- Department of Environmental Sciences and Engineering, The Gillings School of Global Public Health, The Water Institute at UNC, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
In 2016, nearly 60% of the population of India practiced open defecation (OD), which was 4 times the global rate, and reducing OD in India will be essential in meeting Sustainable Development Goal (SDG) 6.2 and improving global public health. The government of India launched the Swachh Bharat Mission (SBM) in 2014 with one key goal for all Indian states to achieve OD-free (ODF) status by 2019. Despite reports from the Government of India on the success of SBM, the true ODF status of Indian states is still unknown. A systematic review of peer-reviewed literature was conducted to assess the impact of SBM on OD in India, evaluate the barriers to reducing OD, and provide recommendations for future interventions to reduce or eliminate OD in India. A total of 237 publications were screened, and 22 were selected for inclusion. While the Prime Minister declared India ODF in 2019, studies suggest that the government monitoring system overestimates numbers of ODF villages and toilet coverage. Reasons for households’ continued OD practice include financial constraints, lack of water supply, governmental mistrust, cultural beliefs, and personal preference. Community incentives and penalties have been used to encourage proper sanitation practices with varying success. Overarching strategies and approaches that have worked well across study districts to reduce OD include high involvement of district leadership and innovative behavior-change and local community mobilization campaigns.
1 Introduction
Open defecation (OD) refers to the practice of defecating or disposing of human feces in fields, forests, bushes, bodies of water, or other open spaces (WHO and UNICEF, 2021). Given its linkages to human health, dignity, and gender equity, eliminating OD has remained a global goal and water, sanitation, and hygiene (WASH) sector priority (Beardsley et al., 2021; Sprouse et al., 2022) manifesting in an international agreement on the human right to water and sanitation and the United Nations SDG 6.2 to achieve by 2030 access to adequate and equitable sanitation and hygiene for all and end OD (United Nations, 2022). Between 2000 and 2020, the World Health Organization/United Nations Children’s Fund Joint Monitoring Programme (JMP) reported that the proportion of the global population practicing OD decreased from 21% to 6%; however, an estimated 494 million people still practice OD, of whom 90% live in rural areas of sub-Saharan Africa and Central and Southern Asia (WHO and UNICEF, 2021).
In 2016, an estimated 60% of the population of India practiced OD, which was 4 times the global rate (Alexander et al., 2016). Because India may still be a major contributor to global OD rates, reducing the practice will be essential in meeting the 2030 SDG target 6.2. According to JMP reported data, India is responsible for the largest drop in OD between 2015 and 2020 in terms of absolute numbers among all countries, yet high rates of OD in India persist (WHO and UNICEF, 2021). The JMP estimated that 15% of India’s population practiced OD in 2020, with rates varying between 1% and 70% across states (WHO and UNICEF, 2021). India’s National Family Health Survey (NFHS) estimated that 19% of India’s population practiced OD in 2021 (IIPS and ICF, 2021; WHO and UNICEF, 2021). However, several studies have indicated that rates of OD in India are underestimated. Vyas et al. (2019) found a 20-percentage point higher rate of OD at the individual level than was reported by the NFHS at the household level. Yogananth and Bhatnagar (2018) found that nearly 55% of households in the state of Tamil Nadu practiced OD despite having a household toilet, compared to 38% reported by the 2016 NFHS (IIPS and ICF, 2017).
The JMP estimated that in 2020, 46% of India’s population had access to safely managed sanitation services, that is, improved sanitation facilities that are not shared with other households and where excreta are safely disposed of onsite or transported and treated offsite. (WHO and UNICEF, 2021). This estimate of sanitation coverage is similar to other countries regionally—Bangladesh (39%) and Nepal (49%) — as well as globally—including Ecuador (42%) and Albania (49%) (WHO and UNICEF, 2021). However, while these countries have similar estimates of safely managed sanitation coverage, estimates of OD varied. Albania, Bangladesh, and Ecuador were all estimated to have rates of OD less than 1%, compared to an estimated 10% in Nepal and 15% in India, suggested that India is lagging behind in improving defecation practices both regionally and globally (WHO and UNICEF, 2021).
Lack of adequate WASH services and OD are most commonly associated with excreta-related infectious diseases and diarrhea (Cairncross et al., 2010; Manga, 2017; Manga et al., 2022). OD enables disease-causing pathogens to spread from the feces of one person to the mouth of another via contaminated water, food, or fomites (Capone et al., 2022). A systematic review of the health impacts of OD in India and Kenya found associations of OD with soil-transmitted helminth infections, hookworm infestations, poor birth outcomes, poor nutrition, increased risk of sexual violence among women, and psychosocial stress (Saleem et al., 2019). Declines in OD correspond to decreases in the prevalence of diarrheal morbidity (Njuguna, 2016). Reductions in OD, and corresponding reductions in WASH-related morbidity, may be achieved by improving access to basic or improved sanitation services. Improved sanitation facilities hygienically separate excreta from human contact, and basic sanitation refers to the use of improved sanitation facilities that are not shared by other households (WHO and UNICEF, 2021). Safely managed sanitation refers to the use of improved facilities that are not shared by other households, and where excreta are safely disposed of on-site or removed and treated off-site. The JMP estimated that 71% of India had access to basic or safely managed sanitation in 2020 (WHO and UNICEF, 2021).
To accelerate efforts to achieve country-wide sanitation coverage and reduce WASH-related disease in line with SDG 6, the Prime Minister of India launched the Swachh Bharat Mission (SBM) in 2014. One key objective of the SBM was for all Indian villages, districts, and states to improve public health by achieving open defecation free (ODF) status by 2019 based on household-level surveys (Government of India, 2022). ODF is defined in SBM guidelines as no visible feces found in the environment/village and, b) every household as well as public/community institution(s) using safe technology option for disposal of feces, as defined by the Ministry of Drinking Water and Sanitation. However, the effectiveness of SBM in eliminating OD in Indian states is still not well understood.
SBM sought to engage all people in the task of cleaning homes, workplaces, villages, cities and surroundings, in a collective quest. The objectives of SBM included: a) Bring about an improvement in the general quality of life in rural areas by promoting cleanliness, hygiene and eliminating open defecation, b) Accelerate sanitation coverage in rural areas to achieve the vision of Swachh Bharat, c) Motivate communities to adopt sustainable sanitation practices and facilities through awareness creation and health education, d) Encourage cost effective and appropriate technologies for ecologically safe and sustainable sanitation, e) Develop community managed sanitation systems focusing on scientific Solid and Liquid Waste Management systems for overall cleanliness in the rural areas, and f) Create significant positive impact on gender and promote social inclusion by improving sanitation especially in marginalized communities (Government of India, 2018). The strategy for obtaining these objectives included augmenting the institutional capacity of districts to undertake behavior change at the grassroots level, strengthening the capacities of implementing agencies to roll out program components in a timely manner and to measure collective outcomes, and incentivizing the performance of state-level institutions to implement behavioral change activities in communities.
Because large portions of India’s population may continue to practice OD—up to 70% of the population in certain states—and lack access to basic or safely managed sanitation facilities, as established by the JMP and NFHS, it is important to evaluate the impact of SBM on OD and sanitation access in India (WHO and UNICEF, 2021). This is the first study to conduct a systematic review of published literature assessing the impacts of SBM on OD practices. The objectives of this review were to 1) assess the impact of SBM on OD, 2) evaluate the barriers to eliminating OD, and 3) provide recommendations for future interventions to reduce or eliminate OD in India. These study findings may be used to inform future initiatives focused on reducing OD following government-wide sanitation hardware campaigns.
2 Methodology
2.1 Search strategy
A systematic review of published literature from PubMed, Scopus, and the Global Health database within EBSCO was conducted. Search terms were related to the Swachh Bharat Mission, open defecation, and states within India. Synonyms of these search terms in addition to other keywords were used. Initial searches including the Swachh Bharat Mission yielded few results; searches were modified to include Swachh Bharat Abhiyan, Clean India Mission, and Nirmal Bharat Abhiyan as well as keywords including by not limited to Rural, Urban, Toilet Construction, and Household Sanitation. A complete list of search terms is available in the Supplementary Table S1.
Database searches were limited to articles published in English in 2014 or later, and the final search was conducted on 8 June 2022. All studies were uploaded to Covidence, a systematic review production online tool, where duplicate studies were removed. Two reviewers screened the remaining studies by title and abstract for relevance. The final selection of studies occurred after a full text review of articles.
2.2 Document selection and eligibility criteria
Studies selected for inclusion must have assessed the impacts of the SBM on OD practices in India. Studies reporting on ending open defecation under other programs and campaigns were excluded. Studies reported in languages other than English were excluded. Commentaries, viewpoints, and other review articles were excluded from this review, as we sought to evaluate primary evidence of rates of OD in India. Study data were then extracted, which included study design, location, sample size, study description, data collection methods, and main findings such as impacts on OD or qualitative factors affecting latrine access and use.
2.3 Quality appraisal
Quality assessment was performed by one reviewer and involved describing the level of evidence (Ackley et al., 2008; Brownson et al., 2009; Manga et al., 2023; Muoghalu et al., 2023) and risk of bias (Sterne et al., 2016; Higgins et al., 2022; Conaway et al., 2023) that were then used to rate the overall certainty of the articles. Quality assessment results are provided in Table 2.
A level of evidence was assigned to studies based on the methodological quality of the article design and applicability. Levels were ranked as A, B, or C, with Level A being the highest level of evidence and Level C being the lowest level of evidence. Level A was reserved for randomized controlled trials (RCTs), as systematic reviews were excluded from this review (Ackley et al., 2008). Other types of peer-reviewed research such as cross-sectional studies were rated at Level B. Level C was assigned to formative research and pilot studies (Brownson et al., 2009).
The risk of bias was evaluated using the risk-of-bias tool (RoB 2) for RCTs (Higgins et al., 2022), and the Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool for other study types (Sterne et al., 2016). The RoB 2 analysis involved the evaluation of bias that arose from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in outcome measurements, and bias in selection of the reported results (Higgins et al., 2022). Domains in ROBINS-I that are not included in RoB 2 include bias due to confounding, selection bias, and bias in classification of interventions (Sterne et al., 2016).
Overall certainty ratings imply confidence that the true effects lie near the estimated effect determined in the study. Studies at Level A were initially given a high certainty, studies at Level B were rated intermediate, and studies at Level C were initially rated as low. Overall certainty was then either increased or decreased based on risk of bias estimates. Based on the information obtained through this review, recommendations for future interventions, modifications, and programs were provided.
3 Results
3.1 Study selection
We identified 237 documents from databases including Scopus, PubMed, and Global Health by Ebscohost. After screening for duplicates and excluding documents that did not meet our inclusion criteria, we reviewed the full texts of 53 studies for further assessment. Of these, we further excluded studies that did not describe and analyze primary data, documents that referenced identical data and findings, and documents in which the interventions to reduce OD were not a part of the SBM. In total, 22 of the total 237 documents were included in this review. Figure 1 presents a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram of the literature screening and article selection process.

FIGURE 1. Process for selecting studies in this review of the effectiveness of the Swachh Bharat Mission on reducing OD in India.
3.2 Summary of findings
A detailed summary of the study findings, including study designs, locations, sample sizes, descriptions, data collection methods, and main findings, is shown in Table 1.
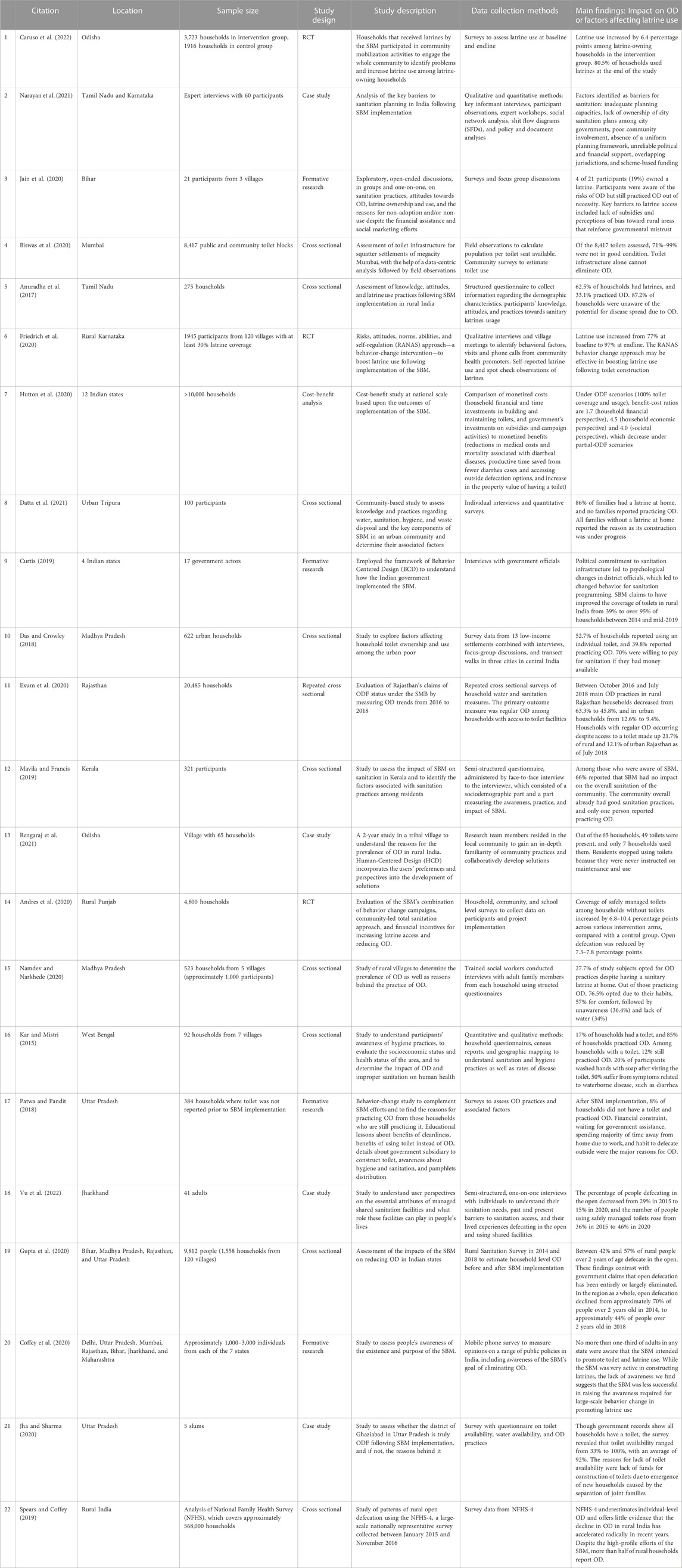
TABLE 1. Summary of included studies’ location, sample size, design, data collection methods, and main findings relevant to the impact of the SBM on OD practices in India.
3.2.1 Geographic locations of included studies
Thirteen Indian states were represented across the literature. Six studies reported experiences from more than one state, region, or territory in India, so there is overlap among the locations in some studies. Most studies reported experiences from Uttar Pradesh (n = 4, 18%), Bihar (n = 3, 14%), Madhya Pradesh (n = 3, 14%), Rajasthan (n = 3, 14%), and Maharashtra (n = 3, 14%). The remaining studies were conducted in Odisha, Tamil Nadu, Karnataka, Jharkhand, Tripura, Kerala, West Bengal, and Punjab. Figure 2 shows a map highlighting the frequency of study locations.

FIGURE 2. Frequency of Indian states/territories that are the study area of focus in articles included in this review. Tripura, Kerala, West Bengal, and Punjab appeared in one study each (4%); Odisha, Tamil Nadu, Karnataka, and Jharkhand appeared in two studies each (9%); Bihar, Madhya Pradesh, Rajasthan, and Maharashtra appeared in 3 studies each (14%); and Uttar Pradesh appeared in 4 studies (18%).
3.2.2 Quality assessment of included studies
Of the 22 included studies, three (14%) were RCTs rated as Level A, as shown in Table 2. This review also included 10 cross-sectional studies (45%) that were rated as Level B. The remaining nine studies (41%) were formative research or case studies that were ranked as Level C.
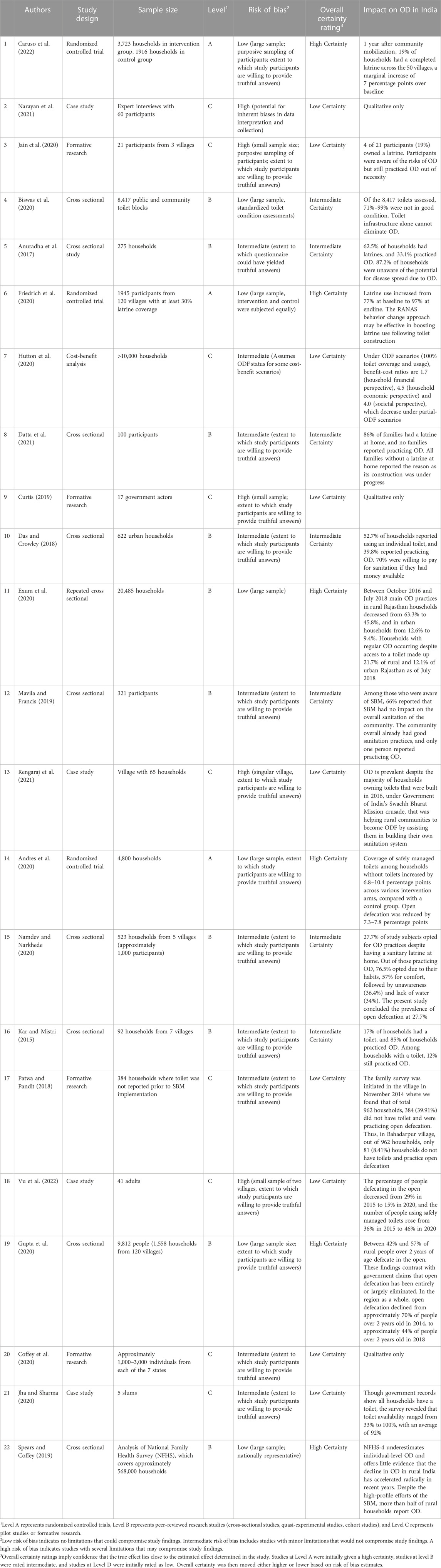
TABLE 2. Quality assessment of studies included in this review of the effectiveness of the SBM in reducing OD practices in India.
According to the Cochrane guidelines, certain study limitations can increase the risk of bias and therefore decrease the overall certainty rating. A low risk of bias score implies confidence that there were no major or minor sources of bias that could have influenced results. An intermediate risk of bias indicates the presence of one major or several minor study limitations, and a high risk of bias indicates the presence of more than one crucial limitation that may seriously compromise the validity of study findings (Sterne et al., 2016; Anthonj et al., 2020; Higgins et al., 2022).
Seven studies (23%) were scored a low risk of bias. Among these, three were RCTs that had large sample sizes with thousands of participants, randomization via random number generator or lotter, and little to no missing outcome data. Biswas et al. (2020), Exum et al. (2020), Gupta et al. (2020), and Spears and Coffey (2019) conducted cross-sectional studies with large and/or nationally representative sample sizes and adjustments for potential confounders that led to their low risk of bias judgment.
Ten studies (45%) were scored an intermediate risk of bias, among which six were cross-sectional studies with questionnaires or interviews leading to uncertainty in the extent to which participants may be willing to provide truthful answers. The other four studies rated as intermediate risk of bias were formative research or case studies that had hundreds of participants but used purposive sampling techniques for particular populations of interest, leading to the potential for biases in data collection.
Five studies (23%) were scored a high risk of bias, all of which were formative research or case studies. This rating was due to small sample sizes, the use of convenience sampling, self-reported defecation practices, potential for courtesy bias, and the lack of follow-up.
3.2.3 Impacts of SBM on OD
Several studies found that government claims of improved toilet coverage and increases in ODF villages were overreported. While India’s Prime Minister declared the country ODF in 2019, assessments of toilet coverage following SBM implementation ranged from 19% in rural Bihar (Jain et al., 2020) to 92% in urban Uttar Pradesh (Jha and Sharma, 2020). India’s NFHS reported that 19% of India’s total population practiced OD in 2021 (IIPS and ICF, 2021). Andres et al. (2020) found that coverage of improved sanitation among households without toilets increased by 6.8–10.4 percentage points from 2014 to 2019, and open defecation reduced by 7.3 percentage points.
Among households that owned latrines, several studies found that latrine ownership did not necessarily indicate latrine use. Namdev and Narkhede (2020) found that among households in rural Madhya Pradesh, 27.7% of households with toilets at home practiced OD. Caruso et al. (2022) showed that among households in Odisha, only 60.4% of those that received new latrines during the SBM used their latrines. Biswas et al. (2020) found that among all public and community toilets in Mumbai,71%–99% were not in good condition, and toilet infrastructure is not directly correlated with reductions in OD. Exum et al. (2020) found modest reductions in OD in rural Rajasthan between 2016 and 2018, though rates of OD remained high–OD decreased from 63.3% to 45.8% among rural households with latrine access, and households regularly practicing OD despite 21.7% of rural Rajasthan and 12.1% of urban Rajasthan having access to a toilet.
Rates of OD also varied by urban and rural location. Studies conducted in urban locations found higher rates of latrine coverage and lower rates of OD than those conducted in rural areas (Exum et al., 2020; Jha and Sharma, 2020; Datta et al., 2021). Urban latrine coverage was found to be 86% and 92% in urban Tripura and urban Uttar Pradesh, respectively (Jha and Sharma, 2020; Datta et al., 2021). Exum et al. (2020) found that, from 2016 to 2018, main OD practices in rural Rajasthan households decreased from 63.3% to 45.8%, and in urban households from 12.6% to 9.4%.
3.2.4 Barriers to eliminating OD in India
Narayan et al. (2021) conducted key informant interviews to identify barriers to latrine use, and found that unreliable financial support, inadequate planning capacities, and poor community involvement were major factors contributing to continued open defecation. Das and Crowley (2018) also found affordability to be a key hurdle to sanitation program success, though 70% of participants expressed willingness to pay Rs.25-100 ($0.30–1.20 USD) monthly for connection to a networked sewer system. Kumar (2017) found that the current government subsidy of 12,000 rupees ($145 USD) per toilet limits the technologies available to each household, disallowing households from choosing better technology that best fits their local context.
Hutton et al. (2020) conducted a cost-benefit analysis of the SBM based on inputs from household level surveys in which monetized costs (household financial and time investments in building and maintaining toilets, and government’s investments on subsidies and campaign activities) were compared to monetized benefits (reductions in medical costs and mortality associated with diarrheal diseases, productive time saved from fewer diarrhea cases and accessing outside defecation options, and increase in the property value of having a toilet). Under ODF scenarios, corresponding to 100% toilet coverage and usage, benefit-cost ratios were 1.7 (household financial perspective), 4.5 (household economic perspective) and 4.0 (societal perspective), which suggest that SBM was highly cost-beneficial when communities are free of OD.
Jain et al. (2020) surveyed rural households to explore perspectives on open defecation and latrine use, and the socio-economic and political reasons for these perspectives in rural Bihar and found that residents perceive a development bias against rural areas that reinforces governmental distrust. While a subsidy can help some households construct latrines, Jain et al. (2020) found that the amount of the subsidy and the manner of its disbursement are key to its usefulness.
Vu et al. (2022) identified structural barriers to sanitation access, including uncertain land rights, lack of space for a toilet, and inadequate water supply. Managed shared facilities could play an important role in helping eliminate OD while preventing adverse outcomes, though having a shared facility does not mean it is accessible. Participants noted having to travel far distances as a barrier to latrine use (Vu et al., 2022). A lack of public participation and poor maintenance led to poor toilet conditions which led to a lack of use by individuals (Biswas et al., 2020; Rengaraj et al., 2021). While studies showed modest increases in rates of toilet coverage following SBM implementation, toilets were often not appropriately used or maintained. Biswas et al. (2020) showed that nearly all toilets in Mumbai were in poor condition.
Anuradha et al. (2017) found a lack of funds, a lack of interest in latrine construction, and a lack of knowledge about the potential for disease spread as barriers to latrine use. Continued OD may also be due to habit, personal comfort, spending most of the day at work away from home, or cultural beliefs that OD is a form of purity and strength, which is more common in rural areas (Patwa and Pandit, 2018; Namdev and Narkhede, 2020). However, Jain et al. refuted the prevalence of the notion that people open defecate by choice and instead stated that they found most participants vehemently opposed this notion and insisted that they do not wish to OD and instead OD out of necessity (2020).
3.2.5 Interventions for reducing OD following SBM implementation
Three studies conducted behavior-change interventions to boost latrine uptake following the SBM (Friedrich et al., 2020; Rengaraj et al., 2021; Caruso et al., 2022). Caruso et al. (2022) randomly assigned 66 latrine-owning villages to receive either no intervention (control group) or a behavioral intervention involving community meetings and activities, mothers’ meetings, household visits, and latrine repairs. Friedrich et al. (2020) conducted qualitative interviews and village meetings to identify barriers to reducing OD, as well as used community health promoter visits and phone calls to encourage latrine use. This demonstrates that while the SBM did provide services, there were more opportunities unaddressed to further encourage latrine usage and additional interventions had to bridge the gap.
After conducting their community mobilization and behavior-change campaign to increase latrine use over roughly 10 months, Caruso et al. (2022) found that latrine use increased from 60.4% at baseline to 80.5% at endline. Friedrich et al. (2020) found that, after 2 years of intervention, latrine use increased from 77% to 97%.
Caruso et al. (2022) suggested that time and cost constraints of the SBM prevented the intervention from addressing all known behavioral factors, notably water access and latrine design. For example, those with government-funded latrines are more likely to open defecate than those with privately constructed latrines due to the design features limited by cost such as smaller pit sizes. Both Caruso et al. (2022); Friedrich et al. (2020) suggested that behavioral campaigns to increase latrine uptake and use should target change-resistant individuals, and behavioral interventions could complement future latrine use promotion in India.
Rengaraj et al. (2021) performed in-depth interactions with community members over 2 years to understand the deeper issues associated with continued OD and developed a water filtration and distribution system to address the root cause of the community’s water and sanitation challenges. Rengaraj et al. (2021) determined that longer commitment using a bottom-up participatory and user-centered approach was key in bringing about a higher social impact in reducing OD at the community level.
4 Discussion
Our systematic review sought to identify studies assessing the impact of SBM on OD, evaluate the successes and shortcomings of SBM in reducing OD and the reasoning behind it, and provide recommendations for future interventions to reduce or eliminate OD in India. We found evidence that government claims of India’s universal latrine coverage and ODF status were overrepresented, which may be due to the use of household-level data which assumes everyone in the household is using the latrine instead of individual-level data which considers that some members of the household may still be practicing open defecation in government monitoring efforts. There are many households in which some people use the latrine while others defecate in the open, which is especially true of government-provided latrines, which are more likely to be used by only some household members than privately constructed latrines (Spears and Coffey, 2019). We also found variation among studies in reported rates of OD and latrine coverage among Indian states, urban and rural locations, and socioeconomic levels. This suggests that a more robust monitoring system to assess OD at the individual level is needed to adequately assess ODF status.
Many studies found that OD remained prevalent despite SBM, with rates ranging from 15% in Jharkhand (Vu et al., 2022), 30%–40% in Tamil Nadu and Madhya Pradesh (Anuradha et al., 2017; Das and Crowley, 2018; Namdev and Narkhede, 2020), to 44% in a multi-state study (Gupta et al., 2020). Some studies reported no or very little OD, though these had smaller sample sizes and used self-reported data during face-to-face interviews, which may be more susceptible to response bias (Mavila and Francis, 2019; Datta et al., 2021).
Poverty and lack of financial support were identified as key barriers to latrine construction. Government subsidies can help some households construct latrines, dependent on the amount of the subsidy and the method of disbursement, though the current government subsidy scheme is viewed as poor and inadequate (Jain et al., 2020). The current government subsidy of 12,000 rupees ($145 USD) per toilet limits the technologies available to each household, disallowing households from choosing better technology that best fits their local context (Kumar, 2017). The financial aspects of government efforts to reduce OD need to be improved to encourage households to finance latrine construction.
Other barriers to latrine access and use were identified as poor community involvement in SBM implementation, governmental mistrust, and a lack of knowledge about the risks associated with OD. This suggests that, in addition to providing clean, accessible, and affordable sanitation facilities, sanitation programming should also focus on involving communities in implementation to rebuild trust and encourage latrine use. Caruso et al. (2022); Friedrich et al. (2020) conducted community mobilization and behavior-change interventions in villages that received toilets from the SBM to boost latrine use. These interventions resulted in roughly 20 percentage point increases in latrine use, suggesting that targeted behavior-change techniques may be effective in increasing latrine use among households that already have latrines.
Additionally, behavior-change campaigns among government officials may be key to promoting sanitation coverage. Curtis (2019); Bhanot et al. (2017) found that high-level political support for sanitation programming, ambitious SDGs and disruptive leadership changed environments in districts, which led to mindset changes in district officials and contributed to changed behavior in support of the SBM. District officials also reported becoming emotionally involved in the program and felt pride at their achievement in ridding villages of OD (Curtis, 2019). Setting targets and monitoring them is important to hold district leaders accountable for results (Curtis, 2019). Rewarding and recognizing progress can encourage government leaders to continue the promoting sanitation programming.
Hutton et al. (2020) conducted a cost-benefit analysis of the SBM based on cost-benefit model inputs of household-level surveys and found that the program was highly cost-beneficial when communities are free of OD. However, as several studies showed that government claims of improved toilet coverage or an increase in ODF villages were notably overreported, these benefits are likely overestimated.
Community incentives and penalties have been used to encourage proper sanitation practices with varying success. Monetary incentives can be used to encourage household latrine construction, and to repair and renovate nonfunctioning toilets (Jain et al., 2020; Caruso et al., 2022). Furthermore, latrine construction and proper sanitation practices were often accomplished through coercions. Villagers reported guards with sticks being posted to chase people away from common open defecation sites, and local officials often threatened people who did not build latrines (Gupta et al., 2020). It is unknown whether the gains accomplished through coercion will be sustainable.
Overall, preference for OD cannot be solely attributable to material or educational deprivation, as beliefs, values, and cultures also play an important role in people’s decisions to reject affordable latrines (Coffey et al., 2016). Many recommendations surrounding drivers of latrine construction focus on the household’s enabling environment, though sanitation research should emphasize the need to look beyond these household-level drivers to understand social-structural determinants of latrine uptake (Jain et al., 2020). For example, when examining women’s preferences for latrines, a lack of water creates a hesitancy to build; women hesitate to build individual household latrines when sufficient water supply is unavailable because they are the ones who will be burdened with fetching more water from far taps (Mohan, 2017).
While water availability does affect the choice for open defecation, water availability is not the sole factor in determining OD practices, as OD still occurs in households that have access to water (Spears and Coffey, 2019). In one study, 34% of subjects who practiced OD listed lack of water as a reason (Kar and Mistri, 2015). In addition to improving infrastructure, providing educational, community-based services in conjunction with sanitation programming is necessary to encourage households to reduce OD as a sustainable, affordable, and culturally appropriate solution.
In order to meet SDG 6.2 — to achieve access to adequate and equitable sanitation and hygiene for all and end open defecation by 2030 — the United Nations suggests using the proportion of the population using safely managed sanitation services and a hand-washing facility with soap and water as indicators. SDG 6.3.1 also refers to increasing the proportion of domestic and industrial wastewater flows safely treated as an indicator of improving safely managed sanitation (United Nations, 2022). However, as indicated by the JMP, measures of waste containment, storage, and onsite treatment vary widely among countries and among data collection methods (WHO and UNICEF, 2021). For example, in Canada, surveys to assess onsite treatment use “No problems last time pumped, maintained, or inspected” as a measure of containment, while in Nigeria, containment is measured in terms of “No leaks or overflow” (WHO and UNICEF, 2021). For more accurate comparisons among countries, standardized definitions of waste containment, in addition to standard inspection techniques, are needed.
While this systematic review provided a comprehensive overview of the existing peer-reviewed literature on the effectiveness of the SBM in reducing OD and barriers to continued reductions in OD practices, a few limitations were noted. This review was limited by the literature databases to which we had access: PubMed, Scopus, and the EBSCO Global Health database. Searches of other databases, including those containing grey literature and government reports, could have provided a different perspective on OD practices in India. Included studies were also only written in English, and the article search did not include any Hindi journals or publications that could have further informed this systematic review. Additionally, only 13 of the 36 Indian states and territories were represented in the studies in this review. Future work should assess all Indian states and territories to understand the true impact of the SBM on OD practices.
5 Conclusion
While the SBM has improved access to latrines, this systematic review shows that India is yet to be completely ODF. Government reports overestimate the SBM’s progress in eliminating OD, and there are substantive gaps in the literature that are not inclusive of all states in India. The studies included in this review show a lack of sanitation planning, adequate financial support, and awareness as major barriers to latrine use and eliminating OD.
Poor community involvement in SBM implementation, governmental mistrust, and a lack of knowledge about the risks associated with OD were additional barriers associated with higher rates of OD. This suggests that, in addition to providing clean, accessible, and affordable sanitation facilities, sanitation programming should also focus on involving communities in implementation to rebuild trust and encourage latrine use. A lack of public participation and poor maintenance led to poor toilet conditions, which in turn led to a lack of use by individuals. While studies showed modest increases in rates of toilet coverage following SBM implementation, toilets were often not appropriately used or maintained.
Behavior-change interventions among communities and government officials may be key to promoting both latrine coverage and use in India. High-level political support for sanitation programming, ambitious SDGs and disruptive leadership changed environments in districts, which led to mindset changes in district officials and contributed to changed behavior in support of the SBM. Setting targets and monitoring them is important to hold district leaders accountable for results. However, for more accurate comparisons among countries to achieve the SDGs, standardized definitions of waste containment, in addition to standard inspection techniques, are needed.
There is a need for research that looks beyond household-level drivers to understand the social-structural determinants of latrine uptake and long-term successful engagement with communities. Overarching strategies and approaches that have worked well across studies include high involvement of district leadership, pivotal role played by local government members and community motivators, innovative promotional methods and local campaigns, and the use of community incentives. In addition to improving infrastructure, providing educational, community-based services in conjunction with sanitation programming is necessary to encourage households to reduce OD as a sustainable, affordable, and culturally appropriate solution.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
AV: Conceptualization; Methodology; Formal Analysis; Investigation; Writing-original draft preparation; Visualization. LS: Conceptualization; Methodology; Formal Analysis; Investigation; Writing-original draft preparation; Visualization. RB: Formal Analysis; Investigation; Writing-Review and Editing; Visualization. SL: Formal Analysis; Investigation; Writing-Review and Editing; Visualization. AS: Investigation; Resources; Writing-Review and Editing; Supervision. MM: Conceptualization; Methodology; Formal Analysis; Investigation; Resources; Writing-Review and Editing; Visualization and Supervision. All authors read and approved the final manuscript.
Funding
This work was supported and funded by the Water Institute at the University of North Carolina.
Acknowledgments
We are grateful to Carrie Baldwin-SoRelle at the Health Sciences Library at the University of North Carolina, Chapel Hill, for assistance in selecting search terms and electronic databases and in finding the full text of articles.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fenvs.2023.1141825/full#supplementary-material
References
Ackley, B. J., Swan, B. A., Ladwig, G., and Tucker, S. (2008). Evidence-based nursing care guidelines: Medical-surgical interventions. St. Louis, MO: Mosby Elsevier.
Alexander, K., Allton, C., Felsman, C., Hahn, M., Okegbe, T., Palmer, D., et al. (2016). Ending open defecation in India: Insights on implementation and behavior change for Swachh Bharat Abhiyan. New Jersey: Princeton University.
Andres, L. A., Deb, S., Joseph, G., Larenas, M. I., and Grabinsky Zabludovsky, J. (2020). A multiple-arm, cluster-randomized impact evaluation of the Clean India (Swachh Bharat) Mission program in rural Punjab. India: World Bank Policy Research Working Paper.
Anthonj, C., Setty, K. E., Ezbakhe, F., Manga, M., and Hoeser, C. (2020). A systematic review of water, sanitation and hygiene among Roma communities in Europe: Situation analysis, cultural context, and obstacles to improvement. Int. J. Hyg. Environ. Health 226, 113506. doi:10.1016/j.ijheh.2020.113506
Anuradha, R., Dutta, R., Raja, J. D., Lawrence, D., Timsi, J., and Sivaprakasam, P. (2017). Role of community in Swachh Bharat Mission. Their knowledge, attitude and practices of sanitary latrine usage in rural areas, Tamil Nadu. Indian J. community Med. Official Publ. Indian Assoc. Prev. Soc. Med. 42 (2), 107. doi:10.4103/0970-0218.205213
Beardsley, R., Cronk, R., Tracy, W., Fleming, L., Ng'ambi, M., Tidwell, J. B., et al. (2021). Factors associated with safe child feces disposal in Ethiopia, India, and Zambia. Int. J. Hyg. Environ. health 237, 113832. doi:10.1016/j.ijheh.2021.113832
Bhanot, A., Agarwal, V., Awasthi, A., and Sharma, A. (2017). “Making India open-defecation-free: Lessons from the swachh bharat mission–gramin process evaluation,” in Social marketing (UK: Routledge).
Biswas, R., Arya, K., and Deshpande, S. (2020). More toilet infrastructures do not nullify open defecation: A perspective from squatter settlements in megacity Mumbai. Appl. Water Sci. 10 (4), 96–99. doi:10.1007/s13201-020-1169-4
Brownson, R. C., Fielding, J. E., and Maylahn, C. M. (2009). Evidence-based public health: A fundamental concept for public health practice. Annu. Rev. Public Health 30, 175–201. doi:10.1146/annurev.publhealth.031308.100134
Cairncross, S., Hunt, C., Boisson, S., Bostoen, K., Curtis, V., Fung, I. C., et al. (2010). Water, sanitation and hygiene for the prevention of diarrhoea. Int. J. Epidemiol. 39, i193–i205. doi:10.1093/ije/dyq035
Capone, D., Barker, T., Cumming, O., Flemister, A., Geason, R., Kim, E., et al. (2022). Persistent ascaris transmission is possible in urban areas even where sanitation coverage is high. Environ. Sci. Technol. 56 (22), 15969–15980. doi:10.1021/acs.est.2c04667
Caruso, B. A., Sclar, G. D., Routray, P., Nagel, C., Majorin, F., Sola, S., et al. (2022). Effect of a low-cost, behaviour-change intervention on latrine use and safe disposal of child faeces in rural Odisha, India: A cluster-randomised controlled trial. Lancet Public Health 6, e110–e121. doi:10.1016/s2542-5196(21)00324-7
Coffey, D., Gupta, A., Hathi, P., Spears, D., Srivastav, N., and Vyas, S. (2016). “Understanding open defecation in rural India: Untouchability, pollution, and latrine pits,”. International Growth Center (IGC), reference no. F-35114-INC-2.
Coffey, D., Spears, D., and Hathi, P. (2020). Assessing high-profile public messaging for sanitation behaviour change: Evidence from a mobile phone survey in India. Waterlines 39 (4), 240–252. doi:10.3362/1756-3488.19-00011
Conaway, K., Lebu, S., Heilferty, K., Salzberg, A., and Manga, M. (2023). On-site sanitation system emptying practices and influential factors in asian low- and middle-income countries: A systematic review. Hyg. Environ. Health Adv. 6, 100050. doi:10.1016/j.heha.2023.100050
Curtis, V. (2019). Explaining the outcomes of the 'clean India' campaign: Institutional behaviour and sanitation transformation in India. BMJ Glob. health 4 (5), e001892. doi:10.1136/bmjgh-2019-001892
Das, P., and Crowley, J. (2018). Sanitation for all: A panglossian perspective? J. Water, Sanitation Hyg. Dev. 8 (4), 718–729. doi:10.2166/washdev.2018.011
Datta, A., Somani, A., Karmakar, N., and Nag, K. (2021). A study on knowledge and practices regarding swachh bharat mission among urban population of Agartala city, North East India. Med. J. Dr. DY Patil Vidyapeeth 14 (5), 529. doi:10.4103/mjdrdypu.mjdrdypu_65_20
Exum, N. G., Gorin, E. M., Sadhu, G., Khanna, A., and Schwab, K. J. (2020). Evaluating the declarations of open defecation free status under the swachh bharat (‘Clean India’) mission: Repeated cross-sectional surveys in Rajasthan, India. BMJ Glob. Health 5 (3), e002277. doi:10.1136/bmjgh-2019-002277
Friedrich, M., Balasundaram, T., Muralidharan, A., Raman, V. R., and Mosler, H. J. (2020). Increasing latrine use in rural Karnataka, India using the risks, attitudes, norms, abilities, and self-regulation approach: A cluster-randomized controlled trial. Sci. Total Environ. 707, 135366. doi:10.1016/j.scitotenv.2019.135366
Government of India (2018). Guidelines for swachh bharat mission. https://jalshakti-ddws.gov.in/sites/default/files/SBM(G)_Guidelines.pdf.
Government of India (2022). Swachh bharat mission: About SBM. https://swachhbharatmission.gov.in/sbmcms/index.htm.
Gupta, A., Khalid, N., Deshpande, D., Hathi, P., Kapur, A., Srivastav, N., et al. (2020). Revisiting open defecation evidence from a panel survey in rural North India, 2014–18. Econ. Political Wkly. 55 (21), 55–63.
Higgins, J. P. T., Savović, J., Page, M. J., Elbers, R. G., and Sterne, J. A. C. (2022). “Chapter 8: Assessing risk of bias in a randomized trial,” in Cochrane handbook for systematic reviews of interventions version 6.3 (Canada: Cochrane).
Hutton, G., Patil, S., Kumar, A., Osbert, N., and Odhiambo, F. (2020). Comparison of the costs and benefits of the clean India mission. World Dev. 134, 105052. doi:10.1016/j.worlddev.2020.105052
International Institute for Population Sciences (IIPS) and ICF (2017). National family health survey (NFHS-4), 2015-16: India. https://dhsprogram.com/pubs/pdf/FR339/FR339.pdf.
International Institute for Population Sciences (IIPS) and ICF (2021). National family health survey (NFHS-5), 2019-21: India. http://rchiips.org/nfhs/NFHS-5Reports/NFHS-5_INDIA_REPORT.pdf.
Jain, A., Wagner, A., Snell-Rood, C., and Ray, I. (2020). Understanding open defecation in the age of Swachh Bharat Abhiyan: Agency, accountability, and anger in rural Bihar. Int. J. Environ. Res. public health 17 (4), 1384. doi:10.3390/ijerph17041384
Jha, P. K., and Sharma, V. (2020). “On ground study of the ODF status of ghaziabad district, UP,” in Solid waste policies and strategies: Issues, challenges and case studies (Singapore: Springer).
Kar, S., and Mistri, B. (2015). Practice of open defecation and its effect on human health in simlapal block, bankura, West Bengal. J. Interacademia 19 (3), 378–390.
Manga, M., Kolsky, P., Rosenboom, J. W., Ramalingam, S., Sriramajayam, L., Bartram, J., et al. (2022). Public health performance of sanitation technologies in Tamil Nadu, India: Initial perspectives based on E. coli release. Int. J. Hyg. Environ. Health 243, 113987. doi:10.1016/j.ijheh.2022.113987
Manga, M., Muoghalu, C. C., and Acheng, P. O. (2023). Inactivation of faecal pathogens during faecal sludge composting: a systematic review. Environ. Technol. Rev. 12 (1), 150–174. doi:10.1080/21622515.2023.2182719
Manga, M. (2017). The feasibility of Co-omposting as an upscale treatment method for faecal sludge in urban Africa. Leeds, United Kingdom: School of Civil Engineering, University of Leeds. Available at: http://etheses.whiterose.ac.uk/16997/.
Mavila, A. D., and Francis, P. T. (2019). Impact of swachh bharat abhiyan on residents of cochin corporation. Indian J. Community Med. Official Publ. Indian Assoc. Prev. Soc. Med. 44, S19. doi:10.4103/ijcm.ijcm_24_19
Mohan, R. (2017). Swachh bharat mission (gramin): Bottlenecks and remedies. Econ. political Wkly. 52 (20), 1–5.
Muoghalu, C. C., Semiyaga, S., and Manga, M. (2023). Faecal sludge emptying in sub-saharan Africa, south and southeast Asia: A systematic review of emptying technology choices, challenges, and improvement initiatives. Front. Environ. Sci. 11, 158. doi:10.3389/fenvs.2023.1097716
Namdev, G., and Narkhede, V. (2020). Reasons of open defecation behavior in rural households of bhopal, Madhya Pradesh, India. Natl. J. Community Med. 11 (03), 103–106. doi:10.5455/njcm.20200116054019
Narayan, A. S., Maurer, M., and Lüthi, C. (2021). The clean plan: Analysing sanitation planning in India using the CWIS planning framework. J. Water, Sanitation Hyg. Dev. 11 (6), 1036–1047. doi:10.2166/washdev.2021.130
Njuguna, J. (2016). Effect of eliminating open defecation on diarrhoeal morbidity: An ecological study of nyando and nambale sub-counties, Kenya. BMC public health 15, 712. doi:10.1186/s12889-016-3421-2
Patwa, J., and Pandit, N. (2018). Open defecation-free India by 2019: How villages are progressing? Indian J. community Med. official Publ. Indian Assoc. Prev. Soc. Med. 43 (3), 246–247. doi:10.4103/ijcm.IJCM_83_18
Rengaraj, V., Simmon, A., Vikash, S., Zel, R., Adhikari, H., Sherpa, P., et al. (2021). “Addressing sanitation and health challenges in rural India through socio-technological interventions: A case study in Odisha,” in 2021 IEEE 9th Region 10 Humanitarian Technology Conference (R10-HTC), Bangalore, 30 September 2021.
Saleem, M., Burdett, T., and Heaslip, V. (2019). Health and social impacts of open defecation on women: A systematic review. BMC public health 19 (1), 158. doi:10.1186/s12889-019-6423-z
Spears, D., and Coffey, D. (2019). Open defecation in rural India, 2015–16: Levels and trends in NFHS-4. Econ. Political Wkly. 53 (9).
Sprouse, L., Liles, A., Cronk, R., Bauza, V., Tidwell, J. B., and Manga, M. (2022). Interventions to address unsafe child feces disposal practices in the asia-pacific region: A systematic review. H2Open J. 5 (4), 583–602. doi:10.2166/h2oj.2022.137
Sterne, J. A., Hernán, M. A., Reeves, B. C., Savović, J., Berkman, N. D., Viswanathan, M., et al. (2016). ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ Clin. Res. ed.) 355, i4919. doi:10.1136/bmj.i4919
United Nations (UN) (2022). Sdg 6: Ensure availability and sustainable management of water and sanitation for all. New York: United Nations.
Vu, S., Jain, A., Harrison, C., Ghimire, P., and Graham, J. P. (2022). Someone should be there to take care of it”: A case study of users’ views of managed shared sanitation facilities in Jharkhand, India. Am. J. Trop. Med. Hyg. 106 (4), 1135–1140. doi:10.4269/ajtmh.21-0654
Vyas, S., Srivastav, N., Mary, D., Goel, N., Srinivasan, S., Tannirkulam, A., et al. (2019). Measuring open defecation in India using survey questions: Evidence from a randomised survey experiment. BMJ open 9 (9), e030152. doi:10.1136/bmjopen-2019-030152
WHO and UNICEF (2021). Progress on household drinking water, sanitation, and hygiene: 2000-2020, five years into the SDGs. Switzerland: WHO and UNICEF Joint Monitoring Programme.
Keywords: open defecation, Swachh Bharat Mission, water, sanitation, and hygiene (WASH), India, sanitation interventions, open defecation-free
Citation: VerKuilen A, Sprouse L, Beardsley R, Lebu S, Salzberg A and Manga M (2023) Effectiveness of the Swachh Bharat Mission and barriers to ending open defecation in India: a systematic review. Front. Environ. Sci. 11:1141825. doi: 10.3389/fenvs.2023.1141825
Received: 10 January 2023; Accepted: 19 April 2023;
Published: 09 May 2023.
Edited by:
Kangning Xu, Beijing Forestry University, ChinaReviewed by:
Nidhi Nagabhatla, The United Nations University Institute on Comparative Regional Integration Studies (UNU-CRIS), BelgiumMeifang Li, Central South University Forestry and Technology, China
Min Jiang, Jiangsu University of Technology, China
Copyright © 2023 VerKuilen, Sprouse, Beardsley, Lebu, Salzberg and Manga. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Musa Manga, bW1hbmdhQGVtYWlsLnVuYy5lZHU=, bXVzYS5tYW5nYUBtYWsuYWMudWc=
†These authors contributed equally to this work and share first authorship
 Anna VerKuilen†
Anna VerKuilen† Lauren Sprouse
Lauren Sprouse Rachel Beardsley
Rachel Beardsley Sarah Lebu
Sarah Lebu Aaron Salzberg
Aaron Salzberg Musa Manga
Musa Manga