- Department of General Practice, University Hospital Würzburg, Würzburg, Germany
Background: Weight bias and stigma are prevalent problems in health care professionals and medical students. They have consequences on care quality and, thus, on health of patients with overweight and obesity. We implemented a new course unit “Prevention and Counseling for Weight Management” thematizing the etiology of weight gain and weight stigma. The purpose of this study was to evaluate changes in students' weight-related attitudes after a structured educational intervention.
Methods: We used an inverted classroom design: a theoretical module for self-study followed by a practical module in presence. This evaluation study investigated the weight bias and causal attribution of 213 medical students (73.7% female) in the 6th semester. Students completed a questionnaire before and after the course, including the Fat Phobia Scale (FPS) and ratings of causal attribution. Questionnaires were generated with EvaSys©. We used t-tests, ANOVAs and Pearson correlations for analysis.
Results: About 96% of the students showed negative attitudes. We found an averaged weight bias in students (FPS = 3.63) and a small decrease in weight bias after the course (FPS = 3.44). The students categorized internal factors as the most important cause of weight gain. After the course, internal factors decreased while external factors increased in relevance. As not intended, biological factors of weight attribution decreased in relevance.
Conclusions: The majority of our students showed weight bias. Medical education like our course can help to reduce negative weight-related attitudes. Curricula and clinical trainings should address weight bias to raise awareness and improve health care for patients with higher weight.
1 Introduction
Overweight and obesity represent one of the most significant public health challenges of our time (WHO, 2024; Schienkiewitz et al., 2022). According to the World Health Organization, 43% adults worldwide are overweight and 16% adults live with obesity (WHO, 2024). In Germany, about 34.5% adults are overweight and 19% live with obesity (Schienkiewitz et al., 2022). A higher body weight is related to an increasing risk for several serious physical health problems, e.g., cardiovascular diseases or type 2 diabetes (Collaborators, 2017; Donini et al., 2020; Kloock et al., 2023). Further, weight-related bias and stigma are prevalent psychosocial consequences of overweight and obesity (Spahlholz et al., 2016). Weight bias can be defined as negative beliefs about and negative attitudes toward individuals due to their weight. Weight bias and prejudice lead to weight stigma that appears in negative social stereotypes and further in weight-related devaluation, exclusion and discrimination (WHO, 2017). In western societies, higher weight is often associated with, e.g., laziness, a lack of discipline, willpower and motivation (Puhl and Heuer, 2009). As one explanation for weight stigma, these negative stereotypes result from the distorted assumptions that higher weight is a lifestyle problem that is mostly under the individuals' control. Internal factors (e.g., personality, low motivation) are predominantly used as explanations for higher body weight, while external or biological factors are given less consideration (e.g., environment, genes) (Puhl and Heuer, 2009; Pantenburg et al., 2012). Thus, individuals living with overweight or obesity are blamed for their weight due to personal failure (Mata and Hertwig, 2018).
Experiencing weight stigmatization has far-reaching health consequences for individuals. Particularly, it is associated with mental health outcomes as, e.g., a higher risk for depression, anxiety, suicidality, eating disorders, body dissatisfaction and low self-esteem (Daly et al., 2020; Puhl et al., 2020; Emmer et al., 2020). Further, persistent or repeated stigmatization as a chronic stress factor can lead to dysfunctional physiological (e.g., increased cortisol and inflammation) and behavioral changes (e.g., stress regulation through eating, avoiding activity) associated with gaining or maintaining weight, resulting in a vicious circle (see Figure 1) (Puhl et al., 2020; Tomiyama et al., 2018; Sikorski et al., 2015; Major et al., 2014; Schvey et al., 2011; Vartanian and Shaprow, 2008). The individual health consequences of weight stigmatization also lead to consequences for the society. Delayed or inadequate medical treatment or new health problems caused by stigmatization can result in higher and avoidable healthcare costs. Further, the inability to work due to health impairments causes additional costs for the society (Singh et al., 2019).
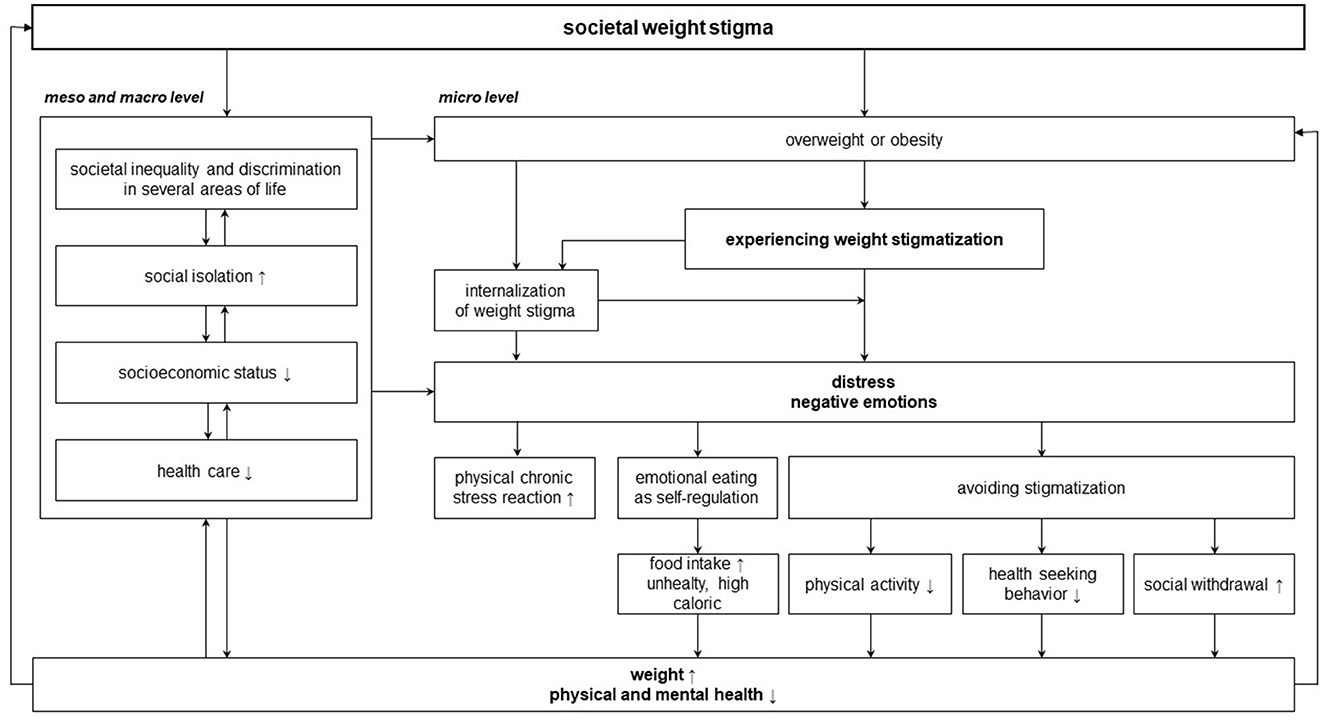
Figure 1. Vicious circle of weight stigma on the micro level, meso and macro level (adapted by Major et al., 2017).
Weight stigma can be found in different settings, also in the health care setting among various health care professions like primary care physicians and among medical students (Pantenburg et al., 2012; Tomiyama et al., 2018; Phelan et al., 2015; Miller Jr et al., 2013; Lawrence et al., 2021; Puhl et al., 2014). Physicians with biased attitudes are more likely to prejudge patients with higher weight as being not self-controlled, will-weak, and unmotivated to improve health and less adherent to medication (Ferrante et al., 2006; Glauser et al., 2015; Huizinga et al., 2009; Ruelaz et al., 2007). Further, studies demonstrate that weight stigma in physicians has a negative impact on interpersonal and technical quality of their health care work (Puhl and Heuer, 2009; Phelan et al., 2022; Puhl and Brownell, 2013). Physicians use patient-centered communication less frequently, spend less contact time and provide less educational information to patients with higher weight (Pantenburg et al., 2012; Phelan et al., 2015; Huizinga et al., 2009; Hebl and Xu, 2001). Patients experience negative judgements for their weight, banal weight loss advice and a lack of respect, compassion, understanding and empathy in primary care settings (Ferrante et al., 2006; Ananthakumar et al., 2020; Farrell et al., 2021; Gudzune et al., 2014; Anderson and Wadden, 2004; Brown et al., 2006). Thus, patients often delay or avoid prevention care due to weight stigma (Ferrante et al., 2006; Alegria Drury and Louis, 2002; Wee et al., 2000). The negative influence of experienced stigmatization on health seeking behavior may lead to late or irregular medical care visits. That may end up in a deterioration of their health and increased morbidity and mortality (see Figure 1, adapted by Major et al., 2017) (Phelan et al., 2022; Alberga et al., 2016; Mensinger et al., 2018).
Several studies have shown that also medical students have stigmatizing attitudes toward patients with higher weight and attributed overweight on internal factors (Pantenburg et al., 2012; Miller Jr et al., 2013; Puhl et al., 2014; Persky and Eccleston, 2011; Phelan et al., 2014). A study revealed the role of model learning: Medical students, who perceived negative attitudes about patients with obesity to be normative in medical school, showed poorer patient-centered behavior, like less friendliness, attentiveness, respectfulness and interactivity when interacting in a role play with a role patient with obesity (Phelan et al., 2021). These findings fit with the fact that current medical school curricula still do not adequately address the problem of stigmatization of obesity and the treatment of obesity (Bowden and Petty, 2024). As medical students will be the next generation of doctors, their attitudes influence highly the working with patients in future practice. The results illustrate the need to raise awareness to weight stigma in medical schools to reduce weight stigmatization of students and lately to improve quality of care for patients living with higher weight. Further, the results also require early and longitudinal interventions in medical training from medical studies to practice would be helpful to reduce weight stigma and even improve weight-related treatments (Bowden and Petty, 2024; Talumaa et al., 2022).
Some studies reported interventions like lecture modules (Renold et al., 2023), podcast episodes (Heidebrecht et al., 2024), e-learnings and videos with vignettes (Koran-Scholl et al., 2023). However, more evidence is needed to identify relevant factors of effective educational interventions reducing weight stigma. While some studies reported positive effects of interventions, others did not (Alberga et al., 2016). Beside theoretical knowledge, experts recommend interventions on weight stigma should include experiences of those affected and evoke empathy (Bowden and Petty, 2024).
In order to deal with the reported and often unconscious mechanisms of weight stigma, the Department of General Practice, University Hospital Würzburg (UKW), implemented a new course unit that addressed weight counseling and weight stigmatization.
Studying medicine in Germany takes 6 years and ends with a state examination. Two years of basic science are followed by 3 years of clinical studies with theory and patient contact. The final year takes place exclusively in a clinical context.
In this study, we want to investigate the attitudes and causal attributions of medical students as well as the changes after participating in the new course unit. We also aim to evaluate the course regarding its effectiveness to reduce weight bias and improve knowledge and counseling skills. First, we hypothesized that medical students show negative weight-related attitudes and attribute higher weight to internal rather than external or biological factors. Secondly, we assumed a decrease of negative attitudes and internal attribution as well as an increase of external and/or biological attribution during the course. Finally, we supposed an improvement of knowledge about overweight and obesity and counseling skills.
2 Methods
2.1 Study design
This evaluation study in a pre-post-design examined the weight bias of medical students of the 6th semester. We introduced a new seminar unit “prevention and counseling for overweight and obesity” based on already successful implemented courses for themes of nicotine and alcohol that has been part of existing teaching subject on “prevention and health promotion” (Lauerer et al., 2021). The course unit was structured in two modules in an inverted classroom format (blended learning), combining online educational material for self-study and traditional place-based classroom methods. The piloting of the course unit took place in winter semester 2022/23 and in summer semester 2023.
In module 1, students acquired theoretical knowledge through an asynchronous e-learning module (knowledge content; see “study materials” and Supplementary material 1). The processing time was about 90 min. Before starting module 1, students had to complete the online weight bias questionnaire (weight bias questionnaire pre; see “materials” and Supplementary material 2). Afterwards, they evaluated the module (evaluation questionnaire module 1; see “materials” and Supplementary material 3a). Digital questionnaires were technically implemented via EvaSys©.
Four to seven weeks later, students participated in the course unit of module 2 in presence. The course unite about obesity lasting 30 min. Here, students practiced a counseling role play in small groups of three students (instructions of role play obesity; see Supplementary material 4) after a short theoretical input about the 5A counseling model (WHO, 2014) in weight management. After the course, the same weight bias questionnaire (see “materials” and Supplementary material 2) was completed again as well as an evaluation questionnaire for module 2 (evaluation questionnaire module 2; see “materials' and Supplementary material 3b). Questionnaires were in a paper-pencil-format.
2.2 Study sample
A total of 291 students participated in the course (winter 22/23: n = 148, 50.9%; summer 23: n = 143, 49.1%). The pre- and post-questionnaire data were successfully matched using individual codes for 213 students (73.2% of all students; winter 22/23: n = 111; summer 23: n = 102). Matching was not possible for 38 pre-questionnaires (13.1%) and 40 post-questionnaires (13.7%). Consequently, 42 unmatched cases were excluded from the analysis. For detailed information, see Supplementary material 5.
2.3 Study materials
2.3.1 Learning material
The e-learning (module 1) was created with the online tool Prezi© (Prezi.com). Theoretical basics were imparted about obesity, prevention and the 5A counseling model. The 5A model (ask, advise, assess, assist, arrange WHO, 2014) is a widely used brief verbal intervention for smoking cessation and for other behavioral changes. It is based on the concept of Motivational Interviewing according to Miller and Rollnick (2012) and is used for supporting patients in behavioral change (Batra et al., 2015; Panel, 2008). The topic of “weight bias and stigmatization” addressed the contexts in which weight stigmatization occurs (particularly in health care), the underlying causes, the consequences, and prevention. The learning material included multimedia elements like videos and podcasts. In the present course of module 2, students practiced a role play according to the 5A model for a counseling of weight management. Each group consisted of three students with the roles of a patient, a (last-year-) student working in a primary care setting and an observer. Beforehand, students were sensitized for the perspective of a patient with higher weight in context of a consultation through a power point presentation (see Supplementary material 1). Psychological and medical docents and student-tutors supervised the role plays.
2.3.2 Weight bias questionnaire (WBQ)
The questionnaire (Supplementary material 2) was developed referring to other studies (Pantenburg et al., 2012; Schwenke et al., 2020; Sikorski et al., 2012). It was structured into three sections and contained 29 items.
- Demographic: Students were asked for an individual matching code and sociodemographic variables including age, gender, and weight categories (BMI range).
- Fat Phobia Scale: Weight-related attitudes toward obesity were measured with the German adaption of the short form of the Fat Phobia Scale (FPS) (Bacon et al., 2001; Stein et al., 2014). The FPS is a well-established questionnaire for examining beliefs and attitudes toward people with higher weight. Each of the 14 items shows an opposite pair of adjectives on a scale from 1 to 5 (e.g., attractive vs. unattractive; willpower vs. no willpower). Previous research used a cut off about a mean score ≥ 2.5, that indicated mainly negative weight-related attitudes. The higher the mean score, the higher the negative attitudes tendency toward obesity (Sikorski et al., 2012).
- Causal Attribution: The attribution of causes of obesity were rated on a 5-point-likert scale (1 = not relevant at all for causing obesity, 5 = highly relevant for causing obesity). Referring to other studies (Puhl and Heuer, 2009; Panel, 2008), there were 11 possible causes of obesity from different factors: internal factors (e.g., lack of willpower and discipline), external factors (e.g., oversupply of food), biological factors (e.g. hormonal and genetic factors) and knowledge factors (e.g. missing knowledge about food) (see also Supplementary material 6).
2.3.3 Evaluation questionnaire module 1 and 2
The 19-item questionnaire (Supplementary material 3) contained single- and multiple-choice questions, 5-point Likert- and 6-point scales and open questions. There were questions about overall grade (German school grade: 1 = very good, 6 = insufficient), subjective learning success (5-point Likert scale) for a current assessment and a retrospective assessment before the course and a separate feedback for the new introduced unit ‘obesity'.
2.4 Statistical analysis
The statistical analyses were performed using SPSS® Statistics (IBM®, Version 24.0) (Corp. I., 2016) and R Version 4.3.2 (Team, 2020). Two cases were excluded because more than 3 items were missing in the Weight Bias Questionnaire (WBQ). Due to a transmission error, the item 14 of the FPS in the post WBQ of the two first courses in winter semester 22/23 was systematically missing for 44 cases. For these cases, we calculated the FPS score only for 13 items of the scale. To check the randomness of other missing values, the MCAR (Missing completely at random) test according to Little was performed (Little, 1988). Missing values of the data showed unsystematic patterns. Due to the sample size, we assumed that parametric analysis was appropriated if variables were not normal distributed. For reliability analysis, Cronbach's alpha was calculated to assess the internal consistency of the FPS and causal attribution factors (see Supplementary material 7).
For the analysis of weight bias and causal attribution, the mean FPS scores before and after the course unit as well as mean scores of causal attribution factors (internal factors with additionally subfactors: energy balance, personal factors; external factors; biological factors; knowledge factors) were calculated (see Supplementary material 6) (Schwenke et al., 2020). Data were analyzed descriptively for gender, age, BMI (categories: < 18.5 underweight, 18.5–24.9 normal weight, 25–29.9 overweight, ≥ 30 obesity), FPS scores and causal attribution factors.
We used ANOVA with repeated measures and non-parametric tests to analyse the FPS and causal attributions of higher weight as well as correlations of attitudes and causal attributions. For more details regarding test requirements, see Supplementary material 7.
2.5 Data management and privacy police
The study was approved of by the Ethics committee of the University of Würzburg, Germany (Reference number: 20230704 02). The participation was voluntary and pseudonymised with individual codes. After matching, codes were deleted so that it was no longer possible to draw conclusions about the identity. Students were informed about study theme, and a return of completed questionnaire was taken as consent to participate in the study.
3 Results
3.1 Characteristics of the sample
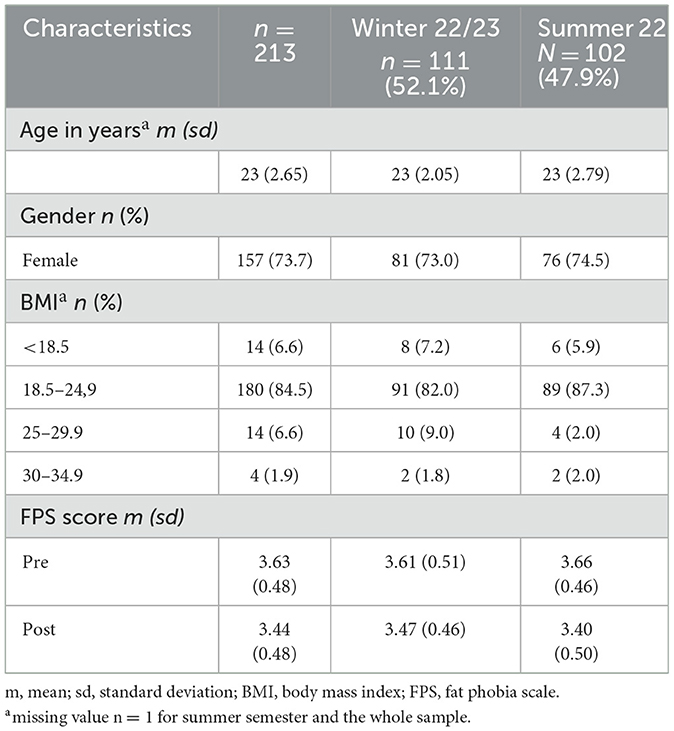
The mean age of the matched sample was 23 years, 73.7% were female, and 84.5% (n = 180) had a normal weight. Table 1 shows further sample information. The response rate was 88%. There were no differences between the semesters regarding to age, gender and BMI (all p ≥ 0.100) for matched data.
3.2 Weight-related attitudes
The mean FPS score for the sample with matched pre- and post-data (n = 213) was 3.63 (SD = 0.48) at the start and 3.44 (SD = 0.48) after the course unit. Before the course, approximately 96.7% of students had a mean score of ≥ 2.5, compared to 95.3% after the course.
A two-way ANOVA with repeated measures [factors: 1. FPS (pre, post), 2. semester (winter 22/23, summer 23)] revealed that there was no difference between the semesters (F(1, 211) = 0.38; p = 0.846) regarding their FPS score. There was no interaction between semester and measure time (pre, post) (F(1, 211) = 3.304, p = 0.071). The comparison of the FPS scores before and after the course unit showed a small but significant effect (F(1, 211) = 36.80, p = 0.001, η2 = 0.149). After the course, the FPS scores were lower than before. Further, the Kruskal-Wallis test demonstrated no significant results (pre: H(2) = 0.246, p=.884; post: H(2) = 1.929, p = 0.384). After correction the Wilcoxon tests showed significant differences in FPS scores over time for normal weight (Z = −6.69, p = 0.003), but not for underweight (BMI < 18.5; Z = −2.36, p = 0.054) and overweight (BMI ≥ 25; Z = −0.131, p > 0.999). A two-way robust ANOVA with repeated measures [factors: 1. FPS (pre, post), 2. gender (female, male)] showed changes over time (F(1, 134.65) = 28.53, p < 0.001, η2 = 0.126) and a difference between female and male participants (F(1, 152.46) = 13.74, p < 0.001, η2 = 0.043). Male students showed higher FPS scores compared to female students. The interaction of time and gender was not significant (p = 0.666).
3.3 Causal attribution
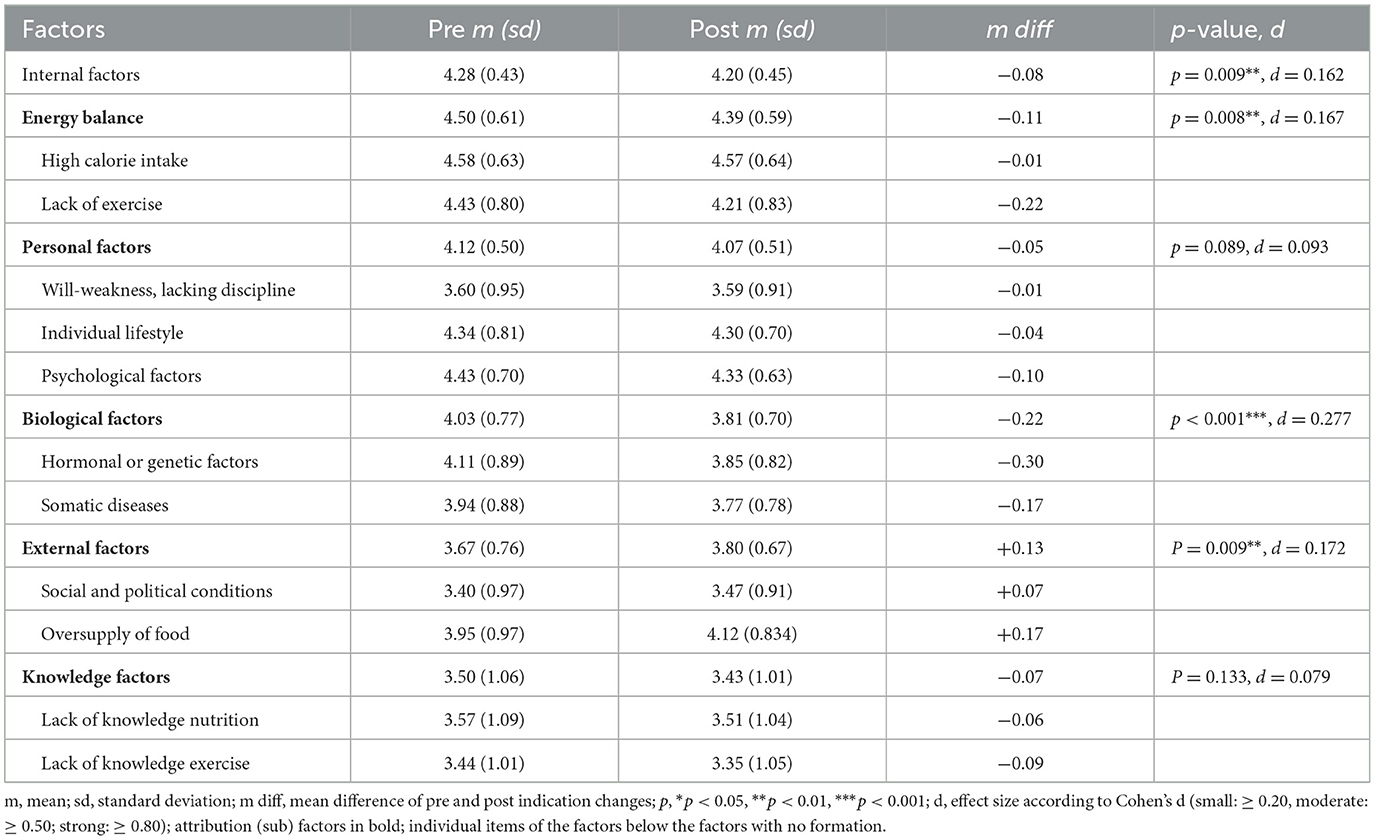
A two-way ANOVA with repeated measures [factors: 1. causal attribution factor over time (pre, post), 2. comparison of causal attribution factors (internal, external, biological, knowledge)] revealed a significant main effect for time and for causal attribution factor (time: F(1, 212) = 4.233, p = 0.041; causal attribution: GG: F(2.43, 515.84) = 65.150, p < 0.001). Causal attribution ratings changed over time and relevance ratings of causal attribution factors differ. Also the interaction effect was significant (GG: F(2.44, 517.87) = 8.131, p < 0.001). The changes of causal attribution over time was dependent on the attributional factors.
The post-hoc comparison of the simple main effect “time” showed a significant decrease of attribution on internal factors and biological factors and a significant increase of attribution on external factors. The ratings for each factor and results of the t-tests are presented in Table 2 and Figure 2.
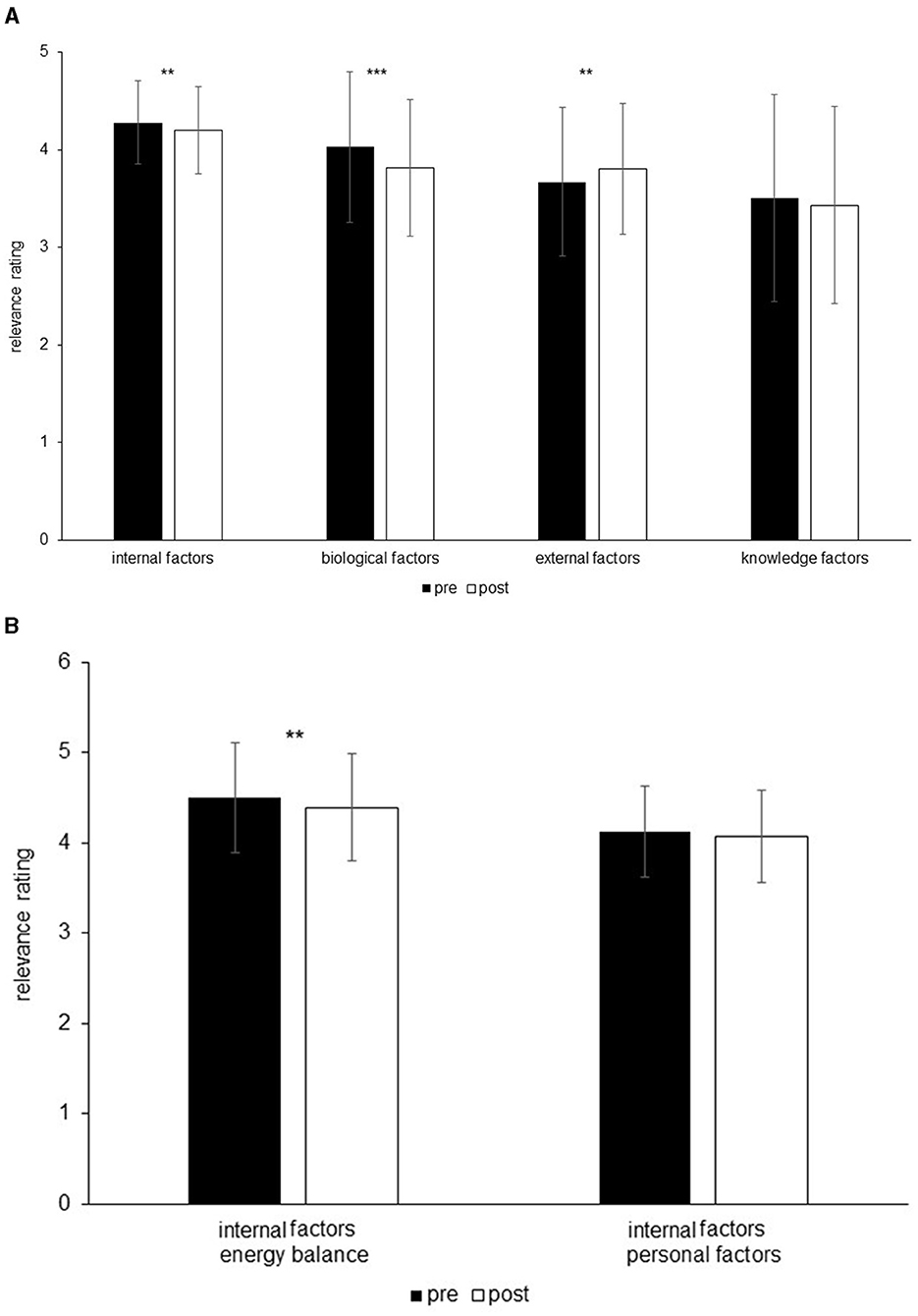
Figure 2. Causal attribution factors over time (A) and subfactors of intern attribution factors over time (B). p: **p < 0.01, ***p < 0.001.
The analysis of a simple main effect (differences between the causal factors) before and after the course unit was significant (pre: GG: F(2.52, 534.18) = 51.776, p < 0.001, η2 = 0.126; post: GG: F(2.33, 494.62) = 46.786, p < 0.001, η2 = 0.181). In holm-corrected post-hoc tests, all factors before the course differed significantly from each other (p ≤ 0.013). After the course, all causal factors except biological factors and external factors (p = 0.914) differed significantly from each other (all other p < 0.001).
3.4 Relation of fat phobia scale and causal attribution
The correlative analysis revealed small significant correlations between the mean score of the Fat Phobia Scale and mean score of attribution factors. Significant correlations can be found in Table 3.
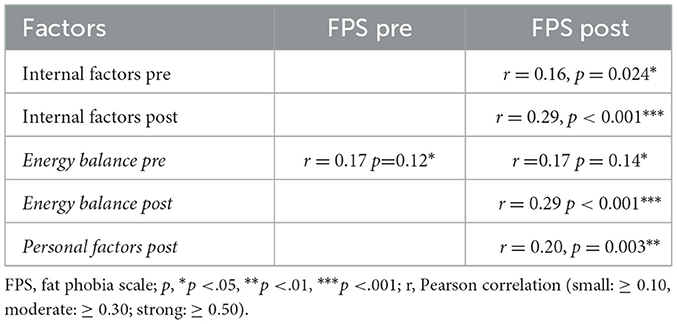
Table 3. Significant Pearson correlation of causal attribution factors and FPS for both measure time points (n = 213).
The changes over time for each variable were also correlated. Here, mean score changes of the FPS and mean score changes of the factor “personal internal causes” showed small but significant correlations (r = 0.148, p = 0.031).
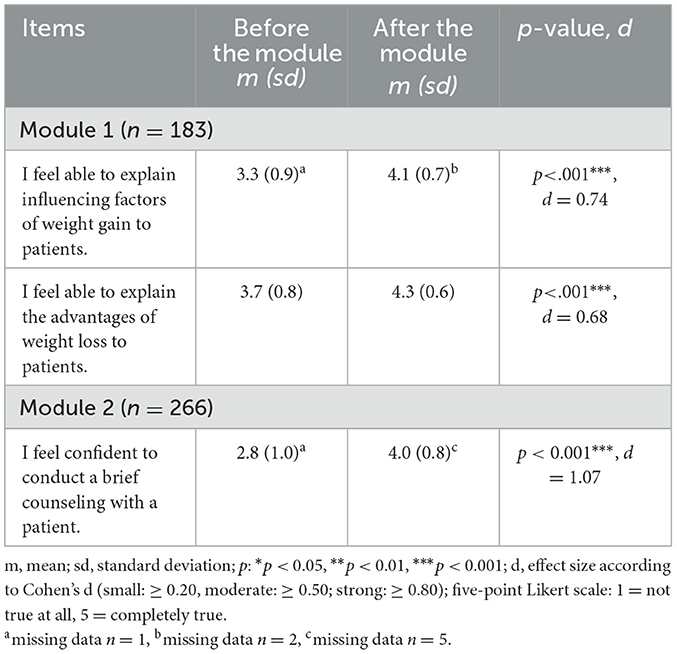
3.5 Evaluation of the course
The theoretical module 1 received the German school grade “good” (n = 180, md = 2; ratings from 1 = “very good” to 6 = “insufficient”). The course expanded students' theoretical and practical knowledge. Students reported that they were interested in the topic “overweight and obesity” and rated it as practically relevant for them. After completing the asynchronous e-learning (Module 1), students reported a significant improvement in their ability to explain the factors influencing weight gain and the benefits of weight loss (Table 4). After the module 2, the students felt significantly more confident to conduct a brief counseling with a patient regarding weight management. About 88% of the students (n = 241) recommended offering the course unit again next semester, while 2.6% (n = 7) did not recommend it, and 5.8% (n = 16) chose not to respond. For detailed information, see Tables 4, 5.
4 Discussion
This study assessed weight bias and the causal attribution of weight among 6th semester medical students and explored changes in weight-related attitudes following the introduction of a new course unit titled “Prevention and Counseling for Overweight and Obesity”.
4.1 Weight-related attitudes on the fat phobia scale
In our study, about 96.7% of the students showed negative attitudes toward people with overweight and obesity before the course. The Fat Phobia Scale (FPS) mean score before the learning intervention can be interpreted as an average level of “fat phobia” (Bacon et al., 2001). This score is comparable to the general population (Stein et al., 2014) and to the results of other studies. In a German study, Pantenburg and colleagues showed similar stigmatization attitudes in medical students (Pantenburg et al., 2012). Also an American study with medical students found similar results (Nestorowicz and Saks, 2021). A systematic review and meta-analysis calculated a similar pooled FPS mean score of five studies among different health care professions. Healthcare professionals and medical students, as observed in our study, exhibited weight-related negative attitudes comparable to those found in the general population, suggesting that medical knowledge and training alone do not necessarily prevent discriminatory tendencies (Pantenburg et al., 2012). Other studies suggest the social acceptance and commonly expression of weight-related stigmatization in clinical practice and medical training, so students may perceive weight bias as normal and acceptable in the health care system (Puhl et al., 2014; Wear et al., 2006).
We found differences in weight-related attitudes between gender: Male students showed a higher mean score than female students. This gender-related finding is consistent with other studies (Schwenke et al., 2020; Puhl et al., 2008, 2015). Perhaps, women are more aware of prejudice and discrimination because they are more affected by weight-related stigmatization themselves (Puhl et al., 2008), or women use more implicit stigmatization and therefore show lower scores in explicit measurements as in our study (Schwartz et al., 2003). Results might suggest that our intervention was only effective for students with normal weight. However, the non-significant effects for the underweight and overweight groups could also be due to the small sample sizes in these groups. Regardless of our results, studies have found no differences in stigmatization depending on the BMI (Pantenburg et al., 2012; Hilbert et al., 2013). Following the social identity theory (Tajfel, 1979), people evaluate their own social group more positive than other groups. One might expect that people with higher BMI show less weight stigma. In general, the findings of the link between weight stigma and own weight were mixed. When interpreting such results, it is important to consider the characteristics of the sample and the context of the study. German medical students are a very selected population – children of academics and rarely obese. Further, the region of the population has an influence on weight bias. For example, a study showed lower weight bias in high-obese regions (Berkessel et al., 2024). Previous research pointed out that this in-group-effect is complex and depends on several factors like perceived weight, in-group identification and concerning about their group status (Standen et al., 2024; Brochu et al., 2020).
4.2 Causal attribution of higher weight
In our study, students rated internal factors as more relevant for gaining weight than biological and external factors. The internal sub factor “energy balance” was more important for the students than the sub factor “personal factors”. Biological factors were the second most relevant followed by external factors. These findings are in line with those of previous studies with medical students and physicians (Pantenburg et al., 2012; Mata and Hertwig, 2018; Schwenke et al., 2020). The results may indicate an attributional bias that describes the tendency to overestimate internal, personal causes, that seem controllable, and to disregard external, situational causes: Body weight is perceived as controllable, and the responsibility for that is primarily attributed to the individual, while the “choices” or “opportunities” that individuals have to lose weight are overestimated (Mata and Hertwig, 2018; Crandall et al., 2001). Although a positive energy balance contributes to weight gain, the etiology of overweight and obesity consists of complex, multifactorial pathophysiological mechanisms (Pantenburg et al., 2012). The relevance of genetic and environmental factors and their interaction is still underestimated. Several prior findings support this bias through the association of internal attribution and more negative attitudes as well as the association of biological attribution and more positive attitudes (Schwenke et al., 2020). Our results show a small positive relation between the relevance of internal factors and negative attitudes. In contrast to previous studies, the descriptive ratings of “hormonal and genetic factors” were higher than the ratings of “will-weakness and lack of discipline”. This may indicate that has already been some awareness of the biological influence toward weight among our students.
4.3 Changes of weight-related attitudes after the course
The small but significant reduction of stigmatizing attitudes after our course may emphasize a sensitization of weight-related stigmatization through the course unit.
Alegria Drury and Louis (2002) named four approaches to reduce weight bias: the information approach, the lived experience approach, the self-reflection approach and the role model approach. In our course unit, we used elements of the information, lived experience and self-reflection approach (e.g., presentation with information, questions, videos, role play). We focused on teaching the complex, multifactorial etiology of weight gain and pointed out the relevance of biological and external factors.
Several studies showed the effectiveness of educational strategies (e.g., lecture) in reducing weight stigmatization among medical students (Alberga et al., 2016). Especially teaching the uncontrollable causes of obesity decreased implicit weight bias. Nevertheless, there are also studies showing no effect (Alberga et al., 2016). A reason for the small change in attitudes may be the temporal stability of (implicit) attitudes (Prislin, 1996). Thus, changing attitudes through just one intervention might be difficult. We also observed changes in causal attribution of weight gain. The relevance of the internal sub factor ‘energy balance' and the biological factors decreased while the relevance of external factors increased. These findings are partly in line with our assumptions: While our course unit seemed to increase the relevance of external factors successfully, the intended change in biological factors and personal factors did not work. A possible reason might be, that our information about biological factors were too unspecific. Perhaps, the biological factors are less relevant in contrast to behavioral and external factors in our presentation (module 1). In fact, interventions based on attributional changes are not sufficient to reduce weight stigmatization, and the long-term effects are unclear. Further course complements could include contact with patients with higher weight (e.g., videos with patients telling their stories) or to role models with positive attitudes, as a true change needs a change in social attitudes (Alberga et al., 2016). Here, however, it is important to ensure a protected environment for the patients so as not to harm them when they expose themselves to students. An overview of further strategies for destigmatization in health care is described by Pull (Puhl, 2023).
4.4 Strengths and limitations
As there is an insufficient number of studies that investigate interventions for reducing weight bias in medical students and health professionals, our study aimed to close a gap in research. Our course unit combined several approaches and used multimedia and different didactic methods to address the level of knowledge, skills and attitudes, providing ideas for design, methods and improvements of medical students' trainings. Additionally, we examined a large and representative sample of medical students.
Our study has some limitations. Firstly, we did not use a randomized controlled trial due to organizational reasons: our course took place during the current semester and it was not possible to test different teaching or examination formats A control group (e.g., no contents to weight stigma) would have been better in order to be able to attribute the effect to the intervention and to exclude confounder. We exclusively relied on self-assessments of explicit attitudes that could have made the purpose of our survey relatively easy to identify. As a result, there is a possibility that participants' responses were influenced by social desirability (Krumpal, 2013). Students may have answered more positive than they actually think about patients with obesity. While incorporating implicit measurements could have addressed this bias, it was not feasible in our study. Consequently, the extent of stigmatization found in our results may be underestimated. Attitudes are relatively time-stable and our course unit just took place once a time. A replication or a follow-up of the study may be useful to investigate long-term effects of our intervention. Our course unit mainly focused on an attributional approach. As mentioned before, this could not be sufficient for a greater change in attitudes. We also failed to change biological attribution in the intended way. There are course adaptions needed for being more successful in changing weight bias and causal attributions.
4.5 Further research
Further research is needed to investigate effective interventions of individual and setting approaches for a reduction of stigmatization. Our teaching module during the 6th semester is one of many courses offered during medical study. Students receive many influences from other courses and - after finishing - experience major changes in their own role when they start their career as young doctors. Longitudinal observation of attitudes even after graduation would be ideal. There is the need for specific and longitudinal training to improve attitudes toward overweight and obesity in the whole health care system to overcome weight-related stigmatization and discrimination in health care.
4.6 Conclusion
This study highlights the importance of incorporating weight bias awareness into medical curricula and training programs. It suggests that both medical students and health care professionals should be regularly sensitized to this issue throughout their medical education and specialty training to help mitigate weight bias.
Data availability statement
All materials and data generated or analyzed during this study are included in this article and its Supplementary material files. The raw data supporting the conclusions of this article will be made available by the corresponding authors, without undue reservation.
Ethics statement
This study protocol was reviewed and approved by the Ethics committee of the University of Würzburg, Germany, approval number 20230704 02. The participation in the study was voluntary. Participants were informed about study before the participation. A return of a filled questionnaire was taken as informed consent to participate in the study. The data were pseudonymised with individual codes for a comparison over time. After matching, the codes were deleted for a complete anonymization and so that no conclusions could be made about identity anymore.
Author contributions
JR: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft. MKr: Investigation, Supervision, Writing – review & editing. ET: Investigation, Writing – review & editing. MKo: Formal analysis, Supervision, Writing – review & editing. AS: Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We thank our students their interest and participation in this study. We thank Yvonne Kaußner for her supervision of the statistical analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2025.1565119/full#supplementary-material
References
Alberga, A. S., Pickering, B. J., Alix Hayden, K., Ball, G. D., Edwards, A., Jelinski, S., et al. (2016). Weight bias reduction in health professionals: a systematic review. Clin. Obes. 6, 175–188. doi: 10.1111/cob.12147
Alegria Drury, C. A., and Louis, M. (2002). Exploring the association between body weight, stigma of obesity, and health care avoidance. J. Am. Acad. Nurse Pract. 14, 554–561. doi: 10.1111/j.1745-7599.2002.tb00089.x
Ananthakumar, T., Jones, N. R., Hinton, L., and Aveyard, P. (2020). Clinical encounters about obesity: systematic review of patients' perspectives. Clin. Obes. 10:e12347. doi: 10.1111/cob.12347
Anderson, D. A., and Wadden, T. A. (2004). Bariatric surgery patients' views of their physicians' weight-related attitudes and practices. Obes. Res. 12, 1587–1595. doi: 10.1038/oby.2004.198
Bacon, J. G., Scheltema, K. E., and Robinson, B. E. (2001). Fat phobia scale revisited: the short form. Int. J. Obes. 25, 252–257. doi: 10.1038/sj.ijo.0801537
Batra, A., Hoch, E., Mann, K., and Petersen, K. U. (2015). S3-Leitlinie Screening, Diagnose und Behandlung des schädlichen und abhängigen Tabakkonsums. Verlag: Springer Berlin Heidelberg. doi: 10.1007/978-3-662-47084-8
Berkessel, J. B., Ebert, T., Gebauer, J. E., and Rentfrow, P. J. (2024). On the unequal burden of obesity: obesity's adverse consequences are contingent on regional obesity prevalence. Psychol. Sci. 35, 1260–1277. doi: 10.1177/09567976241265037
Bowden, E. L., and Petty, E. M. (2024). Perspectives on weight stigma and bias in medical education: implications for improving health outcomes. WMJ 123, 160–162.
Brochu, P. M., Banfield, J. C., and Dovidio, J. F. (2020). Does a common ingroup identity reduce weight bias? Only when weight discrimination is salient. Front. Psychol. 10:3020. doi: 10.3389/fpsyg.2019.03020
Brown, I., Thompson, J., Tod, A., and Jones, G. (2006). Primary care support for tackling obesity: a qualitative study of the perceptions of obese patients. Br. J. Gen. Pract. 56, 666–672.
Collaborators, G. O. (2017). Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 377, 13–27. doi: 10.1056/NEJMoa1614362
Crandall, C. S., D'Anello, S., Sakalli, N., Lazarus, E., Nejtardt, G. W., Feather, N., et al. (2001). An attribution-value model of prejudice: anti-fat attitudes in six nations. Pers. Soc. Psychol. Bull. 27, 30–37. doi: 10.1177/0146167201271003
Daly, M., Robinson, E., and Sutin, A. R. (2020). Perceived overweight and suicidality among US adolescents from 1999 to 2017. Int. J. Obes. 44, 2075–2079. doi: 10.1038/s41366-020-0620-9
Donini, L. M., Rosano, A., Di Lazzaro, L., Lubrano, C., Carbonelli, M., Pinto, A., et al. (2020). Impact of disability, psychological status, and comorbidity on health-related quality of life perceived by subjects with obesity. Obesity Facts 13, 191–200. doi: 10.1159/000506079
Emmer, C., Bosnjak, M., and Mata, J. (2020). The association between weight stigma and mental health: a meta-analysis. Obes. Rev. 21:e12935. doi: 10.1111/obr.12935
Farrell, E., Hollmann, E., le Roux, C. W., Bustillo, M., Nadglowski, J., and McGillicuddy, D. (2021). The lived experience of patients with obesity: a systematic review and qualitative synthesis. Obes. Rev. 22:e13334. doi: 10.1111/obr.13334
Ferrante, J. M., Ohman-Strickland, P., Hudson, S. V., Hahn, K. A., Scott, J. G., Crabtree, B. F., et al. (2006). Colorectal cancer screening among obese vs. non-obese patients in primary care practices. Cancer Detect. Prevent. 30, 459–465. doi: 10.1016/j.cdp.2006.09.003
Glauser, T. A., Roepke, N., Stevenin, B., Dubois, A. M., and Ahn, S. M. (2015). Physician knowledge about and perceptions of obesity management. Obes. Res. Clin. Pract. 9, 573–583. doi: 10.1016/j.orcp.2015.02.011
Gudzune, K. A., Bennett, W. L., Cooper, L. A., and Bleich, S. N. (2014). Patients who feel judged about their weight have lower trust in their primary care providers. Patient Edu. Couns. 97, 128–131. doi: 10.1016/j.pec.2014.06.019
Hebl, M. R., and Xu, J. (2001). Weighing the care: physicians' reactions to the size of a patient. Int. J. Obes. 25, 1246–1252. doi: 10.1038/sj.ijo.0801681
Heidebrecht, C., Fierheller, D., Martel, S., Andrews, A., Hollahan, A., Griffin, L., et al. (2024). Raising awareness of anti-fat stigma in healthcare through lived experience education: a continuing professional development pilot study. BMC Med. Educ. 24:64. doi: 10.1186/s12909-023-04889-8
Hilbert, A., Ried, J., Zipfel, S., and de Zwaan, M. (2013). Stigmatisierung bei Adipositas. Adipositas-Ursachen, Folgeerkrankungen, Therapie. 7, 150–153. doi: 10.1055/s-0037-1618820
Huizinga, M. M., Cooper, L. A., Bleich, S. N., Clark, J. M., and Beach, M. C. (2009). Physician respect for patients with obesity. J. Gen. Intern. Med. 24, 1236–1239. doi: 10.1007/s11606-009-1104-8
Kloock, S., Ziegler, C. G., and Dischinger, U. (2023). Obesity and its comorbidities, current treatment options and future perspectives: challenging bariatric surgery? Pharmacol. Ther. 251:108549. doi: 10.1016/j.pharmthera.2023.108549
Koran-Scholl, J., Geske, J., Khandalavala, K. R., and Khandalavala, B. (2023). Teaching module for obesity bias education: incorporating comprehensive competencies and innovative techniques. BMC Med. Educ. 23:340. doi: 10.1186/s12909-023-04310-4
Krumpal, I. (2013). Determinants of social desirability bias in sensitive surveys: a literature review. Qual. Quant. 47, 2025–47. doi: 10.1007/s11135-011-9640-9
Lauerer, E., Tiedemann, E., Polak, T., and Simmenroth, A. (2021). Can smoking cessation be taught online? A prospective study comparing e-learning and role-playing in medical education. Int. J. Med. Educ. 12:12. doi: 10.5116/ijme.5ff9.bccc
Lawrence, B. J., Kerr, D., Pollard, C. M., Theophilus, M., Alexander, E., Haywood, D., et al. (2021). Weight bias among health care professionals: a systematic review and meta-analysis. Obesity 29, 1802–1812. doi: 10.1002/oby.23266
Little, R. J. A. (1988). Test of missing completely at random for multivariate data with missing values. J. Am. Stat. Assoc. 83, 1198–1202. doi: 10.1080/01621459.1988.10478722
Major, B., Hunger, J. M., Bunyan, D. P., and Miller, C. T. (2014). The ironic effects of weight stigma. J. Exp. Soc. Psychol. 51, 74–80. doi: 10.1016/j.jesp.2013.11.009
Major, B., Tomiyama, J., and Hunger, J. M. (2017). “The negative and bidirectional effects of weight stigma on health,” in The Oxford Handbook of Stigma, Discrimination, and Health, Oxford Library of Psychology, Online Edn, eds. B. Major, J. F. Dovidio, and B. G. Link (Oxford: Oxford Academic), 499–519. doi: 10.1093/oxfordhb/9780190243470.013.27
Mata, J., and Hertwig, R. (2018). Public beliefs about obesity relative to other major health risks: representative cross-sectional surveys in the USA, the UK, and Germany. Ann. Behav. Med. 52, 273–286. doi: 10.1093/abm/kax003
Mensinger, J. L., Tylka, T. L., and Calamari, M. E. (2018). Mechanisms underlying weight status and healthcare avoidance in women: a study of weight stigma, body-related shame and guilt, and healthcare stress. Body Image 25, 139–147. doi: 10.1016/j.bodyim.2018.03.001
Miller Jr, D. P., Spangler, J. G., Vitolins, M. Z., Davis, M. S. W., Ip, E. H., Marion, G. S., et al. (2013). Are medical students aware of their anti-obesity bias? Acad. Med. J. Assoc. Am. Med. Coll. 88:978. doi: 10.1097/ACM.0b013e318294f817
Miller, W. R., and Rollnick, S. (2012). Motivational Interviewing: Helping People Change. New York, NY: The Guilford Press.
Nestorowicz, S., and Saks, N. (2021). Addressing bias toward overweight patients: a training program for first-year medical students. Med. Sci. Educ. 31, 1115–1123. doi: 10.1007/s40670-021-01282-2
Panel, D. G. (2008). Treating Tobacco Use and Dependence: 2008 Update. Atlanta, GA: US Department of Health and Human Services.
Pantenburg, B., Sikorski, C., Luppa, M., Schomerus, G., König, H. H., Werner, P., et al. (2012). Medical students' attitudes towards overweight and obesity. PLoS ONE 7:e48113. doi: 10.1371/journal.pone.0048113
Persky, S., and Eccleston, C. P. (2011). Medical student bias and care recommendations for an obese vs. non-obese virtual patient. Int. J. Obes. 35, 728–735. doi: 10.1038/ijo.2010.173
Phelan, S. M., Bauer, K. W., Bradley, D., Bradley, S. M., Haller, I. V., Mundi, M. S., et al. (2022). A model of weight-based stigma in health care and utilization outcomes: evidence from the learning health systems network. Obes. Sci. Pract. 8, 139–46. doi: 10.1002/osp4.553
Phelan, S. M., Burgess, D. J., Yeazel, M. W., Hellerstedt, W. L., Griffin, J. M., van Ryn, M., et al. (2015). Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 16, 319–326. doi: 10.1111/obr.12266
Phelan, S. M., Dovidio, J. F., Puhl, R. M., Burgess, D. J., Nelson, D. B., Yeazel, M. W., et al. (2014). Implicit and explicit weight bias in a national sample of 4,732 medical students: the medical student changes study. Obesity 22, 1201–1208. doi: 10.1002/oby.20687
Phelan, S. M., Puhl, R. M., Burgess, D. J., Natt, N., Mundi, M., Miller, N. E., et al. (2021). The role of weight bias and role-modeling in medical students' patient-centered communication with higher weight standardized patients. Patient Educ. Couns. 104, 1962–1969. doi: 10.1016/j.pec.2021.01.003
Prislin, R. (1996). Attitude stability and attitude strength: one is enough to make it stable. Eur. J. Soc. Psychol. 26, 447–77. doi: 10.1002/(SICI)1099-0992(199605)26:3<447::AID-EJSP768>3.0.CO;2-I
Puhl, R., and Brownell, K. D. (2013). Bias, discrimination and obesity. Health Hum. Rights Chang. World 9, 581–606. doi: 10.1038/oby.2001.108
Puhl, R. M. (2023). Weight stigma and barriers to effective obesity care. Gastroenterol. Clin. 52, 417–428. doi: 10.1016/j.gtc.2023.02.002
Puhl, R. M., Andreyeva, T., and Brownell, K. D. (2008). Perceptions of weight discrimination: prevalence and comparison to race and gender discrimination in America. Int. J. Obes. 32, 992–1000. doi: 10.1038/ijo.2008.22
Puhl, R. M., and Heuer, C. A. (2009). The stigma of obesity: a review and update. Obesity 17:941. doi: 10.1038/oby.2008.636
Puhl, R. M., Himmelstein, M. S., and Pearl, R. L. (2020). Weight stigma as a psychosocial contributor to obesity. Am. Psychol. 75:274. doi: 10.1037/amp0000538
Puhl, R. M., Latner, J. D., O'Brien, K., Luedicke, J., Danielsdottir, S., Forhan, M. A., et al. (2015). Multinational examination of weight bias: predictors of anti-fat attitudes across four countries. Int. J. Obes. 39, 1166–1173. doi: 10.1038/ijo.2015.32
Puhl, R. M., Luedicke, J., and Grilo, C. M. (2014). Obesity bias in training: attitudes, beliefs, and observations among advanced trainees in professional health disciplines. Obesity 22, 1008–1015. doi: 10.1002/oby.20637
Renold, C., Deferm, N. P., Hauser, R., Gerber, P., Bueter, M., Thalheimer, A., et al. (2023). The effect of a multifaceted intervention including classroom education and bariatric weight suit use on medical students' attitudes toward patients with obesity. Obes. Facts. 16:381. doi: 10.1159/000530405
Ruelaz, A. R., Diefenbach, P., Simon, B., Lanto, A., Arterburn, D., Shekelle, P. G., et al. (2007). Perceived barriers to weight management in primary care-perspectives of patients and providers. J. Gen. Intern. Med. 22, 518–522. doi: 10.1007/s11606-007-0125-4
Schienkiewitz, A., Kuhnert, R., Blume, M., and Mensink, G. (2022). Übergewicht und Adipositas bei Erwachsenen in Deutschland-Ergebnisse der Studie GEDA 2019/2020-EHIS. J. Health Monit. 7, 21–28. doi: 10.25646/10293
Schvey, N. A., Puhl, R. M., and Brownell, K. D. (2011). The impact of weight stigma on caloric consumption. Obesity 19, 1957–1962. doi: 10.1038/oby.2011.204
Schwartz, M. B., Chambliss, H. O. N., Brownell, K. D., Blair, S. N., and Billington, C. (2003). Weight bias among health professionals specializing in obesity. Obesity research. 11, 1033–1039. doi: 10.1038/oby.2003.142
Schwenke, M., Luppa, M., Pabst, A., Welzel, F. D., Löbner, M., Luck-Sikorski, C., et al. (2020). Attitudes and treatment practice of general practitioners towards patients with obesity in primary care. BMC Fam. Pract. 21, 1–8. doi: 10.1186/s12875-020-01239-1
Sikorski, C., Luppa, M., Brähler, E., König, H.- H., and Riedel-Heller, S. G. (2012). Obese children, adults and senior citizens in the eyes of the general public: results of a representative study on stigma and causation of obesity. PLoS ONE. 7:e46924. doi: 10.1371/journal.pone.0046924
Sikorski, C., Luppa, M., Luck, T., and Riedel-Heller, S. G. (2015). Weight stigma “gets under the skin”-evidence for an adapted psychological mediation framework-a systematic review. Obesity 23, 266–276. doi: 10.1002/oby.20952
Singh, K., Russell-Mayhew, S., von Ranson, K., and McLaren, L. (2019). Is there more to the equation? Weight bias and the costs of obesity. Can. J. Public Health 110, 17–20. doi: 10.17269/s41997-018-0146-2
Spahlholz, J., Baer, N., König, H. H., Riedel-Heller, S. G., and Luck-Sikorski, C. (2016). Obesity and discrimination-a systematic review and meta-analysis of observational studies. Obesity Rev. 17, 43–55. doi: 10.1111/obr.12343
Standen, E. C., Ward, A., and Mann, T. (2024). The role of social norms, intergroup contact, and ingroup favoritism in weight stigma. PLoS ONE. 19:e0305080. doi: 10.1371/journal.pone.0305080
Stein, J., Luppa, M., Ruzanska, U., Sikorski, C., König, H. H., Riedel-Heller, S. G., et al. (2014). Measuring negative attitudes towards overweight and obesity in the German population - psychometric properties and reference values for the German short version of the fat phobia scale (FPS). PLoS ONE 9:e114641. doi: 10.1371/journal.pone.0114641
Tajfel, H. (1979). “An integrative theory of intergroup conflict,” in The Social Psychology of Intergroup Relations (Monterey, CA: Brooks-Cole).
Talumaa, B., Brown, A., Batterham, R. L., and Kalea, A. Z. (2022). Effective strategies in ending weight stigma in healthcare. Obes Rev. 23:e13494. doi: 10.1111/obr.13494
Team, R. C. R. (2020). A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing.
Tomiyama, A. J., Carr, D., Granberg, E. M., Major, B., Robinson, E., Sutin, A. R., et al. (2018). How and why weight stigma drives the obesity 'epidemic'and harms health. BMC Med. 16, 1–6. doi: 10.1186/s12916-018-1116-5
Vartanian, L. R., and Shaprow, J. G. (2008). Effects of weight stigma on exercise motivation and behavior: a preliminary investigation among college-aged females. J. Health Psychol. 13, 131–8. doi: 10.1177/1359105307084318
Wear, D., Aultman, J. M., Varley, J. D., and Zarconi, J. (2006). Making fun of patients: medical students' perceptions and use of derogatory and cynical humor in clinical settings. Acad. Med. 81, 454–462. doi: 10.1097/01.ACM.0000222277.21200.a1
Wee, C. C., McCarthy, E. P., Davis, R. B., and Phillips, R. S. (2000). Screening for cervical and breast cancer: is obesity an unrecognized barrier to preventive care? Ann. Intern. Med. 132, 697–704. doi: 10.7326/0003-4819-132-9-200005020-00003
WHO (2014). Toolkit for Delivering the 5A's and 5R's Brief Tobacco Interventions to TB Patients in Primary Care. Geneva: World Health Organization.
WHO (2024). Fact Sheet, Obesity and Overweight 2024. WHO. Available online at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
Keywords: weight stigma, medical education, overweight and obesity, general medicine, blended learning
Citation: Ruck J, Krauthausen M, Tiedemann E, Koch MJ and Simmenroth A (2025) Awareness to weight stigma: the effect of a multi-approach course unit on weight-related stigmatization among medical students. Front. Educ. 10:1565119. doi: 10.3389/feduc.2025.1565119
Received: 22 January 2025; Accepted: 31 March 2025;
Published: 25 April 2025.
Edited by:
Nina Pereza, University of Rijeka, CroatiaReviewed by:
Kimberly Jamie, Durham University, United KingdomPatricia Perez-Cornejo, Autonomous University of San Luis Potosí, Mexico
Copyright © 2025 Ruck, Krauthausen, Tiedemann, Koch and Simmenroth. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jessica Ruck, cnVja19qMUB1a3cuZGU=
 Jessica Ruck
Jessica Ruck Maike Krauthausen
Maike Krauthausen Elena Tiedemann
Elena Tiedemann Anne Simmenroth
Anne Simmenroth