- 1School of Nursing, Bengbu Medical University, Bengbu, China
- 2General Practice Education and Development Center, Bengbu Medical University, Bengbu, China
- 3Fuyang First People’s Hospital, Fuyang, China
- 4School of Marxism, Bengbu Medical University, Bengbu, China
- 5The First Affiliated Hospital of Bengbu Medical University, Bengbu, China
- 6The First People's Hospital of Bengbu, Bengbu, China
- 7No. 902 Hospital of the People’s Liberation Army Joint Logistics and Security Force, Bengbu, China
Introduction: Post-traumatic growth is the positive psychological changes that an individual may undergo after coping with traumatic events. It can help individuals alleviate negative emotions, reduce physical and mental stress, and enhance self-efficacy. This study aims to characterize the latent profiles of spouses’ post-traumatic growth and to explore the related factors for each subgroup based on the ABC-X model.
Methods: 210 breast cancer couples participated in the survey through convenience sampling and completed the General Information Questionnaire, Post-Traumatic Growth Inventory, Dyadic Coping Inventory, and Resilience Scales.
Results: Latent profile analysis revealed three distinct post-traumatic growth profiles among breast cancer patients’ spouses: low growth-emerging edge group (30.9%), medium growth-moderate progress group (48.7%), and high growth-transcending self group (20.3%). Multivariate logistic regression showed that factors influencing post-traumatic growth in spouses with breast cancer include type of place of residence, resilience, negative coping styles, the number of chemotherapy treatments for the patient, and cancer stage.
Conclusion: There is significant heterogeneity in post-traumatic growth among spouses. Future research could utilize precise psychological interventions to improve post-traumatic growth based on the diverse psychological profiles of spouses, thereby enhancing the mental health of the spousal population.
1 Introduction
Currently, breast cancer (BC) ranks as the leading malignancy encountered by women, posing a severe threat to their physical and mental health. Data show that BC accounts for 11.7% of new cancer cases globally (2.26 million out of 19.29 million). BC accounts for 9.2% (420,000) of the 4.57 million new cancer diagnoses in China, making China as the nation with the highest incidence of breast cancer (1). For BC patients, the whole process, from the early diagnosis of the disease to the subsequent radiotherapy, undoubtedly has tremendous physical and mental impacts, severely impairing their healthy lives (2). The family systems theory states that the members of a family interact through emotion, cognition and behavior to form a dynamic network system in which any one member’s behavioral change can ripple through to affect others and the overall family structure (3). Couples are mutually dependent on each other as the emotional family line; therefore, the suffering caused by the disease and treatment suffered by the patient not only reduces the quality of life of the spouses but may also bring about psychological disturbances (4). Notably, 60% of BC patients’ primary caregivers are their spouses (5). Spouses participate in the treatment process of the patients not only to provide for a variety of caregiving needs but also to connect emotionally with the patient, providing comfort, hope, and encouragement, becoming advocates for the patient’s healthcare, managers of self-regulation of emotions, and also connecting with other people for emotional and psychological support, which can help to alleviate multiple stressors (6). Approximately 62% of spouses of BC patients experience clinically significant emotional distress compared to other caregivers, severely affecting their well-being and marital quality (7).
As the field of positive psychology continues to expand, researchers have found that individuals are able to use their wisdom to change their self-perceptions when they experience major stressful events (e.g., life adversities), in order to acquire positive outlooks and values, known as post-traumatic growth (PTG) (8). When confronted with abrupt stressful incidents, spouses, acting as the patient’s caregivers, can still gain positive psychological benefits from the caregiving process. This contributes to diminishing the stress of caregiving, alleviating psychological distress, and enhancing self-efficacy (9). PTG is like a soothing agent for the soul, allowing those who have suffered from the baptism of life to find the courage and strength to move forward and rediscover the meaning and value of life. However, current research often assesses PTG through aggregate scale scores, overlooking population heterogeneity. Latent profile analysis (LPA) is a statistical method of data clustering based on individual characteristics, which classifies populations with similar characteristics through the exogenous variables of the study population and calculates the number and proportion of people in each category, which makes it easier to analyze the features and influencing factors of the population’s various profiles later on and to apply targeted interventions using the profiles as a whole (10). Therefore, this method was used in the current study to investigate the latent profiles of PTG within the spouses’ group.
Resilience is the self-recovery ability of an individual after experiencing adversity that helps him or her adapt, overcome difficulties, and continue to move forward in a positive direction (11). Studies have found that higher resilience facilitates psychological recovery and self-growth in patients (12). When an individual and their intimate partner share coping mechanisms and approaches when encountering a stressful circumstance, this is referred to as dyadic coping (DC) (13). Research suggests that negative coping strategies may obstruct PTG, whereas positive DC may enhance relationship satisfaction and improve patients’ or couples’ psychosocial adaptation (14, 15). Although prior studies have examined the associations between resilience, DC, and PTG, it is unclear whether these factors influence spouses’ PTG.
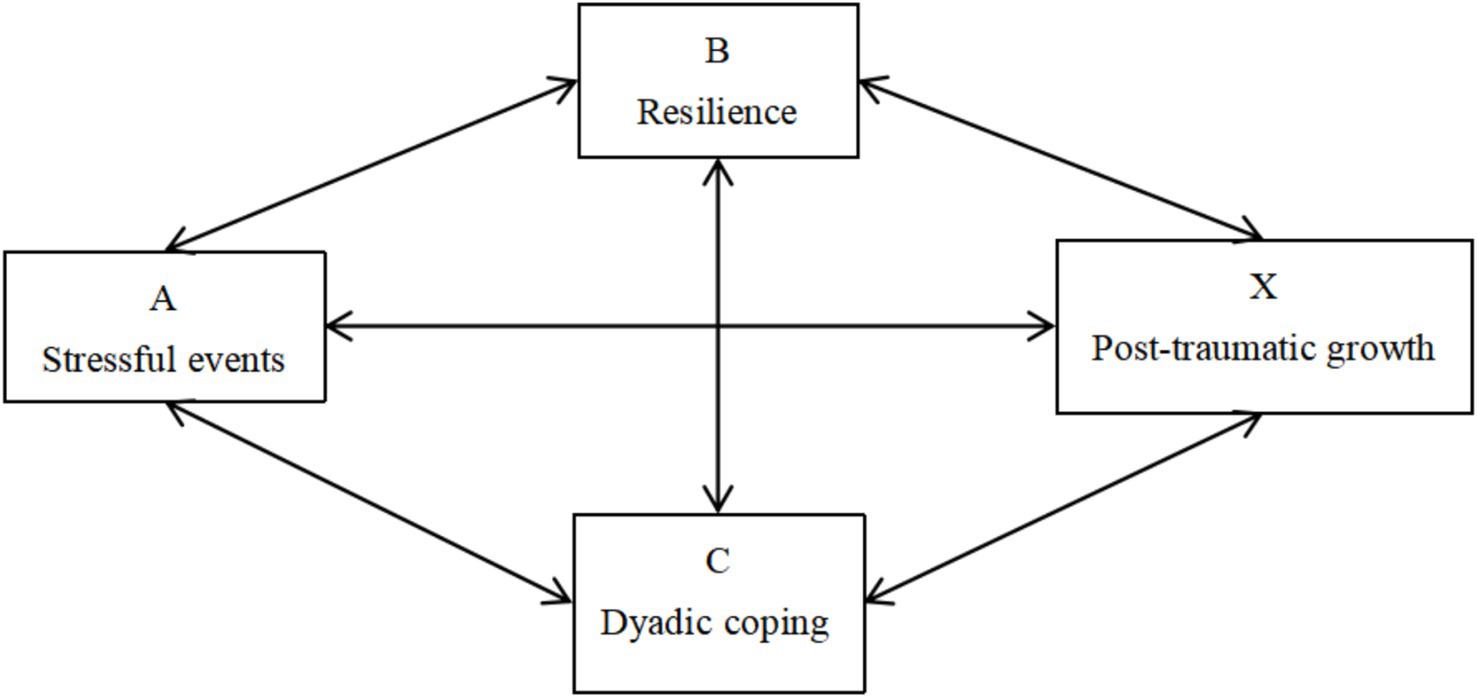
The ABC-X model is a theoretical framework for analyzing how families cope with stress and consists of four factors: A represents the stressor event that disrupts the family structure; B represents the resources available to the individual experiencing family stress; C represents the person’s opinions or evaluation of going through the traumatic situation; and X represents the outcome of the stress or crisis brought about by the family event (16). Based on this model, we hypothesized that the resources an individual possesses (resilience) and the cognitive appraisal of a stressful event (dyadic coping) predict the effects of events on individuals (post-traumatic growth). Figure 1 presents the theoretical framework of our research. Accordingly, this study aimed to (1) exploring the potential characteristics of PTG among partners of BC patients, and (2) identifying the impact of DC and resilience on PTG across various subgroups of BC patients’ spouses. Exploring these influences could assist healthcare professionals develop strategies to enhance PTG and life quality for spouses of BC patients, offering a benchmark for clinical interventions.
2 Methods
2.1 Study design and participants
This study utilized a cross-sectional design. From July to December 2023, hospitalized breast cancer patients and their spouses who met the inclusion/exclusion criteria were recruited from the oncology department of a tertiary hospital in Bengbu, China. Inclusion criteria: patients: (1) Female BC patients requiring chemotherapy after surgery; (2) No evidence of recurrence or metastasis; (3) Knowledge of their condition and consent to participate in this research. Spouses: (1) People who are willing to participate in this study, are literate, and have average comprehension abilities; (2) Legal spouse of the patient. Exclusion criteria: (1) Those with mental illness cannot cooperate with this study; (2) No traumatic events in the last 3 months. The sample size involved a consideration of the study variables’ influential factors, multiplied by a factor of 5–10 (17), resulting in an initial estimate of 100–200 participants for the 20 variables under investigation. Ultimately, this study enrolled a final sample size of 210 dyads (patient-spouse pairs).
2.2 Recruitment
Participants were initially screened through an electronic medical record system. The screening mainly included demographic characteristics (age, occupation, etc.) and clinical characteristics (cancer stage and surgical manner, etc.). During the patients’ hospitalization, the investigator, assisted by the ward nurse manager, actively communicated with potential participants; this interaction enhanced the trust of participants in the researcher. In the process, the investigator learned about the patients’ perception of the disease and confirmed the spouses’ status as caregivers. The investigator then introduced herself and informed the patients and spouses about the study’s purpose and data collection procedures. The patient-spouse dyads were included in the study only if both the patient and the spouse met the inclusion criteria and provided consent.
2.3 Ethical considerations
This study was approved by the Ethics Committee of Bengbu College (Approval No. 2023369). Before data collection, the researcher informed the participants about the purpose and significance of the study, as well as the data confidentiality measures, and explained them that the data will only be used for this research. All participants voluntarily agreed to take part in the research and provided their written consent.
2.4 Measures
2.4.1 General information questionnaire
The general information questionnaire collected demographic and clinical characteristics, including: the patient’s educational level, chemotherapy protocol, cancer stage and surgical manner, the spouse’s age, educational level, per capita monthly household income, et al.
2.4.2 Post-traumatic growth inventory (PTGI)
The scale, which Wang et al. (18) translated and localized, was used to assess the beneficial improvements that spouses of patients with BC after experiencing a traumatic event. There are 20 items in 5 dimensions: Personal Strength, Relating to Others, Spiritual Change, Appreciation of Life, New Possibilities, with each entry receiving a rating between 0 and 5, totaling 100 points. Higher scores predict the individual reaps more positive psychological change from the traumatic event. The PTGI scale’s Cronbach’s α in our research was 0.856.
2.4.3 Connor and Davidson’s resilience scale (CDRS)
Translated and localized by Yu and Zhang (19), this scale was adopted to evaluate the adaptive capacity of individuals after experiencing a stressful event with BC patients’ spouses. 25 entries in 3 dimensions (Tenacity, Strength, and Optimism), with each entry receiving a rating between 0 and 4, totaling 100 points. The CDRS scale’s Cronbach’s α in our research was 0.873.
2.4.4 Dyadic coping inventory (DCI)
Translated and localized by Xu et al. (20) to assess BC couples’ ability to dealing with shock events. This study’s scale, comprising 37 items across 6 dimensions-Stress communication, Supportive coping, Common coping, Delegated coping, Negative coping, Coping evaluation. The DCI scale’s Cronbach’s α for spouses in our research was 0.877.
2.5 Data collection
Participants were selected according to the study criteria. Questionnaires were distributed with the consent of the other party before the formal survey, and couples completed them separately. If participants had difficulties understanding any items, researchers provided standardized explanations to assist them. All questionnaires were collected immediately upon completion, and participants were thanked for their time.
2.6 Statistical analysis
Data from spouses were analyzed using the SPSS 26.0 software. Normally distributed data were characterized by means and standard deviations, while categorical variables were described using frequencies and percentages. For univariate analyses of spouses of BC patients, the Kruskal-Wallis H test was employed to evaluate ordered categorical data, the chi-square test or Fisher’s exact test for group comparisons, and multivariate logistic regression to identify factors potentially influencing PTG categories. Statistical significance was set at p < 0.05.
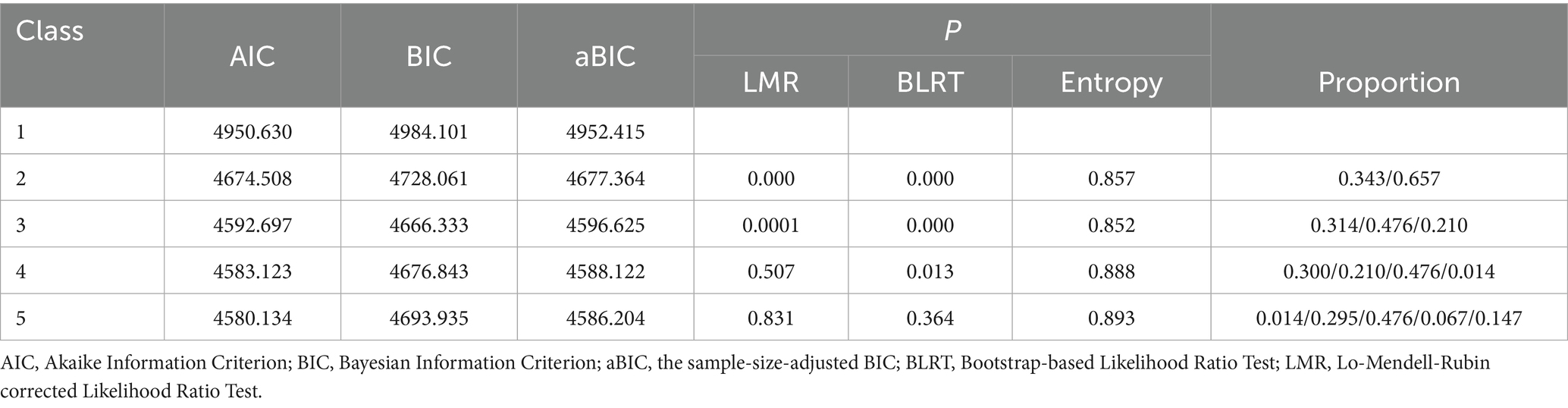
LPA of spousal PTG was conducted using Mplus 7.4 software. Starting with a one-category model, incremental steps were taken until the optimal latent profile emerged. The fit indices for assessing the optimal latent profile were the Akaike Information Criterion (AIC), the Bayesian Information Criterion (BIC), and the sample-size-adjusted BIC (aBIC). A lower value signifies a better model fit. Entropy of information (Entropy), ranges between 0 and 1; a value approaching 1 indicates a higher precision in the classification of the profiles. The Lo–Mendell–Rubin corrected Likelihood Ratio Test (LMR) and Bootstrap-based Likelihood Ratio Test (BLRT), suggest that when p < 0.05, the model with the current number of K classifications is superior to the model with K−1 classifications in terms of classification performance (10).
3 Results
3.1 General information questionnaires
Questionnaires were finally collected from 210 BC couples in this study. The patient’s average age was 47.42 years (SD = 7.825); 69.5% had two or more children; 54.8% had been diagnosed for < 3 months; 57.1% had cancer stage II; 43.8% of the chemotherapy protocol were A/EC; 30.5% received < 2 chemotherapy treatments. The average age of spouses was 48.50 years (SD = 8.320); 53.8% of them lived in towns/urban; 35.7% of families had a per capita monthly income of <3,000 yuan; only 0.9% had a college degree and above.
3.2 Subgroups identified by LPA
Through gradual increases of profile categories, five potential profile models were fitted. Table 1 displays the model fit indices for every profile, which shows that when the profiles are 4 and 5, one of the profiles accounted for 0.01, demonstrating no practical significance. In contrast, when the profile is 3, the LMR and BLRT tests are both significant (p < 0.05) and entropy > 0.8, and the posterior probability of each profile is 90.7–95.6%, which were greater than 80%. These findings confirm the reliability of the 3 profiles, which was consequently selected as the suitable model.
3.3 Characteristics and nomenclature of latent profiles
Figure 2 depicts the average scores across the five dimensions of PTG for the three profiles. Profile 1 demonstrated consistently lower dimension scores than the other two profiles. Indicating participants were in early growth stages, thus being named “Low Growth-Emerging Edge Group,” accounting for 31.43% (66/210); Profile 2 showed intermediate scores with dimension means slightly above average, reflecting that these individuals have adapted to the changes and are growing in a smooth and sustained manner, hence being named “Medium Growth-Moderate Progress Group,” accounting for 47.62% (100/210); Profile 3 exhibited the highest scores overall and “Relating to Others group” has a higher mean value than the average value of the dimensions. Its dimension scores were higher than those of the other two groups, and “Appreciation of Life” dimension score was significantly higher than those of the other dimensions, so it is named “High Growth-Transcending Self Group,” accounting for 20.95% (44/210).
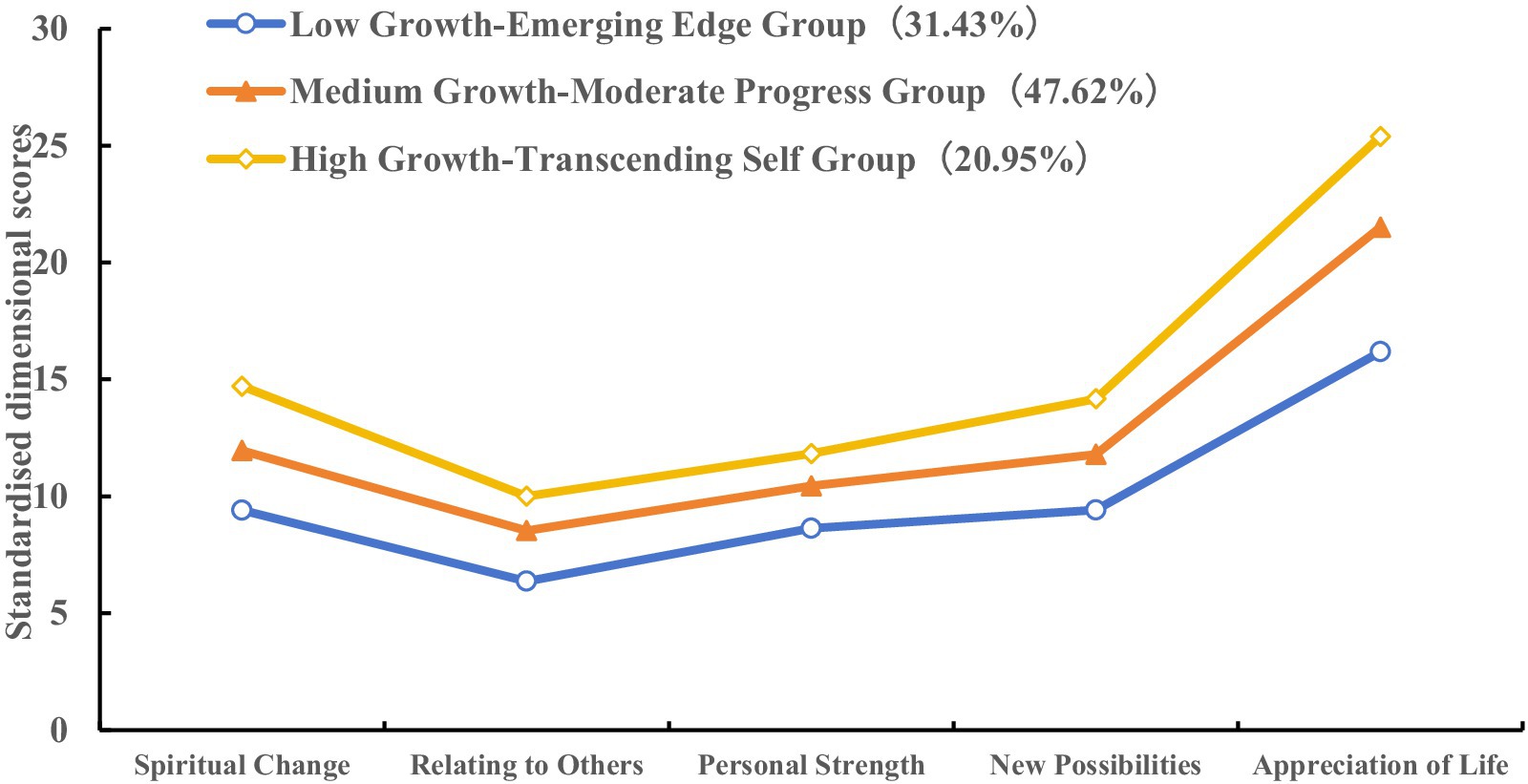
Figure 2. The characteristic distribution of three latent profiles of post-traumatic growth in spouses of breast cancer patients.
3.4 Univariate analysis of PTG
The univariate analysis showed statistically significant differences (p < 0.05) among the three PTG profiles of spouses, particularly regarding several crucial factors: place of residence, monthly household income per capita, cancer stage at diagnosis, the number of chemotherapy treatments, the chemotherapy treatment protocol, resilience levels, and DC strategies. These findings are detailed in Table 2 highlighting the heterogeneity in the PTG experiences of spouses.
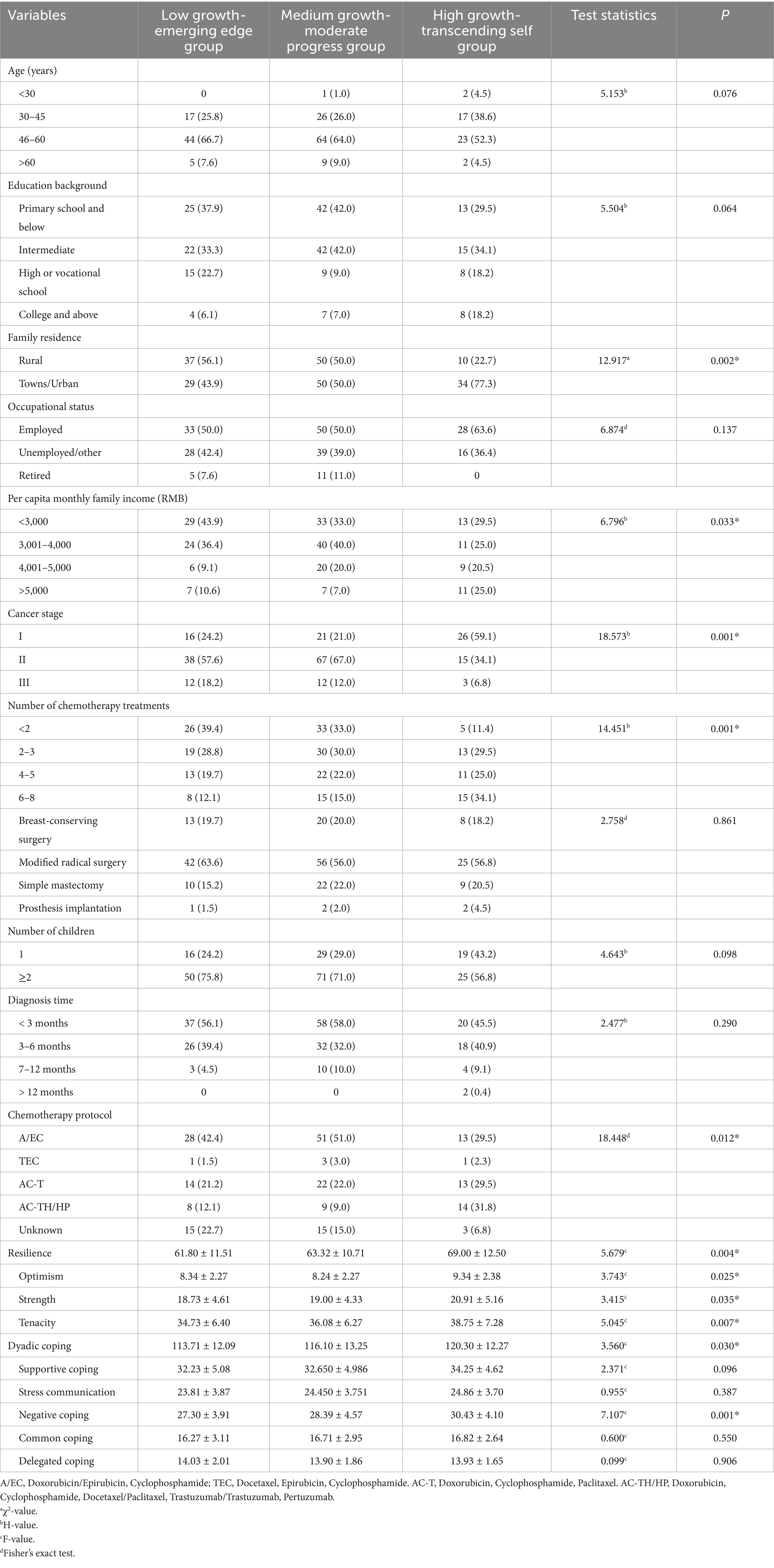
Table 2. Univariate analysis of post-traumatic growth in spouses of breast cancer patients (n = 210).
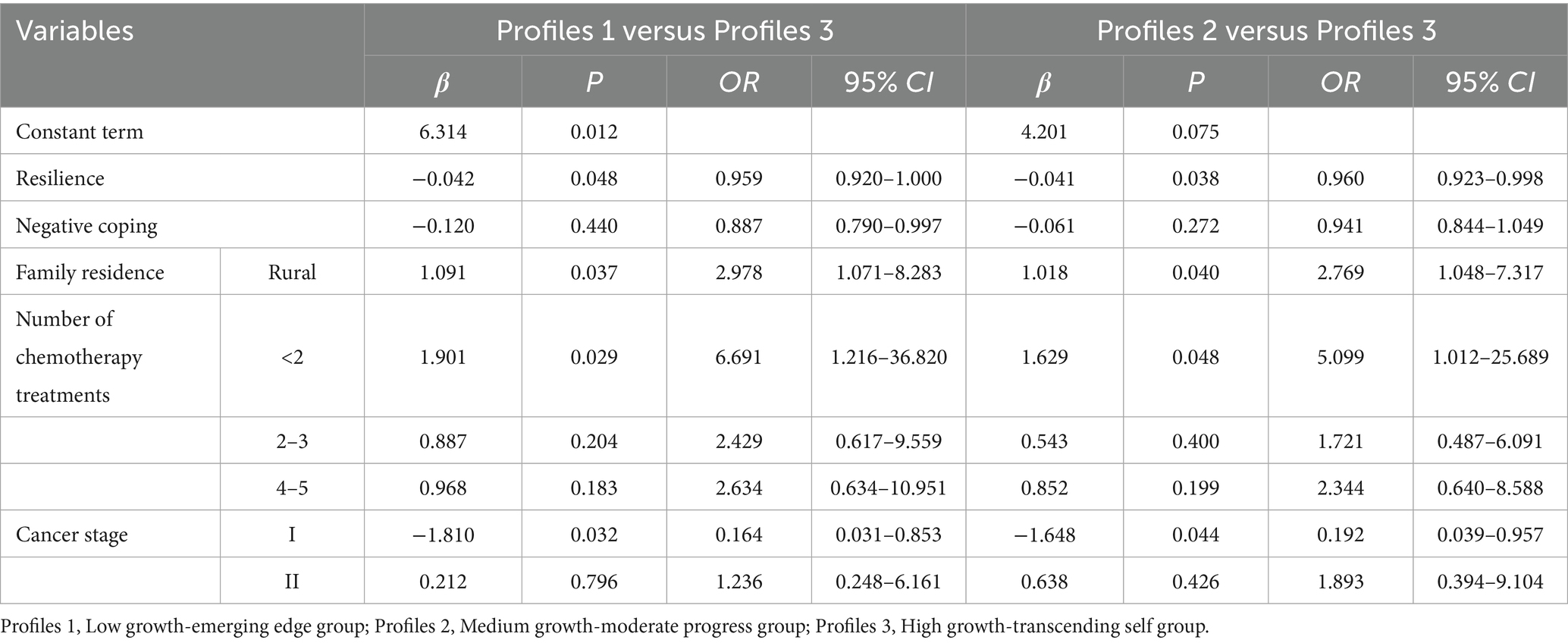
3.5 Multifactor analyses of three latent profile
Multivariate logistic regression analyses were conducted on the three latent profiles of PTG among BC patients’ spouses, using variables significant in the univariate serving as predictors and the latent profile of PTG of spouses as outcome variables, to explore the determinants of spousal PTG. See Table 3.
4 Discussion
4.1 Three latent profiles exist for PTG in BC patients’ spouses
Our study identified three distinct latent profiles of PTG in BC patients’ spouses using the LPA approach. The model fit indices confirmed significant interindividual variability in spouses’ PTG manifestations. The low growth-emerging edge group, at 31.43%, scored, lower than the other two groups on the overall dimensions of the three profiles, and the “Relating to Others” dimension was significantly lower than the other dimensions. Possible reasons are the low per capita income of the families in this group; the treatment of BC is characterized as continuous, expensive, cyclical and long-term, and good family economic income is a protective factor for the PTG of the spouses. Families with a low income have difficulty coping with the enormous economic pressure and psychological burden brought about by the cost of the treatment (21, 22), which leads to difficulties in generating positive psychological changes in the spouses. In addition, the “Relating to Others” group is a valuable resource for individuals to obtain social support. In establishing relationships with others, individuals not only gain emotional, informational, and social support but also enhance their ability to cope with challenges and grow psychologically (23). Therefore, medical personnel should choose appropriate treatment plans in clinical practice according to the family’s financial situation, and for particularly poor families, social financial assistance can be provided through channels such as the Water Drop Fundraising to alleviate the urgent need for disease treatment and the patients’ worries about seeing a doctor. The medium growth-moderate progress group, comprising 47.62%, is the most populous among the three profiles, which may be that the families in this group have middle income, their spouses are mainly middle-aged people with middle school education, and their families and careers are stable. Even though they may feel fearful during the process of fighting cancer, the middle income of the family, the national health insurance policy for the benefit of the people, the inclusion of biological products in the list of medicines for health insurance, and the execution of the ‘dual-channel’ health insurance reimbursement mechanism have all helped to alleviate their financial pressure. These factors have enabled families to provide better diagnostic protocols and care for their patients, reducing fear among spouses and increasing motivation for treatment (24). The high growth-transcending self group, which accounted for 20.95%, showed the greatest extent of post-traumatic growth among the three subgroups. This group outperformed the others with a much better score on the “Appreciation of Life” dimension. This could be because, in comparison to the other profiles, this one is younger and better educated, which could be explained by the reason that this group is younger and has a higher education level, which helps to improve their cognitive ability and health information literacy. They can have more comprehensive access to disease information and cognitive experiences, broader access to information about the disease, emotional support, and cognitive experiences so that the spouses in this group achieve higher PTG for the spouses as they support patients in their battle against cancer (25–27).
4.2 Factors influencing LPA
Rural residence spouses of BC patients who live in the “low growth-emerging edge group” are 1.091 times more numerous than those in the “high growth-transcending self group.” The outcomes are similar to Lu et al.’s (26) study findings. The reasons for this may be, firstly, that in the low growth-emerging edge group, the family income of families living in rural areas is predominantly < 3,000 yuan, and oncology treatment is faced with expensive medical costs, which are unaffordable, exacerbating the spouse’s pessimism and the burden of caregiving, and hampering the emergence of positive psychology (22); Secondly, rural medical and health resources and equipment, as well as access to knowledge of disease popularization activities, are lower than in towns (28). For the treatment of cancer, spouses and patients need to travel to tertiary hospitals, surrounded by unfamiliar people and environments, and the high cost of medical expenditures aggravates the spouse’s fear of the disease, resulting in a reduction in the level of PTG. In addition, in rural areas, the influence of the traditional concept of “cancer,” the labeling of cancer-related illnesses as “incurable,” and the sense of social alienation from those around them can lead to low self-esteem among spouses, which is not conducive to PTG (29). Therefore, we can establish an effective social support system to give psychological support to spouses, such as appealing to friends and relatives to give material or spiritual support to the patient’s family. The government can give appropriate subsidies according to the actual situation of the family of the cancer patient. To better comprehend the psychological condition of their wives and enable them to feel supported by society in their duty as caregivers, medical personnel should communicate more effectively with them. Offer appropriate psychological treatment. Encourage spouses to participate in lectures on disease knowledge in the department to make up for the blind spot of disease knowledge, and at the same time, promote the continuation of care service of Internet+ for them to change the cognition of the disease and elevate the degree of PTG.
The patient’s number of chemotherapy treatments was <2. Patients’ spouses had a higher probability of being classified in the “low growth-emerging edge group” (OR = 6.691, p = 0.029). In agreement with the findings of Lafuenti et al. (30) Some of the patients in this study with <2 chemotherapy treatments were in the post-surgical stage, when the chemotherapy protocol was unknown, and the diagnosis of BC and the absence of breasts subjected the patients to double physical and psychological harm, with the postoperative limb inconvenience, the lack of knowledge related to subsequent chemotherapy, and the prognosis of the disease exacerbating the patients’ psychological stress (31). In the face of sudden events that break the routine and orderly life, the spouse needs to give more care and comfort to the patient, as well as adapt to the change of family roles, which will undoubtedly produce negative psychology in the spouse and hinder the generation of his PTG. With the increase in the number of chemotherapy treatments, the spouse’s caregiving competency improve, the patient’s self-care ability improves and gradually adapts to the treatment plan, and the spouse experiences his value in caregiving, which is conducive to his PTG.
The lower the spouse’s negative coping score, the higher the probability of belonging to the “low growth-emerging edge group.” In agreement with the study of Suo et al. (15). Spouses play many roles in the patient’s disease treatment and recovery process: emotional supporters, family caregivers, financial supporters, decision-making participants, et al. Multiple pressures will undoubtedly produce problems affecting their health, such as sleep disorders, psychological pain, anxiety, et al., and spouses will use avoidance, concealment, and other negative coping styles to divert cancer-related communication and alleviate the patient’s fear of the disease. However, these protective buffering behaviors by spouses are not only detrimental to the generation of their PTG but also lead to less communication and intimacy in couples, which exacerbates the patient’s anxieties about their condition (15, 32). Therefore, medical personnel focus on the patient’s disease treatment at the same time and cannot ignore the psychological attention of the spouse. It should be regarded as husband and wife working together to cope with the pressure of the community to correct the patient’s or spouse’s negative coping and to enhance the positive DC, such as communication and support for each other so as to promote the two sides of the positive psychological changes and the adaptation to the disease.
The likelihood of spouses with cancer stage I patients being categorized under the “high growth-transcending self group” is higher in this research, similar to the findings of Liu et al. (33). Cancer staging assesses the severity of a tumor’s malignancy and the extent of its spread, and the prognosis and survival of patients can be predicted by tumor staging. Patients in the early clinical stage are characterized by mild disease, good prognosis, and long survival, and their spouses have higher hope and confidence in treatment (34). The later the clinical stage, the more likely it is that complications such as metastasis will occur, the patient’s survival rate will be low, treatment options will be limited, and the spouse’s sense of helplessness and hopelessness will increase dramatically, which is not conducive to positive psychology (33). Therefore, medical personnel should focus on the psychology of spouses of late-stage patients and give targeted psychological interventions to alleviate their psychological pain. At the same time, the government, communities, and townships should raise awareness of disease prevention and cancer screening, expand the coverage of the beneficiary population of free health checkups, and increase financial support for health education. Encouraging individuals with financial means to undergo annual routine medical checkups and raising public awareness of self-health will help increase the rate of early diagnosis of diseases, which is crucial for improving the effectiveness of treatments and the overall prognosis for patients.
Spouses with higher resilience showed significantly greater likelihood of belonging to the “high growth-transcending self group,” similar to the study results of Qin et al. (35). Resilience refers to the self-recovery and adaptive capacity of an individual who encounters adversity and shock events by mobilizing his or her internal and external resources and tapping into intrinsic cognitive and psychological attributes (36). Research has pointed out that resilience is a facilitator of PTG; when facing traumatic experiences, couples with strong resilience exhibit good acceptance and resilience, actively mobilize their intrinsic psychological traits, and make full use of external resources to make self-adjustment to adapt to the state of the disease, reduce the psychological burden, and improve their resilience, which facilitates the enhancement of PTG (35). Therefore, medical staff can help elevate PTG by reducing the spouse’s sense of shame, increasing his confidence in the caregiving process, and improving his ability to adapt to the illness through peer support exchange sessions, psychological intervention methods, and information support.
4.3 Limitations
Our study’s limitations include: Firstly, the causal relationship between the independent and dependent variables is not yet clear because the design of this study is a cross-sectional type. Future studies should utilize longitudinal tracking to examine the possible causal relationships between these variables. Secondly, the participants were only from the spouses of breast cancer patients in one hospital in Bengbu, China, which limited the external validity of the research results. Multi-center and large-sample studies can be conducted in the future to verify these findings. Additionally, the present study, with only spouses, neglected to consider the interactions of PTG between couples; therefore, in the future, the heterogeneity of different profiles of PTG could be explored for couples as a whole, providing a theoretical basis for the development of family-centred dyadic interventions.
5 Conclusion
In this research, through LPA, three latent profiles of PTG were identified in BC patients’ spouses, with differences in the distribution of resilience, coping styles, cancer stage, and the number of chemotherapy treatments across profiles. In the future, healthcare professionals can use resilience as a target for intervention, identify different types of spouses based on influencing factors, and further explore differentiated intervention options to enhance their resilience and standard of living and improve PTG chemotherapy treatments across profiles.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The study received ethical approval by Bengbu University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
XD: Methodology, Writing – review & editing, Software, Writing – original draft. XY: Data curation, Conceptualization, Methodology, Writing – review & editing, Funding acquisition, Supervision. YD: Writing – review & editing, Supervision, Methodology. ZS: Conceptualization, Writing – review & editing, Methodology. YX: Methodology, Conceptualization, Writing – review & editing. CS: Writing – review & editing, Resources. YC: Writing – review & editing, Resources. YS: Writing – review & editing, Investigation. XX: Writing – review & editing, Investigation. ShuZ: Investigation, Writing – review & editing. ZZ: Writing – review & editing, Investigation. ShiZ: Writing – review & editing, Investigation. YY: Writing – review & editing, Investigation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by grants from 2023 Postgraduate Innovation Plan of Bengbu Medical College (grant numbers Byycx23023); 2023 Medical Education Research Project of the Medical Education Branch of the Chinese Medical Association and the National Centre for Medical Education Development (grant numbers 2023B014); Quality Engineering Project of Anhui Provincial Department of Education (grant numbers 2021xqhzsjjd051 & 2021xsxxkc & 2022msgzs034); Bengbu Medical University Research Topics (grant numbers 2023byfy142sk & 2023byzd166sk).
Acknowledgments
We sincerely thank the participants in this study and the hospital nursing faculty for their help and support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sung, H, Ferlay, J, Siegel, RL, Laversanne, M, Soerjomataram, I, Jemal, A, et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
2. Fang, H, Zeng, Y, Liu, Y, and Zhu, C. The effect of the PERMA model-based positive psychological intervention on the quality of life of patients with breast cancer. Heliyon. (2023) 9:e17251. doi: 10.1016/j.heliyon.2023.e17251
3. White, J. Understanding family process: basics of family systems theory. J Comp Fam Stud. (1993) 26:281–2.
4. Congard, A, Christophe, V, Duprez, C, Baudry, AS, Antoine, P, Lesur, A, et al. The self-reported perceptions of the repercussions of the disease and its treatments on daily life for young women with breast cancer and their partners. J Psychosoc Oncol. (2019) 37:50–68. doi: 10.1080/07347332.2018.1479326
5. Sandgren, AK, Mullens, AB, Erickson, SC, Romanek, KM, and McCaul, KD. Confidant and breast cancer patient reports of quality of life. Qual Life Res. (2004) 13:155–60. doi: 10.1023/B:QURE.0000015287.90952.95
6. Acquati, C, Head, KJ, Rand, KL, Alwine, JS, Short, DN, Cohee, AA, et al. Psychosocial experiences, challenges, and recommendations for care delivery among Partners of Breast Cancer Survivors: a qualitative study. Int J Environ Res Public Health. (2023) 20:2786. doi: 10.3390/ijerph20042786
7. Goerling, U, Bergelt, C, Muller, V, and Mehnert-Theuerkauf, A. Psychosocial distress in women with breast Cancer and their partners and its impact on supportive care needs in partners. Front Psychol. (2020) 11:564079. doi: 10.3389/fpsyg.2020.564079
8. Tedeschi, RG, and Calhoun, LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress. (1996) 9:455–71. doi: 10.1007/BF02103658
9. Song, Y, Wang, M, Zhu, M, Wang, N, He, T, Wu, X, et al. Benefit finding among family caregivers of patients with advanced cancer in a palliative treatment: a qualitative study. BMC Nurs. (2024) 23:397. doi: 10.1186/s12912-024-02055-z
10. Ma, H, Hu, K, Wu, W, Wu, Q, Ye, Q, Jiang, X, et al. Illness perception profile among cancer patients and its influencing factors: a cross-sectional study. Eur J Oncol Nurs. (2024) 69:102526. doi: 10.1016/j.ejon.2024.102526
11. Luo, D, Eicher, M, and White, K. Individual resilience in adult cancer care: a concept analysis. Int J Nurs Stud. (2020) 102:103467. doi: 10.1016/j.ijnurstu.2019.103467
12. Wan, X, Huang, HT, Peng, QW, Yu, NX, Zhang, YM, Ding, YM, et al. A meta-analysis on the relationship between posttraumatic growth and resilience in people with breast cancer. Nurs Open. (2023) 10:2734–45. doi: 10.1002/nop2.1540
13. Bodenmann, G. Dyadic coping-a systematic-transactional view of stress and coping among couples: theory and empirical finding. Eur Rev Appl Psychol. (1997) 47:137–40.
14. Wang, Y, Wang, S, Tong, L, Zhuang, J, Xu, Y, Wu, Y, et al. Relationships between body image, dyadic coping and post-traumatic growth in breast cancer patients: a cross-sectional study. Front Psychol. (2024) 15:1368429. doi: 10.3389/fpsyg.2024.1368429
15. Suo, RF, Zhang, LJ, Tao, HM, Ye, FL, Zhang, YN, and Yan, J. The effects of dyadic coping and marital satisfaction on posttraumatic growth among breast cancer couples. Support Care Cancer. (2021) 29:5425–33. doi: 10.1007/s00520-021-06121-z
16. Hill, R. Families under stress: Adjustment to the crises of war separation and return. New York: Harper (1949).
17. Ertefaie, A, Small, DS, and Rosenbaum, PR. Quantitative evaluation of the trade-off of strengthened instruments and sample size in observational studies. J Am Stat Assoc. (2018) 113:1122–34. doi: 10.1080/01621459.2017.1305275
18. Wang, J, Chen, Y, Wang, YB, and Liu, XH. Revision of the posttraumatic growth inventory and testing its reliability and validity. J Nurs Sci. (2011) 26:26–8. doi: 10.3870/hlxzz.2011.14.026
19. Yu, X, and Zhang, J. Factor analysis and psychometric evaluation of the Connor Davidson resilience scale (CD-RISC) with Chinese people. Soc Behav Pers. (2007) 35:19–30. doi: 10.2224/sbp.2007.35.1.19
20. Xu, F, Hilpert, P, Randall, AK, Li, Q, and Bodenmann, G. Validation of the dyadic coping inventory with Chinese couples: factorial structure, measurement invariance, and construct validity. Psychol Assess. (2016) 28:e127–40. doi: 10.1037/pas0000329
21. Liu, R, Liu, JZ, Zhang, XB, Ai, QY, Li, H, Meng, LM, et al. Systematic evaluation of post-traumatic growth level and its infiuencing factors in breast cancer patients. Psychol Mon. (2024) 19:13–7. doi: 10.19738/j.cnki.psy.2024.04.003
22. Cui, C, Wang, K, An, J, and Jin, C. Current status and influencing factors of post-traumatic growth in maintenance hemodialysis. Int J Nurs Sci. (2017) 4:362–6. doi: 10.1016/j.ijnss.2017.09.008
23. Wang, F, Zhang, S, Liu, C, and Ni, Z. Post-traumatic growth and influencing factors among parents of premature infants: a cross-sectional study. BMC Psychol. (2023) 11:388. doi: 10.1186/s40359-023-01360-7
24. National Healthcare Security Administration. Notice of the state administration of taxation of the Ministry of Finance on to do a good job of 2023 basic medical insurance for urban and rural residents [Z]. China; State Administration of Taxation. (2023). Avaiable online at: https://www.nhsa.gov.cn/art/2024/8/26/art_104_13632.html
25. Fekih-Romdhane, F, Riahi, N, Achouri, L, Jahrami, H, and Cheour, M. Social support is linked to post-traumatic growth among Tunisian postoperative breast cancer women. Healthcare (Basel). (2022) 10:1710. doi: 10.3390/healthcare10091710
26. Lu, W, Xu, C, Hu, X, Liu, J, Zhang, Q, Peng, L, et al. The relationship between resilience and posttraumatic growth among the primary caregivers of children with developmental disabilities: the mediating role of positive coping style and self-efficacy. Front Psychol. (2021) 12:765530. doi: 10.3389/fpsyg.2021.765530
27. Casellas-Grau, A, Sumalla, EC, Lleras, M, Vives, J, Sirgo, A, Leon, C, et al. The role of posttraumatic stress and posttraumatic growth on online information use in breast cancer survivors. Psychooncology. (2018) 27:1971–8. doi: 10.1002/pon.4753
28. Liu, Y, Li, Y, Chen, L, Li, Y, Qi, W, and Yu, L. Relationships between family resilience and posttraumatic growth in breast cancer survivors and caregiver burden. Psychooncology. (2018) 27:1284–90. doi: 10.1002/pon.4668
29. Wu, Y, Yan, Z, Fornah, L, Zhao, J, and Wu, S. The mediation effect of social support between stigma and social alienation in patients with stroke. Front Public Health. (2023) 11:1290177. doi: 10.3389/fpubh.2023.1290177
30. Lafuenti, L, Dinapoli, L, Mastrilli, L, Savoia, V, Linardos, M, Masetti, R, et al. Post-traumatic growth in oncological patients during the COVID-19 pandemic. Health Psychol Rep. (2024) 12:142–53. doi: 10.5114/hpr/169165
31. Chen, YY. Study on the current situation of benefit finding and its influencing factors among spouses of women with breast cancer [D]. Yangzhou, China; Yangzhou University (2021)
32. Shi, GY, Shi, TY, Liu, Y, and Cai, YJ. Relationships between dyadic coping, intimate relationship and post-traumatic growth in patients with breast cancer: a cross-sectional study. J Adv Nurs. (2021) 77:4733–42. doi: 10.1111/jan.14946
33. Liu, Z, Thong, MSY, Doege, D, Koch-Gallenkamp, L, Bertram, H, Eberle, A, et al. Prevalence of benefit finding and posttraumatic growth in long-term cancer survivors: results from a multi-regional population-based survey in Germany. Br J Cancer. (2021) 125:877–83. doi: 10.1038/s41416-021-01473-z
34. Zhang, QY, Xiao, S, Wei, TT, Chen, XC, Sun, LY, Li, J, et al. Benefit finding and its influencing factors for caregivers of patients with cancer. Chin J Pract Nurs. (2017) 33:598–602. doi: 10.3760/cma.j.issn.1672-7088.2017.08.010
35. Qin, XQ, Feng, YS, Qu, FL, Luo, YR, Chen, BY, Chen, MY, et al. Posttraumatic growth among parents of children with autism Spectrum disorder in China and its relationship to family function and mental resilience: a cross-sectional study. J Pediatr Nurs. (2021) 57:E59–67. doi: 10.1016/j.pedn.2020.10.026
Keywords: breast cancer, patients, spouses, post-traumatic growth, latent profile analysis
Citation: Duan X, Yang X, Duan Y, Shen Z, Xiong Y, Sun C, Chen Y, Shao Y, Xu X, Zhao S, Zhang Z, Zhang S and Yang Y (2025) A latent profile analysis of post-traumatic growth in spouses of breast cancer patients. Front. Public Health. 13:1634910. doi: 10.3389/fpubh.2025.1634910
Edited by:
Mosad Zineldin, Linnaeus University, SwedenReviewed by:
María Cantero-García, Universidad a Distancia de Madrid, SpainSusana Pedras, University of Lusíada, Portugal
Guoqian He, Sichuan University, China
Copyright © 2025 Duan, Yang, Duan, Shen, Xiong, Sun, Chen, Shao, Xu, Zhao, Zhang, Zhang and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiumu Yang, MDcwMDAxM0BiYm11LmVkdS5jbg==
 Xiaocui Duan
Xiaocui Duan Xiumu Yang
Xiumu Yang Yongli Duan3
Yongli Duan3 Yujiao Shao
Yujiao Shao Shiqing Zhang
Shiqing Zhang