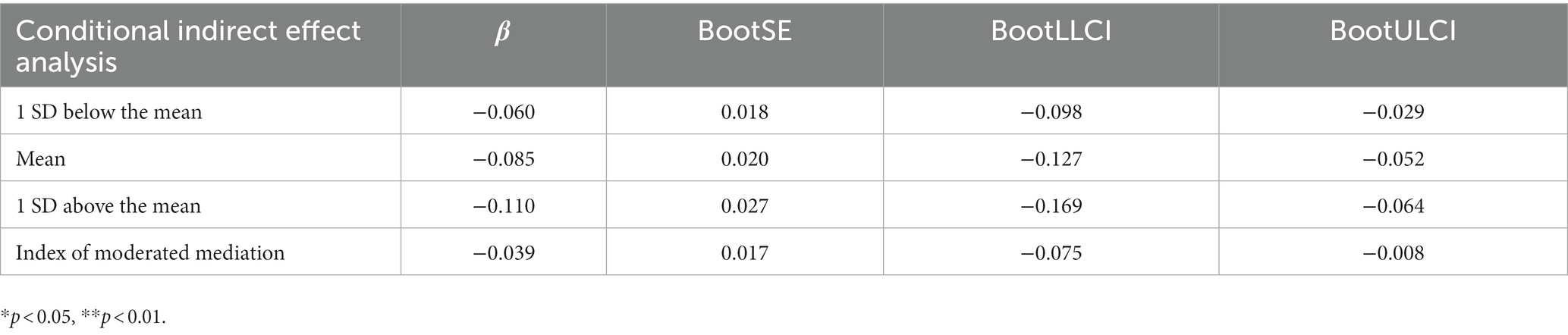
To further interpret how coping style and regulatory focus interact, we performed a simple slope analysis (see Figure 2). For the military personnel with a high regulatory focus index, mature coping styles were negatively predictive of psychological symptoms (Bsimple = −2.55, t = −5.88, p < 0.001). For those with a low regulatory focus index, the negative predictive effect of mature coping styles on psychological symptoms was diminished (Bsimple = −1.39, t = −4.55, p < 0.001). This suggests that the tendency for mental health levels to improve with the use of mature coping styles rises significantly as the tendency to promote focus increases.
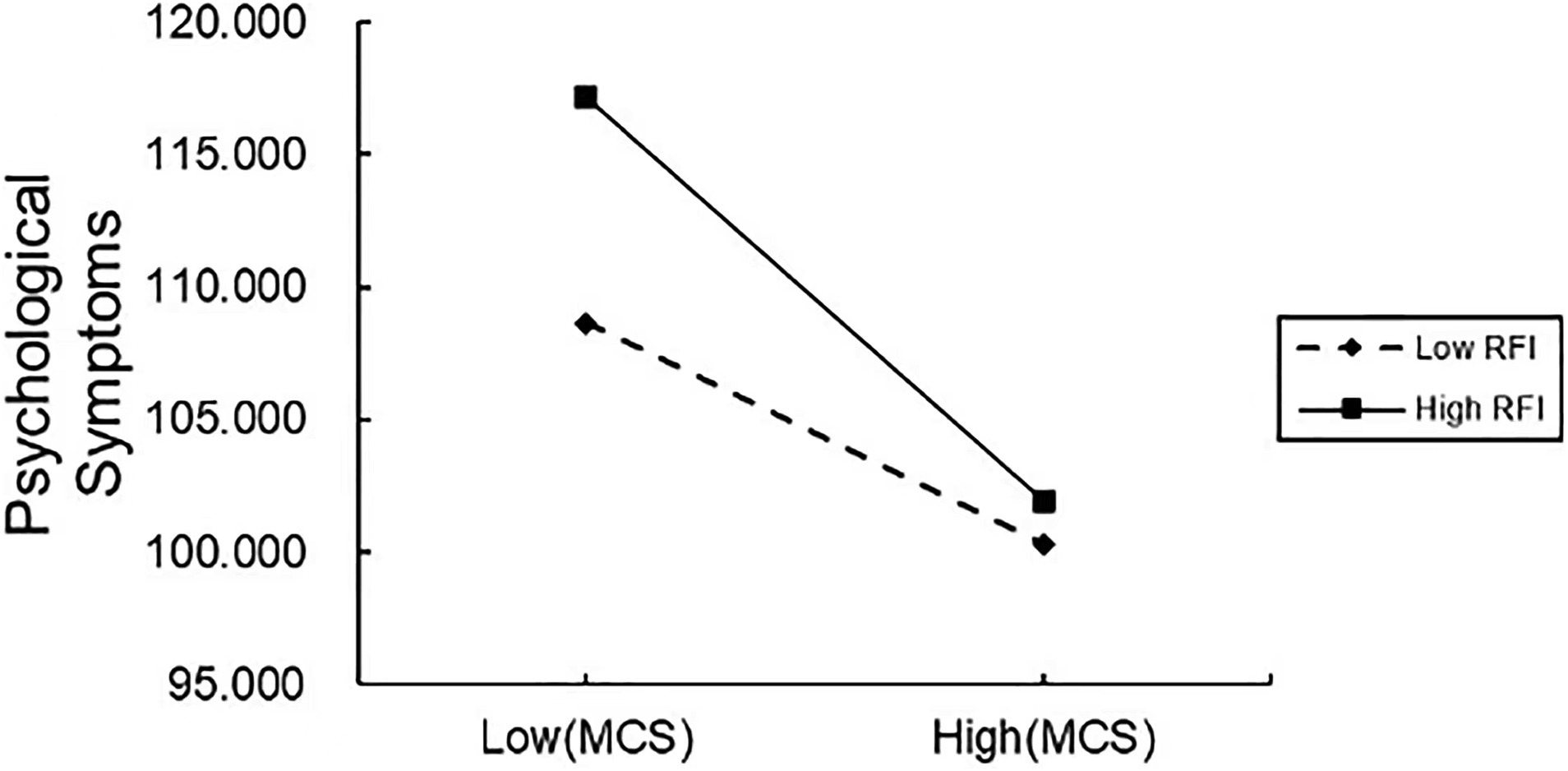
Figure 2. Moderated effect of regulatory focus on the relationship between psychological symptoms and a mature coping style. MCS, mature coping style; RFI, regulatory focus index.
As shown in Table 5, resilience has a conditional indirect effect on psychological symptoms, mediated by mature coping styles at different values of the regulatory focus index. The indirect effect of mature coping styles was stronger at 1 standard deviation above the mean [β = −0.110, 95% CI (−0.169, −0.064)] than at 1 standard deviation below the mean [β = −0.060, 95% CI (−0.098, −0.029)].
4. Discussion
Military personnel faced multidimensional stress during the COVID-19 pandemic, which increased their risk of developing psychological and psychiatric disorders (4). In the context of the pandemic, there was a decrease in the accessibility of timely and effective psychological interventions due to the prioritization of clinical treatments. In such instances of decreased resources, a shift in focus to protective factors for mental health is needed to prevent non-combat attrition and ensure combat readiness for the military population.
We investigated how resilience, coping styles, and regulatory focus influenced the mental health of military personnel during the COVID-19 pandemic. Resilience had a significant negative effect on psychological symptoms, and we identified the mediating roles of mixed and mature coping styles. Furthermore, regulatory focus negatively moderated the effect of mature coping styles on psychological symptoms.
4.1. Theoretical and practical implications
Our results have enriched the literature on the relationship between positive psychological resources and mental health outcomes in several ways. Firstly, the current study provides evidence and support for focusing on psychological services for military populations during the pandemic. Although previous studies have examined resilience and variables relating to mental health in military personnel, most of the literature is oriented toward the outcomes and occurrences of mental illness and focuses on clinical interventions (25, 27, 54, 55). In the context of public health emergencies, where medical resources are more centered on clinical treatments and psychological services are less accessible, the focus must be shifted to the prevention of mental illness and the mechanisms by which protective factors play a role. However, research on resilience in relation to mental health in pandemic contexts is still fairly limited for active-duty military personnel. The present study indicates that resilience has a positive effect on the psychological well-being of military personnel and serves as a protective factor for mental health in the pandemic context. This is consistent with past findings that resilience reduces negative outcomes from stressful events (19–21).
Secondly, we developed a conceptual framework in which we considered coping styles (mature, immature, and mixed) as mediating mechanisms that act on mental health through resilience. Specifically, we found that mature coping styles, such as problem-solving and help-seeking, were significantly and positively correlated with resilience and negatively correlated with psychological symptoms. We also found that mixed coping styles were significantly and negatively correlated with resilience but positively correlated with psychological symptoms. Immature coping styles, such as self-blaming and escaping, were not significantly correlated with resilience or psychological symptoms. Stress theory suggests that different stressors lead to different coping styles, and during the stress process, coping is highly correlated with emotion regulation. Specifically, certain coping strategies that avoid reality are always associated with adverse mental health outcomes, while other coping strategies have varying outcomes in different contexts (56), which is partially consistent with our findings. Notably, immature coping styles were not significantly correlated with either resilience or mental health outcomes in the current study. This may be related to the culture advocated by the military environment in which all military personnel are expected to function at a high level of proficiency in stressful situations (3). Negative or immature coping styles were the least commonly used coping strategies in relevant research with military personnel (3, 57). This suggests that encouraging the military population to adopt mature coping styles (i.e., help-seeking behaviors during stressful events) in military management and psychological services can better alleviate psychological symptoms in stressful situations.
Finally, we explored a critical boundary condition in the relationship between coping styles and psychological symptoms. The regulatory focus index was significantly and positively related to resilience, and mature coping styles were more effective at protecting mental health among military personnel with a high regulatory focus index. As the coping process is intricate and multifaceted, it is sensitive to environmental demands and resources as well as to personality traits that affect the perception of stress and use of resources for coping (56). In response to stressful situations, individuals adjust their cognition and behavior through two independent modes of self-regulation with distinct preferences for goal attainment and strategically different ways of coping: the promotion focus and prevention focus, respectively characterized by eagerness and by cautiousness and avoidance (40–42). Since a high regulatory focus index represents an individual’s preference for promotion-focused self-regulation, this implies that promotion-focused individuals can more successfully resist psychological threats arising from stressful events by enhancing their maturity-based coping skills. This finding can be explained by regulatory fit theory, which states that the effect occurring via the pursuit of goals matches self-regulation (58–60). Promotion-focused individuals are motivated by positive outcomes in the pursuit of goals and adopt more proactive strategies. This makes mature coping styles (such as problem-solving and help-seeking) match their goal-seeking strategy, resulting in better outcomes in stressful situations (27, 38) due to the regulatory fit effect.
4.2. Limitations and future research directions
Our research is restricted by some limitations. First, the study was cross-sectional, which means it can only reflect correlations among the variables. Future studies should examine causal patterns using longitudinal and experimental methods. Second, in previous studies on military populations, justifying was found to be significantly and negatively associated with help-seeking behaviors (31) and positively associated with negative coping styles (61). In the current study, however, justifying was positively associated with psychological symptoms and mature coping styles. This implies that justifying, as a mixed coping style, has a different working mechanism that significantly influences mental health outcomes when individuals cope with stressful events. Future studies should explore this association in greater depth. Finally, military personnel with different positions may have varying coping styles and levels of mental health. In the existing studies on Chinese military personnel, demographic variables, such as age, gender, education level, and military rank, are significantly correlated with mental health symptoms (e.g., anxiety, social anxiety disorder) (61–63). Moreover, in relevant studies conducted in western countries, sociodemographic characteristics, such as race, ethnicity, marital status, and enlistment age, can all affect the mental health of military personnel (64–66). As such, future research would benefit from focusing on specific personnel categories to develop more targeted guidance for psychological services.
5. Conclusion
We developed a moderated mediating model to explain the effects of resilience on the psychological well-being of military personnel. The current research has confirmed that coping styles—especially mature coping styles—play a fundamental role in the relationship between resilience and psychological symptoms in military populations, and may have been essential protective factors of mental health during the pandemic. Furthermore, this study indicates that promotion-focused individuals can more effectively resist the psychological threats associated with stressful events by enhancing the practice of mature coping styles. Besides advocating for a military culture which maintains the mental health of personnel, encouraging military members to contact significant others (e.g., telephone family and friends), as well as ask for advice or assistance from organization members when faced with specific problems, can benefit individuals’ successful adaption in stressful situations (3, 57). These findings offer insights and intervention strategies for mental healthcare in the military.
Data availability statement
The datasets presented in this article are not readily available because in accordance with participant privacy and ethical requirements, we do not permit the sharing of data. Requests to access the datasets should be directed to Y2FvZmVpQGppYW5nbmFuLmVkdS5jbg==.
Ethics statement
The studies involving humans were approved by Air Force Medical University evaluated and authorized the investigation, which was conducted with the informed consent of all participants. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
FC performed the research and wrote the paper. WX and ZY assisted with the research and analyzed the data. JL provided technical guidance. DW conceptualized the current study and provided financial support. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the General Project of Philosophy and Social Science Research of Colleges and Universities in Jiangsu Province (2021SJA0851) and the Fundamental Research Funds for the Central Universities (JUSRP12072).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Montemurro, N . The emotional impact of COVID-19: from medical staff to common people. Brain Behav Immun. (2020) 87:23–4. doi: 10.1016/j.bbi.2020.03.032
2. Hill, ML, Nichter, B, Na, PJ, Norman, SB, Morland, LA, Krystal, JH, et al. Mental health impact of the COVID-19 pandemic in U.S. military veterans: a population-based, prospective cohort study. Psychol Med. (2023) 53:945–56. doi: 10.1017/S0033291721002361
3. Clemons, EP . Monitoring anxiety levels and coping skills among military recruits. Mil Med. (1996) 161:18–21. doi: 10.1093/milmed/161.1.18
4. Paredes, MR, Apaolaza, V, Fernandez-Robin, C, Hartmann, P, and Yañez-Martinez, D. The impact of the COVID-19 pandemic on subjective mental well-being: the interplay of perceived threat, future anxiety and resilience. Pers Individ Differ. (2021) 170:110455. doi: 10.1016/j.paid.2020.110455
5. Wynn, G, Morganstein, JC, Jetly, R, Ford, SC, Vance, MC, Meyer, EG, et al. Military mental health and COVID-19. J Mil Veteran Fam Health. (2020) 6:21–6. doi: 10.3138/jmvfh-2020-0048
6. Kessler, RC, Heeringa, SG, Stein, MB, Colpe, LJ, Fullerton, CS, Hwang, I, et al. Thirty-day prevalence of DSM-IV mental disorders among nondeployed soldiers in the US Army: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). JAMA Psychiatry. (2014) 71:504–13. doi: 10.1001/jamapsychiatry.2014.28
7. Cates, DS . Minimizing psychological distress and promoting resilience during quarantine: piloting the town hall model. Prof Psychol Res Pract. (2021) 52:260–71. doi: 10.1037/pro0000382
8. Jew, CL, Green, KE, and Kroger, J. Development and validation of a measure of resiliency. Meas Eval Couns Dev. (1999) 32:75–89. doi: 10.1080/07481756.1999.12068973
9. Fullerton, DJ, Zhang, LM, and Kleitman, S. An integrative process model of resilience in an academic context: resilience resources, coping strategies, and positive adaptation. PLoS One. (2021) 16:e0246000. doi: 10.1371/journal.pone.0246000
10. Hoopsick, RA, Homish, DL, Collins, RL, Nochajski, TH, Read, JP, Bartone, PT, et al. Resilience to mental health problems and the role of deployment status among U.S. Army Reserve and National Guard Soldiers. Soc Psychiatry Psychiatr Epidemiol. (2020) 56:1299–310. doi: 10.1007/s00127-020-01899-5
11. Peck, BS, and Parcell, ES. Talking about mental health: dilemmas U.S. military service members and spouses experience post deployment. J Fam Commun. (2021) 21:90–106. doi: 10.1080/15267431.2021.1887195
12. Ureña, S, Taylor, MG, and Carr, DC. The impact of military service exposures and psychological resilience on the mental health trajectories of older male veterans. J Aging Health. (2021) 33:237–48. doi: 10.1177/0898264320975231
13. Daffey-Moore, E . Why is building psychological resilience relevant to UK service personnel in order to improve military mental health? BMJ Mil Health. (2018) 166:89–94. doi: 10.1136/jramc-2018-000962
14. Bartone, PT, Hystad, SW, Eid, J, and Brevik, JI. Psychological hardiness and coping style as risk/resilience factors for alcohol abuse. Mil Med. (2012) 177:517–24. doi: 10.7205/milmed-d-11-00200
15. Bartone, PT, Johnsen, BH, Eid, J, Hystad, SW, and Laberg, JC. Hardiness, avoidance coping, and alcohol consumption in war veterans: a moderated-mediation study. Stress Health. (2017) 33:498–507. doi: 10.1002/smi.2734
16. Thomassen, ÅG, Hystad, SW, Johnsen, BH, Johnsen, GE, Laberg, JC, and Eid, J. The combined influence of hardiness and cohesion on mental health in a military peacekeeping mission: a prospective study. Scand J Psychol. (2015) 56:560–6. doi: 10.1111/sjop.12235
17. Wooten, NR . Deployment cycle stressors and post-traumatic stress symptoms in Army National Guard women: the mediating effect of resilience. Soc Work Health Care. (2012) 51:828–49. doi: 10.1080/00981389.2012.692353
18. Peng, L, Ye, Y, Wang, L, Qiu, W, Huang, S, Wang, L, et al. Chain mediation model of perceived stress, resilience, and social support on coping styles of Chinese patients on hemodialysis during COVID-19 pandemic lockdown. Med Sci Monit. (2022) 28:e935300. doi: 10.12659/MSM.935300
19. Foster, K, Roche, M, Giandinoto, J-A, and Furness, T. Workplace stressors, psychological well-being, resilience, and caring behaviours of mental health nurses: a descriptive correlational study. Int J Ment Health Nurs. (2020) 29:56–68. doi: 10.1111/inm.12610
20. Heath, C, Sommerfield, A, and von Ungern-Sternberg, BS. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: a narrative review. Anaesthesia. (2020) 75:1364–71. doi: 10.1111/anae.15180
21. Labrague, LJ . Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: a systematic review of quantitative studies. J Nurs Manag. (2021) 29:1893–905. doi: 10.1111/jonm.13336
22. Hoopsick, RA, Benson, KR, Homish, DL, and Homish, GG. Resiliency factors that protect against post-deployment drug use among male US Army Reserve and National Guard Soldiers. Drug Alcohol Depend. (2019) 199:42–9. doi: 10.1016/j.drugalcdep.2019.02.017
23. KT Green, PS Calhoun, and MF Dennis, Mid-Atlantic Mental Illness Research, Education and Clinical Center Workgroup; Jean C Beckham eds. Exploration of the resilience construct in posttraumatic stress disorder severity and functional correlates in military combat veterans who have served since September 11, 2001. J Clin Psychiatry. (2010) 71:823–30. doi: 10.4088/JCP.09m05780blu
24. Zhao, X, Wang, J, and Shi, C. The influence of mental resilience on the positive coping style of air force soldiers: a moderation-mediation model. Front Psychol. (2020) 11:550. doi: 10.3389/fpsyg.2020.00550
25. Rakesh, G, Morey, RA, Zannas, AS, Malik, Z, Marx, CE, Clausen, AN, et al. Resilience as a translational endpoint in the treatment of PTSD. Mol Psychiatry. (2019) 24:1268–83. doi: 10.1038/s41380-019-0383-7
26. Rakesh, G, Clausen, AN, Buckley, MN, Clarke-Rubright, E, Fairbank, JA, Wagner, HR, et al. The role of trauma, social support, and demography on veteran resilience. Eur J Psychotraumatol. (2022) 13:2058267. doi: 10.1080/20008198.2022.2058267
27. Youssef, NA, Green, KT, Beckham, JC, and Elbogen, EB. A 3-year longitudinal study examining the effect of resilience on suicidality in veterans. Ann Clin Psychiatry. (2013) 25:59–66. doi: 10.17615/ds9s-k061
28. Folkman, S . Stress: appraisal and coping In: MD Gellman and JR Turner, editors. Encyclopedia of behavioral medicine. New York, NY: Springer (2013). 1913–5.
29. Woltin, K-A, Sassenberg, K, and Albayrak, N. Regulatory focus, coping strategies and symptoms of anxiety and depression: a comparison between Syrian refugees in Turkey and Germany. PLoS One. (2018) 13:e0206522. doi: 10.1371/journal.pone.0206522
30. Skinner, EA, Edge, K, Altman, J, and Sherwood, H. Searching for the structure of coping: a review and critique of category systems for classifying ways of coping. Psychol Bull. (2003) 129:216–69. doi: 10.1037/0033-2909.129.2.216
31. Zhang, J, Cui, M, Wang, W, Lu, H, Wu, Q, Zhu, X, et al. The coexistence of coping resources and specific coping styles in stress: evidence from full information item bifactor analysis. PLoS One. (2014) 9:e96451. doi: 10.1371/journal.pone.0096451
32. Zhang, Y, Kong, F, Wang, L, Chen, H, Gao, X, Tan, X, et al. Mental health and coping styles of children and adolescent survivors one year after the 2008 Chinese earthquake. Child Youth Serv Rev. (2008) 32:1403–9. doi: 10.1016/j.childyouth.2010.06.009
33. Dewe, PJ, O’Driscoll, MP, and Cooper, CL. Coping with work stress: a review and critique. New York, U.S.: Wiley Blackwell (2010).
34. Folkman, S, and Moskowitz, JT. Stress, positive emotion, and coping. Curr Dir Psychol Sci. (2000) 9:115–8. doi: 10.1111/1467-8721.00073
35. Wang, P, Xiong, Z, and Yang, H. Relationship of mental health, social support, and coping styles among graduate students: evidence from Chinese universities. Iran J Public Health. (2018) 47:689–97.
36. Wu, C, Liu, Y, Ma, S, Jing, G, Zhou, W, Qu, L, et al. The mediating roles of coping styles and resilience in the relationship between perceived social support and posttraumatic growth among primary caregivers of schizophrenic patients: a cross-sectional study. BMC Psychiatry. (2021) 21:58. doi: 10.1186/s12888-021-03058-9
37. Zhou, K, Ning, F, Wang, X, Wang, W, Han, D, and Li, X. Perceived social support and coping style as mediators between resilience and health-related quality of life in women newly diagnosed with breast cancer: a cross-sectional study. BMC Womens Health. (2022) 22:198. doi: 10.1186/s12905-022-01783-1
38. Delegach, M, and Katz-Navon, T. Regulatory foci and well-being: coping flexibility and stressor appraisal as explanatory mechanisms. Int J Stress Manag. (2021) 28:117–29. doi: 10.1037/str0000219
39. Li, R, Liu, H, Yao, M, and Chen, Y. Regulatory focus and subjective well-being: the mediating role of coping styles and the moderating role of gender. J Psychol. (2019) 153:714–31. doi: 10.1080/00223980.2019.1601066
40. Higgins, ET . Beyond pleasure and pain. Am Psychol. (1997) 52:1280–300. doi: 10.1037/0003-066x.52.12.1280
41. Higgins, JE, and Endler, NS. Coping, life stress, and psychological and somatic distress. Eur J Personal. (1995) 9:253–70. doi: 10.1002/per.2410090403
42. Crowe, E, and Higgins, ET. Regulatory focus and strategic inclinations: promotion and prevention in decision-making. Organ Behav Hum Decis Process. (1997) 69:117–32. doi: 10.1006/obhd.1996.2675
43. Brockner, J, and Higgins, ET. Regulatory focus theory: implications for the study of emotions at work. Organ Behav Hum Decis Process. (2001) 86:35–66. doi: 10.1006/obhd.2001.2972
44. Jung, HS, and Yoon, HH. Understanding regulatory focuses. Int J Contemp Hosp Manag. (2015) 27:283–307. doi: 10.1108/IJCHM-07-2013-0288
45. Derogatis, LR, and Unger, R. Symptom checklist-90-revised. The Corsini encyclopedia of psychology (2010) 1–2. doi: 10.1002/9780470479216.corpsy0970
46. Connor, KM, and Davidson, JRT. Development of a new resilience scale: the Connor–Davidson resilience scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
47. Xiao, JH, and Xu, XF. The reliability and validity research of coping style questionnaire. Chin Ment Health J. (1996) 10:164–8.
48. Bond, M, Gardner, ST, Christian, J, and Sigal, JJ. Empirical study of self-rated defense styles. Arch Gen Psychiatry. (1983) 40:333–8. doi: 10.1001/archpsyc.1983.01790030103013
49. Folkman, S, Lazarus, RS, Gruen, RJ, and Delongis, A. Appraisal, coping, health status, and psychological symptoms. J Pers Soc Psychol. (1986) 50:571–9. doi: 10.1037/0022-3514.50.3.571
50. Higgins, ET, Friedman, RS, Harlow, RE, Idson, LC, Ayduk, ON, and Taylor, A. Achievement orientations from subjective histories of success: promotion pride versus prevention pride. Eur J Soc Psychol. (2001) 31:3–23. doi: 10.1002/ejsp.27
51. Camacho, CJ, Higgins, ET, and Luger, L. Moral value transfer from regulatory fit: what feels right is right and what feels wrong is wrong. J Pers Soc Psychol. (2003) 84:498–510. doi: 10.1037/0022-3514.84.3.498
52. Baron, RM, and Kenny, DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. (1986) 51:1173–82. doi: 10.1037/0022-3514.51.6.1173
53. Hayes, AF . Beyond Baron and Kenny: statistical mediation analysis in the new millennium. Commun Monogr. (2009) 76:408–20. doi: 10.1080/03637750903310360
54. Castro, CA, and Kintzle, S. Suicides in the military: the post-modern combat veteran and the Hemingway effect. Curr Psychiatry Rep. (2014) 16:460. doi: 10.1007/s11920-014-0460-1
55. Pan, Y, Cai, W, Dong, W, Xiao, J, Yan, J, and Cheng, Q. Behavior characteristics of the attention network of military personnel with high and low trait anxiety. Medicine. (2017) 96:e6630. doi: 10.1097/MD.0000000000006630
56. Folkman, S, and Moskowitz, JT. Coping: pitfalls and promise. Annu Rev Psychol. (2004) 55:745–74. doi: 10.1146/annurev.psych.55.090902.141456
57. Rice, V, and Liu, B. Personal resilience and coping part II: identifying resilience and coping among U.S. military service members and veterans with implications for work. Work. (2016) 54:335–50. doi: 10.3233/wor-162301
58. Higgins, ET . Making a good decision: value from fit. Am Psychol. (2000) 55:1217–30. doi: 10.1037/0003-066x.55.11.1217
59. Higgins, ET . Value from regulatory fit. Curr Dir Psychol Sci. (2005) 14:209–13. doi: 10.1111/j.0963-7214.2005.00366.x
60. Higgins, ET, and Pinelli, F. Regulatory focus and fit effects in organizations. Annu Rev Organ Psychol Organ Behav. (2020) 7:25–48. doi: 10.1146/annurev-orgpsych-012119-045404
61. Jiang, Y, Sun, YF, Yang, YB, Tang, JJ, Wu, SJ, Miao, DM, et al. Gender differences in coping styles of Chinese military officers undergoing intensive training. Mil Psychol. (2013) 25:124–35. doi: 10.1037/h0094954
62. Wang, H, Zhang, R, Chen, Y, Wang, H, Zhang, Y, Gan, J, et al. Social anxiety disorder in the Chinese military: prevalence, comorbidities, impairment, and treatment-seeking. Psychiatry Res. (2014) 220:903–8. doi: 10.1016/j.psychres.2014.07.063
63. Yang, Z, Cao, F, Lu, H, Zhu, X, and Miao, D. Changes of anxiety in Chinese military personnels over time: a cross-temporal meta-analysis. Int J Ment Heal Syst. (2014) 8:19. doi: 10.1186/1752-4458-8-19
64. Bergman, BP, Mackay, D, Fear, N, and Pell, J. Age at entry to UK military service and long-term mental health. BMJ Mil Health. (2021) 169:212–7. doi: 10.1136/bmjmilitary-2021-001786
65. Beymer, MR, Apostolou, A, Smith, CM, Paschane, DM, Gomez, SA, James, TD, et al. Mental health outcomes among American Indian and Alaska native U.S. army soldiers: a serial cross-sectional analysis. Mil Med. (2023) 188:e2292–9. doi: 10.1093/milmed/usad049
Keywords: military personnel, mental health, resilience, coping style, regulatory focus, COVID-19
Citation: Cao F, Li J, Xin W, Yang Z and Wu D (2023) The impact of resilience on the mental health of military personnel during the COVID-19 pandemic: coping styles and regulatory focus. Front. Public Health. 11:1240047. doi: 10.3389/fpubh.2023.1240047
Edited by:
Samer El Hayek, Erada Center for Treatment and Rehab, United Arab EmiratesReviewed by:
Meenakshi Shukla, Allahabad University, IndiaPeter Kamstra, The University of Melbourne, Australia
Copyright © 2023 Cao, Li, Xin, Yang and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Di Wu, d3VkaTA0MjZAb3V0bG9vay5jb20=
 Fei Cao
Fei Cao Juan Li1
Juan Li1 Wei Xin
Wei Xin Di Wu
Di Wu