- 1Department of Therapy and Rehabilitation, Ağrı İbrahim Çeçen University, Ağrı, Türkiye
- 2Department of Guidance and Psychological Counselling, Ağrı İbrahim Çeçen University, Ağrı, Türkiye
- 3Special Education Department, College of Education, Salahaddin University, Erbil, Iraq
- 4Department of English, College of Education, Bayan University, Erbil, Iraq
- 5Faculty of Science and Letters, Department of Psychology, Ağrı İbrahim Çeçen University, Ağrı, Türkiye
- 6Graduate Studies and Research, Lebanese American University, Beyrut, Lebanon
- 7Department of Measurement and Assessment, Van Yüzüncü Yıl University, Van, Türkiye
- 8Post-Graduate School of Occupational Health, Università Cattolica del Sacro Cuore, Rome, Italy
- 9Health Service Department, Italian State Police, Ministry of the Interior, Milan, Italy
- 10Occupational Medicine/Health Technology Assessment and Safety Research Unit, Clinical-Technological Innovations Research Area, Bambino Gesù Children’s Hospital, IRCCS, Rome, Italy
Individuals with a satisfactory level of job satisfaction are much less likely to feel hopeless about their future and are more likely to perform efficiently in the workplace. General work stress (i.e., the work-related stress subjectively experienced) is a significant predictor of suicide cognitions. Furthermore, it has been posited that satisfaction and hope are fundamental to life from an existential perspective. We, therefore, tested a hypothetical model of general work stress, suicide cognitions, hopelessness, and job satisfaction. The data were collected from 416 health-care workers through a convenience sampling method. The mediation analysis results revealed significant negative and positive relationships among general work stress, suicide conceptions, hopelessness, and job satisfaction. The findings indicate that hopelessness and job satisfaction have a parallel mediating effect in the relationship between general work stress and suicide cognitions. The result of the study is of great importance, which suggests that interventions to alleviate hopelessness and work stress and to boost the job satisfaction of medical staff may help prevent suicide cognitions.
Introduction
Work stress refers to the mental and physical discomfort health-care staff in health-care workplaces experience because of their duties (1, 2). General work stress arises due to the interaction between employees and their work, negatively affecting mental and physical health, reducing the employee’s standard of living, and causing various work-related negativities (3). As well as having physical consequences such as behavioral disorders, there may also be mental consequences such as depression, burnout, anxiety, and suicidal thoughts (4, 5). A variety of types of stress may affect an employee’s performance at work, such as job stress, academic stress, environmental stress, health stress, relationship stress, and especially family stress (6–8).
Work stress can create intense pressure on health-care workers (9, 10). Several epidemiological studies have indicated that employees exposed to work stress may experience intense suicidal thoughts (11–14). An effort-reward imbalance (ERI) model describes the disparity between employee job pressure, the amount of effort they put into their jobs, and the low reward they get (15). Those who put forth great effort at work and perform tasks that risk their health will likely experience chronic work-related stress in the long run if the reward they receive is not commensurate with their effort (16). Employees may ultimately realize their thoughts are hurting them, resulting in suicidal thoughts (17, 18). It is essential to disclose other risk factors that may lead to suicide cognitions in health-care workers to prevent suicide (19). Health-care workers have been found to have higher suicide cognitions than the general population due to work stress (20–22).
The work stress in health-care staff can be associated with various mental health problems (e.g., depression, anxiety, and stress) (23). According to Godifay et al. (24), health-care workers may be at greater risk for work stress than others, and it is closely linked to job satisfaction. In general, job satisfaction refers to a sense of well-being based on the profession’s role in society, the experience of the employee, and the ability to evaluate them as a professional (25). The level of job satisfaction has been reported to affect the quality and delivery of health-care services and mediate the relationship between patient health outcomes (26).
Job satisfaction is closely related to individuals’ emotional relationship with their work and the pleasure and dissatisfaction they feel while doing their work (27). The high job satisfaction of health-care workers reduces their work stress while also helping them to perform more effectively. (28, 29). A lack of job satisfaction results in reduced ability to be productive at work and problems with attendance and negativity, which may result in termination from the position (30). Health workers are more likely to increase their work productivity if they are satisfied with their jobs, and those with increased work stress are less likely to be satisfied with their jobs (31–33). Stress may result in a decrease in job satisfaction and an increase in mental health symptoms such as anxiety, depression, and thoughts of suicide (34–39). Among health-care workers, stress at work may have led to problems in personal relationships, concentration problems, and physical problems, leading to hopelessness (40, 41). In addition to work-related stress, personal isolation, the possibility of death, and fatigue caused by wearing protective clothing for an extended period of time may have contributed to hopelessness among health-care personnel (41–45).
Hopelessness has been associated with psychological concepts such as work-related stress, suicide, anxiety, conflict, and burnout (43, 46–48). This refers to emotional states in which the individual believes any attempt to affect change will be futile (49). The studies suggest that self-harm, anxiety, fear, anxiety, depression, and suicidal ideation are some negative outcomes that hopelessness might be related (50, 51). Suicide can result from an individual’s belief that they are unable to do something due to hopelessness (52, 53). Hopelessness theory suggests that individuals may develop a greater risk of suicidal ideation when they perceive themselves trapped in an impossible situation without a sense of escape or improvement (52). This may lead individuals to consider suicide a viable option to escape their pain if they do not have hope for the future.
Aims and objectives
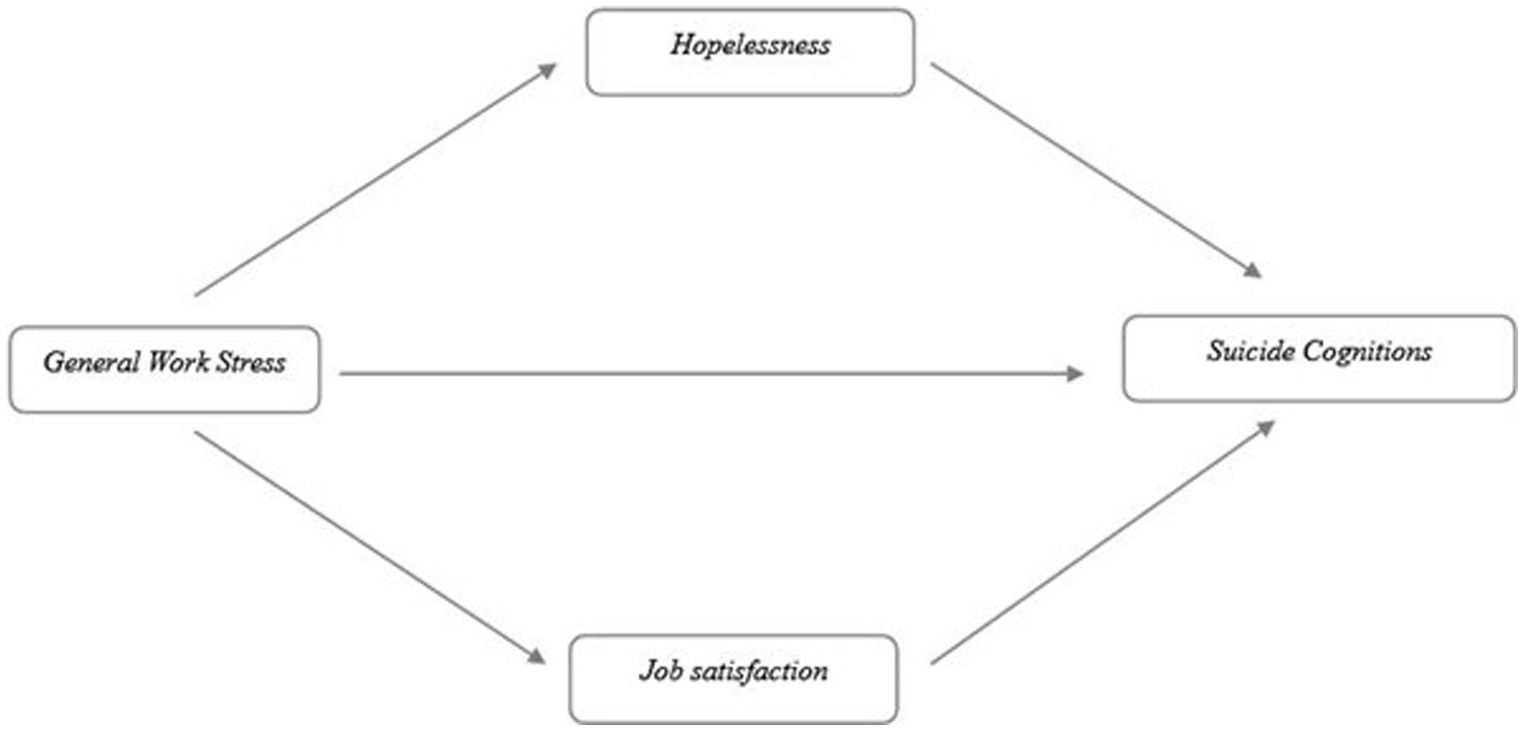
This cross-sectional study is grounded in the framework of the Hopelessness Theory and Effort–Reward Imbalance. Previous empirical research has demonstrated that general work-related stress is a significant predictor of suicide cognitions (54, 55). Additionally, various studies have identified the relationships between general work stress, suicide cognitions, hopelessness, and job satisfaction (22, 32, 33, 47, 54, 56–58). In light of both theoretical foundations and empirical evidence, we propose a new model to investigate the relationships between the above-mentioned variables. This model examines the mediating effect of hopelessness and job satisfaction in the relationship between general work stress and suicide cognitions (see Figure 1). The following hypotheses were addressed in our study: (i) general work stress would have a significant negative impact on job satisfaction and a significant positive impact on hopelessness and suicide cognitions, (ii) hopelessness would serve as a mediating factor in the relationship between general work stress and suicide cognitions, and (iii) job satisfaction would serve as a mediator in the relationship between general work stress and suicide cognitions.
Method
Participants and ethics
Participants included 416 medical staff (70.9% female and 121 male) working in Türkiye. The age range of the participants was 21–60, with a mean age of 26.96 (SD = 7.16). They self-expressed themselves regarding their socioeconomic status (Low SES = 28.8%, Moderate SES = 64.9%, and High SES = 6.3%). Eligibility criteria included (i) being a health worker, (ii) working in any public or private health institution, (iii) participating voluntarily. Incentives were not provided to participants. The ethics committee at the university of the first author approved the study (reference number: E.73559). The study was conducted from October 2022 to May 2023.
Power analysis
The power analysis was performed in order to reveal accurately and strongly the relationships between the predictor and predicted variable determined within the scope of the study. The analysis was conducted using the G* Power 3.1.9.7 program to determine the sample size required. Accordingly, with conventional significance levels of 0.05 and power of 0.80, a small effect size is defined as r = 0.20 (59). A total of 395 samples were required based on the results of the analysis. Upon reaching a sufficient sample size, the power analysis was repeated as a post hoc procedure under the same conditions. The power of the sample size of the study was calculated as 0.82 (1-β err probe). The results of this analysis indicate that the sample had a sufficient level of power for the analyses.
Measures
General Work Stress Scale [GWSS: (60); Turkish version: (61)]. The GWSS was developed to measure one’s general work stress level. The scale includes 9 items (e.g., Have you ever lost your temper due to stress at work? or When you are stressed at work, do you forget to complete important tasks?), and all items are rated on a 5-point Likert scale type ranging from 1 (Never) to 5 (Every time). The higher the score, the greater the level of general work stress. Cronbach’s α was 0.91, and McDonald’s ω was 0.91, in this study.
Suicide Cognitions Scale [SCS: (Rudd et al., unpublished)1; Turkish version: (62)]. The BRS was developed to measure one’s suicide cognitions. The scale includes 18 items (e.g., My only solution to my problems is to end my life. Or I would rather die right now than endure this unbearable pain). The higher the score on the scale, the greater the level of suicide cognition. Cronbach’s α was 0.95, and McDonald’s ω was 0.95, in this study.
Beck Hopelessness Scale [BHS: (63, 64)]. The BHS was developed to measure one’s hopelessness level by using 20 items including true and false propositions (e.g., As I cannot change myself, it is best to stop trying. Or Even when something goes wrong, it is comforting to know that things will not always remain the same). Higher scores on the scale indicate greater hopelessness. Cronbach’s α was 0.75, and McDonald’s ω was 0.75, in this study.
Job Satisfaction Scale [JSS: (65); Turkish version: (66)]. The BRS was developed to measure positive emotional state resulting from the subjective perception of the person’s work experiences. The scale includes 5 items ranging from 1 (Strongly disagree) to 5 (Strongly agree) (e.g., My job is enjoyable to me. Or My current job is very satisfying to me). A higher score on the scale indicates, a higher level of suicide cognition. In this study, Cronbach’s α was 0.81, and McDonald’s ω was 0.81.
Procedures
We followed the Declaration of Helsinki at all stages of the study. We used an online survey to collect data. The online survey provided participants with a brief explanation of the study’s purpose. Health-care professionals working at different hospitals in Turkey received an invitation text/email containing study information and an informed consent form. It provided information about the study, including its objectives and duration, assurances of anonymity and confidentiality, and voluntary participation in the study. Additionally, the survey is stated to be limited to one completion per participant. The questionnaires were administered only after informed consent had been obtained from the participants. Participants in the study were asked whether they would be willing to participate voluntarily. Those who indicated that they had not participated in the study voluntarily were not permitted to continue. There was a warning to participants that if they did not wish to fill out the questionnaires or if they did not feel comfortable, they could leave at any time during the research. Participants were eligible for inclusion if they were over 18 years of age, participating voluntarily, and were health workers. To avoid trust problems that may arise during the answering process on the scales, they have been asked not to enter their personal information into the online form. The confidentiality and anonymity of the responses were assured. Since the research subject was suicide cognitions, some participants did not want to complete questionnaires. We did not include in the study those participants who refused to participate.
Data analysis
A number of assumptions, including multicollinearity and normality, were tested before the primary analysis was conducted. The skewness and kurtosis statistics were calculated in order to test the assumption of normality. The Variance inflation factor (VIF), Tolerance statistics, and Condition index have been computed to test the multicollinearity assumption. There should be a tolerance value of less than 0.2, a VIF value of less than 10, and a condition index of less than 15 (67, 68). A Mahalanobis distance was calculated to remove outliers, and it was determined that 23 participants should be removed from the data set as a result of the analysis. Outliers are often detected by using a technique called Mahalanobis distance (69, 70). After examining the preliminary analysis, we tested a parallel mediation model to determine whether hopelessness and job satisfaction mediated the relationship between general work stress and suicide cognitions. A confidence interval of 95% was used to explain the indirect effects of the proposed model (71). In order to test whether indirect effects were significant, bias-corrected bootstrapping procedures were applied. The bootstrap value was set to 10,000. We analyzed all of the data using SPSS 26.0 and used the R-based Jamovi 1.6.23 (The Jamovi Project, 2022) in conjunction with the jAMM module for the mediation analysis (72).
Results
Table 1 presents participants’ demographic details, including means (M) and standard deviations (SD) for the variables. An independent sample t-test was performed to compare the general work stress, suicidal cognitions, hopelessness, and job satisfaction by gender, marital status, and Covid-19 experience. General work stress, suicidal cognitions, hopelessness, and job satisfaction did not differ significantly based on gender and Covid-19 experience. There were statistically significant differences in general work stress, hopelessness, and job satisfaction for single health-care staff compared with those who were married (35.41 vs. 40.66).
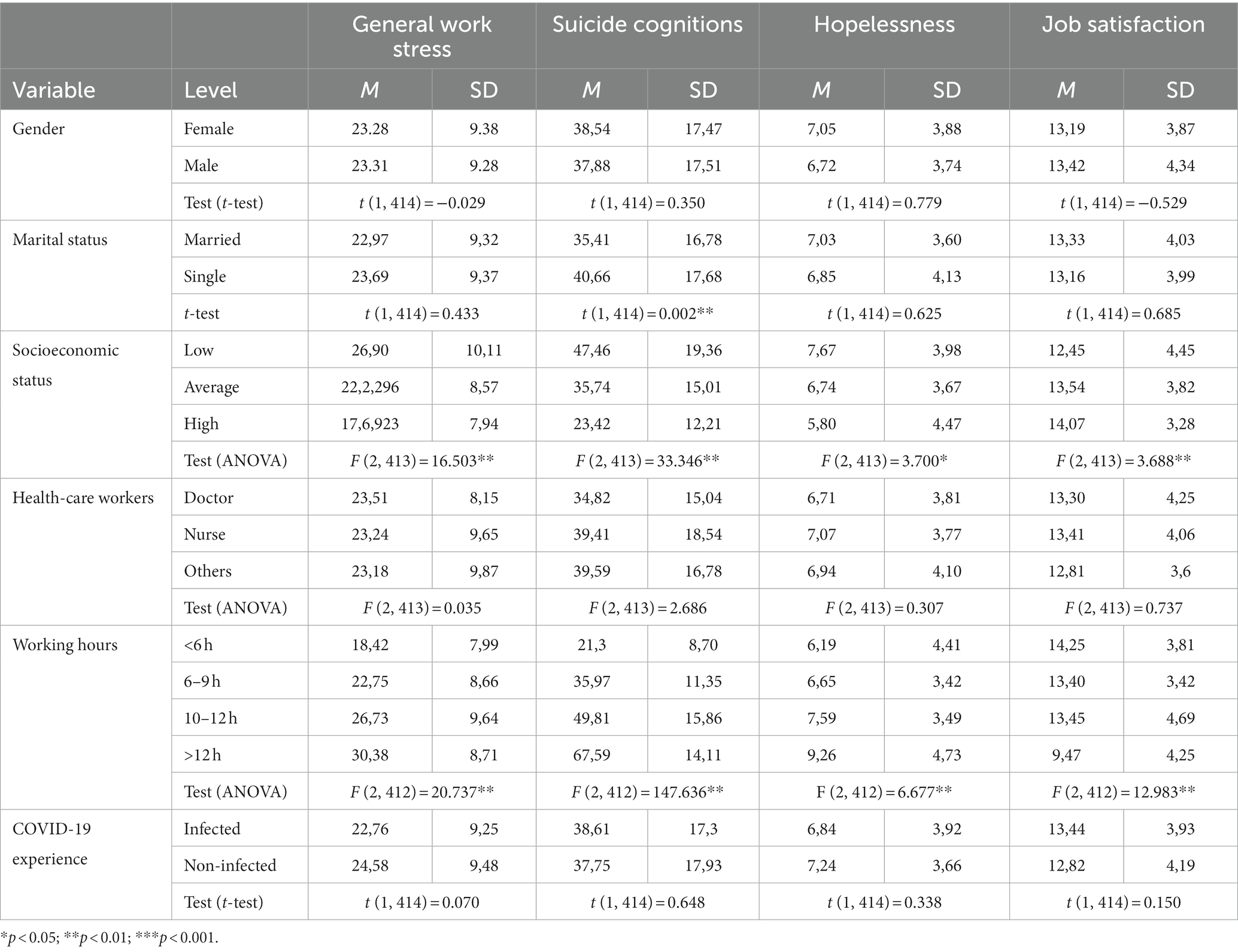
Table 1. Demographic characteristics of the sample and descriptive characteristics of scales (N = 416).
One-way ANOVA was used to examine general work stress, suicidal cognitions, hopelessness, and job satisfaction by socioeconomic status, occupation, and working hours (see Table 1). There were statistically significant differences between group means concerning socioeconomic status and working hours, while there were no differences in occupation. In order to reveal the source of the difference, a Tukey post-hoc test was conducted. The results indicated that low (26.90 ± 10.11), and average socioeconomic status (22.23 ± 8.57) had more general work stresses than high socioeconomic status (17.69 ± 7.95). Low (47.46 ± 19.36), and average socioeconomic status (35.74 ± 15.01) had more suicide cognitions than high socioeconomic status (23.42 ± 12.22). Moreover, low socioeconomic status (7.67 ± 3.99) had more hopelessness than high socioeconomic status (5.80 ± 4.47). To detect the difference of source for working hours, a Tukey post hoc test was conducted. According to the results, the general work stress of healthcare workers who work over 12 h (30.38 ± 8.70), between 10 and 12 h (26.73 ± 9.64), and between 6 and 9 h (22.74 ± 8.66) was significantly higher than that of those who work less than 6 h (18.42 ± 7.99). The level of suicide cognitions of health care workers working more than 12 h (67.59 ± 14.10), between 9 and 12 h (49.80 ± 15.85), between 6 and 9 h (35.97 ± 11.34), was significantly higher than those working less than 6 h (21.29 ± 8.69). The hopelessness of health-care workers working more than 12 h (9.26 ± 4.25), was significantly higher than those working less than 6 h (6.16 ± 4.40). Besides, the level of job satisfaction of health-care workers working less than 6 h (14.25 ± 3.80), was significantly higher than those working more than 12 h (9.47 ± 4.25).
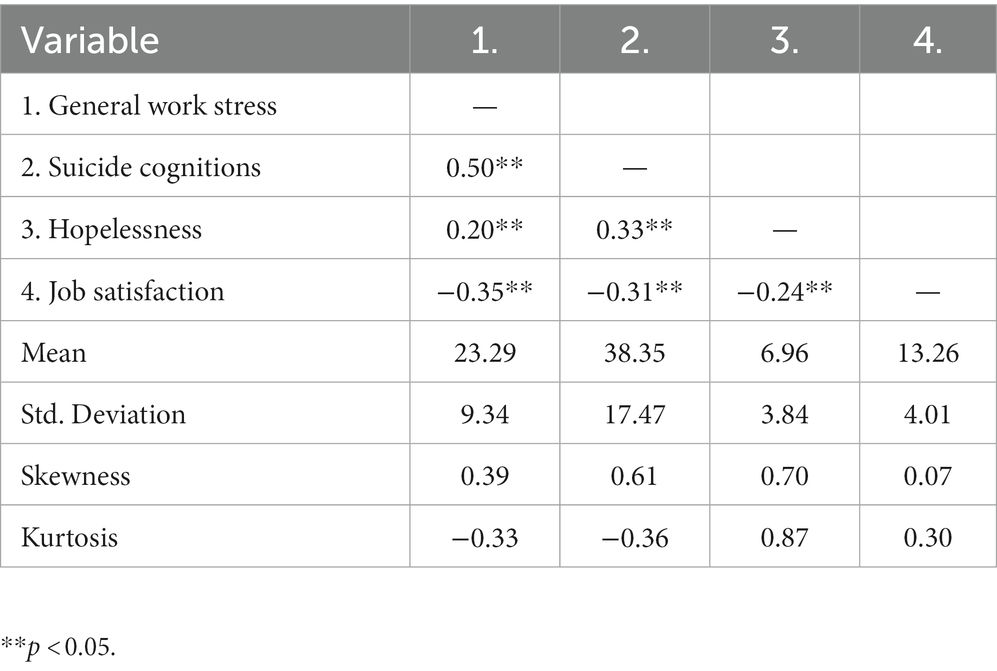
Table 2 presents descriptive statistics and correlation coefficients among the variables included in the study. These variables’ skewness and kurtosis values fall within the acceptable normal distribution range of the proposed threshold value of ±2; therefore, we did not find evidence that the normality assumption had been violated (73). The correlation analysis revealed that general work stress positively and significantly negatively correlated with suicide cognitions and hopelessness, indicating that one variable changes in the same direction as the other. All variables were found to be either low or moderately correlated, according to the study results.
Mediation analysis
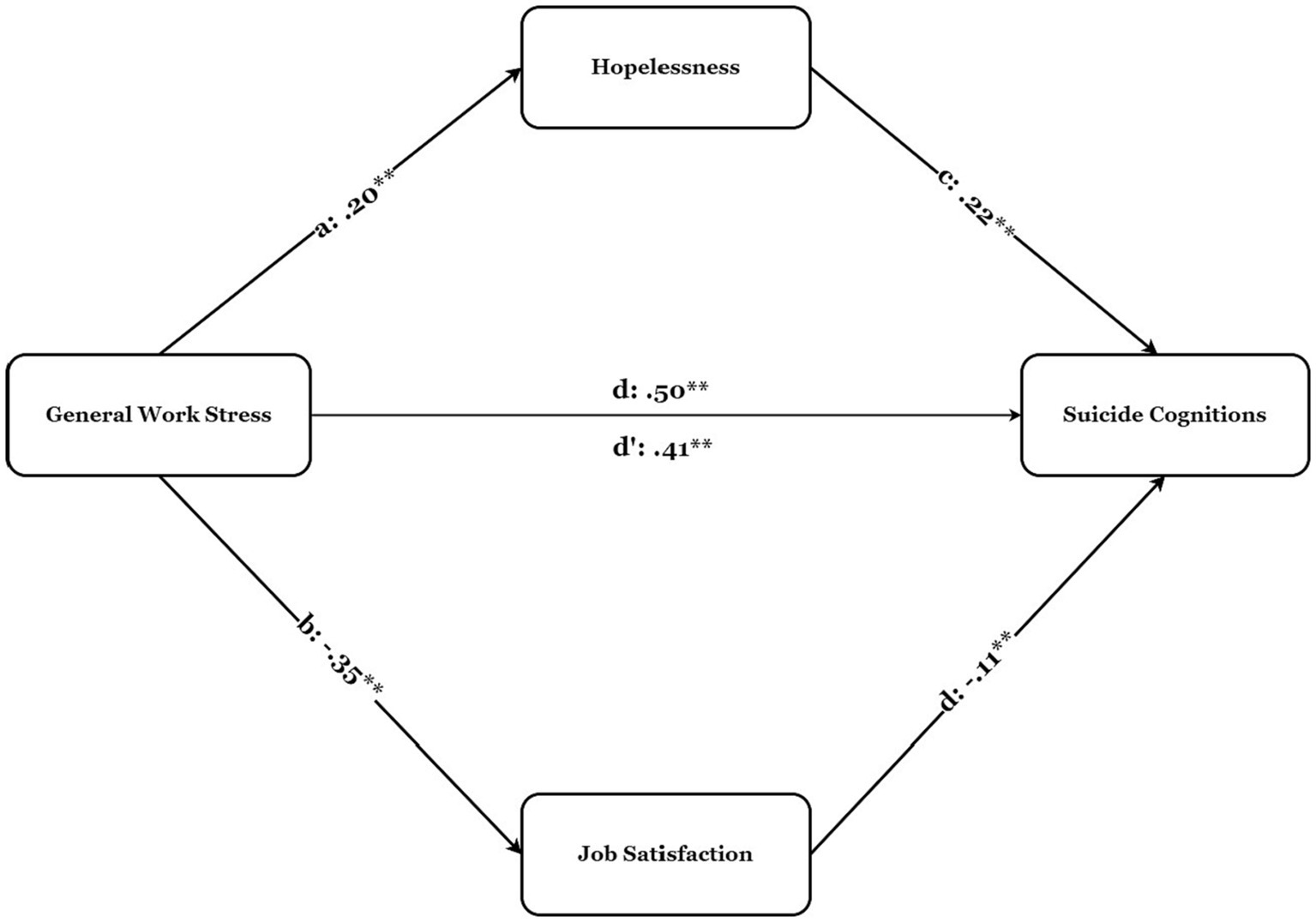
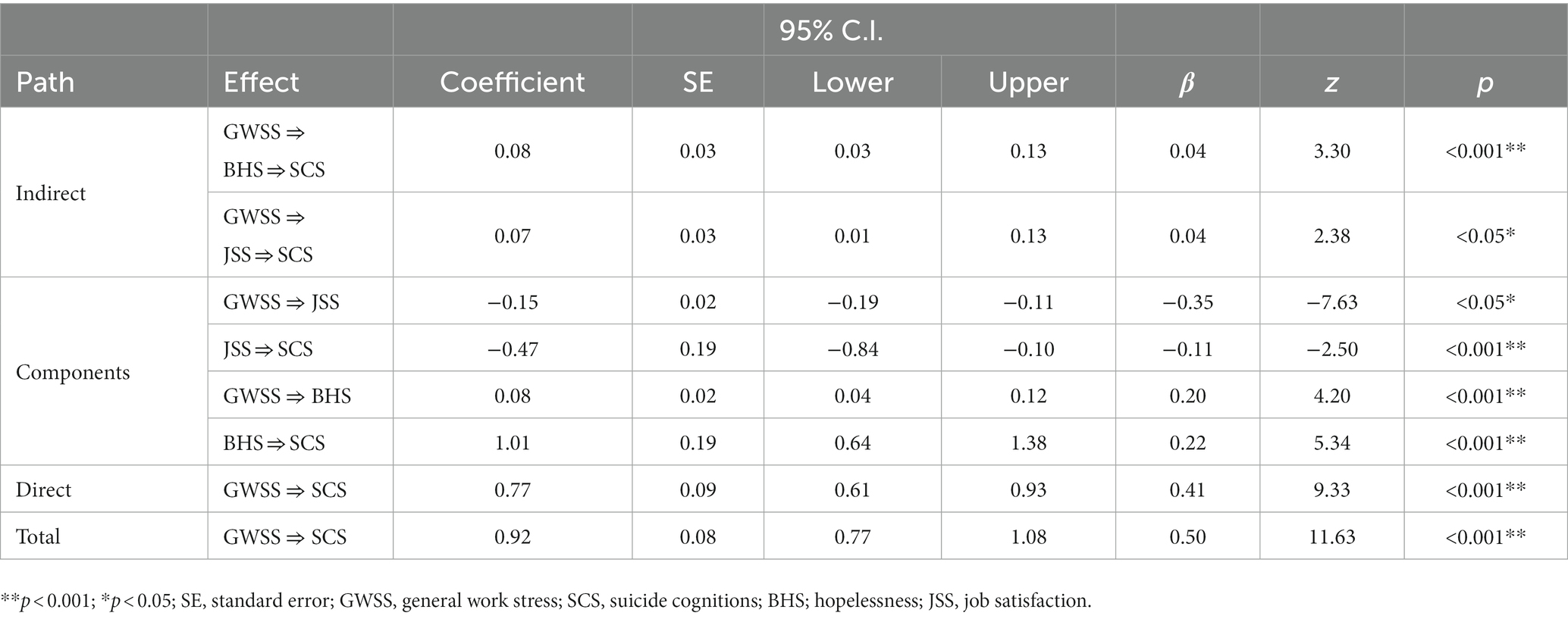
The mediation analysis results are presented in Table 2 and Figure 2. A direct relationship of general work stress on suicide cognitions (total, β = 0.50, p < 0.001) was found. General work stress also had a positive relationship with hopelessness (direct effect, β = 0.20, p < 0.001). It was also a negative relationship with job satisfaction (direct, β = −0.35, p < 0.001). Hypothesis 1 was confirmed based on the results obtained. Path coefficients were examined to examine the relationship between hopelessness and suicide cognitions, and the results indicated that hopelessness had a relationship with suicide cognitions (direct, β = 0.22, p < 0.001). Moreover, job satisfaction also had a relationship with suicide cognitions (direct, β = −0.11, p < 0.001). Hypothesis 2 was confirmed based on the results obtained. The results showed that this coefficient remained significant when mediators were included in the analysis (i.e., hopelessness and job satisfaction) (direct, β = 0.41, p < 0.001). General work stress had a significant indirect relationship with suicide cognitions through hopelessness [indirect = 0.08, SE = 0.03, 95% CI = (0.03, 0.13)]. Furthermore, General work stress had a significant indirect relationship with suicide cognitions through job satisfaction [indirect = 0.07, SE = 0.03, 95% CI = (0.01, 0.13)]. The results indicated that the relationship between general work stress and suicide cognitions was parallelly mediated by hopelessness and job satisfaction. Hypothesis 3 was confirmed based on the results obtained (Table 3).
Discussion
This study aimed to explore the influence of general work stress on suicide cognitions and its potential mediating mechanisms of job satisfaction and hopelessness. As hypothesized, the results of this study demonstrated that general work stress significantly and negatively predicts job satisfaction, while it significantly and positively predicts hopelessness and suicide cognitions. This confirms the first research hypothesis. These results are consistent with the results of previous studies, showing the positive associations between general work stress and suicide cognition (74–76). Considerable job-related stress and are more prone to exhibit a variety of psychological disorders, such as PTSD and suicidal thoughts (77). The greatest rates of psychological distress were recorded among nurses, women workers, frontline health-care workers, younger medical personnel, and employees in locations with higher infection rates, according to a systematic analysis analyzing the mental health concerns among health-care workers after the pandemic (78). Related research has proposed a 7-factor model linking PTSD to elevated suicide risk (79). Another research found that health-care workers were more likely to have mental health problems after exposure to long and irregular work hours (80). In the study of Rahman and Plummer (81), factors associated with nurses’ mental stress and the consequences of suicide were identified. These studies’ findings indicate a strong association between general work stress and suicide cognition.
Researchers examined the path coefficients between hopelessness and suicidal cognitions and found that the former was significantly significant. Accordingly, hopelessness had a mediating effect on the relationship between general work stress and suicide cognitions. The findings support the second hypothesis. When a person engages in ruminative, negative thought patterns, they are more likely to develop hopelessness or suicide cognitions (82, 83), and suicide attempts among those suffering from depression are frequently triggered by hopelessness (84). Therefore, suicide-specific (e.g., poor life-affirming) cognitions may be important in figuring out the associations between depression and despair and suicidal thoughts and actions (85). Although hopelessness and suicide cognitions are positively correlated, some studies have shown that certain practices can boost job satisfaction and reduce negative thoughts, including suicide cognitions (86, 87).
The coefficient remained statistically significant even after adding hopelessness and job satisfaction as mediators. In terms of suicidal cognitions, hopelessness was a major factor associated with general work stress. Moreover, job satisfaction was a strong mediator between general work stress and suicidal ideation. Both feelings of hopelessness and job satisfaction were found to mediate the link between general work stress and suicidal thoughts. As a result of the analysis, the third hypothesis is supported. Consequently, health-care workers with higher levels of work stress and hopelessness but lower levels of job satisfaction tend to have more suicide cognitions. This can lead to a decrease in focus and concentration, as well as productivity and efficiency. It can also lead to increased negative emotions such as anxiety and depression. Ultimately, this can affect health-care workers’ quality of care. Much recent research revealed the relationship between stress and suicide cognitions (88–90), and there are studies giving the association between suicide cognitions and negative thoughts like hopelessness (91–93).
Implications
The present study significantly advances our understanding of the relationship between general work stress and suicide cognitions by showing the mediating roles played by hopelessness and job satisfaction in this relationship. The findings of this study demonstrated the pivotal significance of hopelessness and job satisfaction in dealing with the mental well-being of health-care workers within the workplace context. General work stress increases hopelessness and reduces job satisfaction, which in turn increases suicide cognitions. As higher hopelessness and lower job satisfaction were associated with higher general work stress and suicide cognitions, it is important that hospitals tailor training programs to improve the capacity of health-care workers to effectively cope with stressors and provide better care for patients. The results highlight the need for hospitals and health-care institutions for tailored training programs. These programs should aim to contribute to the coping mechanisms of health-care workers, enabling them to deal with stressors effectively and deliver better care for patients. Such training interventions can be executed through diverse ways, including both conventional face-to-face sessions and contemporary virtual platforms, including social media channels, webinars, and video technologies.
Limitations
While this study enhances our understanding of the associations between general work stress, suicide cognitions, hopelessness, and job satisfaction, it is not exempt from limitations. The cross-sectional design restricts our ability to establish causality among the variables. To address this, future studies could benefit from incorporating longitudinal designs by collecting data at multiple time points to account for dynamic processes influencing the results. Furthermore, the sample demographic characteristics, including age, gender, and socioeconomic status, may have introduced confounding variables. It is important to consider these variables when interpreting the findings. Further research is warranted to validate the results. Additionally, the study relied on online survey data collection, which is susceptible to selection bias and exclusion of participants without internet access due to factors like affordability and accessibility. Therefore, generalizing these findings to the entire population may be challenging. Future studies should aim for a more representative sample, ensuring equal gender representation among health-care workers.
Conclusion
In conclusion, this study contributes to the growing body of literature indicating that various psychological factors, both positive and negative, including hopelessness and job satisfaction, play important roles in influencing suicide cognitions among health-care workers. These findings hold implications for the development and implementation of targeted interventions aimed at addressing factors associated with suicide cognitions. Therefore, these results underscore the significance of hospital-based prevention and intervention services designed to mitigate hopelessness, enhance job satisfaction, and consequently, alleviate the impact of general work stress and suicide cognitions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ağrı İbrahim Çeçen University Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AS: Writing – original draft, Writing – review & editing, Project administration. AK: Project administration, Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software. IA: Writing – review & editing. MY: Conceptualization, Writing – original draft, Writing – review & editing, Supervision, Validation. HÖ: Conceptualization, Data curation, Software, Writing – review & editing. FC: Writing – review & editing. SZ: Funding acquisition, Writing – review & editing.
Funding
This work was supported by the Italian Ministry of Health with Current Research Funds.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
1. ^Rudd MD, Schmitz B, McClenen R, Joiner T, Elkins G, Claassen C. The suicide cognitions scale: a suicide-specific measure of hopelessness. J Abnorm Psychol. (unpublished).
References
1. Rotenstein, LS , Torre, M , Ramos, MA , Rosales, RC , Guille, C , Sen, S, et al. Prevalence of burnout among physicians. JAMA. (2018) 320:1131. doi: 10.1001/jama.2018.12777
2. Yinghao, Z , Dan, Z , Qi, L , Yu, W , Xiaoying, W , Ao, F, et al. A cross-sectional study of clinical emergency department nurses’ occupational stress, job involvement and team resilience. Int Emerg Nurs. (2023) 69:101299. doi: 10.1016/j.ienj.2023.101299
3. Jadidi, A , Irannejad, B , Salehi, M , and Safarabadi, M . Effect of stachys lavandulifolia on occupational stress in emergency medical technicians. Explore. (2023). doi: 10.1016/j.explore.2023.04.003 (in press).
4. Feskanich, D , Hastrup, JL , Marshall, JR , Colditz, GA , Stampfer, MJ , Willett, WC, et al. Stress and suicide in the Nurses' health study. J Epidemiol Comm Health. (2002) 56:95–8. doi: 10.1136/jech.56.2.95
5. Mengist, B , Amha, H , Ayenew, T , Gedfew, M , Akalu, TY , Assemie, MA, et al. Occupational stress and burnout among health care workers in Ethiopia: a systematic review and meta-analysis. Arch Rehabil Res Clin Transl. (2021) 3:100125. doi: 10.1016/j.arrct.2021.100125
6. Gerding, T , Davis, KG , and Wang, J . An investigation into occupational related stress of at-risk workers during COVID-19. Ann Work Expo Health. (2022) 67:118–28. doi: 10.1093/annweh/wxac076
7. Michie, S . Causes and management of stress at work. Occup Environ Med. (2002) 59:67–72. doi: 10.1136/oem.59.1.67
8. Mitchelson, JK , and Burns, LR . Career mothers and perfectionism: stress at work and at home. Personal Individ Differ. (1998) 25:477–85. doi: 10.1016/s0191-8869(98)00069-5
9. Batmaz, H , Türk, N , and Doğrusever, C . The mediating role of hope and loneliness in the relationship between meaningful life and psychological resilience in the covid-19 pandemic. Anemon Muş Alparslan Üniversitesi Sosyal Bilimler Dergisi. (2021) 9:1403–20. doi: 10.18506/anemon.895199
10. Kiziloğlu, B , and Karabulut, N . The effect of personality traits of surgical nurses on COVID-19 fear, work stress and psychological resilience in the pandemic. J Perianesth Nurs. (2023) 38:572–8. doi: 10.1016/j.jopan.2022.10.006
11. Groves, S , Lascelles, K , and Hawton, K . Suicide, self-harm, and suicide ideation in nurses and midwives: a systematic review of prevalence, contributory factors, and interventions. J Affect Disord. (2023) 331:393–404. doi: 10.1016/j.jad.2023.03.027
12. Lin, W , Wang, H , Gong, L , Lai, G , Zhao, X , Ding, H, et al. Work stress, family stress, and suicide ideation: a cross-sectional survey among working women in Shenzhen, China. J Affect Disord. (2020) 277:747–54. doi: 10.1016/j.jad.2020.08.081
13. Loerbroks, A , Cho, S-I , Dollard, MF , Zou, J , Fischer, JE , Jiang, Y, et al. Associations between work stress and suicidal ideation: individual-participant data from six cross-sectional studies. J Psychosom Res. (2016) 90:62–9. doi: 10.1016/j.jpsychores.2016.09.008
14. Xiao, J , Guan, S , Ge, H , Tao, N , Zhang, Y , Jiang, Y, et al. The impact of changes in work stressors and coping resources on the risk of new-onset suicide ideation among Chinese petroleum industry workers. J Psychiatr Res. (2017) 88:1–8. doi: 10.1016/j.jpsychires.2016.12.014
15. Siegrist, J . Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. (1996) 1:27–41. doi: 10.1037/1076-8998.1.1.27
16. Siegrist, J , Starke, D , Chandola, T , Godin, I , Marmot, M , Niedhammer, I, et al. The measurement of effort–reward imbalance at work: European comparisons. Soci Sci Med. (2004) 58:1483–99. doi: 10.1016/s0277-9536(03)00351-4
17. Bathman, LM , Almond, J , Hazi, A , and Wright, BJ . Effort–reward imbalance at work and pre-clinical biological indices of ill-health: the case for salivary immunoglobulin a. Brain Behav Immun. (2013) 33:74–9. doi: 10.1016/j.bbi.2013.05.010
18. Li, J , Loerbroks, A , and Siegrist, J . Effort–reward imbalance at work, parental support, and suicidal ideation in adolescents: a cross-sectional study from Chinese dual-earner families. Saf Health Work. (2017) 8:77–83. doi: 10.1016/j.shaw.2016.09.003
19. Zhuo, L-B , Yao, W , Yan, Z , Giron, MST , Pei, J-J , and Wang, H-X . Impact of effort reward imbalance at work on suicidal ideation in ten European countries: the role of depressive symptoms. J Affect Disord. (2020) 260:214–21. doi: 10.1016/j.jad.2019.09.007
20. Choflet, A , Davidson, J , Lee, KC , Ye, G , Barnes, A , and Zisook, S . A comparative analysis of the substance use and mental health characteristics of nurses who complete suicide. J Clin Nurs. (2021) 30:1963–72. Portico. doi: 10.1111/jocn.15749
21. Montemurro, N . The emotional impact of COVID-19: from medical staff to common people. Brain Behav Immun. (2020) 87:23–4. doi: 10.1016/j.bbi.2020.03.032
22. Stelnicki, AM , Jamshidi, L , Angehrn, A , and Nicholas Carleton, R . Suicidal behaviors among nurses in Canada. Can J Nurs Res. (2020) 52:226–36. doi: 10.1177/0844562120934237
23. Lin, P , Chen, C , Pan, S , Chen, Y , Pan, C , Hung, H, et al. The association between rotating shift work and increased occupational stress in nurses. J Occup Health. (2015) 57:307–15. Portico. doi: 10.1539/joh.13-0284-oa
24. Godifay, G , Worku, W , Kebede, G , Tafese, A , and Gondar, E . Work related stress among health care workers in Mekelle City administration public hospitals, North Ethiopia. Work. (2018) 46:189–95.
25. Locke, EA . The natüre and causes of job satisfaction In: Dunnette MD editor. Handbook of industrial and organizational psychology. Chicago: Rand McNally (1976). 360–581.
26. Fadare, OO , Witry, MJ , Gaither, CA , Doucette, WR , and Schommer, JC . What drives job satisfaction among community pharmacists? An application of relative importance analysis. Explor Res Clin Soc Pharm. (2023) 9:100237. doi: 10.1016/j.rcsop.2023.100237
27. Keser, A , and Öngen Bilir, KB . İş Tatmini Ölçeğinin Türkçe Güvenilirlik Ve Geçerlilik Çalışması. Kırklareli Üniversitesi Sosyal Bilimler Dergisi. (2019) 3:229–39.
28. Chowdhury, SR , Kabir, H , Akter, N , Iktidar, MA , Roy, AK , Chowdhury, MR, et al. Impact of workplace bullying and burnout on job satisfaction among Bangladeshi nurses: a cross-sectional study. Heliyon. (2023) 9:e13162. doi: 10.1016/j.heliyon.2023.e13162
29. Peters, DH , Chakraborty, S , Mahapatra, P , and Steinhardt, L . Job satisfaction and motivation of health workers in public and private sectors: cross-sectional analysis from two Indian states. Hum Resour Health. (2010) 8:1–11. doi: 10.1186/1478-4491-8-27
30. Chaulagain, N , and Khadka, DK . Factors influencing job satisfaction among health-care professionals at Tilganga eye Centre, Kathmandu. Nepal Age. (2012) 35:74–67.
31. El Amri, I , and Benali, B . Job satisfaction among doctors in Morocco. Saf Health Work. (2022) 13:S221. doi: 10.1016/j.shaw.2021.12.1442
32. Pawlowski, P , Labuz-Roszak, B , and Niewiadomska, E . Life satisfaction and job satisfaction among doctors in the Silesian Province Poland. J Neurol Sci. (2019) 405:67. doi: 10.1016/j.jns.2019.10.894
33. Ramirez, AJ , Graham, J , Richards, MA , Gregory, WM , and Cull, A . Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet. (1996) 347:724–8. doi: 10.1016/s0140-6736(96)90077-x
34. Bailey, E , Robinson, J , and McGorry, P . Depression and suicide among medical practitioners in Australia. Intern Med J. (2018) 48:254–8. Portico. doi: 10.1111/imj.13717
35. Huang, JZ , Han, MF , Luo, TD , Ren, AK , and Zhou, XP . Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. (2020) 35:192–5. doi: 10.3760/cma.j.cn121094-20200219-00063
36. Lai, J , Ma, S , Wang, Y , Cai, Z , Hu, J , Wei, N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
37. Luo, M , Guo, L , Yu, M , Jiang, W , and Wang, H . The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – a systematic review and meta-analysis. Psychiatry Res. (2020) 291:113190. doi: 10.1016/j.psychres.2020.113190
38. Ornell, F , Halpern, SC , Kessler, FHP , and de Magalhães Narvaez, JC . The impact of the COVID-19 pandemic on the mental health of health-care professionals. Cad Saude Publica. (2020) 36:e00063520. doi: 10.1590/0102-311x00063520
39. Shaukat, N , Ali, DM , and Razzak, J . Physical and mental health impacts of COVID-19 on health-care workers: a scoping review. International. J Emerg Med. (2020) 13:40. doi: 10.1186/s12245-020-00299-5
40. Karadag, E , Parlar Kilic, S , Ugur, O , and Akyol, MA . Attitudes of nurses in Turkey toward care of dying individual and the associated religious and cultural factors. J Relig Health. (2018) 58:303–16. doi: 10.1007/s10943-018-0657-4
41. Zhang, Y , Kuang, D , Zhang, B , Liu, Y , Ren, J , Chen, L, et al. Association between hopelessness and job burnout among Chinese nurses during the COVID-19 epidemic: the mediating role of career calling and the moderating role of social isolation. Heliyon. (2023) 9:e16898. doi: 10.1016/j.heliyon.2023.e16898
42. Chen, Q , Liang, M , Li, Y , Guo, J , Fei, D , Wang, L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e15–6. doi: 10.1016/s2215-0366(20)30078-x
43. Hacimusalar, Y , Kahve, AC , Yasar, AB , and Aydin, MS . Anxiety and hopelessness levels in COVID-19 pandemic: a comparative study of health-care professionals and other community sample in Turkey. J Psychiatr Res. (2020) 129:181–8. doi: 10.1016/j.jpsychires.2020.07.024
44. Mehta, S , Machado, F , Kwizera, A , Papazian, L , Moss, M , Azoulay, É, et al. COVID-19: a heavy toll on health-care workers. Lancet Respir Med. (2021) 9:226–8. doi: 10.1016/s2213-2600(21)00068-0
45. Pappa, S , Ntella, V , Giannakas, T , Giannakoulis, VG , Papoutsi, E , and Katsaounou, P . Prevalence of depression, anxiety, and insomnia among health-care workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
46. Liao, T , Meng, D , Xiong, L , Wu, S , Yang, L , Wang, S, et al. Long-term effects of Covid-19 on health care workers 1-year post-discharge in Wuhan. Infect Dis Ther. (2021) 11:145–63. doi: 10.1007/s40121-021-00553-0
47. Pompili, M , Rinaldi, G , Lester, D , Girardi, P , Ruberto, A , and Tatarelli, R . Hopelessness and suicide risk emerge in psychiatric nurses suffering from burnout and using specific defense mechanisms. Arch Psychiatr Nurs. (2006) 20:135–43. doi: 10.1016/j.apnu.2005.12.002
48. Yuan, L , Li, Y , Yan, H , Xiao, C , Liu, D , Liu, X, et al. Effects of work-family conflict and anxiety in the relationship between work-related stress and job burnout in Chinese female nurses: a chained mediation modeling analysis. J Affect Disord. (2023) 324:309–16. doi: 10.1016/j.jad.2022.12.112
49. Shea, F , and Hurley, E . Hopelessness and helplessness. Perspect Psychiatr Care. (1964) 2:32–8. doi: 10.1111/j.1744-6163.1964.tb01391.x
50. Chang, EC . Hope and hopelessness as predictors of suicide ideation in Hungarian college students. Death Stud. (2017) 41:455–60. doi: 10.1080/07481187.2017.1299255
51. Marsiglia, FF , Kulis, S , Perez, HG , and Bermudez-Parsai, M . Hopelessness, family stress, and depression among mexican-heritage mothers in the southwest. Health Soci Work. (2011) 36:7–18. doi: 10.1093/hsw/36.1.7
52. Abramson, LY , Alloy, LB , Hogan, ME , Whitehouse, WG , Gibb, BE , Hankin, BL, et al. The hopelessness theory of suicidality. Suicide Sci. (2002) 17–32. doi: 10.1007/0-306-47233-3_3
53. Abramson, LY , Metalsky, GI , and Alloy, LB . Hopelessness depression: a theory-based subtype of depression. Psychol Rev. (1989) 96:358–72. doi: 10.1037/0033-295x.96.2.358
54. Kim, S-Y , Shin, Y-C , Oh, K-S , Shin, D-W , Lim, W-J , Cho, SJ, et al. Association between work stress and risk of suicidal ideation: a cohort study among Korean employees examining gender and age differences. Scand J Work Environ Health. (2020) 46:198–208. doi: 10.5271/sjweh.3852
55. Narita, Z , Okubo, R , Sasaki, Y , Takeda, K , Ohmagari, N , Yamaguchi, K, et al. Association of COVID-19-related discrimination with subsequent depression and suicidal ideation in health-care workers. J Psychiatr Res. (2023) 159:153–8. doi: 10.1016/j.jpsychires.2023.01.025
56. Ozdemir, O , Boysan, M , Guzel Ozdemir, P , and Yilmaz, E . Relationships between posttraumatic stress disorder (PTSD), dissociation, quality of life, hopelessness, and suicidal ideation among earthquake survivors. Psychiatry Res. (2015) 228:598–605. doi: 10.1016/j.psychres.2015.05.045
57. Polanco-Roman, L , and Miranda, R . Culturally related stress, hopelessness, and vulnerability to depressive symptoms and suicidal ideation in emerging adulthood. Behav Ther. (2013) 44:75–87. doi: 10.1016/j.beth.2012.07.002
58. Salma, U , and Hasan, MM . Relationship between job satisfaction and depression, anxiety and stress among the female nurses of Dhaka medical college and hospital. Bangladesh Patient Care. (2020) 20:21. doi: 10.5923/j.phr.20201003.02
60. De Bruin, GP . The dimensionality of the general work stress scale: a hierarchical exploratory factor analysis. SA J Ind Psychol. (2006) 32:68–75. doi: 10.4102/sajip.v32i4.250
61. Teleş, M . Validity and reliability of the Turkish version of the general work stress scale. J Nurs Manag. (2021) 29:710–20. doi: 10.1111/jonm.13211
62. Yiğit, MG , and Yiğit, İ . İntihar Bilişleri Ölçeğinin psikometrik özelliklerinin değerlendirilmesi: Geçerlik ve güvenirlik çalışması. Nesne Psikoloji Dergisi. (2017) 5:363–83. doi: 10.7816/nesne-05-11-02
63. Beck, AT , Weissman, A , Lester, D , and Trexler, L . The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. (1974) 42:861–5. doi: 10.1037/h0037562
64. Durak, A , and Palabıyıkoğlu, R . Beck Umutsuzluk ölçeği geçerlilik çalişmasi. Kriz dergisi. (1994) 2:311–9. doi: 10.1501/0000831
65. Judge, TA , Locke, EA , Durham, CC , and Kluger, AN . Dispositional effects on job and life satisfaction: the role of core evaluations. J Appl Psychol. (1998) 83:17–34. doi: 10.1037/0021-9010.83.1.17
66. Keser, A , and Bilir, KBÖ . İş tatmini ölçeğinin türkçe güvenilirlik ve geçerlilik çalişması. Kırklareli Üniversitesi Sosyal Bilimler Dergisi. (2019) 3:229–39.
67. Albayrak, AS . Çoklu doğrusal bağlantı halinde enküçük kareler tekniğinin alternatifi yanlı tahmin teknikleri ve bir uygulama. ZKÜ Sosyal Bilimler Dergisi. (2005) 1:105–26.
68. Shrestha, N . Detecting multicollinearity in regression analysis. Am J Appl Math Stat. (2020) 8:39–42. doi: 10.12691/ajams-8-2-1
69. Leys, C , Klein, O , Dominicy, Y , and Ley, C . Detecting multivariate outliers: use a robust variant of the Mahalanobis distance. J Exp Soc Psychol. (2018) 74:150–6. doi: 10.1016/j.jesp.2017.09.011
70. Tabachnick, B. G. , Fidell, L. S. , and Ullman, J. B. (2007). Using multivariate statistics 5, 481–498. Boston, MA: Pearson.
71. Preacher, KJ , and Hayes, AF . SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. (2004) 36:717–31. doi: 10.3758/BF03206553
72. Gallucci, M. (2022). jAMM: jamovi advanced mediation models. [jamovi module]. Available at: https://jamovi-amm.github.io/
73. George, D . SPSS for windows step by step: a simple study guide and reference, 17.0 update, 10/e. Boston: Pearson (2010).
74. Ahn, SH , Lee, YJ , Jang, EC , Kwon, SC , Min, YS , and Ryu, SH . A study of job stress, suicidal ideation and suicide attempts in display manufacturing workers: a cross-sectional study. Annals Occup Environ Med. (2020) 32:e16. doi: 10.35371/aoem.2020.32.e16
75. Milner, A , Spittal, MJ , Pirkis, J , and LaMontagne, AD . Suicide by occupation: systematic review and meta-analysis. Br J Psychiatry. (2018) 212:357–65. doi: 10.1192/bjp.bp.113.128405
76. Tahernejad, S , Ghaffari, S , Ariza-Montes, A , Wesemann, U , Farahmandnia, H , and Sahebi, A . Post-traumatic stress disorder in medical workers involved in earthquake response: a systematic review and meta-analysis. Heliyon. (2023) 9:e12794. doi: 10.1016/j.heliyon.2023.e12794
77. Vizheh, M , Qorbani, M , Arzaghi, SM , Muhidin, S , Javanmard, Z , and Esmaeili, M . The mental health of health-care workers in the COVID-19 pandemic: a systematic review. J Diabetes Metab Disord. (2020) 19:1967–78. doi: 10.1007/s40200-020-00643-9
78. Naushad, VA , Bierens, JJ , Nishan, KP , Firjeeth, CP , Mohammad, OH , and Maliyakkal, AM . A systematic review of the impact of disaster on the mental health of medical responders. Prehosp Disaster Med. (2019) 34:632–43. doi: 10.1017/S1049023X19004874
80. Rahman, A , and Plummer, V . COVID-19 related suicide among hospital nurses; case study evidence from worldwide media reports. Psychiatry Research. (2020) 291:113272. doi: 10.1016/j.psychres.2020.113272
81. Batmaz, H , Türk, N , Kaya, A , and Yıldırım, M, Research Assistant . Cyberbullying and cyber victimization: examining mediating roles of empathy and resilience. Curr Psychol. (2022) 1-11:1–11. doi: 10.1007/s12144-022-04134-3
82. Flores-Kanter, PE , García-Batista, ZE , Moretti, LS , and Medrano, LA . Towards an explanatory model of suicidal ideation: the effects of cognitive emotional regulation strategies, affectivity and hopelessness. Span J Psychol. (2019) 22:E43. doi: 10.1017/sjp.2019.45
83. Shareh, H , and Robati, Z . Effect of acceptance and commitment group therapy on cognitive flexibility, suicidal ideation, depression, and hopelessness in conscripts. Iran J Psychiatr Clinical Psychol. (2022) 27:412–27. doi: 10.32598/ijpcp.27.2.225.12
84. Bagge, CL , Lamis, DA , Nadorff, M , and Osman, A . Relations between hopelessness, depressive symptoms and suicidality: mediation by reasons for living. J Clin Psychol. (2014) 70:18–31. doi: 10.1002/jclp.22005
85. Adamopoulos, IP , and Syrou, NF . Associations and correlations of job stress, job satisfaction and burn out in public health sector. Eur J Environ Public Health. (2022) 6:em0113. doi: 10.21601/ejeph/12166
86. Sampson, M , Melnyk, BM , and Hoying, J . The MINDBODYSTRONG intervention for new nurse residents: 6-month effects on mental health outcomes, healthy lifestyle behaviors, and job satisfaction. Worldviews Evid-Based Nurs. (2020) 17:16–23. doi: 10.1111/wvn.12411
87. Awan, S , Diwan, MN , Aamir, A , Allahuddin, Z , Irfan, M , Carano, A, et al. Suicide in health-care workers: determinants, challenges, and the impact of COVID-19. Front Psych. (2022) 12:792925. doi: 10.3389/fpsyt.2021.792925
88. Cai, CZ , Lin, YL , Hu, ZJ , and Wong, LP . Psychological and mental health impacts of COVID-19 pandemic on health-care workers in China: a review. World J Psychiatr. (2021) 11:337–46. doi: 10.5498/wjp.v11.i7.337
89. Martínez-Arriaga, RJ , Dominguez-Rodriguez, A , Herdoiza-Arroyo, PE , Robles-Garcia, R , de la Rosa-Gómez, A , Figueroa González, JA, et al. Suicide risk and associated factors in health-care workers seeking psychological support during COVID-19: a cross-sectional study. Psychol Health Med. (2023) 75:245–53. doi: 10.1136/oemed-2017-104531
90. Dutheil, F , Aubert, C , Pereira, B , Dambrun, M , Moustafa, F , Mermillod, M, et al. Suicide among physicians and health-care workers: a systematic review and meta-analysis. PLoS One. (2019) 14:e0226361. doi: 10.1371/journal.pone.0226361
91. Mandracchia, JT , and Sunderland, MN, To, Y. M . Evaluating the role of interpersonal hopelessness in the interpersonal theory of suicide. Death Stud. (2021) 45:746–50. doi: 10.1080/13548506.2023.2216469
92. Niu, L , Jia, C , Ma, Z , Wang, G , Sun, B , Zhang, D, et al. Loneliness, hopelessness and suicide in later life: a case–control psychological autopsy study in rural China. Epidemiol Psychiatr Sci. (2020) 29:e119. doi: 10.1017/S2045796020000335
Keywords: general work stress, suicide cognitions, hopelessness, job satisfaction, health-care workers
Citation: Sarigül A, Kaya A, Aziz IA, Yıldırım M, Özok HI, Chirico F and Zaffina S (2023) General work stress and suicide cognitions in health-care workers: mediating effect of hopelessness and job satisfaction. Front. Public Health. 11:1254331. doi: 10.3389/fpubh.2023.1254331
Edited by:
M. David Rudd, University of Memphis, United StatesReviewed by:
Alberto Modenese, University of Modena and Reggio Emilia, ItalyMomcilo Mirkovic, University of Pristina, Serbia
Copyright © 2023 Sarigül, Kaya, Aziz, Yıldırım, Özok, Chirico and Zaffina. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Murat Yıldırım, bXVyYXR5aWxkaXJpbUBhZ3JpLmVkdS50cg==; bXVyYXR5aWxkaXJpbXBoZEBnbWFpbC5jb20=
†These authors share last authorship
‡ORCID: Abdulselami Sarigül https://orcid.org/0000-0002-1272-5274
Alican Kaya https://orcid.org/0000-0003-2933-0161
Izaddin Ahmad Aziz https://orcid.org/0009-0004-3683-4522
Murat Yıldırım https://orcid.org/0000-0003-1089-1380
Halil Ibrahim Özok https://orcid.org/0000-0002-6427-6335
Francesco Chirico https://orcid.org/0000-0002-8737-4368
 Abdulselami Sarigül1‡
Abdulselami Sarigül1‡ Alican Kaya
Alican Kaya Izaddin Ahmad Aziz
Izaddin Ahmad Aziz Murat Yıldırım
Murat Yıldırım Francesco Chirico
Francesco Chirico Salvatore Zaffina
Salvatore Zaffina