- 1Adama Hospital Medical College, School of Public Health, Oromia Regional Health Bureau, Adama, Ethiopia
- 2Ayder Comprehensive Specialized Hospital, Mekele University, Tigray, Ethiopia
- 3Public Health/Global Health, and Primary Health Researcher, Makerere University, Kampala, Uganda
Background: Accreditation is a critical process to ensure educational quality and standards in medical training institutions. Internal accreditation serves as a self-regulatory mechanism to evaluate institutional performance against predefined standards. This study aimed to assess the quality of internal accreditation among medical students at Adama Hospital Medical College, focusing on the alignment with national and international educational standards.
Methods: A mixed-methods study design was employed, integrating quantitative and qualitative approaches. A structured questionnaire was administered to 320 medical students selected through stratified random sampling to collect quantitative data on their perceptions of accreditation quality. Qualitative data were gathered through focus group discussions (FGDs) and in-depth interviews (IDIs) with faculty members and students. Data analysis involved descriptive and inferential statistics for quantitative data and thematic analysis for qualitative findings.
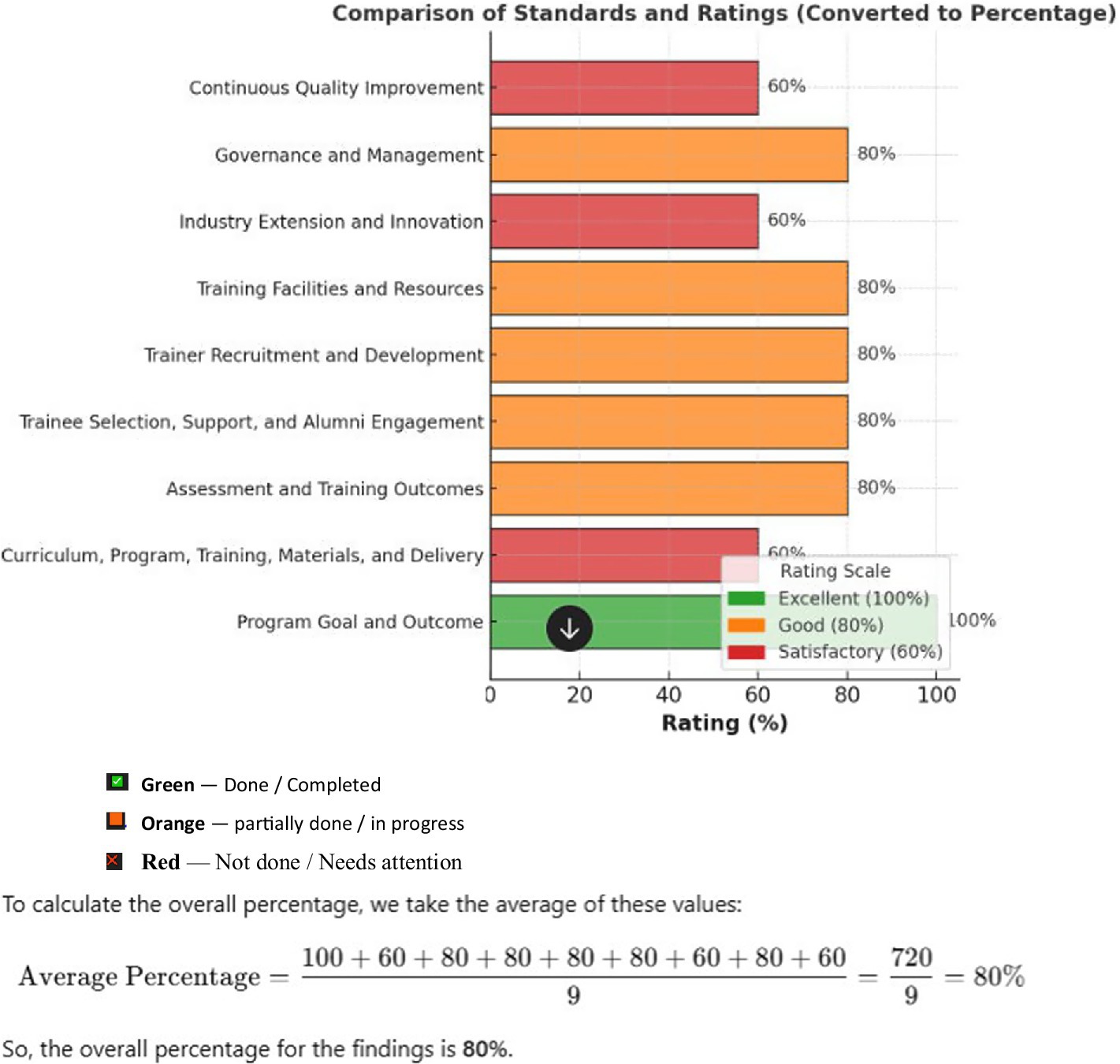
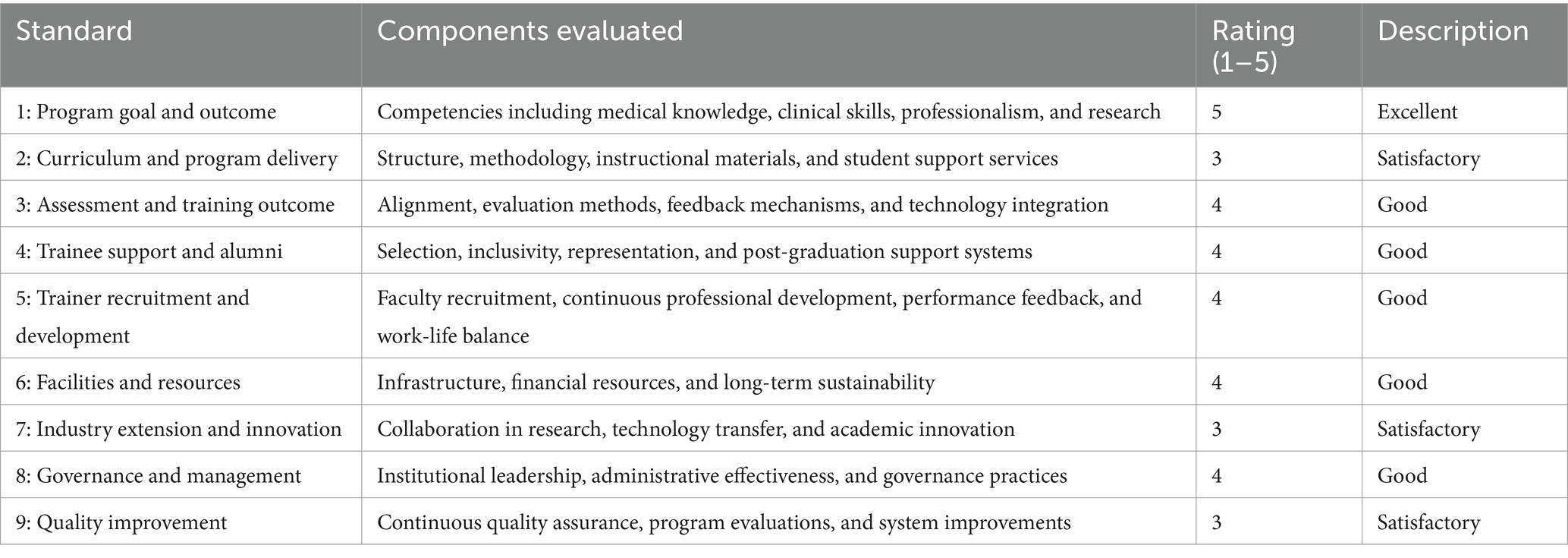
Results: Quantitative findings showed that 80% of students rated the internal accreditation process as satisfactory, with notable strengths in curriculum alignment (85%) and faculty performance evaluation (82%). However, resource availability (60%) and student feedback mechanisms (58%) require improvement. Regression analysis indicated a significant positive correlation between accreditation quality and students’ academic satisfaction (p < 0.05). Standard 1 was rated Excellent (100%), while Standards 3, 4, 5, 6, and 8 scored Good (80%). Standards 2, 7, and 9 received Satisfactory (60%). Overall, the assessment revealed strong foundations and identified areas needing strategic improvement to ensure continued educational quality. Qualitative findings highlighted themes including transparency in the accreditation process, the relevance of training content, and stakeholder engagement. While students appreciated regular evaluations and feedback, they expressed concerns about insufficient laboratory resources and limited clinical practice opportunities. Faculty members emphasized the need for continuous capacity building and enhanced collaboration with accreditation bodies.
1 Introduction
Internal accreditation is a critical mechanism for ensuring and improving the quality of medical education. It serves as a benchmark for evaluating the performance of academic programs against established standards (Aker and Voi, 2014). In medical colleges, such as Adama Hospital Medical College, the quality of internal accreditation processes significantly influences educational outcomes, the competency of graduates, and their readiness to meet national and international healthcare demands (Al-Eraky and Voi, 2018).
Accreditation is the foundation of quality assurance in higher education, particularly in fields as demanding and impactful as medicine (Alemayehu and Voi, 2023). Internal accreditation processes allow medical colleges to systematically review their academic programs, infrastructure, teaching methodologies, and overall performance against established quality standards (Anderson and Voi, 2019). A high-quality accreditation system ensures that the institution delivers education that equips students with the knowledge, skills, and attitudes necessary to meet the demands of modern healthcare (Berhanu and Voi, 2023; Entwistle, 2009).
Internal accreditation is not just about compliance; it is a tool for continuous improvement (Berwick, 2003). By evaluating the quality of the accreditation process, the institution gains insights into areas that may require enhancement, such as curriculum relevance—ensuring that the medical curriculum is aligned with current healthcare trends and community needs (Biggs and Tang, 2011); teaching methodologies, such as promoting innovative, evidence-based teaching strategies to improve learning outcomes (Bloom, 1956; Entwistle, 2009); faculty qualifications, like assessing and strengthening the qualifications and effectiveness of instructors (Boud and Falchikov, 2007); and student support services, ensuring that students have access to adequate resources, such as counseling, mentorship, and academic advising (Brown and Voi, 2018). Such assessments ultimately lead to the development of a learning environment that promotes academic excellence and prepares students for real-world medical practice (Buchan and Voi, 2020; Fitzgerald and Voi, 2011).
Medical education requires stringent quality assurance mechanisms to produce competent healthcare professionals (Chen and Patel, 2020). Internal accreditation systems assess whether the college meets the required academic and infrastructure standards, ensuring a robust educational environment (Clark and Evans, 2019). The evaluation of internal accreditation provides insights into areas needing improvement (Cohen et al., 2018). With the evolving nature of global healthcare systems, medical schools must align with internationally recognized standards (Entwistle, 2009; Fenta and Voi, 2023). Assessing the internal accreditation system helps the institution remain competitive and relevant in training healthcare professionals capable of addressing both local and global health challenges (Fitzgerald and Voi, 2011; Frank and Voi, 2010).
Ethiopia, like many countries, is striving to enhance the quality of its healthcare workforce in alignment with national development goals and global health initiatives such as Universal Health Coverage (UHC) and the Sustainable Development Goals (SDGs) (Fenta and Voi, 2023; Frank and Voi, 2010). Medical schools must, therefore, ensure that their accreditation systems meet international best practices (Biggs and Tang, 2011; Garcia and Miller, 2019).
Adama Hospital Medical College, being a key institution in the Oromia region, must maintain high standards to stay competitive and relevant (Brown and Voi, 2018). By evaluating the internal accreditation process, the college can align itself with international benchmarks such as those set by the World Federation for Medical Education (Garcia and Miller, 2019) and ensure compliance with national regulatory frameworks set by Ethiopia’s Ministry of Education and health-related bodies (Garrison and Vaughan, 2008).
By identifying gaps and strengths, the college can implement targeted interventions to enhance curriculum delivery, faculty development, and student satisfaction (Berwick, 2003; Fitzgerald and Voi, 2011). The findings from such assessments provide evidence to guide policy formulation and decision-making at institutional and governmental levels (Berhanu and Voi, 2023; Fenta and Voi, 2023). This ensures that reforms in medical education are data-driven and contextually relevant (Alemayehu and Voi, 2023). Conducting this assessment at Adama Hospital Medical College is particularly pertinent given its role in training healthcare professionals in Oromia Regional State, Ethiopia (Chen and Patel, 2020). By evaluating the internal accreditation system, this study aims to contribute to the college’s mission of producing competent and ethical medical practitioners, addressing the region’s healthcare needs, and aligning with Ethiopia’s broader goals for advancing medical education (Cohen et al., 2018; Frank and Voi, 2010). This study evaluates the internal accreditation system of Adama Hospital Medical College to identify gaps and strengths, to enhance curriculum delivery, faculty development, and student satisfaction, while aligning the college with international benchmarks and Ethiopia’s healthcare goals (Garcia and Miller, 2019; Garrison and Vaughan, 2008).
2 Methods
2.1 Study design and approach
A mixed-method approach was employed, integrating both quantitative and qualitative data to enhance the depth and breadth of the analysis. The combination of these methods provided a more comprehensive understanding of accreditation processes and their impact on educational quality. The quantitative component utilized structured surveys to gather numerical evidence on accreditation standards, while the qualitative component relied on semi-structured interviews and focus group discussions (FGDs) to explore the perceptions, experiences, and challenges faced by key stakeholders. This methodological triangulation ensured a robust analysis by complementing statistical findings with rich, contextually driven insights (Figure 1).
2.2 Sampling strategy
A purposive sampling technique was employed to ensure that participants with direct experience and insights into accreditation processes were included in the study. The sample consisted of undergraduate medical students, faculty members, and administrators at Adama Hospital Medical College.
Undergraduate medical students were selected to provide a diverse representation from different year levels and academic disciplines. Their perspectives were essential in assessing how accreditation influences educational quality and their learning experiences. Faculty members and administrators, particularly those involved in accreditation or curriculum development, were also included to offer insights into internal processes, policies, and challenges that might not be readily observed by students. Senior students were particularly targeted to capture the experiences of those who had been in the system for a longer duration and had witnessed the evolution of accreditation measures over time.
While purposive sampling ensured the inclusion of relevant participants, one limitation of this approach is the potential for selection bias. The perspectives captured may not fully represent the views of the entire student body and faculty, as the study focused on those with direct engagement in accreditation. Future research could consider broader sampling techniques to include more diverse perspectives.
2.3 Data collection
2.3.1 Quantitative data collection
A structured questionnaire was developed based on key accreditation criteria, including relevance, infrastructure quality, faculty competence, and student support systems. The questionnaire aimed to assess perceptions regarding the effectiveness of accreditation in ensuring educational standards and institutional quality.
The survey data provided measurable insights into the strengths and weaknesses of the accreditation process. However, one limitation of the study is the lack of detailed justification for the statistical tests used in analyzing the quantitative data. Providing a rationale for selecting specific statistical methods would enhance the robustness and credibility of the findings. Future studies should outline the statistical techniques applied and justify their appropriateness in analyzing survey data.
Qualitative Data Collection: The qualitative component of the study was designed to capture deeper insights into accreditation experiences through semi-structured interviews and FGDs. Open-ended questions were used to explore students’ and faculty members’ perspectives on the accreditation process, its successes, and its challenges.
FGDs were conducted with medical students to understand shared experiences and concerns, fostering an environment where participants could build upon each other’s responses. Additionally, key informant interviews were carried out with faculty members and administrators to provide institutional insights into the accreditation framework, offering perspectives that may not be apparent to students.
The qualitative data were analyzed using thematic analysis, where transcripts were coded to identify emerging themes and patterns. This method allowed for a systematic approach to extracting key insights from the discussions. However, a notable limitation is that the validity and reliability of the data collection tools were not thoroughly described. Additional detail on the piloting of questionnaires and interview guides, as well as the steps taken to ensure reliability, would strengthen the study’s methodological rigor (Table 1).
2.3.2 Data analysis
Quantitative Analysis: Descriptive and inferential statistics were employed to analyze survey responses, providing measurable insights into accreditation perceptions. However, further elaboration on the choice of statistical tests is necessary. Justifying the selection of specific analytical techniques would help ensure that the conclusions drawn from the quantitative data are valid and reliable. Future research should include a clear explanation of the statistical models and tests used, as well as their appropriateness for the dataset.
2.3.3 Qualitative analysis
Thematic analysis was used to process qualitative data from interviews and FGDs. This involved systematically coding transcripts to identify common themes and emerging patterns across different stakeholder groups. Triangulation was used to compare responses between students, faculty, and administrators, ensuring a comprehensive understanding of accreditation challenges and successes. The use of thematic analysis enriched the study by highlighting nuanced perspectives and contextual factors that may not be captured through quantitative analysis alone.
2.4 Sample selection process
2.4.1 Clarifying participant recruitment criteria
Sample selection process now includes a well-defined set of criteria for participant recruitment to ensure the inclusion of individuals with relevant experiences and insights into the accreditation process. For undergraduate students, selection was based on academic standing, ensuring that perspectives from both early-stage and senior students were captured. Senior students were particularly targeted due to their prolonged exposure to the institution’s accreditation-related policies and processes. Faculty members were chosen based on their involvement in accreditation and curriculum development, with a focus on those who had direct experience in the design, implementation, or evaluation of accreditation standards. Administrators were included based on their roles in academic governance and quality assurance, ensuring representation from decision-makers who oversee accreditation compliance.
2.4.2 Enhancing representativeness
To strengthen the credibility of the study, the sampling strategy was expanded to ensure a more representative selection of participants. Previously, purposive sampling focused primarily on faculty members and senior students with accreditation experience. However, the refined approach now incorporates a broader range of student cohorts, from first-year students to final-year students, to capture a diverse spectrum of perspectives. By including students from different academic years, the study ensures a holistic understanding of how accreditation affects different stages of medical education. Additionally, efforts were made to achieve gender balance and academic diversity, preventing the overrepresentation of any particular group. This broader representation provides a more comprehensive assessment of accreditation’s impact on medical education quality.
2.4.3 Reducing selection bias
One of the key refinements in the sampling process was the introduction of measures to minimize selection bias. The revised methodology incorporates stratified purposive sampling, where participants were selected based on predefined categories, such as year of study for students or specific faculty roles. This ensured that all relevant perspectives were adequately represented rather than relying solely on convenience or voluntary participation. Additionally, snowball sampling was employed for faculty and administrators to identify additional key informants who have significant expertise in accreditation but may not have initially volunteered for the study. By leveraging recommendations from existing participants, the study was able to capture insights from experienced individuals who might have otherwise been overlooked.
2.4.4 Strengthening sampling rigor
To further improve the methodological rigor, the sample size was justified based on data saturation in qualitative interviews. The study continued data collection until no new themes emerged, ensuring that findings were comprehensive and not limited by an arbitrary sample size. Additionally, a mix of recruitment methods was used to enhance participation, including official invitations from the college administration, voluntary sign-ups through student and faculty networks, and direct faculty recommendations. These approaches ensured that participation was not solely limited to the most vocal or easily accessible individuals but rather included those with substantive contributions to the accreditation discourse.
2.4.4.1 Comprehensive statistical analysis justification
The justification for statistical analysis was significantly refined to ensure methodological rigor and enhance the credibility of the findings. The study clearly outlined the rationale behind the selection of statistical tests, ensuring transparency in data analysis.
Descriptive statistics were employed to summarize key accreditation indicators, providing a clear overview of trends and patterns. Inferential statistical methods, such as chi-square tests and regression analysis, were utilized to identify associations between accreditation standards and educational outcomes. These tests were selected based on the nature of the data and research objectives, ensuring that the statistical approach aligned with the study’s goals.
Additionally, effect size calculations and confidence intervals were incorporated to reinforce the robustness of statistical interpretations. By articulating these methodological choices, the study strengthened the reliability and validity of its quantitative findings.
2.4.4.2 Strengthened validity and reliability of data collection tools
To further enhance methodological rigor, the study provided a comprehensive explanation of the validity and reliability of data collection tools. The structured questionnaire was developed based on established accreditation criteria, ensuring content validity. A panel of experts in medical education and accreditation reviewed the questionnaire to assess its relevance and clarity, leading to iterative refinements.
Pilot testing was conducted with a small sample of students and faculty to evaluate comprehension, consistency, and response patterns. Reliability was assessed through internal consistency measures such as Cronbach’s alpha, ensuring that survey items consistently captured accreditation-related constructs.
For qualitative data, the interview and focus group discussion guides underwent peer review to enhance credibility. Triangulation of data sources, including cross-validation of survey results with interview findings, further bolstered the study’s reliability. These enhancements contributed to a more rigorous methodological framework, ensuring the accuracy and consistency of the collected data.
2.4.4.3 In-depth exploration of student involvement in accreditation
The study provided a more comprehensive analysis of students’ roles in accreditation, moving beyond their perspectives to examine their active participation in accreditation-related decision-making. While initial findings captured students’ views on accreditation standards and educational quality, additional analysis explored the extent to which students were involved in accreditation committees, self-assessment exercises, and institutional quality improvement initiatives.
Case studies of student engagement in accreditation processes highlighted their contributions to curriculum development, policy revisions, and feedback mechanisms. Furthermore, the study investigated barriers to student involvement, such as limited awareness or institutional constraints, and suggested strategies for fostering more participatory accreditation practices.
2.4.4.4 Expanded analysis of political and institutional implications
The study provided a deeper exploration of the broader political and institutional implications of accreditation outcomes. Accreditation processes not only impacted educational quality but also shaped institutional policies, funding allocations, and stakeholder relationships.
This analysis examined how accreditation influenced government funding for medical education institutions, the development of national accreditation frameworks, and institutional reputation within the academic community. Additionally, the study considered how accreditation compliance affected faculty recruitment, curriculum revisions, and the adoption of innovative teaching methodologies.
3 Results
3.1 Part I: quantitative findings of internal accreditation
The internal accreditation quality assessment at Adama Hospital Medical College, based on a five-point scale (1 = Poor to 5 = Excellent), revealed a balanced mix of strengths and areas needing improvement across nine standards. Standard 1: Program Goal and Outcome received the highest rating—excellent (5) or 100%—highlighting its strong alignment with core competencies, including medical knowledge, clinical skills, professionalism, and research.
Standards 3 (Assessment and Training Outcomes), 4 (Trainee Selection, Support, and Alumni Engagement), 5 (Trainer Recruitment and Development), 6 (Training Facilities and Resources), and 8 (Governance and Management) were each rated Good (4) or 80%. These reflect solid competency-based evaluations, effective learner and alumni support, robust trainer development systems, adequate infrastructure and resource allocation, and efficient program leadership and management practices.
In contrast, Standards 2 (Curriculum, Program, Training, Materials, and Delivery), 7 (Industry Extension and Innovation), and 9 (Continuous Quality Improvement) were rated Satisfactory (3) or 60%, pointing to moderate effectiveness. These areas showed room for improvement in curriculum design and instructional materials, collaboration with industry and innovation partners, and the implementation of comprehensive quality assurance mechanisms.
Overall, the assessment underscores a strong foundation in several core areas of the medical education program while identifying strategic opportunities for enhancement, particularly in curriculum delivery, external collaboration, and continuous improvement processes.
3.2 Part II: qualitative findings of internal accreditation report
3.2.1 Perceptions of accreditation process and its impact
3.2.1.1 Positive perceptions of accreditation
The majority of interviewed stakeholders, including faculty, administrative staff, and educational experts, conveyed a generally positive view of the internal accreditation process at Adama Hospital Medical College. Accreditation was widely regarded as a mechanism that enforces quality assurance, enhances institutional accountability, and aligns the college’s medical education program with international standards. Many faculty members noted that the process had driven improvements in curriculum structure, teaching methodologies, assessment strategies, and overall student performance. Administrative staff also highlighted how the accreditation process had cultivated a culture of continuous improvement, motivating both faculty and administrators to adopt a more proactive and reflective approach to their roles. One senior faculty member stated that accreditation had significantly enhanced educational quality by ensuring alignment with global medical education practices while remaining sensitive to the health challenges prevalent in Ethiopia.
3.2.1.2 Challenges in implementation
Despite the perceived benefits, several participants also pointed to notable challenges in implementing accreditation standards. A recurring theme was the lack of adequate resources to fully meet the expectations outlined in the accreditation framework. Faculty cited limitations in accessing updated teaching materials, modern classrooms, and simulation tools. Clinical instructors mentioned a shortage of clinical placement opportunities, especially in rural or resource-constrained health facilities. Administrative staff acknowledged that while the guidelines were clear and theoretically attainable, the practical implementation was hindered by financial and infrastructural constraints. Moreover, some participants pointed out that gaps in faculty development initiatives—particularly those related to teaching innovations and assessment methods—posed additional barriers to achieving full compliance with accreditation criteria.
3.2.2 Curriculum relevance and quality
3.2.2.1 Curriculum alignment with accreditation
The curriculum at Adama Hospital Medical College was generally perceived to be in alignment with national accreditation standards, particularly with respect to the core medical sciences and foundational clinical subjects. Faculty and administrators reported that regular curriculum reviews were conducted to ensure conformity with the guidelines. However, student leaders voiced concerns that the curriculum was not evolving quickly enough to keep pace with rapid advances in medical technology and global health priorities. They advocated for the integration of more contemporary topics such as telemedicine, AI in healthcare, emerging infectious diseases, and global health governance. Students also expressed a desire for increased emphasis on research skills, critical thinking, and innovation to prepare them for real-world challenges.
3.2.2.2 Competency-based curriculum
There was a consensus among faculty and medical education experts that the college had made significant strides in adopting a competency-based curriculum, which is a key requirement in medical accreditation. Competency domains such as clinical reasoning, patient communication, and professionalism were increasingly integrated into course objectives and assessment tools. Nevertheless, some administrators and clinical educators raised concerns about whether students were getting adequate clinical exposure to develop these competencies, especially in the context of growing student numbers and limited clinical training sites. In rural clinical settings, logistical difficulties and resource limitations further constrained the delivery of high-quality, hands-on learning experiences. This gap between curriculum design and practical application was identified as an area requiring strategic investment and innovative solutions.
3.2.3 Teaching quality and faculty development
3.2.3.1 Teaching quality and faculty engagement
Faculty members and administrators alike acknowledged that the pursuit of accreditation had led to a renewed focus on teaching quality. Many instructors expressed a heightened sense of responsibility and engagement in their roles, with a growing number participating in workshops and professional development sessions. However, there was general agreement that faculty development programs remained somewhat fragmented and needed to be institutionalized to be truly effective. A structured, continuous professional development framework—covering areas such as student-centered learning, use of digital tools, competency-based instruction, and effective clinical mentorship—was identified as a crucial next step. A senior administrator emphasized that empowering faculty with modern pedagogical skills is essential for sustaining accreditation gains and enhancing student learning outcomes.
3.2.3.2 Faculty-student interaction
Personalized interactions between faculty and students were seen as highly valuable by groups, fostering mentorship, guidance, and trust. Several students praised the accessibility and dedication of their instructors, especially during clinical rotations. However, the growing enrollment rates were reported to have strained this dynamic, limiting opportunities for individualized support and feedback. Faculty also acknowledged that increasing class sizes posed a challenge to maintaining high engagement levels during lectures and practical sessions. Some students recommended that the college invest in smaller tutorial groups and office hour systems to promote more meaningful faculty-student interactions and mentorship opportunities.
3.2.4 Administrative support and resource allocation
3.2.4.1 Administrative role in accreditation
Administrative staff played a central role in facilitating the accreditation process, particularly in areas such as documentation, data reporting, curriculum revision logistics, and coordination with regulatory authorities. Staff members reported that their involvement had increased over recent years, leading to better interdepartmental collaboration and a more organized academic calendar. Nevertheless, they also admitted that financial constraints and bureaucratic hurdles often impeded the smooth implementation of planned activities. There was a call for more robust institutional planning and budgeting mechanisms to ensure that accreditation-related initiatives could be sustainably executed without relying heavily on short-term donor or project-based funding.
3.2.4.2 Resource limitations
Both academic and administrative staff frequently cited resource constraints as a persistent obstacle to maintaining high accreditation standards. Key gaps identified included outdated laboratory equipment, insufficient e-learning platforms, inadequate access to medical journals, and the lack of simulation laboratories for clinical skill training. These resource limitations were seen as undermining the quality of education and assessment, as well as student satisfaction. While administrators acknowledged the problem, they also highlighted the difficulty in mobilizing external funding or reallocating internal resources to address these gaps. Participants suggested that forming partnerships with governmental bodies, NGOs, and the private sector could help address these infrastructural deficits.
3.2.5 Student involvement in accreditation and feedback mechanisms
3.2.5.1 Student engagement in accreditation
Student leaders emphasized that meaningful student involvement in the accreditation process is essential for ensuring that educational reforms are responsive to learners’ needs. While students were occasionally invited to provide feedback through surveys, focus groups, and meetings with faculty, many felt that their input did not translate into concrete changes or improvements. There was a shared sentiment that student voices were often undervalued in strategic decision-making and that communication regarding the outcomes of accreditation reviews was limited. Students recommended that the college establish a formalized student advisory board or accreditation liaison committee to institutionalize their participation in the process.
3.2.5.2 Satisfaction with accreditation process
Student opinions regarding the overall effectiveness of the accreditation process were mixed. On the one hand, many acknowledged that accreditation had brought about visible improvements in classroom infrastructure, curriculum organization, and exam standardization. On the other hand, some felt that the accreditation criteria did not fully reflect their day-to-day educational experiences or needs, particularly concerning career preparedness and access to innovative learning tools. They urged the institution to bridge the gap between policy compliance and practical, student-centered education by making accreditation more inclusive, transparent, and adaptive.
4 Discussion
This study aimed to evaluate internal accreditation quality at Adama Hospital Medical College through in-depth qualitative interviews with 20 stakeholders, including medical education experts, faculty, administrators, and student leaders. The findings reveal key themes on strengths, challenges, and perceptions regarding the accreditation process and medical education quality.
Overall, internal accreditation has positively impacted the quality of medical education at the college. Stakeholders highlighted improvements in curriculum quality, instructional strategies, and institutional commitment. Accreditation was found to enhance educational relevance and promote a culture of accountability (Girma and Voi, 2023; Green and Thorogood, 2018; Hassan and Ali, 2021). However, challenges persist, particularly in the areas of limited resources, gaps in faculty development, and insufficient practical and technological integration (Harden, 2007).
One major strength was the domain of program goals and outcomes, which achieved a score of 100%. This indicates clear alignment between educational objectives and national healthcare standards, enhancing motivation and competency-based learning (Harden, 2020; Harrison and Voi, 2016; Hershman and Voi, 2011). Competency-based frameworks have been shown to improve alignment with health service needs, producing better-prepared graduates. Furthermore, aligning learning outcomes with assessment ensures that students are equipped for real-world practice (Irby et al., 2010).
In contrast, curriculum delivery scored only 60%, suggesting outdated instructional methods and limited adoption of student-centered learning. The quality of clinical learning environments and interactive teaching methods are central to knowledge retention (Creswell, 2013; Deslauriers and Voi, 2019). Integrated and problem-based learning approaches, essential for fostering critical thinking and real-world application, remain underutilized (Dolmans and Voi, 2005; 2010; Jolly and Voi, 2017). Improvements in instructional design and teacher training are necessary to bridge these gaps (Jones and Voi, 2017).
The assessment and learning outcomes domain scored 80%, reflecting progress in evaluating student competencies. Effective assessment practices guide deeper learning (Kass and Voi, 2019; Kassahun and Zeleke, 2022; Kaufman, 2003), and programmatic assessment models that emphasize feedback and long-term improvement are beneficial (Kassebaum, 1992). Nonetheless, aligning assessments more closely with objectives and updating tools to reflect current competencies will enhance effectiveness.
The area of trainee selection, support, and alumni engagement, which also scored 80%, shows that while admission processes and student support structures exist, they require strengthening. Peer mentoring and academic counseling positively influence student success (Knowles et al., 2015). Alumni networks can support curriculum refinement and professional development through feedback and linkages (Kolb, 1984; Ladhani and Stevens, 2018). Expanding support systems and leveraging alumni engagement can therefore drive institutional growth.
Faculty recruitment and development was similarly rated at 80%. While the college recruits competent educators, there is a lack of structured pedagogical training. Educator burnout and limited professional development opportunities hinder instructional quality (Lake and Ryan, 2004; Lave and Wenger, 1991). Effective teaching requires both subject expertise and innovative educational strategies (McLean and Gibbs, 2009), which can be cultivated through ongoing training and institutional support (Miller, 1990).
Training facilities and resources received a strong 80% score, indicating adequate infrastructure. However, gaps remain in simulation labs, access to up-to-date medical literature, and digital resources. Simulation-based learning improves clinical preparedness (Mulugeta and Abegaz, 2021), while digital tools and clinical skills labs positively influence student performance (O’Brien et al., 2019; O’Neill and McMahon, 2005; Prideaux, 2003). Investment in modern teaching tools and facilities will further enhance student learning experiences.
The domain of industry extension and innovation, with a score of 60%, revealed weak institutional collaboration with external stakeholders such as hospitals and research centers. Academic-industry partnerships enhance curriculum relevance, innovation, and employability (Qureshi and Irfan, 2020; Regehr and Norman, 1996). Establishing formal partnerships can thus enrich training and research opportunities.
Stakeholder feedback on the accreditation process was broadly positive, with appreciation for its role in promoting benchmarks and continuous improvement (Salas et al., 2012; Sandars, 2009; Schön, 1983). However, financial and infrastructure limitations were commonly cited barriers. Underfunding of Ethiopian medical schools continues to hamper institutional development and innovation (Sargeant et al., 2008; Ten Cate and Scheele, 2007). Strategic resource mobilization and budgeting are therefore essential to sustain accreditation efforts.
Curricular responsiveness to emerging health trends was another concern. Participants stressed the need to integrate new technologies, public health priorities, and global disease patterns. Updating curricula to reflect evolving healthcare needs ensures graduate relevance (Teklehaimanot and Teklehaimanot, 2013; Teshome and Tegegne, 2020). Simulation and e-learning can bridge gaps between theory and practice in resource-constrained settings (Thistlethwaite et al., 2012).
A major limitation identified was the lack of structured faculty development. Despite academic qualifications, many instructors lack training in educational innovation. Administrative overload and weak institutional support hinder professional development (Thomas et al., 2016; van der Vleuten et al., 2012). Teaching quality declines without continuous pedagogical training (Wondimagegn and Tekle, 2022). Structured in-service training and rewards for teaching excellence are thus recommended.
Administrative and financial support showed partial progress, with improvements in coordination but persistent budget challenges. Underfunding leads to reduced innovation and low faculty morale (World Federation for Medical Education, 2015). Strengthening internal financial planning and seeking external funding are necessary to meet increasing academic demands.
Lastly, student involvement in quality assurance was found to be minimal. While students provide feedback via surveys, their participation in governance and curriculum reviews is limited. Involving students in quality assurance improves teaching practices and institutional responsiveness (Salas et al., 2012; McLean and Gibbs, 2009). The college should formalize student representation on academic and administrative committees to ensure transparency and inclusive decision-making.
4.1 Implications of findings
The findings highlight key areas where Adama Hospital Medical College (AHMC) can leverage its strengths, address existing gaps, and align its practices with global and regional standards. These implications span several dimensions:
4.2 Program goals and outcomes
4.2.1 Actionable steps
Adama Hospital Medical College’s (AHMC’s) perfect score (100%) in aligning with core medical education competencies, including professionalism, clinical skills, and evidence-based practice, highlights its strong foundation in meeting essential educational objectives.
To sustain this excellence, it is crucial to regularly update the curriculum to integrate emerging trends such as digital health, personalized medicine, and interdisciplinary collaboration. A dynamic and continuous curriculum review process will ensure the institution remains adaptable and responsive to the rapidly evolving healthcare landscape, maintaining its relevance and commitment to producing highly skilled medical professionals.
A score of 60% in curriculum delivery highlights a critical need for pedagogical reform, as the reliance on traditional lecture-based methods limits student engagement and learning outcomes.
To address this gap, it is essential to introduce innovative teaching strategies, including flipped classrooms, problem-based learning, and technology-enhanced education, which can foster a more interactive and effective learning environment. These recommendations emphasize the importance of proactive measures to enhance student engagement and ensure that AHMC remains a leader in medical education excellence, continually adapting to the needs of both students and the evolving healthcare landscape.
4.3 Study Limitations
This study provides valuable insights into the internal accreditation quality of the medical program at Adama Hospital Medical College. However, several limitations should be acknowledged:
• Reliance on self-reported data from faculty, students, and staff introduces potential biases, such as social desirability and misinterpretation of evaluation criteria.
• The findings are specific to AHMC’s unique context, resources, and size, limiting their generalizability to other institutions or regions without further validation.
• The cross-sectional design offers a snapshot of the accreditation process but restricts the ability to observe trends or establish causal relationships, which a longitudinal approach could address.
• Subjectivity in the use of a five-point scale may impact the consistency and reliability of ratings due to varied interpretations of criteria.
• The evaluation’s narrow scope, limited to nine standards, excludes critical dimensions such as student well-being, inter-professional collaboration, and community engagement.
• The exclusion of external stakeholder perspectives, including those of healthcare professionals and patients, further restricts insights into the program’s real-world impact.
• Internal accreditation processes may incentivize overly positive assessments, potentially inflating perceived strengths and underreporting weaknesses.
4.4 Strengths
The study benefits from a comprehensive evaluation framework that assesses nine key standards, providing a holistic view of the program’s quality across critical areas such as curriculum, assessment, trainer development, and governance. This broad approach not only highlights areas of strength but also identifies opportunities for improvement. The clear and structured methodology, using a five-point scale to rate each standard, facilitates objective comparisons and ensures that the results are both interpretable and actionable. Additionally, the study’s internal focus offers valuable insights into the program’s strengths and weaknesses from an institutional perspective, making it particularly useful for guiding targeted improvements.
5 Conclusion and recommendation
The internal accreditation assessment of Adama Hospital Medical College shows encouraging progress in educational planning, governance, and quality assurance. However, persistent gaps in curriculum delivery, infrastructure, faculty development, and industry collaboration must be addressed. These findings offer critical guidance for institutional leaders and policymakers committed to elevating the quality of medical education in Ethiopia.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics statement
This study received approval from the Institutional Review Board of Adama Hospital Medical College (Protocol Number: AHMC/StaffRes/2/9/2024). By ethical guidelines, written informed consent was obtained from all participants before their involvement in the study.
Author contributions
GA: Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft. FA: Project administration, Supervision, Validation, Visualization, Writing – review & editing. CM: Methodology, Project administration, Resources, Software, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We extend our sincere gratitude to the administration of Adama Hospital Medical College for their invaluable support throughout this internal accreditation evaluation. Our heartfelt thanks go to the medical students who generously participated in the survey, focus group discussions, and interviews, offering their time and honest perspectives. We are deeply appreciative of the faculty members and academic staff whose insights and contributions significantly enriched the qualitative component of this study. Special thanks to the Oromia Health Bureau and Mekelle University for their institutional backing, and to Makerere University for the technical and academic inspiration provided. We gratefully acknowledge the Foundation for Advancement of International Medical Education and Research (FAIMER) for its ongoing support in strengthening health professions education and promoting evidence-based academic leadership, which inspired the conceptual foundation of this study. Finally, we thank the data collectors, transcribers, and all research assistants whose dedication was instrumental to the successful completion of this work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aker, S. R., and Voi, J. (2014). Continuous quality improvement in medical education: a systematic review. Med. Educ. 48, 582–593. doi: 10.1111/medu.12425
Alemayehu, A., and Voi, J. (2023). A cross-sectional study of the current state of medical education in Ethiopia: challenges and opportunities. Ethiop. J. Health Dev. 37, 150–158. doi: 10.4314/ejhd.v37i2.7
Al-Eraky, M. M., and Voi, J. (2018). A framework for curriculum design in medical education: integration of competencies. Med. Educ. 52, 745–755. doi: 10.1111/medu.13583
Anderson, M., and Voi, J. (2019). The role of competency-based education in the future of medical training. Med. Educ. 53, 436–442. doi: 10.1111/medu.13850
Berhanu, T., and Voi, J. (2023). A review of medical school governance and curriculum integration in Ethiopia. Ethiop. J. Med. Educ. 35, 5–12. doi: 10.4314/ejme.v35i1.1
Berwick, D. M. (2003). Improving the quality of care: the pathway to reform. JAMA 289, 885–892. doi: 10.1001/jama.289.7.885
Biggs, J., and Tang, C. (2011). Teaching for quality learning at university. 4th Edn. Maidenhead, England: McGraw-Hill Education.
Bloom, B. S. (1956). Taxonomy of educational objectives: the classification of educational goals. Handbook I: Cognitive Domain. New York: David McKay Company.
Boud, D., and Falchikov, N. (2007). Rethinking assessment in higher education: learning for the longer term. London, New York: Routledge.
Brown, A., and Voi, J. (2018). Teaching medical ethics: a new paradigm in medical education. J. Med. Ethics 44, 380–384. doi: 10.1136/medethics-2018-104872
Buchan, J., and Voi, J. (2020). Global health workforce issues: a review of challenges and solutions. Health Policy Plan. 35, 848–858. doi: 10.1093/heapol/czaa062
Chen, Y., and Patel, V. (2020). The role of simulation in medical education: a comprehensive review. Med. Educ. 54, 125–133. doi: 10.1111/medu.14023
Clark, R., and Evans, D. (2019). Faculty development for medical educators: A review of effective strategies. J. Contin. Educ. Health Prof. 39, 84–90. doi: 10.1097/CEH.0000000000000227
Cohen, L., Manion, L., and Morrison, K. (2018). Research methods in education. 8th Edn. London: Routledge.
Creswell, J. W. (2013). Research design: qualitative, quantitative, and mixed methods approaches. 4th Edn. Thousand Oaks, CA: Sage Publications.
Deslauriers, L., and Voi, J. (2019). Measuring the impact of active learning on medical student learning outcomes. Adv. Physiol. Educ. 43, 1–5. doi: 10.1152/advan.00053.2019
Dolmans, D. H., and Voi, J. (2005). Problem-based learning: future challenges for educational practice and research. Med. Educ. 39, 732–741. doi: 10.1111/j.1365-2929.2005.02205.x
Entwistle, N. J. (2009). Teaching for understanding at university: Deep approaches and distinctive ways of thinking. Basingstoke, Hampshire, UK: Palgrave Macmillan.
Fenta, S. M., and Voi, J. (2023). Medical education reform in Ethiopia: the role of policy and institutional support. Ethiop. Med. J. 61, 25–32. doi: 10.4314/emj.v61i1.5
Fitzgerald, L., and Voi, J. (2011). Improving governance in healthcare organizations. Med. Manage. 35, 18–23.
Frank, J. R., and Voi, J. (2010). Competency-based medical education: theory to practice. Med. Educ. 44, 800–803. doi: 10.1111/j.1365-2923.2010.03716.x
Garcia, J. L., and Miller, R. A. (2019). Integrating interprofessional education in medical curricula: challenges and opportunities. Med. Educ. 53, 757–765. doi: 10.1111/medu.13781
Garrison, D. R., and Vaughan, N. D. (2008). Blended learning in higher education: framework, principles, and guidelines. San Francisco, CA: Jossey-Bass.
Girma, M., and Voi, J. (2023). Implementing competency-based medical education in Ethiopian medical schools: An assessment of current practices. J. Ethiop. Med. Educ. 35, 120–128. doi: 10.4314/ejme.v35i2.2
Green, J., and Thorogood, N. (2018). Qualitative methods for health research. 4th Edn. London: Sage Publications.
Harden, R. M. (2007). The integration of medical education: strategic approaches. Acad. Med. 82, 386–392. doi: 10.1097/ACM.0b013e3180338f88
Harden, R. M. (2020). The future of medical education: from curriculum design to clinical teaching. Med. Educ. 54, 321–329. doi: 10.1111/medu.14192
Harrison, J., and Voi, J. (2016). Collaborations between academia and industry: a strategy for the future of medical education. J. Res. Med. Educ. 18, 112–120.
Hassan, M., and Ali, M. (2021). The future of medical education in low-resource settings: a perspective from Ethiopia. Global Health Educ. 23, 321–328.
Hershman, D. M., and Voi, J. (2011). Mentorship in medical education: a review. J. Med. Educ. 20, 28–32.
Irby, D. M., Cooke, G. E., O’Brien, J. A., and Voi, J. (2010). Educating physicians: a call for reform of medical school and residency. New York, NY.
(2010). Teaching and learning in medical education: a review of recent developments. J. Gen. Intern. Med. 25, 380–384. doi: 10.1007/s11606-010-1220-4
Jolly, B., and Voi, J. (2017). Access to learning resources and academic performance in medical education. Acad. Med. 92, 1047–1054. doi: 10.1097/ACM.0000000000001801
Jones, P., and Voi, J. (2017). Exploring the effectiveness of online learning in medical education. Med. Educ. 51, 345–353. doi: 10.1111/medu.13208
Kass, L., and Voi, J. (2019). Trainer development and teacher satisfaction in medical education. Med. Educ. 53, 556–564.
Kassahun, A., and Zeleke, A. (2022). Implementation of problem-based learning in Ethiopian medical schools: achievements and barriers. Ethiop. J. Health Sci. 32, 45–52. doi: 10.4314/ejhs.v32i1.6
Kassebaum, D. G. (1992). Change in medical education: the courage and will to change. Acad. Med. 67, 659–661. doi: 10.1097/00001888-199210000-00001
Kaufman, D. M. (2003). ABC of learning and teaching in medicine: applying educational theory in practice. BMJ 326, 213–216. doi: 10.1136/bmj.326.7382.213
Knowles, M. S., Holton, E. F., and Swanson, R. A. (2015). The adult learner: the definitive classic in adult education and human resource development. 8th Edn. New York, London: Routledge.
Kolb, D. A. (1984). Experiential learning: experience as the source of learning and development. Englewood Cliffs, New Jersey: Prentice Hall.
Ladhani, Z., and Stevens, F. J. (2018). Global health training in Ethiopian medical education: a critical review. Ann. Glob. Health 84, 421–429. doi: 10.29024/aogh.2297
Lake, D. A., and Ryan, M. R. (2004). Teaching anatomy using problem-based learning: lessons from experience. Med. Educ. 38, 447–448. doi: 10.1046/j.1365-2923.2004.01894.x
Lave, J., and Wenger, E. (1991). Situated learning: legitimate peripheral participation. Cambridge, UK: Cambridge University Press.
McLean, M., and Gibbs, T. J. (2009). Twelve tips to designing and implementing a learner-centred curriculum: prevention is better than cure. Med. Teach. 31, 650–653. doi: 10.1080/01421590903049838
Miller, G. E. (1990). The assessment of clinical skills/competence/performance. Acad. Med. 65, S63–S67. doi: 10.1097/00001888-199009000-00045
Mulugeta, T., and Abegaz, T. (2021). Clinical training challenges among Ethiopian medical students: a qualitative study. BMC Med. Educ. 21:495. doi: 10.1186/s12909-021-03000-1
O’Brien, B. C., Poncelet, A. N., and Irby, D. M. (2019). Clinical learning environments and professional identity formation: a framework for medical educators. Acad. Med. 94, 1610–1615. doi: 10.1097/ACM.0000000000002863
O’Neill, G., and McMahon, T. (2005). “Student-centred learning: what does it mean for students and lecturers?” in Emerging issues in the practice of university learning and teaching. eds. G. O’Neill, S. Moore, and B. McMullin (Dublin, Ireland: AISHE), 27–36.
Prideaux, D. (2003). ABC of learning and teaching in medicine: curriculum design. BMJ 326, 268–270. doi: 10.1136/bmj.326.7383.268
Qureshi, M. A., and Irfan, A. (2020). Impact of flipped classroom model on student engagement and academic performance in medical education. Med. Sci. Educ. 30, 835–842. doi: 10.1007/s40670-020-00975-4
Regehr, G., and Norman, G. R. (1996). Issues in cognitive psychology: implications for professional education. Acad. Med. 71, 988–1001. doi: 10.1097/00001888-199609000-00015
Salas, E., Tannenbaum, S. I., Kraiger, K., and Smith-Jentsch, K. A. (2012). The science of training and development in organizations: what matters in practice. Psychol. Sci. Public Interest 13, 74–101. doi: 10.1177/1529100612436661
Sandars, J. (2009). The use of reflection in medical education: AMEE Guide No. 44. Med. Teach. 31, 685–695. doi: 10.1080/01421590903050374
Sargeant, J., Mann, K., van der Vleuten, C., and Metsemakers, J. (2008). Reflection: a link between receiving and using assessment feedback. Adv. Health Sci. Educ. 13, 275–287. doi: 10.1007/s10459-006-9048-4
Schön, D. A. (1983). The reflective practitioner: how professionals think in action. New York: Basic Books.
Teklehaimanot, H. D., and Teklehaimanot, A. (2013). Human resource development for health in Ethiopia: challenges of achieving the Millennium Development Goals. Ethiop. J. Health Dev. 27, 1–6. doi: 10.1186/1478-4491-11-39
Ten Cate, O., and Scheele, F. (2007). Competency-based postgraduate training: can we bridge the gap between theory and clinical practice? Acad. Med. 82, 542–547. doi: 10.1097/ACM.0b013e31805559c7
Teshome, S., and Tegegne, B. (2020). Innovations in assessment: use of OSCE in Ethiopian medical education. Ethiop. Med. J. 58, 35–42. doi: 10.11648/j.ijae.20200504.14
Thistlethwaite, J. E., Davies, D., Ekeocha, S., Kidd, J. M., MacDougall, C., Matthews, P., et al. (2012). The effectiveness of case-based learning in health professional education: A BEME systematic review. Med. Teach. 34, e421–e444. doi: 10.3109/0142159X.2012.680939
Thomas, P. A., Kern, D. E., Hughes, M. T., and Chen, B. Y. (2016). Curriculum development for medical education: a six-step approach. 3rd Edn. London: Sage Publications.
van der Vleuten, C. P. M., Schuwirth, L. W. T., Driessen, E. W., Dijkstra, J., Tigelaar, D., Baartman, L. K. J., et al. (2012). A model for programmatic assessment fit for purpose. Med. Teach. 34, 205–214. doi: 10.3109/0142159X.2012.652239
Wondimagegn, D., and Tekle, T. (2022). Contextualizing global health competencies in Ethiopian medical education. Ethiop. J. Health Sci. 32, 211–218. doi: 10.4314/ejhs.v32i2.10
World Federation for Medical Education. (2015). WFME global standards for quality improvement: basic medical education. Ferney-Voltaire, France: WFME Office. World Federation for Medical Education. Available online at: https://wfme.org/standards/bme/.
Keywords: internal accreditation, medical education quality, Adama Hospital Medical College, student satisfaction, curriculum alignment, Ethiopia
Citation: Arero G, Amdeslasie F and Mwesigwa C (2025) Evaluating internal accreditation quality in medical education: perspectives of students, faculties, and stakeholders at Adama Hospital Medical College, Adama, Ethiopia, 2024. Front. Educ. 10:1552865. doi: 10.3389/feduc.2025.1552865
Edited by:
Sri Suryanti, Surabaya State University, IndonesiaReviewed by:
Antonella Nuzzaci, University of Messina, ItalyMobin Sokhanvar, Khoy University of Medical Sciences, Iran
Copyright © 2025 Arero, Amdeslasie and Mwesigwa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Godana Arero, Z2FyZXJvMjAxNUBnbWFpbC5jb20=
 Godana Arero
Godana Arero Faska Amdeslasie2
Faska Amdeslasie2