- 1Department of Graduate School, Wannan Medical College, Wuhu, China
- 2Department of Gerontology, Yijishan Hospital, the First Affiliated Hospital of Wannan Medical College, Wuhu, China
- 3School of Humanities and Management Science, Wannan Medical College, Wuhu, China
- 4Anhui Key Laboratory of Philosophy and Social Sciences for Public Health Crisis Management, Wuhu, China
- 5Department of Emergency and Critical Care Nursing, School of Nursing, Wannan Medical College, Wuhu, China
- 6Department of Internal Medicine Nursing, School of Nursing, Wannan Medical College, Wuhu, China
- 7Department of Surgery Nursing, School of Nursing, Wannan Medical College, Wuhu, China
- 8Department of Pediatric Nursing, School of Nursing, Wannan Medical College, Wuhu, China
- 9Department of Gynecology and Obstetrics Nursing, School of Nursing, Wannan Medical College, Wuhu, China
Objective: This study aimed to assess the prevalence of post-traumatic stress disorder (PTSD) and its influencing factors among intern nursing students after the full liberalization of the COVID-19 prevention and control policy in China.
Methods: Participants completed the online survey from January 14 to January 19, 2023. A demographic questionnaire, COVID-19 and internship-related questionnaire, the Fear of COVID-19 scale, the Primary Care PTSD Screen, and the Connor-Davidson Resilience Scale were used to conduct the online survey.
Results: Of 438 participants, 88.4% tested positive for COVID-19 in the last 6 months. The prevalence of fear, resilience, and PTSD was 16.9, 15.5, and 11.2%, respectively. Direct care of COVID patients in hospital (OR = 2.084, 95%CI 1.034 ~ 4.202), the experience of occupational exposure (OR = 2.856, 95%CI 1.436 ~ 5.681), working with an experienced team (OR = 2.120, 95%CI 1.070 ~ 4.198), and fear COVID-19 (OR = 8.269, 95%CI 4.150 ~ 16.479) were significantly and positively associated with PTSD in nursing internship students.
Conclusion: After COVID-19 full liberalization in China, intern nursing students still experienced pandemic-related mental distress, which can bring PTSD. Adequate support and counseling should be provided, as needed, to intern nursing students who are about to enter the workforce and have experienced severe PTSD symptoms related to COVID-19. Our findings indicated that should understand the importance of screening, formulate intervention strategies and preventive measures to address psychosocial problems, and provide coping skills training to intern nursing students.
1 Introduction
The Coronavirus disease 2019 (COVID-19) was labeled as a pandemic by the World Health Organization (1), in March 2020. With highly contagious, morbidity and mortality, COVID-19 has posed numerous challenges to all aspects of life and health. From the beginning of the COVID-19 pandemic through the fall of 2022, the Chinese government adhered to a set of “zero COVID” policies for nearly 3 years, such as closing national borders, city-wide lockdown, monitoring “Health Code,” nucleic acid testing, temperature screening, and tracking and quarantining of infected individuals and their direct and indirect contacts (2).
To minimize the impact of the epidemic on economic and social development, on November 11, 2022, the National Health Commission of China issued a “20 Measures policy.” With this policy, some of the strict prevention and control measures were relaxed, only lock-downing the infected areas and buildings, identification of close contacts and infected persons, shortening the period of isolation for medical observation, eliminating the inbound flight fusion mechanism, and large-scale testing and reporting no longer mandatory. Beginning on December 7, 2022, the “20 Measures policy” was replaced with the “10 Measures policy” (3). Under this policy, nucleic acid testing and health codes for inter-regional personnel have been eliminated. Close contacts and infected persons were isolated and quarantined at home. The school conducts offline teaching and ensures normal life. On December 27, 2022, policies of comprehensive liberalization were implemented. A new case of coronavirus infection released from quarantine. Nucleic acid testing and reporting were voluntary. Close contacts and high-risk areas were no longer identified (4). By the end of December 2022, some new sub-variants of Omicron caused the Chinese population a second wave of breakthrough infections in a short time (5). The Chinese Center for Disease Control and Prevention (CDC) reported a positive rate of 29.2% (the number of COVID-19 Nucleic Acid positive tests peaked at 6.94 million), and 2.867 million visits to the doctor for fever (6).
The alteration in learning styles implies that this year’s nursing students face a higher risk during their placements than before the COVID-19 pandemic (7, 8). The nursing curriculum in China comprises 3 years of face-to-face pre-clinical teaching followed by a 1-year internship before the pandemic. Interactive basic nursing skills are normally taught and practiced in every training class. In response to the COVID-19 pandemic, all measures were adopted to reduce the proportion of infected persons. Our educators offered online courses for nursing students instead of in-person learning and interrupted the clinical practice (9).
Earlier studies in the pandemic have reported that nursing students had high levels of distress in their clinical placements, related to the cancelation of clinical placements and transfer to simulated learning (10). The transformation of learning structure and the ways of teaching has resulted in nursing students being exposed to greater risks after the full liberalization of COVID-19 in China. This factor may increase the prevalence of post-traumatic stress disorder (PTSD) caused by COVID-19 pandemic-related experiences (11). After the full liberalization of COVID-19, the SARS-COV-2 omicron variant rapidly accelerated its spread, leading to breakthrough infections in the Chinese population within a short period. Previous research showed that the COVID-19 ongoing stress amplifies negative impacts on student mental health (12). The surge in cases has placed a huge burden on their daily work which might make them vulnerable to psychological problems (12). Studies of health workers at the frontline have shown that increased workload, fear for their health and that of their families and colleagues, lack of personal protective equipment, stigmatization, and caring for patients who have contracted the virus during the pandemic can lead to psychological distress (13, 14). Several studies explored the psychological and mental health impacts of the first wave of the COVID-19 epidemic on nursing students, showing an increase in fear, anxiety, depression, and sleep problems (15, 16).
Participating in nursing internships, they may have to work in a COVID clinical placement and directly care for clinical patients with suspected and confirmed COVID-19. For nursing students, they may fear infection due to a lack of physical preparedness or fear of contagion of the virus to friends and family. When providing hospice services, they may lack the emotional preparedness to witness a patient’s suffering or death. Therefore, these factors may make them more susceptible to PTSD. Posttraumatic stress disorder (PTSD) is a psychiatric disorder that occurs in some people after experiencing a shocking, disturbing, frightening, or dangerous traumatic event. Symptoms of PTSD manifest as intrusiveness (flashbacks or recurrent intrusive thoughts), avoidance (avoidance of the traumatic event that may trigger distressing memories), cognitive and mood changes (negative and distorted beliefs that lead to alienation from others), and altered arousal and reactivity (irritability, reckless behavior, hypervigilance, susceptibility to shock and sleep problems) (17).
Trauma from COVID-19 may cause PTSD among nursing students (11). Nursing students are more likely than other care providers to experience anxiety and psychological stress due to their inadequate skills, inexperience, eagerness to complete their education, uncertainty about the conclusion of the pandemic, and youth-related emotions (18). Studies have found that after a three-month COVID-19 lockdown, nursing students in Spain showed PTSD with a prevalence of 26.7% (19). During the initiation of the COVID-19 pandemic, the prevalence of PTSD among Chinese nursing students was 44.5% (20). Studies in China in 2022 have found that the prevalence of PTSD among nursing students was 15.42% (13). However, to our knowledge, after the full liberalization of COVID-19, the impact has not been evaluated among the intern nursing students in China who were providing health care, when Omicron variant infections spread rapidly and the surge in cases led to another large-scale epidemic. Therefore, the purpose of this study was to examine the prevalence of fear, resilience, and posttraumatic stress disorder (PTSD) and the factors contributing to psychological distress among nursing students entering clinical wards after the full liberalization of COVID-19.
2 Materials and methods
2.1 Ethical considerations
All participants provided informed consent. The study was approved by the Ethics Committee of the nursing department of Wannan Medical College (approval number 20220004).
2.2 Design and participants
2.2.1 Design
The website link has been provided via social platforms (e.g., WeChat and QQ) from 14 January to 19 January 2023. Participants for the study were selected through a snowball sampling process. The professor sent the link (Online surveys are available on the Wen Juan Xing platform) to the head of each class who was willing to distribute it to the students in the class. All participants gave informed consent and understood the purpose of the study. Finally, 438 students completed the survey, and the response rate was 68.87%.
2.2.2 Participants
Participants were recruited from a medical university who are spread across 28 different hospitals in Anhui for internships.
Criteria for inclusion were (1) undergraduate nursing students, (2) voluntary participation in research, and (3) completion of a 9-month internship.
Four hundred and thirty-eight participants completed the survey.
2.3 Assessment and evaluation
2.3.1 Demographic factors
The following demographic characteristics were assessed: age, gender (male or female), living area (rural, town, city), monthly household income per capita (¥ <2,000, ¥ 2001–6,000, ¥ 6,001–10,000, ¥ >10,001).
2.3.2 COVID-19 and internship-related questions
The following questions were asked with a yes/no answer: Q1. Have you been infected with COVID-19 in the last 6 months? Q2. Have you been isolated in the last 6 months? Q3. Has a friend or relative of yours died as a result of COVID-19 infection? Q4. Are you worried about a second or third wave of viral spikes from COVID-19? Q5. Did you often have direct contact with or care for COVID-19 patients in the hospital during your internship? Q6. Did you experience any negative incidents in the hospital during your internship (e.g., verbal or physical violence)? Q7. Did you have any professional exposure during your internship? Q8. Have you been assigned to work with an experienced care team during your internship?
2.3.3 The fear of COVID-19
Fear of COVID-19 Scale (FCV-19S) was used to assess the COVID-19 fears’ levels of participants (21). This seven-item tool was rated on a five-point Likert scale. One is “strongly disagree” and five are “strongly agree.” The total score (ranges from 7 to 35) is calculated by combining the scores of all items. Coronavirus-19 fear increases with a higher score. A cut-off score of 21 and above has been proposed to differentiate the severity of fears associated with COVID-19 (22).
2.3.4 Resilience
Connor-Davidson Resilience Scale (CD-RISC 10) was used to measure psychological resilience (23). The CD-RISC has 10 self-assessment items, with answers ranging from “0- not true at all” to “4 true nearly all the time.” The maximum total score is 40, calculated from the sum of each question. A threshold score of 30 and above indicated greater resilience to stress. The Chinese version showed good structure validity (24).
2.3.5 PTSD
The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) was used to examine PTSD symptoms of internship nursing students in Anhui, China after the full liberalization of China’s COVID-19 prevention and control policy (25). The total scores of this 5-item scale ranged from 0 to 5, with two answers for each item (0 = No, 1 = Yes). Above the cut-off value, 3 has been identified as a reference screening for PTSD.
2.4 Statistical analysis
Statistical analyses were conducted by using version 21.0 of IBM SPSS (Chicago, IL, United States). Demographic characteristics, COVID-19-related questions, and internship-related questions were described by frequencies and proportions. Chi-Square was used to assess for comparison of categorical variables. A binary logistic regression analysis using the forward stepwise method with the occurrence of PTSD as a dependent variable was performed. Odds ratios (ORs) and 95% confidence intervals (CIs) were used to estimate associations. p values were two-tailed and considered to indicate statistical significance at the <0.05 level. The statistical analysis was conducted by Hairong Liu.
3 Results
3.1 Demographic characteristics
The mean age of the nurse students was 22.11 ± 0.92 years. Of the 438 nurse students investigated in this study, 76.5% were female; 50.9% were from rural, 25.8% were from town, and 23.3% were from city. Most participants (53.2%) had a per capita household income range of RMB ¥ 2,001 ~ 6,000 per month (Table 1).
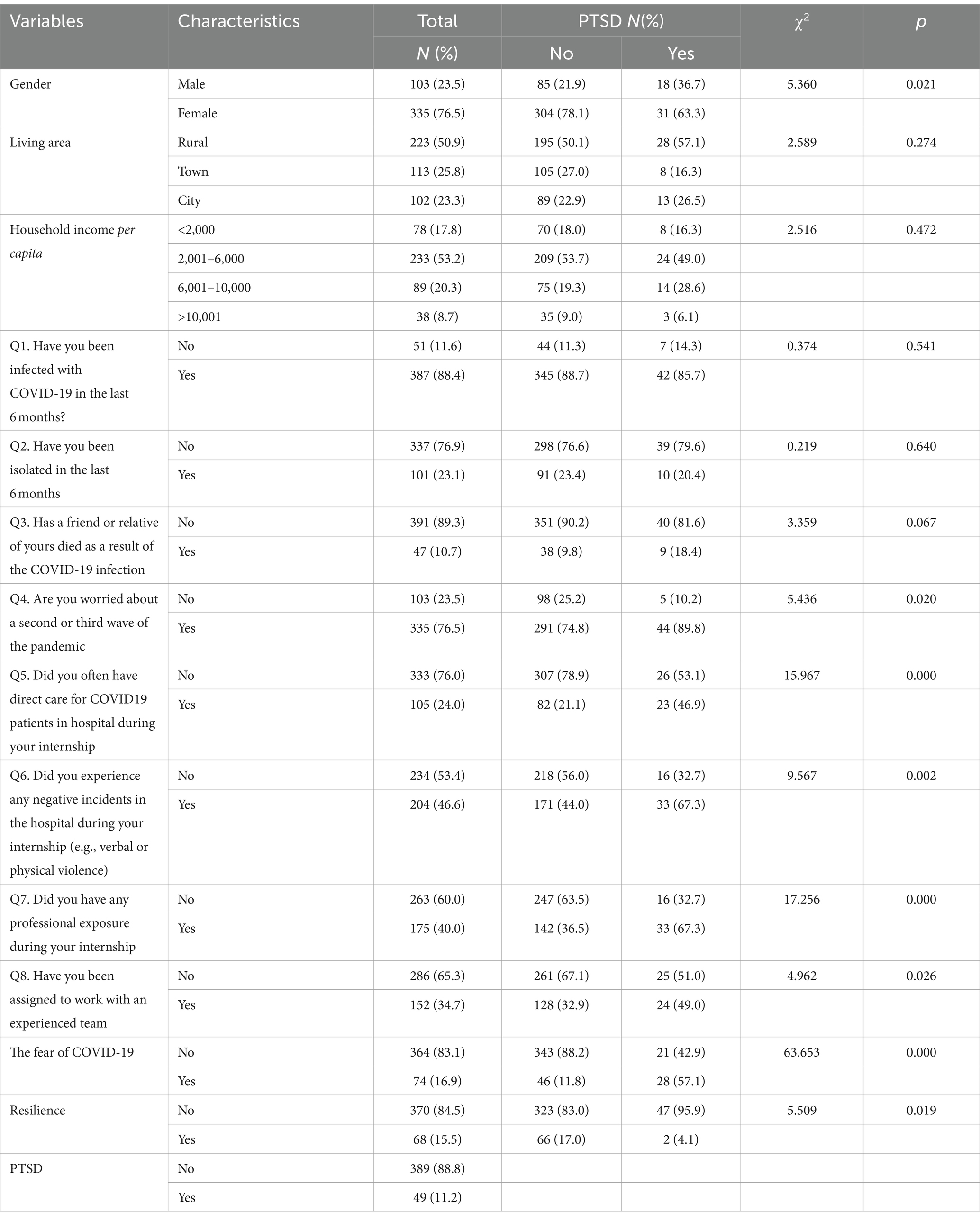
Table 1. Sample characteristics and analysis of variables for possible association with PTSD (N = 438).
3.2 COVID-19 and internship-related questions
The distribution of COVID-19 and internship-related issues is displayed in Table 1. The majority of the participants (88.4%) tested positive for COVID-19 in the last 6 months. 23.1% of the participants declared that they had been isolated in the last 6 months. 10.7% of the participants had friends or relatives who died as a result of COVID-19 infection. More than three-quarters of the participants (76.5%) worried about a second or third wave of the pandemic. 24% of samples directly cared for patients with COVID-19. Participants reported experiencing verbal or physical violence and occupational exposure during hospital internships in 46.6 and 40% of cases, respectively. One-third reported working with an experienced team.
3.3 The level of fear, resilience, and PTSD
The mean score of Fear, Resilience, and PTSD information in Anhui, China was 15.24 ± 4.86, 23.46 ± 5.81, and 0.78 ± 1.24, respectively. The prevalence of fear, resilience, and PTSD was 16.9, 15.5, and 11.2%, respectively. Of the respondents with PTSD symptoms, 63.3% were female, 57.1% were from rural areas, 49% had a monthly per capita household income between ¥ 2,001 and ¥ 6,000, 85.7% had tested positive for COVID-19 in the past 6 months; 20.4% of the participants indicated that they had been isolated in the last 6 months, 18.4% of the participants had a friend or relative who had died from COVID-19 infection, 89.8% were concerned about a second or wave 3 pandemic, 46.9% directly cared for COVID-19 patients, 67.3% had experienced verbal or physical violence in hospital, and experienced occupational exposure, 49.0% were assigned to an experienced team, 57.1% were afraid of COVID-19, 95.9% had poor resilience.
3.4 Associated factors of PTSD
There were several factors in the research identified to be significantly associated with the occurrence of PTSD through a Chi-square test, including gender (p = 0.021), fear of a second or third pandemic wave (p = 0.020), direct care of COVID patients in the hospital (p = 0.000), the experience of verbal or physical violence at work (p = 0.002), the experience of occupational exposure in the hospital (p = 0.000), working with an experienced team (p = 0.026), fear-19 (p = 0.000), and resilience (p = 0.019) (Table 1).
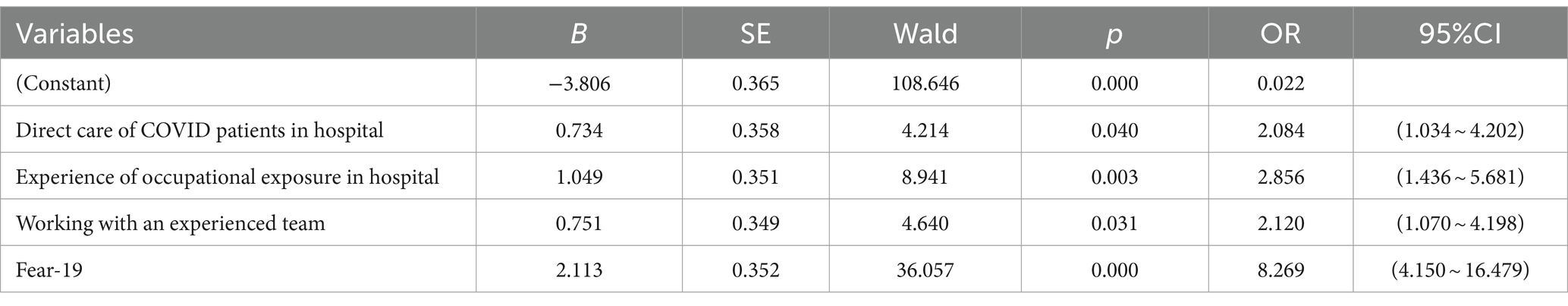
The results of the binary logistic regression analysis showed that direct care of COVID patients in hospital (OR = 2.084, 95%CI 1.034 ~ 4.202), the experience of occupational exposure (OR = 2.856, 95%CI 1.436 ~ 5.681), working with an experienced team (OR = 2.120, 95%CI 1.070 ~ 4.198), and fear-19 (OR = 8.269, 95%CI 4.150 ~ 16.479) were significantly and positively associated with a higher risk of PTSD in nursing internship students (Table 2).
4 Discussion
Due to the unpredictable nature of epidemics, after COVID-19 was fully liberalized in China, Omicron variant infections spread rapidly and the surge in cases led to another large-scale epidemic. More than 80% of the intern nursing students have been infected, and over 75% of students are worried about another COVID-19 pandemic wave. Therefore, following the full liberalization of China’s COVID-19 prevention and control policy, it is still necessary to know the prevalence of PTSD and its influence factors among intern nursing students.
4.1 The prevalence of PTSD
The present study was to assess positive PTSD cases in intern nursing students and to identify associated risk factors after the full liberalization of COVID-19 in China. The prevalence of PTSD was found to be 11.2% among intern nursing students. 16.9% of students expressed fear of COVID-19. The level of PTSD in our sample is lower than those reported by the studies invested in the initial phase of the COVID-19 outbreak, the prevalence in Spain and China was 26.7 and 44.5%, respectively (19, 20). The proportion of the sample reporting lower levels of PTSD than the Australian study (49.4%) (26). Compared to the domestic literature in 2022 (15.42%), the prevalence of PTSD in the study was relatively lower (11.2%) (13). Differential exposure, and the diminishment of symptoms over time, may explain the lower levels of symptom reporting in our sample.
In the international, nursing management is essential to the delivery of care and effective organization (27). During the COVID-19 crisis, nursing managers and leaders are leading the way in responding to the special requirements of their workforce. Nurse managers at all levels are being put to the test in a unique set of circumstances brought about by the response to the COVID-19 epidemic in terms of their practical and ethical judgment (28). To reduce stress for nurses, they need to provide suitable rest days and personal safety measures, arrange support services, rotate allocations of critical patients, and be accessible to staff (29). According to Shahrour’s research, coping with self-efficacy can lessen the impact of psychological stress on nurses’ traumatic experiences and healthcare institutions should provide psychosocial support for nurses (29). Nurse leaders should actively participate in protecting the personal safety of their employees by working closely with hospital administration to ensure and provide personal safety measures (29). At the same time, the leaders or managers themselves need support from other colleagues (30).
4.2 Influencing factors on PTSD
Our respondents reported that direct care of patients with COVID-19, the experience of occupational exposure, working with an experienced team, and fear-19 were significantly associated with the severity of PTSD symptoms.
4.2.1 Direct care of COVID patients in hospital
The study found that intern nursing students, as caregivers of COVID-19 patients, hold a positive correlation with PTSD. After the COVID-19 epidemic, medical students may experience higher levels of stress than non-medical students (31). When it comes to primary and secondary infectious disease prevention, nurses are the leading proactive partners (32). A significant risk of infection exists for nursing interns who care for patients in hospitals who have the COVID-19 virus, whether suspected or confirmed. To carry out their jobs, frontline nurses frequently work under pressure and sometimes may even risk their lives (33, 34). The students lacked experience in providing care for those infected with COVID-19, and even experienced nurses required psychological support throughout the pandemic. They have to make difficult choices about patient care in unpredictable and exhausting conditions. For example, inconsistent access to protective equipment, shifting guidelines, high-nurse–patient ratios, and increased workload and hours (35–37). The public was afraid of contracting COVID-19, including friends and family. Some people avoided, harassed, and even blamed medical professionals including nurses and nursing students for spreading COVID-19 (38–40). The possibility of contracting COVID-19 and infecting their families worried the nursing students who worked in the hospital as well (41). Moreover, nurses who provide direct care to COVID-19 patients frequently see patients suffering and death, which may cause them to become emotionally distressed and tired (42). As a result, it may cause a great deal of psychological stress, anxiety, and depression. Formulating long-term strategies and delivery of interventions to address psychosocial problems in intern nursing students are necessary. In Huang’s research, more psychological support, adequate medical protective equipment, training in coping strategies, and developing interventions to block the spread of infectious diseases, could improve the quality of patient care (43).
4.2.2 Experience of occupational exposure in hospital
The study found that experience of occupational exposure in hospitals is another variable, which was positively correlated with PTSD in intern nursing students. Wilson et al. found that first responders experience occupational exposures that are regularly linked to PTSD (44). It was partly in accordance with this research. The occupational exposure to nursing is wide and includes things such as needlestick injuries (45), radiation exposure (46), body fluid exposure (47), and violent workplace environments (48). Of those who had experienced occupational exposure, 67.35% were nursing staff (49). It may related to the fact that nurses need to perform many operations such as oral care, sputum suction, and monitoring vital signs. Liu’ research found similar results that nurses may face a higher risk of occupational exposure to COVID-19 patients (50). It was caused by their increased time spent on wards, direct patient care, and responsibility for gathering sputum for viral testing. Several studies indicated that female are more prone to occupational exposure than their male counterparts (51, 52). The effects of PTSD brought on by occupational exposure can be extremely burdens to individuals, their families, their places of employment, and society at large (53). Compared to individuals without this diagnosis, those with PTSD diagnoses are more likely to report physical illnesses, suicide attempts, poor quality of life, additional mental disorders, and disability (54, 55). Understanding the present state of occupational exposure in intern nursing students will be beneficial in enhancing prevention awareness, preventing occupational exposure, and promoting their physical and mental well-being. To deliver effective education, the teachers need to learn about the characteristics of the nursing student cohort served by the lesson and design the lesson accordingly (56). Distance learning is being added to nursing programs more and more to improve learning opportunities and meet the increased diversity among learners (56). According to Magdalinou’s research, student and teacher interaction is crucial, and an online course with a proper design could facilitate it (57). Moreover, the use of interactive teaching methods would promote learning, and prompt technical support would decrease technological problems and encourage distance learning (57).
4.2.3 Working with an experienced team
It is worth noting that student collaboration with an experienced team is another factor influencing PTSD in intern nursing students. Experienced frontline nurses are more likely to care for infected patients. This result indicates that nursing students working with experienced teams may have higher rates of infection. Studies in southern Iran have shown that nursing students caring for COVID-19 patients face high levels of death anxiety (18). Many studies conducted during the pandemic, focused on the Psychological and mental impact on first-line healthcare workers and showed that the frontline healthcare workers had anxiety, depression, stress, and PTSD (58, 59). After years, they were still fighting with contagion caused by Sars-CoV-2. The study conducted by Claponea RM shows that female gender, not having children, and single marital status, have a high level of burnout Syndrome (60). Burnout can have negative consequences (61). The experienced team was already fatigued and exhausted (62–65). These include reduced quality of care, absenteeism, turnover, and reduced commitment (27). Providing emotional support interventions for intern nursing students is required (66). To reduce anxiety and stress, the faculty should create a structured learning environment, follow the course schedule, communicate changes or updates promptly, modify assignments to fit the learning environment, take self-care, extend grace, and make use of campus, local, and national resources (67).
4.2.4 Fear COVID-19
This study also found that the fear of a second or third wave pandemic was significantly associated with the severity of PTSD symptoms. Because of its deadly features, COVID-19 presented a new worldwide threat (e.g., rapid transmission, uncertainty about the transmission method, incubation period, unpredictable mortality rate, and manifestation), which rapidly evoked anxiety and fear in the Chinese population and worldwide (68). Many countries promote the transition of universities from on-site teaching and learning activities to online or virtual modalities (69). Logically, this COVID-19 epidemic and these preventive measures may have a substantial negative effect on mental health, causing widespread stress, anxiety, depression, and fear (70). The impact of PTSD on intern nursing students is profound, Students have difficulty defining their professional identities, fitting in with the team, and fearing COVID-19. Their psychological conditions were quickly made worse by long-term isolation and uncertainty (71). Even though the majority of students (67.07%) did not actively participate in the treatment of COVID-19 patients, there was still a degree of concern about contracting the virus (72). Compared with adults, students are a more vulnerable population. A recent meta-analysis, which included 33 different researchers from 18 different countries and conducted among university students, confirmed that the fear of COVID-19 was related to PTSD (73). Nursing students are worried about their future professions and study due to the uncertainty about their future careers. They also suffer constant pressure due to factors like separation from family and fear of infection, which raises the possibility of triggering PTSD (74). Consequently, nursing students and educational administrators must recognize the importance of the screening, prevention, and psychological intervention of PTSD. Schools and hospitals should concentrate on teaching nursing students all available coping methods to increase their capacity to control their emotions and effective coping tools to enhance the lives of nursing students, and their families (75).
4.3 Strengths and limitations of the study
The research has several strengths. First, this research included 438 participants from different hospitals, which ensured the accuracy of this research. Second, the measures of the fear of COVID-19, resilience, and PTSD were widely applied and validated instruments to thoroughly understand the research questions. Finally, its potential contribution to the field of public health, as it presents the prevalence of PTSD and its influencing factors among intern nursing students after the full liberalization of the COVID-19 prevention and control policy in China.
Several limitations may have an impact on the interpretation of the study. Such as self-report surveys, misinterpretation, and self-report bias could happen. Second, the data was accessed from the participants with social media (smartphones, WeChat, blogs, and computers). Thus, the recruited sample with no Internet was not examined. Third, the interns in this study were from a university in Anhui Province, so the sample cannot be generalized to nursing interns throughout China. In the future, the study will be expanding sample size and conducting multi-center, large-sample studies.
5 Conclusion
After COVID-19 full liberalization in China, intern nursing students still experienced pandemic-related mental distress, which can bring PTSD. Adequate support and counseling should be provided, as needed, to intern nursing students who are about to enter the workforce and have experienced severe PTSD symptoms related to COVID-19. Our findings indicated that should understand the importance of screening, formulate intervention strategies and preventive measures to address psychosocial problems and provide coping skills training to intern nursing students.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YS: Writing – original draft, Writing – review & editing. XianL: Funding acquisition, Writing – original draft, Writing – review & editing. HL: Data curation, Funding acquisition, Methodology, Software, Writing – review & editing. XiaoL: Project administration, Writing – review & editing. LS: Project administration, Writing – review & editing. LZ: Project administration, Supervision, Writing – review & editing. CW: Writing – review & editing. JL: Project administration, Writing – review & editing. ML: Project administration, Writing – review & editing. DZ: Project administration, Writing – review & editing. YL: Project administration, Writing – review & editing. TY: Funding acquisition, Project administration, Supervision, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by The foundation of Anhui provincial education department of Education (2023AH051730, 2023AH040236), The Teaching Quality and Teaching Reform Project Foundation of Wannan Medical College (2022jbgs10, 2021zybz02, 2021jyxm47), and Scientific Research Priority Projects Foundation of Wannan Medical College (WK2023SZD01).
Acknowledgments
We appreciate all participants, as well as the members of the research team for their time and contribution.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
PTSD, Post-traumatic stress disorder; ORs, Odds rations; CIs, Confidence intervals; CDC, Chinese Center for Disease Control and Prevention; FCV-19S, Fear of COVID-19 scale; CD-RISC, Connor-Davidson resilience scale; PC-PTSD-5, Primary care PTSD screen for DSM-5
References
1. Cucinotta, D, and Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. (2020) 91:157–60. doi: 10.23750/abm.v91i1.9397
2. Liu, W, Guan, WJ, and Zhong, NS. Strategies and advances in combating COVID-19 in China. Engineering (Beijing). (2020) 6:1076–84. doi: 10.1016/j.eng.2020.10.003
3. Xinhua. [Internet]. China Focus: COVID-19 response further optimized with 10 new measures (2022). Available at: https://english.news.cn/20221207/ca014c043bf24728b8dcbc0198565fdf/c.html.
4. China TNHCotPsRo. [Internet]. Circular on the issuance of a general programme for the implementation of "Type B B control" for novel coronavirus infections . (2022). Available at: https://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11815/202212/t20221227_263122.html.
5. Ge, J . The COVID-19 pandemic in China: from dynamic zero-COVID to current policy. Herz. (2023) 48:226–8. doi: 10.1007/s00059-023-05183-5
6. Prevention CCfDCa . COVID-19 clinical and surveillance data—December 9, 2022 to April 27, 2023, China [Internet]. (2023). Available at: https://weekly.chinacdc.cn/fileCCDCW/cms/news/info/upload/e712e241-fbcb-426b-9ac8-551ce6fd7ccc.pdf.
7. Rayan, A . Psychological impacts of transition to distance learning due to COVID-19 on nursing students. Int J Ment Health Nurs. (2023) 32:767–77. doi: 10.1111/inm.13139
8. Fernandez, R, Green, H, Middleton, R, Halcomb, E, and Moxham, L. Development and evaluation of the altered student study environment tool: a tool to measure nursing student concerns relating to academic progression during the COVID-19 pandemic. Nurs Educ Perspect. (2022) 43:147–51. doi: 10.1097/01.NEP.0000000000000936
9. Cao, W, Fang, Z, Hou, G, Han, M, Xu, X, Dong, J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
10. Lovrić, R, Farčić, N, Mikšić, Š, and Včev, A. Studying during the COVID-19 pandemic: a qualitative inductive content analysis of nursing students’ perceptions and experiences. Educ Sci. (2020) 10:188. doi: 10.3390/educsci10070188
11. Joseph, RA, Turner, T, Lee, C, Akers, SW, Whorley, E, and Goodrich, C. Impact of COVID-19 on nursing students. J Christ Nurs. (2022) 39:250–7. doi: 10.1097/CNJ.0000000000000951
12. Dewart, G, Corcoran, L, Thirsk, L, and Petrovic, K. Nursing education in a pandemic: academic challenges in response to COVID-19. Nurse Educ Today. (2020) 92:104471. doi: 10.1016/j.nedt.2020.104471
13. Zhang, D, Qin, L, Huang, A, Wang, C, Yuan, T, Li, X, et al. Mediating effect of resilience and fear of COVID-19 on the relationship between social support and post-traumatic stress disorder among campus-quarantined nursing students: a cross-sectional study. BMC Nurs. (2023) 22:164. doi: 10.1186/s12912-023-01319-4
14. Gheshlagh, RG, Hassanpour-Dehkordi, A, Moradi, Y, Zahednezhad, H, Mazaheri, E, and Kurdi, A. Prevalence of psychological disorders among health workers during the COVID-19 pandemic: a systematic review and Meta-analysis. Int J Prev Med. (2023) 14:25. doi: 10.4103/ijpvm.ijpvm_212_21
15. Kochuvilayil, T, Fernandez, RS, Moxham, LJ, Lord, H, Alomari, A, Hunt, L, et al. COVID-19: knowledge, anxiety, academic concerns and preventative behaviours among Australian and Indian undergraduate nursing students: a cross-sectional study. J Clin Nurs. (2021) 30:882–91. doi: 10.1111/jocn.15634
16. Mohamed, SH . Stress and anxiety among junior nursing students during the initial clinical training: a descriptive study at College of Health Sciences, University of Bahrain. Am J Nurs Res. (2019) 7:995–9. doi: 10.12691/ajnr-7-6-13
17. Association AP . What is posttraumatic stress disorder (PTSD)? [Internet]. (2021). Available at: https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd.
18. Mohammadi, F, Masoumi, Z, Oshvandi, K, Khazaei, S, and Bijani, M. Death anxiety, moral courage, and resilience in nursing students who care for COVID-19 patients: a cross-sectional study. BMC Nurs. (2022) 21:150. doi: 10.1186/s12912-022-00931-0
19. Mendez-Pinto, I, Antuña-Casal, M, and Mosteiro-Diaz, MP. Psychological disorders among Spanish nursing students three months after COVID-19 lockdown: a cross-sectional study. Int J Ment Health Nurs. (2022) 32:479–89. doi: 10.1111/inm.13086
20. Gao, J, Wang, F, Guo, S, and Hu, F. Mental health of nursing students amid coronavirus disease 2019 pandemic. Front Psychol. (2021) 12:699558. doi: 10.3389/fpsyg.2021.699558
21. Ahorsu, DK, Lin, CY, Imani, V, Saffari, M, Griffiths, MD, and Pakpour, AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Heal Addict. (2020) 20:1537–45. doi: 10.1007/s11469-020-00270-8
22. Liu, H, Zhou, N, Zhou, Z, Tao, X, Kong, Y, and Zhang, M. Symptoms of post traumatic stress disorder and their relationship with the fear of COVID−19 and COVID−19 burden among health care workers after the full liberalization of COVID−19 prevention and control policy in China: a cross-sectional study. BMC Psychiatry. (2023) 23:902. doi: 10.1186/s12888-023-05399-z
23. Campbell-Sills, L, and Stein, MB. Psychometric analysis and refinement of the connor–Davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress. (2007) 20:1019–28. doi: 10.1002/jts.20271
24. Yu, X, and Zhang, J. A comparison between the Chinese version of Ego-resiliency scale and Connor-Davidson resilience scale. Psychol Sci. (2007) 30:1169–71. doi: 10.16719/j.cnki.1671-6981.2007.05.035
25. Prins, A, Bovin, MJ, Smolenski, DJ, Marx, BP, Kimerling, R, Jenkins-Guarnieri, MA, et al. The primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J Gen Intern Med. (2016) 31:1206–11. doi: 10.1007/s11606-016-3703-5
26. Usher Am, K, Jackson, D, Massey, D, Wynaden, D, Grant, J, West, C, et al. The mental health impact of COVID-19 on pre-registration nursing students in Australia: findings from a national cross-sectional study. J Adv Nurs. (2022) 79:581–92. doi: 10.1111/jan.15478
27. Bodenheimer, T, and Sinsky, C. From triple to quadruple aim: Care of the Patient Requires Care of the provider. Ann Fam Med. (2014) 12:573–6. doi: 10.1370/afm.1713
28. Newham, R, and Hewison, A. Covid-19, ethical nursing management and codes of conduct: an analysis. Nurs Ethics. (2021) 28:82–90. doi: 10.1177/0969733020988316
29. Shahrour, G, and Dardas, LA. Acute stress disorder, coping self-efficacy and subsequent psychological distress among nurses amid COVID-19. J Nurs Manag. (2020) 28:1686–95. doi: 10.1111/jonm.13124
30. Antonio, MR, and Rosa María, GD. El Liderazgo Pedag Ógico: Competencias Necesarias Para Desarrollar Un Programa De Mejora En Un Centro De Educaci Ón Secundaria. Perspectiva Educacional. (2014) 53:91–113. doi: 10.4151/07189729-Vol.53-Iss.1-Art.127
31. Ye, W, Ye, X, Liu, Y, Liu, Q, Vafaei, S, Gao, Y, et al. Effect of the novel coronavirus pneumonia pandemic on medical students’ psychological stress and its influencing factors. Front Psychol. (2020) 11:548506. doi: 10.3389/fpsyg.2020.548506
32. Tung, YJ, Lo, KKH, Ho, RCM, and Tam, WSW. Prevalence of depression among nursing students: a systematic review and meta-analysis. Nurse Educ Today. (2018) 63:119–29. doi: 10.1016/j.nedt.2018.01.009
33. Mo, Y, Deng, L, Zhang, L, Lang, Q, Liao, C, Wang, N, et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag. (2020) 28:1002–9. doi: 10.1111/jonm.13014
34. Catton, H . Global challenges in health and health care for nurses and midwives everywhere. Int Nurs Rev. (2020) 67:4–6. doi: 10.1111/inr.12578
35. Bruyneel, A, Gallani, MC, Tack, J, d'Hondt, A, Canipel, S, Franck, S, et al. Impact of COVID-19 on nursing time in intensive care units in Belgium. Intens Criti Care Nurs. (2021) 62:102967. doi: 10.1016/j.iccn.2020.102967
36. Cohen, J, and YvdM, R. Contributing factors to personal protective equipment shortages during the COVID-19 pandemic. Prev Med. (2020) 141:106263. doi: 10.1016/j.ypmed.2020.106263
37. LoGiudice, JA, and Bartos, S. Experiences of nurses during the COVID-19 pandemic: a mixed-methods study. AACN Adv Crit Care. (2021) 32:14–26. doi: 10.4037/aacnacc2021816
38. Abdulah, DM, Mohammedsadiq, HA, and Liamputtong, P. Experiences of nurses amidst giving care to COVID-19 patients in clinical settings in Iraqi Kurdistan: a qualitative descriptive study. J Clin Nurs. (2021) 31:294–308. doi: 10.1111/jocn.15909
39. Bhanot, D, Singh, T, Verma, SK, and Sharad, S. Stigma and discrimination during COVID-19 pandemic. Front Public Health. (2021) 8:577018. doi: 10.3389/fpubh.2020.577018
40. Koh, D . Occupational risks for COVID-19 infection. Occup Med Oxford. (2020) 70:3–5. doi: 10.1093/occmed/kqaa036
41. Lancet, T . COVID-19: protecting health-care workers. Lancet. (2020) 395:922. doi: 10.1016/S0140-6736(20)30644-9
42. Alharbi, J, Jackson, D, and Usher, K. The potential for COVID-19 to contribute to compassion fatigue in critical care nurses. J Clin Nurs. (2020) 29:2762–4. doi: 10.1111/jocn.15314
43. Huang, L, Lei, W, Xu, F, Liu, H, and Yu, L. Emotional responses and coping strategies in nurses and nursing students during Covid-19 outbreak: a comparative study. PLoS One. (2020) 15:e0237303. doi: 10.1371/journal.pone.0237303
44. Wilson, S, Guliani, H, and Boichev, G. On the economics of post-traumatic stress disorder among first responders in Canada. J Commun Safety Well-Being. (2016) 1:26–31. doi: 10.35502/jcswb.6
45. Cho, E, Lee, H, Choi, M, Park, SH, Yoo, IY, and Aiken, LH. Factors associated with needlestick and sharp injuries among hospital nurses: a cross-sectional questionnaire survey. Int J Nurs Stud. (2013) 50:1025–32. doi: 10.1016/j.ijnurstu.2012.07.009
46. Andreassi, MG, Piccaluga, E, Guagliumi, G, Del Greco, M, Gaita, F, and Picano, E. Occupational health risks in cardiac catheterization laboratory workers. Circ Cardiovasc Interv. (2016) 9:e003273. doi: 10.1161/CIRCINTERVENTIONS.115.003273
47. Zhang, L, Li, Q, Guan, L, Fan, L, Li, Y, Zhang, Z, et al. Prevalence and influence factors of occupational exposure to blood and body fluids in registered Chinese nurses: a national cross-sectional study. BMC Nurs. (2022) 21:298. doi: 10.1186/s12912-022-01090-y
48. Spector, PE, Zhou, ZE, and Che, XX. Nurse exposure to physical and nonphysical violence, bullying, and sexual harassment: a quantitative review. Int J Nurs Stud. (2014) 51:72–84. doi: 10.1016/j.ijnurstu.2013.01.010
49. Liu, H, Wang, Y, He, HY, Liu, LB, Zhang, Q, Chen, JL, et al. Experience of comprehensive interventions in reducing occupational exposure to COVID-19. J Infect Public Health. (2021) 14:201–5. doi: 10.1016/j.jiph.2020.12.011
50. Liu, Z, Wu, J, Shi, X, Ma, Y, Ma, X, Teng, Z, et al. Mental health status of healthcare Workers in China for COVID-19 epidemic. Ann Glob Health. (2020) 86:128. doi: 10.5334/aogh.3005
51. Biswas, A, Harbin, S, Irvin, E, Johnston, H, Begum, M, Tiong, M, et al. Sex and gender differences in occupational Hazard exposures: a scoping review of the recent literature. Curr Environ Health Rep. (2021) 8:267–80. doi: 10.1007/s40572-021-00330-8
52. Pappa, S, Ntella, V, Giannakas, T, Giannakoulis, VG, Papoutsi, E, and Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
53. Torchalla, I, and Strehlau, V. The evidence base for interventions targeting individuals with work-related PTSD: a systematic review and recommendations. Behav Modif. (2017) 42:273–303. doi: 10.1177/0145445517725048
54. Sareen, J, Cox, BJ, Stein, MB, Afifi TOFleet, C, and Asmundson, GJ. Physical and mental comorbidity, disability, and suicidal behavior associated with posttraumatic stress disorder in a large community sample. Psychosom Med. (2007) 69:242–8. doi: 10.1097/PSY.0b013e31803146d8
55. Brady, KT, Killeen, TK, Brewerton, T, and Lucerini, S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry. (2000) 61:22–32.
56. Sowan, AK, and Jenkins, LS. Designing, delivering and evaluating a distance learning nursing course responsive to students needs. Int J Med Inform. (2013) 82:553–64. doi: 10.1016/j.ijmedinf.2013.02.004
57. Magdalinou, A, Liaskos, J, Isaakidou, M, and Mantas, J. The transition to distance learning in the era of Covid-19 pandemic: the perceptions and experiences of nursing students. Stud Health Technol Inform. (2022) 295:495–8. doi: 10.3233/SHTI220773
58. Hossain, MR, Patwary, MM, Sultana, R, and Browning, MHEM. Psychological distress among healthcare professionals during the early stages of the COVID-19 outbreak in low resource settings: a cross-sectional study in Bangladesh. Front Public Health. (2021) 9:701920. doi: 10.3389/fpubh.2021.701920
59. Leng, M, Wei, L, Shi, X, Cao, G, Wei, Y, Xu, H, et al. Mental distress and influencing factors in nurses caring for patients with COVID-19. Nurs Crit Care. (2020) 26:94–101. doi: 10.1111/nicc.12528
60. Claponea, RM, Pop, LM, Iorga, M, and Iurcov, R. Symptoms of burnout syndrome among physicians during the outbreak of COVID-19 pandemic—a systematic literature review. Healthcare. (2022) 10:979. doi: 10.3390/healthcare10060979
61. Maslach, C . Finding solutions to the problem of burnout. Consult Psychol J Pract Res. (2017) 69:143–52. doi: 10.1037/cpb0000090
62. Sagherian, K, Steege, LM, Cobb, SJ, and Cho, H. Insomnia, fatigue and psychosocial well-being during COVID-19 pandemic: a cross-sectional survey of hospital nursing staff in the United States. J Clin Nurs. (2023) 32:5382–95. doi: 10.1111/jocn.15566
63. Mary Pappiya, E, Mubarak Al Baalharith, I, Arulappan, J, Missiriya Jalal, S, Venkatesan, K, Salem Al Grad, H, et al. Stress and burnout among frontline nurses during COVID-19 pandemic in a middle eastern country. Sage Open Nurs. (2023) 9:23779608231185918. doi: 10.1177/23779608231185918
64. Real-Ramírez, J, Alberto García-Bello, L, Robles-García, R, Martínez, M, Adame-Rivas, K, Balderas-Pliego, M, et al. Well-being status and post-traumatic stress symptoms in health workers attending mindfulness sessions during the early stage of the COVID-19 epidemic in Mexico. Salud Mental. (2021) 43:303–10. doi: 10.17711/SM.0185-3325.2020.041
65. Cai, Z, Cui, Q, Liu, Z, Li, J, Gong, X, Liu, J, et al. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J Psychiatr Res. (2020) 131:132–7. doi: 10.1016/j.jpsychires.2020.09.007
66. Härkänen, M, Pineda, AL, Tella, S, Mahat, S, Panella, M, Ratti, M, et al. The impact of emotional support on healthcare workers and students coping with COVID-19, and other SARS-CoV pandemics – a mixed-methods systematic review. BMC Health Serv Res. (2023) 23:751. doi: 10.1186/s12913-023-09744-6
67. Fitzgerald, A, and Konrad, S. Transition in learning during COVID-19: student nurse anxiety, stress, and resource support. Nurs Forum. (2021) 56:298–304. doi: 10.1111/nuf.12547
68. Alshehri, FS, Alatawi, Y, Alghamdi, BS, Alhifany, AA, and Alharbi, A. Prevalence of post-traumatic stress disorder during the COVID-19 pandemic in Saudi Arabia. Saudi Pharm J. (2020) 28:1666–73. doi: 10.1016/j.jsps.2020.10.013
69. Zhai, Y, and Du, X. Addressing collegiate mental health amid COVID-19 pandemic. Psychiatry Res. (2020) 288:113003. doi: 10.1016/j.psychres.2020.113003
70. Al Sulais, E, Mosli, M, and AlAmeel, T. The psychological impact of COVID-19 pandemic on physicians in Saudi Arabia: a cross-sectional study. Saudi J Gastroenterol. (2020) 26:249–55. doi: 10.4103/sjg.SJG_174_20
71. Rubin, GJ, and Wessely, S. The psychological effects of quarantining a city. BMJ (Clinical Research Ed). (2020) 368:m313. doi: 10.1136/bmj.m313
72. Ulenaers, D, Grosemans, J, Schrooten, W, and Bergs, J. Clinical placement experience of nursing students during the COVID-19 pandemic: a cross-sectional study. Nurse Educ Today. (2021) 99:104746. doi: 10.1016/j.nedt.2021.104746
73. Şimşir, Z, Koç, H, Seki, T, and Griffiths, MD. The relationship between fear of COVID-19 and mental health problems: a meta-analysis. Death Stud. (2021) 46:515–23. doi: 10.1080/07481187.2021.1889097
74. Knipe, D, Evans, H, Marchant, A, Gunnell, D, and John, A. Mapping population mental health concerns related to COVID-19 and the consequences of physical distancing: a Google trends analysis. Wellcome Open Res. (2020) 5:82. doi: 10.12688/wellcomeopenres.15870.1
Keywords: post-traumatic stress disorder, resilience, fear, intern nursing students, COVID-19, China
Citation: Sun Y, Li X, Liu H, Li X, Sun L, Zhang L, Wang C, Li J, Liu M, Zhang D, Lei Y and Yuan T (2024) PTSD prevalence and factors in intern nursing students after COVID-19 full liberalization in China: a cross-sectional study. Front. Public Health. 12:1374977. doi: 10.3389/fpubh.2024.1374977
Edited by:
Yoshihisa Fujino, University of Occupational and Environmental Health Japan, JapanReviewed by:
Antonella Bodini, National Research Council, ItalyAneta Grochowska, University of Applied Sciences in Tarnow, Poland
Copyright © 2024 Sun, Li, Liu, Li, Sun, Zhang, Wang, Li, Liu, Zhang, Lei and Yuan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ting Yuan, eXVhbnRpbmdAd25tYy5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
 Yuanhao Sun
Yuanhao Sun Xiangdong Li2†
Xiangdong Li2† Lin Zhang
Lin Zhang Dongmei Zhang
Dongmei Zhang Ting Yuan
Ting Yuan