- 1Department of General Surgery, The First Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang, China
- 2Department of Psychological Sleep, The Psychological Health Center of Harbin First Specialized Hospital, Harbin, Heilongjiang, China
- 3Department of General Surgery, The Second Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang, China
- 4Department of Internal Medicine, Shenzhen Guangming District Maternal and Child Health Hospital, Shenzhen, Guangdong, China
- 5Department of General Practice, The Affiliated Luohu Hospital of Shenzhen University Medical School, Shenzhen, Guangdong, China
Background: Colorectal cancer (CRC) is a leading cause of mortality globally. While survival rates have improved, postoperative patients face psychosocial challenges such as social alienation and stigma, which affect their recovery. Psychological resilience may serve as a protective factor, but its role in mediating the effects of stigma on social alienation in CRC patients is not well understood.
Objective: This study aims to examine the mediating role of psychological resilience in the relationship between perceived stigma and social alienation among postoperative colorectal cancer patients.
Method: A cross-sectional study was conducted with 382 postoperative CRC patients from three tertiary hospitals in Harbin and Shenzhen, China, between January 2023 and December 2024. Participants completed self-report measures of perceived stigma, psychological resilience, and social alienation. Data were analyzed using hierarchical regression and bootstrapping to test the mediation model.
Result: Perceived stigma was positively correlated with social alienation and negatively with psychological resilience. Psychological resilience partially mediated the relationship between stigma and social alienation, explaining 30.8% of the total effect. Significant differences in social alienation were found based on gender, age, and stoma status.
Conclusion: Psychological resilience plays a crucial role in reducing social alienation in postoperative CRC patients. Interventions focused on enhancing resilience could help mitigate stigma and improve social reintegration. Community-based resilience programs are recommended for supporting CRC survivors.
1 Introduction
Colorectal cancer (CRC) is one of the most commonly diagnosed malignancies worldwide, ranking third in incidence and second in mortality (1). With advancements in screening and surgical techniques, early detection and treatment of CRC have become more accessible. These improvements have led to higher survival rates and an increasing number of long-term survivors (2). However, patients still face significant postoperative challenges that go beyond physical recovery (3). These include emotional distress, altered body image, and difficulty reintegrating into social life. Together, these factors may hinder rehabilitation and reduce quality of life (4).
As health systems shift from acute, hospital-based care to chronic disease management, community-based care has gained importance (5, 6). Community nursing not only offers ongoing medical follow-up but also delivers psychosocial support. It helps facilitate patients' return to social life and promotes adherence to healthy behaviors (7). Community-based health education—through peer support, workshops, or digital platforms—can enhance self-efficacy and reduce disease-related misconceptions (8). It also helps foster a more inclusive social environment. For CRC survivors recovering at home, such community-level interventions are essential for sustained recovery and social reintegration (9).
Among the major psychosocial challenges confronting CRC survivors is social alienation—a condition marked by reduced social participation, feelings of isolation, and perceived disconnection from others (10). This problem is especially pronounced among postoperative patients who experience physical aftereffects such as a stoma, bowel dysfunction, or chronic fatigue. These conditions can lead to embarrassment and cause patients to avoid public or social interaction (11). Mounting evidence suggests that social alienation reduces quality of life and raises the risk of mental health problems. It may also negatively affect long-term health outcomes (12).
One key psychological factor associated with social alienation is perceived stigma. In illness contexts, stigma involves feelings of shame, inferiority, or fear of social judgment due to one's health status or visible symptoms (13). CRC survivors may feel stigmatized because of altered bowel habits, visible colostomy bags, or fear of misunderstanding by others (14). When this stigma is internalized, it often causes social withdrawal and deepens the sense of alienation.
However, not all patients are equally affected. Stress and coping theory proposes that psychological reactions to illness-related stressors—such as stigma—are shaped by coping resources like resilience (15, 16). Psychological resilience is defined as the capacity to adapt positively to stress and adversity (17). It may buffer the harmful effects of stigma. Resilient individuals are more likely to stay emotionally stable, seek support, and maintain social engagement despite illness (18). Importantly, resilience is a changeable trait. It can be strengthened through targeted interventions. Community-based education and psychosocial support offer effective ways to build resilience in CRC survivors (19).
Previous studies in breast cancer (20), HIV (21), and lung cancer (22) populations have identified the mediating role of resilience in the stigma-psychological distress relationship. However, little is known about this mechanism in the context of CRC, particularly during the early stages of postoperative recovery when stigma and social vulnerability are most pronounced.
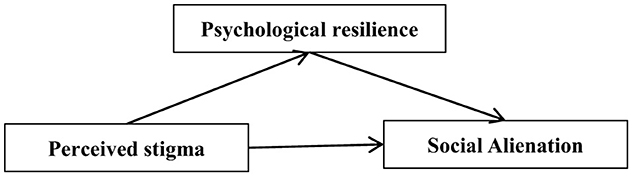
Therefore, the present study seeks to investigate the mediating role of psychological resilience in the relationship between perceived stigma and Social Alienation in postoperative colorectal cancer patients (Figure 1). Based on the Stress and Coping Theory, propose the following hypotheses:
H1: Perceived stigma is positively associated with social alienation;
H2: Perceived stigma is negatively associated with psychological resilience;
H3: Psychological resilience is negatively associated with social alienation;
H4: Psychological resilience mediates the relationship between perceived stigma and social alienation.
This study aims to clarify the psychological mechanisms that hinder social reintegration among CRC survivors by testing the proposed hypotheses. It also seeks to provide empirical support for resilience-based interventions in community nursing and educational programs. These efforts may help promote more holistic and patient-centered colorectal cancer care.
2 Methods
2.1 Participants
This cross-sectional study was conducted between January 2023 and December 2024 at three tertiary general hospitals located in Harbin and Shenzhen, China. A convenience sampling method was employed to recruit participants from the general surgery departments of these hospitals. Eligible participants were identified by attending physicians and invited to participate if they met the following criteria: (1) aged 18 years or older; (2) histologically confirmed diagnosis of CRC and had undergone radical surgery; (3) clear awareness of their disease status; and (4) the ability to read and complete questionnaires independently or with assistance. Patients were excluded if they: (1) had cognitive impairment or major psychiatric illness; (2) had metastatic disease or severe organ dysfunction; or (3) were currently enrolled in psychosocial intervention programs. A total of 382 participants were enrolled. All participants provided written informed consent prior to participation. The study was approved by the Ethics Committee of the First Affiliated Hospital of Harbin Medical University (2024IIT179).
2.2 Instruments
2.2.1 Demographic questionnaire
Demographic and clinical characteristics, including gender, age, marital status, education, monthly income, stoma status, chemotherapy history, and time post surgery, were collected through structured questionnaires and medical record review.
2.2.2 Social alienation
Social alienation was assessed using a 17-item instrument derived from validated research on cancer patients, with each item rated on a five-point Likert scale (1 = strongly disagree to 5 = strongly agree) (23). The total score ranges from 17 to 85, where higher scores represent greater perceived social alienation. The Cronbach's α in the present sample was 0.84.
2.2.3 Perceived stigma
Perceived Stigma was measured using Social Impact Scale (24). The scale consists of 24 items, divided into four dimensions: social isolation (seven items), economic discrimination (three items), social exclusion (nine items), and internal shame (five items). The items are scored using the Likert four-point scoring system, where 4 = strongly agree, 3 = agree, 2 = disagree, and 1 = strongly disagree. The total score of the scale is the sum of the scores of each item, ranging from 24 to 96 points. The higher the score, the higher the perceived sense of shame. The Cronbach's α for the scale in this study was 0.86.
2.2.4 Resilience scale specific to cancer
This scale is the only scale developed to evaluate the psychological resilience of cancer patients (25). It includes 25 items divided into five dimensions: nonspecific resilience components (Items 1–6), disease benefits (Items 7–11), support and response (Items 12–16), hope for the future (Items 17–21), and meaning of existence (Items 22–25). The scale is scored using a five-point Likert scale, and the total score is 25–125 points. The higher the score is, the better the resilience. The Cronbach's α coefficient is 0.85, and the structural validity is 0.901, which indicates good reliability and validity.
2.3 Quality control
All investigators and data collectors received standardized training before data collection. Questionnaires were completed in a quiet room prior to hospital discharge or during outpatient follow-up. Participants with limited literacy were assisted by trained researchers to ensure consistency and data validity. Double data entry and consistency verification were performed using EpiData 3.1 to minimize input errors.
2.4 Statistical analysis
Data analysis was performed using SPSS version 26.0. Descriptive statistics were computed for all variables. Independent sample t-tests or ANOVA were used for univariate analyses to examine differences in social alienation scores across demographic groups. Pearson's correlation coefficients were calculated to assess associations between stigma, resilience, and social alienation. To test the hypothesized mediation model, we conducted a series of hierarchical regression analyses following the procedures proposed by Baron and Kenny. Bootstrapping with 5,000 resamples was used to estimate the indirect effects and corresponding 95% confidence intervals. Mediation was confirmed if the indirect effect was significant and the confidence interval excluded zero. The proportion of mediation was calculated as the ratio of the indirect effect to the total effect. A two-tailed P-value < 0.05 was considered statistically significant.
3 Results
3.1 Demographic characteristics
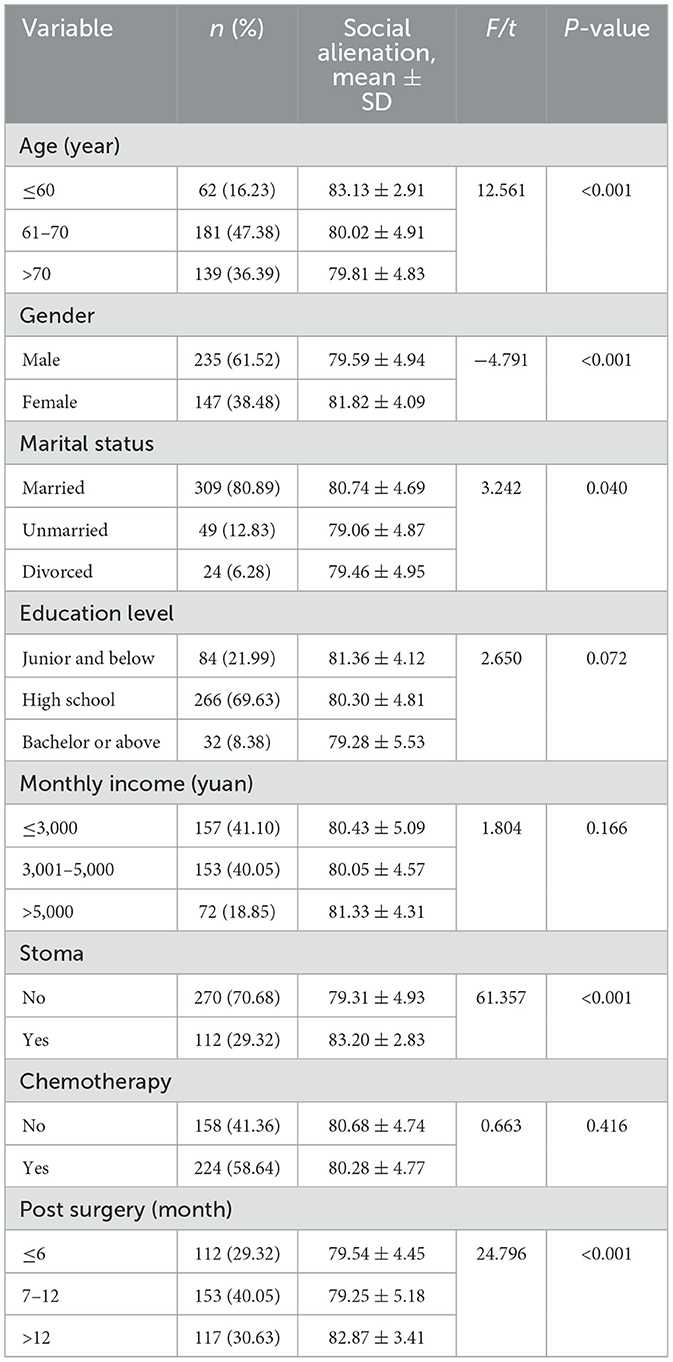
382 postoperative colorectal cancer patients were included. Most participants were aged 61–70 years (47.38%), male (61.52%), and married (80.89%). Regarding education, 69.63% had completed high school, and 8.38% held a bachelor's degree or above. Monthly income was ≤ 5,000 yuan in 81.15% of patients. Stoma formation was reported in 29.32% of cases, and 58.64% had received chemotherapy. Time since surgery was >12 months in 30.63% of patients, 7–12 months in 40.05%, and ≤ 6 months in 29.32%. Independent t-tests and ANOVAs revealed significant differences in social alienation scores across several demographic subgroups. Females reported significantly higher social alienation scores than males (t = −4.791, P < 0.001). Participants younger than 60 years showed significantly higher levels of alienation compared to those aged 60–70 or above 70 (F = 12.561, P < 0.001). Patients with a stoma also reported higher alienation (t = −7.832, P < 0.001). Regarding postoperative time, patients more than 12 months post surgery had significantly higher alienation scores compared to those earlier in recovery (F = 24.796, P < 0.001). Marital status and education level approached significance, while chemotherapy status did not show a significant association with social alienation. Details were presented in Table 1.
3.2 Common method deviation test
To assess the potential for common method variance, Harman's single-factor test was employed. An exploratory factor analysis of all items across the three psychological scales yielded 27 factors with eigenvalues >1. The first factor accounted for 3.195% of the total variance, which is below the critical threshold of 40%, indicating that common method bias was not a significant concern in this study.
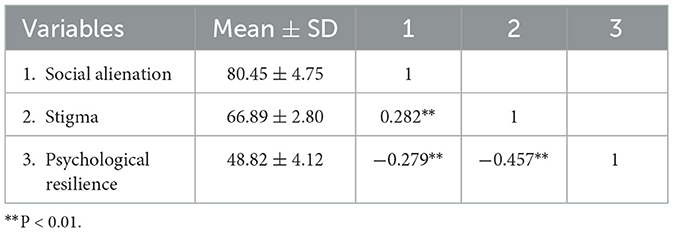
3.3 Correlation analysis
The mean scores for perceived stigma, psychological resilience, and social alienation were (66.89 ± 2.80), (48.82 ± 4.12), and (80.45 ± 4.75), respectively (Table 2). Pearson correlation analysis revealed that perceived stigma was positively correlated with social alienation (r = 0.282, P < 0.01) and negatively correlated with psychological resilience (r = −0.457, P < 0.01). Additionally, psychological resilience was negatively correlated with social alienation (r = −0.279, P < 0.01).
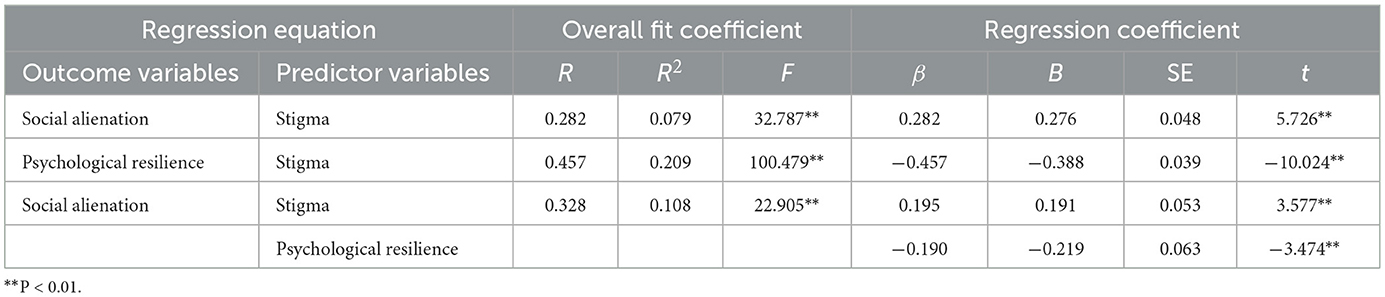
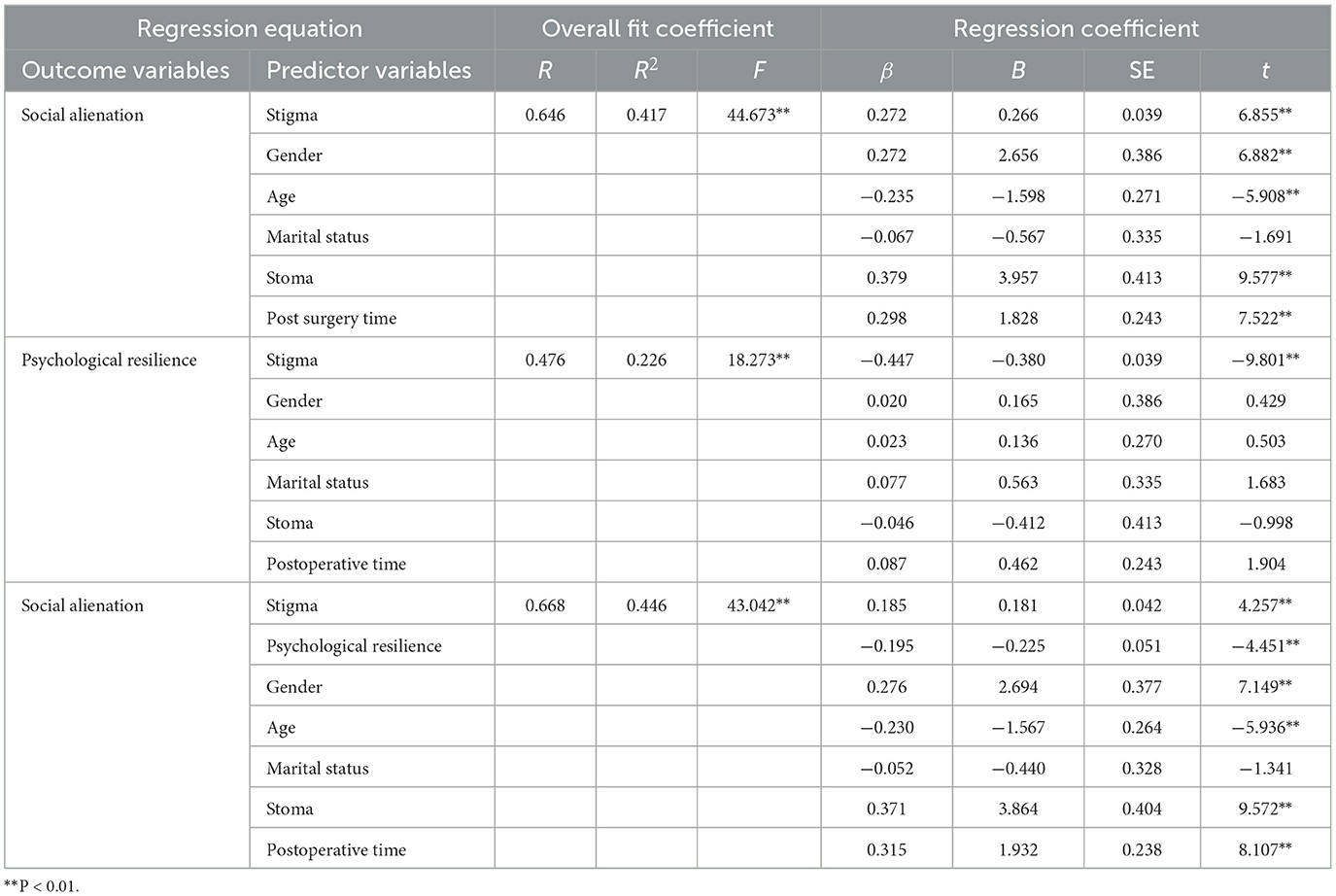
3.4 Mediation analysis
Hierarchical regression analyses based on Baron and Kenny's approach confirmed the mediating role of psychological resilience in the relationship between stigma and social alienation. In the first step, stigma significantly predicted social alienation (B = 0.276, P < 0.001). In the second step, stigma significantly predicted psychological resilience (B = −0.388, P < 0.001). In the third step, when both stigma and psychological resilience were included as predictors, stigma (B = 0.191, P < 0.001) and psychological resilience (B = −0.219, P < 0.001) significantly predicted social alienation (Table 3). Bootstrapping analysis (5,000 samples) showed that the indirect effect was 0.085 [95% CI: (0.038, 0.139)], while the direct effect was 0.191 [95% CI: (0.086, 0.296)], accounting for 30.8% of the total effect, confirming a statistically significant partial mediation (Figure 2).
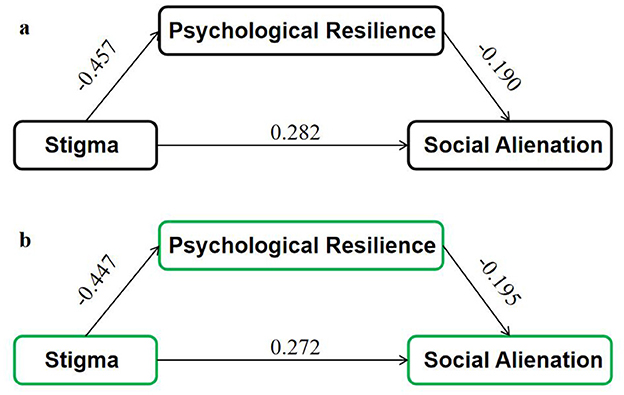
Figure 2. Mediation models of the effect of stigma on social alienation via psychological resilience. (a) Unadjusted model, (b) adjusted model controlling for gender, age, stoma status, and postoperative time.
3.5 Sensitivity analysis
To ensure robustness, a sensitivity analysis was conducted by including gender, age group, stoma status, and postoperative time as covariates in the mediation model. The mediating effect of psychological resilience remained significant [indirect effect = 0.082, 95% CI: (0.035, 0.128)], with a mediation proportion of 29.6%. All key demographic covariates remained significant predictors of social alienation, indicating that the mediation model was stable across different subgroups. Results were presented in Table 4 and Figure 2.
4 Discussion
This study investigated the relationships among perceived stigma, psychological resilience, and social alienation in postoperative CRC patients. The findings revealed that social alienation levels were notably higher among patients who were younger ( ≤ 60 years), female, had undergone stoma formation, or were more than 12 months post surgery. Perceived stigma was positively correlated with social alienation and negatively correlated with psychological resilience. Furthermore, psychological resilience was found to partially mediate the relationship between perceived stigma and social alienation, accounting for ~30.8% of the total effect. These results underscore the significant role of psychological resilience in mitigating the adverse impact of stigma on social alienation among CRC patients.
The observed positive association between perceived stigma and social alienation is consistent with previous findings that stigma contributes to social withdrawal and isolation among cancer patients (26). For example, Wang et al. (27) reported that higher levels of perceived stigma were linked to greater social dysfunction in CRC patients with a stoma. Similarly, Wu et al. (28) found that stigma impaired social connectedness among stroke patients, resulting in increased feelings of alienation.
The mediating role of psychological resilience identified in this study is consistent with prior research. For instance, Ben Salah et al. (29) found that resilience mediated the relationship between sleep quality and social isolation during the COVID-19 pandemic. Similarly, a Chinese study by Wu et al. (30) showed that family resilience significantly influenced social isolation in stroke patients. These findings collectively indicate that psychological resilience acts as a protective factor against the adverse impact of stigma on social integration. Thus, interventions that strengthen resilience may help reduce social alienation in CRC patients.
The observed relationships among perceived stigma, psychological resilience, and social alienation in postoperative CRC patients can be effectively interpreted through Lazarus and Folkman's Stress and Coping Theory (31, 32). This theory suggests that psychological responses to stressors are shaped by individuals' cognitive appraisals and available coping resources. In this framework, perceived stigma acts as a psychosocial stressor, while psychological resilience serves as a coping mechanism that can buffer its negative effects (33, 34). Among CRC patients, stigma often stems from concerns about body image, bowel dysfunction, and the presence of a stoma—factors that may lead to shame and social withdrawal (35, 36). Such negative self-perceptions can intensify psychological stress and hinder reintegration into social life. Psychological resilience, defined as the ability to adapt positively in the face of adversity, helps individuals reframe these challenges, maintain emotional stability, and adopt active coping strategies. Higher resilience has been linked to improved social functioning and lower levels of isolation in cancer survivors (37). These findings highlight the protective role of resilience in mitigating the impact of stigma on social engagement. Moreover, resilience is dynamic and modifiable, meaning it can be strengthened through targeted interventions (38). Programs such as cognitive-behavioral therapy, peer support groups, and community-based initiatives have shown promise in enhancing resilience among cancer patients (39).
By strengthening these coping resources, such interventions may help alleviate perceived stigma and social alienation, thereby enhancing the quality of life among postoperative CRC patients. This study highlights the potential of community health education in improving the psychosocial wellbeing of postoperative CRC patients by addressing key factors such as perceived stigma and psychological resilience. Based on the Stress and Coping Theory, interventions that reduce stigma and enhance resilience can significantly mitigate social alienation and improve patient outcomes. To translate these findings into practice, operational strategies must be defined. A feasible community-based resilience program could involve collaboration among several key actors. Community health workers, including nurses and public health educators, can take the lead in delivering psychoeducation, organizing peer support groups, and conducting cognitive-behavioral training workshops tailored to the CRC population. These programs should be culturally adapted and regularly held in community health centers or through digital platforms to ensure broad accessibility. Hospitals can serve as referral hubs, identifying high-risk patients during postoperative follow-ups and connecting them to community programs. Social workers and psychologists may be mobilized through local health bureaus to provide individual or group interventions, especially for patients with high stigma levels. Additionally, digital health tools such as telehealth platforms and mobile apps can facilitate communication between patients and providers, enabling continuous psychosocial monitoring and resilience coaching. Policymakers should support the integration of these community services into routine cancer survivorship care, ensuring sustainable funding and standardized guidelines. By fostering hospital-community linkages and leveraging multidisciplinary teams, these operational models can effectively reduce social alienation and promote long-term recovery in CRC survivors.
5 Strengths and limitations
This study provides novel insights into the psychosocial dynamics of postoperative CRC patients by investigating the mediating role of psychological resilience in the relationship between perceived stigma and social alienation. The multicenter sampling from three tertiary hospitals in Harbin and Shenzhen improves the generalizability of the findings across geographically and socioeconomically diverse populations. Additionally, the use of validated instruments for all key constructs enhances the study's methodological rigor and construct validity. However, several limitations should be acknowledged. First, the cross-sectional design limits causal inferences, and the directionality of the observed associations cannot be confirmed. Second, the use of self-reported questionnaires may be subject to recall or social desirability biases. Third, the study did not assess important covariates such as patients' perceived social support, pre-existing mental health conditions, or concurrent life stressors, which could confound or moderate the observed relationships. Fourth, no qualitative data were collected to contextualize patients' experiences of stigma or social withdrawal, which limits the depth of interpretation (40).
To address these limitations, future studies should adopt longitudinal designs to examine the temporal sequence and causal pathways linking stigma, resilience, and social alienation. Incorporating standardized measures of social support and psychiatric history would allow for more comprehensive modeling and risk adjustment. Furthermore, integrating qualitative interviews or mixed-methods designs could capture the nuanced coping strategies and contextual factors shaping psychosocial outcomes. Finally, intervention studies, particularly within community health settings, are needed to evaluate the effectiveness of resilience-building programs and stigma-reduction education in improving social reintegration and quality of life among CRC patients.
6 Conclusion
In summary, this study highlights the significant role of psychological resilience in mediating the relationship between perceived stigma and social alienation among postoperative CRC patients. The findings underscore the need for comprehensive care approaches that address not only the physical but also the psychosocial aspects of patient wellbeing. By integrating resilience-building interventions and stigma-reduction efforts into postoperative care, healthcare providers can enhance social reintegration and overall quality of life for CRC survivors.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of the First Affiliated Hospital of Harbin Medical University (2024IIT179). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
XG: Investigation, Writing – original draft, Conceptualization. YW: Investigation, Writing – original draft. QH: Writing – original draft, Methodology, Data curation. RZ: Writing – original draft, Formal analysis, Validation. SL: Writing – original draft, Conceptualization. YH: Supervision, Writing – review & editing. YZ: Resources, Writing – review & editing. BG: Writing – review & editing, Supervision, Project administration.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the transverse project from Harbin Medical University (22992200017, 22992210007).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. (2024) 74:229–63. doi: 10.3322/caac.21834
2. Rossi AM, Hibler BP, Navarrete-Dechent C, Lacouture ME. Restorative oncodermatology: diagnosis and management of dermatologic sequelae from cancer therapies. J Am Acad Dermatol. (2021) 85:693–707. doi: 10.1016/j.jaad.2020.08.005
3. Liao Y, Liu X, Wu X, Li C, Li Y. Social isolation profiles and conditional process analysis among postoperative enterostomy patients with colorectal cancer. BMC Psychol. (2024) 12:782. doi: 10.1186/s40359-024-02304-5
4. Li G, Qin R, Zhao X, Zhao D, Li P. Limitations on participation and global quality of life among CRC survivors with permanent stomas: moderated mediation analysis of psychological distress and family functioning. Support Care Cancer. (2023) 31:526. doi: 10.1007/s00520-023-07993-z
5. Kotronoulas G, Papadopoulou C, Burns-Cunningham K, Simpson M, Maguire R. A systematic review of the supportive care needs of people living with and beyond cancer of the colon and/or rectum. Eur J Oncol Nurs. (2017) 29:60–70. doi: 10.1016/j.ejon.2017.05.004
6. Moreno PI, Ramirez AG, San Miguel-Majors SL, Castillo L, Fox RS, Gallion KJ, et al. Unmet supportive care needs in Hispanic/Latino cancer survivors: prevalence and associations with patient-provider communication, satisfaction with cancer care, and symptom burden. Support Care Cancer. (2019) 27:1383–94. doi: 10.1007/s00520-018-4426-4
7. Portillo MC, Cowley S. Social rehabilitation in long-term conditions: learning about the process. J Adv Nurs. (2011) 67:1329–40. doi: 10.1111/j.1365-2648.2010.05600.x
8. Borowski SC, Siembida EJ, Nygren K, Bellizzi KM. Correlates of mental health in survivors of colorectal cancer: the influence of individual, family, and community level factors. J Behav Ther Ment Health. (2016) 1:24–37. doi: 10.14302/issn.2474-9273.jbtm-16-1105
9. Hoon LS, Chi Sally CW, Hong-Gu H. Effect of psychosocial interventions on outcomes of patients with colorectal cancer: a review of the literature. Eur J Oncol Nurs. (2013) 17:883–91. doi: 10.1016/j.ejon.2013.05.001
10. Caravati-Jouvenceaux A, Launoy G, Klein D, Henry-Amar M, Abeilard E, Danzon A, et al. Health-related quality of life among long-term survivors of colorectal cancer: a population-based study. Oncologist. (2011) 16:1626–36. doi: 10.1634/theoncologist.2011-0036
11. Li G, He X, Qin R, Yao Q, Dong X, Li P. Linking stigma to social isolation among colorectal cancer survivors with permanent stomas: the chain mediating roles of stoma acceptance and valuable actions. J Cancer Surviv. (2024). doi: 10.1007/s11764-024-01614-2. [Epub ahead of print].
12. Stavropoulou A, Vlamakis D, Kaba E, Kalemikerakis I, Polikandrioti M, Fasoi G, et al. “Living with a stoma”: exploring the lived experience of patients with permanent colostomy. Int J Environ Res Public Health. (2021) 18:8512. doi: 10.3390/ijerph18168512
13. Francis SE, Brumbaugh JT, An J, Bartley EJ, McNeil DW. Internalized stigma mediates the relationship between pelvic pain severity and both depression and anxiety in women with chronic pelvic pain. Womens Health. (2025) 21:17455057251344381. doi: 10.1177/17455057251344381
14. Vrinten C, Gallagher A, Waller J, Marlow LAV. Cancer stigma and cancer screening attendance: a population based survey in England. BMC Cancer. (2019) 19:566. doi: 10.1186/s12885-019-5787-x
15. Wen X, Wang D, Li N, Qin X, Gu D. The construction of the structural equation model of burden, benefit finding, and anxiety-depression of esophageal cancer caregivers based on Lazarus stress and coping theory. Ann Palliat Med. (2021) 10:7644–52. doi: 10.21037/apm-21-1466
16. Au CH, Wong CS, Law CW, Wong MC, Chung KF. Self-stigma, stigma coping and functioning in remitted bipolar disorder. Gen Hosp Psychiatry. (2019) 57:7–12. doi: 10.1016/j.genhosppsych.2018.12.007
17. Labrague LJ. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: a systematic review of quantitative studies. J Nurs Manag. (2021) 29:1893–905. doi: 10.1111/jonm.13336
18. Qi X, Zhang W, Wang K, Pei Y, Wu B. Social isolation and psychological well-being among older Chinese Americans: does resilience mediate the association? Int J Geriatr Psychiatry. (2022) 37:1–9. doi: 10.1002/gps.5791
19. Dai J, Sun D, Li B, Zhang Y, Wen M, Wang H, et al. Mixed-mode mindfulness-based cognitive therapy for psychological resilience, self esteem and stigma of patients with schizophrenia: a randomized controlled trial. BMC Psychiatry. (2024) 24:179. doi: 10.1186/s12888-024-05636-z
20. Zamanian H, Amini-Tehrani M, Jalali Z, Daryaafzoon M, Ramezani F, Malek N, et al. Stigma and quality of life in women with breast cancer: mediation and moderation model of social support, sense of coherence, and coping strategies. Front Psychol. (2022) 13:657992. doi: 10.3389/fpsyg.2022.657992
21. Turan B, Budhwani H, Yigit I, Ofotokun I, Konkle-Parker DJ, Cohen MH, et al. Resilience and optimism as moderators of the negative effects of stigma on women living with HIV. AIDS Patient Care STDS. (2022) 36:474–82. doi: 10.1089/apc.2022.0185
22. Cho S, Ryu E. The mediating effect of resilience on happiness of advanced lung cancer patients. Support Care Cancer. (2021) 29:6217–23. doi: 10.1007/s00520-021-06201-0
23. Su SS, Dong YM, Zheng W, Wang DD, Liu ML, Liu H, et al. Development and psychometric test of social isolation assessment questionnaire for cancer patients. J Nurs. (2023) 30:51–6. doi: 10.16460/j.issn1008-9969.2023.17.051
24. Pan AW, Chung L, Fife BL, Hsiung PC. Evaluation of the psychometrics of the social impact scale: a measure of stigmatization. Int J Rehabil Res. (2007) 30:235–8. doi: 10.1097/MRR.0b013e32829fb3db
25. Ye ZJ, Liang MZ, Zhang HW, Li PF, Ouyang XR, Yu YL, et al. Psychometric properties of the Chinese version of resilience scale specific to cancer: an item response theory analysis. Qual Life Res. (2018) 27:1635–45. doi: 10.1007/s11136-018-1835-2
26. Choudhury A. Impact of social isolation, physician-patient communication, and self-perception on the mental health of patients with cancer and cancer survivors: national survey analysis. Interact J Med Res. (2023) 12:e45382. doi: 10.2196/45382
27. Wang M, Xu Y, Yang BX, Luo D, Hou H, Liu Q, et al. A longitudinal study of resilience and social function in patients with colorectal cancer and stomas. J Psychosom Res. (2025) 189:112013. doi: 10.1016/j.jpsychores.2024.112013
28. Wu Y, Yan Z, Fornah L, Zhao J, Wu S. The mediation effect of social support between stigma and social alienation in patients with stroke. Front Public Health. (2023) 11:1290177. doi: 10.3389/fpubh.2023.1290177
29. Ben Salah A, DeAngelis BN, al'Absi M. Resilience and the role of depressed and anxious mood in the relationship between perceived social isolation and perceived sleep quality during the COVID-19 pandemic. Int J Behav Med. (2021) 28:277–85. doi: 10.1007/s12529-020-09945-x
30. Wu XJ, Ke K, Liu H, Zhan SP, Wang L, He JF. Social isolation in the young and middle-aged patients with stroke: role of social support, family resilience and hope. Front Psychiatry. (2025) 16:1499186. doi: 10.3389/fpsyt.2025.1499186
31. Lazarus RS. Coping theory and research: past, present, and future. Psychosom Med. (1993) 55:234–47. doi: 10.1097/00006842-199305000-00002
32. Lee Y, Song Y. Coping as a mediator of the relationship between stress and anxiety in caregivers of patients with acute stroke. Clin Nurs Res. (2022) 31:136–43. doi: 10.1177/10547738211021223
33. Scholz U, Bierbauer W, Lüscher J. Social stigma, mental health, stress, and health-related quality of life in people with long COVID. Int J Environ Res Public Health. (2023) 20:3927. doi: 10.3390/ijerph20053927
34. Kwon T. Social stigma, ego-resilience, and depressive symptoms in adolescent school dropouts. J Adolesc. (2020) 85:153–63. doi: 10.1016/j.adolescence.2020.11.005
35. Yang Y, Wang HY, Chen YK, Chen JJ, Song C, Gu J. Current status of surgical treatment of rectal cancer in China. Chin Med J. (2020) 133:2703–11. doi: 10.1097/CM9.0000000000001076
36. Song L, Pang Y, Zhang J, Tang L. Body image in colorectal cancer patients: a longitudinal study. Psychooncology. (2021) 30:1339–46. doi: 10.1002/pon.5688
37. Ribeiro-Gonçalves JA, Costa PA, Leal I. Loneliness, ageism, and mental health: the buffering role of resilience in seniors. Int J Clin Health Psychol. (2023) 23:100339. doi: 10.1016/j.ijchp.2022.100339
38. Ye B, Li Y, Bao Z, Gao J. Psychological resilience and frailty progression in older adults. JAMA Netw Open. (2024) 7:e2447605. doi: 10.1001/jamanetworkopen.2024.47605
39. Joyce S, Shand F, Tighe J, Laurent SJ, Bryant RA, Harvey SB. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open. (2018) 8:e017858. doi: 10.1136/bmjopen-2017-017858
Keywords: colorectal cancer, stigma, social alienation, psychological resilience, community health, postoperative care
Citation: Guo X, Wang Y, Han Q, Zhang R, Liu S, Huang Y, Zhang Y and Guo B (2025) Integrating psychological resilience into community health strategies: addressing stigma-induced social alienation in postoperative colorectal cancer patients. Front. Public Health 13:1618599. doi: 10.3389/fpubh.2025.1618599
Received: 26 April 2025; Accepted: 30 June 2025;
Published: 16 July 2025.
Edited by:
Lei Shi, Guangzhou Medical University, ChinaReviewed by:
Angel Puig-Lagunes, Universidad Veracruzana, MexicoLiu Chengzhi, Capital Medical University, China
Copyright © 2025 Guo, Wang, Han, Zhang, Liu, Huang, Zhang and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Botang Guo, aG11Z2J0QGhyYm11LmVkdS5jbg==; Yan Zhang, emhhbmd5YW44MzQ1QDE2My5jb20=; Yuenan Huang, aHVhbmd5dWVuYW5AaHJibXUuZWR1LmNu
 Xin Guo
Xin Guo Yuqin Wang1
Yuqin Wang1 Yuenan Huang
Yuenan Huang Botang Guo
Botang Guo