- 1Center for Health Promotion and Prevention Research, School of Public Health, University of Texas Health Science Center at Houston, Houston, TX, United States
- 2UTHealth Institute for Implementation Science, The University of Texas Health Science Center, Houston, TX, United States
- 3Center for Mental Health Services Research, Brown School, Washington University in St. Louis, St. Louis, MO, United States
- 4Center for Dissemination and Implementation, Institute for Public Health, Washington University in St. Louis, St. Louis, MO, United States
- 5Division of Infectious Diseases, John T. Milliken Department of Medicine, School of Medicine, Washington University in St. Louis, St. Louis, MO, United States
- 6Department of Work and Social Psychology, Faculty of Psychology and Neurosciences, Maastricht University, Maastricht, Netherlands
Editorial on the Research Topic
Implementation Mapping for selecting, adapting and developing implementation strategies
The development, or selection and tailoring, of strategies to implement evidence-based interventions (EBIs) is essential for closing the research-to-practice gap and improving health and health equity. Although Intervention Mapping (1) includes planning implementation strategies within its 6-step protocol for planning, implementing, and evaluating multilevel interventions, the standalone process for designing implementation strategies for existing EBIs via Implementation Mapping (IM) (2) was introduced in 2019. It is a helpful tool for guiding the design and tailoring of strategies to enhance intervention adoption, implementation, and sustainment. IM draws from the fields of health promotion and implementation science. It includes five tasks: (1) conduct a needs and assets assessment and identify program adopters and implementers; (2) state adoption and implementation outcomes and performance objectives, identify determinants, and create matrices of change objectives; (3) choose theoretical methods and select or design implementation strategies; (4) produce implementation protocols and materials; and (5) evaluate implementation outcomes. The tasks are iterative, with previous tasks revisited throughout to ensure all implementers, outcomes, determinants, and objectives are addressed.
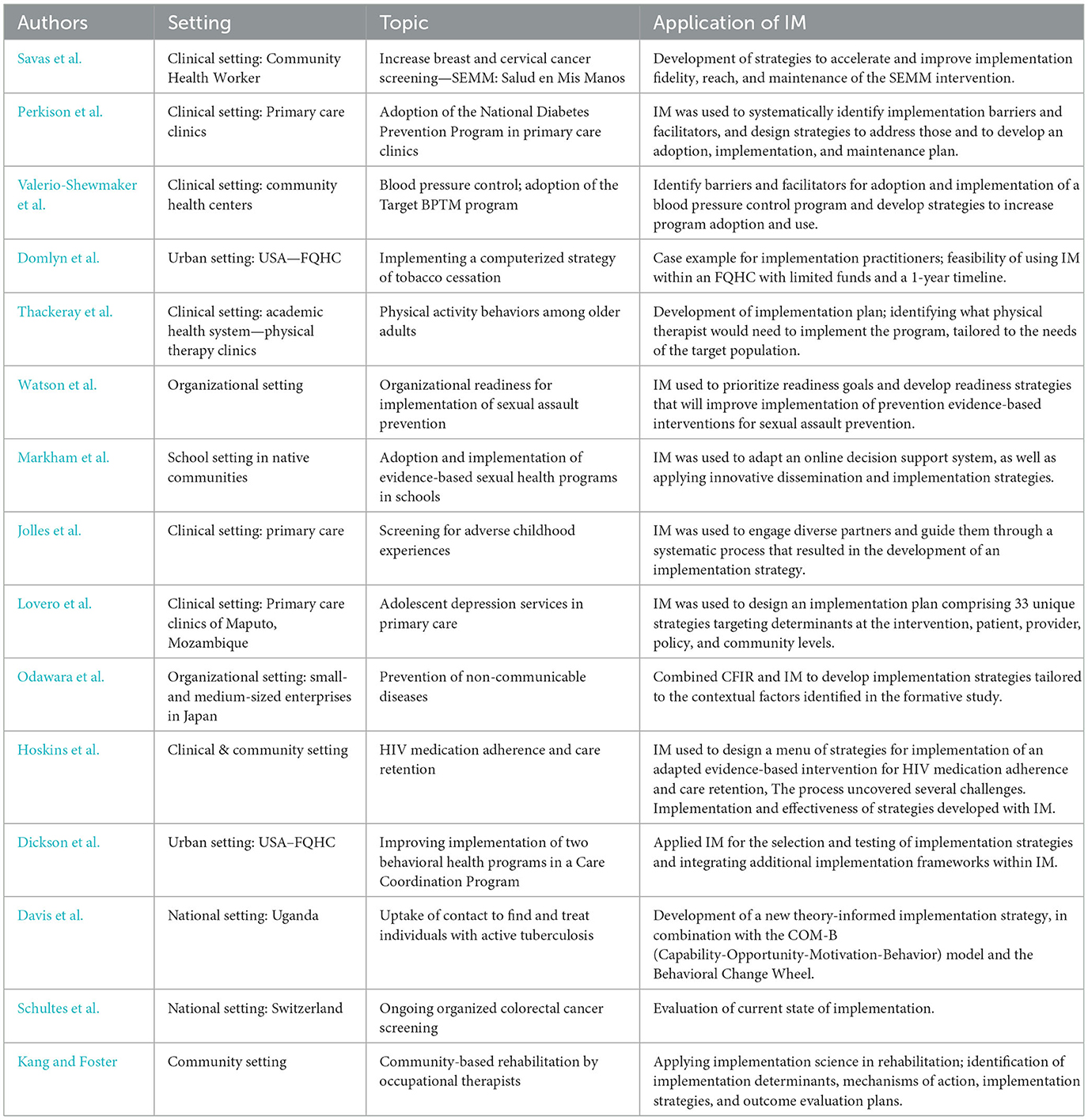
IM addresses two priorities in implementation science by enhancing the design and/or tailoring of implementation strategies and facilitating a better understanding of the mechanisms through which implementation strategies work (3–5). This Research Topic is dedicated to Implementation Mapping methods, with 15 articles representing a range of settings, topics, and applications (see Table 1).
Below, we highlight examples of the application of IM (by IM Task) in several of the published studies.
Task 1: Implementation Needs and Assets Assessment: Several articles in this issue describe the use of mixed methods to identify implementation determinants prior to designing strategies to address them. Perkison et al. conducted a needs and assets assessment among frontline staff in community health centers. They employed mixed methods to assess implementation determinants for the National Diabetes Prevention Program (NDPP) by administering a 56-item online survey and conducting 1-h qualitative interviews. The assessments explored determinants at patient, provider, and organizational levels to inform a multilevel and multicomponent implementation strategy to improve adoption and use of NDPP.
Task 2: Adoption and Implementation Outcomes, Performance Objectives, Determinants, and Change Objectives: Thackeray et al. identified adoption and implementation outcomes for use of Coach2Move, a physical therapy intervention for older adults with a musculoskeletal condition. The team focused on adoption and implementation behaviors of clinic managers and physical therapists. They utilized the Consolidated Framework for Implementation Research to examine implementation determinants and described implementation actions (“implementation performance objectives”). They used this information to build a logic model that described the hypothesized mechanisms of action. They also created matrices of change objectives that considered both the specific actions that needed to be carried out to implement the program and determinants that influenced those actions. These matrices helped inform implementation strategy content.
Task 3: Selection of Theoretical Methods and Design of Implementation Strategies: Lovero et al. collaborated with community partners, including policymakers, providers, and representatives from local and non-governmental organizations, to design implementation strategies. They organized collaborative workshops to create implementation research logic models (6) and selected strategies aligned with Expert Recommendations for Implementing Change (ERIC) (7). They also identified new strategies for determinants not well-addressed by ERIC, tailored them to the specific context, and evaluated their priority and feasibility. They specified their strategies using Proctor et al.'s recommendations (8). Two other studies, Savas et al. and Davis et al., exemplified the use of theoretical methods in strategy selection. Savas et al. employed “A Taxonomy of Behavior Change Methods” (9) to guide their approach, while Davis et al. used COM-B and the Behavior Change Wheel (10). Markham et al. demonstrated how to effectively link determinants and change objectives, theoretical change methods (including parameters for their use), and implementation strategies (see Table 4 of that article).
Task 4: Production of Implementation Protocols and Materials: Informed Tasks 2 and 3, Savas et al. provided a design document for their implementation strategy, which provided details to the creative team on the objectives, determinants addressed, theoretical change method, and other guidance needed to develop the material. They also included protocols and final implementation materials.
Task 5: Evaluation of Implementation Outcomes: Kang and Foster used IM to develop implementation strategies for a rehabilitation goal setting and goal management intervention. The IM process informed evaluation plans to explore the impact of implementation strategies using a mixed-methods study. They used self-reported surveys to measure process outcomes, considering the change objectives identified in Task 2. The results of this evaluation can offer valuable insights into the mechanisms of implementation strategies and provide an example of how this information can inform further strategy refinement. An acknowledged limitation was that self-reported outcomes may not always align with objectively assessed performance.
Studies described in the special topics issue focused on various socio-ecological levels and settings including primary health care clinics, Federally Qualified Health Centers (FQHCs), businesses, organizations, schools, a university, and community implementation with community health workers. Two studies describe the application of IM on the national level, in Switzerland and Uganda. See Table 1 for details.
Each article described the IM process, giving varied attention to stating implementation goals, identifying and changing implementation determinants, applying strategies to promote dissemination and implementation, and acknowledging the role of relevant partners. Several studies used IM to integrate the application of several theories and frameworks.
The published articles in this issue show how IM can advance implementation science in several ways including the (1) use of theory in the development of implementation strategies, (2) use of logic models to identify mechanisms, (3) development of implementation research questions, (4) design of studies to evaluate implementation strategies, (5) integration of community engagement in planning strategies to enhance implementation, and sustainment, and (6) planning for broad scale-up and spread.
This Research Topic showcases how IM can contribute to bridging the research-to-practice gap to improve health and health equity. Too many EBIs are not put into practice or are implemented slowly, inequitably, or with poor fidelity. This compromises the potential of research findings in improving healthcare and health promotion efforts. IM outlines a practical method for planning implementation strategies that integrates community engagement, new data, theory and frameworks, and existing evidence. Just as the systematic planning of interventions has improved their effectiveness, IM holds promise for improving the appropriateness, quality, and impact of implementation strategies, which ultimately stands to yield improvements in population health.
Author contributions
MF: Original revised draft, Review and editing, Writing—original draft. BP: Writing—review and editing. GT: Original draft, Writing—review and editing.
Acknowledgments
The authors would like to thank Dr. Eunyoung Kang for her assistance in data curation and manuscript writing and editing. Acknowledge the following grant support from the NIH (K01MH113806, R01CA262325, R01AA030480, R25MH080916, U24HL154426, P50CA19006, R01DA047876, P50MH126219) and the AHRQ (R13HS025632, NIH 5UL1TR003167, and CDC 1U48DP006408-01-00).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bartholomew Eldridge LK, Markham CM, Ruiter RAC, Fernández ME, Kok G, Parcel GS. Planning Health Promotion Programs: An Intervention Mapping Approach. 4th ed San Francisco: Jossey-Bass, Inc. (2016).
2. Fernandez ME, Ten Hoor GA, van Lieshout S, Rodriguez SA, Beidas RS, Parcel G, et al. Implementation mapping: Using intervention mapping to develop implementation strategies. Front Public Health. (2019) 7:1–15. doi: 10.3389/fpubh.2019.00158
3. Powell BJ, Fernandez ME, Williams NJ, Aarons GA, Beidas RS, Lewis CC, et al. Enhancing the impact of implementation strategies in healthcare: A research agenda. Front Public Health. (2019) 7:1–9. doi: 10.3389/fpubh.2019.00003
4. Lewis CC, Powell BJ, Brewer SK, Nguyen AM, Schriger SH, Vejnoska SF, et al. Advancing mechanisms of implementation to accelerate sustainable evidence-based practice integration: protocol for generating a research agenda. BMJ Open. (2021) 11:e053474. doi: 10.1136/bmjopen-2021-053474
5. Geng EH, Baumann AA, Powell BJ. Mechanism mapping to advance research on implementation strategies. PLoS Med. (2022) 19:e1003918. doi: 10.1371/journal.pmed.1003918
6. Smith JD, Li DH, Rafferty MR. The Implementation Research Logic Model: a method for planning, executing, reporting, and synthesizing implementation projects. Implement Sci. (2020) 15:84. doi: 10.1186/s13012-020-01041-8
7. Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci. (2015) 10:1–14. doi: 10.1186/s13012-015-0209-1
8. Proctor EK, Powell BJ, McMillen JC. Implementation strategies: Recommendations for specifying and reporting. Implement Sci. (2013) 8:1–11. doi: 10.1186/1748-5908-8-139
9. Kok G, Gottlieb NH, Peters GY, Mullen PD, Parcel GS, Ruiter RAC, et al. taxonomy of behaviour change methods: An Intervention Mapping approach. Health Psychol Rev. (2016) 10:297–312. doi: 10.1080/17437199.2015.1077155
Keywords: implementation science, Implementation Mapping, Intervention Mapping, implementation strategies, adaptation, mechanisms of implementation strategies
Citation: Fernandez ME, Powell BJ and Ten Hoor GA (2023) Editorial: Implementation Mapping for selecting, adapting and developing implementation strategies. Front. Public Health 11:1288726. doi: 10.3389/fpubh.2023.1288726
Received: 04 September 2023; Accepted: 20 September 2023;
Published: 17 October 2023.
Edited and reviewed by: Christiane Stock, Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Institute of Health and Nursing Science, Germany
Copyright © 2023 Fernandez, Powell and Ten Hoor. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria E. Fernandez, TWFyaWEuRS5GZXJuYW5kZXpAdXRoLnRtYy5lZHU=
 Maria E. Fernandez
Maria E. Fernandez Byron J. Powell
Byron J. Powell Gill A. Ten Hoor
Gill A. Ten Hoor