- 1The Pain Education Team to Advance Learning (PETAL) Collaboration
- 2IIMPACT in Health, University of South Australia, Kaurna Country, Adelaide, SA, Australia
- 3NICM Health Research Institute, Westmead, NSW, Australia
- 4Centre for Rehabilitation, School of Health and Life Sciences, Teesside University, Middlesbrough, United Kingdom
- 5Integrated Musculoskeletal Service, North Tees and Hartlepool NHS Foundation Trust, Stockton-on-Tees, United Kingdom
- 6Persistent Pain Research Group, Hopwood Centre for Neurobiology, Lifelong Health Theme, South Australia Health and Medical Research Institute (SAHMRI), Kaurna Country, Adelaide, SA, Australia
- 7Consumer Advisor, IIMPACT in Health, University of South Australia, Kaurna Country, Adelaide, SA, Australia
- 8MedHealth Research, MedHealth, Melbourne, VIC, Australia
- 9Monash University Accident Research Centre, Monash University, Clayton, VIC, Australia
- 10Department of Rehabilitation Medicine, University Medical Center Groningen, University of Groningen, Groningen, Netherlands
- 11Child Health Evaluative Sciences, the Research Institute, The Hospital for Sick Children and Lawrence S. Bloomberg, Faculty of Nursing, The University of Toronto, Toronto, ON, Canada
Pain Neuroscience Education (PNE) emerged over two decades ago in response to the incoherence between evidence-based pain management strategies, and consumer and clinician understandings of “how pain works”. Many clinical trials have investigated the effects of PNE either as a standalone intervention or embedded within a more complex care package, with mixed results. A range of research methods have been used to explore the inconsistent effects of PNE. Together they (i) identify significant shortcomings and limitations of PNE and (ii) raise the possibility that gaining a broadly scientifically accurate understanding of “how pain works” may be critical for subsequent pain and disability improvements. Both learnings strongly suggest that we need to do better. Extensive research incorporating several interest-holders has led to updated content and language and criticisms of both are addressed. The method of PNE has also been updated, with integration of educational frameworks, teaching strategies and tactics, patient resources and clinical tools that all aim to promote the likelihood that patients will learn key concepts and operationalise them to improve their pain, function and quality of life. Pain Science Education is used to differentiate the new approach from PNE.
Introduction
About 30 years ago, a new kind of patient pain education emerged. The content of this education focussed on contemporary understandings of neurophysiology of pain in general, and chronic pain in particular. It first emerged as “intensive neurophysiology education” (1–4) and has become best known as “pain neuroscience education”, or PNE (5). Over 35 randomised controlled trials (RCTs) have tested it, against active, sham and no intervention/usual care comparators. About a decade ago, a mixed picture of evidence from these RCTs was emerging; health care professionals (HCPs) were sometimes reporting that PNE is too difficult to do; patients participating in PNE were reporting feeling invalidated. Clinical audit data however, were suggesting that if PNE is effective in changing understanding, then pain and disability reductions would tend to follow. These factors led to substantial changes in content and educational strategy and the development of patient education resources, tools, tactics and guides. The interdisciplinary, international PETAL Collaboration renamed these newer versions “pain science education”, for two reasons: (i) to differentiate, from PNE, patient education that incorporates these developments in content and method, and (ii) to reflect that wider range of scientific knowledge (rather than just “neuroscience”) that is now included. Here we aimed to provide the historical context of PNE, outline the impetus for, and evidence by which, changes in content and delivery strategies have emerged, provide the scientific developments that are driving progress in patient pain education, discuss criticisms of the content, and present a snapshot of the current state of this fast-moving field.
Historical context: a new kind of pain education emerges as a new intervention
About 30 years ago, rapid advance in the scientific understanding of “how pain works”, facilitated by the seminal discovery of central sensitisation (6) and including pain's protective function, multifactorial nature, dynamic nature over time, and the most effective ways of treating it (7), had created a vast disconnect between scientific and common understanding of the problem of chronic pain. The common understanding remained rooted in a simplistic structural pathology model in which chronic pain was taken to reflect chronic tissue pathology. Evidence-based cognitive-behavioural interventions seemed in contrast to this common understanding. In response to the disconnect, a new educational approach called “intensive neurophysiology education” emerged in 2002 (1–4). The intervention became widely known as “explaining pain” (8), after the primary resource Explain Pain (9), and subsequently, “pain neuroscience education” (PNE) (5). This approach is still being widely taught and delivered under that name and in this article we use “PNE” to refer to the original intervention and to differentiate it from more modern approaches to patient pain education.
The impact of this disconnect between common and scientific understanding of pain, could be seen in patient perspectives on pain management programs that focussed not on pain reduction but on living well despite pain (10). The discovery in 1983 of central sensitisation lent weight to the idea that pain reduction was no longer a reasonable expectation. Central sensitisation was demonstrated after peripheral nerve constriction, whereby second order neurones in the spinal cord became upregulated and responsive to non-nociceptive stimuli (6). That discovery led to some seeing chronic pain as an immutable disorder of the spinal cord (11). The original biopsychosocial model (12) also lent weight to this idea—it posited that the impact of pain involves biological, psychological and social influences. Loeser's 1983 adaptation of the biopsychosocial model to the “onion skin” metaphor (13) brought a more pain-specific framework; psychologists were able to re-purpose cognitive behavioural therapies (CBTs) that were established for other diagnoses such as depression, to help patients decrease the impact of pain on their quality of life (14). Guidelines began to include cognitive and behavioural strategies and education about how to use them in the early 2000's (15).
Our consumer-focussed research identified a significant challenge with this shift towards CBT-based pain management. Many people with chronic pain and many health professionals who treated them, found it difficult to reconcile a CBT and self-management based approach with their understanding of “how pain works”—they found the suggestion confusing and invalidating (1, 2, 4). It was an understandable response: if one understands the presence and degree of pain intensity to accurately signal the presence and degree of tissue damage, then interventions that do not directly target those tissues will of course appear to be nonsense. There was a clear need for a new intervention that could provide patients with an understanding of why CBTs and self-management were biologically sensible. PNE therefore, aimed to enable and empower consumers to engage in CBTs and self-management through first explaining why, not just how, to do it. One can readily see the connection between this early mission and the taglines of public-facing modern day public pain education initiatives such as Pain Revolution (https://www.painrevolution.org)—“rethink, re-engage, recover” and Flippin' Pain (https://www.flippinpain.co.uk)—“engage, educate, empower”.
Clinical trials of PNE have produced mixed results
The earliest randomised controlled trials (RCTs) of PNE compared it to conventional pain education matched for dose, setting and resources, or to an active care comparator, a usual care comparator, or to a waiting list comparator. Those RCTs, in individuals with chronic pain, demonstrated medium to large effects on pain-related neurophysiology knowledge, and small effects on movement-evoked pain, pain-related worry, pain-related self-efficacy, usual pain intensity and pain-related disability (1–4). Since those trials, other trials have been undertaken in various countries, in various settings, and with various diagnostic groups, with the content and format of PNE remaining very consistent. Over 35 RCTs and several meta-analyses on PNE as a stand-alone intervention, and over 50 RCTs of more complex interventions that integrate PNE content, have been undertaken (5, 16–20) (see https://www.petalcollaboration.org/clinical-trials-of-pain-education.html for a list of RCTs). Some studies conclude that PNE as a stand-alone intervention imparts small to medium benefits across a range of outcomes, in a range of chronic pain conditions, in a range of settings and languages e.g., (5), but others report benefit in variables such as knowledge change, catastrphising and fear of pain and (re)injury, but not in pain or disability (19, 21). Opinion pieces advocate for PNE (22–25), but recent commentaries have identified significant challenges and limitations (26–28).
Real world experience of PNE elucidates challenges and limitations
Barriers for clinicians
Significant barriers to the implementation of PNE exist. To date, the only major implementation trial in which physiotherapists were trained in PNE (16 h, 8 h online and 8 h face-to-face) or not (29), was a cluster-randomised implementation study that revealed improved pain-related self-efficacy but not better pain or disability outcomes for patients of the PNE-trained physiotherapists. Health professionals have reported significant challenges in delivering PNE such as: limited appointment time; patient-related factors including a lack of perception of education as an intervention in its own right; clinician-specific issues, such as limited confidence in the implementation process (30). Anecdotally, health professionals have told us that (i) some patients do incredibly well but others do not, (ii) they “try the pain talk” or “do explain pain”, but most patients “don’t buy it” or “don’t want it”. Such anecdotes are also borne out in qualitative analysis of primary care practitioner perspectives, which also suggest health professionals attribute difficulties with PNE to too complex content or patient/learner attitude or capacity, but not to a lack of educational expertise or training (31).
Some health professionals consider that the learning objectives of PNE contradict early pioneers of sensory neurophysiology or certain philosophical and semantic principles (32) [see (33) for a pragmatic commentary on the latter]. Others perceive that educating patients about how pain works undermines their own clinical framework or authority, but the largest group understand and accept the merit and intent of pain education and feel they lack the skills and confidence to deliver it effectively (30). Less experienced clinicians have expressed heightened apprehension about using PNE, concerned that unsuccessful implementation could harm therapeutic relationships (30). Although some services, for example many Canadian pediatric pain programs, stipulate education as mandatory before other care commences, health professionals in other jurisdictions (particularly in adult care) have reported that they stopped pain education altogether “because it is too hard and most patients don’t want it” (31). These results are consistent with the apparent ineffectiveness of PNE training for health professionals, at least as it was delivered in one implementation trial (21). Taken together, the available evidence suggests improvements are needed in the content and method of PNE and the training and support of health professionals to implement it.
Barriers for patients
People living with chronic pain have identified that good pain education is a high care priority, but that they seldom receive it (34). Our real-world data suggest that even “good” education may not be as helpful as we would like. We have investigated this by looking at PNE-related outcomes in clinical practice, outside of research studies. We collected data on knowledge, worry, pain and disability outcomes in a rolling outcome evaluation of over 1,500 consecutive patients, all of whom participated in PNE, with 93% follow-up rate. We used the only assessment for pain knowledge available—the neurophysiology of pain questionnaire (NPQ) (7) and its 12-item revised version (rNPQ) (35). We have previously presented data from 799 of the consumer cohort, all of whom used the original PNQ, and full details of the cohort and the range of diagnoses included, are presented there (36). Two patterns in the outcome evaluation data cast light on the implementation trial outcomes, the qualitative analyses and health professional anecdotes mentioned above.
Pattern 1 in the data: after PNE, less than half of all patients demonstrate an understanding of pain biology that aligns with scientific understanding
The vast majority of change in pain-related knowledge, occurred during the phase in which PNE was the dominant component of care. Mean (SD) change during that time was 4.5 (1.6) points, with a range of 0–9 points (total tool range = 0–19 for NPQ and 0–12 for rNPQ; representing a pre-post large effect size ∼1.5) (36). On the basis of extensive previous work (1, 2, 4), we estimated that a score of >10 on the NPQ and >8 on the rNPQ reflected a conceptualisation of pain that is consistent with contemporary pain science. Forty-six percent of patients reached this threshold; all maintained the shift and a further 4% reached the threshold 5 months later. That is, only half of the patients who participated in PNE delivered by experienced pain educators, learnt its key conceptual objectives.
Pattern 2 in the data: long-term outcomes are better when learning objectives are achieved early on
Patients completed pain (0–100 Numerical Rating Scale (NRS) of “average pain over that last two days”) and disability [patient-specific functional scale (37)] assessments between 12 and 18 months after their initial appointments. The mean (SD) reduction in usual pain was 36 (19)/100; the mean increase in function was 62 (19)% of the maximum possible score. However, those who achieved the threshold level in NPQ/rNPQ at one month, went on to report a bigger decrease in pain and increase in function than those who did not achieve the threshold level (Table 1).
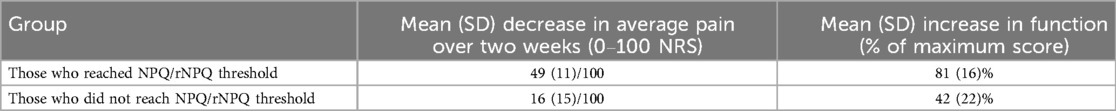
Table 1. A more scientifically based understanding of pain biology early in treatment is associated with a bigger decrease in pain and increase in function 12–18 months later.
Suboptimal patient experiences
The findings from the above outcome evaluation mirror the results of a series of qualitative studies exploring patients’ experience of PNE (one 90 min group session) within clinical settings. The extent of pain reconceptualisation with PNE appears highly variable, for example a positive experience:
“.it also reassured me that I wasn’t going barmy … it [PNE] explained that I’m not. What I am experiencing is real and it explained why, without something necessarily being wrong … things like the sensitivity is a kind of new thing that no one had offered before.” (Participant B post-PNE (38) page 1391)
In contrast, some found the PNE content irrelevant to themselves, their pain and their situation-
“It was just basically stubbing your toe .. I don’t want to know about my toe. I've stubbed my toe, fair enough and I know it last days. But I want to know about why I’ve got the constant pain in my spine. And it just didn't materialise.” (Participant J post-PNE) (39) page 59.
That the content of PNE can lack relevancy, a problem potentially exacerbated by the brief and didactic nature of PNE delivery within a group setting, was a consistent theme across studies (38–40) and points to the need for a stronger consumer voice in guiding the content of pain education. Moreover, even when the content is relevant, and clinical benefits ensue, we have often observed what we call “partial and patchy” reconceptualization: patients describe their pain with some language inconsistent with contemporary pain science:
“Because you assume if you’re in constant pain its damage to the nerves and something you're doing is aggravating it and just what's causing the constant pain rather than it being (reinjured) and it was explained about the with the heightened sensitivity.” (Participant C post-PNE) (39), page 59,
and other language inconsistent with contemporary pain science:
I believe it's the damage to the discs in my spine. (Participant C post-PNE) (39) page 59.
These patterns from real world evaluation data and qualitative research studies show that there is significant room for improvement for PNE in both content and strategy. Participant reflections on a PNE-based complex chronic back pain intervention are corroborative: of all components of the treatment, the educational component was the most difficult; some didn't expect nor want “a pain talk”; some felt invalidated by it; some “couldn’t understand what the health professional was going on about” (41). Although outcome evaluation data do not allow for causal conclusions, they provide a clear hypothesis for testing: when education is successful, the likelihood of reducing pain and disability is high; when it is not, that likelihood is low and may be accompanied by negative therapeutic experiences. It is not unreasonable to propose that reconceptualization of “how pain works” might be a critical determinant of response to care.
Criticisms of the content of pain science education
The content of Pain Science Education has not escaped criticism. Those criticisms can be grouped into “its content is wrong” and “its delivery is invalidating or dangerous”. These criticisms are rare, but those who hold them are very vocal, primarily through social media channels, or via letters of concern sent to our dissemination and outreach partners, our employers, research funders or the learned societies of which we are members. Respectful and constructive criticism is critical in science, particularly in a field such as ours in which substantial knowledge and translational gaps, inconsistent terminology and field-specific jargon, exist. We take the opportunity here to discuss these criticisms.
Is the content of modern pain education “wrong”?
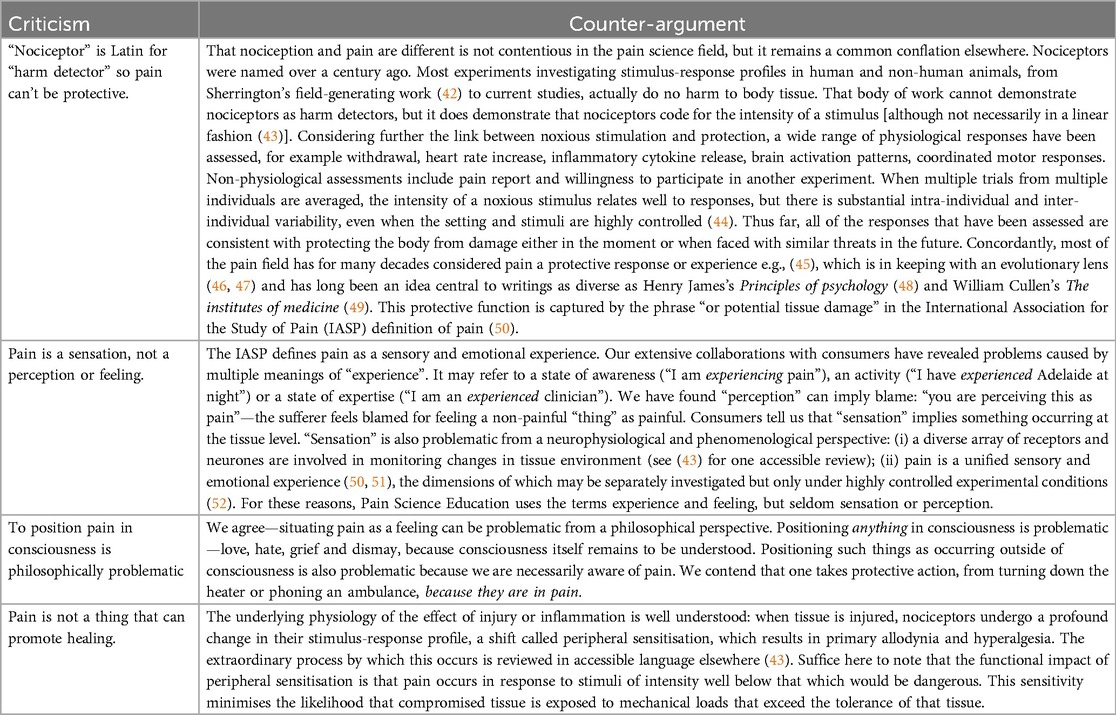
It is difficult in science to conclude things to be definitively wrong or right. However, Tables 2–4 present the most common criticisms of the “Essential Pain Facts”, derived through the research outlined below under “Potential solutions”.
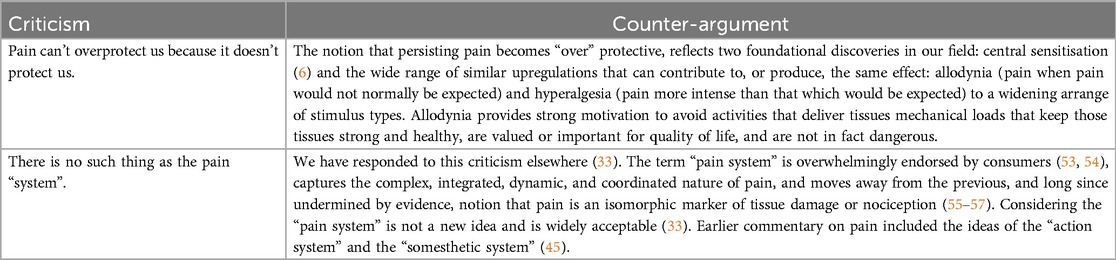
Table 3. Criticisms of the pain science concept “Persisting pain overprotects us and prevents recovery.”
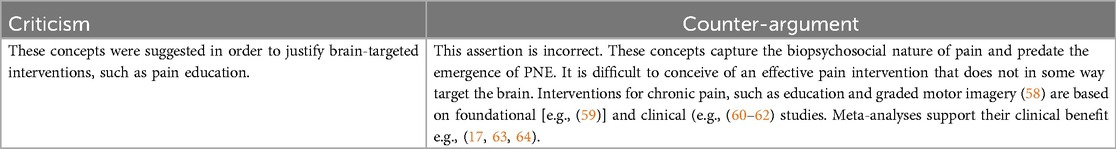
Table 4. Criticism of the pain science concepts “Many factors influence pain” AND “there are many ways to reduce pain and gradually recover.”
Is the public communication of modern pain science concepts invalidating and dangerous?
We are among those to argue that shifting community norms and consumer expectations around pain care and recovery has the potential to reduce common barriers to participating in guideline-based care and promote better clinical outcomes (30, 65, 66). Our patient partners have also identified that society-wide knowledge translation interventions that target misconceptions about pain and its management, are needed (67). Our recent meta-analyses showed that population beliefs about pain management can be positively shifted in line with guideline-based care (i.e., “staying active”, “avoiding rest”) using contemporary media campaigns (65). However, care must be taken to understand the audience and communicate with them appropriately, so as to avoid the messages being delivered in a poorly contextualised way, leading to misinterpretation, and feelings of invalidation or potentially iatrogenesis (33, 68). We have also demonstrated that approximately half of all public health education programs are unsuccessful for those from marginalised and minoritised communities (ie those who may most need the programs) and that co-developing education programs with the target audience is critical to address their needs (69). We have identified the need for better pain education delivery for disadvantaged groups such as those from ethnically minoritized groups, those with low health literacy, and those who receive their care through an interpreter (68, 70). Relevant here is the wider need across the pain field to better understand the social context of research participants, a need that has triggered a global push to include a minimum equity-relevant data set in all human pain research (71–76).
Building better pain education involves partnerships with consumers (e.g., members of the public, people with lived experience of pain and their carers/families, and patient reference groups) in the design, planning and delivery of public-facing pain education initiatives and resources [e.g., (77), see also painrevolution.org and flippinpain.co.uk]. Even so, this does not guarantee that all outreach will be acceptable by all people and in all contexts. For example, as part of ongoing efforts to optimise accessibility of Pain Revolution's public facing resources and professional development offerings within its Local Pain Educator, Local Pain Collective, and Rural Outreach Tour initiatives, Pain Revolution regularly consults consumers. It undertook two mini-surveys to arrive at the terms “Essential Pain Facts” and “Pain System Hypersensitivity”. Figure 1 provides a brief summary of these surveys and their results. The themes derived in response to Survey 2 (Figure 1) bear some resemblance to the documented characteristics of nociplastic pain (78).
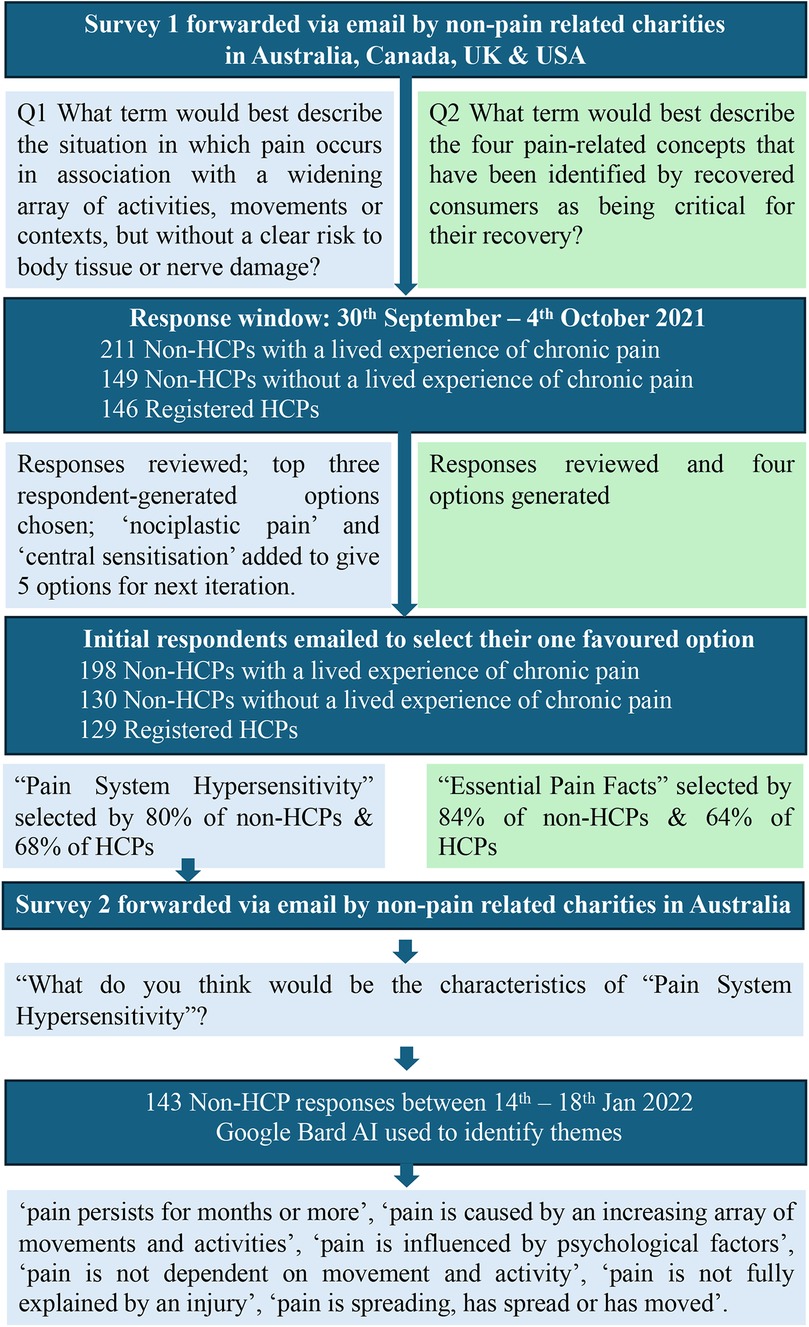
Figure 1. Brief summary of two consumer surveys undertaken by pain revolution, which arrived at the terms “Pain System Hypersensitivity” and “Essential Pain Facts” (survey 1) and validated the former as a suitable proxy for “nociplastic pain” (survey 2). HCP = health care professional; AI = artificial intelligence tool.
Is reconceptualization of how pain works important for subsequent pain and disability improvements?
Recently, three clinical trials of complex multimodal treatments that aimed to shift patients' understanding of the problem of back pain, have shown clinical benefit over and above that offered by their comparator (a sham intervention (79), an open label placebo or usual care (80, 81). Two of those trials were grounded in, and included, PNE (79, 80). They also included planned analyses of whether reconceptualization of the problem contributed to the clinical benefit. The first used a mediation analysis approach and showed that the vast majority of the overall treatment effect of a PNE-grounded intervention [the “Resolve” approach (82)] on pain at post-treatment (global effect of intervention = −0.96 [−1.47 to −0.28]) was mediated by the change in the participants' understanding of their back pain problem, assessed after the PNE component of the program (effect of mediator = −0.96 [−1.47 to −0.64]); the effects were very similar for disability (83). The other clinical trial (80) asked participants before and after treatment about their understanding of the cause(s) of their back pain. They showed that re-attribution of back pain, from tissue-related pathology to psychological stress and brain-related mechanisms, was highly related to clinical improvement (84). These trials of complex interventions suggest that reconceptualization of how pain works seems to be an important determinant of subsequent pain and disability improvements. We contend that these findings are also consistent with the possibility that reconceptualization of “how pain works” might be a critical determinant of response to care in the real world. Efforts to make pain education better seem warranted.
Potential solutions
Changing content and method
Numerous scientific studies, which involved hundreds of recovered consumers and health professionals, and dozens of pain, education and learning scientists (28, 30, 33, 38–41, 53, 83, 85–87) have led to significant changes in content and learning objectives. Full coverage of that work is beyond the scope of this review, but in brief: several cohorts of consumers who self-identified as having improved or completely recovered from a chronic pain condition, were interviewed or surveyed about what they learnt or did that lead to their recovery. These data formed the basis of the iterative development of “key learning objectives for pain education” (43, 53) (see https://www.painrevolution.org/painfacts for brief two-page “fact sheets” for each objective). These concepts were prioritised for importance by consumers and cross-checked for accuracy according to published scientific papers, by an interdisciplinary group of active pain researchers, and for acceptability by an interdisciplinary group of practising health and medical professionals. Finally, through collaboration with a health communications firm and more consumer consultation, four key concepts were derived and, through final consumer and clinician surveys, were labelled “Essential Pain Facts” (28, 82).
Extensive research has also been directed towards improving how PNE could be implemented more effectively [e.g., (19, 30)]. This has meant drawing on more contemporary approaches to curriculum development and lesson plans [e.g., (43)] and using more contemporary educational frameworks and strategies [see (28)]. Modern pain education takes a constructivist approach to learning, integrates active, constructive, interactive and inventive learning tasks (88), includes a range of teaching “tactics” during educational encounters, and uses novel clinical tools such as sequential art, storytelling, active tasks and virtual-reality mediated embodied experiences. The theoretical frameworks and some strategies have been drawn from education research, where they have been shown to improve learning in over 300 meta-analyses of data from several million participants (89). Other strategies are based on the principles that govern the neurophysiology of learning (43); others are grounded in social cognitive theory (90). It is important to acknowledge that many clinicians have already begun to use contemporary teaching methods to enhance their educational offerings, although up to 40% of health professionals who regularly deliver pain education are unable to name an educational strategy (30).
In 2023, the Pain Education Team to Advance Learning (PETAL) Collaboration was formed. This international, interdisciplinary collaboration of researchers, clinicians and consumers engaged in pain education research and seeking to synergise international efforts, elected to use “Pain Science Education” to describe modern pain education. There were two reasons for this move: (i) to differentiate, from PNE [which is still taught and delivered in its original form (28)], modern patient education that incorporates these developments in content and method, and (ii) to reflect that wider range of scientific knowledge (rather than just “neuroscience”) that is now included.
The intent of making pain education better is clear: maximise learning about how pain works in order to optimise endorsement and adoption of a graded reactivation and self-management approach to recovery. The logic is simple: if the didactic “old school” PNE approach is one of the most effective treatments we currently have for chronic pain (91), then much more effective education (i.e., a “stronger dose”) is likely to be more beneficial, and thus deliver better clinical outcomes. Robust clinical trials will support or refute this logic.
Co-designed resources and sequential art
Co-designed education involves authentic and meaningful engagement with learners (consumers, clinicians and the public) and health professionals throughout the design and development stages, ensuring that tools and resources resonate with their needs, thereby improving acceptability and uptake (92). Pain Science Education draws heavily on co-design methods as well as progress in educational and conceptual change sciences (28). Tools and resources are designed to enrich the learning environment, provide learning opportunities for learners with a wider range of skills and previous educational attainment, and make learning more enjoyable and meaningful—promoting what Hattie and O'Donoghue call the “will” and “thrill” of learning (89). The strategies embedded in these tools are not unique to patient pain education, but have only recently been integrated into it. One such strategy is sequential art, known colloquially as “comics” or “cartoons”, which can be presented in isolation—conveying a specific point— and also as a coherent whole in which certain characters assist to build a longer, cohesive narrative (93). For example, character development of Snoopy and Charlie Brown in Peanuts allows their personality and context to infer complex meanings and inferences (94). Randomised controlled experiments demonstrate that the use of sequential art enhances learning outcomes across several domains (95).
Recent patient-targeted pain education resources for the general public use sequential art (e.g., https://www.tamethebeast.org and flippinpain.co.uk/formula/), for children and youth (96, 97) and for adults with chronic pain (82, 98). The development of these resources involved individual stories to target a specific concept, linking concepts and inferring more complex, nuanced concepts through the development of characters across multiple stories. Extensive consumer involvement during development promotes the relevance, readability and acceptability of the resources, but the international use of the resources means that colloquial language and cultural references, which can offer powerful learning opportunities, are necessarily limited.
We also co-designed a series of brief animated videos in partnership with people living with osteoarthritis to challenge common misconceptions (e.g., osteoarthritis is caused by “wear and tear” of joint cartilage) that reduce participation in guideline-based care. Using Pain Science Education concepts to provide compelling alternative narratives (e.g., “bioplasticity of cartilage”), our pilot data (n = 291) showed that a single view trial of these animations led to medium to large reductions in misconceptions in both lay people (with and without OA) and health professionals (99). People with OA also reported reduced fear of movement and an increased intention to exercise, and feedback on the videos was highly positive, with many citing the clear and patient-friendly explanations. The positive reception was unlikely to reflect resonance with pre-held beliefs. To the contrary, the content probably challenged pre-held beliefs: over 70% of consumers reported that it was different from information previously provided to them by health professionals. We do not know whether this reflects poor knowledge or poor education strategy of their previous providers.
The ancient (100) tactic of storytelling can foster deeper engagement with the studied material and has long been thought to improve the extent of learning and retention (101). Storytelling interventions, by altering health-related societal norms, have been shown to impact major public health issues, including sexual health, substance use, hypertension control, and vaccination, across diverse international contexts including culturally diverse communities (102). Storytelling can stimulate and maintain interest in the topic, provide a structure for delivery and remembering the material, and improve the connection between the educator and the learner (103, 104). Examples in the pain field include the children's comic book “Medikidz Explain Chronic Pain: What's Up with Moira's Grandad” (105) and “Painful Yarns. Metaphors and stories to help understand the biology of chronic pain” (106). The former addresses the challenges that older people with chronic pain experience when trying to explain to their grandchildren why they are sometimes unable to play with them because of their condition. The latter consists of short stories used as metaphors for pain science concepts; a small clinical trial suggested it improved understanding of pain biology (107). Our patient partners have also highlighted the potential of patient testimonial storytelling: “Storytelling is powerful. There is nothing like someone else's experience with a good outcome—it shows that it can work.” Supplementary material 1 [(67), p. 6].
VR-enhanced pain education and modern pain education tactics
One tool that has enhanced educational outcomes in mainstream education is virtual reality (VR)-mediated embodied learning experiences. A meta-analysis of 43 trials, undertaken in several education settings, reported medium to large effect sizes on a range of learning outcomes, including cognitive, intellectual, motor and behavioural outcomes (108). VR-enhanced education creates experiences within a virtual environment, usually via head-mounted goggles, that target specific learning objectives. Using VR to enhance health education has been explored in women undergoing breast cancer (109) or cardiac (110) surgery. VR is not new to the chronic pain space (111), and others have delivered the didactic “presentation-based’ PNE using VR goggles (112, 113), reporting positive results. Using VR to deliver content in a similar way to how it might be delivered face-to-face or online seems a missed opportunity—the learning potential created by VR is likely to come from generating compelling and memorable experiences and active learning activities.
We have assisted one VR-based platform in its objective to generate experiences and activities, to achieve deep learning of PSE's learning objectives. Three independent research groups have undertaken preliminary investigation: Skidmore et al. (114) found that the Reality Health VR-enhanced pain education platform (Reality Health, Sydney, Australia) is easy for health professionals to use; provides credibility for using education as an intervention; provides users with safe experiences that reinforce and rapidly consolidate PSE's learning objectives. Mardon et al. (115) found it to be feasible, acceptable and safe for use with war Veterans with and without post-traumatic stress, and health professionals who treat them: key themes were novelty, compelling learning experiences, enjoyable, easy to use, and made complex concepts easy to understand. Kennedy et al. (116) evaluated the platform with patients on a waiting list for specialist pain services in Australia: 28 participants, 11% identifying as Australian Aboriginal origin and 9 as being born overseas, rated highly its ease of use (4.6/5), enjoyment (4.7/5), and their desire to use it again (4.3/5); 23 reported improvement with physical activities and mood, and 19 reported improvement in pain levels after the VR-based program. Clinical audit data appear promising: 315 long-term injured workers completed a VR-enhanced pain education program, showing substantial pre-post reductions in pain, pain interference and self-efficacy (full outcome evaluation data are presented with permission at https://www.petalcollaboration.org). Whether or not VR-enhanced PSE improves clinical outcomes more effectively than PSE without VR is yet to be investigated in a clinical trial.
With or without access to VR-enhanced pain education, a range of tactics can be employed by pain educators to enhance deep learning of PSE's learning objectives (82, 98). Using a modified ICAP conceptual change framework (88, 117), tasks that foster deep learning, from “active”, to “constructive” and “interactive/inventive” tasks, should improve pain education outcomes, just as they have been shown to do in conventional educational contexts. The RECLAIMA acronym (Table 5) can guide clinicians towards simple tactics that they can use “in the moment” to push learners towards deeper learning, and the SALAD task (28) can be used to integrate constructive and inventive strategies into reading, video-based or audio-based “homework”.
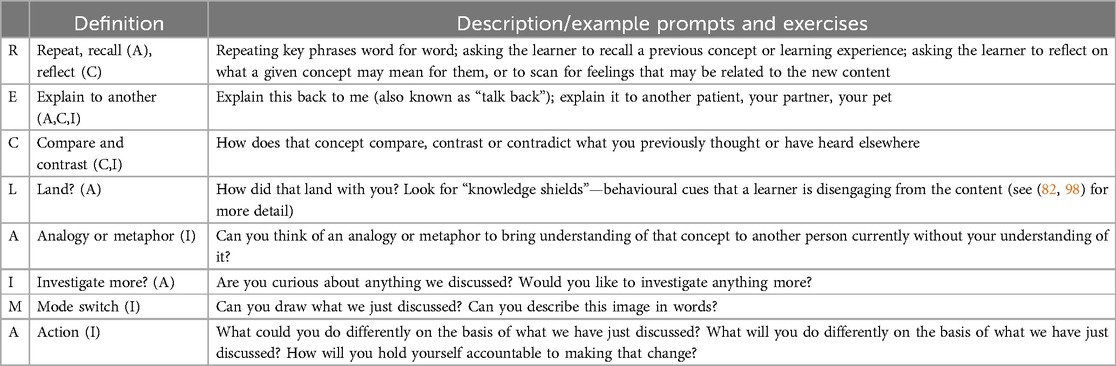
Table 5. The RECLAIMA tactics list. Letters in parentheses (A), (C), (I), denote the level of learning involved according to a modified version of the ICAP Framework (88)—Active (A), Constructive (C) or Interactive/Inventive (I).
Conclusion and summary
We aimed to provide an account of pain education focussed on imparting scientifically accurate understanding of “how pain works”, its emergence over 20 years ago and its substantial adaptation and growth since then. RCTs consistently show improvements in cognitive variables such as knowledge, self-efficacy and fear, but evidence around pain and disability improvements is mixed. A range of methods have been used to demonstrate that reconceptualization of “how pain works” may be a key determinant of subsequent clinical improvement. Critically, challenges to the implementation of early iterations clearly identified the need for more relevant content and better educational strategy. These content and strategy changes have led to what is now termed Pain Science Education, which targets specific learning objectives broadly covered by the Essential Pain Facts, and includes a range of strategies and clinical tools and resources.
Where to from here? We contend that the health education field has great scope for improvement and that there is a pressing obligation for us to make pain education better. Our research groups are prioritising co-design with consumers and end users. We are also exploring methods to push modern understanding to the wider public, for example via Pain Revolution (https://www.painrevolution.org), Flippin' Pain (https://www.flippinpain.co.uk) and the EQUiPP Project (https://www.equipp.org.au), which is employing a “micro-community” precision co-design approach to formulating general public pain messaging strategies. Further priorities include increasing knowledge and skills among health professionals across the health system and development of resources to assist health professionals fast track the changes in understanding that seem to most closely relate to subsequent improvement and often recovery.
Author contributions
GLM: Conceptualization, Funding acquisition, Writing – original draft, Writing – review & editing. AM: Writing – original draft, Writing – review & editing. JW: Writing – original draft, Writing – review & editing. FB: Writing – original draft, Writing – review & editing. MVW: Writing – original draft, Writing – review & editing. TB: Writing – original draft, Writing – review & editing. JL: Writing – original draft, Writing – review & editing. DS: Writing – original draft, Writing – review & editing. MR: Writing – original draft, Writing – review & editing. JS: Writing – original draft, Writing – review & editing. CR: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. GLM and the PETAL Collaboration are supported by a Leadership Investigator grant from the National Health & Medical Research Council of Australia (ID 1178444). AKM is supported by a philanthropic research grant from the Wilson Foundation. FB is supported by Medical Research Future Fund Clinical Trials Activity grant (ID 2023048). MVW is supported by a Research Training Program domestic (RTPd) stipend from the Commonwealth of Australia.
Conflict of interest
GLM is unpaid scientific advisor to Reality Health VR-pain education. He has also received support from: Reality Health, ConnectHealth UK, Institutes of Health California, AIA Australia, Workers’ Compensation Boards and professional sporting organisations in Australia, Europe, South and North America. Professional and scientific bodies have reimbursed him for travel costs related to presentation of research on pain and pain education at scientific conferences/symposia. He has received speaker fees for lectures on pain, pain education and rehabilitation. He receives royalties for books on pain and pain education. He is non-paid CEO of the non-profit Pain Revolution. AM has been reimbursed travel costs related to presentations on pain at scientific conferences/symposia. She has received speaker fees for lectures on pain and pain education. FB has been reimbursed travel costs related to presentations on pain at scientific conferences/symposia. She has received speaker fees for lectures on pain and pain education. She is a member of the Scientific Programming Committee for the Australian Pain Society. TB has received income from Pain Revolution and for participation in co-design research projects. JL participated in the RESOLVE clinical trial, for which first author GLM was a Chief Investigator. Pain Adelaide Stakeholders' Consortium reimbursed him for travel costs to present at their conference. DS holds a research position with MedHealth. MR has expenses reimbursements and speaker fees for presentations on pain and rehabilitation. CR is a named inventor on a patent for a sensory discrimination training based medical device which could be used in the management of persistent pain conditions. He is also the community pain champion for the Flippin Pain™ campaign which is run by Connect Health Ltd. He has received research funding from NIHR, Innovate UK, Medtronics Ltd., MediDirect Ltd., 2PD Ltd., and The Health Foundation. He has received expenses reimbursements and speaker fees for presentations on pain and rehabilitation.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Correction Note
This article has been corrected with minor changes. These changes do not impact the scientific content of the article.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Moseley L. Combined physiotherapy and education is efficacious for chronic low back pain. Aust J Physiother. (2002) 48(4):297–302. doi: 10.1016/S0004-9514(14)60169-0
2. Moseley GL. Joining forces—combining cognition-targeted motor control training with group or individual pain physiology education: a successful treatment for chronic low back pain. J Man Manip Therap. (2003) 11:88–94. doi: 10.1179/106698103790826383
3. Moseley GL. Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. Eur J Pain. (2004) 8(1):39–45. doi: 10.1016/S1090-3801(03)00063-6
4. Moseley GL, Nicholas MK, Hodges PW. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain. (2004) 20(5):324–30. doi: 10.1097/00002508-200409000-00007
5. Louw A, Zimney K, Puentedura EJ, Diener I. The efficacy of pain neuroscience education on musculoskeletal pain: a systematic review of the literature. Physiother Theory Pract. (2016) 32(5):332–55. doi: 10.1080/09593985.2016.1194646
6. Woolf CJ. Evidence for a central component of post-injury pain hypersensitivity. Nature. (1983) 306(5944):686–8. doi: 10.1038/306686a0
7. Moseley L. Unraveling the barriers to reconceptualization of the problem in chronic pain: the actual and perceived ability of patients and health professionals to understand the neurophysiology. J Pain. (2003) 4(4):184–9. doi: 10.1016/S1526-5900(03)00488-7
8. Moseley GL, Butler DS. 15 years of explaining pain—the past, present and future. J Pain. (2015) 16(9):807–13. doi: 10.1016/j.jpain.2015.05.005
9. Butler DS, Moseley GL, Sunyata . Explain Pain. 2nd edn. Adelaide, Australia: Noigroup Publications (2003). p. 133.
10. Gatchel R, Turk D. Psychological Approaches to Pain Management. New York City, NY: The Guilford Press (1996). p. 519.
11. George SZ, Bishop MD. Chronic musculoskeletal pain is a nervous system disorder… now what? Phys Ther. (2018) 98(4):209–13. doi: 10.1093/ptj/pzy002
12. Engel GL. The need for a new medical model: a challenge for biomedicine. Science. (1977) 196(4286):129–36. doi: 10.1126/science.847460
13. Loeser JD. Concepts of pain. In: Stanton Hicks M, Boaz R, editors. Chronic Low Back Pain. New York: Raven Press (1982). p. 109–42.
14. Bradley LA. Cognitive-behavioral therapy for chronic pain. In: Gatchel RJ, Turk DC, editors. Psychological Approaches to Pain Management. New York: The Guildford Press (1996). p. 131–47.
15. Sanders SH, Harden RN, Vicente PJ. Evidence-based clinical practice guidelines for interdisciplinary rehabilitation of chronic nonmalignant pain syndrome patients. Pain Pract. (2005) 5(4):303–15. doi: 10.1111/j.1533-2500.2005.00033.x
16. Saracoglu I, Akin E, Aydin Dincer GB. Efficacy of adding pain neuroscience education to a multimodal treatment in fibromyalgia: a systematic review and meta-analysis. Int J Rheum Dis. (2022) 25(4):394–404. doi: 10.1111/1756-185X.14293
17. Bulow K, Lindberg K, Vaegter HB, Juhl CB. Effectiveness of pain neurophysiology education on musculoskeletal pain: a systematic review and meta-analysis. Pain Med. (2021) 22(4):891–904. doi: 10.1093/pm/pnaa484
18. Clarke CL, Ryan CG, Martin DJ. Pain neurophysiology education for the management of individuals with chronic low back pain: systematic review and meta-analysis. Man Ther. (2011) 16(6):544–9. doi: 10.1016/j.math.2011.05.003
19. Watson JA, Ryan CG, Cooper L, Ellington D, Whittle R, Lavender M, et al. Pain neuroscience education for adults with chronic musculoskeletal pain: a mixed-methods systematic review and meta-analysis. J Pain. (2019) 20(10):1140 e1–e22. doi: 10.1016/j.jpain.2019.02.011
20. Suso-Marti L, Cuenca-Martinez F, Alba-Quesada P, Munoz-Alarcos V, Herranz-Gomez A, Varangot-Reille C, et al. Effectiveness of pain neuroscience education in patients with fibromyalgia: a systematic review and meta-analysis. Pain Med. (2022) 23(11):1837–50. doi: 10.1093/pm/pnac077
21. Khosrokiani Z, Letafatkar A, Hadadnezhad M, Sokhanguei Y. Comparison the effect of pain neuroscience and pain biomechanics education on neck pain and fear of movement in patients with chronic nonspecific neck pain during the COVID-19 pandemic. Pain Ther. (2022) 11(2):601–11. doi: 10.1007/s40122-022-00371-3
22. Goudman L, Huysmans E, Ickmans K, Nijs J, Moens M, Putman K, et al. A modern pain neuroscience approach in patients undergoing surgery for lumbar radiculopathy: a clinical perspective. Phys Ther. (2019) 99(7):933–45. doi: 10.1093/ptj/pzz053
23. Malfliet A, Leysen L, Pas R, Kuppens K, Nijs J, Van Wilgen P, et al. Modern pain neuroscience in clinical practice: applied to post-cancer, paediatric and sports-related pain. Braz J Phys Ther. (2017) 21(4):225–32. doi: 10.1016/j.bjpt.2017.05.009
24. Louw A, Nijs J, Puentedura EJ. A clinical perspective on a pain neuroscience education approach to manual therapy. J Man Manip Ther. (2017) 25(3):160–8. doi: 10.1080/10669817.2017.1323699
25. Nijs J, Wijma AJ, Leysen L, Pas R, Willaert W, Hoelen W, et al. Explaining pain following cancer: a practical guide for clinicians. Braz J Phys Ther. (2019) 23(5):367–77. doi: 10.1016/j.bjpt.2018.12.003
26. Wand BM, Cashin AG, McAuley JH, Bagg MK, Orange GM, Moseley GL. The fit-for-purpose model: conceptualizing and managing chronic nonspecific low back pain as an information problem. Phys Ther. (2023) 103(2):pzac151. doi: 10.1093/ptj/pzac151
27. Roose E, Nijs J, Moseley GL. Striving for better outcomes of treating chronic pain: integrating behavioural change strategies before, during, and after modern pain science education. Braz J Phys Ther. (2023) 27(6):100578. doi: 10.1016/j.bjpt.2023.100578
28. Moseley GL, Leake HB, Beetsma AJ, Watson JA, Butler DS, van der Mee A, et al. Teaching patients about pain: the emergence of pain science education, its learning frameworks and delivery strategies. J Pain. (2024) 25(5):104425. doi: 10.1016/j.jpain.2023.11.008
29. Lane E, Magel JS, Thackeray A, Greene T, Fino NF, Puentedura EJ, et al. Effectiveness of training physical therapists in pain neuroscience education for patients with chronic spine pain: a cluster-randomized trial. Pain. (2022) 163(5):852–60. doi: 10.1097/j.pain.0000000000002436
30. Wilson MV, Braithwaite FA, Arnold JB, Stanton TR. Real-world implementation of pain science education and barriers to use in private practice physiotherapy settings: an Australia-wide cross-sectional survey. Pain. (2025). doi: 10.1097/j.pain.0000000000003521
31. Mankelow J, Ryan CG, Green PW, Taylor PC, Martin D. An exploration of primary care healthcare professionals’ understanding of pain and pain management following a brief pain science education. BMC Med Educ. (2022) 22(1):211. doi: 10.1186/s12909-022-03265-2
32. Cohen M, Weisman A, Quintner J. Pain is not a “thing”: how that error affects language and logic in pain medicine. J Pain. (2022) 23(8):1283–93. doi: 10.1016/j.jpain.2022.03.235
33. Moseley GL, Pearson N, Reezigt R, Madden VJ, Hutchinson MR, Dunbar M, et al. Considering precision and utility when we talk about pain. Comment on Cohen et al. J Pain. (2023) 24(1):178–81. doi: 10.1016/j.jpain.2022.05.010
34. Slater H, Jordan JE, O’Sullivan PB, Schutze R, Goucke R, Chua J, et al. “Listen to me, learn from me”: a priority setting partnership for shaping interdisciplinary pain training to strengthen chronic pain care. Pain. (2022) 163(11):e1145–e63. doi: 10.1097/j.pain.0000000000002647
35. Catley MJ, O'Connell NE, Moseley GL. How good is the neurophysiology of pain questionnaire? A Rasch analysis of psychometric properties. J Pain. (2013) 14(8):818–27. doi: 10.1016/j.jpain.2013.02.008
36. Lee H, McAuley JH, Huebscher M, Kamper SJ, Traeger AC, Moseley GL. Does changing pain-related knowledge reduce pain and improve function through changes in catastrophizing? Pain. (2016) 157(4):922–30. doi: 10.1097/j.pain.0000000000000472
37. Chatman AB, Hyams SP, Neel JM, Binkley JM, Stratford PW, Schomberg A, et al. The Patient-Specific Functional Scale: measurement properties in patients with knee dysfunction. Phys Ther. (1997) 77(8):820–9. doi: 10.1093/ptj/77.8.820
38. King R, Robinson V, Ryan CG, Martin DJ. An exploration of the extent and nature of reconceptualisation of pain following pain neurophysiology education: a qualitative study of experiences of people with chronic musculoskeletal pain. Patient Educ Couns. (2016) 99(8):1389–93. doi: 10.1016/j.pec.2016.03.008
39. Robinson V, King R, Ryan CG, Martin DJ. A qualitative exploration of people’s experiences of pain neurophysiological education for chronic pain: the importance of relevance for the individual. Man Ther. (2016) 22:56–61. doi: 10.1016/j.math.2015.10.001
40. King R, Robinson V, Elliott-Button HL, Watson JA, Ryan CG, Martin DJ. Pain reconceptualisation after pain neurophysiology education in adults with chronic low back pain: a qualitative study. Pain Res Manag. (2018) 2018:3745651. doi: 10.1155/2018/3745651
41. Rizzo RR, Wand BM, Leake HB, O'Hagan ET, Bagg MK, Bunzli S, et al. “My back is fit for movement”: a qualitative study alongside a randomized controlled trial for chronic low back pain. J Pain. (2023) 24(5):824–39. doi: 10.1016/j.jpain.2022.12.009
42. Sherrington C. The Integrative Action of the Nervous System. New Haven: Yale University Press (1906). p. 411.
43. Moseley GL, Butler DS. Explain Pain Supercharged. Adelaide: NOIgroup Publications (2017). p. 234.
44. Madden VJ, Kamerman PR, Catley MJ, Bellan V, Russek LN, Camfferman D, et al. Variability in experimental pain studies: nuisance or opportunity? Br J Anaesth. (2021) 126(2):e61–e4. doi: 10.1016/j.bja.2020.11.005
45. Melzack R, Wall PD. Pain mechanisms: a new theory. Science. (1965) 150(699):971–9. doi: 10.1126/science.150.3699.971
46. Walters ET. Nociceptive biology of molluscs and arthropods: evolutionary clues about functions and mechanisms potentially related to pain. Front Physiol. (2018) 9:1049. doi: 10.3389/fphys.2018.01049
47. Walters ET, Crook RJ, Neely GG, Price TJ, Smith ESJ. Persistent nociceptor hyperactivity as a painful evolutionary adaptation. Trends Neurosci. (2023) 46(3):211–27. doi: 10.1016/j.tins.2022.12.007
49. Cullen W, Cadell T, Elliot C. Institutions of Medicine: Part I. Physiology; for the Use of the Students in the University of Edinburgh. The third edition, corrected ed. Edinburgh: Printed for Charles Elliot.., and T. Cadell, Strand, London. printed for Charles Elliot; and T. Cadell, London (1785).
50. Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised international association for the study of pain definition of pain: concepts, challenges, and compromises. Pain. (2020) 161(9):1976–82. doi: 10.1097/j.pain.0000000000001939
51. Reneman MF, Selb M, Korwisi B, Barke A, Escorpizo RS, Tu SW, et al. Towards harmonizing the concepts and definitions of pain in the World Health Organization’s family of international classifications. Pain. (2023) 164(6):1240–4. doi: 10.1097/j.pain.0000000000002854
52. Talbot K, Madden VJ, Jones SL, Moseley GL. The sensory and affective components of pain: are they differentially modifiable dimensions or inseparable aspects of a unitary experience? A systematic review. Br J Anaesth. (2019) 123(2):e263–72. doi: 10.1016/j.bja.2019.03.033
53. Leake HB, Mardon A, Stanton TR, Harvie DS, Butler DS, Karran EL, et al. Key learning statements for persistent pain education: an iterative analysis of consumer, clinician and researcher perspectives and development of public messaging. J Pain. (2022) 23(11):1989–2001. doi: 10.1016/j.jpain.2022.07.008
54. Mardon AK, Chalmers KJ, Heathcote LC, Curtis L-A, Freedman L, Malani R, et al. “I wish I knew then what I know now”—pain science education concepts important for female persistent pelvic pain: a reflexive thematic analysis. Pain. (2024) 165(9):1990–2001. doi: 10.1097/j.pain.0000000000003205
56. Bayer TL, Baer PE, Early C. Situational and psychophysiological factors in psychologically induced pain. Pain. (1991) 44(1):45–50. doi: 10.1016/0304-3959(91)90145-N
57. Bayer TL, Coverdale JH, Chiang E, Bangs M. The role of prior pain experience and expectancy in psychologically and physically induced pain. Pain. (1998) 74(2-3):327–31. doi: 10.1016/s0304-3959(97)00196-6
58. Moseley GL, Butler DS, Beames TB, Giles TJ. The Graded Motor Imagery Handbook. Adelaide: Noigroup Publications (2012). p. 143.
59. Moseley GL. Why do people with complex regional pain syndrome take longer to recognize their affected hand? Neurology. (2004) 62(12):2182–6. doi: 10.1212/01.wnl.0000130156.05828.43
60. Moseley GL. Graded motor imagery for pathologic pain—a randomized controlled trial. Neurology. (2006) 67(12):2129–34. doi: 10.1212/01.wnl.0000249112.56935.32
61. Moseley GL. Graded motor imagery is effective for long-standing complex regional pain syndrome: a randomised controlled trial. Pain. (2004) 108(1-2):192–8. doi: 10.1016/j.pain.2004.01.006
62. Bowering KJ, Butler DS, Fulton IJ, Moseley GL. Motor imagery in people with a history of back pain, current back pain, both, or neither. Clin J Pain. (2014) 30(12):1070–5. doi: 10.1097/AJP.0000000000000066
63. Bowering KJ, O'Connell NE, Tabor A, Catley MJ, Leake HB, Moseley GL, et al. The effects of graded motor imagery and its components on chronic pain: a systematic review and meta-analysis. J Pain. (2013) 14(1):3–13. doi: 10.1016/j.jpain.2012.09.007
64. O'Connell NE, Wand BM, McAuley JH, Marston L, Moseley GL. Interventions for treating pain and disability in adults with complex regional pain syndrome-an overview of systematic reviews. Cochrane Database Syst Rev. (2013) 2013(4):CD009416. doi: 10.1002/14651858.CD009416.pub2
65. Braithwaite F, Deshpande S, Buchbinder R, Dennett L, St. Jean C, Krebs B, et al. Contemporary media campaigns for musculoskeletal pain: a systematic review and meta-analysis with social marketing benchmarking. J Pain. (2024) 28:104739. doi: 10.1016/j.jpain.2024.104739
66. Ryan CG, Karran EL, Wallwork SB, Pate JW, O'Keeffe M, Fullen BM, et al. We are all in this together-whole of community pain science education campaigns to promote better management of persistent pain. J Pain. (2024) 25(4):902–17. doi: 10.1016/j.jpain.2023.10.024
67. Braithwaite FA, Arnold J, Davis A, Gwilt I, MacIntyre E, Morris S, et al. Osteoarthritis consumers as co-researchers: identifying consumer insights to improve osteoarthritis management by co-designing translational research solutions. Osteoarthritis Cartilage. (2023) 31(7):944–53. doi: 10.1016/j.joca.2023.03.004
68. Pun J, Franklin J, Ryan CG. Healthcare professionals’ experiences of delivering pain science education to adults from ethnically minoritised groups. Musculoskelet Sci Pract. (2024) 74:103196. doi: 10.1016/j.msksp.2024.103196
69. Karran EL, Grant AR, Lee H, Kamper SJ, Williams CM, Wiles LK, et al. Do health education initiatives assist socioeconomically disadvantaged populations? A systematic review and meta-analyses. BMC Public Health. (2023) 23(1):453. doi: 10.1186/s12889-023-15329-z
70. Browne S, Schofield P, Ryan CG. The experiences of physiotherapists delivering pain science education via an interpreter: a mixed-methods online survey. Physiother Theory Pract. (2024):1–10. doi: 10.1080/09593985.2024.2396553
71. Karran EL, Cashin AG, Barker T, Boyd MA, Chiarotto A, Mohabir V, et al. Development of recommendations for a minimum dataset for Identifying Social factors that Stratify Health Opportunities and Outcomes (ISSHOOs) in pain research. MethodsX. (2024) 12:102496. doi: 10.1016/j.mex.2023.102496
72. Karran EL, Cashin AG, Barker T, Boyd MA, Chiarotto A, Dewidar O, et al. The ‘what’and ‘how’of screening for social needs in healthcare settings: a scoping review. PeerJ. (2023) 11:e15263. doi: 10.7717/peerj.15263
73. Karran EL, Cashin AG, Barker T, Boyd MA, Chiarotto A, Dewidar O, et al. Using PROGRESS-plus to identify current approaches to the collection and reporting of equity-relevant data: a scoping review. J Clin Epidemiol. (2023) 163:70–8. doi: 10.1016/j.jclinepi.2023.09.017
74. Yap ZL, Summers SJ, Grant AR, Moseley GL, Karran EL. The role of the social determinants of health in outcomes of surgery for low back pain: a systematic review and narrative synthesis. Spine J. (2022) 22(5):793–809. doi: 10.1016/j.spinee.2021.11.013
75. Karran EL, Fryer CE, Middleton JW, Moseley GL. Exploring the social determinants of health outcomes for adults with low back pain or spinal cord injury and persistent pain: a mixed methods study. J Pain. (2022) 23(9):1461–79. doi: 10.1016/j.jpain.2022.04.001
76. Karran EL, Grant AR, Moseley GL. Low back pain and the social determinants of health: a systematic review and narrative synthesis. Pain. (2020) 161(11):2476–93. doi: 10.1097/j.pain.0000000000001944
77. Leake HB, Heathcote LC, Ferencz N, Birnie KA, Davis A, Karran EL, et al. Co-design and evaluation of pain science messages on social media with adolescents with a history of chronic pain. J Pain. (2024) 25(9):104580. doi: 10.1016/j.jpain.2024.104580
78. Fitzcharles MA, Cohen SP, Clauw DJ, Littlejohn G, Usui C, Hauser W. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet. (2021) 397(10289):2098–110. doi: 10.1016/S0140-6736(21)00392-5
79. Bagg MK, Wand BM, Cashin AG, Lee H, Hübscher M, Stanton TR, et al. Effect of graded sensorimotor retraining on pain intensity in patients with chronic low back pain: a randomized clinical trial. JAMA. (2022) 328(5):430–9. doi: 10.1001/jama.2022.9930
80. Ashar YK, Gordon A, Schubiner H, Uipi C, Knight K, Anderson Z, et al. Effect of pain reprocessing therapy vs placebo and usual care for patients with chronic back pain: a randomized clinical trial. JAMA Psychiatry. (2022) 79(1):13–23. doi: 10.1001/jamapsychiatry.2021.2669
81. Kent P, Haines T, O’Sullivan P, Smith A, Campbell A, Schutze R, et al. Cognitive functional therapy with or without movement sensor biofeedback versus usual care for chronic, disabling low back pain (RESTORE): a randomised, controlled, three-arm, parallel group, phase 3, clinical trial. Lancet. (2023) 401(10391):1866–77. doi: 10.1016/S0140-6736(23)00441-5
82. Moseley GL, Butler DS, Leake HB, Wand BM, McAuley JH. Resolve Back Pain Handbook. Adelaide: NOIgroup Publications (2024).
83. Cashin AG, Lee H, Wand BM, Bagg MK, O'Hagan ET, Rizzo RRN, et al. Mechanisms of education and graded sensorimotor retraining in people with chronic low back pain: a mediation analysis. Pain. (2023) 164(12):2792–800. doi: 10.1097/j.pain.0000000000002978
84. Ashar YK, Lumley MA, Perlis RH, Liston C, Gunning FM, Wager TD. Reattribution to mind-brain processes and recovery from chronic back pain: a secondary analysis of a randomized clinical trial. JAMA Netw Open. (2023) 6(9):e2333846. doi: 10.1001/jamanetworkopen.2023.33846
85. Mardon A, Leake H, Wilson M, Karran E, Parker R, Malani R, et al. Key pain science education concepts for persistent pelvic pain: an e-Delphi study of expert clinicians. Aust N Z Cont J. (2023) 29(2):42.
86. Mardon A, Chalmers J, Heathcote L, Freedman L, Malani R, Parker R, et al. What pain science concepts are important to females with persistent pelvic pain? A reflexive thematic analysis. Aust N Z Cont J. (2023) 29(2):43.
87. Leake HB, Moseley GL, Stanton TR, O'Hagan ET, Heathcote LC. What do patients value learning about pain? A mixed-methods survey on the relevance of target concepts after pain science education. Pain. (2021) 162(10):2558–68. doi: 10.1097/j.pain.0000000000002244
88. Chi MTH, Adams J, Bogusch EB, Bruchok C, Kang S, Lancaster M, et al. Translating the ICAP theory of cognitive engagement into practice. Cogn Sci. (2018). doi: 10.1111/cogs.12626
89. Hattie JAC, Donoghue GM. Learning strategies: a synthesis and conceptual model. NPJ Sci Learn. (2016) 1:16013. doi: 10.1038/npjscilearn.2016.13
90. Bandura A. Human agency in social cognitive theory. Am Psychol. (1989) 44(9):1175–84. doi: 10.1037/0003-066X.44.9.1175
91. Ho EK, Chen L, Simic M, Ashton-James CE, Comachio J, Wang DXM, et al. Psychological interventions for chronic, non-specific low back pain: systematic review with network meta-analysis. Br Med J. (2022) 376:e067718. doi: 10.1136/bmj-2021-067718
92. Penuel WR, Allen A-R, Henson K, Campanella M, Patton R, Rademaker K, et al. Learning practical design knowledge through co-designing storyline science curriculum units. Cogn Instruct. (2022) 40(1):148–70. doi: 10.1080/07370008.2021.2010207
93. Chute H. Comics as literature? Reading graphic narrative. Publ Modern Language Assoc Am. (2008) 123(2):452–65. doi: 10.1632/pmla.2008.123.2.452
94. Cohn N. You're a good structure, charlie brown: the distribution of narrative categories in comic strips. Cogn Sci. (2014) 38(7):1317–59. doi: 10.1111/cogs.12116
95. Topkaya Y, Batdi V, Burak D, ÖZkaya A. The effectiveness of using comics in education: a meta-analytic and meta-thematic analysis study. Ahmet Keleşoğlu Eğitim Fakültesi Dergisi. (2023). doi: 10.38151/akef.2023.92
96. Pate JW. Zoe and Zak’s Pain Hacks Book Series 1–5. Adelaide, Australia: NOIgroup Publications (2023). p. 28–44.
97. Pate JW, Heathcote LC, Simons LE, Leake H, Moseley GL. Creating online animated videos to reach and engage youth: lessons learned from pain science education and a call to action. Paediatr Neonatal Pain. (2020) 2(4):131–8. doi: 10.1002/pne2.12015
98. Moseley GL, Butler DS, Stanton TR. The Knee Osteoarthritis Handbook. Adelaide: Noigroup Publications (2023).
99. Braithwaite FA. Working with Osteoarthritis Consumers as Co-Researchers—Co-Designing Translational Research Solutions and Busting Osteoarthritis Myths. San Diego Pain Summit; 1–3 March 2024. San Diego, CA: San Diego Pain Summit (2024).
100. Oktaviana AA, Joannes-Boyau R, Hakim B, Burhan B, Sardi R, Adhityatama S, et al. Narrative cave art in Indonesia by 51,200 years ago. Nature. (2024) 631(8022):814–8. doi: 10.1038/s41586-024-07541-7
101. Bower GH, Clark MC. Narrative stories as mediators for serial learning. Psychon Sci. (1969) 14(4):181–2. doi: 10.3758/BF03332778
102. Perrier MJ, Martin Ginis KA. Changing health-promoting behaviours through narrative interventions: a systematic review. J Health Psychol. (2018) 23(11):1499–517. doi: 10.1177/1359105316656243
103. Davidson MR. A phenomenological evaluation: using storytelling as a primary teaching method. Nurse Educ Pract. (2004) 4(3):184–9. doi: 10.1016/S1471-5953(03)00043-X
104. Shaw AC, McQuade JL, Reilley MJ, Nixon B, Baile WF, Epner DE. Integrating storytelling into a communication skills teaching program for medical oncology fellows. J Cancer Educ. (2019) 34(6):1198–203. doi: 10.1007/s13187-018-1428-3
105. Chilman-Blair K, DeLoache S. Medikidz Explain Chronic Pain: What’s Up with Moira’s Grandad. London: Medikidz Publishing (2012). p. 32.
106. Moseley GL. Painful Yarns: Metaphors & Stories to Help Understand the Biology of Pain. Oxford: Dancing Giraffe Press (2007).
107. Gallagher L, McAuley J, Moseley GL. A randomized-controlled trial of using a book of metaphors to reconceptualize pain and decrease catastrophizing in people with chronic pain. Clin J Pain. (2013) 29(1):20–5. doi: 10.1097/AJP.0b013e3182465cf7
108. Yu Z, Xu W. A meta-analysis and systematic review of the effect of virtual reality technology on users’ learning outcomes. Comput Appl Eng Educ. (2022) 30(5):1470–84. doi: 10.1002/cae.22532
109. Jimenez YA, Cumming S, Wang W, Stuart K, Thwaites DI, Lewis SJ. Patient education using virtual reality increases knowledge and positive experience for breast cancer patients undergoing radiation therapy. Support Care Cancer. (2018) 26(8):2879–88. doi: 10.1007/s00520-018-4114-4
110. van der Linde-van den Bor M, Frans-Rensen SA, Slond F, Liesdek OCD, de Heer LM, Suyker WJL, et al. Patients’ voices in the development of pre-surgical patient education using virtual reality: a qualitative study. PEC Innov. (2022) 1:100015. doi: 10.1016/j.pecinn.2021.100015
111. Goudman L, Jansen J, Billot M, Vets N, De Smedt A, Roulaud M, et al. Virtual reality applications in chronic pain management: systematic review and meta-analysis. JMIR Serious Games. (2022) 10(2):e34402. doi: 10.2196/34402
112. Brown L, DiCenso-Fleming T, Ensign T, Boyd AJ, Monaghan G, Binder DS. Chronic pain education delivered with a virtual reality headset in outpatient physical therapy clinics: a multi-site exploratory trial. Am J Transl Res. (2023) 15(5):3500–10.37303618
113. McConnell R, Lane E, Webb G, LaPeze D, Grillo H, Fritz J. A multicenter feasibility randomized controlled trial using a virtual reality application of pain neuroscience education for adults with chronic low back pain. Ann Med. (2024) 56(1):2311846. doi: 10.1080/07853890.2024.2311846
114. Skidmore N, Ryan CG, Mankelow J, Martin D. Acceptability and feasibility of virtual reality to promote health literacy in primary care from the health professional’s view: a qualitative study. Patient Educ Couns. (2024) 123:108179. doi: 10.1016/j.pec.2024.108179
115. Mardon AK, Wilson D, Leake HB, Harvie D, Andrade A, Chalmers KJ, et al. The acceptability, feasibility, and usability of a virtual reality pain education and rehabilitation program for Veterans: a mixed-methods study. Front Pain Res. (2025) 6:1535915. doi: 10.3389/fpain.2025.1535915
116. Kennedy H, Doherty D, Boyd M, Thong I, Harris N, Weeks P, et al., editors Acceptability of using an immersive Virtual Reality platform for Pain Education: perspectives of patients in a randomised clinical trial. 45 Annual Scientific Meeting of the Australian Pain Society; Melbourne, Australia (2025).
Keywords: chronic pain, back pain, pain education, constructivism, explain pain, virtual reality
Citation: Moseley GL, Mardon A, Watson J, Braithwaite F, Wilson MV, Barker T, Lawrence J, Sheppard D, Reneman MF, Stinson J and Ryan CG (2025) From didactic explanations to co-design, sequential art and embodied learning: challenges, criticisms and future directions of patient pain education. Front. Pain Res. 6:1536112. doi: 10.3389/fpain.2025.1536112
Received: 28 November 2024; Accepted: 31 March 2025;
Published: 9 May 2025;
Corrected: 5 June 2025.
Edited by:
Shirin Modarresi, McMaster University, CanadaReviewed by:
Ordoñez-Mora L. T., University of Santiago de Cali, ColombiaJustine Dee, Thomas Jefferson University, United States
Copyright: © 2025 Moseley, Mardon, Watson, Braithwaite, Wilson, Barker, Lawrence, Sheppard, Reneman, Stinson and Ryan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: G. Lorimer Moseley, TG9yaW1lci5tb3NlbGV5QGdtYWlsLmNvbQ==
 G. Lorimer Moseley
G. Lorimer Moseley Amelia Mardon
Amelia Mardon James Watson
James Watson Felicity Braithwaite1,2,6
Felicity Braithwaite1,2,6 Monique V. Wilson
Monique V. Wilson Dianne Sheppard
Dianne Sheppard Michiel F. Reneman
Michiel F. Reneman Jennifer Stinson
Jennifer Stinson Cormac G. Ryan
Cormac G. Ryan