- 1Department of Neurology, Institute of Neuroscience, Key Laboratory of Neurogenetics and Channelopathies of Guangdong Province and Ministry of Education of China, The Second Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong, China
- 2Department of Neurology, The Fifth Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong, China
- 3Guilin Medical College, Guilin, Guangxi, China
- 4Guangdong Pharmaceutical University, Guangzhou, Guangdong, China
Background: The development of neurology closely correlates with improvements in medical education, which provides essential knowledge and skills to tackle the growing global challenge of neurological disorders. This study aimed to perform a bibliometric analysis to assess the key areas and trends concerning the interface between neurology and medical education for the period spanning from 2000 to 2023.
Objective: This study aimed to perform a bibliometric analysis to assess the key areas and trends concerning the interface between neurology and medical education for the period spanning from 2000 to 2023.
Methods: We gathered articles from the Web of Science Core Collection database and employed two bibliometric tools, CiteSpace and VOSviewer, to evaluate and quantify various impact and collaboration metrics. Our analysis included annual publication data, journals, co-cited journals, countries/regions, institutions, authors, and co-cited authors. Furthermore, we identified emerging research areas linked to neurology and medical education by investigating the co-occurrence and bursts of keywords and co-cited references.
Results: From 2000 to 2023, a total of 900 articles investigating the correlation between neurology and medical education were published in 297 academic journals. These articles were authored by 4,399 researchers from 893 institutions across 92 countries/regions. The United States, England, and Canada emerged as the leading countries in this field, with the United States maintaining a dominant position. Harvard University was identified as the most productive institution. Gilbert Donald L emerged as the top author, while Jozefowicz Rf recorded the highest number of co-citations. The journal Neurology was not only the most prolific in publishing articles at the intersection of neurology and medical education but was also the journal that received the most co-citations. The main themes of these articles centered around psychology, education, social health, nursing, and medicine, with keywords frequently relating to education, students, and neurological disorders.
Conclusion: Neurophobia within neurology medical education remains a significant area of research, contributing to a deeper understanding of the relationship between neurology and medical training. Emerging areas such as resident education, medical education training, developmental neurology, and parental involvement may offer valuable guidance and new insights for further research in the field of neurology education.
1 Introduction
The field of neurology, a specialized branch of medicine, is dedicated to diagnosing, treating, and gaining insights into disorders that influence the nervous system, including the brain, spinal cord, and peripheral nerves. Neurology is vital for managing various conditions, from epilepsy and stroke to neurodegenerative issues like Alzheimer's and Parkinson's disease (An et al., 2023). The ongoing development within neurology closely correlates with improvements in medical education, which prepares healthcare practitioners with the essential knowledge and skills to tackle the growing global challenge of neurological disorders (Abbasi et al., 2025).
In neurology, medical education encompasses various levels, including undergraduate, graduate, and continuing education, integrating theoretical concepts, hands-on clinical experience, and research opportunities. However, neurology is the most difficult subject in the medical school curriculum, which leads to a lack of confidence in managing neurology patients (Jukna et al., 2023; Pakpoor et al., 2014; Raskurazhev et al., 2021). Over time, the methods of teaching have shifted from conventional, lecture-based techniques to more innovative, student-focused strategies that involve simulation training, digital resources, and collaborative efforts across different professional disciplines (Chhetri, 2017; Shiels et al., 2017). These improvements strive to foster competency-based learning, improve patient outcomes, and accommodate the intricacies of today's healthcare environments. The diversity of neurological disorders and the complexity of their pathological mechanisms impose significant demands on the systematic design of educational content. Concurrently, medical education is undergoing a digital transformation, rendering traditional teaching methods increasingly inadequate in meeting the modern medical students' needs for dynamic knowledge updates, cultivation of clinical thinking, and integration of practical skills (Lattouf, 2022). Particularly under the influence of emerging technologies, such as virtual reality and AI, as well as the principles of evidence-based medicine, the development of an efficient, precise, and scalable neurology education system has become an urgent challenge that must be addressed (Hassell et al., 2023).
The framework of bibliometric analysis serves as a robust tool for assessing the development and influence of research in the domains of neurology and medical education. By exploring trends in publications, citation patterns, and thematic developments, bibliometric investigations can pinpoint key research areas, significant publications, and new frontiers of interest. This methodology not only charts the academic landscape but also uncovers existing gaps and potential avenues for future inquiry, thus guiding the progress of neurology and its incorporation into medical education. Compared to traditional reviews, bibliometrics has the advantage of being based on large sample data, thereby avoiding researcher bias. Techniques such as keyword co-occurrence and citation analysis can reveal knowledge connections. Additionally, it can dynamically track the development trajectory of a discipline and predict future research directions (Karlapudi et al., 2022).
Currently, the application of bibliometrics in the field of medical education has covered subjects such as surgery and nursing, systematic analysis specifically targeting neurology teaching remains scarcely reported (Ateş and Korkmaz, 2025). Previous research has focused on the analysis of single teaching methods, lacking a comprehensive assessment of the global research landscape in neurology education. This study is the first to introduce bibliometrics in the field of neurology education, innovatively mapping the global knowledge landscape of neurology education research by mining literature data from the Web of Science database over the past 20 years, revealing core research forces and international collaboration patterns. It identifies critical time nodes and driving factors for the iteration of teaching technologies, uncovering hotspots of research in recent years. The research findings are expected to provide theoretical support for optimizing the design of neurology courses, facilitating cross-institutional collaboration. This examination deepens our comprehension of how medical education contributes to the progress of neurology and provides insights into enhancing educational methodologies within this essential sector.
2 Materials and methods
2.1 Data collection
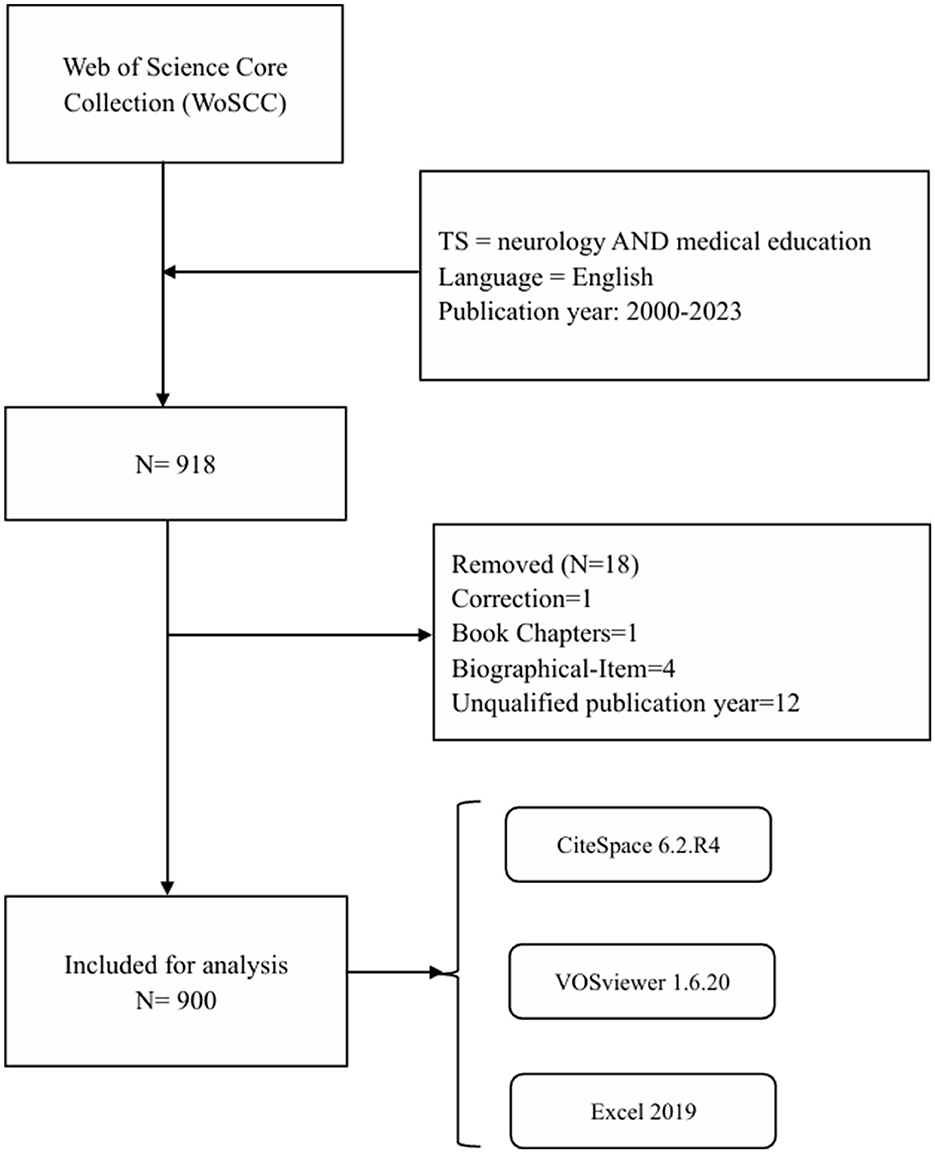
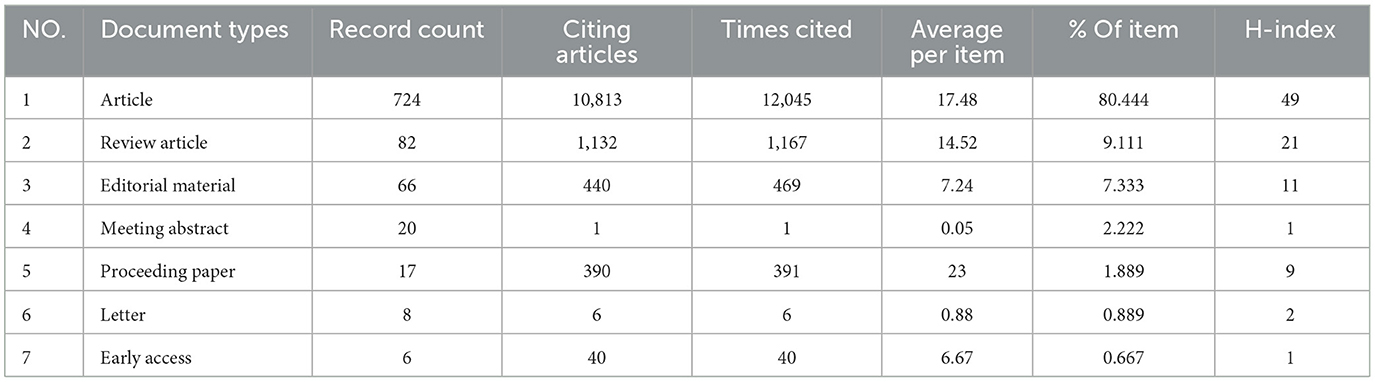
The database known as the Web of Science Core Collection (WoSCC) is widely used in bibliometric research and encompasses the Science Citation Index Expanded (SCIE), Social Science Citation Index (SSCI), and Emerging Sources Citation Index (ESCI). Data was obtained from the WoSCC database on September 23, 2024, to avoid any potential deviation due to daily updates. The search strategy used was [TS = (medical education AND neurology)] AND [Language = (English)], limiting the publication years to between 2000 and 2023. The results obtained from the search were saved in “Full Record and Cited References” and “Plain Text” formats. For further analysis, the downloaded files were renamed to “download_*.txt,” making them suitable for use with CiteSpace software. Notably, 918 documents comprising 10 document types were obtained. To enhance the significance of the data, the documents that are irrelevant to our restrictions were removed: (1) 12 of publication year which are unqualified, (2) 4 of document types are correction (n = 1), book chapter (n = 1) and Biographical-Item (n = 2). Therefore, 900 documents were finally collected to further research (Figure 1). The document types of each paper were listed in Table 1, the number of Articles have the highest count and H-index (n = 724, H-index = 49), followed by Review Articles (n = 82, H-index = 21) and Editorial Material (n = 66, H-index = 11).
2.2 Data analysis
We employed CiteSpace 6.2.R4 (developed by Chaomei Chen), VOSviewer 1.6.20 (created by Nees Jan van Eck and Ludo Waltman), alongside Microsoft Excel 2019, to conduct our bibliometric analysis and visualization. The initial phase involved data cleaning wherein terms such as “alzheimer disease” and “alzheimers-disease” were consolidated into “alzheimers-disease,” and “eeg (electroencephalography)” was standardized to “eeg (Paunkov et al., 2019).”
CiteSpace serves as an effective tool for bibliometric and visual analysis, particularly in identifying collaboration patterns, significant themes, structural elements, prospective trends, and dynamics within scientific disciplines. Therefore, we leveraged CiteSpace to scrutinize the co-occurrence of different nations, regions, and institutions. Additionally, we looked into the dual-map of journals, timelines of references, citation bursts, keyword evolution, and keyword bursts. The following parameters were employed: timespan (2000-2023), slices per year (1), no pruning, selection criteria (Top N = 100), and a minimum burst duration of 2 years. Cluster labels were derived through light semantic indexing (LSI) and the log-likelihood ratio (LLR) method, while other settings remained as default. Within the CiteSpace visualization, node sizes correspond to the frequency of co-occurrences, and the connecting lines highlight the co-occurrence relationships. Node and line colors vary by year, shifting from gray to red to represent the timeline from 2000 to 2023. Nodes represented by purple circles indicate a high betweenness centrality (≥0.10), acting as connectors among different networks (Song C. et al., 2024).
VOSviewer is a bibliometric tool that excels in creating and visualizing knowledge maps, illustrating different types of clusters, overlays, or density colors. It has been utilized to analyze the co-occurrence of authors alongside co-cited authors, journals with their co-cited counterparts, as well as co-cited references and keywords. We employed full counting as the method for data representation; other thresholds are detailed in the corresponding chapter. In the cluster map, the node size corresponds to co-occurrence frequencies, while identical colors denote the same cluster. Additionally, links illustrate co-occurrence relationships, with the thickness reflecting a computed strength value, which is directly related to the number of joint publications by two researchers or the frequency of two keywords appearing together. In density maps, the size of words and the brightness of yellow are positively correlated with co-citation frequency. The overlay map uses color to signify the average publication year.
To analyze annual publications, we utilized Excel software. Additionally, we retrieved the impact factor (IF), journal citation reports (JCR) for various journals, and the H-index for scholars from the Web of Science on September 23, 2024.
3 Results
3.1 Annual growth trend
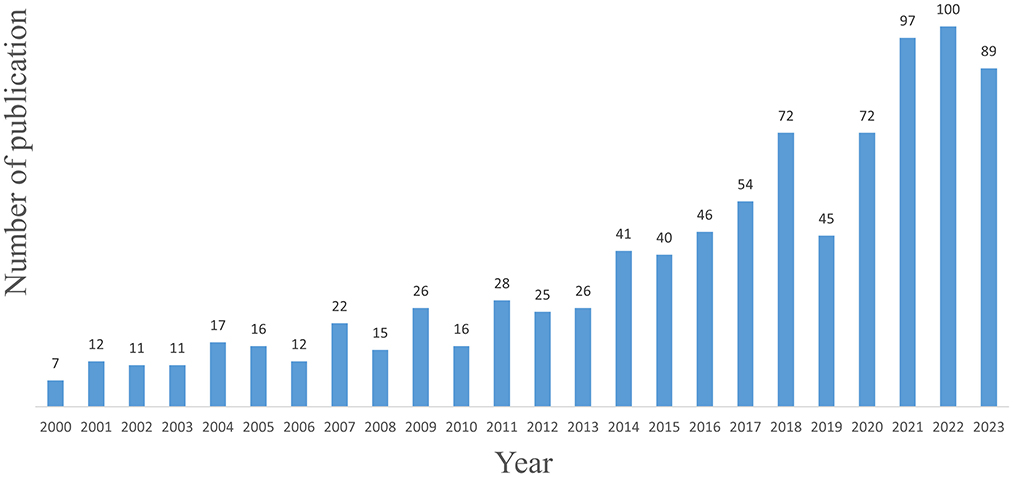
We screened 900 articles from the WoSCC database for analysis (Figure 1, Supplementary Table 1). The overall number of articles from 2000 to 2010 was still relatively small, but the number of articles increased gradually during the period from 2011 to 2023 (Figure 2).
3.2 Distribution of countries/regions and institutions
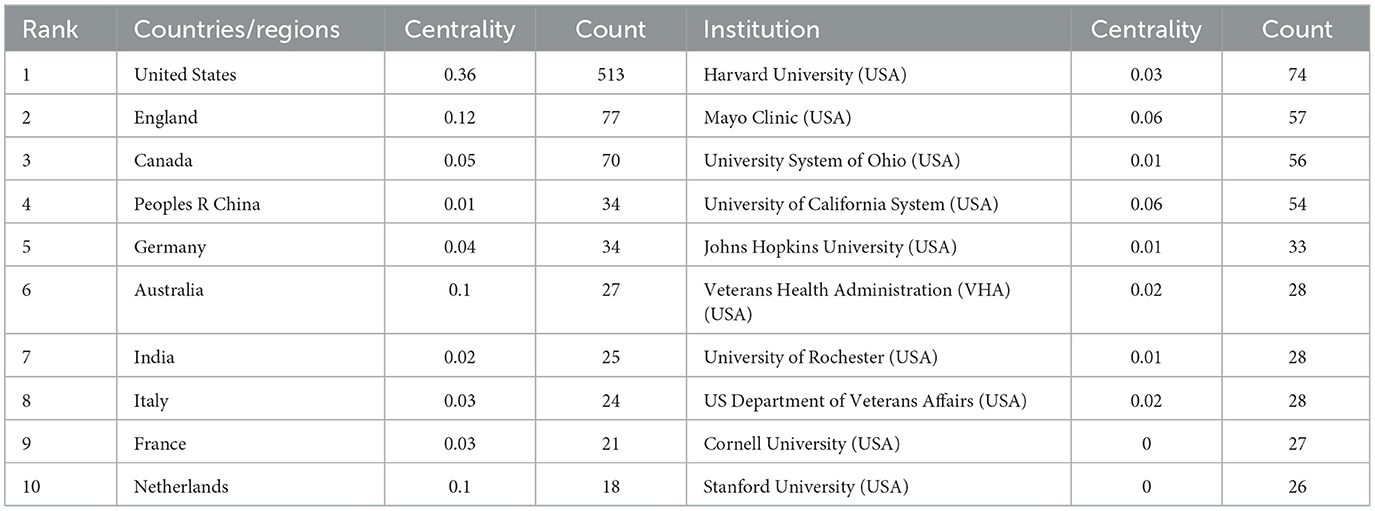
Among the total of 900 articles, 724 are research articles and 82 are reviews, which together account for the majority of the publications (Table 1). These articles originate from 92 countries/regions and 893 institutions (Supplementary Tables 2, 3). The United States has the highest number of publications (N = 513), followed by England (N = 77) and Canada (N = 70). However, Canada's centrality is less than 0.1, suggesting that it may not serve as a central node in research related to neurology medical education (Figure 3A). The top 10 contributors are listed in Table 2. In contrast, the United States exhibits a higher centrality (centrality = 0.36). The density of country/region co-occurrence is 0.138, reflecting a strong connection among them. Harvard University is identified as the most productive institution, although its centrality is relatively low (n = 74, centrality = 0.03), followed by Mayo Clinic (n = 57, centrality = 0.06) and the University System of Ohio (n = 56, centrality = 0.03). In contrast, King's College Hospital (n = 5, centrality = 0.09) and the University of London (n = 23, centrality = 0.08) demonstrate higher centrality (Figure 3B, Table 2).
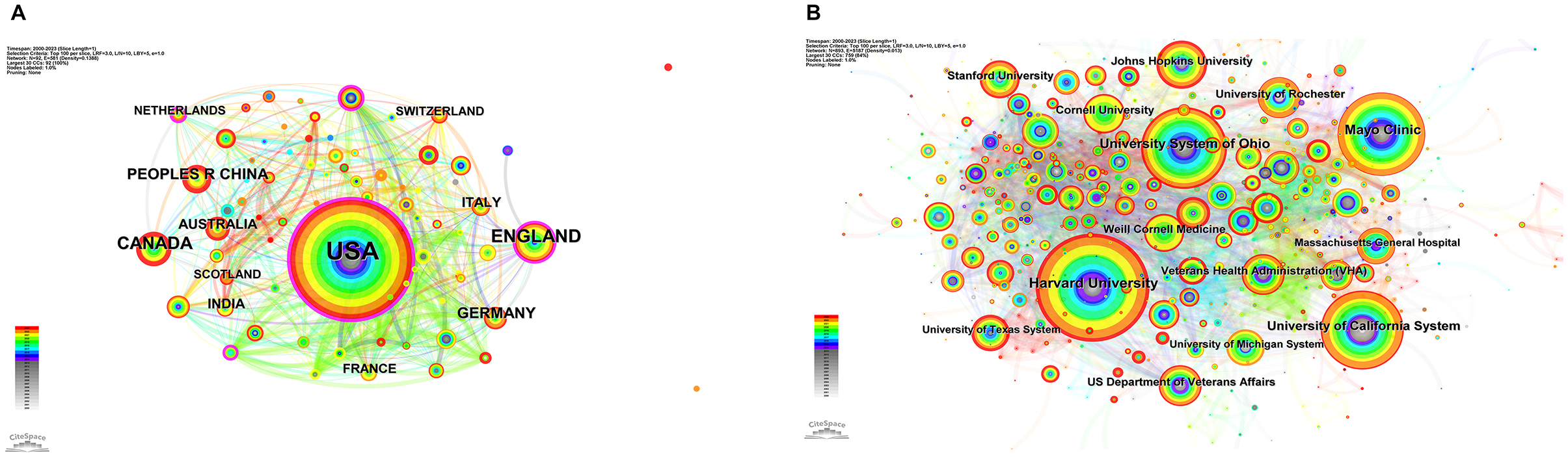
Figure 3. The co-occurrence map of countries and regions (A) and institutions (B) in research about neurology and medical education. The node size reflects co-occurrence frequencies, while the links illustrate co-occurrence relationships. The color of the nodes and lines represent different years, with colors transitioning from blue to red as the timeline progresses from 2000 to 2023. Nodes depicted in purple circles indicate high betweenness centrality (≥0.1).
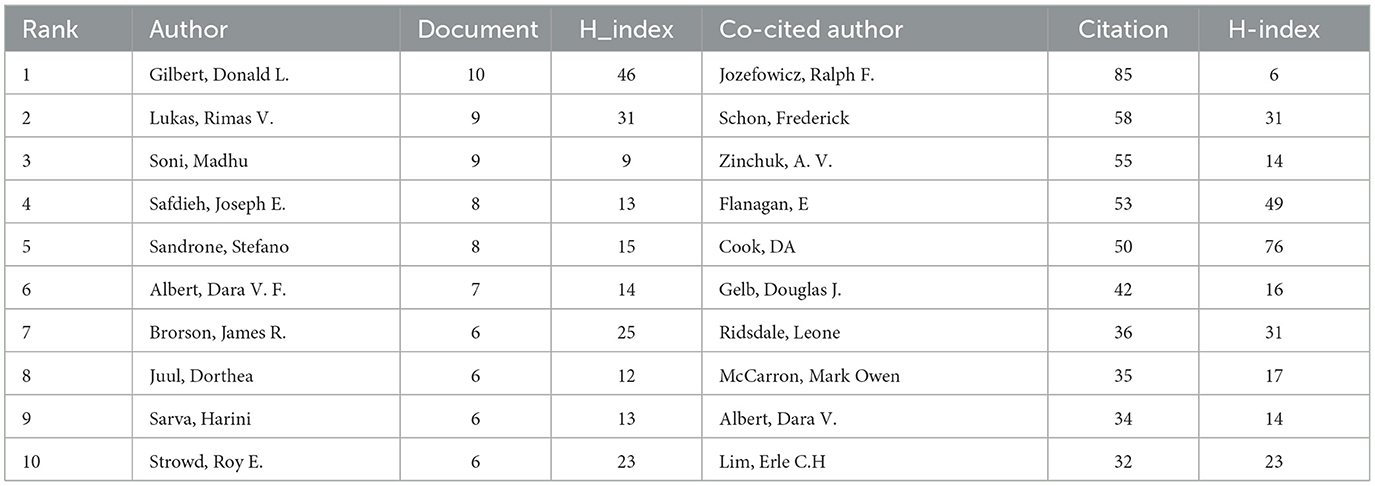
3.3 Author and co-cited author
A total of 4,339 authors participated in the research on neurology medical education (Figure 4A; Supplementary Table 4). The top ten authors collectively published more than six articles, while 74 authors produced at least three papers; however, 28 of these authors are not interconnected (Figure 4A). Gilbert Donald L from Cincinnati Children's Hospital Medical Center authored the highest number of neurology-related articles (n = 10), followed by Lukas Rimas V and Soni Madhu (Table 3). Figure 4A features seven colors, each representing a distinct cluster among the authors. Active collaborations typically occur within the same cluster, as seen with Sarva Harini and Weber Daniel. Additionally, there are collaborations between different clusters, exemplified by Albert Dara V. F. and Gilbert Donald L.
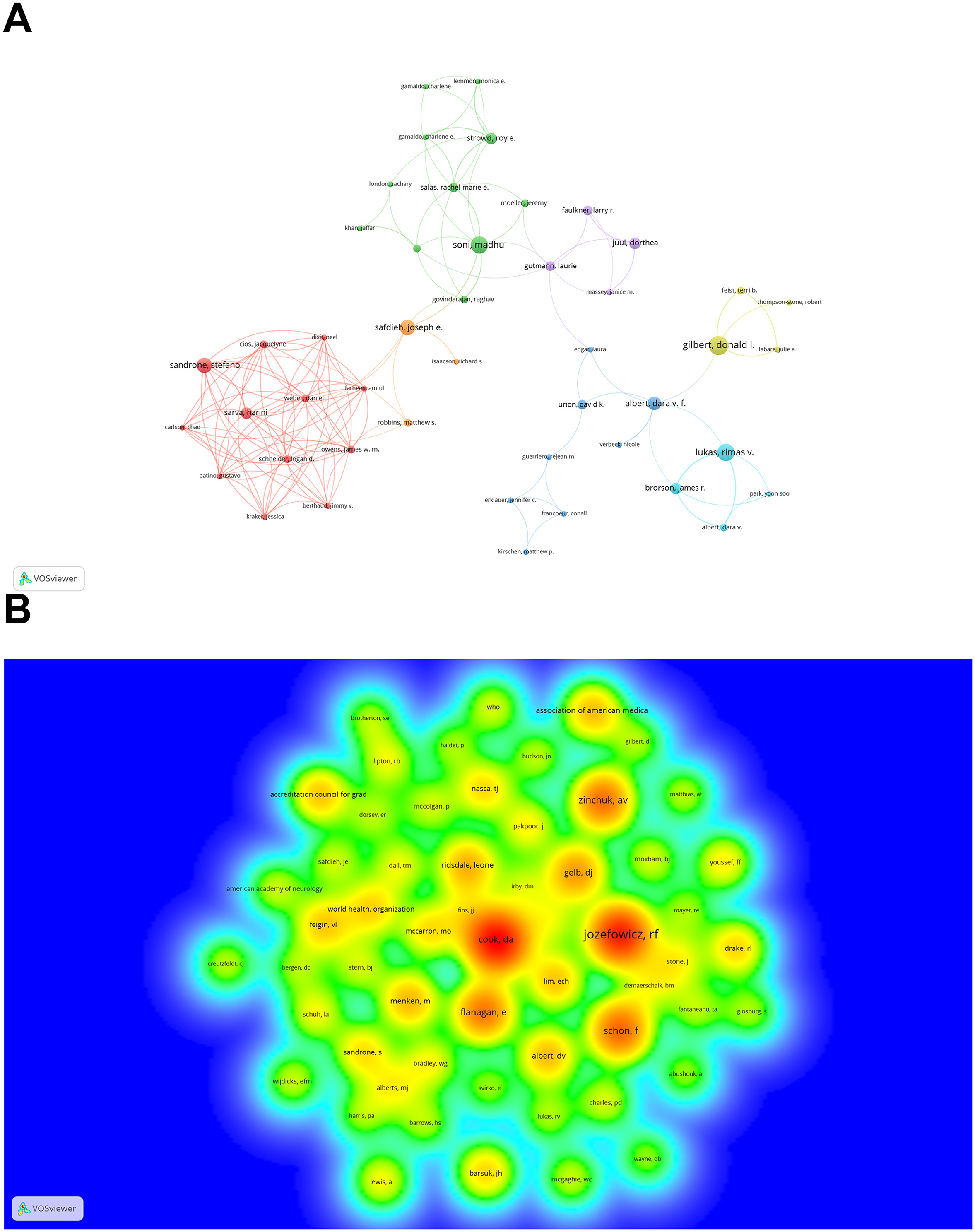
Figure 4. The co-occurrence authors (A) and co-cited authors (B) in research about neurology and medical education. (A) The size of each node reflects the co-occurrence frequencies of the authors, while the links indicate the co-occurrence relationships between them. The thickness of these links is proportional to the number of publications co-authored by the two researchers, and nodes of the same color represent authors within the same cluster. (B) The size of the words, the size of the circles, and the opacity of the yellow color are positively correlated with the frequency of co-citation.
Co-cited authors are authors who are cited in an article. Among the 17,656 cited authors, five have been cited more than 50 times (Figure 4B, Supplementary Table 5). Figure 4B is presented as a density plot, effectively illustrating high-frequency co-cited authors, with warmer colors indicating a greater number of citations. As detailed in Table 3, Figure 4B, Jozefowicz Rf, Schon F, and Zinchuk Av were the most frequently co-cited authors.
Due to the inherent limitations of CiteSpace and VOSviewer visualizations, these figures cannot encompass all available information. Consequently, we provide the complete data in Supplementary Table 5, as well as in the figure below.
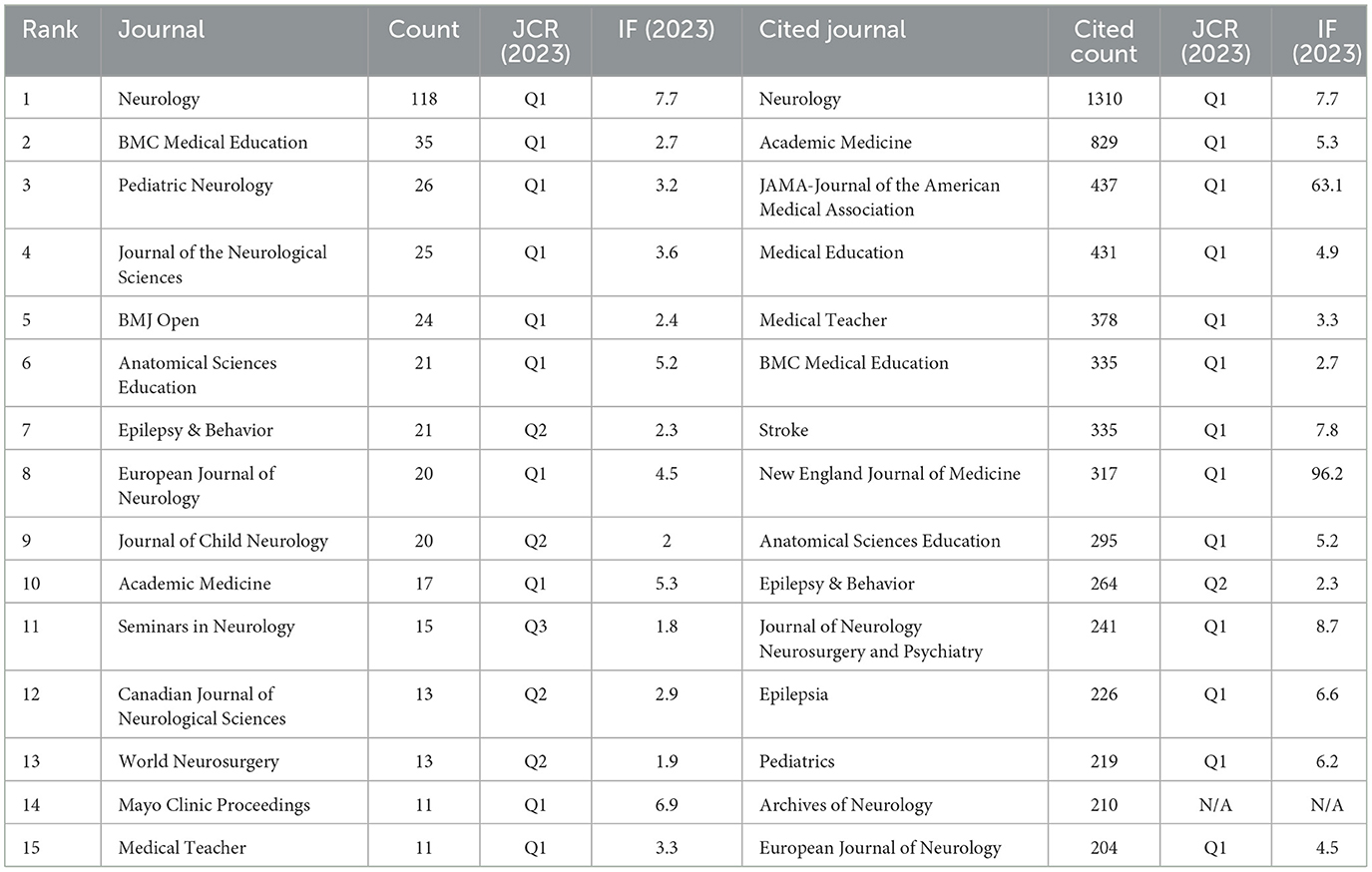
3.4 Journal and co-cited journal
A total of 297 journals published research on the relationship between neurology and medical education, with the top 15 journals contributing 390 articles, which accounts for 43.33% of the total (see Table 4, Supplementary Table 6). The journal with the highest number of publications is Neurology (n = 118), followed by BMC Medical Education (n = 35) and Pediatric Neurology (n = 26). Among 7,130 co-cited journals that received a total of 26,241 citations (Supplementary Table 7), 28 journals had more than 100 citations. Neurology (n = 1,310), Academic Medicine (n = 829), and JAMA-Journal of the American Medical Association (n = 437) received the highest number of citations. Furthermore, the top 15 co-cited journals accounted for 22.98% of all cited sources (see Table 4).
The dual-map overlay demonstrating the distribution of topics within academic journals is depicted in Figure 5. On the left side, the citing journals are displayed, while the cited journals are featured on the right, with colored lines representing the relationships of citations. As shown in Figure 5, there are two main citation paths: one originating from journals in Neurology, Sports, and Ophthalmology leading to those in Health, Nursing, and Medicine, and another stemming from Psychology, Education, and Social journals. The first path shows a notable frequency of citations, with a high f-value of 62,890, whereas the second path exhibits a strong citation relationship indicated by its z-value of 4.1560464. Moreover, there are two significant citation pathways from journals in Medicine, Medical, and Clinical fields to both Health, Nursing, and Medicine journals and to Psychology, Education, and Social journals. Figure 5 illustrates that both Health, Nursing, and Medicine journals along with Psychology, Education, and Social journals receive citations from both Neurology, Sports, and Ophthalmology journals, as well as from Medicine, Medical, and Clinical journals.
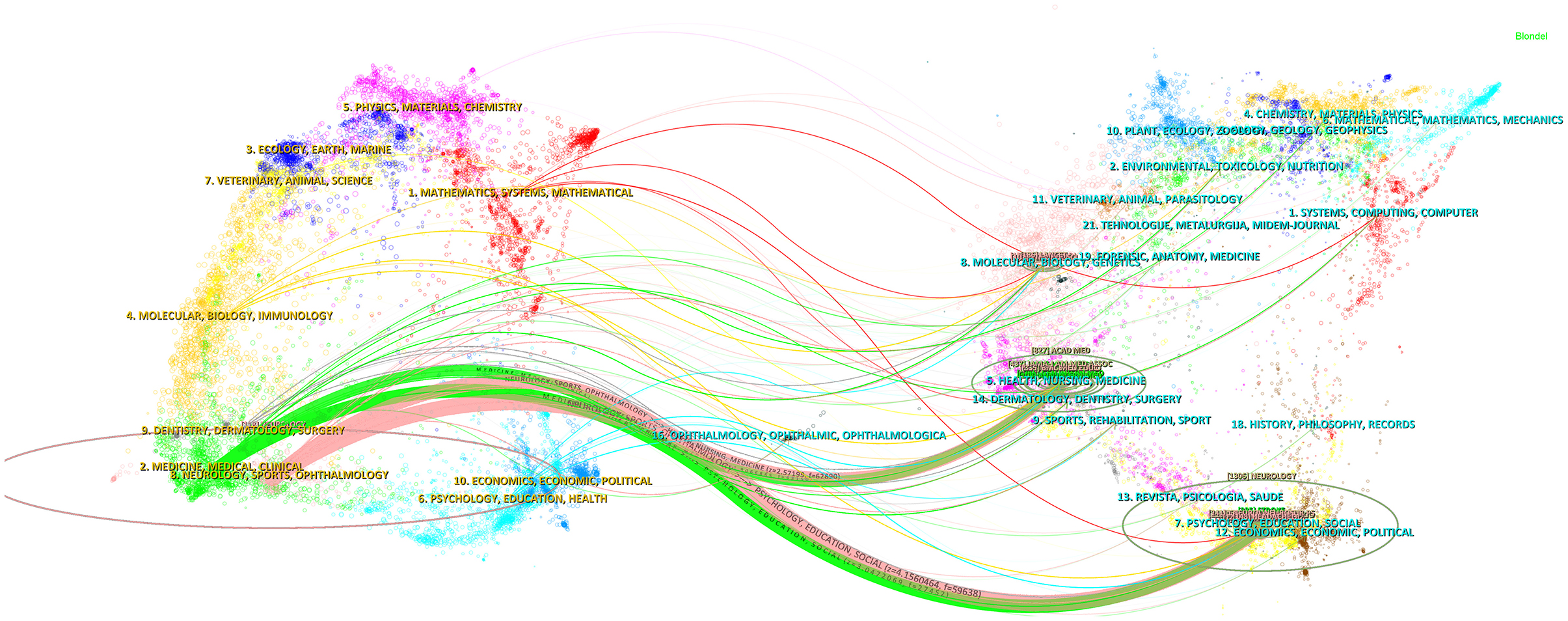
Figure 5. The dual-map overlay of journals on neurology and medical education. The citing journals are on the left, the cited journals are on the right, and the colored path represents the citation relationship.
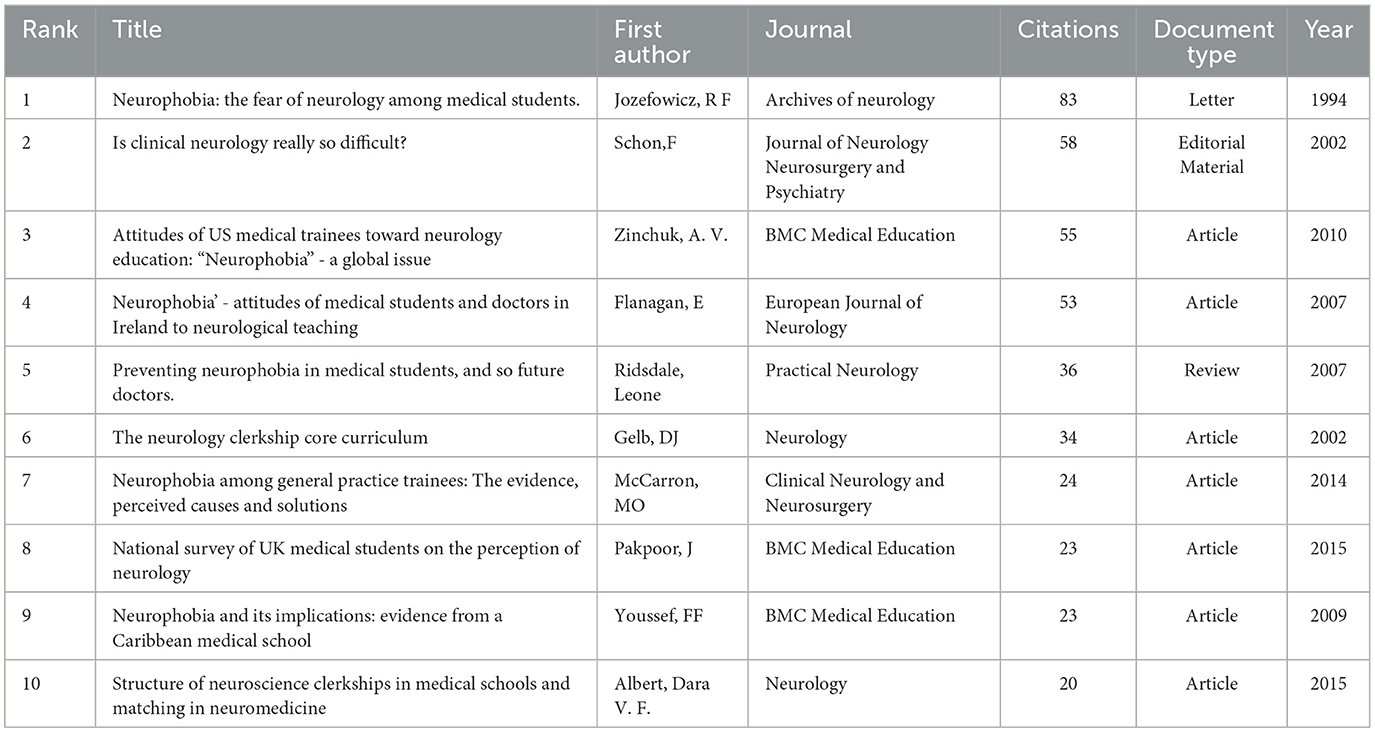
3.5 Co-cited reference and reference burst
Out of the 22,574 references cited, 38 were mentioned a minimum of 10 times (refer to Supplementary Table 8). As shown in Table 5, the ten most co-cited works received at least 20 mentions. Remarkably, the most frequently co-cited work is a letter authored by Jozefowicz RF et al., published in the Archives of Neurology in 1994 (n = 83) (Jozefowicz, 1994). Additionally, among the top 10 references, seven were articles, while the remaining included letters, editorial pieces, and reviews. The reference timeline view illustrates the evolution of research hotspots over time. The most frequent items in each cluster are designated as cluster labels, and the remaining items are detailed in Supplementary Table 9. As shown in Figure 6, cluster #7 (psychiatry education/gross anatomy) emerged earlier, whereas clusters #1 (medical education/neuroanatomy education), 2 (mental health/podcasting), 4 (cognitive heuristics/neurosurgery), 6 (clinical neurophysiology/online teaching), and #8 (.../virtual learning) are ongoing, which can be regarded as novel-edge research.
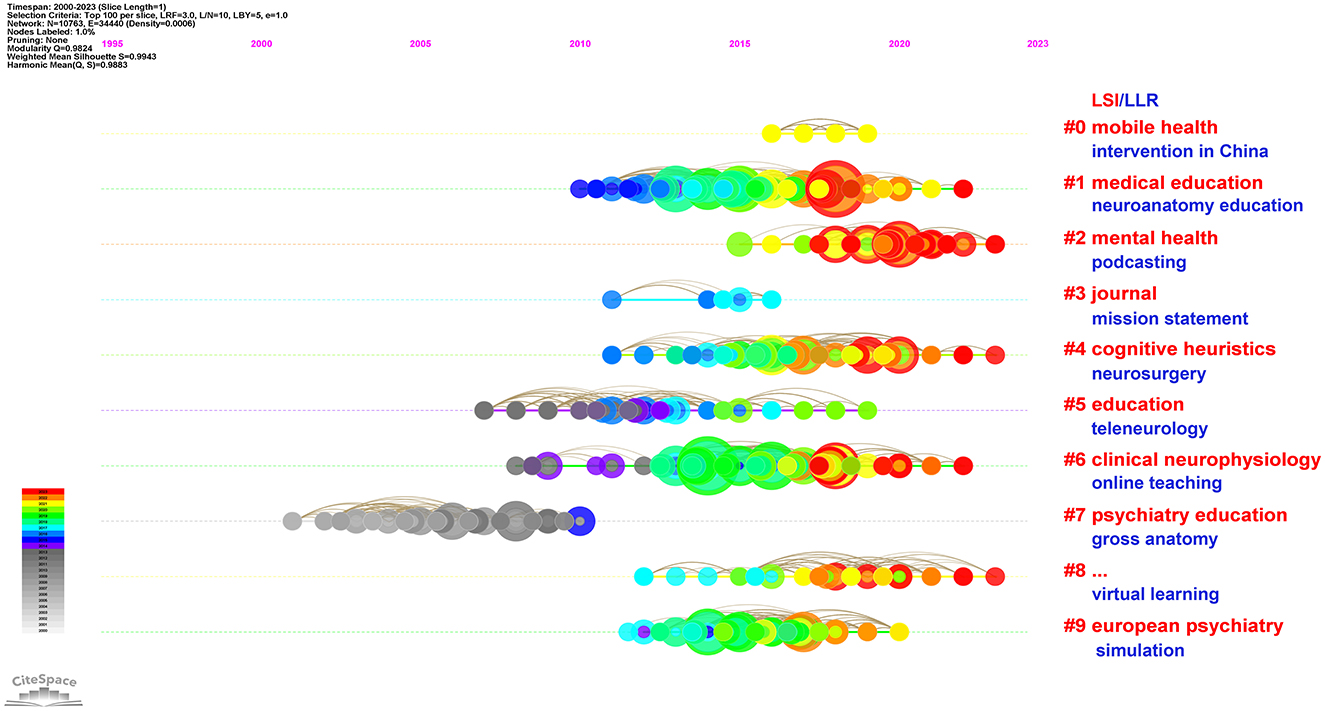
Figure 6. Timeline view of co-cited references related to neurology and medical education. Each horizontal line representing a distinct cluster. A smaller number indicates a larger cluster, with #0 denoting the largest cluster. The size of each node reflects the frequency of co-citation, while the links illustrate the co-cited relationships. The color of the nodes and lines corresponds to different years, with nodes positioned according to their first year of co-citation. Cluster labels were derived from titles using Light Semantic Indexing (LSI) in red and Log-Likelihood Ratio (LLR) in blue.
References exhibiting citation bursts are those that have been cited significantly more frequently over a specific period. A total of 265 references were identified as having citation bursts, with the top 20 listed in Figure 7. The strongest burst (strength = 5.76) occurred in a paper titled “Structure of neuroscience clerkships in medical schools and matching in neuromedicine,” published in Neurology by Dara V Albert in 2015 (Albert et al., 2015), which experienced a citation burst from 2016 to 2018. Additionally, there are no references currently experiencing a burst.
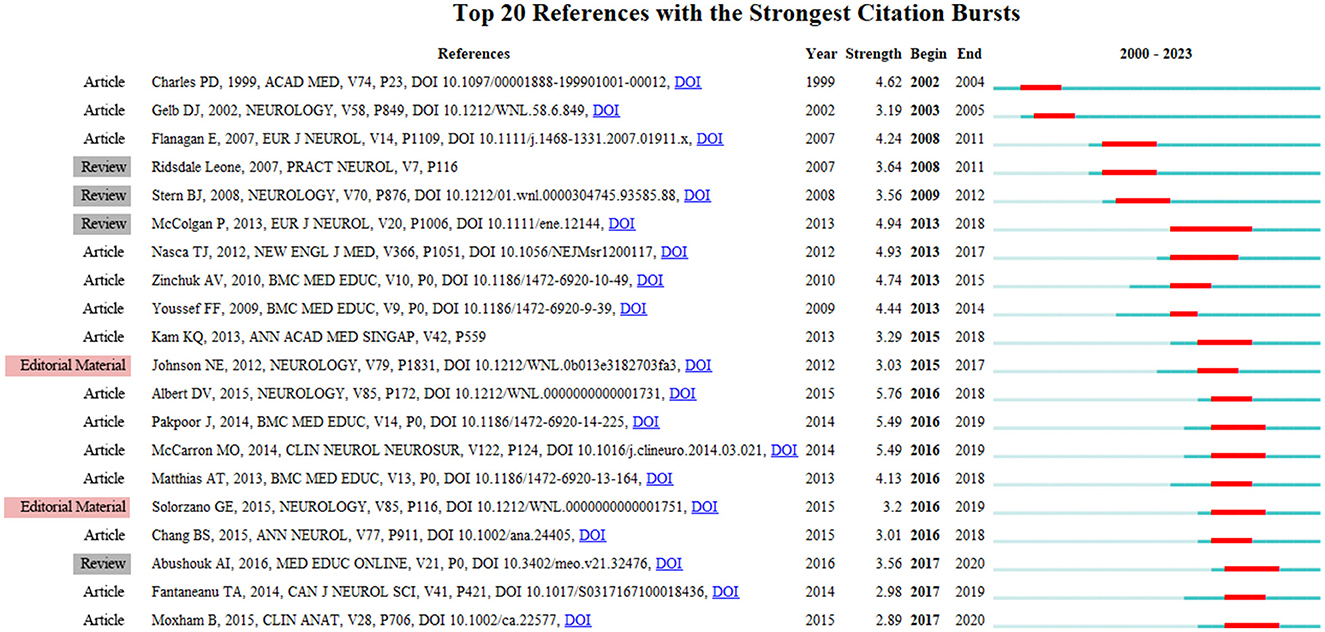
Figure 7. Timeline view of co-cited references related to neurology and medical education. Top 20 references with the strongest citation bursts involved in neurology and medical education. The blue bars indicate references that have been published, while the red bars represent periods of heightened citation activity.
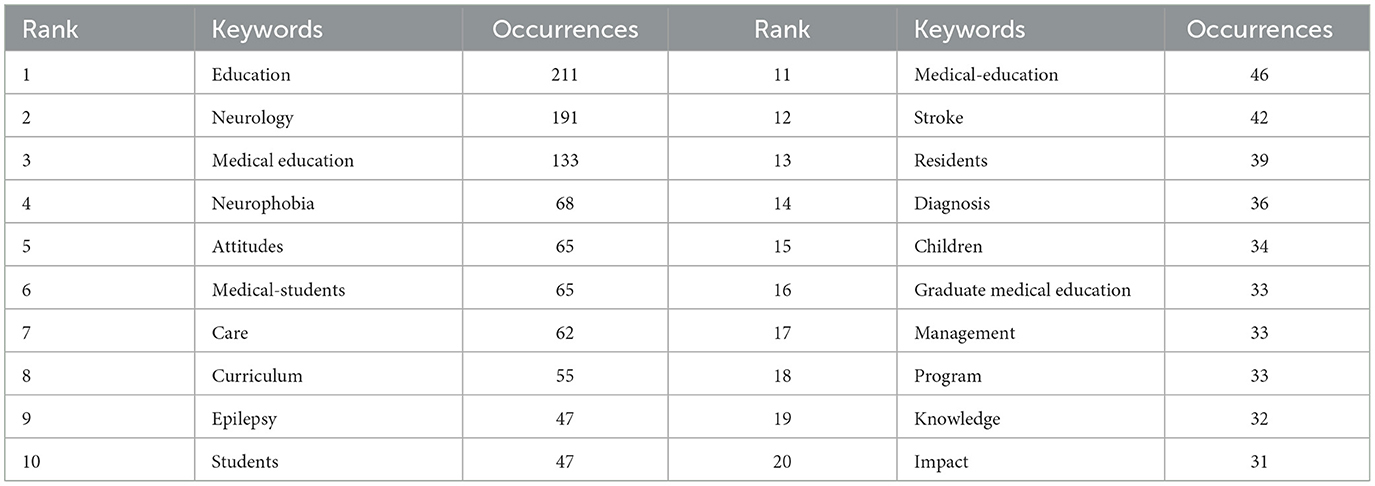
3.6 Keyword analysis of trending research topic
A total of 2,993 keywords were extracted, with 106 keywords appearing at least 10 times and 40 keywords appearing at least 20 times (see Supplementary Table 10). Table 6 indicates that 'education' was the most frequent keyword (n = 211), followed by “neurology” (n = 191) and “medical education” (n = 133). The keywords most commonly associated with neurological diseases and medical education include “neurophobia” (n = 68), “epilepsy” (n = 47), and “stroke” (n = 42).
Figure 8A presents a high-frequency keyword overlay map (n ≥ 15), where the color represents the average year of publication. Notably, 'neuroanatomy,' 'anatomy,' 'neurosurgery,' 'intervention,' and 'people' are emerging fields, indicated in yellow. The timeline view in Figure 8B illustrates the top two high-frequency keywords in each cluster over time. It is evident that nine of the ten clusters (excluding #7) are still active. Among these, cluster #0 (medical education/neuroanatomy education) is the largest, followed by cluster #1 (knowledge/critical care), cluster #2 (neurology residents/students), and cluster #3 (graduate medical education/resident education). Additional information is provided in Supplementary Table 11.
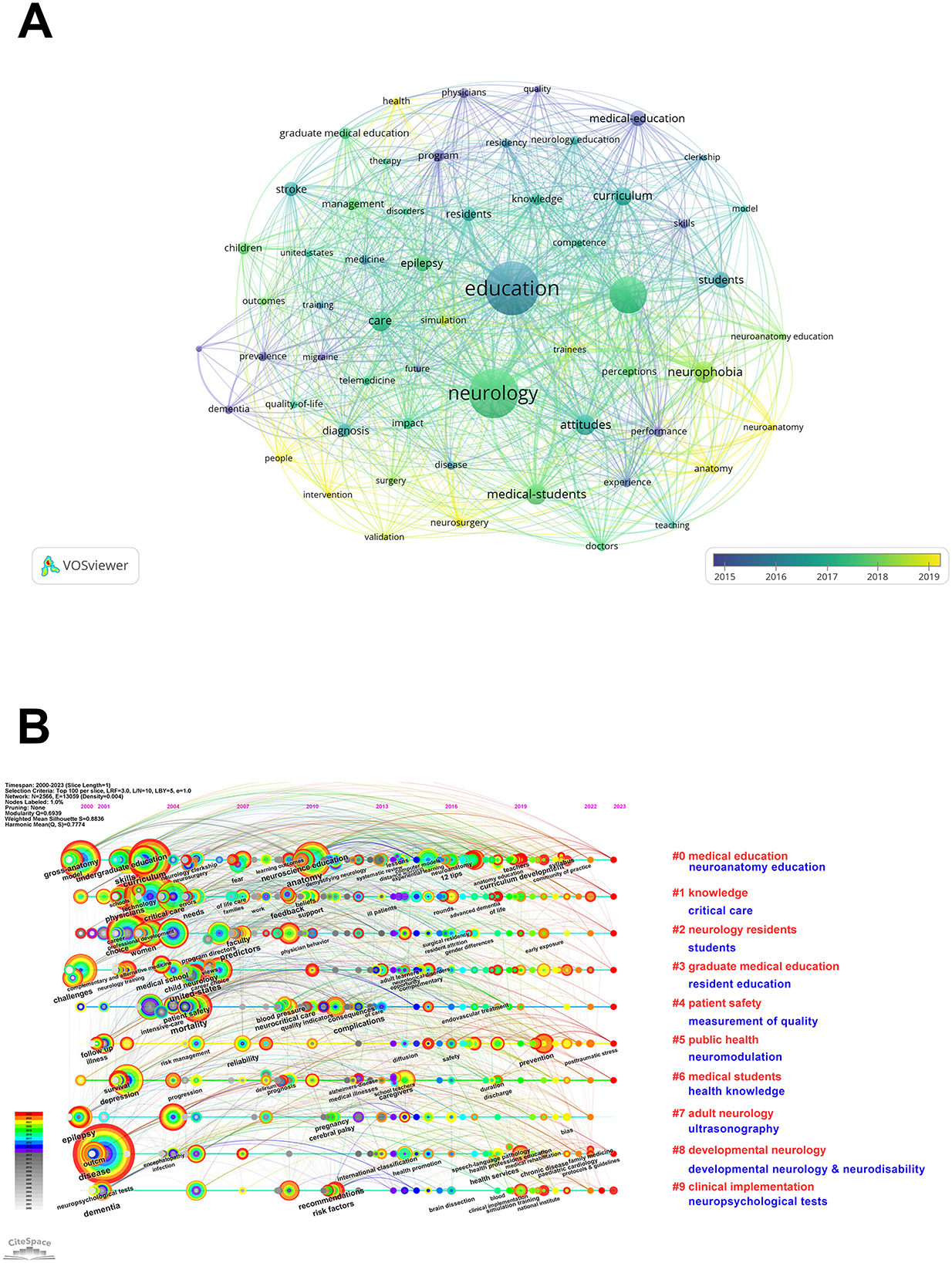
Figure 8. (A) The overlay map of keywords related to neurology and medical education. The size of each node corresponds to the frequency of co-occurrences, while the links represent the relationships between these co-occurring keywords. The thickness of each link is proportional to the number of times two keywords co-occur, and the color of the links indicates the average year of publication. (B) The timeline view of keywords related to neurology and medical education. Each horizontal line represents a cluster; the smaller the number, the larger the cluster, with #0 being the largest. The time is indicated at the top, while keywords are positioned at their initial co-occurrence time within the cluster. Cluster labels were derived from title and abstract information using Light Semantic Indexing (LSI) in red and Log-Likelihood Ratio (LLR) in blue.
Keyword bursts refer to those that have been cited with significant frequency over a specific period. As illustrated in Figure 9, “receptor neurophobia” exhibited the strongest burst (strength = 5.28), followed by “medicine” (n = 3.65) and “American academic” (n = 3.47). Notably, “resident education,” “medical education and training,” “developmental neurology & neurodisability,” and “parents” continued to show bursts of activity through 2023.
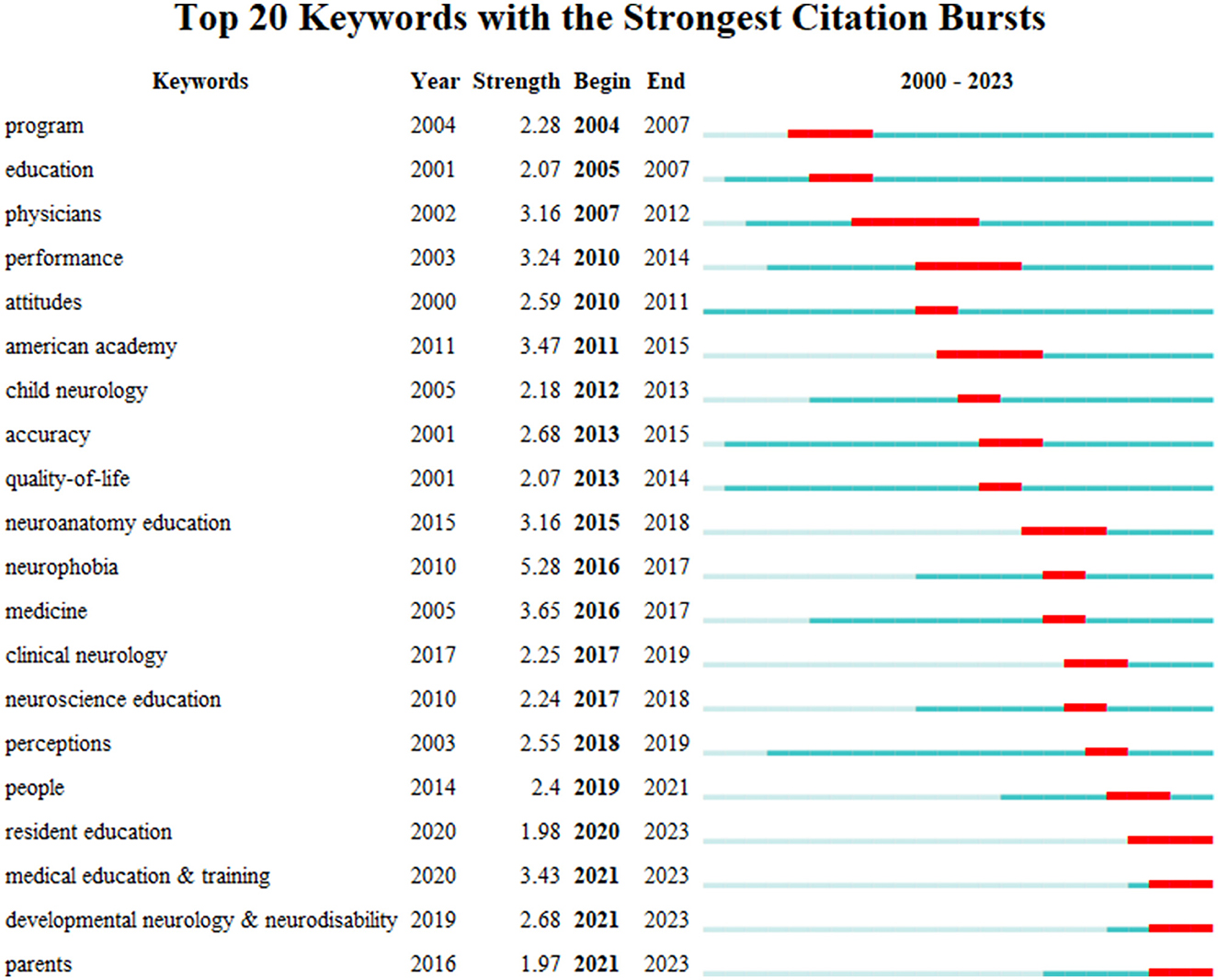
Figure 9. The timeline view of keywords related to neurology and medical education. Top 20 keywords with the strongest citation bursts, the red bars mean citation burstness.
4 Discussion
4.1 General information
Based on data from the WoSCC database spanning from 2000 to 2023, a total of 900 articles exploring the relationship between neurology and medical education were published across 297 academic journals. These articles were authored by 4,339 individuals from 893 institutions representing 92 countries and regions. The growing body of research indicates an increasing interest in the association between neurology and medical education. The investigation of neurology and medical education began in 1950 when Woltman reported on the neurological aspects of the Minnesota experiment in graduate medical education (Woltman, 1950). Since then, research in this area has progressed steadily. Over the past decade, the number of publications on neurology and medical education has significantly increased, with the volume of articles published between 2010 and 2023 nearly quadrupling compared to those published between 2000 and 2010.
In analyzing country and regional involvement, the number of published articles and centrality are key factors to consider. High centrality nodes (≥0.10) indicate the 'bridge' effect these countries and regions have on the global cooperation network. Table 2, Figure 3 illustrate that the United States, England, and Canada lead in research on neurology and medical education. Among the top 10 institutions publishing research projects, all are located in the United States. Notably, Canada has centrality values below 0.1, while the United States and England have centrality values of 0.36 and 0.12, respectively, suggesting their dominant positions in neurology and medical education research. Furthermore, the United States, England, Australia, and the Netherlands all have centralities exceeding 0.1, underscoring their significant roles in global research on neurology and medical education. Overall, active collaboration among these countries and institutions is evident in terms of network density. Therefore, strengthening international cooperation with the United States in medical education is conducive to the development of neurology teaching.
Among the top 10 authors and co-cited authors, Donald L Gilbert has published the most articles on neurology and medical education research, underscoring his significant contributions to these fields. Gilbert, a Full Professor at Cincinnati Children's Hospital Medical Center, specializes in pediatric neurological diseases, including movement disorders and Tourette Syndrome. He has also identified common mechanisms linking transcranial magnetic stimulation and behavioral disorders. Notably, one of his studies published in the journal Pediatric Neurology in 2016 demonstrated that the requirement of 12 months of adult neurology training for Child Neurology and Neurodevelopmental Disability certification does not align with the views of the majority of program directors (Valencia et al., 2016). Jozefowicz Ralph F. is the leading co-cited author, specializing in medical education and neuromuscular disease at the University of Rochester. His research primarily focuses on neurology education, residency training in neurology, and the education of medical students. In 1994, Jozefowicz published a study in Archives of Neurology that investigated the concept of neurophobia, which he defined as a fear of the neural sciences and clinical neurology stemming from students' inability to apply their knowledge of basic sciences to clinical situations. These negative sentiments are relevant to the study of neurology in medical school (Jozefowicz, 1994).
The journal Neurology is recognized for publishing a substantial amount of research in the fields of neurology and medical education, and it is distinguished by having the highest number of co-citations. This assertion is supported by the fact that three of the top ten highly cited papers were published in Neurology and BMC Medical Education. These journals primarily concentrate on cellular neurology, medical education, and related disciplines. Furthermore, Neurology ranks first in the number of articles published, highlighting its significance in the dissemination of research concerning neurology and medical education. Dual-map analysis indicates that research in these areas is predominantly centered around psychology, nursing, education, and social sciences.
The set of references that are frequently cited together within a specific research community may reflect the collective knowledge base. Among the top ten cited references, six primarily address neurophobia in neurological education, emphasizing the importance of confronting this phenomenon, along with its implications and potential solutions. Additionally, two articles focus on the neurology clerkship: one presents a core curriculum outlining the clinical neurology skills and knowledge necessary for adequate preparation (Gelb et al., 2002), while the other evaluates the status of the neurology clerkship in U.S. medical schools and its impact on graduates entering the field (Albert et al., 2015). These findings suggest that neurophobia significantly influences medical education in neurology through its effects on medical students.
Regarding burst analysis, the absence of references currently in burst indicates a need for further study on the intersection of neurology and medical education. The strongest burst suggests a neurology clerkship and highlights opportunities for students to connect with peers who are matching neuromedicine residencies. Two references from 2020 are noteworthy: one discusses evidence-based recommendations and educational interventions aimed at addressing neurophobia in medical education, while the other establishes internationally recognized standards and provides guidelines related to neuroanatomical knowledge.
4.2 The hotspots and trending
Nowadays, it is very important for researchers to quickly understand current research hot spots. Therefore, bibliometrics provides a quantitative method that can reflect research hot spots in the academic field through keyword co-occurrence. Overlap and timeline views can reflect the development of new research, and reference clusters and citation bursts can represent emerging topics. This study attempts to objectively evaluate through keyword co-occurrence (Tables 5, 6), keyword overlap and timeline (Figure 8), keyword burst (Figure 9), reference timeline (Figure 6), reference burst (Figure 7), etc. Neurology and hot spots and trending medical education research.
4.2.1 Neurophobia in neurological medical education
Neurophobia, defined as the fear or aversion to studying and understanding neurology, is a well-documented phenomenon within medical education. Coined in 1994 by Jozefowicz (1994), the term encapsulates the reluctance exhibited by medical students and professionals to engage deeply with neurology, primarily due to its perceived complexity.
Neurology often receives less emphasis compared to other medical specialties. Short rotations and fragmented courses contribute to insufficient familiarity with the subject (Flanagan et al., 2007; Youssef, 2009). The detailed neuroanatomy, neurophysiology, and diagnostic tools presented in a condensed format can overwhelm students, reinforcing the perception of neurology as a challenging field (Matthias et al., 2013). Traditional lectures frequently fail to contextualize theoretical knowledge within clinical scenarios, leaving students unprepared for practical applications. As a result, students often perceive neurology questions as disproportionately difficult, which further discourages them from studying the subject (Ridsdale, 2009). Additionally, neurophobia may significantly impact medical education; students may avoid engaging deeply with neurology, leading to gaps in their knowledge and skills (Zinchuk et al., 2010; Han et al., 2024). This fear can deter students from pursuing neurology as a specialty, exacerbating the shortage of neurologists in many regions (Solorzano and Józefowicz, 2015). Consequently, general practitioners and other specialists may lack confidence in addressing neurological complaints, potentially resulting in misdiagnoses, delayed care, or over-referrals (Freeman et al., 2013).
To address this situation, several strategies should be considered. Integrating neurology earlier and more extensively into the medical curriculum can help demystify the subject (Walzman and Luzzi, 2005). Courses should maintain a balance between foundational knowledge and clinical applications. Innovative teaching methods such as problem-based learning, simulations, virtual reality, and flipped classrooms can enhance student engagement (Jao et al., 2005; Anwar et al., 2015; Hudson, 2006; Wiles, 2013). Longer neurology rotations and mentorship programs with neurologists can also boost students' confidence and interest in the field (Ridsdale et al., 2007). Furthermore, addressing stereotypes and fostering a culture of curiosity rather than fear can encourage students to approach neurology with an open mind (Tan et al., 2011). Addressing neurophobia can enable students to more effectively comprehend complex neuroanatomical, physiological, and pathological mechanisms, thereby forming a more robust knowledge network. Overcoming fear allows students to analyze neurological cases more calmly and objectively, perform localization and qualitative diagnoses, formulate reasonable treatment plans, and reduce misdiagnoses or delays caused by avoidance. By enhancing interest and reducing psychological barriers in career choices, it helps increase the number of applicants for neurology residency programs, alleviating the global shortage of neurologists.
4.2.2 Resident education in neurology medical education
Neurology residency programs represent a critical phase in the education and training of future neurologists, facilitating the transition of medical graduates from foundational knowledge to specialized clinical expertise (Song A. et al., 2024; Sutherland et al., 2024). Effective resident education in neurology must encompass a wide array of competencies, ranging from diagnostic precision to empathetic patient care, while also adapting to advancements in medical science and healthcare systems (Cavallieri et al., 2025).
Residents encounter a diverse spectrum of neurological conditions, including stroke, epilepsy, neurodegenerative diseases, and neuromuscular disorders (Talai et al., 2024; Williams et al., 2022; Reis-Carneiro et al., 2024). Through supervised patient care, residents gain confidence in conducting neurological examinations, interpreting diagnostic studies, and formulating treatment plans. Training in procedures such as lumbar punctures, EEG interpretation, and botulinum toxin injections equips residents with essential practical skills (Sheikh et al., 2024). Many programs encourage or mandate participation in research projects, thereby allowing residents to contribute to the advancement of the field of neurology (Reis-Carneiro et al., 2024; Gottlieb-Smith et al., 2024). Given the rigorous demands of neurology residency, programs are increasingly integrating wellness initiatives to support residents' mental health and promote a healthy work-life balance.
Neurology encompasses vast and rapidly evolving fields, necessitating that residents master complex concepts while maintaining clinical proficiency. However, residents often contend with long hours and heavy workloads, which limit opportunities for self-directed learning and research (Raza et al., 2022). The emotional toll of neurological residency can be significant, given the chronic or life-threatening nature of many neurological diseases. Therefore, it is essential to implement strategies that enhance the education of neurology residents (Valencia et al., 2016). Incorporating active learning methods, such as simulation-based training and case-based discussions, can improve engagement and practical skills (George et al., 2018; Adams et al., 2018). Additionally, experienced neurologists can offer valuable guidance on career development, research opportunities, and coping strategies to manage the demands of residency (Lamb et al., 2022). Collaborative learning with other specialties promotes a holistic approach to patient care (Edmunds and Brown, 2010; Shalev and Jacoby, 2019). Encouraging participation in research and quality improvement projects fosters critical thinking and innovation skills.
Through curriculum innovation, mentorship, and a strong emphasis on interdisciplinary collaboration, neurology residency programs can effectively prepare residents to provide high-quality, compassionate neurological care while simultaneously advancing the field through research and leadership (Ten Cate and Durning, 2007). Resident education facilitates the transition of neurological knowledge into clinical skills, cultivates the clinical thinking of residents, establishes a cognitive system for neurological diseases, and enhances students' clinical diagnostic capabilities. Research in this area is beneficial for reserving clinical physicians in neurology and promoting the development of the discipline.
4.2.3 The medical education in developmental neurology
Developmental neurology, the study of growth, maturation, and disorders of the nervous system across the lifespan, is a crucial component of neurology medical education (Sanders et al., 2024). A thorough understanding of developmental processes is essential for accurately diagnosing and managing a variety of neurological conditions, particularly those that affect children and young adults (Robbins et al., 2017).
This field provides valuable insights into the structural and functional maturation of the brain and nervous system, which is critical for comprehending how deviations from typical development can lead to neurological disorders. Many developmental neurological conditions have lifelong implications; therefore, neurologists must be well-versed in the progression of these disorders to deliver age-appropriate care and anticipate future challenges (Scher, 2024).
However, medical students and residents often have limited opportunities to observe and manage pediatric and developmental neurological cases, particularly in programs lacking dedicated pediatric neurology rotations (Robbins et al., 2017; Marzolf et al., 2022; Gorelick et al., 2024). Furthermore, advances in neurogenetics, neuroimaging, and developmental neuroscience continually reshape our understanding of these conditions, necessitating ongoing updates to educational content. Developmental neurology frequently intersects with other disciplines, such as pediatrics, psychiatry, and rehabilitation medicine, which can complicate the delineation of roles and responsibilities in multidisciplinary care (Shalev and Jacoby, 2019; Juul et al., 2019; Gilbert et al., 2013).
Developmental neurology should be integrated throughout the continuum of medical education, beginning with preclinical courses in neuroanatomy and neurophysiology and extending to clinical rotations that emphasize pediatric neurology (Scher, 2024). Case studies that involve real-world scenarios are essential for contextualizing theoretical knowledge and demonstrating the practical application of developmental neurology concepts (Eyre et al., 2024; Aminoff et al., 2007). Additionally, training must prioritize effective communication with families, advocacy for necessary resources, and the consideration of psychosocial factors associated with developmental neurological conditions (Mohammad et al., 2024; Mohammad, 2024). Promoting developmental neurology medical education helps to address the shortcomings of traditional neurology teaching in the dynamic processes of development, fostering interdisciplinary diagnostic and therapeutic thinking. This can reflect the application of ethical and humanistic education in medical education.
4.3 Outlook and limitations
This study represents the first bibliometric analysis systematically examining publications in neurology and medical education over the past two decades. Unlike traditional reviews, bibliometric analysis offers a novel and objective perspective on the evolving trends within this research field. We employed various bibliometric software tools for analysis, yielding more results across multiple dimensions (Shen et al., 2022). This study aims to enhance public understanding of the significance of neurology in medical education, provide scholars with a comprehensive overview of research in this area, and offer objective guidance for the future development of neurology and medical education research. However, this study has certain limitations. Firstly, we exclusively searched the WoSCC database for published English articles, thereby excluding non-WoSCC and non-English publications. Nonetheless, English articles in WoSCC are the most frequently utilized data source in bibliometrics and can represent a substantial portion of the relevant information. Secondly, the bibliometric methodology relies on natural language processing, which may introduce biases, as noted in other bibliometric studies (Yan et al., 2021). Despite these limitations, our findings provide a more comprehensive and objective overview of the field. Furthermore, the sample reflects the current volume of research on neurology and medical education, indicating that this area is an emerging direction for future inquiry.
5 Conclusion
In summary, research on neurology and medical education has progressed steadily over the past two decades, characterized by active collaboration. The United States holds a prominent position in this research domain. Donald L. Gilbert has published the highest number of articles, while Jozefowicz Ralph F. is the most frequently co-cited author. Neurophobia in neurology medical education remains a prevalent research topic, contributing to a better understanding of the interplay between neurology and medical education. Emerging areas of focus include resident education, medical education training, developmental neurology, and parental involvement, which may offer guidance and new insights for future research in the field of neurology medical education.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
YF: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft. ZW: Conceptualization, Formal analysis, Investigation, Resources, Software, Writing – original draft. YZ: Conceptualization, Data curation, Formal analysis, Investigation, Software, Writing – original draft. GH: Conceptualization, Data curation, Formal analysis, Methodology, Software, Writing – original draft. ZC: Conceptualization, Data curation, Formal analysis, Software, Writing – original draft. GZ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Writing – original draft. JiF: Conceptualization, Data curation, Formal analysis, Investigation, Software, Supervision, Writing – original draft. JuF: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Basic and Applied Basic Research Fund of Guangdong Province (2022A1515220024), the Basic and Applied Basic Research Fund of Guangzhou science project (2024A04J3630), Guangzhou Medical Key Discipline Construction Project (2025-2027).
Acknowledgments
Each author contributed important content during manuscript drafting or revision and accepts accountability for the overall work, and all the authors agreed on the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2025.1610465/full#supplementary-material
References
Abbasi, F., Ayremlu, P., and Niazkhani, Z. (2025). From classroom to clinic: evaluating a clinical pathology course to strengthen pathology report literacy of medical interns. BMC Med. Educ. 25:490. doi: 10.1186/s12909-025-07001-4
Adams, T., Newton, C., Patel, H., Sulistio, M., Tomlinson, A., Lee, W., et al. (2018). Resident versus faculty member simulation debriefing. Clin. Teach. 15, 462–466. doi: 10.1111/tct.12735
Albert, D. V., Yin, H., Amidei, C., Dixit, K. S., Brorson, J. R., Lukas, R. V., et al. (2015). Structure of neuroscience clerkships in medical schools and matching in neuromedicine. Neurology 85, 172–176. doi: 10.1212/WNL.0000000000001731
Aminoff, M. J., Massey, J. M., Scheiber, S. C., and Juul, D. (2007). American Board of P, Neurology: certification in neuromuscular medicine: a new neurologic subspecialty. Muscle Nerve 35, 409–410. doi: 10.1002/mus.20763
An, L., Qin, J., Jiang, W., Luo, P., Luo, X., Lai, Y., et al. (2023). Non-invasive and accurate risk evaluation of cerebrovascular disease using retinal fundus photo based on deep learning. Front. Neurol. 14:1257388. doi: 10.3389/fneur.2023.1257388
Anwar, K., Shaikh, A. A., Sajid, M. R., Cahusac, P., Alarifi, N. A., Al Shedoukhy, A., et al. (2015). Tackling student neurophobia in neurosciences block with team-based learning. Med. Educ. Online 20:28461. doi: 10.3402/meo.v20.28461
Ateş, E., and Korkmaz, E. K. (2025). Randomized control trial in nursing education: a bibliometric analysis and visualization. Nurse Educ. Pract. 86:104394. doi: 10.1016/j.nepr.2025.104394
Cavallieri, F., Sellner, J., Akhvlediani, T., Bassetti, C. L., Bereczki, D., Fanciulli, A., et al. (2025). The European academy of neurology NeuroCOVID-19 task force: a lesson for the future. Eur. J. Neurol. 32:e16321. doi: 10.1111/ene.16321
Chhetri, S. K. (2017). E-learning in neurology education: principles, opportunities and challenges in combating neurophobia. J. Clin. Neurosci. 44, 80–83. doi: 10.1016/j.jocn.2017.06.049
Edmunds, S., and Brown, G. (2010). Effective small group learning: AMEE Guide No. 48. Med. Teach. 32, 715–726. doi: 10.3109/0142159X.2010.505454
Eyre, H. A., Hynes, W., Ayadi, R., Manes, F., and Swieboda, P. (2024). Brain capital is crucial for global sustainable development. Lancet Neurol. 23, 233–235. doi: 10.1016/S1474-4422(24)00031-0
Flanagan, E., Walsh, C., and Tubridy, N. (2007). 'Neurophobia'–attitudes of medical students and doctors in Ireland to neurological teaching. Eur. J. Neurol. 14, 1109–1112. doi: 10.1111/j.1468-1331.2007.01911.x
Freeman, W. D., Vatz, K. A., Griggs, R. C., and Pedley, T. (2013). The workforce task force report: clinical implications for neurology. Neurology 81, 479–486. doi: 10.1212/WNL.0b013e31829d8783
Gelb, D. J., Gunderson, C. H., Henry, K. A., Kirshner, H. S., and Józefowicz, R. F. (2002). The neurology clerkship core curriculum. Neurology 58, 849–852. doi: 10.1212/WNL.58.6.849
George, J. R., Tyroch, A. H., and Milan, S. A. (2018). Third-year medical student impressions of resident teaching in simulated and clinical settings. Am. Surgeon 84, 334–337. doi: 10.1177/000313481808400314
Gilbert, D. L., Patterson, M. C., Pugh, J. A., Ridel, K. R., Reynolds, T. Q., Valencia, I., et al. (2013). Views of recently first-certified US child neurologists on their residency training. J. Child Neurol. 28, 332–339. doi: 10.1177/0883073812473644
Gorelick, P. B., Hainsworth, A. H., and Wallin, A. (2024). What will it take to achieve brain health globally? Cereb. Circ. 6:100209. doi: 10.1016/j.cccb.2024.100209
Gottlieb-Smith, R., Rogers, D., and Gilbert, D. L. (2024). Modified delphi study to establish consensus about child neurology residency education: next-gen training. Neurology 103:e210002. doi: 10.1212/WNL.0000000000210002
Han, F., Zhang, D. D., Zhang, Y., Zhou, L. X., Zhu, Y. C., Ni, J., et al. (2024). Prevalence of neurophobia among medical students and young doctors: a systematic review and meta-analysis. BMC Med. Educ. 24:1286. doi: 10.1186/s12909-024-06303-3
Hassell, L. A., Absar, S. F., Chauhan, C., Dintzis, S., Farver, C. F., Fathima, S., et al. (2023). Pathology education powered by virtual and digital transformation: now and the future. Arch. Pathol. Lab. Med. 147, 474–491. doi: 10.5858/arpa.2021-0473-RA
Hudson, J. N. (2006). Linking neuroscience theory to practice to help overcome student fear of neurology. Med. Teach. 28, 651–653. doi: 10.1080/01421590600726409
Jao, C. S., Brint, S. U., and Hier, D. B. (2005). Making the neurology clerkship more effective: can e-textbook facilitate learning? Neurol. Res. 27, 762–767. doi: 10.1179/016164105X35639
Jozefowicz, R. F. (1994). Neurophobia: the fear of neurology among medical students. Arch. Neurol. 51, 328–329. doi: 10.1001/archneur.1994.00540160018003
Jukna, Š., Puteikis, K., and Mameniškiene, R. (2023). Perception of neurology among undergraduate medical students - what can be done to counter neurophobia during clinical studies? BMC Med. Educ. 23:447. doi: 10.1186/s12909-023-04405-y
Juul, D., Lyness, J. M., Thomas, C. R., and Faulkner, L. R. (2019). Primary care and neurology in psychiatry residency training: a survey of early career psychiatrists. Acad. Psychiatry 43, 51–55. doi: 10.1007/s40596-018-0922-6
Karlapudi, V., Paleti, S. T., Kambhampati, S. B. S., and Vaishya, R. (2022). Bibliometric analysis of orthopaedic related publications by Indian authors from the last decade. J. Clin. Orthop. Trauma 25:101775. doi: 10.1016/j.jcot.2022.101775
Lamb, C. R., Guerra, S., and Sorensen, M. J. (2022). Qualities of excellent resident and attending teachers recognized by medical students: a qualitative analysis of nominations for surgical clerkship teaching awards. Am. J. Surg. 224, 552–556. doi: 10.1016/j.amjsurg.2022.02.004
Lattouf, O. M. (2022). Impact of digital transformation on the future of medical education and practice. J. Card. Surg. 37, 2799–2808. doi: 10.1111/jocs.16642
Marzolf, B. A., Plegue, M. A., Okanlami, O., Meyer, D., and Harper, D. M. (2022). Are medical students adequately trained to care for persons with disabilities? PRiMER 6:34. doi: 10.22454/PRiMER.2022.878147
Matthias, A. T., Nagasingha, P., Ranasinghe, P., and Gunatilake, S. B. (2013). Neurophobia among medical students and non-specialist doctors in Sri Lanka. BMC Med. Educ. 13:164. doi: 10.1186/1472-6920-13-164
Mohammad, K. (2024). Standardizing clinician training and patient care in the neonatal neurocritical care: a step-by-step guide. Semin. Perinatol. 48:151924. doi: 10.1016/j.semperi.2024.151924
Mohammad, K., Molloy, E., and Scher, M. (2024). Training in neonatal neurocritical care: a case-based interdisciplinary approach. Semin. Fetal Neonat. Med. 29:101530. doi: 10.1016/j.siny.2024.101530
Pakpoor, J., Handel, A. E., Disanto, G., Davenport, R. J., Giovannoni, G., Ramagopalan, S. V., et al. (2014). National survey of UK medical students on the perception of neurology. BMC Med. Educ. 14:225. doi: 10.1186/1472-6920-14-225
Paunkov, A., Chartoumpekis, D. V., Ziros, P. G., and Sykiotis, G. P. (2019). A bibliometric review of the Keap1/Nrf2 pathway and its related antioxidant compounds. Antioxidants 8:353. doi: 10.3390/antiox8090353
Raskurazhev, A., Kuznetsova, P., Khizhnikova, A. E., Klochkov, A., Bakulin, I., Annushkin, V., et al. (2021). Neuropoly: an educational board game to facilitate neurology learning. Front. Syst. Neurosci. 15:688210. doi: 10.3389/fnsys.2021.688210
Raza, M., Madhwani, A., Jehan, F., and Saeed, S. (2022). Perspectives of residents, students and faculty about residents as teachers at a University Hospital in Karachi. J. Pak. Med. Assoc. 72, 714–744. doi: 10.47391/JPMA.1361
Reis-Carneiro, D., Skoric, M. K., Habek, M., Adamec, I., Calandra-Buonaura, G., Cortelli, P., et al. (2024). Autonomic nervous system education in Europe: EAN/EFAS/INUS survey on curricula and skills in autonomic medicine of European neurology residents and consultants. Eur. J. Neurol. 31:e16515. doi: 10.1111/ene.16515
Ridsdale, L. (2009). No more neurophobia: welcome neurology in general practice. Brit. J. Gen. Pract. 59, 567–569. doi: 10.3399/bjgp09X453756
Ridsdale, L., Massey, R., and Clark, L. (2007). Preventing neurophobia in medical students, and so future doctors. Pract. Neurol. 7, 116–123.
Robbins, M. S., Haut, S. R., Lipton, R. B., Milstein, M. J., Ocava, L. C., Ballaban-Gil, K., et al. (2017). A dedicated scholarly research program in an adult and pediatric neurology residency program. Neurology 88, 1366–1370. doi: 10.1212/WNL.0000000000003626
Sanders, J. S., Williams, K., Thompson, D., and Shapiro, H. F. (2024). Enhancing comfort of resident physicians treating adults with intellectual and developmental disabilities by facilitating meaningful interactions. Front. Med. 11:1264958. doi: 10.3389/fmed.2024.1264958
Scher, M. S. (2024). Interdisciplinary fetal-neonatal neurology training improves brain health across the lifespan. Front. Neurol. 15:1411987. doi: 10.3389/fneur.2024.1411987
Shalev, D., and Jacoby, N. (2019). Neurology training for psychiatry residents: practices, challenges, and opportunities. Acad. Psychiatry. 43, 89–95. doi: 10.1007/s40596-018-0932-4
Sheikh, I. S., Katyal, R., Hadjinicolaou, A., Bibby, B. M., Olandoski, M., Nascimento, F. A., et al. (2024). The online educational tool “Roadmap to EEGs” significantly improved trainee performance in recognizing EEG patterns. Epileptic. Disord. 26, 435–443. doi: 10.1002/epd2.20227
Shen, J., Shen, H., Ke, L., Chen, J., Dang, X., Liu, B., et al. (2022). Knowledge mapping of immunotherapy for hepatocellular carcinoma: a bibliometric study. Front. Immunol. 13:815575. doi: 10.3389/fimmu.2022.815575
Shiels, L., Majmundar, P., Zywot, A., Sobotka, J., Lau, C. S. M., Jalonen, T. O., et al. (2017). Medical student attitudes and educational interventions to prevent neurophobia: a longitudinal study. BMC Med. Educ. 17:225. doi: 10.1186/s12909-017-1055-4
Solorzano, G. E., and Józefowicz, R. F. (2015). Neurophobia: a chronic disease of medical students. Neurology 85, 116–117. doi: 10.1212/WNL.0000000000001751
Song, A., Safdieh, J. E., and Robbins, M. S. (2024). Group text messaging as a residency teaching tool in outpatient neurology and headache: a mixed-methods observational study. Headache. 65, 539–544. doi: 10.1111/head.14870
Song, C., Yao, L., Song, Y., and Liu, L. (2024). The hotspots and trends of nursing master's education in China: a bibliometric analysis from 2000 to 2022. BMC Med. Educ. 24:1082. doi: 10.1186/s12909-024-06005-w
Sutherland, H. W., Moeller, J. J., and Schaefer, S. M. (2024). Education research: what medical students value in neurology residents: a qualitative study to inform resident as teacher curricula. Neurol. Educ. 3:e200135. doi: 10.1212/NE9.0000000000200135
Talai, A., Freedman, D. A., and Albert, D. V. F. (2024). Education research: educating child neurology residents about psychogenic nonepileptic seizures: a needs assessment. Neurol. Educ. 3:e200111. doi: 10.1212/NE9.0000000000200111
Tan, N. C., Kandiah, N., Chan, Y. H., Umapathi, T., Lee, S. H., Tan, K., et al. (2011). A controlled study of team-based learning for undergraduate clinical neurology education. BMC Med. Educ. 11:91. doi: 10.1186/1472-6920-11-91
Ten Cate, O., and Durning, S. (2007). Dimensions and psychology of peer teaching in medical education. Med. Teach. 29, 546–552. doi: 10.1080/01421590701583816
Valencia, I., Feist, T. B., and Gilbert, D. L. (2016). Program director survey: attitudes regarding child neurology training and testing. Pediatr. Neurol. 57, 17–21. doi: 10.1016/j.pediatrneurol.2015.12.011
Walzman, M., and Luzzi, G. A. (2005). Foundation training and genitourinary medicine. Sexually Transmitted Infect. 81:99. doi: 10.1136/sti.2004.014423
Wiles, C. M. (2013). Introducing neurological examination for medical undergraduates–how I do it. Pract. Neurol. 13, 49–50. doi: 10.1136/practneurol-2012-000282
Williams, S., Raheim, S. A., Khan, M. I., Rubab, U., Kanagala, P., Zhao, S. S., et al. (2022). Cardiac autonomic neuropathy in type 1 and 2 diabetes: epidemiology, pathophysiology, and management. Clin. Ther. 44, 1394–1416. doi: 10.1016/j.clinthera.2022.09.002
Woltman, H. W. (1950). Presidential address: the neurologic aspect of the Minnesota experiment in graduate medical education; a personal accounting. Trans. Am. Neurol. Assoc. 51, 1–7.
Yan, W. T., Lu, S., Yang, Y. D., Ning, W. Y., Cai, Y., Hu, X. M., et al. (2021). Research trends, hot spots and prospects for necroptosis in the field of neuroscience. Neural Regener. Res. 16, 1628–1637. doi: 10.4103/1673-5374.303032
Youssef, F. F. (2009). Neurophobia and its implications: evidence from a Caribbean medical school. BMC Med. Educ. 9:39. doi: 10.1186/1472-6920-9-39
Keywords: bibliometric analysis, neurology, medical education, neurophobia, higher education
Citation: Fan Y, Wang Z, Zhang Y, Hu G, Cao Z, Zeng G, Fu J and Fu J (2025) Trends in neurology medical education: a bibliometric analysis (2000–2023). Front. Educ. 10:1610465. doi: 10.3389/feduc.2025.1610465
Received: 12 April 2025; Accepted: 09 June 2025;
Published: 25 June 2025.
Edited by:
Nina Pereza, University of Rijeka, CroatiaReviewed by:
Cleci Werner da Rosa, The University of Passo Fundo, BrazilCarlos Quispe-Vicuña, National University of San Marcos, Peru
Copyright © 2025 Fan, Wang, Zhang, Hu, Cao, Zeng, Fu and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiaming Fu, MTgzNzc0NzMwN0BxcS5jb20=; Junyi Fu, ZnVqdW55aUBnemhtdS5lZHUuY24=
†These authors have contributed equally to this work
 Yongxiang Fan1,2†
Yongxiang Fan1,2† Guangxin Hu
Guangxin Hu Jiaming Fu
Jiaming Fu Junyi Fu
Junyi Fu