- 1Medical College, Yangzhou University, Yangzhou, Jiangsu, China
- 2Department of Orthopedics, Affiliated Hospital of Yangzhou University, Yangzhou University, Yangzhou, Jiangsu, China
Background: The Chinese government’s long-term healthcare strategy and the short-term pandemic of COVID-19 have highlighted the urgent need for clinically skilled and multidisciplinary-orientated healthcare professionals to address future healthcare challenges.
Objective: This systematic review analyzes the current state and future directions of medical education in China, drawing on various studies to provide insights into optimizing medical training and aligning it with national healthcare needs.
Methods: A systematic review of existing literature on Chinese medical education reforms was conducted. The analysis focused on key aspects such as medical education systems, regional disparities, curriculum development, and management structures. Comparisons with international medical education models were also included to identify potential areas for improvement.
Discussion: China’s medical education system operates through multiple parallel mechanisms, with ongoing efforts to enhance regional coordination, diversify curricula, and improve collaboration between educational institutions and healthcare providers. Comparisons with foreign models suggest several key reforms: establishing a unified medical degree system with clear objectives, prioritizing general practitioners and primary care training, integrating medical humanities and public health education, and strengthening the governance of medical schools and affiliated hospitals.
Conclusion: This systematic review provides a comprehensive overview of the evolving landscape of medical education in China, identifies challenges and opportunities, and proposes targeted reforms. These insights may serve as a reference for policymakers and educators working to enhance medical training and healthcare delivery in China.
Introduction
In recent decades, Chinese government has never stopped the actions in optimizing the medical education system to adapt the rapidly growing healthcare demand (Hou et al., 2014). In order to meet the demand for high-quality medical personnel in China’s healthcare, the reform of medical education in China has gone through several epoch-making stages, including the merge of independent medical schools into comprehensive universities in 1998 (Hsieh and Tang, 2019); the establishment of the accreditation system for clinical medical specialties in 2008 (Geffen et al., 2014); the initiation of the standardized residency training system in 2013 (Hsieh and Tang, 2019); the accreditation by the World Federation of China’s clinical medicine program in 2020; and the medical education development in China entered a new era with the release of the “Healthy China 2030 Planning Outline” put the people’s healthcare issues to a national strategic level (Song et al., 2017).
The global outbreak of COVID-19 has brought the unprecedented burden to the healthcare system all round the world. The COVID-19 pandemic underscored the severe deficit of medical resources, in which the shortage of medical personnel is more striking. The fight against COVID-19 has directly tested the medical education system worldwide (Yang et al., 2020). For example, the pressure on hospitals to provide clinical training for medical students increased dramatically during the COVID-19 pandemic, and Chinese medical schools quickly moved to online learning and included modules on infectious disease prevention and control in their online curricula, but the coverage of online training for primary care physicians still needs to be improved. Therefore, it accelerated the adjustment of China’s medical education and training model (Li et al., 2020). The noble spirit and superior medical skills shown by the medical staff in times of crisis highlighted the success of medical personnel training in China. However, while huge progress has been made in medical education, it is also clear that medical personnel will need to acquire more comprehensive capabilities in the future, such as multidisciplinary integration and crisis response skills. Driven by both the government’s long-term healthcare strategy and the short-term outbreak of COVID-19, we should objectively examine the challenges faced by medical education system in China. We also have to consider the developing direction of medical education in China by referencing the models of other medical education systems from a longer-term perspective. Existing studies often focus on isolated aspects; this review synthesizes policy documents, empirical research, and case studies to provide a comprehensive reform framework.
Methods
Study design
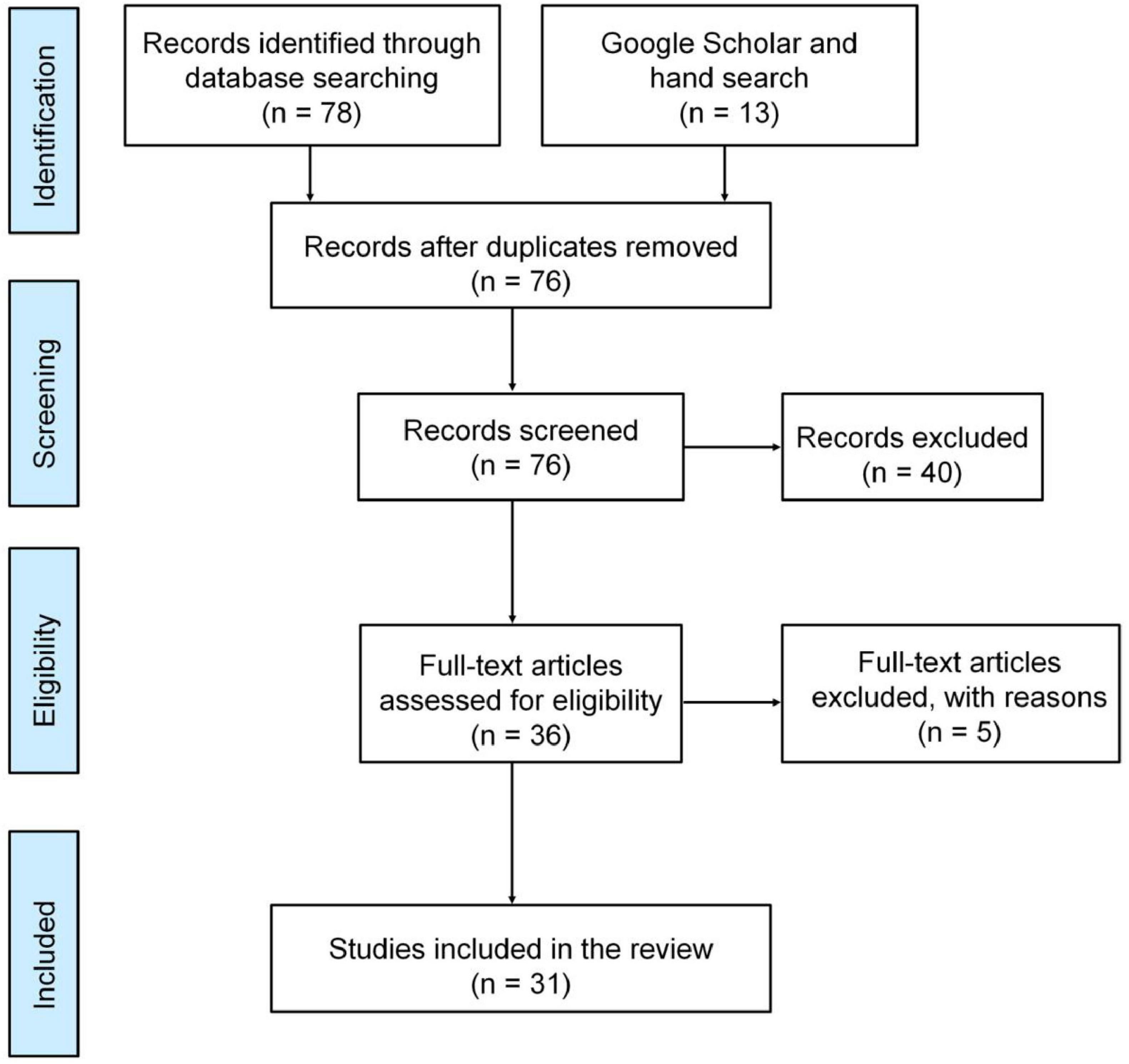
This study follows a systematic review approach to analyze the current state and future directions of medical education in China. The review adheres to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to ensure transparency, reproducibility, and methodological rigor. A thematic analysis was employed to synthesize findings across selected studies.
Literature search strategy
A comprehensive literature search was conducted in the Web of Science and PubMed databases to identify relevant studies published between 2012 and August 2024. The search terms included “Medical education reform,” “Curriculum development,” “General practitioners,” “Public health education,” “China,” and “COVID-19.” Additionally, a manual search of relevant journals and internet sources was performed to enhance the comprehensiveness of the review. All authors contributed to refining the search strategy and reviewing the retrieved articles.
Inclusion and exclusion criteria
Studies were selected based on the following criteria
• Inclusion criteria: Experimental and non-experimental studies written in English that discuss the current state, challenges, or future directions of medical education in China.
• Exclusion criteria: Dissertations, letters, commentaries, opinions, and editorial articles were excluded.
Study selection and data extraction
The literature selection process was conducted in several stages:
1. Initial screening: A total of 78 articles were retrieved from the database searches. An additional 13 articles were identified through manual searches.
2. Duplicate removal: Using EndNote X9 (Clarivate Analytics, USA), 15 duplicate articles were removed.
3. Title and abstract screening: Two authors independently screened the remaining 76 articles based on the inclusion and exclusion criteria, selecting 36 articles for full-text review.
4. Full-text review: Two authors independently assessed the full texts of these 36 articles and discussed their relevance. Studies were evaluated using the CASP checklist; low-quality articles (e.g., commentaries without data) were excluded. After excluding 5 articles that did not align with the study’s objectives, a final set of 31 articles was included in the review.
5. Data extraction: Key information, including study design, methodology, findings, and conclusions, was extracted from the selected articles using a standardized data extraction form. Any discrepancies were resolved through discussion among the authors.
Data analysis
A qualitative thematic analysis was conducted to synthesize findings across selected studies. The analysis followed Braun and Clarke’s framework:
1. Familiarization: Repeated reading of included studies to identify recurrent concepts.
2. Coding: Open coding of text segments related to medical education reforms (e.g., “curriculum integration,” “rural training gaps”).
3. Theme development: Codes were grouped into higher-order themes (e.g., “Curriculum Structure,” “Regional Disparities,” “Governance Challenges”) through iterative discussion.
4. Validation: Themes were cross-checked against original data to ensure interpretive consistency.
Findings were categorized into four primary themes relevant to China’s medical education system:
• l lCurriculum structure and reform
• l lInstitutional governance and accreditation
• l lRegional disparities in medical education
• l lComparative analysis with international models
Patterns, challenges, and proposed reforms were identified and summarized. No statistical meta-analysis was conducted due to the heterogeneity of study designs and methodologies.
Synthesis and reporting
Results were organized thematically and visualized in Figure 1, detailing exclusions at each stage.
Results
Current medical education in China
With the rapid growth of medical education in China, colleges are trying the best to deliver more highly qualified medical personnel to the healthcare service. However, we are still facing challenges on the way forward.
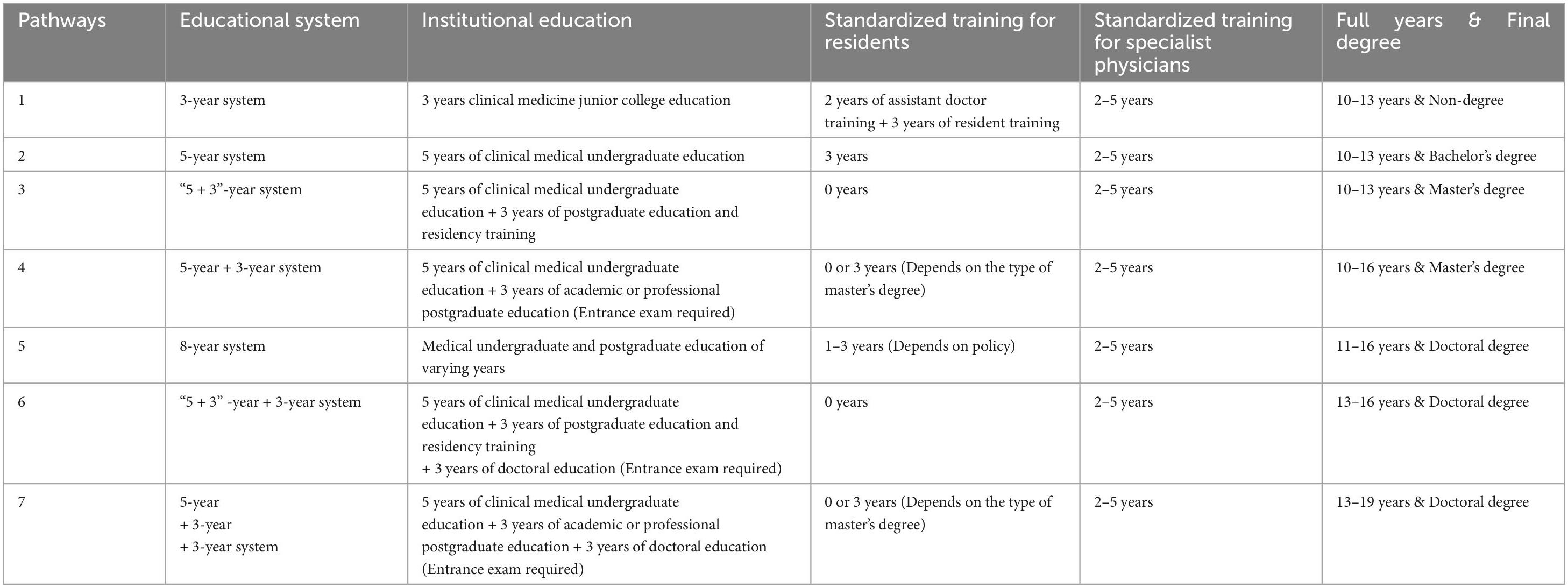
Parallel running of multiple medical education mechanisms
The basic path of medical education is clear in China, but there are multiple ways to complete clinical medical education (3-year, 5-year, “5 + 3” integration, 8-year) (Wu et al., 2014). With the strengthening of coordination and cooperation between education and healthcare facilities, China has gradually established a standardized medical personnel training system that bridges college education and post-graduation education. College education is a prerequisite for applying to practice medicine (Wu et al., 2014). There are two stages of post-graduation education: the first stage is residency training, which is now mandatory (Zeng et al., 2013); The second stage is specialist physician training, which has not yet been fully implemented. Table 1 shows the main pathways to main ways to complete medical education in China.
Postgraduate degrees in China are divided into professional degrees and academic degrees. The professional postgraduate focuses on the development of clinical skills during the 3 years of study. A professional degree master’s graduate certificate, degree certificate, physician qualification certificate and standardized training completion certificate are awarded after successful graduation (Zhang et al., 2013). It is allowed to apply for a professional doctoral education in following days. Academic postgraduates receive 3 years of scientific research training and award academic degree master’s graduate certificate and degree certificate after publication in peer-reviewed national or international journals. After a further 3 years of standardized residency training and physician qualification examinations, the academic master is eligible to conduct clinical activities in the hospital. Continuing academic doctoral education is also an option for academic masters. Medical graduates with an academic degree tend to pursue medical research in the future (Wu et al., 2014). Professional postgraduate degrees focus on clinical skills for grassroots service, while academic postgraduate degrees require research training, often leading to academic careers. This dual-track system addresses diverse needs but may limit research capacity in rural areas.
Synergistic development of medical education in different regions
Different living environments, behaviors, and economic situations lead to differences in the demand for medical resources between rural and urban rural and urban areas in China (Chen et al., 2019; Liu and Mao, 2020). The parallel running of multiple medical education mechanisms has produced a diverse range of medical personnel to meet the demand for healthcare services in different regions. The “5 + 3” integrated and 8-year medical graduates tend to stay in cities to provide demanding healthcare services. The 5-year undergraduate education and 3-year junior college education have been delivering medical personnel to rural areas in recent years (Qing et al., 2015).
In addition, China has been strengthening the training of primary health care personnel with a focus on general practitioners since 2017. The “Opinions on Medical Education Reform” issued by China clearly proposes to combine 3-year junior college education with a 2-year general practice residency training program to train as Assistant General Practitioners (AGPs). AGPs are required to provide basic care under the supervision of a supervising physician to serve rural areas. In the future, they can become General Practitioners (GPs) and practice independently after passing standardized training and assessment. The policy strongly supports the recruitment of rural students to medical schools, and tuition fees are waived for students who are oriented to rural areas after graduation, which is of great significance to the demand for personnel in rural areas (Zhang et al., 2013). The gap between urban and rural medical standards cannot be ignored. The establishment of hierarchical treatment and urban assistance to rural areas in China are also making efforts to promote the coordinated development of medical services (Jin Y. et al., 2020; Liu et al., 2019). The Tiered Medical System (TMS) has the capacity to facilitate the rational allocation and utilization of resources. China’s TMS is predicated on the categorization of healthcare institutions into three levels: primary (township clinics), secondary (county hospitals), and tertiary (urban hospitals) (Hao et al., 2017). The overarching objective of this categorization is to facilitate the transfer of non-emergency and chronic disease management to primary care facilities. Research conducted in Zhejiang Province has demonstrated that the implementation of the TMS can effectively reduce overcrowding in tertiary hospitals, provided that the first choice of primary care center is increased by 10%. This approach has the potential to save RMB 251.0 million from urban hospitals, which can then be allocated to primary care (Hao et al., 2017). The TMS has been demonstrated to effectively promote the coordinated development of rural and urban healthcare.
Continuous improvement of the diversified medical curriculum
With the growing demand for medical care, China has incorporated the medical humanities into its curriculum in addition to emphasizing the development of professional skills for medical students (Chang et al., 2014; Song and Tang, 2017). Medical humanities belong to interdisciplinary education, which includes disciplines such as philosophy, sociology, political theory and pedagogy. Medical humanities education can enhance the social responsibility, empathy and understanding of medical students (Song et al., 2017). For example, the Nanjing University of Traditional Chinese Medicine offers a course on “Narrative Medicine”, which can improve medical students’ attitudes toward death, their ability to cope with death, and their attitudes toward caring for terminally ill patients by integrating patient stories with narrative pedagogy (Zhu et al., 2023). This study helps medical schools to understand the importance and urgency of medical humanities education. Furthermore, it provides a constructive approach that has the potential to enhance medical students’ empathy. However, most medical schools in China face a shortage of teachers and funding for the development of the humanities. Reports indicate that there is a lack of 200,000 pediatricians, over 200,000 anesthesiologists, and 161,000 general practitioners in China (Qiu et al., 2018; Wu et al., 2016). Undergraduate courses directed at pediatrics, anesthesiology, and general medicine have been gradually promoted in China.
The outbreak of COVID-19 has tested the development of public health disciplines in China (Hong et al., 2020). Public health-related infectious diseases, microbiology, epidemiology, and evidence-based medicine have been present in undergraduate medical education, which has provided a solid foundation for the active performance of Chinese medical personnel in the fight against the epidemic. The low proportion of public health courses and the lack of training in public health emergencies require more attention in China (Yang et al., 2020). The ongoing epidemic has also contributed to a change in teaching methods. The internet-based distance learning becoming more widely accepted by public. Distance learning with easily updated and disseminated also meet the medical needs of different regions and is more conducive to the development of medical education in remote rural areas (Wong et al., 2010). Funding, technology and quality assurance are areas where distance learning needs to be improved in the future (Peng et al., 2014).
Multiple department collaborative management mechanism in medical education
Medical education in China includes college education and post-graduation education, which are completed in schools and affiliated hospitals (Zhang et al., 2013). It is significant to improve the management mechanisms of schools and affiliated hospitals. China has established a management mechanism for medical education with the participation of multiple departments, including education, health and finance, to jointly negotiate major policies and issues in medical education. The Ministry of Education is responsible for the administration and teaching management in affiliated hospitals. The medical services provided by the affiliated hospitals have not changed, and medical services remain the responsibility of the health department, thus creating a situation where the education department, the health department and the university share management. This multiple management is prone to problems of unclear division of responsibilities and complex working procedures (Pei et al., 2002). For example, the approval process for new medical school projects often involves overlapping responsibilities between the Ministry of Education and the Ministry of Health, leading to longer and less efficient decision-making. Faculty allocation and funding allocation are also affected by the complexity of multiple administrations, leading to a lag in the allocation of teaching resources to hospitals affiliated with underdeveloped cities (Frenk et al., 2022). Actively improving the management system will benefit the development of medical education in China.
Discussion
This systematic review delineates the current state of medical education in China, highlighting its rapid evolution alongside persistent challenges. Our analysis reveals a system striving to balance standardization with regional adaptability, clinical training with research capacity, and traditional pedagogy with innovative reforms. While China has made progress in expanding its medical education system, the coexistence of multiple training pathways and regional disparities continues to create inconsistencies in physician training. The integration of medical humanities, public health education, and general practice remains insufficient, which may limit the ability of future healthcare professionals to meet the diverse needs of the population. Additionally, the collaboration between medical schools and affiliated hospitals needs further optimization to ensure a more cohesive and practical training experience for students. During the development of medical education, China has constantly learned from the experiences of foreign developed countries (Bo et al., 2014). In the following, we discuss these results in relation to some typical foreign medical education models and propose actionable recommendations.
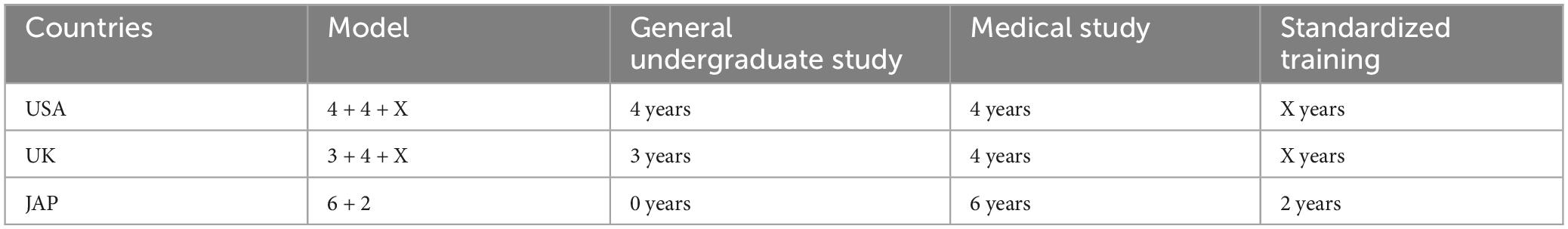
American mode
The “4 + 4” model established by United States (US) is well known: medical students need to complete 4 years of general university education and receive a bachelor’s degree before entering medical school. After admission to medical school, medical students undergo 4 years of medical education, culminating in an M.D. degree (Mowery, 2015). Earning an M.D. is a prerequisite for admission to practice medicine. Medical students enter the residency training after completing the medical school (Cui and Wang, 2016). They register as general practitioners after the first phase of training, and as specialists after the second phase of training in related specialties. Many medical schools in the US also promote the M.D./Ph.D. program, which is to add the Ph.D. training to M.D. (Harding et al., 2017). It usually requires 4–5 years of research training with the goal of developing leaders in the field of medical research.
British mode
Students in the UK apply to university after high school, and after 3 years of general undergraduate study they go on to medical school for 4 years of medical study. Or they enter university after high school for 2 years of pre-clinical study followed by 2–3 years of clinical medicine. The final degree is the Bachelor of Medicine and Surgery (MBBS), which is a requirement for physician registration. In the UK, there are medical masters and doctoral degrees, but they are not directly linked to the practice of medicine. After obtaining the MBBS, medical students have to go through several stages of post-graduate medical education, including pre-registration residency, senior residency, chief residency and senior chief residency (Lambert and Goldacre, 2005). In the chief residency stage, physicians can apply for the doctoral degree, which is awarded after a period of full-time research in a research position with corresponding results; surgeons can obtain a master’s degree after 1–1.5 years of full-time research work. The master’s and doctoral degrees are not necessarily linked to post-graduate education, but chief residents may not be promoted to senior chief resident until obtaining master’s or doctoral degrees (Alamri, 2016).
Japanese mode
Medical schools in Japan are a 6-year program for high school graduates, and a bachelor’s degree in medicine is awarded upon graduation (Tsunekawa et al., 2020). Obtaining a bachelor’s degree in medicine is a requirement for admission as a physician. After graduating, medical undergraduates take the national medical examination and are certified as physicians (Kozu, 2006). A further 2 years of clinical training is required to become a full-fledged clinician. After completing their undergraduate education, medical students can pursue 4–8 years of postgraduate education to obtain a Ph.D. degree. The goal of the Ph.D. degree is clearly to develop the knowledge and abilities necessary to conduct independent medical research (Onishi, 2018; Teo, 2007). Table 2 shows the models of medical education in developed countries.
In order to promote medical education reform, China could adopt the following adaptive policies:
Building unified medical degrees with clear objectives
To establish a system of training clinical medical talents with “5 + 3” (5 years of undergraduate education in clinical medicine + 3 years of standardized residency training or 3 years of postgraduate education for master’s degree in clinical medicine) as the mainstay and “3 + 2” (3 years of specialist education in clinical medicine + 2 years of training for assistant general practitioners) as a supplement. The master’s degree will be abolished and a separate M.D. degree in medicine will be established (Hou et al., 2014). In the “5 + 3” integrated medical professional training model, the M.D. degree will be conferred directly upon completion of 5 years of undergraduate education, 3 years of standardized training and specialist training in relevant disciplines. The MD degree is also awarded to those who have completed the 8-year clinical education. The purpose of the “5 + 3” and the 8-year training model is to cultivate medical personnel with excellent clinical capabilities. Medical professionals with an interest in research may receive 2–3 years of research training after obtaining M.D. degree, and then be awarded an additional Ph.D. degree after achieving certain achievements in the relevant field. The “3 + 2” program provides high-quality medical staffs for the grassroots.
Focusing on general practitioners and primary care
Increasing the training of general practitioners through standardized training for residence and training for assistant general practitioners. Improving the training policy for directed general practice, and expanding the scale of general practitioner training appropriately according to demand. Enhancing policy and financial support for medical schools in disadvantaged areas. Giving full play to the leading role of high-level medical colleges to improve the level of education run by weak colleges. Improving the health service capacity of rural grassroots medical personnel through expert support and cadre training. It is recommended that a grassroots-oriented doctor training program should be developed to encourage medical staffs to join the grassroots (Ran et al., 2020). More efforts should be made to improve the working environment in rural areas to enhance the attractiveness of the grassroots medical career (Russell et al., 2017). The career development prospects of grassroots doctors should be broadened, and preferential policies should be formulated in terms of title assessment, social security and job establishment. Giving praise and rewards to doctors who have been rooted in the grassroots, and enhancing the sense of professional honor and belonging of grassroots doctors (Sen Gupta et al., 2008).
Strengthening medical humanities and public health education
In order to improve the humanistic quality of medical students, it is recommended that colleges set up medical humanities research centers and incorporate humanities into the curriculum (Mangione et al., 2018). It is also necessary to increase policy guidance and financial support to build a capable team of humanistic education teachers. Regular humanities forums are held in schools and hospitals to actively create a humanities atmosphere and provide a platform for all medical students to interact with each other (Graham et al., 2016). Experts in medical humanities are regularly hired to give lectures on humanities to medical students. Emphasis should be placed on the exemplary role of clinical lead teachers in medical humanities education. Increasing social acceptance is a prerequisite for promoting the development of public health (Jin H. et al., 2020). Actively adjust the structure of medical personnel and provide policy preference for students applying for public health in undergraduate and postgraduate enrollment. The proportion of public health subjects in the curriculum is appropriately increased. Increase investment in public health education and establish “public health emergency drill centers” in provinces to provide regular training for medical personnel in responding to various public health emergencies (Yang et al., 2020).
Improving the management mechanism between colleges and affiliated hospitals
It is suggested that to give full play to the function of medical schools in coordinating the development of medical education (Ludmerer, 2004). A certain degree of autonomy in enrollment, teaching, discipline construction, scientific research, talent introduction, and funding management should be granted to medical schools (Buja, 2019). It is a good choice to give the medical school the authority to manage and supervise the teaching and scientific research of affiliated hospitals. Granting medical schools right to review medical technical titles makes them an academic management entity. It is important to establish communication channels and feedback mechanisms to achieve synergy between colleges and clinical institutions.
Conclusion
Although medical education in China has developed rapidly and made certain achievements, it needs further reform driven by both the Government’s long-term healthcare strategy and the short-term outbreak of COVID-19 epidemic. This review integrates the current situation of medical education in China and successful foreign medical education models, and then proposes interventions for reform in order to cultivate medical personnel that meet future needs in China. This review may serve as a reference for the educational efforts of medical schools in China.
Author contributions
KL: Data curation, Investigation, Writing – original draft, Writing – review and editing. HC: Conceptualization, Supervision, Writing – review and editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by Graduate Education Reform Program of Yangzhou University (132031074) and Postgraduate Research and Practice Innovation Program of Jiangsu Province (SJCX22-1819).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alamri, Y. (2016). The combined medical/PhD degree: A global survey of physician-scientist training programmes. Clin. Med. (Lond). 16, 215–218. doi: 10.7861/clinmedicine.16-3-215
Bo, H., Zhang, D. H., Zuo, T. M., Xue, D. B., Guo, J. S., Liu, M. N., et al. (2014). Survey and analysis of the current state of residency training in medical-school-affiliated hospitals in China. BMC Med. Educ. 14:111. doi: 10.1186/1472-6920-14-111
Buja, L. M. (2019). Medical education today: All that glitters is not gold. BMC Med. Educ. 19:110. doi: 10.1186/s12909-019-1535-9
Chang, Y., Zhou, X., and Zhang, Y. (2014). Medical humanity: How do we learn it? Chin. Med. J. 127, 4292–4294.
Chen, J., Pu, M., and Hou, W. (2019). The trend of the Gini coefficient of China (1978-2010). J. Chin. Econ. Bus. Stud. 17, 261–285. doi: 10.1080/14765284.2019.1663695
Cui, Y., and Wang, T. (2016). [From the residency training in the united states to see the challenges and directions of china residency standardized training]. Zhongguo Fei Ai Za Zhi 19, 321–327. doi: 10.3779/j.issn.1009-3419.2016.06.03
Frenk, J., Chen, L. C., Chandran, L., Groff, E. O. H., King, R., Meleis, A., et al. (2022). Challenges and opportunities for educating health professionals after the COVID-19 pandemic. Lancet 400, 1539–1556. doi: 10.1016/S0140-6736(22)02092-X
Geffen, L., Cheng, B., Field, M., Zhao, S., Walters, T., and Yang, L. (2014). Medical school accreditation in China: A Sino-Australian collaboration. Med. Teach. 36, 973–977. doi: 10.3109/0142159X.2014.917286
Graham, J., Benson, L. M., Swanson, J., Potyk, D., Daratha, K., and Roberts, K. (2016). Medical humanities coursework is associated with greater measured empathy in medical students. Am. J. Med. 129, 1334–1337. doi: 10.1016/j.amjmed.2016.08.005
Hao, Z., Yue, L., Shu-Yan, G. U., Xue-Mei, Z., Yu-Hang, Z., Yu-Xuan, G. U., et al. (2017). Whether tiered medical care system is effective in saving costs? Cost savings estimation of the medical care system after tiered optimization in Zhejiang Province based on system dynamics model. Chin. J. Health Policy.
Harding, C. V., Akabas, M. H., and Andersen, O. S. (2017). History and outcomes of 50 years of physician-scientist training in medical scientist training programs. Acad. Med. 92, 1390–1398. doi: 10.1097/ACM.0000000000001779
Hong, Z., Li, N., Li, D., Li, J., Li, B., Xiong, W., et al. (2020). Telemedicine during the COVID-19 pandemic: Experiences from Western China. J. Med. Int. Res. 22:e19577. doi: 10.2196/19577
Hou, J., Michaud, C., Li, Z., Dong, Z., Sun, B., Zhang, J., et al. (2014). Transformation of the education of health professionals in China: Progress and challenges. Lancet 384, 819–827. doi: 10.1016/S0140-6736(14)61307-6
Hsieh, C.-R., and Tang, C. (2019). The multi-tiered medical education system and its influence on the health care market-China’s flexner report. Hum. Resources Health 17:50. doi: 10.1186/s12960-019-0382-4
Jin, H., Dong, G., Zou, L., Shen, X., and Li, D. (2020). History and status quo of higher public health education in China. Public Health Rev. 41:12. doi: 10.1186/s40985-020-00120-x
Jin, Y., Xu, J., Zhu, W., Zhang, Y., Xu, L., and Meng, Q. (2020). Synergy of policies to strengthen primary care: Evidence from a national repeated cross-sectional study. BMC Health Serv. Res. 20:865. doi: 10.1186/s12913-020-05695-4
Kozu, T. (2006). Medical education in Japan. Acad. Med. 81, 1069–1075. doi: 10.1097/01.ACM.0000246682.45610.dd
Lambert, T. W., and Goldacre, M. J. (2005). Progression of junior doctors into higher specialist training. Med. Educ. 39, 573–579. doi: 10.1111/j.1365-2929.2005.02179.x
Li, L., Xv, Q., and Yan, J. (2020). COVID-19: The need for continuous medical education and training. Lancet Respir. Med. 8:e23. doi: 10.1016/S2213-2600(20)30125-9
Liu, J., and Mao, Y. (2020). Continuing medical education and work commitment among rural healthcare workers: A cross-sectional study in 11 western provinces in China. BMJ Open 10:e037985. doi: 10.1136/bmjopen-2020-037985
Liu, J., Zhu, B., Zhang, N., He, R., and Mao, Y. (2019). Are medical graduates’ job choices for rural practice consistent with their initial intentions? a cross-sectional survey in Western China. Int. J. Environ. Res. Public Health 16:3381. doi: 10.3390/ijerph16183381
Ludmerer, K. M. (2004). The development of American medical education from the turn of the century to the era of managed care. Clin. Orthop. Relat. Res. 422, 256–262. doi: 10.1097/01.blo.0000131257.59585.b0
Mangione, S., Chakraborti, C., Staltari, G., Harrison, R., Tunkel, A. R., Liou, K. T., et al. (2018). Medical students’ exposure to the humanities correlates with positive personal qualities and reduced burnout: A multi-institutional U.S. survey. J. Gen. Int. Med. 33, 628–634. doi: 10.1007/s11606-017-4275-8
Mowery, Y. M. (2015). A primer on medical education in the United States through the lens of a current resident physician. J. Thorac. Dis. 7, E473–E481. doi: 10.3978/j.issn.2072-1439.2015.10.05
Onishi, H. (2018). History of Japanese medical education. Korean J. Med. Educ. 30, 283–294. doi: 10.3946/kjme.2018.103
Pei, L., Legge, D., and Stanton, P. (2002). Hospital management in China in a time of change. Chin. Med. J. (Engl) 115, 1716–1726.
Peng, Y., Wu, X., Atkins, S., Zwarentein, M., Zhu, M., Zhan, X. X., et al. (2014). Internet-based health education in China: A content analysis of websites. BMC Med. Educ. 14:16. doi: 10.1186/1472-6920-14-16
Qing, Y., Hu, G., Chen, Q., Peng, H., Li, K., Wei, J., et al. (2015). Factors that influence the choice to work in rural township health centers among 4,669 clinical medical students from five medical universities in Guangxi. China. J. Educ. Eval. Health Prof. 12:40. doi: 10.3352/jeehp.2015.12.40
Qiu, Y., Liu, Y., Ren, W., Qiu, Y., and Ren, J. (2018). Internet-Based and mobile-based general practice: Cross-sectional survey. J. Med. Int. Res. 20:e266. doi: 10.2196/jmir.8378
Ran, Y., Gao, H., Han, D., Hou, G., Chen, Y., and Zhang, Y. (2020). Comparison of inpatient distribution amongst different medical alliances in a county: A longitudinal study on a healthcare reform in rural China. Int. J. Equity Health 19:142. doi: 10.1186/s12939-020-01260-x
Russell, D. J., McGrail, M. R., and Humphreys, J. S. (2017). Determinants of rural Australian primary health care worker retention: A synthesis of key evidence and implications for policymaking. Aust. J. Rural Health 25, 5–14. doi: 10.1111/ajr.12294
Sen Gupta, T. K., Muray, R. B., McDonell, A., Murphy, B., and Underhill, A. D. (2008). Rural internships for final year students: Clinical experience, education and workforce. Rural Remote Health 8:827.
Song, P., and Tang, W. (2017). Emphasizing humanities in medical education: Promoting the integration of medical scientific spirit and medical humanistic spirit. Biosci. Trends 11, 128–133. doi: 10.5582/bst.2017.01092
Song, P., Jin, C., and Tang, W. (2017). New medical education reform in China: Towards healthy China 2030. Biosci. Trends 11, 366–369. doi: 10.5582/bst.2017.01198
Teo, A. (2007). The current state of medical education in Japan: A system under reform. Med. Educ. 41, 302–308. doi: 10.1111/j.1365-2929.2007.02691.x
Tsunekawa, K., Suzuki, Y., and Shioiri, T. (2020). Identifying and supporting students at risk of failing the national medical licensure examination in japan using a predictive pass rate. BMC Med. Educ. 20:419. doi: 10.1186/s12909-020-02350-8
Wong, G., Greenhalgh, T., and Pawson, R. (2010). Internet-based medical education: A realist review of what works, for whom and in what circumstances. BMC Med. Educ. 10:12. doi: 10.1186/1472-6920-10-12
Wu, L., Wang, Y., Peng, X., Song, M., Guo, X., Nelson, H., et al. (2014). Development of a medical academic degree system in China. Med. Educ. Online 19, 23141–23141. doi: 10.3402/meo.v19.23141
Wu, Q., Zhao, L., and Ye, X. C. (2016). Shortage of healthcare professionals in China. BMJ 354:i4860. doi: 10.1136/bmj.i4860
Yang, D. Y., Cheng, S. Y., Wang, S. Z., Wang, J. S., Kuang, M., Wang, T. H., et al. (2020). Preparedness of medical education in China: Lessons from the COVID-19 outbreak. Med. Teach. 42, 787–790. doi: 10.1080/0142159X.2020.1770713
Zeng, J., Zeng, X. X., and Tu, Q. (2013). A gloomy future for medical students in China. Lancet 382, 1878–1878. doi: 10.1016/S0140-6736(13)62624-0
Zhang, Q., Lee, L., Gruppen, L. D., and Ba, D. (2013). Medical education: Changes and perspectives. Med. Teach. 35, 621–627. doi: 10.3109/0142159X.2013.789495
Keywords: medical education reform, curriculum development, general practitioners, public health education, China, COVID-19
Citation: Li K and Chen H (2025) Running medical education system and its development in China. Front. Educ. 10:1513854. doi: 10.3389/feduc.2025.1513854
Received: 19 October 2024; Accepted: 19 May 2025;
Published: 04 June 2025.
Edited by:
Nina Pereza, University of Rijeka, CroatiaReviewed by:
Mohamed Elhassan Abdalla, University of Limerick, IrelandAnil Kumar Marapaka, Purdue University, United States
Copyright © 2025 Li and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hao Chen, aGNoZW4yMDIwQHl6dS5lZHUuY24=
 Ke Li
Ke Li Hao Chen
Hao Chen