- 1Pediatric Oncology Unit, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy
- 2Department of Woman and Child Health and Public Health, Università Cattolica del Sacro Cuore, Rome, Italy
- 3National Etruscan Museum of Villa Giulia, Rome, Italy
- 4Ministry of Cultural Heritage and Activities and Tourism, Rome, Italy
Pediatric oncology patients face multifaceted challenges extending beyond disease pathophysiology and therapeutic interventions. Cancer treatment frequently disrupts fundamental developmental processes, compromising physical and emotional functioning, social relationships, and cognitive maturation. While conventional biomedical approaches remain essential for disease control, they inadequately address the comprehensive psychosocial needs of children requiring sustained therapeutic support. To address these unmet psychosocial needs, the initiative draws on principles from museum education and arts-in-health, integrating cultural engagement as a therapeutic strategy within pediatric oncology care. The ETRUscan museum For Kids (ETRU4KIDS) program represents an innovative interdisciplinary collaboration between the Pediatric Oncology Department at Fondazione Gemelli IRCCS and Rome’s National Etruscan Museum of Villa Giulia. This initiative demonstrates how cultural institutions can serve as therapeutic adjuvants, providing evidence-based psychosocial interventions that specifically target emotional processing, quality of life optimization, and psychological resilience enhancement tailored to pediatric developmental requirements. The protocol incorporates structured museum experiences, interactive educational workshops, and Etruscan-inspired ceramic art therapy sessions designed to create therapeutic environments where cultural engagement and creative expression facilitate psychological healing. A prospective observational study enrolled 25 pediatric oncology patients. Outcome measures utilized validated assessment instruments including the Visual Analogue Scale (VAS), Arts Observation Scale (ArtsObS), and Pediatric Quality of Life Inventory (PedsQL). Results demonstrated statistically significant improvements: emotional wellbeing showed VAS score increases of 3.2 ± 1.4 points (p < 0.001), creative engagement reflected 42% ArtsObS score enhancement (p < 0.01), and overall quality of life exhibited 18% PedsQL improvement (p < 0.01). ETRU4KIDS provides a replicable framework for integrating cultural-artistic interventions into comprehensive pediatric oncology care.
Introduction
Childhood cancer diagnosis profoundly disrupts family dynamics and developmental trajectories, extending far beyond immediate medical concerns. Contemporary pediatric oncology has achieved remarkable survival improvements, with cure rates exceeding 80% for many childhood malignancies (Hunger et al., 2012). Nonetheless, the intervention’s immediate benefits have exposed a range of complex, long-lasting consequences—such as cognitive impairments, enduring psychological distress, and impaired social development—that persist after treatment concludes. The sterile hospital environment, while medically essential, often causes psychological distress in young patients. Clinical settings typically lack the warmth and familiarity children require for optimal emotional regulation and developmental continuity. This environmental challenge has catalyzed innovative approaches to humanizing healthcare spaces while maintaining medical safety standards.
Health-related quality of life research in pediatric oncology has evolved to recognize that effective treatment must preserve childhood’s essential elements alongside disease management (Varni et al., 2001). Several pioneering initiatives demonstrate the therapeutic potential of museum-based interventions in healthcare settings. The Victoria and Albert Museum’s Hospital Outreach program in the United Kingdom exemplifies how museum resources and creative tools can be brought directly into clinical contexts to promote engagement and empowerment among pediatric patients. Similar innovative programs documented in the American Alliance of Museums report “Museums On Call: How Museums Are Addressing Health Issues” showcase successful implementations across diverse healthcare settings, providing evidence that ETRU4KIDS builds upon an established foundation while offering unique features.
The World Health Organization’s comprehensive evidence review supporting arts and cultural engagement in health promotion has validated these approaches across diverse populations (Fancourt and Finn, 2019). Recent systematic reviews have further substantiated the therapeutic value of cultural interventions, demonstrating significant benefits for psychological wellbeing, social connection, and cognitive function across various pediatric populations (Fancourt and Finn, 2019; Fraser et al., 2015).
Museum-based health interventions represent a particularly promising development in the intersection of cultural heritage and therapeutic practice. Museums, as non-formal educational environments, possess unique characteristics that distinguish them from traditional therapeutic settings: they offer culturally rich, aesthetically stimulating spaces that promote curiosity, wonder, and social interaction (Silverman, 2010; Chatterjee and Noble, 2013). The museum context provides what Hooper-Greenhill (2007) describes as “transformative learning environments” where individuals can engage with cultural heritage in personally meaningful ways, fostering identity development and social connection.
The therapeutic potential of museum environments has been increasingly recognized in healthcare contexts. Studies by Ander et al. (2013) and Thomson et al. (2018) demonstrate that museum-based interventions can reduce anxiety, improve mood, and enhance social engagement among vulnerable populations. Museums offer what Dodd and Jones (2014) term “safe spaces for risk-taking,” where individuals can explore new identities and experiences without the clinical pressures often associated with traditional therapeutic settings.
Beyond immediate psychological benefits, museum engagement can provide enduring psychosocial resources, aligning with theoretical frameworks such as Bourdieu’s concept of cultural capital. Cultural heritage engagement activates multiple therapeutic mechanisms simultaneously. According to Bourdieu’s theory of cultural capital, engagement with cultural institutions provides individuals with resources for meaning-making and identity construction (Bourdieu, 2002). For children in oncology care, such engagement not only offers emotional respite but also supports developmental continuity and resilience during prolonged medical treatment. This is particularly significant as illness often disrupts normal identity development processes. Museums provide alternative contexts for exploring self-concept and maintaining connections to broader cultural narratives beyond the medical experience (Newman et al., 2013).
The sensory and aesthetic dimensions of museum environments contribute additional therapeutic benefits. Environmental psychology research demonstrates that exposure to beautiful, meaningful spaces can reduce cortisol levels, activate reward centers in the brain, and promote psychological wellbeing (Vessel et al., 2013; Menninghaus et al., 2017). These neurobiological responses provide the foundation for observable improvements in mood, attention, and social engagement documented in museum-based health interventions.
This biopsychosocial model provides the primary conceptual foundation, recognizing health and illness as products of complex interactions among biological, psychological, and social factors (Engel, 2012). Contemporary developments in this model emphasize the importance of environmental and cultural factors in health outcomes, with recent research demonstrating that social determinants and cultural engagement significantly influence treatment adherence, psychological resilience, and long-term recovery (Marmot and Wilkinson, 2016; Clift et al., 2009). Effective therapeutic interventions must therefore address multiple experiential dimensions simultaneously.
Recent advances in neuroscience have clarified how aesthetic and cultural experiences can modulate physiological and psychological processes that impact health outcomes. Neuroimaging studies demonstrate that art engagement activates reward centers, reduces stress-related neural network activity, and promotes neurotransmitter release associated with wellbeing (Vessel et al., 2012). Subsequent research has identified specific neural pathways through which cultural engagement influences health outcomes, including activation of the default mode network associated with self-reflection and meaning-making (Belfi et al., 2019; Sachs et al., 2016). This emerging evidence provides biological plausibility for therapeutic effects observed in arts-based health interventions.
Developmental perspectives are particularly crucial for pediatric populations. Childhood and adolescence represent periods of rapid growth across cognitive, emotional, social, and physical domains. Cancer treatment can significantly disrupt normal developmental processes, potentially causing long-term impacts on academic achievement, social relationships, and psychological adjustment (Schulte and Barrera, 2010). Cultural and educational interventions that maintain engagement with learning, creativity, and social interaction can support continued development despite challenging treatment circumstances. Positive psychology contributes important insights into factors promoting human flourishing and resilience during adversity (Seligman, 2011). This field emphasizes positive emotions, engagement, relationships, meaning, and accomplishment as fundamental to psychological wellbeing. Museum-based interventions naturally align with these principles by providing positive emotional experiences, meaningful cultural engagement, social connections, and creative accomplishment opportunities.
ETRU4KIDS: a collaborative model for museum-based therapeutic interventions
The ETRU4KIDS project emerged from recognition that pediatric oncology care benefits from meaningful partnerships with cultural institutions. The collaboration between Gemelli’s Pediatric Oncology Unit and the National Etruscan Museum represents a systematic effort to formalize therapeutic benefits through structured cultural programming.
This partnership reflects growing healthcare awareness that healing environments extend beyond traditional clinical boundaries (Stuckey and Nobel, 2010; Camic and Chatterjee, 2013). The pediatric oncology team recognized their patients’ need for normalcy, creativity, and joy alongside intensive medical treatment. Museum professionals simultaneously sought to extend their educational mission to vulnerable community populations.
The program development process involved extensive collaboration between healthcare professionals, museum educators, art therapists, and child psychologists to ensure interventions were both therapeutically sound and developmentally appropriate. Initial pilot sessions were conducted with small groups to refine protocols and assess feasibility before full program implementation.
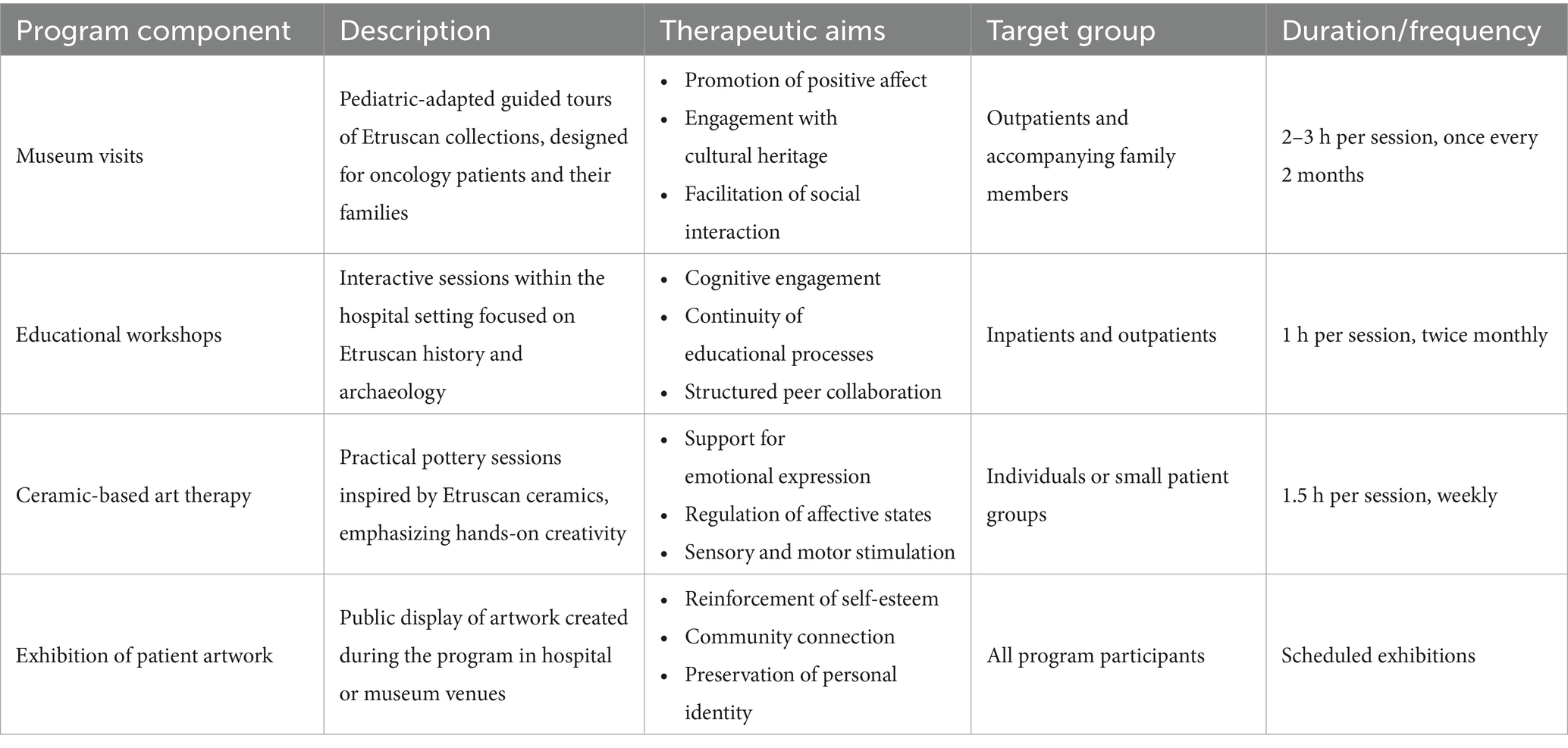
The formal partnership encompasses four interconnected components providing comprehensive therapeutic and educational benefits (Table 1). Guided museum visits form the program cornerstone, offering patients and families opportunities to engage with Etruscan art and culture through specially designed tours accommodating physical and emotional needs of individuals undergoing medical treatment. These visits are structured around the principles of “slow looking” and dialogical engagement, encouraging deep observation and personal reflection rather than information transmission (Burnham and Kai-Kee, 2011).
Educational workshops extend museum experiences into hospital settings, delivering cultural content and interactive learning opportunities to patients unable to participate in off-site activities. These sessions utilize multimedia presentations, hands-on activities, and creative projects exploring Etruscan civilization while complementing formal hospital education services. Workshop design incorporates universal design for learning principles to accommodate diverse cognitive abilities and learning styles among participants (Meyer et al., 2014).
Ceramic therapy sessions represent the program’s most innovative component, combining therapeutic benefits of tactile creative expression with cultural education about Etruscan artistic traditions. These sessions involve collaboration with the Lene Thun Foundation, bringing professional ceramicists into hospital environments to work alongside psychologists and healthcare providers. The ceramic work process provides what art therapists term “embodied learning,” where physical manipulation of materials facilitates emotional processing and stress reduction through sensory engagement (Sholt and Gavron, 2006).
Exhibition opportunities provide meaningful culmination experiences, creating platforms for sharing creative work with broader community audiences while celebrating patient achievements and raising pediatric oncology awareness. These exhibitions serve multiple functions: recognizing patient accomplishments, creating community engagement opportunities, and demonstrating continued creativity and capability of children facing serious illness.
Methodology and assessment
This prospective observational study was conducted at the Pediatric Oncology Unit of Fondazione Policlinico Universitario Agostino Gemelli IRCCS in Rome, Italy, in collaboration with the National Etruscan Museum of Villa Giulia. The study employed a single-group pre-post intervention design with multiple assessment points to evaluate the therapeutic effects of the ETRU4KIDS program.
Program components were delivered across two primary locations based on intervention type and patient needs. Museum visits were conducted on-site at the National Etruscan Museum of Villa Giulia, providing authentic cultural immersion experiences. Public exhibitions were programmed at both the museum and hospital settings to maximize accessibility. Educational workshops and ceramic-based art therapy sessions were delivered within the hospital to accommodate patients with mobility restrictions or medical contraindications to off-site activities.
A total of 25 pediatric oncology patients participated in the study. Inclusion criteria were: (1) ages 6–17 years, (2) confirmed oncological diagnosis, (3) stable medical condition allowing participation in cultural activities, (4) informed consent from parents/guardians, and (5) expected treatment duration of at least 3 months. Exclusion criteria included: (1) severe cognitive impairment preventing program participation, (2) active psychosis or severe psychiatric conditions, (3) isolation precautions preventing group activities, and (4) terminal prognosis with life expectancy <3 months.
Participant demographics were as follows: mean age 11.4 ± 3.2 years (range 6–17), 14 males (56%), and 11 females (44%). Primary diagnoses included solid tumors (n = 15, 60%), brain tumors (n = 6, 24%), and other hematological malignancies (n = 4, 16%).
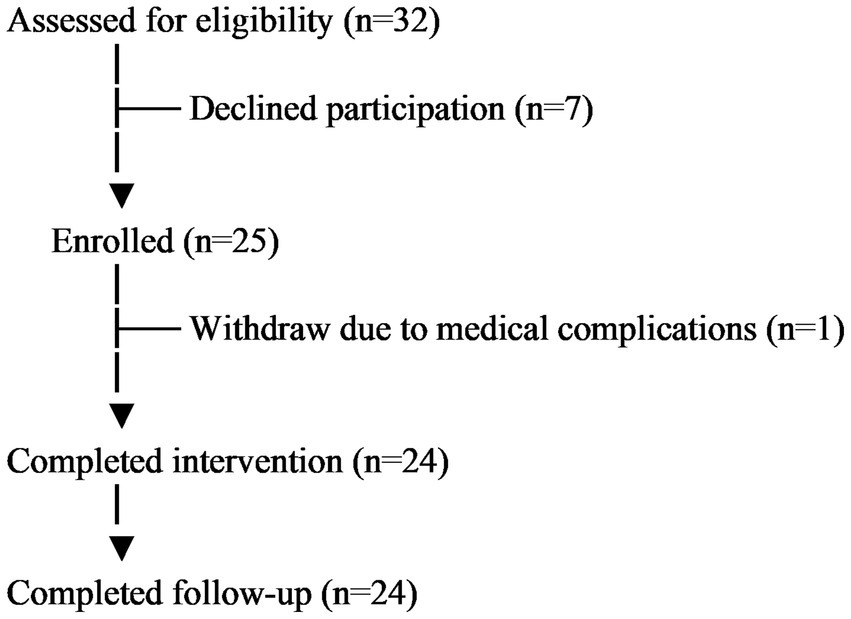
Patients were recruited through referrals from the pediatric oncology medical team during routine clinical visits. Research staff approached eligible families to explain the study and obtain informed consent. The recruitment process emphasized voluntary participation and clarified that program participation would not affect medical care. A total of 32 families were approached, with seven declining participation (response rate: 78%).
Activities were scheduled to accommodate medical treatment schedules, with flexibility for rescheduling based on patient condition. Each session was facilitated by trained museum educators working in collaboration with child life specialists and art therapists.
The ETRU4KIDS program incorporates assessment methodologies designed to capture multifaceted therapeutic benefits while maintaining sensitivity to practical constraints of pediatric oncology populations. The assessment framework reflects contemporary best practices in pediatric health services research while acknowledging unique challenges of evaluating complex psychosocial interventions in vulnerable populations (Camic and Chatterjee, 2013).
A mixed-methods approach combines validated quantitative instruments with qualitative observational data to provide comprehensive evaluation of participant experiences and outcomes. This methodological diversity recognizes that cultural and artistic intervention benefits may be expressed through multiple channels not captured by single assessment approaches.
Quantitative measures
The Visual Analogue Scale serves as a primary tool for assessing subjective emotional states before and after program participation. VAS assessments utilized a 10 cm horizontal line with anchors “very sad/worried” (0) and “very happy/calm” (10). Participants marked their current emotional state, with measurements converted to numerical scores (0–10). VAS assessments were administered before and immediately after each session, with research assistants helping younger children (ages 6–8) understand the scale. This instrument’s simplicity and flexibility make it particularly appropriate for pediatric populations, allowing young children to express feelings through visual representation rather than complex verbal descriptions (Shields et al., 2003). The ArtsObS observational assessment tool provides structured evaluation of creative processes and behavioral engagement during artistic activities (Fancourt and Poon, 2015). Trained observers (n = 3) used the ArtsObS to rate participant engagement across five domains: attention/concentration, creative expression, social interaction, emotional expression, and physical involvement. Ratings were made on 5-point scales (1 = minimal engagement, 5 = high engagement) at 15-min intervals during each session. Inter-rater reliability was established through training sessions achieving Cohen’s kappa ≥0.80 across all domains. This instrument allows trained observers to document changes in patient affect, engagement level, social interaction, and creative expression occurring during program participation. The Pediatric Quality of Life Inventory (PedsQL) offers comprehensive evaluation of health-related quality of life across physical functioning, emotional functioning, social functioning, and school functioning domains (Varni et al., 1999). The age-appropriate versions (child self-report for ages 8–17, parent proxy-report for ages 6–7) were administered at baseline, week 6 (mid-intervention), week 12 (post-intervention), and 4-week follow-up. The PedsQL uses 5-point response scales converted to 0–100 scores, with higher scores indicating better quality of life. This instrument has been extensively validated in pediatric oncology populations and provides standardized measures enabling comparison with other research studies.
Qualitative measures
Semi-structured interviews were conducted with participants at program completion to capture subjective experiences and perceived benefits. Interview guides included questions about program enjoyment, perceived benefits, changes in mood or behavior, and suggestions for improvement. Interviews lasted 15–30 min and were audio-recorded with permission.
Focus groups were conducted with healthcare providers (n = 6) involved in patient care to assess their observations of program effects on patient behavior, treatment cooperation, and overall wellbeing. Focus groups lasted 60 min and were facilitated by an experienced qualitative researcher.
Data collection procedures
Data collection procedures minimize participant burden while ensuring adequate program effect documentation. All assessments were integrated into routine clinical visits when possible to reduce additional hospital visits. Research staff were trained in pediatric research ethics and child-appropriate assessment techniques. Data collection followed a standardized protocol with quality assurance checks conducted weekly. Assessment timing coordinates with medical care schedules to avoid treatment interference while capturing meaningful program-associated changes.
Statistical analysis
Quantitative data analysis employed IBM SPSS Statistics version 28.0. Descriptive statistics characterized participant demographics and baseline measures. For VAS and PedsQL scores, repeated-measures ANOVA examined changes over time, with post-hoc pairwise comparisons using Bonferroni correction. ArtsObS scores were analyzed using multilevel modeling to account for multiple observations per participant. Effect sizes were calculated using Cohen’s d for pre-post comparisons. Statistical significance was set at p < 0.05.
Qualitative interview data were transcribed verbatim and analyzed using thematic analysis following Braun and Clarke's (2023) six-step approach. Two researchers independently coded transcripts, with disagreements resolved through discussion. Themes were developed inductively from the data and validated through member checking with a subset of participants.
Ethical considerations
The study was approved by the Institutional Ethics Committee (ID7436) and conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from parents/guardians. Participants could withdraw at any time without affecting their medical care. All data were de-identified and stored securely with access limited to authorized research personnel.
Results
Of the 25 enrolled participants, 24 (96%) completed the full intervention program (Figure 1). One participant withdrew due to medical complications. No adverse events related to program participation were reported.
VAS scores demonstrated significant improvements in emotional wellbeing over the course of the intervention. Mean baseline VAS scores were 4.2 ± 2.1, improving to 7.4 ± 1.6 at program completion (mean difference: 3.2 ± 1.4 points, Cohen’s d = 1.84, p < 0.001). Improvements were observed as early as week 2 and maintained through 4-week follow-up (7.1 ± 1.8, p < 0.001 compared to baseline).
ArtsObS assessments revealed significant increases in creative engagement over the intervention period. Composite engagement scores increased from 2.8 ± 0.9 at first session to 4.0 ± 0.7 at final session (42% improvement, p < 0.01). The greatest improvements were observed in creative expression (51% increase, p < 0.001) and social interaction domains (38% increase, p < 0.01). Attention/concentration scores showed progressive improvement throughout the program (r = 0.73, p < 0.001).
PedsQL total scores showed significant improvement from baseline (65.2 ± 12.4) to post-intervention (77.1 ± 10.8), representing an 18% increase (p < 0.01, Cohen’s d = 1.03). Domain-specific analyses revealed significant improvements in emotional functioning (23% increase, p < 0.001), social functioning (19% increase, p < 0.01), and school functioning (15% increase, p < 0.05). Physical functioning scores showed modest but non-significant improvement (8% increase, p = 0.12). Benefits were maintained at 4-week follow-up, with total PedsQL scores remaining significantly above baseline (75.8 ± 11.2, p < 0.01).
Thematic analysis of participant interviews revealed four primary themes reflecting the program’s impact on psychosocial wellbeing.
1. Enhanced emotional expression and processing. Participants consistently reported improved ability to express and process complex emotions related to their illness experience. One 14-year-old participant noted: “Working with clay helped me show feelings I could not say with words.” Parents observed that children demonstrated increased emotional vocabulary and willingness to discuss treatment-related concerns following program participation.
2. Strengthened peer connections and social confidence. The group-based nature of activities facilitated meaningful peer relationships among participants facing similar challenges. Children described feeling “understood” by program peers in ways that differed from interactions with healthy classmates. Healthcare providers noted increased social initiative and confidence extending beyond program sessions.
3. Cultural learning as therapeutic distraction. Engagement with Etruscan culture provided meaningful cognitive stimulation and positive distraction from medical concerns. Participants expressed pride in their cultural knowledge acquisition, with several requesting books about Etruscan civilization for continued learning. This intellectual engagement appeared to support maintained academic identity during treatment periods.
4. Creative accomplishment and identity preservation. Completion of ceramic projects reinforced positive self-concept and personal agency. Children described feeling “proud” and “capable” through creative accomplishments, countering illness-related feelings of helplessness. Exhibition participation provides opportunities to share achievements with family and community members, reinforcing social connections and personal identity beyond the patient role.
Healthcare provider focus groups corroborated participant reports, noting improved treatment cooperation, reduced anxiety during medical procedures, and enhanced overall treatment experience among program participants. Providers specifically observed increased resilience and adaptive coping strategies following program participation.
Clinical implementation and practical considerations
Successful ETRU4KIDS implementation requires careful attention to numerous practical considerations arising when integrating cultural programming into acute medical care settings. These implementation challenges reflect the complex intersection of healthcare requirements, educational objectives, cultural programming, and unique needs of pediatric oncology patients and families.
Integration of museum-based activities with ongoing medical care represents a critical implementation consideration (Stuckey and Nobel, 2010). Our experience demonstrated that successful integration required weekly multidisciplinary team meetings involving oncologists, nurses, child life specialists, museum educators, and research coordinators. Treatment schedules were reviewed in advance to optimize activity timing, with contingency plans developed for medical emergencies or unexpected treatment changes. Cancer treatment protocols are intensive and precisely scheduled, with limited flexibility for non-medical activities. The program must therefore maintain sufficient flexibility to accommodate changing medical needs, treatment schedules, and patient energy levels while preserving program integrity and therapeutic objectives.
Medical team input proved crucial for determining appropriate timing and intensity of program participation based on individual patient status, treatment phase, and prognosis. We developed clinical criteria for activity participation including stable vital signs, absence of acute complications, and medical team approval for each session.
Safety considerations are essential when working with immunocompromised pediatric oncology patients, requiring comprehensive protocols for infection control, emergency response, and medical support during program activities. We implemented strict infection control protocols including health screening for all program staff, use of personal protective equipment when indicated, and environmental cleaning procedures exceeding standard museum practices. Emergency response plans were developed for each program location, with medical personnel immediately available during all activities. Museum visits require particular attention to crowd control, environmental safety, and emergency evacuation procedures.
Training and professional development of team members represents another crucial implementation consideration, requiring coordination among professionals from diverse backgrounds including healthcare, education, museum studies, and arts therapy. We conducted multiple sessions of interdisciplinary training covering pediatric development, medical conditions, therapeutic communication, and cultural education techniques. Ongoing supervision and reflective practice sessions were held monthly to address challenges and refine approaches. Each discipline contributes unique expertise and professional standards that must be integrated into cohesive program approaches while maintaining respect for professional boundaries and competencies.
Program implementation required significant resource coordination including staff time, materials, transportation, and space allocation. Sustainability planning included developing fee-for-service models and seeking larger institutional funding commitments.
Therapeutic outcomes and clinical benefits
Psychological and emotional wellbeing represent primary therapeutic targets, addressing significant mental health challenges commonly accompanying pediatric cancer diagnosis and treatment. Research consistently demonstrates elevated anxiety, depression, and post-traumatic stress symptoms among pediatric oncology patients, with effects often persisting beyond treatment completion (Kazak et al., 2004).
Our quantitative findings provide compelling evidence for the program’s psychological benefits. The improvement in VAS emotional wellbeing scores represents a clinically meaningful change, exceeding the minimal clinically important difference established for pediatric populations (Shields et al., 2003). These improvements were observed across all age groups and diagnostic categories, suggesting broad applicability.
Structured cultural activities and creative expression opportunities provide multiple pathways for emotional regulation and psychological support. Aesthetic experiences during museum visits can elicit positive emotional responses counterbalancing stress and fear associated with medical environments. Recent environmental psychology research demonstrates that exposure to beautiful and meaningful spaces can reduce cortisol levels, lower blood pressure, and promote feelings of calm and wellbeing (Corazon et al., 2019; Browning et al., 2018).
Creative expression through ceramic work offers particularly powerful therapeutic benefits, engaging multiple sensory systems while providing opportunities for emotional processing and symbolic expression. Clay work’s tactile nature activates parasympathetic nervous system responses associated with relaxation and stress reduction (Malchiodi, 2012). Our ArtsObS findings document progressive increases in creative engagement, with the largest improvements in creative expression and social interaction domains. These behavioral changes correlated with improved emotional wellbeing scores, supporting the connection between creative engagement and psychological benefits. The creative process allows non-verbal expression of complex emotions and experiences difficult to articulate verbally, particularly important for children lacking vocabulary for describing illness experiences.
Social connection and community engagement represent crucial therapeutic domains addressed by the program. Cancer treatment often results in significant social isolation as patients are separated from normal peer interactions, school activities, and community participation due to medical restrictions. Our qualitative findings strongly support the program’s social benefits, with participants consistently reporting improved peer connections and reduced feelings of isolation. Healthcare providers noted increased social interaction during program days, with some previously withdrawn patients actively engaging with peers.
The improvement in PedsQL social functioning scores provides quantitative confirmation of these qualitative observations. Importantly, these social benefits appeared to generalize beyond program activities, with parents reporting improved social confidence in other contexts.
Group-based program activities provide structured opportunities for peer interaction with other children facing similar challenges. This peer support can be particularly valuable, allowing patients to connect with others who understand their experiences in ways that well-meaning but unaffected peers may not. Research on peer support in pediatric chronic illness documents significant benefits including reduced isolation feelings, improved coping strategies, and enhanced sense of normalcy (Barrera et al., 2009).
Cognitive stimulation and educational continuity represent additional therapeutic targets, addressing potential academic and cognitive impacts of cancer treatment. Chemotherapy and radiation treatments can affect cognitive functioning, including attention, memory, and processing speed, while prolonged school absences can result in academic delays (Fetoni et al., 2016; Roganovic et al., 2024; Sofia et al., 2021; Krull et al., 2013). Our findings suggest that cultural education activities may help maintain cognitive engagement, with improvement in PedsQL school functioning scores indicating enhanced educational readiness and academic confidence. Educational program components provide engaging learning opportunities complementing formal hospital schooling while introducing novel content areas and learning modalities.
Discussion
The ETRU4KIDS project embodies a fundamental reconceptualization of comprehensive pediatric oncology care. Integration of cultural institutions into healthcare delivery challenges traditional boundaries between medical and community settings while demonstrating that healing environments can extend beyond hospital walls.
Our study provides robust evidence for the therapeutic efficacy of museum-based interventions in pediatric oncology populations. The comprehensive assessment approach, employing multiple validated instruments and mixed-methods analysis, strengthens confidence in our findings. The effect sizes observed exceed those typically reported for psychosocial interventions in pediatric populations, suggesting that museum-based approaches may offer particularly powerful therapeutic benefits.
The program’s success in addressing multiple therapeutic domains simultaneously suggests that interdisciplinary approaches combining medical care with cultural, educational, and artistic elements may offer greater therapeutic efficiency and effectiveness than isolated interventions targeting single domains. This holistic approach aligns with contemporary understanding of health and wellbeing as multifaceted constructs requiring comprehensive intervention strategies.
The sustained benefits observed at 4-week follow-up suggest that program effects extend beyond immediate intervention periods, indicating potential for lasting psychological and social improvements. This finding is particularly significant given the chronic nature of cancer treatment and the importance of interventions that provide enduring support.
Healthcare provider observations note improvements in patient cooperation with medical procedures, reduced anxiety during hospital visits, and enhanced overall treatment experience among program participants. These clinical observations suggest museum-based intervention benefits may extend beyond direct therapeutic objectives to positively influence medical care delivery and treatment adherence.
This study contributes significantly to the growing literature on museums as health-promoting environments. Our findings demonstrate that museums can move beyond traditional educational roles to serve as active partners in healthcare delivery, particularly for vulnerable populations. The success of the ETRU4KIDS model suggests that cultural institutions possess unique resources for supporting human wellbeing that complement but do not replicate traditional healthcare services. The collaborative model developed through ETRU4KIDS addresses several challenges identified in previous museum-health partnerships, including sustainability, professional integration, and outcome measurement. Our structured approach to interdisciplinary collaboration, comprehensive assessment, and resource planning provides a replicable framework for similar initiatives.
The ETRU4KIDS findings align with broader evidence supporting arts-based health interventions while contributing unique insights specific to pediatric oncology populations. Our results complement previous studies demonstrating psychological benefits of cultural engagement (Ander et al., 2013; Thomson et al., 2018) while extending evidence to younger, more medically complex populations. The program’s success suggests that museum-based interventions warrant integration into standard psychosocial care protocols for pediatric oncology patients.
Demonstration that cultural institutions can meaningfully contribute to patient care opens new possibilities for healthcare partnerships with community organizations, educational institutions, and cultural centers (Stuckey and Nobel, 2010; Camic and Chatterjee, 2013; Dow et al., 2023). These partnerships could significantly expand resources available to support patient wellbeing while creating opportunities for community engagement and support extending beyond traditional healthcare settings.
The program provides a compelling model for healthcare delivery that honors both scientific rigor and humanistic values, offering hope for more meaningful and effective approaches to supporting children and families facing serious illness. The formal partnership model developed through ETRU4KIDS provides a replicable framework for establishing similar collaborations while addressing practical concerns about safety, liability, and professional coordination.
Several limitations should be acknowledged. The single-group design without a control condition limits causal inferences about program effects. While our findings are encouraging, randomized controlled trials would strengthen evidence for intervention efficacy. The study was conducted at a single institution with a specific cultural partnership, which may limit generalizability to other settings or cultural contexts. The relatively short follow-up period (4 weeks) prevents assessment of longer-term program benefits. Future studies should examine whether improvements persist over months or years following program completion. Additionally, the volunteer nature of participation may have selected families particularly motivated for cultural engagement, potentially overestimating program effects in broader populations. Finally, while our mixed-methods approach provided comprehensive assessment, some important outcomes may not have been captured. Future research might include biological markers of stress and immune function, as well as longer-term outcomes such as treatment adherence and academic achievement.
Future research priorities should include controlled studies comparing museum-based interventions with other established psychosocial interventions for pediatric oncology patients. Such studies would help establish specific therapeutic benefits of cultural engagement relative to other approaches while identifying which patients are most likely to benefit from museum-based interventions.
Longitudinal research examining sustained effects of program participation on patient outcomes represents another critical research priority. Understanding whether benefits persist over time and contribute to longer-term outcomes such as academic achievement, social adjustment, and quality of life requires extended follow-up studies.
Development of standardized outcome measures specifically designed for evaluating cultural and arts-based interventions in pediatric populations represents an important methodological need. While existing instruments provide valuable general quality of life information, they may not capture specific benefits of cultural engagement, creative expression, and aesthetic experiences central to museum-based interventions.
Investigation of biological markers of stress and wellbeing in relation to program participation represents an emerging research area that could provide important insights into physiological mechanisms underlying therapeutic effects of cultural interventions (Saad et al., 2025; Ma et al., 2025; Papathanassoglou et al., 2025). Studies examining cortisol levels, immune function markers, and neuroimaging data could help establish biological plausibility of observed clinical benefits while informing optimal program design and implementation.
Conclusion
The ETRU4KIDS project demonstrates that museum-based interventions can provide significant therapeutic, educational, and social benefits for children and adolescents facing cancer treatment. Our prospective study of 25 pediatric oncology patients provides robust evidence for the efficacy of museum-based psychosocial interventions, with statistically significant improvements observed across multiple validated outcome measures. Through careful collaboration between clinical and cultural institutions, the program has created a comprehensive approach to patient care that honors both medical necessities and fundamental human needs for beauty, creativity, learning, and cultural connection.
The magnitude of improvements observed demonstrates clinically meaningful benefits that compare favorably with other psychosocial interventions. The sustained benefits at follow-up suggest that museum-based approaches may provide lasting psychological and social support extending beyond immediate intervention periods.
The program’s success in addressing multiple therapeutic domains simultaneously suggests that holistic interventions combining diverse therapeutic modalities may offer greater effectiveness than isolated approaches targeting single domains. This finding has important implications for healthcare delivery models and resource allocation decisions in pediatric oncology and potentially other pediatric specialties.
The replicable model developed through ETRU4KIDS addresses key implementation challenges identified in previous cultural health partnerships, including professional integration, safety protocols, assessment frameworks, and sustainability planning. The comprehensive documentation of methods, outcomes, and practical considerations provides other institutions with a blueprint for developing similar programs.
It is important to emphasize that the ETRU4KIDS program represents a psychosocial and rehabilitative intervention focused on emotional processing, quality of life enhancement, and psychological wellbeing support. This intervention does not address the underlying oncological disease itself but rather provides complementary support to enhance the overall treatment experience and patient wellbeing during cancer care.
The ETRU4KIDS experience ultimately demonstrates that healing occurs not only through medical intervention but also through engagement with beauty, creativity, learning, and cultural heritage. This recognition has profound implications for healthcare conceptualization and delivery, suggesting that comprehensive patient care must address the full spectrum of human needs and experiences.
Author contributions
AR: Writing – original draft, Data curation. AG: Writing – original draft, Methodology. VL: Writing – review & editing, Methodology. FM: Methodology, Writing – review & editing. LT: Writing – review & editing. MO: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by internal funding from the Pediatric Oncology Unit, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, and the National Etruscan Museum of Villa Giulia. Additional support was provided by the Lene Thun Foundation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ander, E. E., Thomson, L. J., Noble, G., Menon, U., and Chatterjee, H. (2013). Heritage, health and well-being: assessing the impact of a heritage focused intervention on health and well-being. Int. J. Heritage Stud. 19, 229–242. doi: 10.1080/13527258.2011.651740
Barrera, M., Atenafu, E., and Hancock, K. (2009). Longitudinal health-related quality of life outcomes and related factors after pediatric SCT. Bone Marrow Transplant. 44, 249–256. doi: 10.1038/bmt.2009.24
Belfi, A. M., Vessel, E. A., Brielmann, A., Isik, A. I., Chatterjee, A., Leder, H., et al. (2019). Dynamics of aesthetic experience are reflected in the default-mode network. NeuroImage 188, 584–597. doi: 10.1016/j.neuroimage.2018.12.017
Bourdieu, P. (2002). “The forms of capital” in Handbook of theory and research for the sociology of education. ed. J. Richardson (Westport, CT: Greenwood), 241–258.
Braun, V., and Clarke, V. (2023). Is thematic analysis used well in health psychology? A critical review of published research, with recommendations for quality practice and reporting. Health Psychol. Rev. 17, 695–718. doi: 10.1080/17437199.2022.2161594
Browning, M., Kuo, M., Sachdeva, S., Lee, K., and Westphal, L. (2018). Greenness and school-wide test scores are not always positively associated – a replication of “linking student performance in Massachusetts elementary schools with the ‘greenness’ of school surroundings using remote sensing”. Landsc. Urban Plan. 178, 69–72. doi: 10.1016/j.landurbplan.2018.05.007
Camic, P. M., and Chatterjee, H. J. (2013). Museums and art galleries as partners for public health interventions. Perspect. Public Health 133, 66–71. doi: 10.1177/1757913912468523
Clift, S., Camic, P. M., Chapman, B., Clayton, G., Daykin, N., Eades, G., et al. (2009). The state of arts and health in England. Arts Health 1, 6–35. doi: 10.1080/17533010802528017
Corazon, S. S., Sidenius, U., Poulsen, D. V., Gramkow, M. C., and Stigsdotter, U. K. (2019). Psycho-physiological stress recovery in outdoor nature-based interventions: a systematic review of the past eight years of research. Int. J. Environ. Res. Public Health 16:1711. doi: 10.3390/ijerph16101711
Dodd, J., and Jones, C. (2014). Mind, body, spirit: how museums impact health and wellbeing. Leicester: Research Centre for Museums and Galleries.
Dow, R., Warran, K., Letrondo, P., and Fancourt, D. (2023). The arts in public health policy: progress and opportunities. Lancet Public Health 8, e155–e160. doi: 10.1016/S2468-2667(22)00313-9
Engel, G. L. (2012). The need for a new medical model: a challenge for biomedicine. Psychodyn Psychiatry 40, 377–396. doi: 10.1521/pdps.2012.40.3.377
Fancourt, D., and Finn, S. (2019). What is the evidence on the role of the arts in improving health and well-being? A scoping review. Copenhagen: WHO Regional Office for Europe.
Fancourt, D., and Poon, M. (2015). Validation of the arts observational scale (ArtsObS) for the evaluation of performing arts activities in health care settings. Arts Health 8, 140–153. doi: 10.1080/17533015.2015.1048695
Fetoni, A. R., Ruggiero, A., Lucidi, D., De Corso, E., Sergi, B., Conti, G., et al. (2016). Audiological monitoring in children treated with platinum chemotherapy. Audiol. Neurootol. 21, 203–211. doi: 10.1159/000442435
Fraser, K. D., O'Rourke, H. M., Wiens, H., Lai, J., Howell, C., and Brett-MacLean, P. (2015). A scoping review of research on the arts, aging, and quality of life. Gerontologist 55, 719–729. doi: 10.1093/geront/gnv027
Hooper-Greenhill, E. (2007). Museums and education: purpose, pedagogy, performance. London: Routledge.
Hunger, S. P., Lu, X., Devidas, M., Camitta, B. M., Gaynon, P. S., Winick, N. J., et al. (2012). Improved survival for children and adolescents with acute lymphoblastic leukemia between 1990 and 2005: a report from the children's oncology group. J. Clin. Oncol. 30, 1663–1669. doi: 10.1200/JCO.2011.37.8018
Kazak, A. E., Alderfer, M., Rourke, M. T., Simms, S., Streisand, R., and Grossman, J. R. (2004). Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J. Pediatr. Psychol. 29, 211–219. doi: 10.1093/jpepsy/jsh022
Krull, K. R., Brinkman, T. M., Li, C., Ness, K. K., Srivastava, D. K., Gurney, J. G., et al. (2013). Neurocognitive outcomes decades after treatment for childhood acute lymphoblastic leukemia: a report from the St Jude lifetime cohort study. J. Clin. Oncol. 31, 4407–4415. doi: 10.1200/JCO.2012.48.2315
Ma, C. B., Shang, X., Sun, M., Bo, X., Bai, J., Du, Y., et al. (2025). Emerging multifunctional wearable sensors: integrating multimodal sweat analysis and advanced material technologies for Next-Generation Health Monitoring. ACS Sensors 10, 2388–2408. doi: 10.1021/acssensors.4c03396
Marmot, M., and Wilkinson, R. G. (2016). Social determinants of health. 2nd Edn. Oxford: Oxford University Press.
Menninghaus, W., Wagner, V., Hanich, J., Wassiliwizky, E., Kuehnast, M., and Jacobsen, T. (2017) The distancing-embracing model of the enjoyment of negative emotions in art reception Behav. Brain Sci. 40:e347 doi: 10.1017/S0140525X17000309
Meyer, A., Rose, D. H., and Gordon, D. (2014). Universal design for learning: theory and practice. Wakefield, MA: CAST Professional Publishing.
Newman, A., Goulding, A., and Whitehead, C. (2013). How cultural capital, habitus and class influence the responses of older adults to the field of contemporary visual art. Poetics 41, 456–480. doi: 10.1016/j.poetic.2013.07.001
Papathanassoglou, E., Pant, U., Meghani, S., Saleem Punjani, N., Wang, Y., Brulotte, T., et al. (2025). A systematic review of the comparative effects of sound and music interventions for intensive care unit patients' outcomes. Aust. Crit. Care 38:101148. doi: 10.1016/j.aucc.2024.101148
Roganovic, J., Haupt, R., Bárdi, E., Hjorth, L., Michel, G., Pavasovic, V., et al. (2024). Late adverse effects after treatment for childhood acute leukemia. Acta Med. Acad. 53, 59–80. doi: 10.5644/ama2006-124.438
Saad, H. A., Marzouk, M., Abdelrahman, H., and Moradikor, N. (2025). Mechanisms underlying stress effects on the brain: basic concepts and clinical implications. Prog. Brain Res. 291, 21–47. doi: 10.1016/bs.pbr.2025.01.008
Sachs, M. E., Ellis, R. J., Schlaug, G., and Loui, P. (2016). Brain connectivity reflects human aesthetic responses to music. Soc. Cogn. Affect. Neurosci. 11, 884–891. doi: 10.1093/scan/nsw009
Schulte, F., and Barrera, M. (2010). Social competence in childhood brain tumor survivors: a comprehensive review. Support Care Cancer 18, 1499–1513. doi: 10.1007/s00520-010-0963-1
Seligman, M. E. (2011). Flourish: A visionary new understanding of happiness and well-being. New York: Free Press.
Shields, B. J., Palermo, T. M., Powers, J. D., Grewe, S. D., and Smith, G. A. (2003). Predictors of a child's ability to use a visual analogue scale. Child Care Health Dev. 29, 281–290. doi: 10.1046/j.1365-2214.2003.00343.x
Sholt, M., and Gavron, T. (2006). Therapeutic qualities of clay-work in art therapy and psychotherapy: a review. Art Ther. 23, 66–72. doi: 10.1080/07421656.2006.10129647
Sofia, R., Melita, V., De Vita, A., Ruggiero, A., Romano, A., Attinà, G., et al. (2021). Cardiac surveillance for early detection of late subclinical cardiac dysfunction in childhood Cancer survivors after anthracycline therapy. Front. Oncol. 11:624057. doi: 10.3389/fonc.2021.624057
Stuckey, H. L., and Nobel, J. (2010). The connection between art, healing, and public health: a review of current literature. Am. J. Public Health 100, 254–263. doi: 10.2105/AJPH.2008.156497
Thomson, L. J., Lockyer, B., Camic, P. M., and Chatterjee, H. J. (2018). Effects of a museum-based social prescription intervention on quantitative measures of psychological wellbeing in older adults. Perspect. Public Health 138, 28–38. doi: 10.1177/1757913917737563
Varni, J. W., Seid, M., and Rode, C. A. (1999). The PedsQL: measurement model for the pediatric quality of life inventory. Med. Care 37, 126–139. doi: 10.1097/00005650-199902000-00003
Varni, J. W., Seid, M., and Kurtin, P. S. (2001). PedsQL 4.0: reliability and validity of the pediatric quality of life inventory version 4.0 generic core scales in healthy and patient populations. Med. Care 39, 800–812. doi: 10.1097/00005650-200108000-00006
Vessel, E. A., Starr, G. G., and Rubin, N. (2012). The brain on art: intense aesthetic experience activates the default mode network. Front. Hum. Neurosci. 6:66. doi: 10.3389/fnhum.2012.00066
Keywords: pediatric oncology, museum therapy, cultural interventions, quality of life, ceramic therapy, holistic care, arts-based healing
Citation: Ruggiero A, Guido A, Lecce V, Montuori F, Toniolo L and Osanna M (2025) Museum-based therapeutic interventions in pediatric oncology: the ETRU4KIDS experience as a model for hospital wellness enhancement. Front. Educ. 10:1656998. doi: 10.3389/feduc.2025.1656998
Edited by:
Nevine Nizar Zakaria, Julius Maximilian University of Würzburg, GermanyCopyright © 2025 Ruggiero, Guido, Lecce, Montuori, Toniolo and Osanna. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Antonio Ruggiero, YW50b25pby5ydWdnaWVyb0B1bmljYXR0Lml0
 Antonio Ruggiero
Antonio Ruggiero Antonella Guido1
Antonella Guido1