- 1Department of Media and Communication, City University of Hong Kong, Hong Kong SAR, China
- 2School of Media and Communication, Shenzhen University, Shenzhen, China
Background: Vaccination was a critical step in combating the COVID-19 outbreak, but vaccine hesitancy was a prominent global concern in the pandemic. In China, the behavior of vaccination might be affected by the past vaccine-related scandals.
Objective: This study investigated the factors contributing to vaccine hesitancy in China, with a focus on trust, vaccine risk perception, and self-efficacy. It aims to explore the predictors and mechanisms that influence vaccine hesitancy in China during the pandemic.
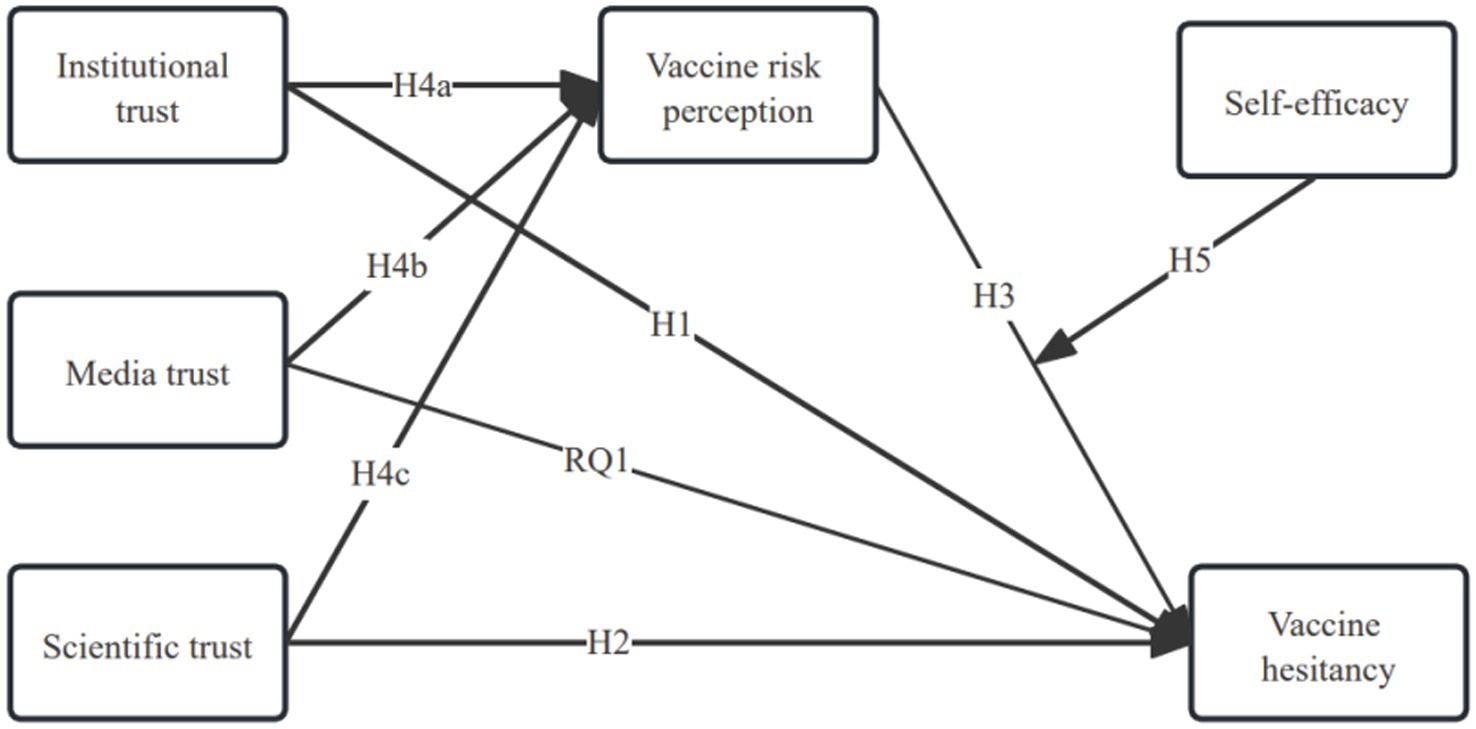
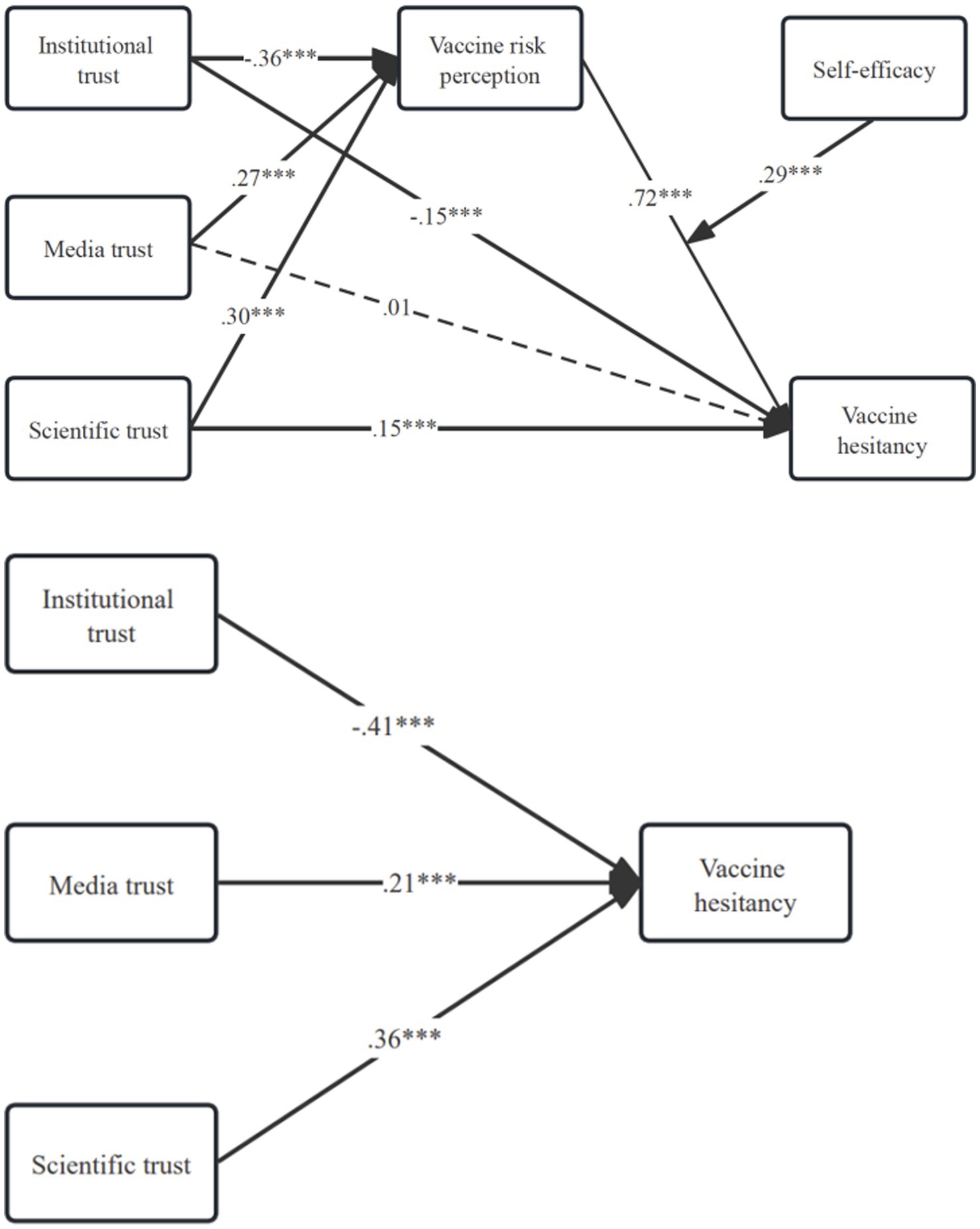
Method: The study utilized a national survey fielded in 2021, with a representative sample of 3,000 Chinese adults. Quota sampling was employed to ensure regional and demographic representation of the sample. Key variables including institutional, media, and scientific trust, vaccine risk perception, and self-efficacy were measured adopting established scales from previous studies. A mediated moderation model was proposed. Trusts were hypothesized to affect vaccine hesitancy through vaccine risk perception. Moderation effect of self-efficacy on the relationship between vaccine risk perception and vaccine hesitancy was also proposed. Mediated moderation regressions were performed for model estimation.
Results: Our analyses show that institutional trust was negatively associated with vaccine hesitancy [b = −0.41, p < 0.001, 95% CI (−0.47, −0.35)], while scientific trust and media trust was positively associated with vaccine hesitancy [b = 0.36, p < 0.001, 95% CI (0.32, 0.40); b = 0.21, p < 0.001, 95% CI (0.15, 0.27)]. Vaccine risk perception was also positively associated with vaccine hesitancy [b = 0.72, p < 0.001, 95% CI (0.68, 0.76)], with self-efficacy moderating the relationship. The relationship was more profound among those who had higher self efficacy [b = 0.29, p < 0.001, 95% CI (0.21, 0.37)]. Additionally, the mediating effects of vaccine risk perception were found.
Conclusion: The findings revealed that trust in institutions significantly reduced vaccine hesitancy by lowering perceived risks. In contrast, media and scientific trust heightened vaccine risk perception and hesitancy. Additionally, the study demonstrated the role of self-efficacy in moderating these effects.
Introduction
Effective vaccines for COVID-19 were a significant development that had the potential to reduce the risk of infection from the virus and mitigate the seriousness of the syndrome. Vaccination was a critical step in combating the COVID-19 outbreak (1). While a certain degree of vaccine hesitancy has been observed among the public for a variety of vaccines (1–3), The development and deployment of the COVID-19 vaccine elicited a notable level of public apprehension. A study that was conducted in 2020 during the pandemic found that approximately 25% of the American and 20% of the Canadian respondents were not willing to get vaccinated even if a COVID-19 vaccine were available (3). In the United Kingdom, 16.6% of respondents were very uncertain about COVID-19 vaccination, and 11.7% indicated strong hesitation (4). Similar reports have shown hesitancy regarding COVID-19 vaccines in other countries (2, 5–7).
In China, COVID-19 vaccine hesitancy was also present during the pandemic. Nearly half of those contacted indicated that they would wait to receive a vaccination until its safety was confirmed (2, 5). China is where the virus was initially identified, and the country has since implemented rigorous public health policies. Following the initial outbreak, the country enforced stringent containment measures; however, the subsequent relaxation of these policies led to widespread transmission across the nation (8). The lifting of the dramatic zero-COVID policy necessitated renewed vaccination drives, mainly targeting vulnerable populations such as older people, to address the challenges posed by new virus variants and ensure widespread immunity (9). However, despite the implementation of a national immunization program, concerns have been raised in China for a long time over the vaccine’s safety and efficacy (10).
Vaccine hesitancy can be defined as a delay in the acceptance or refusal of vaccines despite the availability of vaccination services (11). The 3Cs model proposed by the World Health Organization posits that vaccine hesitancy could be attributed to complacency, convenience, and confidence (12). Among the three factors, confidence appears to be the most salient in China in view of vaccine incidences in the past (13, 14). In this case, confidence refers to how safe people think a vaccine is. It is also related to a person’s confidence in the organizations and people in charge of developing and delivering immunization programs (15). Trust is one of the essential factors that influences vaccine confidence, and trust can be conceptualized with different dimensions (2). In this research, we focused on three facets of trust: institutional, media, and scientific trust.
Institutional trust refers to the public’s belief in the healthcare system’s capability and reliability. It plays a critical role in ensuring that people seek medical care, adhere to treatments, and accept health-related policies. Trust wanes when there are doubts regarding the healthcare system’s quality, openness, and ease of access, which are crucial for positive health outcomes (16). Gilson (17) and Freedman (18) underscore that trust is fundamental to how healthcare functions as a part of society.
Media trust refers to people’s trust in a variety of media outlets. The media historically serve as the primary vehicle for health intervention strategies, significantly influencing public health outcomes (19). Trust in the media is critical for the dissemination and acceptance of health-related information; it affects the extent to which the public adheres to health advisories (20) and engages in recommended health behaviors (21). During the COVID-19 infodemic, widespread misinformation and echo chambers—often reinforced by social media algorithms—undermined confidence in mainstream media and intensified vaccine hesitancy (22–24). Research on media trust during the pandemic further shows that these mechanisms systematically shaped perceptions of information credibility, amplifying doubts about vaccination (25).
Scientific trust refers to the public’s confidence in scientific knowledge, which has been deemed crucial for managing global challenges, such as the COVID-19 pandemic (26–28). Specifically, scientific trust impacts how citizens perceive crises and to what extent they accept related measures (29).
Recent studies have demonstrated that trust plays a complex role in shaping vaccine uptake. For example, the interplay between trust and COVID-19 information consumption was found to significantly influence vaccine and booster uptake (30), Similarly, patterns of news consumption and trust in public health leadership have been shown to shape COVID-19 knowledge and prejudice (31). Patterns of news consumption and trust in public health leadership have been shown to shape COVID-19 knowledge and prejudice (32). These findings suggest that the effects of trust are context-dependent, operating differently across populations and information environments.
Risk perceptions of vaccines is another psychological factor that influences vaccine hesitancy. In China, vaccine hesitancy, deeply influenced by the risk perceptions of vaccines, has posed major challenges to public health. Concerns over vaccine safety induced by past vaccine incidents negatively affect the success of vaccination programs, which are crucial for managing infectious diseases (33). The country’s unique socio-cultural and healthcare contexts require research specifically tailored to Chinese vaccine risk perceptions. However, empirical evidence from China can also provide valuable contributions to global efforts to address vaccine hesitancy (34, 35).
Vaccine hesitancy and trust
Vaccine hesitancy, characterized as a delay in the acceptance or refusal to receive vaccines despite their availability, is influenced by safety concerns, complacency, and inconvenience (11). Trust is a crucial determinant in the decision-making process related to immunization. Public trust in vaccine safety and its influence on immunization refusal has been well documented, while distrust has been found to amplify perceived risks and contribute to increased hesitancy (36, 37). Additionally, Sinuraya et al. (38) highlighted that diminished confidence in authoritative institutions and media further exacerbates skepticism toward vaccines.
During health crises, trust in information sources has significantly influenced information-seeking behavior and the acceptance of health recommendations (39, 40). In addition, healthcare providers play a pivotal role in engendering trust in scientific and epidemiological evidence, thereby affecting vaccination uptake (41, 42).
Scientific trust, which is closely related to public confidence in scientific research regarding vaccine efficacy and safety, played a significant role during the pandemic. This concept affects the public due to their increasing exposure to scientific debates; its potential effect on public perception and health-related behavior has been highlighted often in the literature (43–45).
Institutional trust
Trust in social institutions is based on beliefs in their capability to achieve desired goals effectively and in their commitment to act in the public’s best interests (46–48). As demonstrated in recent studies, institutions providing health information, such as health authorities and advisory bodies, have played a pivotal role in shaping vaccination intentions and behaviors (49).
There is a relationship between individuals’ willingness to be vaccinated and their level of trust in medical professionals, healthcare systems, and the pharmaceutical industry. Higher levels of trust generally indicate stronger intentions to be vaccinated, highlighting the importance of institutional trust in entities such as hospitals and public health agencies (50, 51). For example, it was found that a lower level of institutional trust led to negative attitudes toward vaccines during an Ebola outbreak (52). In Italy, greater trust in national healthcare institutions was found to predict a higher level of willingness to receive vaccines (53). In Saudi Arabia, the decision to receive a COVID-19 vaccine was found to be strongly influenced by trust in the healthcare system, which appeared to outweigh concerns over the virus’s perceived dangers (54).
Studies have shown that the relationships between healthcare providers and patients might account for the link between institutional trust and vaccination intention. Trust in doctors’ recommendations of vaccination facilitates positive doctor–patient communication and improves attitudes toward vaccination (55). Healthcare workers are often more trusted than other sources and, during the COVID-19 pandemic, were viewed as reliable sources of vaccine information (55–60).
Based on the discussion above, we hypothesized the following:
H1: A higher level of institutional trust will be associated with a lower level of vaccine hesitancy.
Media trust
The media’s role as a primary source of health-related information was heightened during the COVID-19 pandemic. Garfin et al. (61) showed that the media acts as a crucial channel through which the public accesses information about health-protective behaviors. The unique position of mass media in communicating risks has been noted by Cottle (62) and Garfin et al. (61), emphasizing its influence in shaping public risk perceptions.
Social media platforms, such as Facebook and Twitter, have served as vital channels for disseminating disease-related information (63–65). However, the credibility of information on these platforms can be affected by personal relationships and trust dynamics within individual users’ networks (66–68). It is strengthened when positive opinion leaders endorse health messages, potentially increasing public trust in the media (69).
In contrast, the prevalence of misinformation in the media, especially social media, presents significant challenges to public health. Misleading content and conspiracy theories proliferating on these platforms have been found to be associated with increased vaccine hesitancy (70–72). The lack of regulatory oversight on social media can exacerbate this issue, leading to a heightened perception of risk regarding COVID-19 vaccines (72, 73). Given this issue, media trust may paradoxically lead to increased perceived vaccine risks and hesitancy.
Therefore, we asked the following:
RQ1: What are the effects of media trust on vaccine hesitancy?
Scientific trust
Scientific trust refers to individuals’ confidence in scientific knowledge and expertise, especially during pandemics (56, 74, 75). Studies have shown that scientific trust is positively associated with adherence to pandemic measures and vaccination uptake (76–78). Moreover, trust in the scientific community has been identified as a decisive factor in encouraging individuals to vaccinate (51, 79).
In the context of a pandemic, cognitive trust—or confidence in scientific knowledge—is paramount (80). It involves a first-order scientific reasoning process through which individuals utilize scientific knowledge for problem solving and decision-making (81, 82). For example, the 2018 Wellcome Global Monitor survey revealed that a social consensus on science might foster a collective acknowledgment of the benefits of vaccination (83). General scientific knowledge is instrumental in acquiring specific virus-related knowledge and can influence risk perception and vaccine acceptance (84). Therefore, we can reasonably argue that individuals with higher scientific trust will be more engaged with vaccination information, thereby increasing their confidence in receiving vaccinations.
Based on the discussion above, we proposed the following:
H2: A higher level of scientific trust will be associated with a lower level of vaccine hesitancy.
Vaccine risk perception and vaccine hesitancy
A key persistent risk is that people, communities, or society might be harmed at a certain time and location (85). Perceived risk refers to people’s subjective attitudes, beliefs, and judgments about potential dangers (86). The overall perception of individual health threats includes two dimensions: perceived severity and perceived susceptibility. The former refers to people’s subjective judgments of the severity of the consequences caused by health threats, while the latter refers to people’s judgments of the probability of being affected by these health threats (87).
In the current research, risk perception is focused on the perceived risk of the COVID-19 vaccine, emphasizing individuals’ subjective perceptions of the potential hazards associated with being vaccinated. Public vaccine hesitancy can be attributed to the potential risk associated with a vaccine (88, 89). The public’s confidence in the safety of vaccinations has been weakened by the frequent occurrence of vaccine scandals. Every year, there are many worldwide incidents of vaccine-induced diseases, disabilities, and even deaths, which increases people’s concerns about the safety of vaccines (90–92). For example, Changsheng Bio-technology, one of China’s largest vaccine producers, provided children with over 250,000 doses of an inferior pertussis vaccine in 2018. These inferior vaccines were manufactured using outdated ingredients accompanied by false batch numbers and manufacturing documents (93–95). This issue induced large-scale criticism of the vaccine industry in China. As a result, even vaccines that were not produced by the involved manufacturer were suspected with regard to their safety.
The case of the COVID-19 vaccines was very unique compared to other vaccines that had been previously used. Their development, clinical trials, and approval for use as an emergency public health product were conducted in a very short time, and there was seemingly insufficient proof of potential long-term effectiveness (96). Because of this, the public might be understandably skeptical about receiving a seemingly new vaccine in terms of a lack of assurance in terms of side effects.
One of the reasons for vaccine hesitancy is uncertainty about the vaccines used. Over the past 10 years, more than 10 vaccine crisis events have occurred in China, which has hurt public confidence in vaccines in general (2, 93, 94, 97, 98). In contrast, the danger presented by COVID-19 might have overshadowed the public’s worries about problematic vaccines (97), making people more likely to receive COVID-19 vaccination when it became available. Based on this discussion, we proposed the following:
H3: A higher level of vaccine risk perception will be associated with a higher level of vaccine hesitancy.
Trust, vaccine risk perception, and vaccine hesitancy
Vaccine hesitancy may be correlated with several factors: the public’s trust in government and healthcare officials has been inconsistent; the legitimacy of science has faced scrutiny; social media platforms have enabled a wider dissemination of dramatic personal experiences; and significant public health and vaccine anxieties have been prevalent in the media (88, 99). These components, collectively, might have influenced individuals’ reluctance to vaccinate.
Trust in healthcare providers and authorities is foundational to the acceptance of medical interventions (17). A link between trust in vaccines and vaccination uptake has been documented, highlighting the mitigating effect of trust on vaccine hesitancy (51). Vaccine risk perception can be reasonably argued as exerting a mediating role in this relationship. Individuals with higher trust in vaccine benefits and safety tended to perceive lower risks associated with vaccines, which increased the rate of vaccine acceptance (100). In contrast, those with diminished trust are prone to perceive higher risks, leading to increased hesitancy (88). The importance of risk perception is further emphasized when a new vaccine is developed. During the initial rollout of COVID-19 vaccines, risk perception was a critical determinant of public willingness to receive the vaccine (59). The interplay among media trust, vaccine risk perception, and vaccine hesitancy was identified as crucial for understanding public health compliance, particularly during global health emergencies such as the COVID-19 pandemic. Media trust significantly influenced public attitudes toward vaccines, as individuals commonly sought health information from media sources (51). Credible media outlets are likely to enhance vaccine uptake by reducing the perceived risks associated with vaccines (101). Conversely, mistrust in the media was found to intensify vaccine hesitancy by amplifying perceived risks (102).
While scientific trust typically fosters compliance with health measures, paradoxically, it may also lead to heightened vaccine risk perceptions due to the critical evaluation of scientific communications and potential side effects. Therefore, individuals’ exposure to scientific information must also consider how that information is perceived and used; it can manifest in proactive engagement with health behaviors and increased vigilance regarding health interventions. Beck’s concept of reflexive conscientization articulates this dynamic, suggesting that informed skepticism is a feature of contemporary attitudes toward science, including pandemic and vaccine safety (103, 104). Following this logic, we argue that individuals with higher scientific trust may be more engaged with vaccination information. They may also exhibit a higher risk perception of a vaccine due to their critical evaluation of scientific claims and concerns about vaccines, thereby increasing vaccine hesitancy.
Based on the discussion above, we propose the following:
H4a: Vaccine risk perception will mediate the relationship between institutional trust and vaccine hesitancy.
H4b: Vaccine risk perception will mediate the relationship between media trust and vaccine hesitancy.
H4c: Vaccine risk perception will mediate the relationship between scientific trust and vaccine hesitancy.
The role of self-efficacy
Self-efficacy is defined as an individual’s belief in their capabilities to execute behaviors necessary to achieve specific goals (105). In the context of health communication, self-efficacy plays a pivotal role in influencing health behaviors, including vaccination decisions (106). It pertains to an individual’s belief in their capacity to modify habits and manage their functions when encountering challenges (107). Research has consistently shown that individuals with higher levels of self-efficacy are more likely to engage in health-promoting behaviors (108).
In the health belief model (HBM), self-efficacy is a critical factor in comprehending and tackling vaccine hesitancy. The HBM proposes that health behaviors are influenced by personal beliefs about health threats, the perceived benefits of and barriers to action, and cues to action (109, 110). Self-efficacy—the belief in one’s ability to perform a behavior—is found to moderate these influences, especially in the context of vaccine hesitancy (108, 111).
Past research has shown that self-efficacy independently predicts not only the intention to vaccinate (112) but also actual vaccination behavior (113, 114). A Hong Kong survey on the human papilloma virus (HPV) vaccination revealed that self-efficacy significantly influenced the uptake of the vaccine among physicians and nurses. It was determined that self-efficacy was the sole significant cognitive and background variable correlated with the acceptance of the HPV vaccine by these healthcare professionals (115). Intervention strategies targeted at increasing self-efficacy have been confirmed to be successful in fostering vaccine acceptance (116). Health communications that inform individuals with the necessary skills and resources increase confidence in being vaccinated, consequently reducing hesitancy (117). Interventions that contained components designed to enhance self-efficacy, such as skill-building activities and empowerment strategies, were more effective at reducing vaccine hesitancy (118). These findings suggest that self-efficacy might be a potential factor that interacts with other predictors within the HBM framework. Therefore, we proposed the following:
H5: Self-efficacy will moderate the relationship between vaccine risk perception and vaccine hesitancy.
Integrating the hypothesized relationships, a mediated moderation model was proposed. The theoretical model is shown in Figure 1.
Materials and methods
Sample
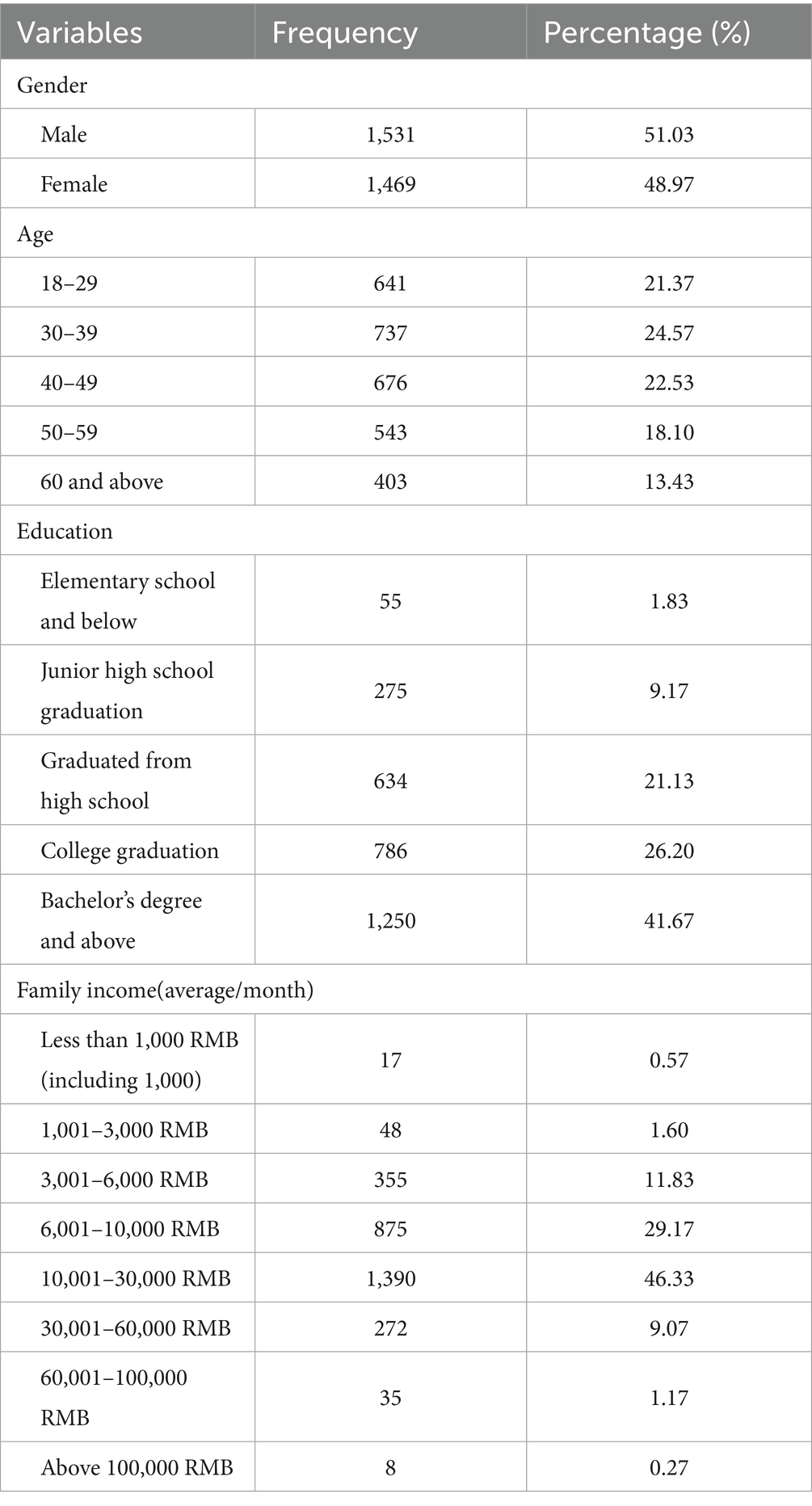
The study was conducted in China from May 31 to July 10, 2021. During that period, the Chinese government deployed a zero-COVID policy nationally. Cross-sectional data were collected through a survey commissioned to a commercial survey research company. To achieve a representative sample, a quota sampling method was employed. The most up-to-date CNNIC (China Internet Network Information Center) report was used to establish the quotas for group subcategories of gender, age, and education (119). The final sample comprised 3,000 Chinese citizens aged 18 and older, with a response rate of 31.96%, calculated following the American Association for Public Opinion Research (AAPOR) standard definition RR1 (120). Although modest, the response rate was acceptable compared to other large-scale online surveys. Quota sampling was used to mitigate potential non-response bias and improve representativeness. The demographic breakdown was 51.03% male and 48.97% female, with ages ranging from 18 to over 60. Approximately 75.5% of respondents reported a monthly household income between 6,000 and 30,000 yuan, and 67.93% held a college degree or higher. Participants were drawn from all major regions of mainland China (East, Central, and West). Urban residents were slightly overrepresented, reflecting the demographic profile of China’s internet users. The skewness toward urban and highly educated participants should be considered when interpreting generalizability of the results. It was further addressed in the Limitations section. The demographic characteristics of the sample are shown in Table 1. The study was approved by the Institutional Review Board of Shenzhen University.
Measures
Control variables
Prior studies have demonstrated that certain demographic factors, including gender, age, education, and income, influence a wide range of behaviors that could be related to the health behaviors examined in this study. Thus, to avoid the potential confounding effects of these variables, we included them as controls in our analysis.
Media trust
Media trust was measured using a five-point Likert scale (1 = completely distrust, 5 = completely trust). Respondents were asked about their trust in central government media, local media, commercial media, social media platforms, search engines, bulletin board systems (BBSs), video apps, and prominent bloggers. These categories reflect the most prominent information channels in China’s media environment. The items were designed based on prior comparative studies of media trust (121, 122) but adapted to the Chinese context.
Institutional trust
Institutional trust was measured using a five-point Likert scale (1 = completely distrust, 5 = completely trust). Respondents indicated their trust in the central government, local governments, police departments, and educational institutions. The measurement draws conceptually from established frameworks of political and institutional trust (123, 124), while tailoring the items to the Chinese governance system.
Scientific trust
Scientific trust was measured using a five-point Likert scale (1 = completely distrust, 5 = completely trust). Respondents were asked about their trust in the knowledge conveyed by scientific researchers and the role of science in different settings. Items were adapted from established surveys on public attitudes toward science, including the U. S. National Science Board’s Science and Engineering Indicators and the European Commission’s Eurobarometer on Science and Technology, which have been widely used to assess trust in science and perceptions of scientists (125, 126). The wording was slightly modified to fit the context of COVID-19.
Vaccine risk perception
Vaccine risk perception was measured using a four-point scale (1 = definitely wrong, 4 = definitely right). Respondents evaluated statements such as “getting vaccinated can cause COVID-19 infection,” “the vaccine’s effectiveness lasts for only a short period, therefore, there is no need for it,” and “people who receive domestic vaccines are likely to experience significant side effects.” These items were adapted from the WHO Vaccine Hesitancy Survey Module (127) and the Vaccine Confidence Project (128), which emphasize concerns about safety, efficacy, and necessity.
Self-efficacy
Self-efficacy was measured using a five-point Likert scale (1 = strongly disagree, 5 = strongly agree). Respondents evaluated statements including “I will encourage those who are close to me to get COVID-19 vaccinations,” “I am very concerned about the COVID-19 vaccine information,” “I believe I have received sufficient information about the COVID-19 vaccine,” and “I will express my opinion about the COVID-19 vaccine on the internet.” These items were adapted based on the Health Belief Model self-efficacy framework (129) and revised to reflect vaccination-related behaviors in the Chinese context.
Vaccine hesitancy
Vaccine hesitancy was measured using a five-point Likert scale (1 = strongly disagree, 5 = strongly agree). Respondents evaluated statements such as “I worry about the side effects of receiving the COVID-19 vaccine,” “I suspect the effectiveness of the COVID-19 vaccine,” “I am concerned about the safety of the COVID-19 vaccine,” and “I lost my confidence with the COVID-19 vaccine due to previous vaccine-related experiences.” These items were adopted from the WHO Vaccine Hesitancy Survey Module (127) on vaccine hesitancy and aligned with the “confidence” dimension of the 5C model (100), with further adjustments to reflect Chinese vaccine scandals.
All the multi-item constructs showed acceptable internal consistency (Cronbach’s α > 0.70). Forward–backward translation procedures ensured accuracy of the Chinese version, and a pilot test with a small group of Chinese respondents confirmed item clarity and cultural relevance.
Data analysis
Data quality was ensured by screening for incomplete or inconsistent responses. Any missing data were handled using listwise deletion, as the proportion of missing responses was low (<2% for key variables). Sensitivity checks confirmed that the demographic profile of the retained sample did not significantly differ from the original before deletion, and all analyses were conducted on the cleaned dataset.
Data analysis was performed using SPSS version 26 and PROCESS macro version 4.1 (130). A descriptive statistical analysis and bivariate correlation analysis were first conducted, followed by estimation of the main effect model. In the second step, the mediation effect was tested using PROCESS Model 4. Finally, we tested the mediated moderation model was examined using PROCESS Model 14. Continuous variables were mean-centered before the analysis, and bootstrapping 5,000 samples with 95% confidence intervals was performed.
Results
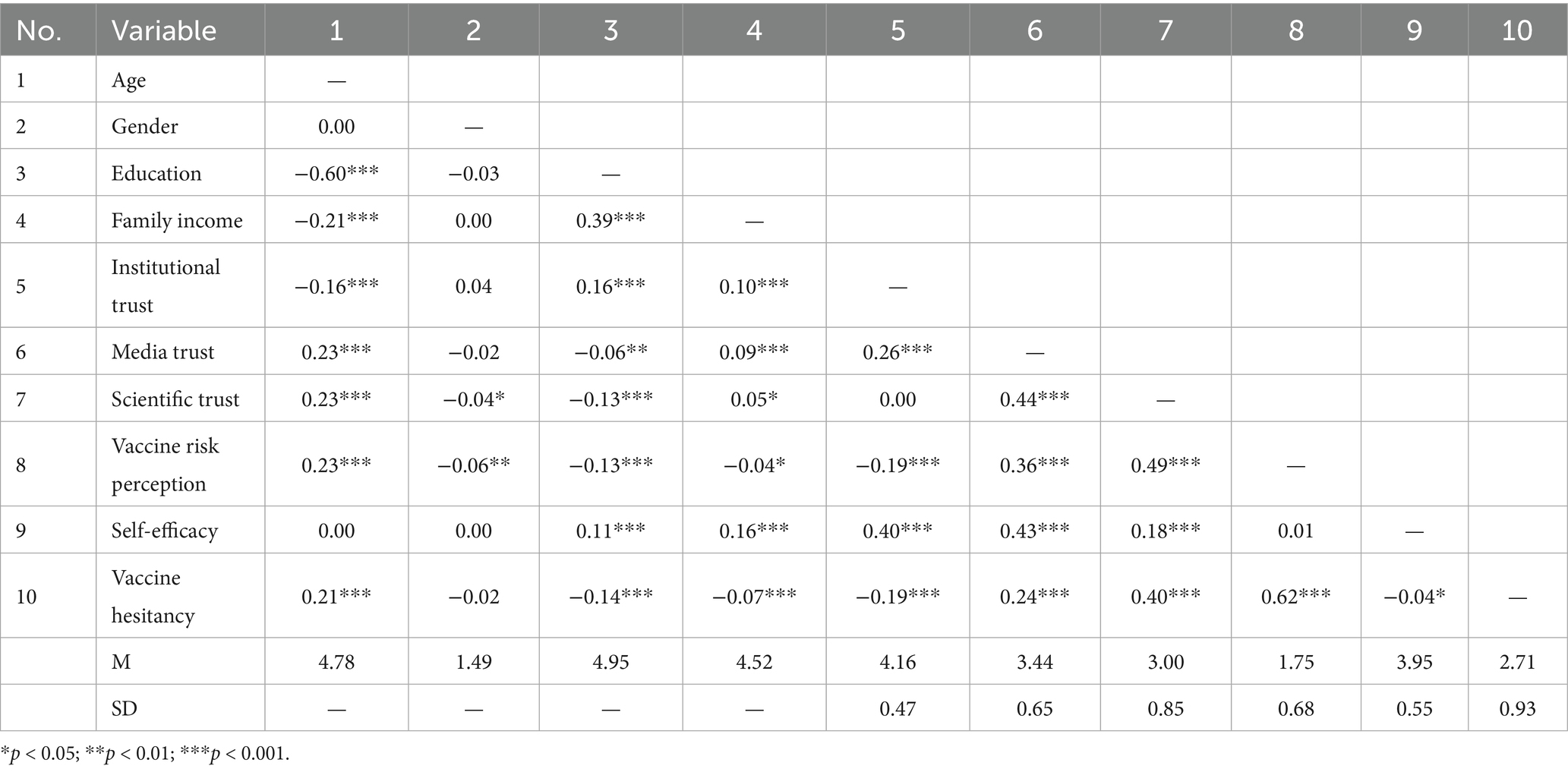
Descriptive statistics and correlations
We first performed a descriptive analysis of the main variables. The results revealed that respondents had a moderate level of trust in the media (M = 3.44, SD = 0.65, Cronbach’s α = 0.89), while institutional trust was relatively high (M = 4.16, SD = 0.47, Cronbach’s α = 0.73). Trust in the central government was rated the highest, with 67.6% of participants assigning it the highest score of 5. Scientific trust was at a moderate level (M = 3.00, SD = 0.85, Cronbach’s α = 0.79). The level of vaccine risk perception was also moderate (M = 1.75, SD = 0.68, Cronbach’s α = 0.88). Approximately 46.8% of the respondents firmly rejected the idea that recipients of domestic vaccines were at a high risk of side effects.
The level of self-efficacy was generally positive (M = 3.95, SD = 0.55, Cronbach’s α = 0.75). Over 86% of the respondents agreed or strongly agreed with encouraging vaccination, and approximately 79% were proactive in seeking and sharing vaccine information.
According to our scale, the level of vaccine hesitancy was moderate (M = 2.71, SD = 0.93, Cronbach’s α = 0.89). Respondents expressed the most concern about the side effects, efficacy, and safety of the vaccines. In addition, there were concerns about economic factors, fears of counterfeit vaccines, and past negative experiences.
The Pearson correlation analysis revealed significant correlations between the independent variables (institutional trust, media trust, and scientific trust) and the dependent variable (vaccine hesitancy). Institutional trust showed a weakly negative correlation (r = −0.19), while media trust and scientific trust exhibited positive correlations (r = 0.24) and (r = 0.40), respectively, with vaccine hesitancy. Vaccine risk perception and vaccine hesitancy showed a strong correlation (r = 0.62). Since all the correlation coefficients fell below the 0.7 threshold, collinearity could be excluded for the variables studied (see Table 2).
Hypothesis testing
H1 posited that a higher level of institutional trust would be associated with a lower level of vaccine hesitancy. As shown in Table 3, there was a significant negative association between institutional trust and vaccine hesitancy [Model 1; b = −0.41, p < 0.001, 95% CI (−0.47, −0.35)], supporting H1.
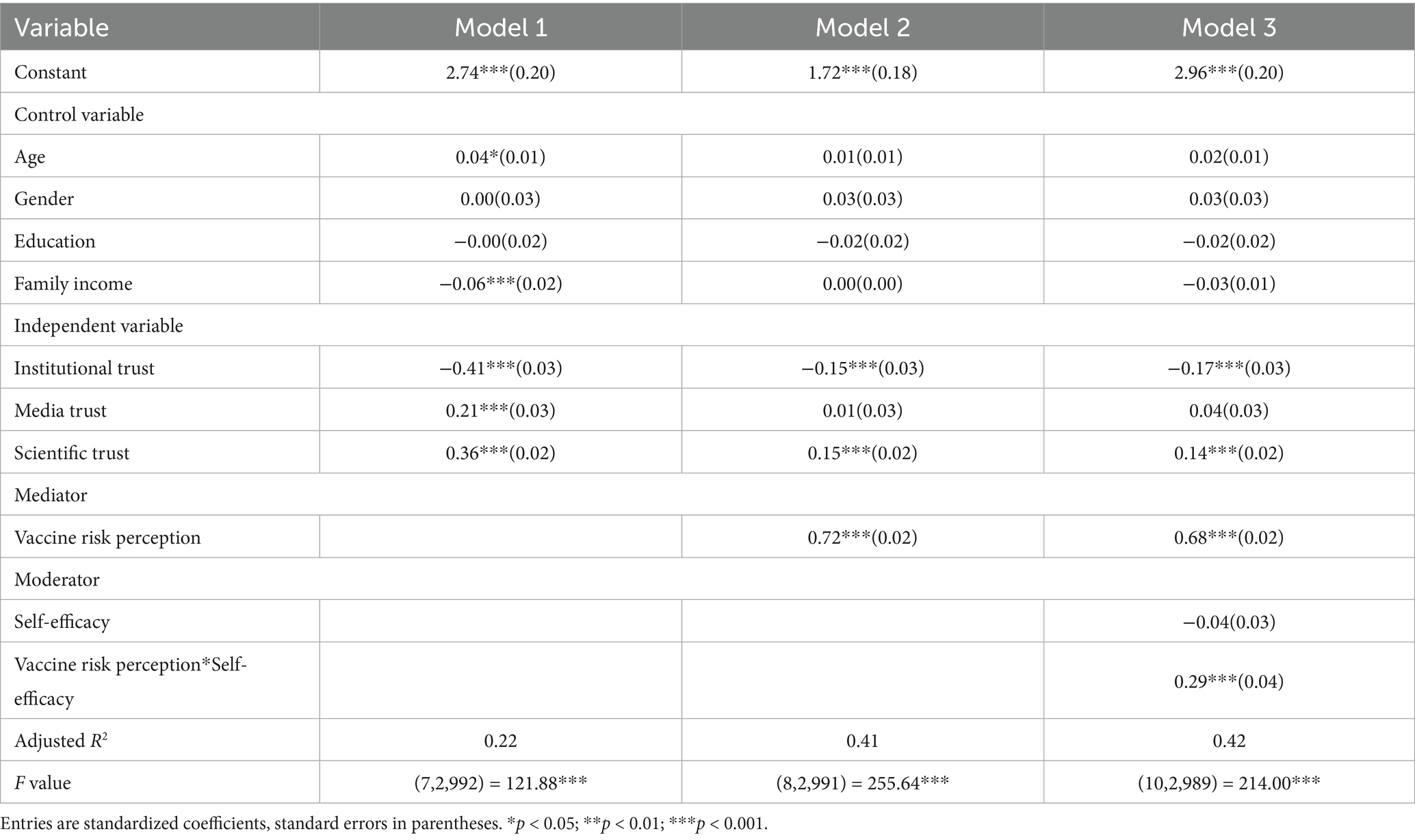
Table 3. Regression analysis of the main effect, mediation effect, and mediated moderation effect on vaccine hesitancy (N = 3,000).
RQ1 inquired about the impact of media trust on vaccine hesitancy. A positive association between media trust and vaccine hesitancy was observed [Model 1; b = 0.21, p < 0.001, 95% CI (0.15, 0.27)], indicating that a higher level of media trust would lead to a higher level of vaccine hesitancy.
H2 proposed that a negative association existed between scientific trust and vaccine hesitancy. As the results show, scientific trust was positively related to vaccine hesitancy [Model 1; b = 0.36, p < 0.001, 95% CI (0.32, 0.40)], indicating that a higher level of scientific trust was linked to a higher level of vaccine hesitancy; thus, H2 was rejected.
H3 proposed that there was a positive association between vaccine risk perception and vaccine hesitancy. Vaccine risk perception was positively associated with vaccine hesitancy [Model 2; b = 0.72, p < 0.001, 95% CI (0.68, 0.76)], supporting H3.
H4a–H4c proposed that vaccine risk perception would mediate the relationships between the trust variables and vaccine hesitancy. The indirect effects of institutional, media, and scientific trust on vaccine hesitancy via vaccine risk perception were examined using Model 4 of the PROCESS Macro. The bootstrapping method (with 5,000 resamples) yielded 95% confidence intervals for indirect effects that did not include zero (institutional trust: −0.29, −0.23; media trust: 0.17, 0.22; scientific trust: 0.19, 0.24). These results indicated that vaccine risk perception served as a mediator in the relationships between each trust variable and vaccine hesitancy, thus supporting H4a–H4c. Although significant, the effect sizes were modest, accounting for roughly 10–15% of the variance in hesitancy outcomes, which is consistent with effect sizes reported in prior health communication research. It suggests that while risk perception is an important mechanism, other psychological or contextual factors possibly exist to account for the mediated paths.
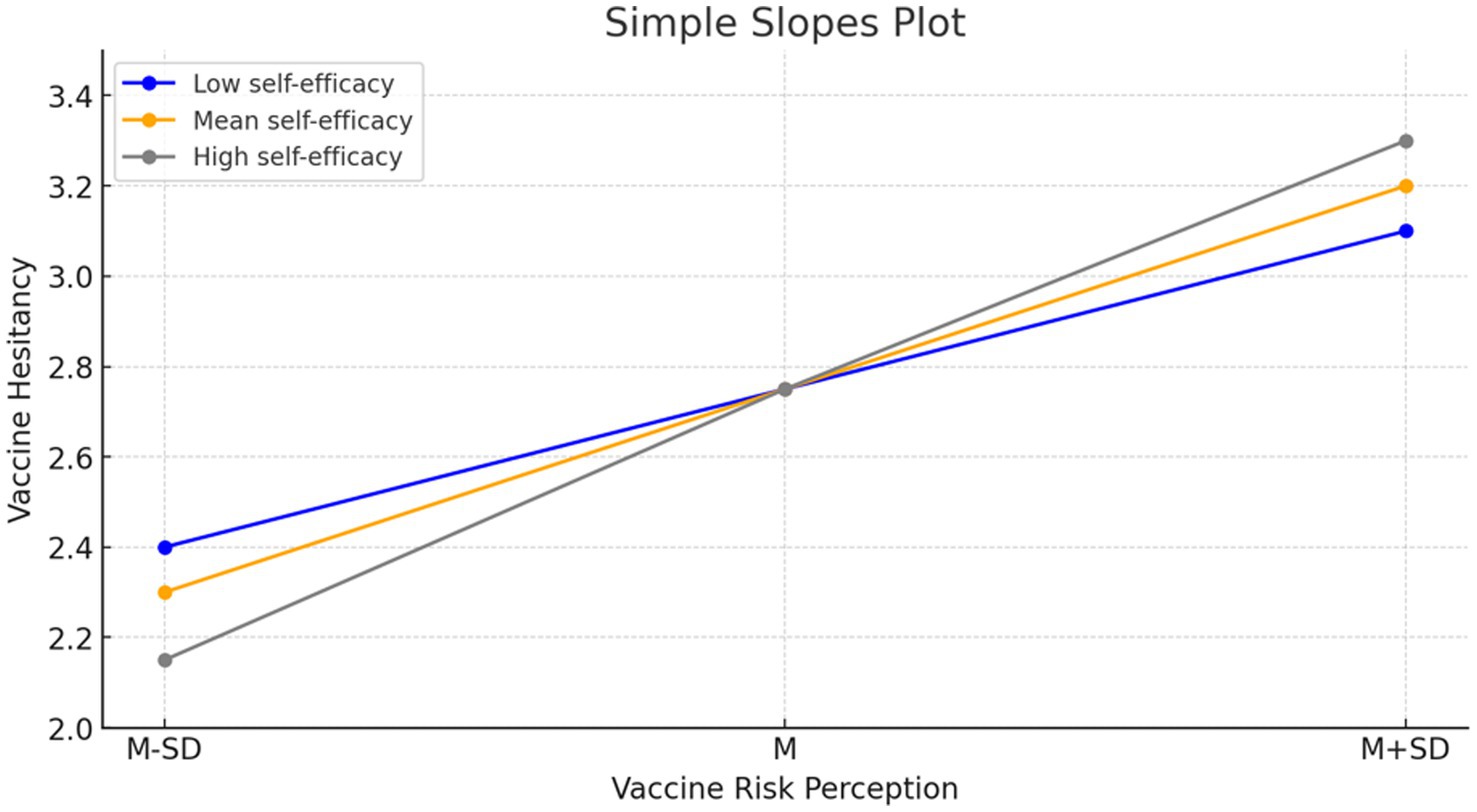
H5 proposed that self-efficacy moderated the relationship between vaccine risk perception and vaccine hesitancy. We found that the moderating effect was significant [Model 3; b = 0.29, p < 0.001, 95% CI (0.21, 0.37)]. The conditional effect was evidenced in that the 95% confidence intervals from the PROCESS Macro Model 14 analysis did not encompass zero (M – 1 SD: 0.45, 0.59; M: 0.63, 0.72; M + 1 SD: 0.78, 0.89). Specifically, the impact of vaccine risk perception on vaccine hesitancy was more intense among individuals with low self-efficacy. In contrast, individuals with high self-efficacy demonstrated low vaccine hesitancy at a lower risk perception level, while increased perceived risk significantly amplified hesitancy among these individuals (see Figure 2). H5 was supported.
The analysis revealed that self-efficacy moderated the relationship between trust and vaccine hesitancy. A negative indirect effect of institutional trust on vaccine hesitancy was observed; it became more intense with increasing self-efficacy (−0.19 at M–1SD; −0.24 at M; −0.30 at M + 1SD). The coefficients at one standard deviation below the mean, at the mean, and at one standard deviation above the mean were −0.19, −0.24, and −0.30, respectively. In contrast, media trust and scientific trust were positively associated with vaccine hesitancy. This association was strengthened at higher levels of self-efficacy, with effect sizes escalating from 0.14 to 0.22, and 0.16 to 0.25. These nuanced findings underscore the multifaceted interplay among trust, self-efficacy, and risk perception in the context of vaccine hesitancy, suggesting that the nature of trust and the level of self-efficacy coalesce to shape perceptions of vaccine risk and the intensity of hesitancy (see Table 4). The overall evaluations are illustrated in Figure 3.
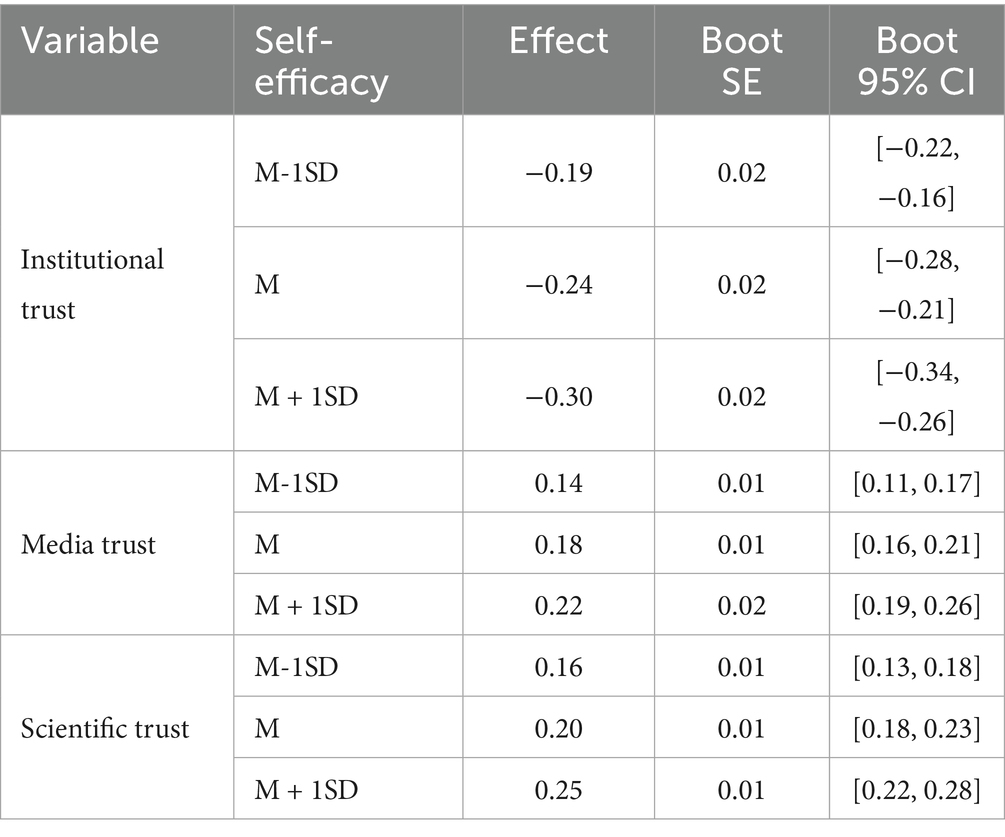
Table 4. Conditional indirect effects of trust variables on vaccine hesitancy moderated by self-efficacy.
Taken together, the mediated moderation analysis showed that the indirect effects of institutional, media, and scientific trust on vaccine hesitancy via risk perception were consistently significant, with effect sizes ranging from small to moderate (|b| = 0.14–0.30). Importantly, these indirect effects were contingent on self-efficacy levels, as visualized in Figure 3: higher self-efficacy amplified both the protective role of institutional trust and the risk-enhancing effects of media and scientific trust. It shows a clear interpretation of how trust and self-efficacy jointly shape vaccine hesitancy.
Discussion
The present study aimed to investigate the relationships among trust in institutions, media, and science; vaccine risk perception; self-efficacy; and vaccine hesitancy. The findings of the study provide insights into the factors that contribute to vaccine hesitancy and highlight the importance of vaccine risk perception and self-efficacy in the context of China, where a zero-COVID policy was deployed.
First, we found that institutional trust had a negative impact on vaccine risk perception and vaccine hesitancy. It is supported by recent evidence showing that individuals with lower institutional trust are more likely to exhibit vaccine hesitancy (131, 132). Similarly, Murphy et al. found that mistrust in authoritative information sources is linked to higher level of COVID-19 vaccine hesitancy in the UK and Ireland (133). Trust in the Chinese government and health authorities reduced hesitancy to obtain the COVID-19 vaccine. This suggests that although there were vaccine scandals in China in the past, people generally still had faith and confidence that the government and health authorities would supply a safe and effective COVID-19 vaccine. Interestingly, trust in science was associated with higher perceived vaccine risk and hesitancy. One explanation is that individuals who strongly trust science also tend to be more scientifically literate and thus more sensitive to uncertainties regarding the rapid development of COVID-19 vaccines. Prior research has shown that risk perception and health behaviors are not always linearly related—greater awareness of risks can sometimes reduce uptake (134). Another explanation is the “double-edged sword” of transparent communication: individuals with higher trust level may take scientific warnings about side effects or incomplete data more seriously, which can heighten caution (135). In the Chinese context, scientific trust often overlaps with reliance on official expert communication, so when messages emphasized uncertainties, those with higher trust were more likely to perceive greater risks (136). Trust in the media induced individuals to perceive that the COVID-19 vaccine was unsafe. Continuous arguments and discussions over vaccine issues during the pandemic period might have had a serious negative impact on citizens’ attitudes. Prior studies confirm that exposure to misinformation and conflicting information substantially reduces vaccination intent (137), and social media further amplified this effect, with widespread false claims contributing to hesitancy (138). In China’s media environment, censorship and selective exposure also played a role: while strict information control limited the spread of rumors, it also reduced transparency, potentially leading some individuals to question official narratives (139, 140). The factors—misinformation, censorship, and selective exposure—jointly shaped how citizens interpreted vaccine safety. Despite advocacy from state governments to promote vaccination, the amount of misinformation, conspiracy theories, and other disorienting types of information was overwhelming on social media, which might have negatively impacted attitudes toward the COVID-19 vaccine.
Second, in the study, we were able to conceptually describe how trust and skepticism influenced public health decisions in the very specific context of the epidemic in China. While having faith in health institutions was beneficial for the public’s desire to be vaccinated, self-efficacy was another critical factor that affected the process of health decision-making. Public health professionals should build trust and encourage people to be well informed and think critically. We found that the public was cautious due to the rapid development of the COVID-19 vaccine, suggesting that trust in science might even increase the skepticism of the public (as they possibly felt proper scientific procedures were not being followed). Cross-national surveys indicate that China had one of the highest estimated vaccine acceptance rates—nearly 90%—among 19 countries studied (141), and domestic data suggest that transparent communication, medical authority endorsements, and vaccination convenience significantly influence public acceptance within China (10). Scientific information, including transparent communication strategies explaining the scientific process and rigorous safety checks for vaccine development, might have provided more objective views on the safety and risks of the COVID-19 vaccine. People who make health decisions based on scientific information might have more concerns, especially about the unknown long-term effects of a new vaccine.
Third, the mediation effect of risk perception between trust in various entities (governmental institutions, media, and the scientific community) and vaccine hesitancy, as found in the study, suggests that fostering trust can attenuate hesitancy by influencing how the public perceives vaccine risks. The positive correlation between vaccine risk perception and hesitancy underscores the challenges posed by historical vaccine scandals, which have indelibly marked collective consciousness. The vaccine related incidents have led to measurable delays in vaccination schedules, as documented after the Changchun Changsheng incident (142). However, the Chinese government’s robust response to the COVID-19 pandemic, which prioritized transparency and safety, played a crucial role in reshaping these perceptions. This was evident during the pandemic when the government’s efforts to communicate effectively about the safety and efficacy of COVID-19 vaccines were instrumental in managing the public’s apprehension. Although transparent communication of vaccine risks may transiently affect uptake, it has been shown to build trust over time (135). Moreover, the psychological impact of compulsory vaccination warrants closer attention: while mandates can rapidly increase coverage, they may also provoke psychological reactance and reduce long-term trust in health authorities (143, 144). The dual effects highlight the need to balance public health goals with respect for individual autonomy, particularly in nations where collective responsibility is highly emphasized. In addition, the role of self-efficacy in moderating the relationship between vaccine risk perception and hesitancy is particularly notable. The results demonstrate that individuals with higher self-efficacy exhibited a more discerning response to vaccine risks, which can either diminish or amplify vaccine hesitancy. The Chinese government introduced mandatory vaccination policies during the pandemic. This policy aimed to achieve high vaccination rates rapidly to control the spread of the virus. While compulsory vaccination can ensure wide-range vaccine uptake, it can also provoke resistance among those who prioritize personal choice or have concerns about vaccine safety.
Limitations and conclusions
The study has a few limitations. First, the sample underrepresents older adults (only 13.4% were aged 60 or above), a key high-risk group, as well as rural residents. Generalization of the results should be made with caution. Second, the response rate was not high (31.96%), although acceptable, it raises the possibility of non-response bias (120). Participants who chose to respond may differ systematically from non-respondents—for instance, being more health-conscious or digitally active. Although quota sampling based on demographic benchmarks improved balance, the bias cannot be ruled out. Third, the measure did not distinguish between sub-dimensions of institutional trust (e.g., healthcare v.s. central government), which may exert distinct effects. Fourth, the survey data were collected during China’s “zero-COVID” policy period amid an active vaccination campaign, so the findings cannot fully extend to other contexts or time periods. Last but not least, the cross-sectional and self-reported design precludes causal inference and may be subject to social desirability bias. Despite these caveats, the study provides timely insights that should be interpreted with appropriate caution.
In conclusion, the study elucidates the dynamics among trust, vaccine hesitancy, vaccine risk perception, and self-efficacy. The findings revealed that trust in institutions significantly reduced vaccine hesitancy by lowering perceived risks. In contrast, media and scientific trust heightened vaccine risk perception and hesitancy. Additionally, the study demonstrated the role of self-efficacy in moderating these effects. This study identified several factors and mechanisms that contribute to vaccine hesitancy and provides insights for dealing with this important public health issue during times of crisis.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The requirement of ethical approval was waived by Institutional review board of Shenzhen University for the studies involving humans because Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board also waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because written informed consent from the participants was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
DH: Investigation, Writing – original draft, Methodology, Formal analysis, Conceptualization. YW: Data curation, Writing – review & editing, Project administration. HL: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Planning Project of Philosophy and Social Sciences in Shenzhen (Grant No. SZ2024B036).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
COVID-19, Coronavirus disease; CI, Confidence Interval; CNNIC, China Internet Network Information Center.
References
1. Pennycook, G, McPhetres, J, Bago, B, and Rand, DG. Beliefs about COVID-19 in Canada, the United Kingdom, and the United States: a novel test of political polarization and motivated reasoning. Personal Soc Psychol Bull. (2022) 48:750–65. doi: 10.1177/01461672211023652
2. Sallam, M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccine. (2021) 9:160. doi: 10.3390/vaccines9020160
3. Taylor, S, Landry, CA, Paluszek, MM, Groenewoud, R, Rachor, GS, and Asmundson, GJG. A proactive approach for managing COVID-19: the importance of understanding the motivational roots of vaccination hesitancy for SARS-CoV2. Front Psychol. (2020) 11:575950. doi: 10.3389/fpsyg.2020.575950
4. Freeman, D, Loe, BS, Chadwick, A, Vaccari, C, Waite, F, Rosebrock, L, et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (oceans) II. Psychol Med. (2022) 52:3127–41. doi: 10.1017/S0033291720005188
5. Machida, M, Nakamura, I, Kojima, T, Saito, R, Nakaya, T, Hanibuchi, T, et al. Acceptance of a COVID-19 vaccine in Japan during the COVID-19 pandemic. Vaccine. (2021) 9:210. doi: 10.3390/vaccines9030210
6. Kourlaba, G, Kourkouni, E, Maistreli, S, Tsopela, CG, Molocha, NM, Triantafyllou, C, et al. Willingness of Greek general population to get a COVID-19 vaccine. Glob Health Res Policy. (2021) 6:3–10. doi: 10.1186/s41256-021-00188-1
7. Thaker, J. The persistence of vaccine hesitancy: COVID-19 vaccination intention in New Zealand. J Health Commun. (2021) 26:104–11. doi: 10.1080/10810730.2021.1899346
8. Goldberg, EE, Lin, Q, Romero-Severson, EO, and Ke, R. Swift and extensive omicron outbreak in China after sudden exit from ‘zero-COVID’ policy. Nat Commun. (2023) 14:3888. doi: 10.1038/s41467-023-39638-4
9. Zhang, M, Wang, Y, Zhang, T, Zhou, J, Deng, Y, Wang, L, et al. Status of and perspectives on COVID-19 vaccination after lifting of the dynamic zero-COVID policy in China. Glob Health Med. (2023) 5:112–7. doi: 10.35772/ghm.2022.01063
10. Wang, J, Lu, X, Lai, X, Lyu, Y, Zhang, H, Fenghuang, Y, et al. The changing acceptance of COVID-19 vaccination in different epidemic phases in China: a longitudinal study. Vaccine. (2021) 9:191. doi: 10.3390/vaccines9030191
11. MacDonald, NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
12. Domek, GJ, O'Leary, S, Bull, S, Bronsert, M, Contreras-Roldan, I, Bolaños, G, et al. Measuring vaccine hesitancy: field testing the WHO SAGE working group on vaccine hesitancy survey tool in Guatemala. Vaccine. (2018) 36:5273–81. doi: 10.1016/j.vaccine.2018.07.046
13. Sun, Y, Li, X, and Guo, D. COVID-19 vaccine hesitancy in China: an analysis of reasons through mixed methods. Vaccine. (2023) 11:712. doi: 10.3390/vaccines11030712
14. Wang, J, Ji, Q, Dong, S, Zhao, S, Li, X, Zhu, Q, et al. Factors influencing vaccine hesitancy in China: a qualitative study. Vaccine. (2021) 9:1291. doi: 10.3390/vaccines9111291
15. Larson, HJ, Schulz, WS, Tucker, JD, and Smith, DM. Measuring vaccine confidence: introducing a global vaccine confidence index. PLoS Curr. (2015) 7:4. doi: 10.1371/currents.outbreaks.ce0f6177bc97332602a8e3fe7d7f7cc4
16. Rădoi, M, and Lupu, A. Understanding institutional trust. What does it mean to trust the health system? In: A Maturo, Š Hošková-Mayerová, DT Soitu, and J Kacprzyk, editors. Recent trends in social systems: Quantitative theories and quantitative models. Studies in systems, decision and control, vol. 66. Berlin: Springer International Publishing (2017). 11–22.
17. Gilson, L. Trust and the development of health care as a social institution. Soc Sci Med. (2003) 56:1453–68. doi: 10.1016/S0277-9536(02)00142-9
18. Freedman, LP. Achieving the MDGs: health systems as core social institutions. Development. (2005) 48:19–24. doi: 10.1057/palgrave.development.1100107
19. Flora, JA, Maibach, EW, and Maccoby, N. The role of media across four levels of health promotion intervention. Annu Rev Public Health. (1989) 10:181–201. doi: 10.1146/annurev.pu.10.050189.001145
20. Prati, G, Pietrantoni, L, and Zani, B. A social-cognitive model of pandemic influenza H1N1 risk perception and recommended behaviors in Italy. Risk Anal. (2011) 31:645–56. doi: 10.1111/j.1539-6924.2010.01529.x
21. Huh, J, Delorme, DE, and Reid, LN. The third-person effect and its influence on behavioral outcomes in a product advertising context: the case of direct-to-consumer prescription drug advertising. Commun Res. (2004) 31:568–99. doi: 10.1177/0093650204267934
22. Zarocostas, J. How to fight an infodemic. Lancet. (2020) 395:676. doi: 10.1016/S0140-6736(20)30461-X
23. Cinelli, M, Quattrociocchi, W, Galeazzi, A, Valensise, CM, Brugnoli, E, Schmidt, AL, et al. The COVID-19 social media infodemic. Sci Rep. (2020) 10:16598. doi: 10.1038/s41598-020-73510-5
24. Pulido, CM, Villarejo-Carballido, B, Redondo-Sama, G, and Gómez, A. COVID-19 infodemic: more retweets for science-based information on coronavirus than for false information. Int Sociol. (2020) 35:377–92. doi: 10.1177/0268580920914755
25. Roozenbeek, J, Schneider, CR, Dryhurst, S, Kerr, J, Freeman, ALJ, Recchia, G, et al. Susceptibility to misinformation about COVID-19 around the world. R Soc Open Sci. (2020) 7:201199. doi: 10.1098/rsos.201199
26. Bostrom, A, Böhm, G, O’Connor, RE, Hanss, D, Bodi-Fernandez, O, and Halder, P. Comparative risk science for the coronavirus pandemic In: A Bostrom, editor. COVID-19. 1st ed. Abingdon: Routledge (2022). 70–9.
27. Bavel, JJV, Baicker, K, Boggio, PS, Capraro, V, Cichocka, A, Cikara, M, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav. (2020) 4:460–71. doi: 10.1038/s41562-020-0884-z
28. Siegrist, M, and Zingg, A. The role of public trust during pandemics. Eur Psychol. (2014) 19:23–32. doi: 10.1027/1016-9040/a000169
29. Vraga, EK, and Jacobsen, KH. Strategies for effective health communication during the coronavirus pandemic and future emerging infectious disease events. World Med Health Policy. (2020) 12:233–41. doi: 10.1002/wmh3.359
30. Juarez, R, Kang, Z, Okihiro, M, Garcia, BK, Phankitnirundorn, K, and Maunakea, AK. Dynamics of trust and consumption of COVID-19 information implicate a mechanism for COVID-19 vaccine and booster uptake. Vaccine. (2022) 10:1435. doi: 10.3390/vaccines10091435
31. Juarez, R, Phankitnirundorn, K, Okihiro, M, and Maunakea, AK. Opposing role of trust as a modifier of COVID-19 vaccine uptake in an indigenous population. Vaccine. (2022) 10:968. doi: 10.3390/vaccines10060968
32. Dhanani, LY, and Franz, B. The role of news consumption and trust in public health leadership in shaping COVID-19 knowledge and prejudice. Front Psychol. (2020) 11:560828. doi: 10.3389/fpsyg.2020.560828
33. Lin, L, Savoia, E, Agboola, F, and Viswanath, K. What have we learned about communication inequalities during the H1N1 pandemic: a systematic review of the literature. BMC Public Health. (2014) 14:484. doi: 10.1186/1471-2458-14-484
34. Han, K, Zheng, H, Huang, Z, Qiu, Q, Zeng, H, Chen, B, et al. Vaccination coverage and its determinants among migrant children in Guangdong, China. BMC Public Health. (2014) 14:203. doi: 10.1186/1471-2458-14-203
35. Lai, X, Zhu, H, Wang, J, Huang, Y, Jing, R, Lyu, Y, et al. Public perceptions and acceptance of COVID-19 booster vaccination in China: a cross-sectional study. Vaccine. (2021) 9:1461. doi: 10.3390/vaccines9121461
36. Karafillakis, E, Hassounah, S, and Atchison, C. Effectiveness and impact of rotavirus vaccines in Europe, 2006–2014. Vaccine. (2015) 33:2097–107. doi: 10.1016/j.vaccine.2015.03.016
37. Taylor, S, Landry, CA, Paluszek, MM, and Asmundson, GJG. Reactions to COVID-19: differential predictors of distress, avoidance, and disregard for social distancing. J Affect Disord. (2020) 277:94–8. doi: 10.1016/j.jad.2020.08.002
38. Sinuraya, RK, Nuwarda, RF, Postma, MJ, and Suwantika, AA. Vaccine hesitancy and equity: lessons learned from the past and how they affect the COVID-19 countermeasure in Indonesia. Glob Health. (2024) 20:11. doi: 10.1186/s12992-023-00987-w
39. Cairns, G, De Andrade, M, and MacDonald, L. Reputation, relationships, risk communication, and the role of Trust in the Prevention and Control of communicable disease: a review. J Health Commun. (2013) 18:1550–65. doi: 10.1080/10810730.2013.840696
40. Taha, SA, Matheson, K, and Anisman, H. The 2009 H1N1 influenza pandemic: the role of threat, coping, and media trust on vaccination intentions in Canada. J Health Commun. (2013) 18:278–90. doi: 10.1080/10810730.2012.727960
41. Pierz, AJ, Rauh, L, Masoud, D, Cruz, AK, Palmedo, PC, Ratzan, SC, et al. Supporting US healthcare providers for successful vaccine communication. BMC Health Serv Res. (2023) 23:423. doi: 10.1186/s12913-023-09348-0
42. Vorsters, A, Bonanni, P, Maltezou, HC, Yarwood, J, Brewer, NT, Bosch, FX, et al. The role of healthcare providers in HPV vaccination programs – a meeting report. Papillomavirus Res. (2019) 8:100183. doi: 10.1016/j.pvr.2019.100183
43. Battiston, P, Kashyap, R, and Rotondi, V. Trust in Science and Experts during the COVID-19 outbreak in Italy. Center for Open Science. (2020).
44. Bromme, R, Mede, NG, Thomm, E, Kremer, B, and Ziegler, R. An anchor in troubled times: trust in science before and within the COVID-19 pandemic. PLoS One. (2022) 17:e0262823. doi: 10.1371/journal.pone.0262823
45. Sulik, J, Deroy, O, Dezecache, G, Newson, M, Zhao, Y, El Zein, M, et al. Facing the pandemic with trust in science. Hum Soc Sci Commun. (2021) 8:982. doi: 10.1057/s41599-021-00982-9
46. Freudenburg, WR. Risk, responsibility and recreancy, vol. 9. Amsterdam, Netherlands: Elsevier Science/JAI Press (2001).
47. Siegrist, M. Trust and risk perception: a critical review of the literature. Risk Anal. (2021) 41:480–90. doi: 10.1111/risa.13325
49. Zimand-Sheiner, D, Zimand-Sheiner, D, Levy, S, Levy, S, Eckhaus, E, and Eckhaus, E. Exploring negative spillover effects on stakeholders: a case study on social media talk about crisis in the food industry using data mining. Sustainability. (2021) 13:10845. doi: 10.3390/su131910845
50. Kang, GJ, Ewing-Nelson, S, Mackey, L, Schlitt, JT, Marathe, A, Abbas, KM, et al. Semantic network analysis of vaccine sentiment in online social media. F1000Res. (2017) 6:137. doi: 10.7490/f1000research.1114137.1
51. Larson, HJ, Clarke, RM, Jarrett, C, Eckersberger, E, Levine, Z, Schulz, WS, et al. Measuring trust in vaccination: a systematic review. Hum Vaccin Immunother. (2018) 14:1599–609. doi: 10.1080/21645515.2018.1459252
52. Vinck, P, Pham, P, Bindu, KK, Bedford, J, and Nilles, EJ. Institutional trust and misinformation in the response to the 2018-19 Ebola outbreak in north Kivu, DR Congo: a population-based survey. Lancet Infect Dis. (2019) 19:529–36. doi: 10.1016/s1473-3099(19)30063-5
53. Prati, C, Pelliccioni, GA, Sambri, V, Chersoni, S, and Gandolfi, MG. COVID-19: its impact on dental schools in Italy, clinical problems in endodontic therapy and general considerations. Int Endod J. (2020) 53:723–5. doi: 10.1111/iej.13291
54. Al-Mohaithef, M, Padhi, BK, and Ennaceur, S. Socio-demographics correlate of COVID-19 vaccine hesitancy during the second wave of COVID-19 pandemic: a cross-sectional web-based survey in Saudi Arabia. Front Public Health. (2021) 9:698106. doi: 10.3389/fpubh.2021.698106
55. Borah, P, and Hwang, J. Trust in doctors, positive attitudes, and vaccination behavior: the role of doctor-patient communication in H1N1 vaccination. Health Commun. (2021) 37:1423–31. doi: 10.1080/10410236.2021.1895426
56. Dror, AA, Eisenbach, N, Taiber, S, Morozov, NG, Mizrachi, M, Zigron, A, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. (2020) 35:775–9. doi: 10.1007/s10654-020-00671-y
57. Grech, V, Bonnici, J, and Zammit, D. WITHDRAWN:vaccine hesitancy in Maltese family physicians and their trainees Vis-à-Vis influenza and novel COVID-19 vaccination. Early Hum Dev. (2020) 2020:105259. doi: 10.1016/j.earlhumdev.2020.105259
58. Kwok, KO, Li, KK, Wei, WI, Tang, A, Wong, SYS, and Lee, SS. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int J Nurs Stud. (2021) 114:103854. doi: 10.1016/j.ijnurstu.2020.103854
59. Lin, C, Tu, P, and Beitsch, LM. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccine. (2020) 9:16. doi: 10.3390/vaccines9010016
60. Ozawa, S, Paina, L, and Qiu, M. Exploring pathways for building trust in vaccination and strengthening health system resilience. BMC Health Serv Res. (2016) 16:639–141. doi: 10.1186/s12913-016-1867-7
61. Garfin, DR, Silver, RC, and Holman, EA. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol. (2020) 39:355–7. doi: 10.1037/hea0000875
62. Cottle, S. Ulrich Beck, `risk society’ and the media a catastrophic view? Eur J Commun. (1998) 13:5–32. doi: 10.1177/0267323198013001001
63. MacKay, M, Colangeli, T, Gillis, D, McWhirter, JE, and Papadopoulos, A. Examining social media crisis communication during early COVID-19 from public health and news media for quality, content, and corresponding public sentiment. Int J Environ Res Public Health. (2021) 18:7986. doi: 10.3390/ijerph18157986
64. Mo, PKH, Luo, S, Luo, S, Mo, PK, Wang, S, Zhao, J, et al. Intention to receive the COVID-19 vaccination in China: application of the diffusion of innovations theory and the moderating role of openness to experience. Vaccine. (2021) 9:129. doi: 10.3390/vaccines9020129
65. Yoo, W, Choi, DH, and Choi, DH. Predictors of expressing and receiving information on social networking sites during MERS-CoV outbreak in South Korea. J Risk Res. (2020) 23:912–27. doi: 10.1080/13669877.2019.1569105
66. Reichelt, J, Reichelt, J, Sievert, J, and Jacob, F. How credibility affects eWOM reading: the influences of expertise, trustworthiness, and similarity on utilitarian and social functions. J Mark Commun. (2014) 20:65–81. doi: 10.1080/13527266.2013.797758
67. Kol, O, Nebenzahl, ID, Lev-On, A, and Levy, S. SNS adoption for consumer active information search (AIS)-the dyadic role of information credibility. Int J Hum Comput Interact. (2021) 37:1504–15. doi: 10.1080/10447318.2021.1898824
68. Zhang, L, Kong, Y, and Chang, H. Media use and health behavior in H1N1 flu crisis: the mediating role of perceived knowledge and fear. Atl J Commun. (2015) 23:67–80. doi: 10.1080/15456870.2015.1013101
69. Turcotte, J, York, C, Irving, J, Scholl, RM, and Pingree, RJ. News recommendations from social media opinion leaders: effects on media trust and information seeking. J Comput Mediat Comm. (2015) 20:520–35. doi: 10.1111/jcc4.12127
70. French, J, Deshpande, S, Evans, WD, Evans, W, Evans, WD, and Obregon, R. Key guidelines in developing a pre-emptive COVID-19 vaccination uptake promotion strategy. Int J Environ Res Public Health. (2020) 17:5893. doi: 10.3390/ijerph17165893
71. Nazli, SB, Nazli, ŞB, Yiğman, F, Yigman, F, Sevindik, M, and Ozturan, DD. Psychological factors affecting COVID-19 vaccine hesitancy. Ir J Med Sci. (2021) 191:71–80. doi: 10.1007/s11845-021-02640-0
72. Oleksy, T, Wnuk, A, Maison, D, and Łyś, A. Content matters. Different predictors and social consequences of general and government-related conspiracy theories on COVID-19. Pers Individ Differ. (2021) 168:110289. doi: 10.1016/j.paid.2020.110289
73. Lockyer, B, Lockyer, B, Islam, S, Rahman, A, Dickerson, J, Pickett, K, et al. Understanding COVID-19 misinformation and vaccine hesitancy in context: findings from a qualitative study involving citizens in Bradford, UK. Health Expect. (2021) 24:1158–67. doi: 10.1111/hex.13240
74. Allington, D, Duffy, B, Wessely, S, Dhavan, N, and Rubin, J. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychol Med. (2021) 51:1763–9. doi: 10.1017/s003329172000224x
75. Hamilton, LC, Hartter, J, and Saito, K. Trust in Scientists on climate change and vaccines. SAGE Open. (2015) 5:275. doi: 10.1177/2158244015602752
76. Bicchieri, C, Fatas, E, Aldama, A, Casas, A, Deshpande, I, Lauro, M, et al. In science we (should) trust: expectations and compliance across nine countries during the COVID-19 pandemic. PLoS One. (2021) 16:e0252892–17. doi: 10.1371/journal.pone.0252892
77. Dohle, S, Wingen, T, Wingen, T, and Schreiber, M. Acceptance and adoption of protective measures during the COVID-19 pandemic: the role of trust in politics and trust in science. Soc Psychol Bull. (2020) 15:1–23. doi: 10.23668/psycharchives.4410
78. Mohammed, A, Johnston, RM, and Van der Linden, C. Public responses to policy reversals: the case of mask usage in Canada during COVID-19. Can Public Policy. (2020) 46:89. doi: 10.3138/cpp.2020-089
79. Pagliaro, S, Sacchi, S, Pacilli, MG, Brambilla, M, Lionetti, F, Bettache, K, et al. Trust predicts COVID-19 prescribed and discretionary behavioral intentions in 23 countries. PLoS One. (2021) 16:334. doi: 10.1371/journal.pone.0248334
80. Irzik, G, and Kurtulmus, F. What is epistemic public trust in science. Br J Philos Sci. (2018) 70:1145–66. doi: 10.1093/bjps/axy007
81. Duncan, RG, Chinn, CA, and Barzilai, S. Grasp of evidence: problematizing and expanding the next generation science standards’ conceptualization of evidence. J Res Sci Teach. (2018) 55:907–37. doi: 10.1002/tea.21468
82. Ravit, GD. What is the value of general knowledge of scientific reasoning? In: GD Ravit, editor. Scientific reasoning and argumentation. Abingdon: Routledge (2018). 77.
83. Sturgis, P, Brunton-Smith, I, and Jackson, J. Trust in science, social consensus and vaccine confidence. Nat Hum Behav. (2021) 5:1528–34. doi: 10.1038/s41562-021-01115-7
84. McPhetres, J, and Zuckerman, M. Religiosity predicts negative attitudes towards science and lower levels of science literacy. PLoS One. (2018) 13:e0207125. doi: 10.1371/journal.pone.0207125
85. Fitzpatrick, K, and LaGory, M. Unhealthy cities: Poverty, race, and place in America. Abingdon: Routledge (2013).
86. Slovic, P, and Peters, E. Risk perception and affect. Curr Dir Psychol Sci. (2006) 15:322–5. doi: 10.1111/j.1467-8721.2006.00461.x
87. Van der Pligt, J. Risk perception and self-protective behavior. Eur Psychol. (1996) 1:34–43. doi: 10.1027/1016-9040.1.1.34
88. Dubé, E, Laberge, C, Guay, M, Bramadat, P, Roy, R, and Bettinger, J. Vaccine hesitancy: an overview. Hum Vaccin Immunother. (2013) 9:1763–73. doi: 10.4161/hv.24657
89. Saied, SM, Saied, EM, Kabbash, IA, and Abdo, SAE. Vaccine hesitancy: beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J Med Virol. (2021) 93:4280–91. doi: 10.1002/jmv.26910
90. Dunning, J, Thwaites, RS, and Openshaw, PJ. Seasonal and pandemic influenza: 100 years of progress, still much to learn. Mucosal Immunol. (2020) 13:566–73. doi: 10.1038/s41385-020-0287-5
91. Gross, L. A broken trust: lessons from the vaccine–autism wars. PLoS Biol. (2009) 7:e1000114. doi: 10.1371/journal.pbio.1000114
92. Maiese, A, Baronti, A, Manetti, AC, Manetti, A, Di Paolo, M, Turillazzi, E, et al. Death after the administration of COVID-19 vaccines approved by EMA: has a causal relationship been demonstrated? Vaccine. (2022) 10:308. doi: 10.3390/vaccines10020308
93. Du, F, Chantler, T, Francis, MR, Sun, FY, Zhang, X, Han, K, et al. The determinants of vaccine hesitancy in China: a cross-sectional study following the Changchun Changsheng vaccine incident. Vaccine. (2020) 38:7464–71. doi: 10.1016/j.vaccine.2020.09.075
94. He, Q, Wang, H, Ma, Y, Wang, Z, Zhang, Z, Li, T, et al. Changes in parents’ decisions pertaining to vaccination of their children after the Changchun Changsheng vaccine scandal in Guangzhou, China. Vaccine. (2020) 38:6751–6. doi: 10.1016/j.vaccine.2020.08.039
95. Yuan, X. China’s vaccine production scare. Lancet. (2018) 392:371. doi: 10.1016/S0140-6736(18)31725-2
96. Puteikis, K, and Mameniškienė, R. Factors associated with COVID-19 vaccine hesitancy among people with epilepsy in Lithuania. Int J Environ Res Public Health. (2021) 18:4374. doi: 10.3390/ijerph18084374
97. Lin, Y, Hu, Z, Zhao, Q, Alias, H, Danaee, M, and Wong, LP. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. (2020) 14:e0008961. doi: 10.1371/journal.pntd.0008961
98. Yaqub, O, Castle-Clarke, S, Sevdalis, N, and Chataway, J. Attitudes to vaccination: a critical review. Soc Sci Med. (2014) 112:1–11. doi: 10.1016/j.socscimed.2014.04.018
99. Kata, A. Anti-vaccine activists, web 2.0, and the postmodern paradigm–an overview of tactics and tropes used online by the anti-vaccination movement. Vaccine. (2012) 30:3778–89. doi: 10.1016/j.vaccine.2011.11.112
100. Betsch, C, Schmid, P, Heinemeier, D, Korn, L, Holtmann, C, and Böhm, R. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. (2018) 13:e0208601. doi: 10.1371/journal.pone.0208601
101. Smith, N, and Graham, T. Mapping the anti-vaccination movement on Facebook. Inf Commun Soc. (2019) 22:1310–27. doi: 10.1080/1369118X.2017.1418406
102. Wilson, SL, and Wiysonge, C. Social media and vaccine hesitancy. BMJ Glob Health. (2020) 5:e004206. doi: 10.1136/bmjgh-2020-004206
103. Beck, U, Giddens, A, and Lash, S. Reflexive modernization: Politics, tradition and aesthetics in the modern social order. Redwood City, CA: Stanford University Press (1994).
104. Olivier, B. Exacerbating Beck’s risk society (1992)–the ‘pandemic’and beyond. Altern Interdiscip J Study Arts Humanit South Afr. (2023) 41:117–62.
105. Bandura, A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. (1977) 84:191–215. doi: 10.1037/0033-295X.84.2.191
106. Bandura, A, Adams, NE, Hardy, AB, and Howells, GN. Tests of the generality of self-efficacy theory. Cogn Ther Res. (1980) 4:39–66. doi: 10.1007/BF01173354
107. Schwarzer, R. Health action process approach (HAPA) as a theoretical framework to understand behavior change. Actual Psicol. (2016) 30:119. doi: 10.15517/ap.v30i121.23458
108. Bandura, A, Freeman, WH, and Lightsey, R. Self-efficacy: The exercise of control. Berlin: Springer (1999).
109. Coe, AB, Gatewood, SB, Moczygemba, LR, and Beckner, JO. The use of the health belief model to assess predictors of intent to receive the novel (2009) H1N1 influenza vaccine. Innov Pharm. (2012) 3:1–11. doi: 10.24926/iip.v3i2.257
110. Rosenstock, IM. The health belief model and preventive health behavior. Health Educ Monogr. (1974) 2:354–86. doi: 10.1177/109019817400200405
111. Strecher, VJ, and Rosenstock, IM. The health belief model In: S Ayers, A Baum, C McManus, S Newman, K Wallston, and J Weinman, editors. Cambridge handbook of psychology, health and medicine. Cambridge, England: Cambridge University Press (1997). 113–7.
112. Godin, G, Vézina-Im, LA, and Naccache, H. Determinants of influenza vaccination among healthcare workers. Infect Control Hosp Epidemiol. (2010) 31:689–93. doi: 10.1086/653614
113. Fall, E, Izaute, M, and Chakroun-Baggioni, N. How can the health belief model and self-determination theory predict both influenza vaccination and vaccination intention? A longitudinal study among university students. Psychol Health. (2018) 33:746–64. doi: 10.1080/08870446.2017.1401623
114. Gerend, MA, and Shepherd, JE. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann Behav Med. (2012) 44:171–80. doi: 10.1007/s12160-012-9366-5
115. Cheung, T, Lau, JT, Wang, JZ, Lau, JTF, Mo, P, Siu, CK, et al. The acceptability of HPV vaccines and perceptions of vaccination against HPV among physicians and nurses in Hong Kong. Int J Environ Res Public Health. (2019) 16:1700. doi: 10.3390/ijerph16101700
116. Stout, ME, Christy, SM, Winger, JG, Vadaparampil, ST, and Mosher, CE. Self-efficacy and HPV vaccine attitudes mediate the relationship between social norms and intentions to receive the HPV vaccine among college students. J Community Health. (2020) 45:1187–95. doi: 10.1007/s10900-020-00837-5
117. Betsch, C, Renkewitz, F, Betsch, T, and Ulshöfer, C. The influence of vaccine-critical websites on perceiving vaccination risks. J Health Psychol. (2010) 15:446–55. doi: 10.1177/1359105309353647
118. Myers, LB, and Goodwin, R. Determinants of adults’ intention to vaccinate against pandemic swine flu. BMC Public Health. (2011) 11:15. doi: 10.1186/1471-2458-11-15
119. China Internet Network Information Center (CNNIC). The 47th statistical report on China’s internet development. (2021). Available online at: https://www.cnnic.com.cn/IDR/ReportDownloads/202104/P020210420557302172744.pdf (Accessed Apr 11, 2024).
120. Smith, TW, Bailar, B, and Couper, M. Standard definitions: Final dispositions of case codes and outcome rates for surveys. 9th ed. Lenexa: American Association for Public Opinion Research (2016).
121. Tsfati, Y, and Cappella, JN. Do people watch what they do not trust? Exploring the association between news media skepticism and exposure. Commun Res. (2003) 30:504–29. doi: 10.1177/0093650203253371
122. Hanitzsch, T, Van Dalen, A, and Steindl, N. Caught in the nexus: a comparative and longitudinal analysis of public trust in the press. Int J Press Politics. (2018) 23:3–23. doi: 10.1177/1940161217740695
123. Levi, M, and Stoker, L. Political trust and trustworthiness. Annu Rev Polit Sci. (2000) 3:475–507. doi: 10.1146/annurev.polisci.3.1.475
124. Newton, K, and Zmerli, S. Three forms of trust and their association. Eur Polit Sci Rev. (2011) 3:169–200. doi: 10.1017/S1755773910000330
125. European Commission. Special Eurobarometer 340: Science and Technology. Brussels: European Commission (2010).
126. National Science Board. Science and engineering indicators 2018. Alexandria: National Science Foundation (2018).
127. WHO SAGE Working Group. Report of the SAGE working group on vaccine hesitancy. Geneva: World Health Organization (2014).
128. Larson, HJ, Jarrett, C, Eckersberger, E, Smith, DMD, and Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. (2014) 32:2150–9. doi: 10.1016/j.vaccine.2014.01.081
129. Champion, VL. Revised susceptibility, benefits, and barriers scale for mammography screening. Res Nurs Health. (1999) 22:341–8. doi: 10.1002/(SICI)1098-240X(199908)22:4<341::AID-NUR8>3.0.CO;2-P
130. Hayes, AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Publications (2017).
131. Krastev, S, Krajden, O, Vang, ZM, Juárez, FPG, Solomonova, E, Goldenberg, MJ, et al. Institutional trust is a distinct construct related to vaccine hesitancy and refusal. BMC Public Health. (2023) 23:2481. doi: 10.1186/s12889-023-17345-5
132. Auchynnikava, A, Habibov, N, Lyu, Y, and Fan, L. On different roles of interpersonal and institutional trust and trust in scientists in shaping COVID-19 vaccine hesitancy. Discov Public Health. (2025) 22:113. doi: 10.1186/s12982-025-00501-0
133. Murphy, J, Vallières, F, Bentall, RP, Shevlin, M, McBride, O, Hartman, TK, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. (2021) 12:29. doi: 10.1038/s41467-020-20226-9
134. Brewer, NT, Chapman, GB, Gibbons, FX, Gerrard, M, McCaul, KD, and Weinstein, ND. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. (2007) 26:136–45. doi: 10.1037/0278-6133.26.2.136
135. Petersen, MB, Bor, A, Jørgensen, F, and Lindholt, MF. Transparent communication about negative features of COVID-19 vaccines decreases acceptance but increases trust. Proc Natl Acad Sci U S A. (2021) 118:e2024597118. doi: 10.1073/pnas.2024597118
136. Dong, D, Xu, RH, Wong, ELY, Hung, CT, Feng, D, Feng, Z, et al. Public preference for COVID-19 vaccines in China: a discrete choice experiment. Health Expect. (2020) 23:1543–78. doi: 10.1111/hex.13140
137. Loomba, S, De Figueiredo, A, Piatek, SJ, De Graaf, K, and Larson, HJ. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat Hum Behav. (2021) 5:337–48. doi: 10.1038/s41562-021-01056-1
138. Skafle, I, Nordahl-Hansen, A, Quintana, DS, Wynn, R, and Gabarron, E. Misinformation about COVID-19 vaccines on social media: rapid review. J Med Internet Res. (2022) 24:e37367. doi: 10.2196/37367
139. Leng, A, Maitland, E, Wang, S, Nicholas, S, Liu, R, and Wang, J. Individual preferences for COVID-19 vaccination in China. Vaccine. (2021) 39:247–54. doi: 10.1016/j.vaccine.2020.12.009
140. Chester, PJ, and Shih, V. Vaccine nationalism: how China’s state media misinform about Western vaccines and highlight the successes of Chinese vaccines to different audiences. J Health Polit Policy Law. (2024) 49:163–87. doi: 10.1215/03616878-10910260
141. Lazarus, JV, Ratzan, SC, Palayew, A, Gostin, LO, Larson, HJ, Rabin, K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. (2021) 27:225–8. doi: 10.1038/s41591-020-1124-9
142. Hou, Z, Lai, X, Liu, Y, Jit, M, Larson, HJ, and Fang, H. Assessing the impact of the 2018 Changchun Changsheng vaccine incident on childhood vaccination in China. Commun Med. (2023) 3:114. doi: 10.1038/s43856-023-00339-0
143. Bardosh, K, De Figueiredo, A, Gur-Arie, R, Jamrozik, E, Doidge, J, Lemmens, T, et al. The unintended consequences of COVID-19 vaccine policy: why mandates, passports and restrictions may cause more harm than good. BMJ Glob Health. (2022) 7:e008684. doi: 10.1136/bmjgh-2022-008684
Keywords: vaccine hesitancy, trust, risk perception, self-efficacy, COVID-19, China
Citation: Huang D, Wu Y and Li H (2025) Why did people refuse vaccination during the pandemic? Exploring the impacts of trust and vaccine risk perception on COVID-19 vaccine hesitancy in China. Front. Public Health. 13:1616129. doi: 10.3389/fpubh.2025.1616129
Edited by:
Mireia Faus, University of Valencia, SpainReviewed by:
Romate John, Central University of Karnataka, IndiaRuben Juarez, University of Hawaii, United States
Copyright © 2025 Huang, Wu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi Wu, eWkud3VAc3p1LmVkdS5jbg==; Hui Li, YmV0dGVybGlodWlAc3p1LmVkdS5jbg==
 Dan Huang
Dan Huang Yi Wu
Yi Wu Hui Li2*
Hui Li2*