- 1Department of Pharmaceutical Chemistry, Faculty of Pharmacy, M. S. Ramaiah University of Applied Sciences, Bangalore, India
- 2Saidu Group of Teaching Hospitals, Saidu Sharif, Pakistan
- 3Department of Pharmacy, University of Peshawar, Peshawar, Pakistan
- 4District Headquarter Hospital-Charsadda, Charsadda, Pakistan
- 5Department of Internal Medicine, Rama Medical College Hospital and Research Centre, Hapur, India
- 6Department of Paediatrics, Dr. D. Y. Patil Medical College Hospital and Research Centre, Dr. D. Y. Patil Vidyapeeth (Deemed-to-be-University), Pune, India
- 7Department of Public Health Dentistry, Dr. D. Y. Patil Dental College and Hospital, Dr. D. Y. Patil Vidyapeeth (Deemed-to-be-University), Pune, India
- 8Clinical Microbiology, RDC, Manav Rachna International Institute of Research and Studies, Faridabad, India
- 9Department of Pharmacy, Abasyn University Peshawar, Peshawar, Pakistan
- 10Department of Pharmacy, CECOS University Peshawar, Peshawar, Pakistan
- 11American University of the Middle East, Kuwait City, Kuwait
- 12Spinghar University Faculty of Medicine, Jalalabad, Afghanistan
Background: The increasing popularity of electronic cigarettes (e-cigarettes) has introduced new public health challenges and concerns. While promoted as safer alternatives to conventional tobacco and as tools for quitting smoking, e-cigarettes have raised alarm about possible long-term health consequences. This systematic review and meta-analysis sought to evaluate the association between electronic cigarette consumption and sleep disturbances.
Methods: We performed comprehensive searches in EMBASE, Web of Science, and PubMed up to September 18, 2024, to locate studies examining the link between e-cigarette use and sleep duration, sleep disorders, and insomnia. A meta-analysis was conducted to calculate pooled odds ratios (ORs). The quality of the studies was evaluated using the Newcastle-Ottawa Scale. Meta-analysis was performed using R software (Version 4.3).
Results: A total of 14 cross-sectional studies were included from 554 unique records screened. E-cigarette users exhibited a notably elevated risk of having shorter sleep duration compared to non-users, with a pooled odds ratio of 1.38 (95% CI: 1.24–1.55). Several studies reported that e-cigarette users also had higher odds of sleep disturbances, such as insomnia and reliance on sleep medications. Among adolescents, e-cigarette use was associated with a 33 to 61% increased risk of inadequate sleep.
Conclusion: E-cigarette use may be associated with sleep disturbances, including shorter sleep duration and increased sleep difficulties. Future long term longitudinal studies are warranted for better evidence.
1 Introduction
Electronic cigarettes (e-cigarettes) are devices that vaporize a liquid containing nicotine, flavorings, and other chemicals, simulating a smoking-like experience without combustion (1). Initially marketed as a safer alternative to traditional tobacco products, e-cigarettes have gained significant popularity (2, 3). However, increasing evidence suggests that their use may be associated with various health issues. Research has highlighted potential risks associated with exposure to e-cigarette aerosols, including impacts on pulmonary function, cardiovascular well-being, and sleep quality (4–7).
Research indicates that nicotine, a primary component in most e-cigarettes, disrupts sleep patterns due to its stimulating properties, leading to difficulty falling asleep and maintaining restful sleep (8, 9). In addition, inhaling e-cigarettes may affect lung function and cause oxidative stress, further contributing to impaired sleep quality (10, 11). Research indicates that e-cigarette use is associated with negative sleep outcomes, including inadequate sleep duration and trouble sleeping. The use of e-cigarettes has been linked to negative effects on sleep health, including increased odds of inadequate sleep duration and trouble sleeping. Research indicates that both current and former e-cigarette users experience significant sleep disturbances compared to non-users. Current e-cigarette users are 1.82 times more likely to experience shorter sleep durations than non-users (12). Among young adults, exclusive e-cigarette users have an increased odds of inadequate sleep duration after adjusting for various co-variates (13). Dual users of e-cigarettes and conventional tobacco report increased sleep latency, taking longer to fall asleep (14). In addition to that, e-cigarette users have reported greater sleep difficulties and a higher reliance on sleep medications compared to non-users (15).
The association between e-cigarette use and poor sleep health is explored by some studies with varying results (16). However, some research suggests that individual factors may influence this relationship, highlighting the complexity of interactions between e-cigarette use and sleep health (15, 16). Despite their growing use, the long-term impact of e-cigarettes on sleep remains understudied, and further research is needed to understand the extent of these disturbances.
A systematic review on this topic has not yet been conducted. Therefore, this systematic review and meta-analysis aim to bridge this research gap by examining the existing literature on the link between e-cigarette use and sleep disturbances. Through the synthesis of findings from various studies, the analysis seeks to offer a detailed understanding of this association. The findings are anticipated to offer valuable insights into the potential psychosocial risks associated with e-cigarette use, laying the groundwork for further studies and informing policymakers and healthcare providers in mitigating the harmful effects of e-cigarette usage.
2 Methods
This systematic review and meta-analysis complied with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to guarantee both clarity and comprehensiveness in its reporting methodology (Supplementary Table S1). The primary goal was to systematically evaluate and consolidate the current evidence on the correlation among e-cigarette usage, sleep duration, sleep disturbances, and insomnia. Additionally, this review has been pre-registered in the PROSPERO.
2.1 Search strategy
A structured search strategy was formulated to locate studies examining the link among e-cigarette consumption and sleep duration, sleep disturbances, and insomnia. A thorough search of various electronic databases, including EMBASE, Web of Science, and PubMed, was carried out from their inception up to September 18, 2024. The search method employed a combination of terms related to e-cigarette use (e.g., “vaping,” “electronic nicotine delivery systems,” “e-cigarettes”) along with terms associated with sleep disorders (e.g., “insomnia,” “sleep disturbances,” “sleep–wake disorders,” “sleep apnea,” and “sleep disorder”). A detailed description of the search strategy is provided in Supplementary Table S2.
2.2 Eligibility criteria
Studies involving the general population were included without restrictions to allow for a wide-ranging and thorough analysis. The main exposure of interest was identified as the use of e-cigarettes, vaping devices, or Electronic Nicotine Delivery Systems (ENDS). However, studies that solely concentrated on conventional tobacco smoking were excluded due to its distinct mechanisms and well-documented effects. In terms of outcomes, we incorporated studies investigating sleep disorders, sleep patterns, abnormal dreams, sleep disturbances, sleep–wake disorders, sleep apnea, parasomnia, difficulties with sleep initiation and maintenance, dyssomnia or insomnia. Eligible study designs included observational studies (cross-sectional, longitudinal, retrospective, prospective, and case–control) to capture the available quantitative evidence on e-cigarette use and sleep disturbances. No experimental studies, such as randomized controlled trials, were identified in our comprehensive search, likely due to the ethical constraints of exposing participants to e-cigarettes and the emerging nature of this research field. To minimize confounding from pre-existing conditions that may independently affect sleep quality, we excluded studies focusing on populations with specific chronic diseases. Qualitative research, policy evaluations, commentaries, case reports, case series, systematic reviews, and animal studies were excluded, as these sources lacked the empirical data necessary to directly answer our research question.
2.3 Study selection
Two reviewers independently screened the titles and abstracts for eligibility using the Nested-Knowledge web platform. Full-text articles of studies identified as potentially relevant were procured and independently scrutinized for eligibility. Any discrepancies were resolved through deliberation or, when required, by consulting a third reviewer.
2.4 Data extraction
Data extraction was performed independently by two reviewers utilizing a standardized template. The extracted data encompassed study attributes (e.g., author, publication year, country, study design, and sample size), participant demographics, and sleep disorder outcomes. Any discrepancies identified during the extraction process were resolved through deliberation or, if necessary, by consulting a third reviewer.
2.5 Quality assessment
The quality evaluation of the studies was performed through the Newcastle-Ottawa Scale, which reviews the cohort selection process, the comparability of the cohorts, and how the exposure or outcome of interest was assessed.
2.6 Statistical analysis
A random effects model was selected for the meta-analysis to account for the heterogeneity in study populations, e-cigarette use patterns, and sleep outcome measures, which likely contribute to variability in effect sizes across studies. This approach allows for a more conservative estimate of the pooled effect while acknowledging between-study differences. The link between e-cigarette use and sleep disorders was analyzed using odds ratios (ORs) with 95% confidence intervals (CIs) (17, 18). The I2 statistic was employed to quantify heterogeneity across the studies, with a 95% prediction interval providing additional insight into the extent of variability. Publication bias was evaluated through funnel plots and Egger’s test. The analysis was conducted using the ‘Meta’ and ‘Metafor’ packages in R statistical software (Version 4.3).
3 Result
3.1 Literature search
The primary search identified a total of 554 records, which was narrowed down to 373 after eliminating 181 duplicates. Each remaining record was evaluated according to our established inclusion criteria, resulting in 44 reports being deemed potentially relevant for full-text review. However, a detailed assessment led to the exclusion of 30 reports, primarily because they did not address the desired outcomes, specifically sleep disturbances in relation to e-cigarette consumption. Ultimately, 14 studies were found to be eligible (12, 15, 16, 19–29) for inclusion in our systematic review and meta-analysis (Figure 1).
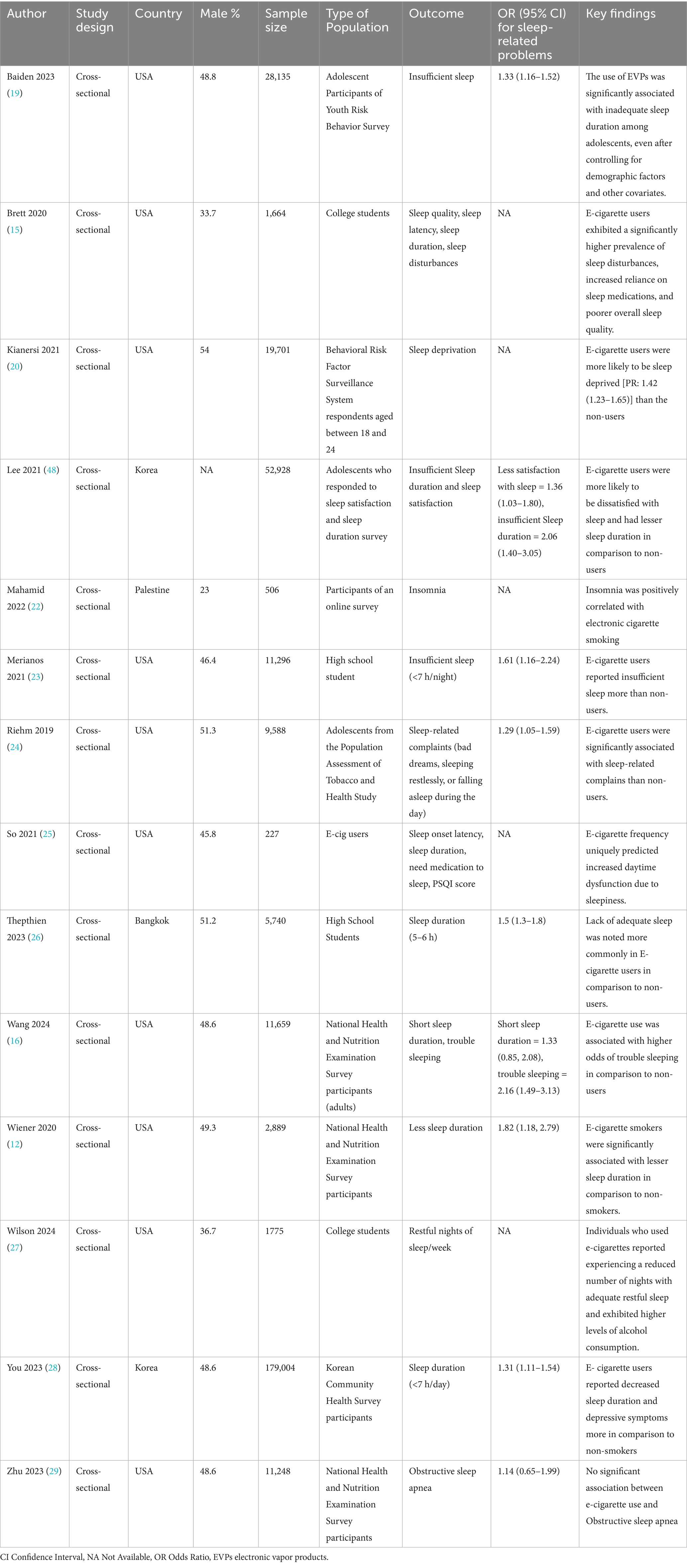
3.2 Characteristics of included studies
This systematic review includes 14 cross-sectional studies across (Table 1) various countries, primarily in the USA, except for a few from Palestine, Korea, and Thailand. The sample sizes of these studies range from 227 to 179,004 participants. These studies utilized a cross-sectional design to examine the connection among e-cigarette use and sleep-related outcomes among various demographic groups, such as teenagers, college students, adults, and the general population. The studies consistently show that e-cigarette users experience poor sleep outcomes, such as reduced sleep quality, shorter sleep duration, and sleep disturbances. Adolescents and young adults are frequently impacted, with vaping linked to sleep deprivation, insomnia, and increased reliance on sleep medications. Multiple studies highlighted the association between e-cigarette use and insufficient sleep duration. The evaluation of study quality is presented in Supplementary Table S3.
The association between e-cigarette use and sleep issues has been widely examined in these included studies revealing a consistent link between e-cigarette use and various sleep disturbances. Several studies, including Baiden et al. (19) and Merianos et al. (23), found that adolescent e-cigarette users were significantly more likely to experience insufficient sleep duration, with OR of 1.33 (95% CI: 1.16–1.52) and 1.61 (95% CI: 1.16–2.24), respectively. Similarly, Brett et al. (15) and Wilson (27) noted that college students who used e-cigarettes reported poorer sleep quality, greater reliance on sleep medications, fewer restful nights, and higher rates of sleep disturbances. Wang et al. (16) found an increased risk of trouble sleeping among e-cigarette users (OR: 2.16, 95% CI: 1.49–3.13). Similar findings were observed by Wiener (12), who linked e-cigarette use to shorter sleep durations (OR: 1.82, 95% CI: 1.18–2.79). Studies also showed that e-cigarette users experienced broader sleep-related complaints. For example, Riehm et al. (24) found that adolescents using e-cigarettes reported more frequent sleep-related issues such as bad dreams and daytime sleepiness (OR: 1.29, 95% CI: 1.05–1.59), while So (25) noted that e-cigarette use predicted increased daytime dysfunction due to sleepiness. In You et al. (28) reported similar associations in Korean adolescents, with e-cigarette users experiencing lower sleep satisfaction and shorter sleep durations (OR: 2.06, 95% CI: 1.40–3.05) and a higher likelihood of insufficient sleep (OR: 1.31, 95% CI: 1.11–1.54). Thepthien (26) observed similar results among high school students in Bangkok (OR: 1.5, 95% CI: 1.3–1.8).
3.3 Meta-analysis of the association between e-cigarette use and sleep duration
We performed a meta-analysis to evaluate the association between e-cigarette usage and inadequate sleep. The pooled odds ratio (OR = 1.38, 95% CI: 1.25 to 1.52) indicates a statistically significant association between insufficient or short sleep and e-cigarette smoking, suggesting a 38% increased risk in those who smoke e-cigarettes. The lack of heterogeneity (I2 = 0%) indicates that the results are consistent across the included studies. Thus, insufficient sleep appears to be a significant risk factor for the outcome of interest in this meta-analysis (Figure 2).
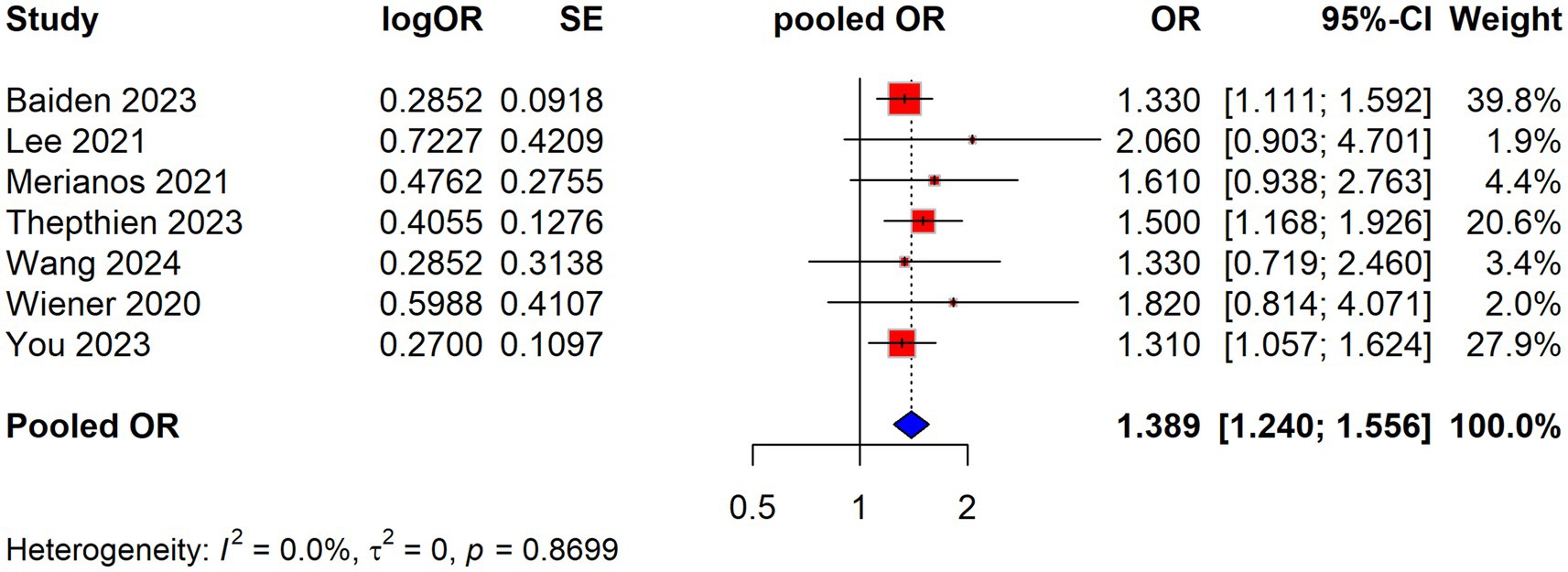
Figure 2. Association between electronic cigarette use and short sleep duration shown by pooled ORs from studies.
3.4 E-cigarette use and obstructive sleep apnea
Only one study reported the association between e-cigarette use and obstructive sleep apnea (29). The study found no significant association, with an OR of 1.14 (95% CI: 0.65–1.99).
3.5 Sensitivity analysis
A sensitivity analysis was performed utilizing the leave-one-out method, showing that the overall results of the meta-analysis are robust. No individual study substantially impacts the pooled OR, as the OR values remain consistent across the different leave-one-out scenarios. Thus, the overall odds ratio can be considered reliable and consistent even when individual studies are excluded from the analysis (Figure 3).
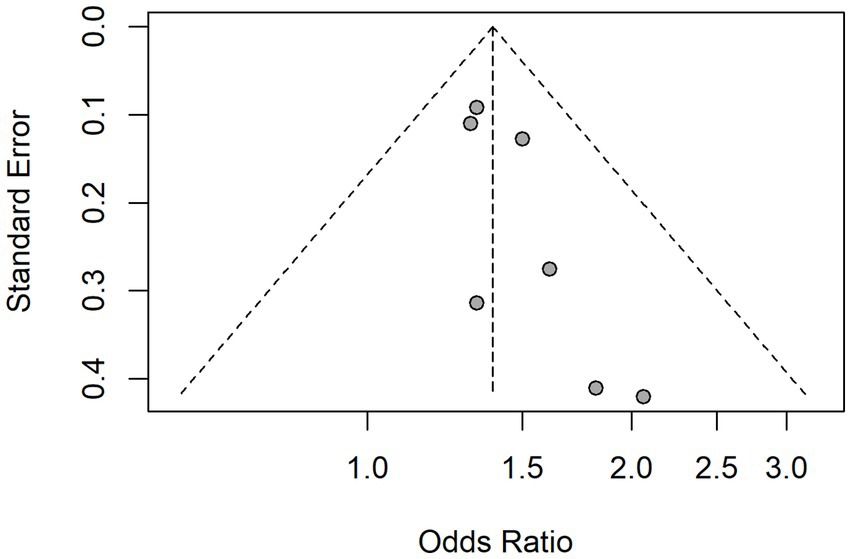
3.6 Publication bias
Publication bias in this meta-analysis was assessed through graphical examination of funnel plots and the application of Egger’s test, as presented in Figure 4. In the funnel plot, there appears to be a slight asymmetry, with more studies clustered on the right side, showing higher odds ratios. The left side contains fewer studies, which may suggest the potential for publication bias. However, the overall spread of the studies does not indicate extreme bias. The Egger test also indicated the possibility of publication bias, with a p-value of 0.03.
4 Discussion
The results of this study offer substantial documentation of a strong link between e-cigarette use and an increased risk of sleep disturbances, including shorter sleep duration, extended sleep latency, and reduced sleep quality. This is particularly concerning given the growing popularity of e-cigarettes, especially among adolescents and young adults. Our analysis shows that e-cigarette users are 39.1% more likely to suffer from inadequate sleep duration. These findings were consistently observed across studies involving both the general population and younger groups, suggesting that the connection between e-cigarette use and sleep problems is widespread and not limited to specific subpopulations.
Sleep is critical for both the physical and mental health of individuals, influencing nearly all aspects of a person’s life either directly or indirectly. Sleep has been given equal importance as healthy diet and physical workout for the better health of individuals (30). Researchers have emphasized the need of promoting importance of sleep health at community level globally (31). Inadequate sleep can affect the immune system thus making sleep deprived individuals more prone to various disease and infections (32, 33). Inadequate sleep for a longer duration can affect mental health of an individual leading to more depression and other related problems (34) Sleep is vital to maintain optimal health and proper day to day functions in our life. As proper sleep is crucial to maintain good health and functioning of body, any sleep related disturbance can not only effect normal physiological functioning of body but also affect various other aspects of individual’s life. Deficiency of sleep can affect productivity and economic growth of individual as well as the nation (35). Lack of adequate sleep can also lead fatigue and thus more road traffic accidents (36). The amount of sleep required for optimal health varies between individuals and is influenced by factors such as age and sociodemographic characteristics. Generally, 7 or more hours of sleep per night is considered necessary for maintaining good health (37). Insufficient sleep can lead to depression and physical activities/health is also affected (28, 38).
E-cigarette use, commonly referred to as vaping, has gained popularity over the past decade, particularly among adolescents and young adults. Recent research has begun to explore the potential health impacts of vaping, including its association with sleep disturbances. Electronic cigarettes, initially promoted as an alternative to conventional cigarettes, have been repeatedly shown to pose significant risks to physical, physiological and mental health (6, 26, 39). Nicotine, the primary addictive component of most e-cigarettes, is a stimulant that affects sleep quality. Nicotine activates β2-containing nAChRs, which are crucial for regulating sleep–wake cycles and micro-arousals. This activation can lead to increased wakefulness and disrupted sleep patterns (40, 41). In studies, nicotine exposure has been shown to diminish protective arousal responses during sleep, exacerbating conditions like sleep-disordered breathing (42). Smokers exhibit higher nocturnal hypoxia indices, indicating that e-cigarette use may similarly impair oxygen saturation during sleep, potentially leading to sleep apnea (43). The correlation between smoking intensity and decreased nocturnal oxygen saturation suggests that e-cigarette users may experience similar respiratory disturbances (44). While causality has yet to be fully established, the data suggest that the stimulant effects of nicotine combined with the other potential irritants in e-cigarette vapor may play a role in negatively affecting sleep. A dose–response relationship exists, where increased smoking correlates with heightened sleep disturbances, including snoring and short sleep (45, 46).
Our study demonstrates that e-cigarette use is associated with various sleep-related disturbances, including reduced sleep duration, increased sleep latency, poor sleep quality, and insomnia. The findings reveal a notable association between e-cigarette use and reduced or insufficient sleep duration, comparable to the harmful effects associated with traditional cigarette smoking (15). Even irregular e-cigarette users experience negative impacts on sleep, including shortened sleep duration and altered sleep quality. Sleep quality encompasses four key attributes: sleep efficiency, sleep latency, sleep duration, and wakefulness after sleep onset. Multiple studies have consistently reported decreased sleep duration and overall poorer sleep quality among e-cigarette users sleep (15, 47). Furthermore, e-cigarette users are more likely to use medications to aid sleep, and conditions such as insomnia and parasomnias are more prevalent in this group compared to non-users (22, 24, 48). Given the critical role of sleep in maintaining overall health, these findings emphasize the need for targeted interventions to reduce e-cigarette use and raise awareness about its impact on sleep health.
A key strength of our study is that significant associations were observed between e-cigarette use and sleep disturbances for most outcomes, with the exception of OSA, where findings were inconclusive. The consistency of the included studies is homogenous. Most of the included studies are of good quality. Our study has some limitations. A key limitation of this review is the reliance on cross-sectional studies, which limits the ability to establish temporality or causality between e-cigarette use and sleep disturbances. The cross-sectional nature of the included studies limits the ability to fully account for these confounders. While some studies adjusted for covariates like age, sex, and smoking status, residual confounding from unmeasured factors, such as psychological conditions or socioeconomic disparities, may persist. The absence of experimental studies in the literature highlights a critical gap, and future research should consider longitudinal or, where ethically feasible, experimental designs to better elucidate the causal pathways. Most of the studies are based in the United States, which may restrict the applicability of the results to populations in other regions. The potential for publication bias also raises concerns regarding the validity of the results. Our analysis might have overlooked important demographic factors that might impact the link between e-cigarette use and sleep disturbances, factors like economic background or underlying psychological conditions.
5 Conclusion
E-cigarettes are often considered as an alternative to conventional cigarettes; however, they are not devoid of harmful effects. Our study clearly highlighted the association between use of e-cigarettes and sleep related disturbances. Adequate sleep is fundamental to overall health and influences various aspects of life, both professional and personal. The use of e-cigarettes should be regulated, with increased public health initiatives and policy interventions aimed at reducing their consumption. Future longitudinal and, where feasible, experimental studies are warranted to establish temporality and causality, addressing the current reliance on observational data accounting for potential confounders, sociodemographic and lifestyle factors.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
HS: Investigation, Writing – review & editing, Methodology, Validation, Visualization. AJ: Investigation, Methodology, Writing – review & editing, Conceptualization, Data curation, Formal analysis. AV: Conceptualization, Investigation, Methodology, Writing – review & editing, Software. RS: Conceptualization, Investigation, Data curation, Writing – original draft. RM: Data curation, Investigation, Methodology, Software, Writing – review & editing. AfU: Investigation, Methodology, Software, Writing – review & editing, Formal analysis, Validation. AR: Methodology, Writing – review & editing, Conceptualization, Data curation, Visualization. MA: Writing – review & editing, Methodology, Resources, Validation, Visualization. AsU: Formal analysis, Investigation, Software, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors acknowledge the Nested-Knowledge, MN, USA for providing the access to the software.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1662234/full#supplementary-material
References
1. Carvalho, MT, Rodrigues, ACF, Rocha, IR, and Pereira, LP. Electronic cigarette use and its systemic repercussions In: LP Pereira, editor. A look at development. Brazil: Seven Editora (2023)
2. Bushi, G, Khatib, MN, Balaraman, AK, Ballal, S, Bansal, P, Tomar, BS, et al. Prevalence of dual use of combustible tobacco and E-cigarettes among pregnant smokers: a systematic review and meta-analysis. BMC Public Health. (2024) 24:3200. doi: 10.1186/s12889-024-20746-9
3. Goel, S, Shabil, M, Kaur, J, Chauhan, A, and Rinkoo, AV. Safety, efficacy and health impact of electronic nicotine delivery systems (ENDS): an umbrella review protocol. BMJ Open. (2024) 14:e080274. doi: 10.1136/bmjopen-2023-080274
4. Shabil, M, Khatib, MN, Ballal, S, Bansal, P, Tomar, BS, Ashraf, A, et al. The impact of electronic cigarette use on periodontitis and periodontal outcomes: a systematic review and meta-analysis. BMC Oral Health. (2024) 24:1197. doi: 10.1186/s12903-024-05018-7
5. Shabil, M, Malvi, A, Khatib, MN, Ganesan, S, Kaur, M, Srivastava, M, et al. Association of electronic cigarette use and risk of COPD: a systematic review and meta-analysis. Npj primary care. Respir Med. (2025) 35:31. doi: 10.1038/s41533-025-00438-6
6. Awad, AA, Itumalla, R, Gaidhane, AM, Khatib, MN, Ballal, S, Bansal, P, et al. Association of electronic cigarette use and suicidal behaviors: a systematic review and meta-analysis. BMC Psychiatry. (2024) 24:608. doi: 10.1186/s12888-024-06012-7
7. Malvi, A, Khatib, MN, Ganesan, S, Kaur, M, Srivastava, M, Barwal, A, et al. Assessing the impact of electronic nicotine delivery systems on chronic obstructive pulmonary disease: A systematic review and meta-analysis. Respir Med. (2025) 241:108059. doi: 10.1016/j.rmed.2025.108059
8. Kaisar, MA, Prasad, S, Liles, T, and Cucullo, L. A decade of e-cigarettes: limited research & unresolved safety concerns. Toxicology. (2016) 365:67–75. doi: 10.1016/j.tox.2016.07.020
9. Hammond, S, and Phillips, J. E-cigarettes and vaping. Workplace Health Saf. (2020) 68:301. doi: 10.1177/2165079920914635
10. Sapru, S, Vardhan, M, Li, Q, Guo, Y, Li, X, and Saxena, D. E-cigarettes use in the United States: reasons for use, perceptions, and effects on health. BMC Public Health. (2020) 20:1518. doi: 10.1186/s12889-020-09572-x
11. Rom, O, Pecorelli, A, Valacchi, G, and Reznick, AZ. Are e-cigarettes a safe and good alternative to cigarette smoking? Ann N Y Acad Sci. (2014) 1340:65–74. doi: 10.1111/nyas.12609
12. Wiener, RC, Waters, C, Bhandari, R, Trickett Shockey, AK, and Alshaarawy, O. The Association of Sleep Duration and the use of electronic cigarettes, NHANES, 2015-2016. Sleep Disord. (2020) 2020:1–12. doi: 10.1155/2020/8010923
13. Merianos, AL, Mahabee-Gittens, EM, Hill, MJ, Olaniyan, AC, Smith, ML, and Choi, K. Electronic cigarette use and cigarette smoking associated with inadequate sleep duration among U.S. young adults. Prev Med. (2023) 175:107712. doi: 10.1016/j.ypmed.2023.107712
14. Advani, I, Gunge, D, Boddu, S, Mehta, S, Park, K, Perera, S, et al. Dual use of e-cigarettes with conventional tobacco is associated with increased sleep latency in cross-sectional study. Sci Rep. (2022) 12:2536. doi: 10.1038/s41598-022-06445-8
15. Brett, EI, Miller, MB, Leavens, ELS, Lopez, SV, Wagener, TL, and Leffingwell, TR. Electronic cigarette use and sleep health in young adults. J Sleep Res. (2019) 29:2902. doi: 10.1111/jsr.12902
16. Wang, S, Nandy, RR, and Rossheim, ME. Associations between e-cigarette use and sleep health among adults in the United States, NHANES 2015–2018. Sleep Med. (2024) 114:220–8. doi: 10.1016/j.sleep.2024.01.005
17. Bushi, G, Padhi, BK, Shabil, M, Satapathy, P, Rustagi, S, Pradhan, KB, et al. Cardiovascular disease outcomes associated with obstructive sleep apnea in diabetics: a systematic review and meta-analysis. Diseases. (2023) 11:103. doi: 10.3390/diseases11030103
18. Shabil, M, Bushi, G, Rai, N, and Abu Serhan, H. Comment on: “efficacy and safety of tebentafusp in patients with metastatic uveal melanoma: A systematic review and meta-analysis”. Hum Vaccin Immunother. (2024) 20:2398870. doi: 10.1080/21645515.2024.2398870
19. Baiden, P, Spoor, SP, Nicholas, JK, Brown, FA, LaBrenz, CA, and Spadola, C. Association between use of electronic vaping products and insufficient sleep among adolescents: findings from the 2017 and 2019 YRBS. Sleep Med. (2023) 101:19–27. doi: 10.1016/j.sleep.2022.10.005
20. Kianersi, S, Zhang, Y, Rosenberg, M, and Macy, JT. Association between e-cigarette use and sleep deprivation in U.S. young adults: results from the 2017 and 2018 behavioral risk factor surveillance system. Addict Behav. (2021) 112:6646. doi: 10.1016/j.addbeh.2020.106646
21. Li, W, Kalan, ME, Kondracki, AJ, Gautam, P, Jebai, R, Erinoso, O, et al. Poor sleep duration and E-cigarette/cigarette use among US adults with cardiovascular diseases: findings from the 2022 BRFSS cross-sectional study. Sleep Breath. (2024) 28:2701–10. doi: 10.1007/s11325-024-03140-y
22. Mahamid, F, Bdier, D, and Damiri, B. Energy drinks, depression, insomnia and stress among Palestinians: the mediating role of cigarettes smoking, electronic cigarettes and waterpipe. J Ethn Subst Abus. (2022) 23:823–38. doi: 10.1080/15332640.2022.2136812
23. Merianos, AL, Jandarov, RA, Choi, K, Fiser, KA, and Mahabee-Gittens, EM. Combustible and electronic cigarette use and insufficient sleep among U.S. high school students. Prev Med. (2021) 147:6505. doi: 10.1016/j.ypmed.2021.106505
24. Riehm, KE, Rojo-Wissar, DM, Feder, KA, Mojtabai, R, Spira, AP, Thrul, J, et al. E-cigarette use and sleep-related complaints among youth. J Adolesc. (2019) 76:48–54. doi: 10.1016/j.adolescence.2019.08.009
25. So, CJ, Meers, JM, Alfano, CA, Garey, L, and Zvolensky, MJ. Main and interactive effects of nicotine product type on sleep health among dual combustible and E-cigarette users. Am J Addict. (2020) 30:147–55. doi: 10.1111/ajad.13130
26. Thepthien, BO, Tinn, CS, and Sharma, R. Establishing the association between traditional tobacco, e-cigarette and dual use and mental health problems among high school students: results from a 2022 behavioral surveillance survey. Int J Ment Health Addict. (2023) 22:4148–68. doi: 10.1007/s11469-023-01109-8
27. Wilson, OWA, Bullen, C, Duffey, M, and Bopp, M. The association between vaping and health behaviors among undergraduate college students in the United States. J Am Coll Heal. (2022) 72:1360–4. doi: 10.1080/07448481.2022.2076097
28. You, MA, Choi, J, and Son, YJ. Associations of dual use of tobacco cigarettes and e-cigarettes, sleep duration, physical activity and depressive symptoms among middle-aged and older Korean adults. Nurs Open. (2023) 10:4071–82. doi: 10.1002/nop2.1667
29. Zhu, H, and Wu, M. A cross-sectional study on the relationship between electronic cigarette and combustible cigarette use with obstructive sleep apnea among U.S. adults: result from NHANES 2015–2018. Arch Public Health. (2023) 81:54. doi: 10.1186/s13690-023-01083-6
30. Liu, X, Yuan, Z, and Ji, Y. The association between electronic cigarettes, sleep duration, and the adverse cardiovascular outcomes: findings from behavioral risk factor surveillance system, 2020. Front Cardiovasc Med. (2022) 9:909383. doi: 10.3389/fcvm.2022.909383
31. Lim, DC, Najafi, A, Afifi, L, Bassetti, C, Buysse, DJ, Han, F, et al. The need to promote sleep health in public health agendas across the globe. Lancet Public Health. (2023) 8:e820–6. doi: 10.1016/S2468-2667(23)00182-2
32. Garbarino, S, Lanteri, P, Bragazzi, NL, Magnavita, N, and Scoditti, E. Role of sleep deprivation in immune-related disease risk and outcomes. Commun Biol. (2021) 4:1304. doi: 10.1038/s42003-021-02825-4
33. Schmitz, NCM, van der Werf, YD, and Lammers-van der Holst, HM. The importance of sleep and circadian rhythms for vaccination success and susceptibility to viral infections. Clocks. Sleep. (2022) 4:66–79. doi: 10.3390/clockssleep4010008
34. Irwin, MR, Carrillo, C, Sadeghi, N, Bjurstrom, MF, Breen, EC, and Olmstead, R. Prevention of incident and recurrent major depression in older adults with insomnia: A randomized clinical trial. JAMA Psychiatry. (2022) 79:33–41. doi: 10.1001/jamapsychiatry.2021.3422
35. Hillman, D, Mitchell, S, Streatfeild, J, Burns, C, Bruck, D, and Pezzullo, L. The economic cost of inadequate sleep. Sleep. (2018) 41:83. doi: 10.1093/sleep/zsy083
36. Sutherland, C, Smallwood, A, Wootten, T, and Redfern, N. Fatigue and its impact on performance and health. Br J Hosp Med. (2023) 84:1–8. doi: 10.12968/hmed.2022.0548
37. Zimmerman, ME, Benasi, G, Hale, C, Yeung, L-K, Cochran, J, Brickman, AM, et al. The effects of insufficient sleep and adequate sleep on cognitive function in healthy adults. Sleep Health. (2024) 10:229–36. doi: 10.1016/j.sleh.2023.11.011
38. Itani, O, Jike, M, Watanabe, N, and Kaneita, Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. (2017) 32:246–56. doi: 10.1016/j.sleep.2016.08.006
39. Larue, F, Tasbih, T, Ribeiro, PAB, Lavoie, KL, Dolan, E, and Bacon, SL. Immediate physiological effects of acute electronic cigarette use in humans: A systematic review and meta-analysis. Respir Med. (2021) 190:106684. doi: 10.1016/j.rmed.2021.106684
40. Léna, C, Popa, D, Grailhe, R, Escourrou, P, Changeux, J-P, and Adrien, J. β2-containing nicotinic receptors contribute to the Organization of Sleep and Regulate Putative Micro-Arousals in mice. J Neurosci. (2004) 24:5711–8. doi: 10.1523/JNEUROSCI.3882-03.2004
41. Feng, H, Qiao, Q-C, Luo, Q-F, Zhou, J-Y, Lei, F, Chen, Y, et al. Orexin neurons to sublaterodorsal tegmental nucleus pathway prevents sleep onset REM sleep-like behavior by relieving the REM sleep pressure. Research. (2024) 7:0355. doi: 10.34133/research.0355
42. Cohen, G, Han, Z-Y, Grailhe, R, Gallego, J, Gaultier, C, Changeux, J-P, et al. β2 nicotinic acetylcholine receptor subunit modulates protective responses to stress: A receptor basis for sleep-disordered breathing after nicotine exposure. Proc Natl Acad Sci. (2002) 99:13272–7. doi: 10.1073/pnas.192463599
43. Liu, T, Zeng, J, Zhao, X, Fu, R, Peng, L, Li, X, et al. Relationship between vascular aging and left ventricular geometry in patients with obstructive sleep apnea hypopnea syndrome-related hypertension. Sci Rep. (2025) 15:6191. doi: 10.1038/s41598-025-89964-4
44. Casasola, GG, Álvarez-Sala, JL, Marques, JA, Sánchez-Alarcos, JMF, Tashkin, DP, and Espinós, D. Cigarette smoking behavior and respiratory alterations during sleep in a healthy population. Sleep Breath. (2002) 6:019–24. doi: 10.1055/s-2002-23152
45. Mehari, A, Weir, NA, and Gillum, RF. Gender and the Association of Smoking with sleep quantity and quality in American adults. Women Health. (2014) 54:1–14. doi: 10.1080/03630242.2013.858097
46. Huang, C, Ding, Y, Xu, S, Chen, R, Jiang, T, Zeng, B, et al. Causal associations of self-reported walking pace with respiratory diseases: A Mendelian randomization analysis. Medicine. (2025) 104:e41746. doi: 10.1097/MD.0000000000041746
47. Gunge, D, Marganski, J, Advani, I, Boddu, S, Chen, YJE, Mehta, S, et al. Deleterious Association of Inhalant use on sleep quality during the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:3203. doi: 10.3390/ijerph182413203
Keywords: electronic cigarettes, insomnia, sleep duration, sleep issues, health problems
Citation: Sulthana H, Jan A, Verma A, Sah R, Mehta R, Ullah A, Rahim A, Alqudimat MR and Ullah A (2025) Impact of electronic cigarette use and sleep duration, sleep issues and insomnia: a systematic review and meta-analysis. Front. Public Health. 13:1662234. doi: 10.3389/fpubh.2025.1662234
Edited by:
Rishabh Kumar Kumar Rana, Shaheed Nirmal Mahto Medical College and Hospital, Dhanbad, IndiaReviewed by:
Apoorva Wasnik, Rajendra Institute of Medical Sciences, IndiaRatnesh Sinha, ESIC Medical College and Hospital, Ranchi, India
Copyright © 2025 Sulthana, Jan, Verma, Sah, Mehta, Ullah, Rahim, Alqudimat and Ullah. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Asmat Ullah, ZHJhc21hdHVsbGFoMDhAZ21haWwuY29t; Mohammad R. Alqudimat TW9oYW1tYWQuQWxxdWRpbWF0QGF1bS5lZHUua3c=
 Huma Sulthana1
Huma Sulthana1 Asif Jan
Asif Jan Amogh Verma
Amogh Verma Asmat Ullah
Asmat Ullah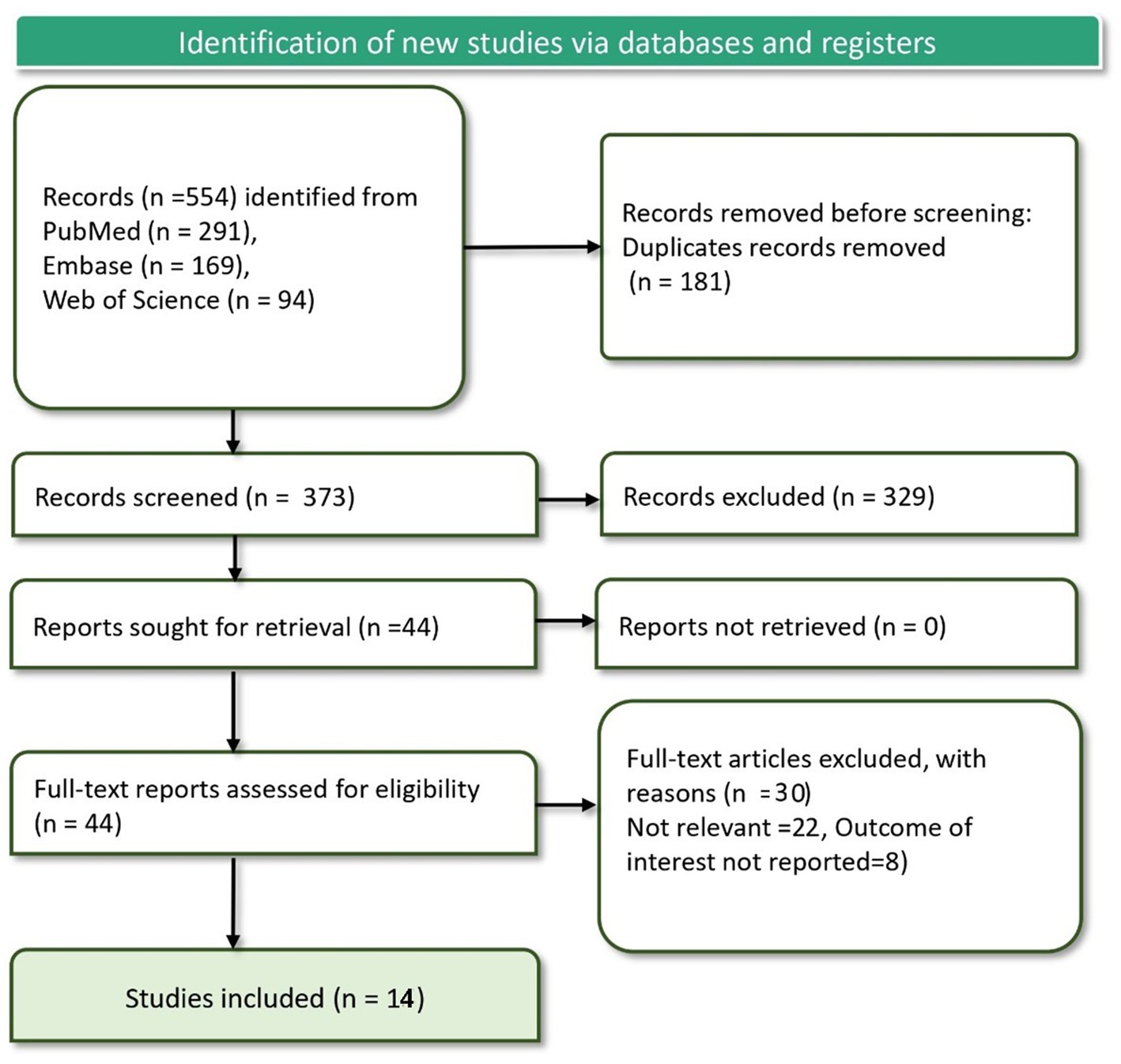
![Sensitivity analysis table and forest plot for a leave-one-out meta-analysis. Studies listed with omission, showing consistent p-values below 0.0001, Tau2 and Tau at zero, and I2 at zero percent. Odds ratios range from 1.362 to 1.430. The pooled odds ratio is 1.389 with a confidence interval of [1.240, 1.556]. The forest plot features red squares for individual studies and a black diamond for the pooled estimate, all aligned around the central reference line.](https://www.frontiersin.org/files/Articles/1662234/fpubh-13-1662234-HTML/image_m/fpubh-13-1662234-g003.jpg)