- Department of Pharmacy Practice, School of Pharmacy, International Medical University, Kuala Lumpur, Malaysia
Background: The diabetes patients’ adherence to prescription medication is 67.5%, which is lower than that of patients with any other medical conditions. Patients with low medication adherence are more likely to experience clinical complications, repeated hospitalizations, increased mortality, and increased healthcare costs, hence, education on disease and medication adherence is vital now. This study aimed to assess the level of medication adherence, medicine and information-seeking behaviour, and the effectiveness of online educational intervention in improving medication adherence and medicine and information-seeking behaviours among patients with diabetes in Klang Valley, Malaysia.
Methods: Individuals aged 12 years and above with a prior diagnosis of diabetes were identified and randomly divided into (control (n=183), and intervention groups (n = 206). Data about their medication adherence and information-seeking behaviour were obtained. As part of the online educational intervention, a month of daily general reminders to take their medications and educational materials about diabetes had provided to them via WhatsApp groups. After a month, the groups were reassessed, and the data were compared.
Results: The results showed that, at baseline, most of the respondents in the control (58.8% females and 53.08% males) and intervention (65.52% females and 85.12% males) groups had a low level of medication adherence. After a month of intervention, medication adherence was significantly improved in the intervention group (91.4% females and 71.28% males) compared to the control group (38.23% females and 44.44% males). At baseline, only 96 (52.45%) respondents in the control group and 110 (52.38%) in the intervention group preferred to read online educational materials to know more about their condition(s), it was improved after a month of intervention in the intervention group where 204 (99.02%) respondents prefer online materials, however no change in the control group response.
Conclusion: The study concludes that medication adherence and information-seeking behaviours among the study population have been significantly improved after a month of structured intervention. Medication adherence plays a crucial role in risk reduction strategies subsequently it improves the patient’s quality of life. Thus, well-planned more robust educational interventions on chronic diseases are warranted to improve the health outcomes of the patients.
1 Introduction
Diabetes is a chronic endocrine disease that affects the body’s ability to efficiently process energy from food resulting in an unusually high glucose level in the blood (1). Diabetes incidence has risen dramatically in almost every part of the world in recent decades, with 415 million people living with the disease worldwide (2). Over the last few decades, they have been an increased prevalence of people diagnosed with diabetes in Malaysia. According to the Malaysian National Health and Morbidity Survey (NHMS), this number has risen from about 11.2% in 2011 to more than 13.4% in 2015, it currently sits at around 18.3% in 2019. That roughly translates to more than 6 million Malaysians currently living with diabetes (3–5).
As the prevalence of diabetes increases, the global cost of care for patients increases especially after complications resulting from diabetes and hospital care (6, 7). From 2010 to 2030, the global economic cost of diabetes will increase by 100%, reaching 490 billion USD (8). Numerous studies have found that early treatment, as well as medication compliance and adherence, are effective in lowering treatment costs and complications associated with diabetes (7, 9).
According to the World Health Organisation (WHO), Medication adherence is defined as “the extent to which a person’s behaviour of taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a healthcare provider” (10). Adherence and compliance are synonymous but cannot be used interchangeably. Compliance is the degree to which a patient obeys the physician’s advice while adherence involves the collaboration between patient and physician to improve the patient’s health by optimising the physician’s medical opinion and patient’s values, ideals, lifestyle, and preference for care (11, 12). Other than complications resulting from non-adherence to disease medications, wastage of medicines is another issue so as disease progression, lower quality of life, and increased burden on medical resources (13, 14).
In chronic diseases such as diabetes, hypertension, and dyslipidaemia, poor adherence is often a common issue. In many Asian countries, the rate of medication non-adherence was reported to be around 40% - 80% (15), while in Malaysia non-adherence rate averages 50% (16). Adherence rates among patients with chronic illness are typically about 50% (17). According to a survey conducted in 2017-18, diabetes patients’ adherence to prescription medication is 68.5% lower than that of patients with many other conditions (18). Low adherence raises the risk of disease complications, causing the physician to prescribe higher doses to contain the disease, increasing the risk of drug side effects even further (19, 20). Patients with low medication adherence are more likely to experience clinical complications, repeated hospitalizations, increased mortality, and increased healthcare costs (21, 22).
According to many reports, diabetes knowledge in developing and underdeveloped countries is quite lacking, especially in Malaysia (3, 23, 24) the knowledge of diabetes can be improved by continuous training by health care practitioners. Given the aforementioned factor, it is clear that further research into Malaysians’ awareness of diabetes mellitus (DM) is needed. As a result, in this study, an attempt was made to assess and improve medication adherence among patients with diabetes in Klang Valley, Malaysia using online educational materials.
It is imperative to figure out whether patients are being adherent to their prescriptions to prevent long-term complications associated with the disease while also reducing healthcare costs and burden. Currently, adherence to chronic disease medications is not being addressed using online educational materials in Malaysia. This study will highlight the effectiveness of using online educational materials in improving the medication adherence of patients living with diabetes in Klang valley. Klang Valley, Malaysia was selected for this current study, as it is the most densely populated region in Malaysia with millions of multiracial populations and the highest number of patients with diabetes. The latest National Diabetes Registry Report 2020 stated 312,094 patients are living with diabetes in this region. The objectives of this present study were to assess the level of medication adherence among the diabetic population, to analyse the medicine and information-seeking behaviour, and to determine the effectiveness of online educational intervention in improving medication adherence and medicine and information-seeking behaviour among the patients with diabetes residing in Klang Valley, Malaysia.
2 Materials and methods
2.1 Study design, setting, and population
This was an interventional study in which the study participants were recruited using a snowball sampling technique, later they were grouped into control and intervention groups using a simple random sampling technique to provide educational intervention. The patients who have been previously diagnosed with any type of diabetes and residing in Klang Valley, Malaysia were selected. They were recruited between December 2020 and March 2021. The patients henceforth respondents, were all recruited through various online channels like Emails, Forums, WhatsApp groups, and referrals. Then the respondents were grouped into two, control and intervention groups. The control group was given the questionnaire to record their baseline responses and after 30 days their responses were once again collected. The intervention group was also administered the questionnaire to record their baseline responses. The respondents in the intervention group were then added to a WhatsApp group created for the sole purpose of providing reminders to take their drugs and they were also circulated with educational materials about diabetes daily. On the initial day of participation, the respondents were requested to fill in the questionnaire along with an informed consent form.
2.2 Inclusion and exclusion criteria of the subjects
The participant who has been clinically diagnosed with Type 1 DM or Type 2 DM (T2DM) or Gestational DM (GDM); and is at least 12 years old; of any gender and race; able to read, understand, and respond to the online questionnaire survey; has no hearing or visual impairment was included in this study. Participants with incomplete responses to the survey were excluded from the study.
2.3 Sample recruitment, randomisation, and intervention
2.3.1 Sample size calculation and sample recruitment
The sample size was calculated using an online Raosoft® sample size calculator with a 5% margin of error, 95% confidence interval, and 50% response distribution. The calculated sample size for the study was 380. The study instrument/questionnaire prepared and included in Google form was used in this study. After their enrollment into the study by answering the study questionnaire, WhatsApp groups were created to provide online intervention to the respondents.
During the initial few weeks of the study, we received very few responses, this may be due to a lack of reach of the study information to the target population. Later, we adopted the snowball sampling technique to recruit the sample size, it has shown very good responses and we have received many participants enrolled in this study.
Snowball sampling is a non-probability sampling technique commonly used when the samples have rare or difficult-to-reach characteristics. This type of sampling is also known as chain-referral sampling. Even though we have more diabetes populations in Malaysia especially in Klang Valley, reaching them during this pandemic period was difficult due to movement control, and the response to the direct online survey was poor. subjects/caregivers, HCPs provide referrals to recruit subjects required for this research study.
2.3.2 Randomisation
The recruited subjects are further grouped into control and intervention groups using a simple random sampling method. Research Randomizer online computer software (https://www.randomizer.org/) was used to divide/randomize the subjects for the control and intervention groups. Two sets of participants for control and intervention groups were planned. Each with approximately 200 participants, with numbers ranging from 1 to 400.
2.3.3 Intervention
In this study, the control group did not receive any intervention throughout the study period. However, their medication adherence level at baseline and final (after a month) was assessed. The intervention group received daily general reminders (WhatsApp messages) about using their medications as well as educational materials (leaflets and pamphlets) on diabetes. The online intervention was carried out for a month by providing daily reminders on their medication consumption/intake and sharing the diabetes educational materials through the created WhatsApp group. At the end of the fourth week, the study instrument/questionnaire was reimplemented, and data was collected using the completed questionnaire.
2.4 Study instrument and intervention materials
The study instrument consists of 3 sections to analyse the respondent’s demographic characteristics, level of medication adherence, and medicine and information-seeking behaviours.
2.4.1 Medication adherence and medicine and information-seeking behaviours questionnaire
In addition to the questions related to respondent’s demography, a structured validated medication adherence scale consists of 8 questions to analyse the respondents’ level of adherence to anti-diabetic medication(s) prepared and validated in English, and Malay language (25, 26), and 12 questions on medicine and information-seeking behaviour were used in this study. The study instrument prepared and validated in English and Malay versions, consisting of a total of 20 questions was used. Patients who scored 8 points on the medication adherence scale were considered to have high adherence, patients who scored >6 and <8 points were considered to have medium adherence, and those who scored ≤6 points were regarded as having low adherence. The description of the questionnaire items is presented in Table 1.
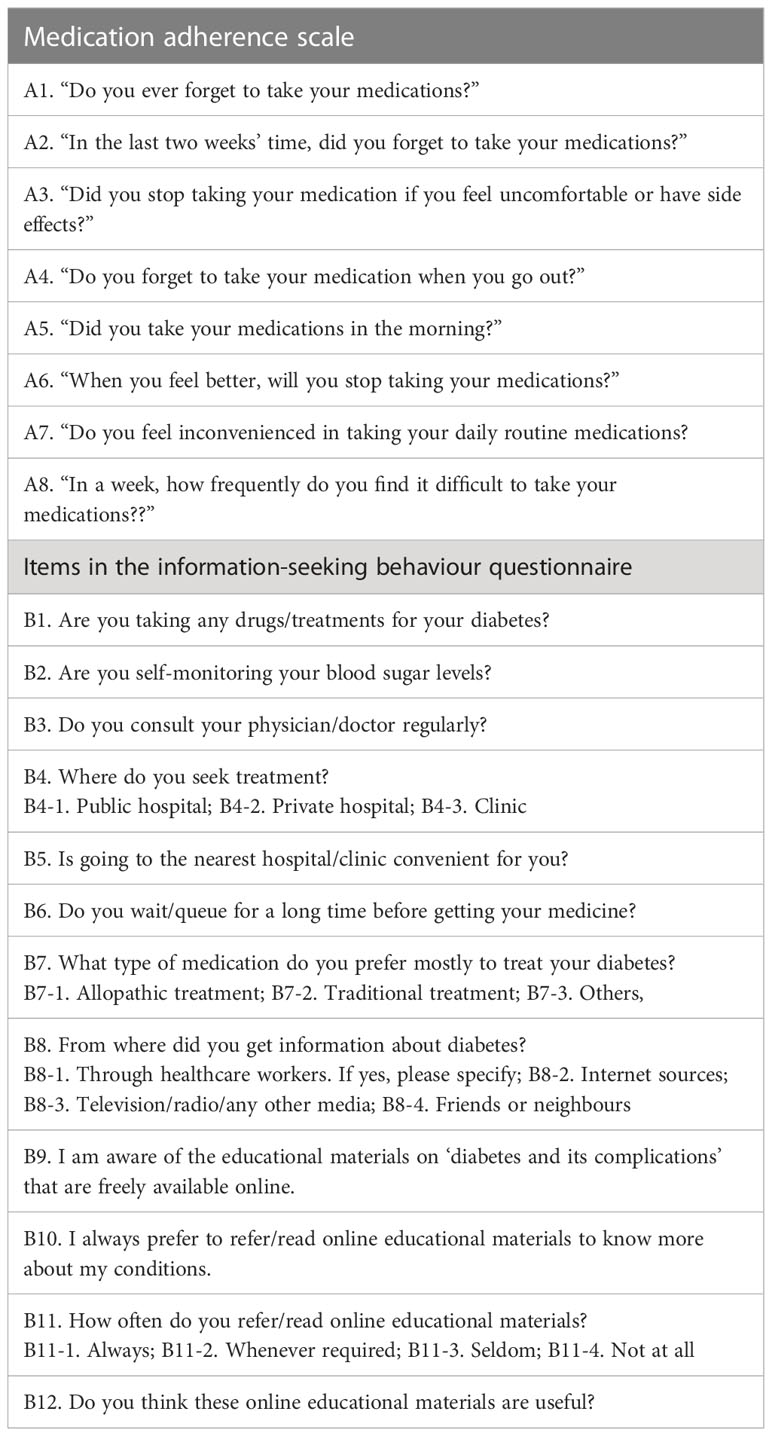
Table 1 Description of items of the medication adherence scale and, medicine and information-seeking behaviour questionnaire.
2.4.2 Educational materials on diabetes for intervention
For educational intervention on the knowledge of diabetes, electronically freely available leaflets or pamphlets/handouts emphasizing diabetes, diabetes complications, and the importance of medication adherence were circulated every day to the intervention group. The educational materials prepared by the Ministry of Health (MoH), Malaysia, Lembaga Farmasi, World Health Organisation (WHO), American Diabetes Association, European Association for the Study of Diabetes, International Diabetes Federation, and other reputed official bodies were used.
2.5 Outcome measures
The primary outcome of the study was an improvement in medication adherence and the secondary outcome was an improvement in medication and information-seeking behaviours among the respondents.
2.6 Ethical considerations
Approval for the present study was obtained from the International Medical University Joint Committee on Research and Ethics (IMU-JC) with the approval number MPP I/2020 (12). The information obtained during the data collection was strictly kept confidential. To maintain anonymity, a random code number was issued to each participant of this study while responding to the questionnaire. Informed written consent was obtained from every participant prior to the inception of the study. The study has not interfered with their current treatment(s) as the study instrument generally assesses their medication adherence, medication-seeking behaviour, and source of information to gain knowledge about the disease and treatment.
2.7 Statistical analysis
The collected data was analyzed for its appropriateness, and calculations were made on the collected data using Statistical Package for Social Sciences (SPSS) version 26.0. The change in medication adherence at baseline and the final (after a month of intervention) was analysed. Finally, the effectiveness of online educational intervention in improving medication adherence was analysed by comparing the control and intervention groups. We performed a χ2 test to explore the differences in the level of adherence to anti-diabetic medications among the public. We also performed an exploratory factor analysis after computing descriptive statistics, internal consistency coefficients, and intersubscale correlation analysis. A p-value < 0.05 was considered statistically significant.
3 Results
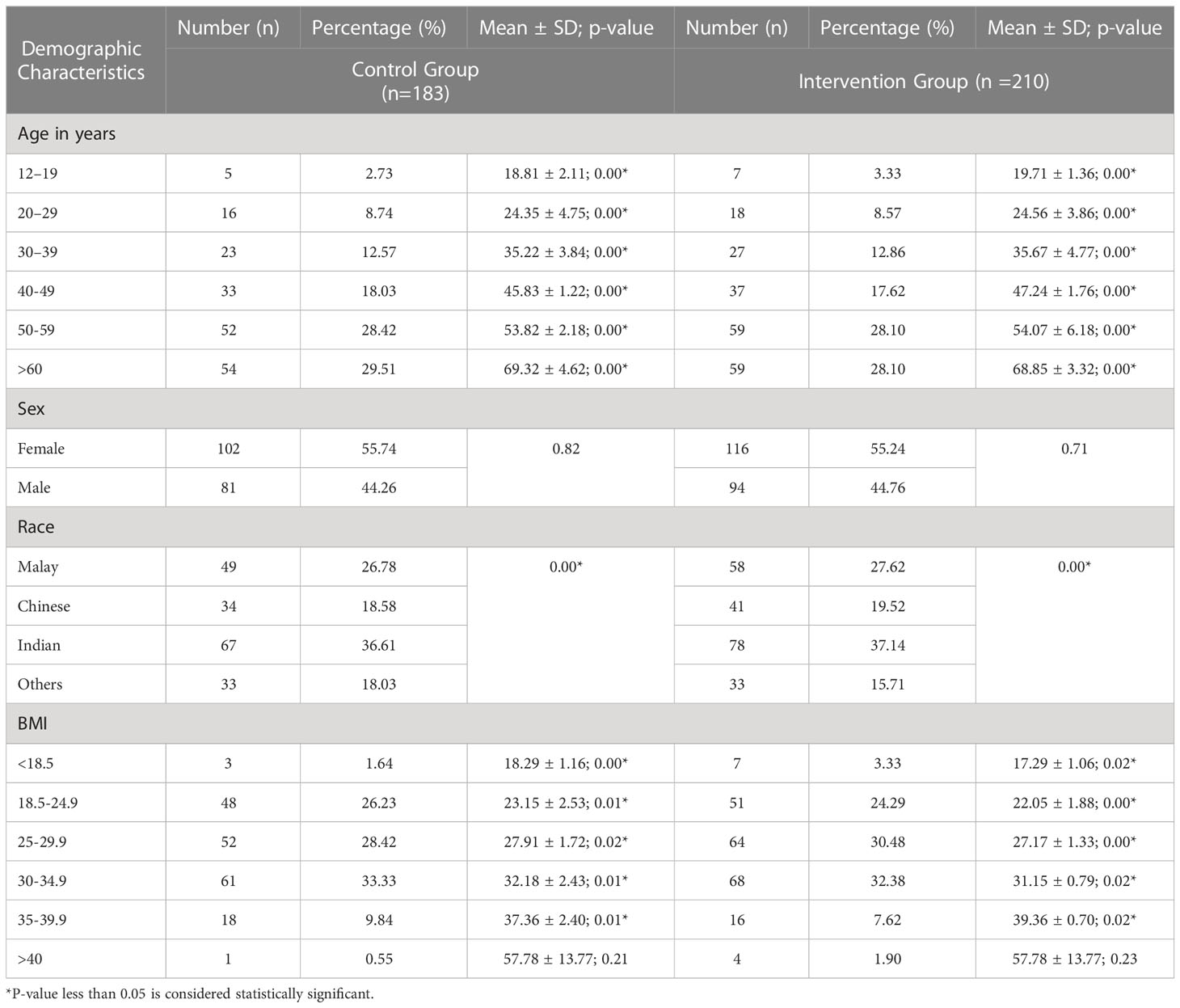
There were 400 subjects initially enrolled in this study, whereas 7 subjects were excluded due to incomplete data and hence only 393 participants were finally included. Out of 393 participants enrolled at baseline, 389 completed the follow-up and intervention in this study, and the response rate was 98.9%. One hundred and eighty-three respondents were included in the control group, and 210 respondents were in the intervention group using a simple random sampling technique. The majority of the respondents were between 50 and 59 years old, which was 28.42% in the control group and 28.10% in the intervention group, followed by those over 60 years old which was 29.51% in the control group and 28.10% in the intervention group respondents. The details of respondents’ demographic characteristics are presented in Table 2.
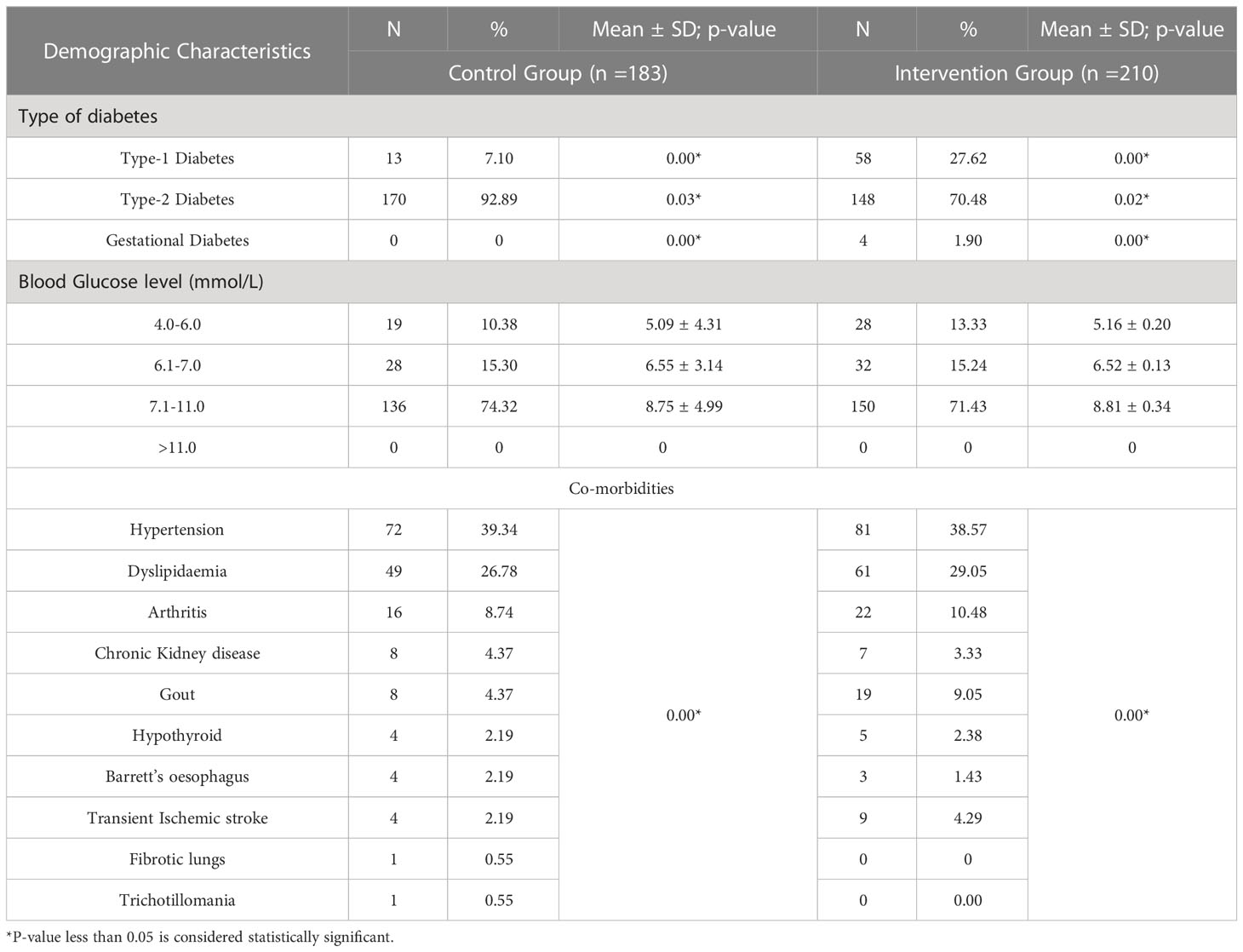
3.1 Diabetes and other comorbid conditions among the respondents
Most of the respondents in the control and intervention groups reported having T2DM, which was 92.89% and 70.48%, respectively, whereas 4 respondents were having gestational diabetes in the intervention group while no gestational diabetes was reported in the control group. For the measurement of random blood glucose levels, most of the respondents in the control group were in the range of 8.1 - 8.5 mmol/L (n=44, 21.90%,), and none of the respondents were in the range of 4.6 - 5.0 mmol/L. This trend can also be seen in the intervention group where the majority were in the range of 8.1- 8.5 mmol/L (n=46, 21.90%) and none was in the range of 4.6- 5.0 mmol/L. The respondents in both groups reported hypertension (control n= 72, 39.34%; intervention n=81, 38.57%) and dyslipidaemia (control n= 49, 26.78%; intervention n= 61; 29.05%) as the two most common comorbidity of diabetes. The results showed that there was a statistically significant difference (p= 0.011) between the age and BMI of the respondents which further highlights obesity as a common risk factor among them. The details are presented in Table 3.
3.2 Medication adherence among the respondents
The analysis showed that the majority of the respondents in both control and intervention groups forget to take their medications and had low adherence scores. However, the adherence level among the intervention groups had a significant improvement during the period of intervention. Table 4 presents how the respondents answered when asked about their medication adherence level at baseline and post-intervention period while in the Supplementary Table 1 further presents the significant changes in medication adherence levels among the diabetes population during different periods.
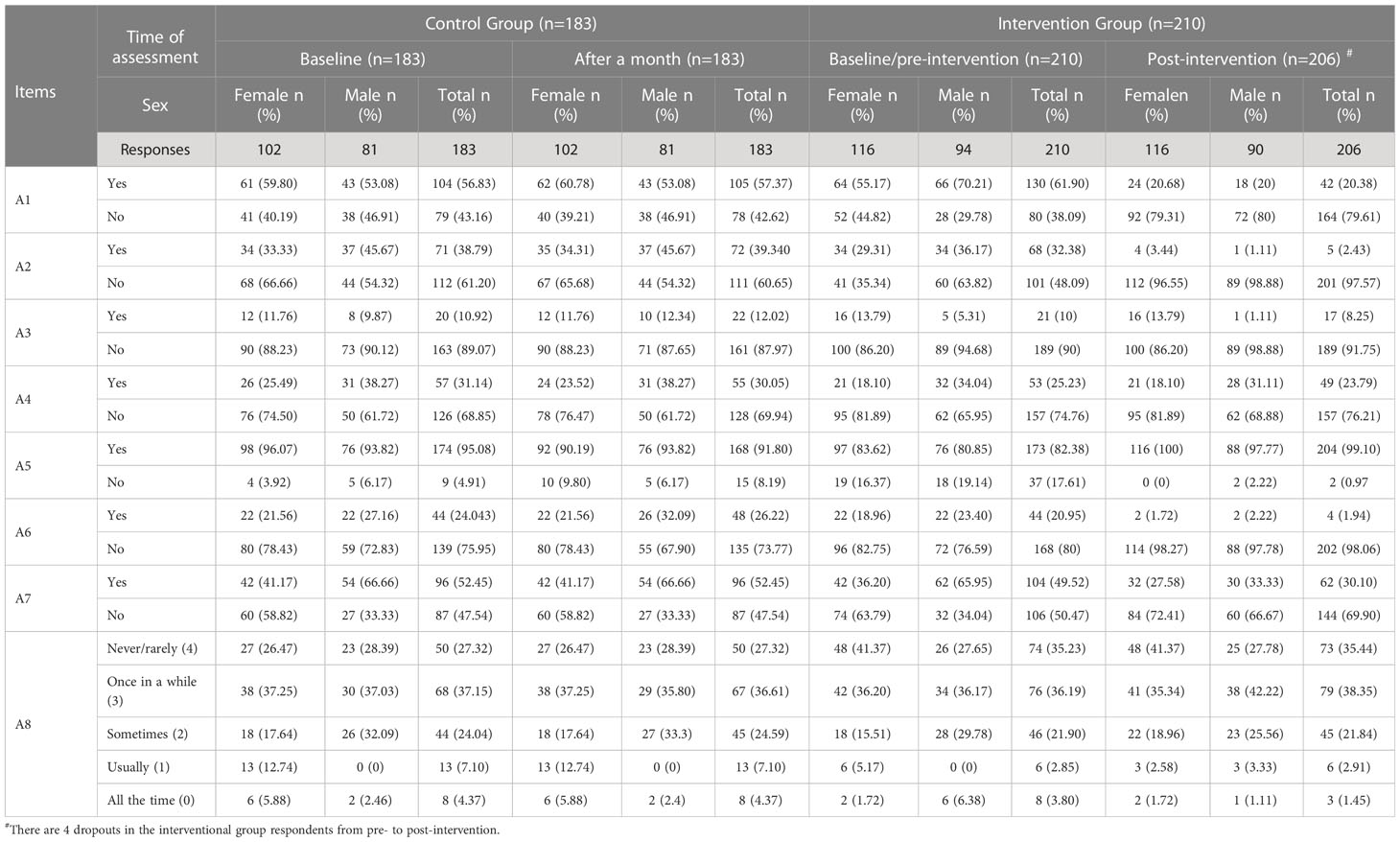
Table 4 Distribution of responses in medication adherence scale during baseline (pre-) and post-intervention (N=393).
When asked if they ever forget to take their medication, a majority in control and intervention groups said ‘Yes’ as they were forgotten to take their medications, which was 56.83% in control and 61.90% in intervention groups. When asked the same question after a month, 57.37% of control group respondents and only 20.38% of intervention group respondents said ‘Yes’ they were sometimes forgotten to take their medication.
When the respondents were asked if they have ever cut back or stopped taking their medications because they felt uncomfortable or had side effects when they took them, 10.92% of the control group respondents and 10% of the intervention group respondents said ‘Yes’. When asked the same question after a month, 12.02% of the control group respondents and 8.25% of intervention respondents said ‘Yes’.
When asked if they took their medication in the morning, the majority of the respondents in the control and intervention groups said ‘Yes’, which was 95.08% and 82.38%, respectively. When asked the same question after a month, 91.80% of the control group respondents and 99.10% of the intervention groups said ‘Yes’.
The respondents were asked at the end of the medication adherence section if they have any difficulty taking their medications. In the control group, 50 (27.32%) respondents said never had any difficulty in taking their medications, 68 (37.15%) said once in a while, 44 (24.04%) sometimes, 13 (7.10%) usually, 8 (4.37%) all the time had difficulty in taking their medications. While the intervention group, 74 (35.23%) respondents said they never had any difficulty in taking their medications, 76 (36.19%) once in a while, 46 (21.90%) sometimes, 6 (2.85%) usually, and 8 (3.80%) all the time find difficulty in taking their medications. Then after a month, they were reassessed and there were not many changes in the control group’s responses, however, the intervention group showed good improvement, in which 73 (35.44%) respondents said they never/rarely faced difficulty in taking their medications, 79 (36.35%) said once in a while, 45 (21.85%) sometimes, 6 (2.91%) usually and only 3 (1.45%) all the time faced difficulty in taking their medications.
The initial assessment of medication adherence showed that most of the respondents in the control (58.8% females and 53.08% males) and intervention (65.52% females and 85.12% males) groups had a low level of medication adherence while only a few had a moderate level of adherence in both control (41.17% females and 46.91% males) and intervention groups (34.48% females and14.89% males). Then after a month of intervention, the results showed that there was a significant increase in medication adherence in the intervention group (91.4% females and 71.28% males) compared to the control group (38.23% females and 44.44% males). Around 110 patients who scored 8 points on the medication adherence scale were considered to have high adherence. The details are presented in the Supplementary Table 1.
3.3 Medicine and information-seeking behaviour among the respondents
The study respondents were analysed for their medicine and information-seeking behaviour. Most of the respondents in this study seek treatment at the public hospital (n =191) followed by the private hospital (n =137) then the clinic (n =65) in all groups and most of them reported they had little wait time before receiving their medications. When asked about where they got information about diabetes, most reported from their healthcare workers, and internet sources, and few responded to getting information from their friends, neighbours, and media. The details are presented in the Supplementary Table 2.
During the baseline of the study, when the respondents were asked if they were aware of the educational materials containing information on diabetes being available online, about half of the control group (n=79, 43.16%) and a majority of the intervention group (n =173, 82.38%) respondents said “Yes”. When asked if they prefer to read online educational materials to know more about their condition, a majority of the respondents in the control group (n=96, 52.45%) and intervention group (n =110, 52.38%) responded “Yes”. When asked the same set of questions after a month, no changes were observed in the control group, while the intervention group showed remarkable improvement in the awareness of educational materials and their preference to read online educational materials (n= 202, 98.05%, and n= 204, 99.02%, respectively).
Then when they were asked how often they read or refer to online materials, most of the respondents in the control group said “whenever required” both at baseline (n= 79, 43.16%) and after a month (n =79, 43.16%), while in the intervention group, “not at all” (n=48, 22.85%) response being the most and “whenever required” (n =9, 46.66%) the lowest, but after a month of intervention, most of the respondents said, “whenever required” (n= 96, 46.60%). Finally, the respondents were asked if they think online educational materials were useful, majority of the control group respondents said “Yes” (n = 142, 77.59%) both at baseline and after a month. However, among the intervention group, 172 respondents said “Yes” (81.90%) at baseline, whereas 202 (98.05%) respondents said “Yes” after a month of intervention.
3.4 Correlation analysis of the responses
Using Two-way Analysis of Variance (ANOVA), a correlation analysis was performed for the responses of the control and intervention groups on the difference in medication adherence level, and medication and information-seeking behaviour at baseline and post-intervention. The correlation was observed significant between control and intervention groups at the 0.01 level (2-tailed), and a significant correlation was observed between the baseline and post-intervention responses at the 0.05 level (2-tailed). Although some responses showed no correlation between them when the responses were analysed for correlation, there was no relationship between them. There was no correlation between the responses for “Did you take your medications yesterday?” and “When you feel like your health condition is under control, do you sometimes stop taking your medications?”. However, the trend shows that most of the responses were significant, especially at the 0.01 level (2-tailed).
4 Discussion
This study aimed to explore the effectiveness of online educational intervention in improving medication adherence among patients with diabetes in Klang Valley, Malaysia. To our knowledge, this is the first study to be done in Southeast Asia that investigates the effectiveness of online educational intervention in improving medication adherence among patients with diabetes. Not only does it include the analysis of medication adherence, but it also does analysis of medicine and information-seeking behaviour of the diabetes patient, in addition to a daily reminder for their medication consumption, an online educational intervention was provided for one month. Whereas in previous studies conducted to analyse medication adherence and medication information-seeking behaviour, the intervention was mostly an hour lecture, workshop conducted within a day, or briefing session before they are assessed.
4.1 Demographic characteristics
According to the NHMS, the prevalence of diabetes in adults older than 60 years in Malaysia is about 30%, and 33.8% in adults between the age range of 50 to 59 (27). Thus, the respondents in this study are a fair representation of the country’s population. An increase in age and BMI will increase the chances of T2DM among the older population. Furthermore, there were more female respondents (55%) in this study than males. Females take a more active role concerning their health than males, according to research (27).
4.2 Adherence to diabetes medications
In this study, we investigated the effectiveness of online educational intervention in improving medication adherence among patients with diabetes living in Klang Valley, Malaysia. At baseline, both the control (female 58.60%, male 53.08%) and intervention (female 65.52%, male 85.12%) groups had a very low level of adherence. We found that the intervention group’s adherence level has increased significantly when compared with their baseline data. In a previous study measuring the adherence level among self-paying and subsidized Malaysians, around 50% of them had a low level of adherence and their adherence level only increased after they were given drug counselling (28, 29). This further purports the low adherence level among Malaysians and improvement in the adherence level only when some form of intervention is given.
Age and gender were found to be important predictors of diabetes medication adherence (30, 31). This suggests that patients with diabetes in their later years were more compliant with their drugs. Another study was conducted to identify the effectiveness of diabetes medication therapy adherence clinic in improving adherence in patients having T2DM in Malaysia. It found that age, medication knowledge, and T2DM with comorbidities were predictors of medication adherence. It further states that the older the age of the diabetes patient the more adherent they are to their medications (32).
Male subjects were found to be more adherent to anti-diabetic drugs than females among the study respondents. However, patient characteristics related to nonadherence have been shown to differ. In general, ethnicity and gender are not reliably linked to patient adherence (32). Furthermore, in our study, there was no significant relationship between the various aspects of compliance and demographic characteristics. This is similar to an earlier study that found no important association between different aspects of patient compliance and sociodemographic characteristics (33).
The intervention given to the respondents comprises educational materials sourced from reputed agencies for a period of one month along with daily reminders to take their medications. The analysis of the medication adherence of the respondents after being given the intervention further revealed that using online educational materials to educate the respondents about their medical condition and how to take their medications properly will result in a better adherence level. A month after the respondents were given the intervention (online educational materials and daily reminders to take their medications), they were reassessed which showed positive results and improved adherence levels.
In improving the adherence level of patients in Malaysia, healthcare providers should conduct periodical assessments of their patients using the medication adherence scale as a self-report and screening tool and encourage their patients on reading educational materials about their medical condition. Proving that indeed, the intervention provided to the current study participants was found to be effective. This result can be also seen in the pharmacist-led study carried out in Malaysia, the patients in this study had poor glycaemic control at baseline but by the end of the study, they reported having a mean HbA1c reduction of 1.73%. The patient’s medication adherence level improved significantly from medium adherence of 7.00 (SD=0.61) to high adherence of 10.84 (SD=0.10) (p<0.001), and everyone reported high adherence after the intervention (32). Meanwhile, our study reported that the respondent’s adherence levels improved significantly from low adherence (female 65.52% and male 85.12%) (p=0.02) to medium or moderate adherence (female 91.4% and male 71.28%) (p=0.01)
This study shows there is no relationship between where healthcare is given and medication adherence. Despite substantial subsidisation of the cost of drugs in public health care settings in Malaysia, poor medication adherence is still prevalent. In a previous study, more than half of the patients with diabetes and hypertension treated in public hospitals and clinics had low adherence levels (28, 30). In this study, more than half of the respondents responded that they go to public hospitals for healthcare.
4.3 Medicine and information-seeking behaviour
According to a previous study conducted in Malaysia, medication-seeking behaviour among Malaysians are particularly low, most Malaysians will only seek medication based on the severity of their illness. The study also noted that the local population prefers to use alternative or traditional treatments for minor ailments like cough or fever and will only seek a physician if the disease is very severe like diabetes or hypertension (29). In the current study, not only did we find out that the medicine information-seeking behaviour among the respondents was poor we also found that a moderate amount of people preferred traditional medicine to other forms of treatment while the majority preferred both (allopathic and traditional treatment), this may be due to different cultural beliefs about disease.
In Malaysia, there has been a steady increase in healthcare facilities and easier access to medicines. According to a survey on medicine use behaviour, most Malaysians (84%) will consult physicians while only 11% will self-medicate (34, 35). The most common reason for the rise in the practice of self-medication among many Malaysians is the easy access and convenience to medicines. Furthermore, in developing countries, people’s decisions about seeking medical help may be influenced by a lack of access to healthcare facilities and common drug shortages (34). However, seeking a physician is not affected by age group but by the perceived severity of illness (25).. This present study showed that consulting the physician or using medicine is not influenced by age group, gender, or race. This finding could be due to the ease of access and availability of healthcare and medicines in Malaysia. It also showed that the majority of the respondents listen and ask their physicians for advice about their medical conditions. In comparison to the previous study, due to the high morbidity rate among the elderly (65 years and above), visiting the healthcare system to obtain prescription medicines is common (36). Young people, on the other hand, are more likely to take care of themselves without needing to see a doctor by purchasing non-prescription medications (37, 38). Obtaining prescription drugs, on the other hand, was affected by people’s perceptions of their health status rather than their age (39–41).
There was a significant improvement in the number of respondents who were aware of educational materials, who know how to access this information, and also who think they are useful for their medical condition compared to the control group. This is because some of the educational materials contain pictures, easy-to-read words, and well-explained information about diabetes and the importance of being adherent to their medication.
As the study was conducted over one month with daily educational materials and medication reminders, the patients may find it beneficial to receive daily reminders. The study encourages the healthcare fraternity and the government to initiate steps to provide online education to the general public on the most common disease conditions of the country with daily reminders on their medication. Software can be developed for this purpose instead of involving HCPs to disseminate the information to avoid workload burden to the existing staff.
This study evident that pharmacist-led online educational intervention is effective in improving medication adherence among patients with diabetes, irrespective of age, sex, race, and comorbid conditions almost all the respondents showed improvement in medication adherence. Moreover, the daily reminders helped them a lot to consume their routine medication on time which has certainly improved their compliance with their medication. The medicine and information-seeking behaviours were initially low, whereas it was good at the final stage after the intervention, which further evident that appropriate educational intervention or program is necessary to seek reliable resources to enlighten the knowledge of disease(s). Patients with improved medication adherence, medicine, and information-seeking behaviour will reduce the morbidity and mortality associated with the disease and also improve their quality of life. Hence, this study strongly suggests the government, ministry of health, universities, and educational institutions conduct more such studies on diabetes and medication adherence periodically to improve the well-being of the people living with this deadly condition.
4.4 Limitations
In this study, the control and intervention groups are not balanced as the respondents were selected online by simple random sampling computer software, thus showing a higher percentage of type 1 diabetes mellitus patients in the intervention group. Potential inaccuracies in patient answers, which are inherent in any self-reported survey, particularly in chronic disease conditions, were one of the study’s limitations. Patients with DM for varying periods (a few months to years) were included in this study, and their perceptions and responses to questions about adherence may differ. Since diabetes patients also have other comorbidities that necessitate the use of other drugs, generalising this study’s adherence level in measuring overall adherence may not be accepted and should be further evaluated. In this study, the reasons for seeking medicines and the types of medications were not examined. As a result, the severity of the disease could affect people’s decision to seek medical help. In the current study, the respondent’s level of education, profession, or employment status were not collected, and these variables may have a direct influence on medication adherence, medicine and information-seeking behaviours. Finally, this study was restricted to a snowball sampling method in the Klang Valley; thus, the findings cannot be applied to all Malaysians.
5 Conclusions
A low level of medication adherence, medicine and information-seeking behaviours are commonly seen among the patients with diabetes in this region. The pharmacist-led education intervention has shown effectiveness in improving medication adherence and information-seeking behaviour. A well-structured periodical intervention provided by the government will be more beneficial to patients with diabetes. As the world is moving towards technology-oriented, providing automated electronic reminders to patients with chronic medical conditions will benefit the patients’ community to cope with their medication regimen.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
This study proposal was reviewed and approved by International Medical University Joint Committee on Research and Ethics (IMU-JC). The patients/participants provided their written informed consent to participate in this study.
Author contributions
All listed authors meet the requirements for authorship. PS led the clinical part of this study. EA, PS, and PI contributed to participants recruitment, sample collection, and the collection of data. PS, and PI contributed to the supervision of the study. EA conducted data extraction and statistical analysis. EA and PS conducted data analyses, results interpretation, and drafted the manuscript. EA, PS, and PI critically revised and commented on the first and subsequent drafts. PS was the principal investigator for this study and fundraiser, who conceptualized and designed this study. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the International Medical University Joint Committee on Research and Ethics (IMU-JC), grant number MPP I/2020 (12), and “The APC was funded by IMU’s Institute for Research, Development and Innovation (IRDI).
Acknowledgments
The authors thank the management of the International Medical University for providing the necessary support and approval to carry out this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcdhc.2023.1132489/full#supplementary-material
References
1. Cole JB, Florez JC. Genetics of diabetes mellitus and diabetes complications. Nat. Rev. Nephrol. (2020) 16(7):377–90. doi: 10.1038/s41581-020-0278-5
2. Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: a review of current evidence. Diabetologia.- (2019) 62(1):3–16. doi: 10.1007/s00125-018-4711-2
3. Hussein Z, Taher SW, Gilcharan Singh HK, Chee Siew Swee W. Diabetes care in Malaysia: Problems, new models, and solutions. Ann. Glob Health (2015) 81(6):851–62. doi: 10.1016/j.aogh.2015.12.016
4. Abdullah N, Murad NAA, Attia J, Oldmeadow C, Kamaruddin MA, Jalal NA, et al. Differing contributions of classical risk factors to type 2 diabetes in multi-ethnic Malaysian populations. Int. J. Environ. Res. Public Health (2018) 15(12):2813. doi: 10.3390/ijerph15122813
5. Akhtar S, Nasir JA, Ali A, Asghar M, Majeed R, Sarwar A. Prevalence of type-2 diabetes and prediabetes in Malaysia: A systematic review and meta-analysis. PloS One (2022) 17(1):e0263139. doi: 10.1371/journal.pone.0263139
6. Dhatariya K, Corsino L, Umpierrez GE. Management of diabetes and hyperglycemia in hospitalized patients. In: Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, et al, editors. Endotext. (South Dartmouth (MA): MDText.com, Inc) (2020).
7. Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci. Rep. (2020) 10(1):14790. doi: 10.1038/s41598-020-71908-9
8. Bommer C, Sagalova V, Heesemann E, Manne-Goehler J, Atun R, Bärnighausen T, et al. Global economic burden of diabetes in adults: Projections from 2015 to 2030. Diabetes Care (2018) 41(5):963–70. doi: 10.2337/dc17-1962
9. Kao CC, Hsieh HM, Lee DY, Hsieh KP, Sheu SJ. Importance of medication adherence in treatment needed diabetic retinopathy. Sci. Rep. (2021) 11(1):19100. doi: 10.1038/s41598-021-98488-6
10. Aravindakshan R, Abraham SB, Aiyappan R. Medication adherence to oral hypoglycemic drugs among individuals with type 2 diabetes mellitus - a community study. Indian J. Community Med. (2021) 46(3):503–7. doi: 10.4103/ijcm.IJCM_985_20
11. Fernandez-Lazaro CI, García-González JM, Adams DP, Fernandez-Lazaro D, Mielgo-Ayuso J, Caballero-Garcia A, et al. Adherence to treatment and related factors among patients with chronic conditions in primary care: a cross-sectional study. BMC Fam Pract. (2019) 20(1):132. doi: 10.1186/s12875-019-1019-3
12. Zhang R, Lu X, Wu W, Shang X. Why do patients follow physicians’ advice? the influence of patients’ regulatory focus on adherence: an empirical study in China. BMC Health Serv. Res. (2019) 19(1):301. doi: 10.1186/s12913-019-4127-9
13. Rathish D, Hemachandra R, Premadasa T, Ramanayake S, Rasangika C, Roshiban R, et al. Comparison of medication adherence between type 2 diabetes mellitus patients who pay for their medications and those who receive it free: a rural Asian experience. J. Health Popul Nutr. (2019) 38(1):4. doi: 10.1186/s41043-019-0161-9
14. Nakajima R, Watanabe F, Kamei M. Factors associated with medication non-adherence among patients with lifestyle-related non-communicable diseases. Pharm. (Basel). (2021) 9(2):90. doi: 10.3390/pharmacy9020090
15. Ganasegeran K, Rashid A. The prevalence of medication nonadherence in post-myocardial infarction survivors and its perceived barriers and psychological correlates: a cross-sectional study in a cardiac health facility in Malaysia. Patient Prefer Adherence. (2017) 11:1975–85. doi: 10.2147/PPA.S151053
16. Mahmood S, Jalal Z, Hadi MA, Khan TM, Haque MS, Shah KU. Prevalence of non-adherence to antihypertensive medication in Asia: a systematic review and meta-analysis. Int. J. Clin. Pharm. (2021) 43(3):486–501. doi: 10.1007/s11096-021-01236-z
17. Ibrahim KM, Schommer JC, Morisky DE, Rodriguez R, Gaither C, Snyder M. The association between medication experiences and beliefs and low medication adherence in patients with chronic disease from two different societies: The USA and the sultanate of Oman. Pharm. (Basel). (2021) 9(1):31. doi: 10.3390/pharmacy9010031
18. Alshehri KA, Altuwaylie TM, Alqhtani A, Albawab AA, Almalki AH. Type 2 diabetic patients adherence towards their medications. Cureus.- (2020) 12(2):e6932. doi: 10.7759/cureus.6932
19. Yadav RK, Kaphle HP, Yadav DK, Marahatta SB, Shah NP, Baral S, et al. Health related quality of life and associated factors with medication adherence among tuberculosis patients in selected districts of gandaki province of Nepal. J. Clin. Tuberc Other Mycobact Dis. (2021) 23:100235. doi: 10.1016/j.jctube.2021.100235
20. Shah NB, Haydek J, Slaughter J, Ashton JR, Zuckerman AD, Wong R, et al. Risk factors for medication nonadherence to self-injectable biologic therapy in adult patients with inflammatory bowel disease. Inflammation Bowel Dis. (2020) 26(2):314–20. doi: 10.1093/ibd/izz253
21. Cutler RL, Fernandez-Llimos F, Frommer M, Benrimoj C, Garcia-Cardenas V. Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open (2018) 8(1):e016982. doi: 10.1136/bmjopen-2017-016982
22. De Avila JL, Meltzer DO, Zhang JX. Prevalence and persistence of cost-related medication nonadherence among Medicare beneficiaries at high risk of hospitalization. JAMA Netw. Open (2021) 4(3):e210498. doi: 10.1001/jamanetworkopen.2021.0498
23. Chinnappan S, Sivanandy P, Sagaran R, Molugulu N. Assessment of knowledge of diabetes mellitus in the urban areas of klang district, Malaysia. Pharm. (Basel). (2017) 5(1):11. doi: 10.3390/pharmacy5010011
24. Humaira AL, Mohd RAH, Noor AZA. Awareness of diabetes mellitus among public attending the primary health centres in Malaysia. J. Qual Meas Anal. (2018) 14:11–23.
25. Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J. Clin. Hypertens. (Greenwich). (2008) 10(5):348–54. doi: 10.1111/j.1751-7176.2008.07572.x
26. Al-Qazaz HKH, Hassali MA, Shafie AA, Sulaiman SA, Sundram S, Morisky DE. The eight-item morisky medication adherence scale MMAS: translation and validation of the Malaysian version. Diabetes Res. Clin. Pract. (2010) 90(2):216–21. doi: 10.1016/j.diabres.2010.08.012
27. Chandran A, Abdullah MN, Abdul F. National diabetes registry report 2013 – 2019. Malaysia: Disease Control Division, Ministry of Health (2021). Available at: https://www.moh.gov.my/moh/resources/Penerbitan/Rujukan/NCD/Diabetes/National_Diabetes_Registry_Report_2013-2019_26082021.pdf.
28. Aziz H, Hatah E, Makmor-Bakry M, Islahudin F, Ahmad Hamdi N, Mok Pok Wan I. A comparison of medication adherence between subsidized and self-paying patients in Malaysia. Malays Fam Physician. (2018) 13(2):2–9.
29. Aziz H, Hatah E, Makmor-Bakry M, Islahudin F, Ahmad Hamdi N, Mok Pok Wan I. Qualitative exploration of the modifiable factors for medication adherence among subsidised and self-paying patients in Malaysia. BMC Health Serv. Res. (2018) 18(1):605. doi: 10.1186/s12913-018-3417-y
30. Ranjbaran S, Shojaeizadeh D, Dehdari T, Yaseri M, Shakibazadeh E. Determinants of medication adherence among Iranian patients with type 2 diabetes: An application of health action process approach. Heliyon.- (2020) 6(7):e04442. doi: 10.1016/j.heliyon.2020.e04442
31. Demoz GT, Wahdey S, Bahrey D, Kahsay H, Woldu G, Niriayo YL, et al. Predictors of poor adherence to antidiabetic therapy in patients with type 2 diabetes: a cross-sectional study insight from Ethiopia. Diabetol. Metab. Syndr. (2020) 12:62. doi: 10.1186/s13098-020-00567-7
32. Alison C, Anselm S. The effectiveness of diabetes medication therapy adherence clinic to improve glycaemic control among patients with type 2 diabetes mellitus: a randomised controlled trial. Med. J. Malaysia. (2020) 75(3):246–53.
33. Xie Z, Liu K, Or C, Chen J, Yan M, Wang H. An examination of the socio-demographic correlates of patient adherence to self-management behaviors and the mediating roles of health attitudes and self-efficacy among patients with coexisting type 2 diabetes and hypertension. BMC Public Health (2020) 20(1):1227. doi: 10.1186/s12889-020-09274-4
34. Dawood OT, Hassali MA, Saleem F, Ibrahim IR, Abdulameer AH, Jasim HH. Assessment of health seeking behaviour and self-medication among general public in the state of penang, Malaysia. Pharm. Pract. (Granada). (2017) 15(3):991. doi: 10.18549/PharmPract.2017.03.991
35. Dawood OT, Hassali MA, Saleem F. A qualitative study exploring medicines use pattern and practice among general public in Malaysia. Pharm. Pract. (Granada). (2016) 14(2):740. doi: 10.18549/PharmPract.2016.02.740
36. Khezrian M, McNeil CJ, Murray AD, Myint PK. An overview of prevalence, determinants and health outcomes of polypharmacy. Ther. Adv. Drug Saf. (2020) 11:2042098620933741. doi: 10.1177/2042098620933741
37. Guirguis A, Chiappini S, Corkery JM, Schifano F. Misuse of prescription and over-the-counter drugs to obtain illicit highs: How pharmacists can prevent abuse. Pharm. J. (2020) 305(7943). doi: 10.1211/PJ.2020.20208538
38. Tesfamariam S, Anand IS, Kaleab G, Berhane S, Woldai B, Habte E, et al. Self-medication with over the counter drugs, prevalence of risky practice and its associated factors in pharmacy outlets of Asmara, Eritrea. BMC Public Health (2019) 19(1):159. doi: 10.1186/s12889-019-6470-5
39. Mortazavi SS, Shati M, Khankeh HR, Ahmadi F, Mehravaran S, Malakouti SK. Self-medication among the elderly in Iran: a content analysis study. BMC Geriatr. (2017) 17(1):198. doi: 10.1186/s12877-017-0596-z
40. Shah K, Halder S, Haider SS. Assessment of knowledge, perception, and awareness about self-medication practices among university students in Nepal. Heliyon.- (2021) 7(1):e05976. doi: 10.1016/j.heliyon.2021.e05976
Keywords: diabetes, education, awareness, hyperglycaemia, medication adherence, information-seeking behavior
Citation: Atolagbe ET, Sivanandy P and Ingle PV (2023) Effectiveness of educational intervention in improving medication adherence among patients with diabetes in Klang Valley, Malaysia. Front. Clin. Diabetes Healthc. 4:1132489. doi: 10.3389/fcdhc.2023.1132489
Received: 27 December 2022; Accepted: 21 February 2023;
Published: 13 March 2023.
Edited by:
Muhammad Shahzad Aslam, Xiamen University, Malaysia, MalaysiaReviewed by:
Mahendran Sekar, Monash University MalaysiaHuai Heng Loh, Universiti Malaysia Sarawak, Malaysia
Karunrat Tewthanom, Silpakorn University, Thailand
Copyright © 2023 Atolagbe, Sivanandy and Ingle. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Palanisamy Sivanandy, UGFsYW5pc2FteVNpdmFuYW5keUBpbXUuZWR1Lm15
 Emmanuel Timilehin Atolagbe
Emmanuel Timilehin Atolagbe Palanisamy Sivanandy
Palanisamy Sivanandy