- 1School of Computing and Augmented Intelligence, Arizona State University, Tempe AZ, United States
- 2ASU-Mayo Center for Innovative Imaging, Tempe, AZ, United States
- 3Department of Neurology, Mayo Clinic, Phoenix, AZ, United States
Background: While prior studies suggest an increased risk of stroke among individuals with migraine, particularly those with migraine with aura, data on how specific migraine characteristics and comorbidities influence this risk across diverse populations remain limited. The All of Us database provides a unique opportunity to address this gap given its large sample size and inclusion of historically underrepresented groups.
Methods: A cross-sectional case-control analysis using multivariable regression models accounting for vascular risk factors and comorbidities was performed to compare the risk of stroke between individuals with and without migraine, odds ratios (OR) using a 95% confidence interval (CI) were calculated.
Results: Within the All of Us database, 31,444 individuals received a migraine diagnosis [female = 25,374/81%, male = 5,391/17%, other = 679/2%; mean (std) age = 54.9 (15.6)] and 379,283 did not have a migraine diagnosis [female = 222,104/59%, male = 149,182/39%, other = 7,997/2%; mean (SD) age = 55.9 (17.2)]. The migraine group had a greater proportion of women (81% vs. 59%), a higher proportion of white individuals (61% vs. 55%) and fewer African American individuals (15% vs. 19%). Compared to the non-migraine group, individuals with migraine had higher rates of comorbidities, including depression (46% vs. 12%), diabetes (16% vs. 7%), tobacco use (36% vs. 15%), hyperlipidemia (52% vs. 24%), hypertension (54% vs. 26%), and atrial fibrillation (3% vs. 2%).
A multivariable regression model adjusted for differences between group demographics and comorbidities found that compared to those without migraine, individuals with migraine had a higher risk of overall stroke [OR 1.97, 95% CI (1.88, 2.07)], ischemic stroke [OR 1.38, 95% CI (1.24, 1.53)] and hemorrhagic stroke [OR 1.75, 95% CI (1.60, 1.92)]. Individuals with chronic migraine had a higher risk of overall stroke compared to the non-migraine group [OR 2.56, 95% CI ( 2.32, 2.84)] and compared to episodic migraine [OR 1.90, 95% CI (1.81, 2.00)]. Those with migraine with aura had a higher risk of stroke compared to individuals with migraine without aura [OR 1.33, 95% CI (1.20, 1.48)].
Conclusions: Individuals with migraine, particularly those with chronic migraine had a higher risk of stroke compared to those without migraine and compared to individuals with episodic migraine. The risk of stroke was higher in those with migraine with aura compared to those with migraine without aura even after adjusting for vascular comorbidities. Our analysis, using data from the All of Us database, confirms previous findings and suggests that while vascular comorbidities are more prevalent in those with migraine, they do not fully account for the increased risk of stroke.
Introduction
Prior studies, reviews and meta-analyses (1–4) suggest that migraine, in particular migraine with aura, is associated with an increased risk of stroke, including both ischemic and hemorrhagic subtypes (5–11). However, data on migraine characteristics, such as headache frequency (chronic migraine, episodic migraine) and the presence of aura, that might contribute to the risk of stroke are sparse. Additionally, much of the existing literature has focused on relatively homogenous populations, limiting the generalizability of findings to individuals from diverse racial, ethnic and socioeconomic backgrounds.
In this study, we interrogate electronic health record data from the All of Us research program which includes over 400,000 participants with approximately 80% of those originating from underrepresented populations. As such, it is one of the most diverse health databases in history and includes participants from demographic groups that are typically underrepresented in human health research (12). We aim to assess the risk of stroke in individuals with migraine compared to non-migraine individuals using the diverse data available from the All of Us database and to assess whether migraine-specific characteristics including aura and headache frequency influences the risk of stroke in those with migraine. Furthermore, we adjusted for multiple vascular comorbidities including hypertension, diabetes, atrial fibrillation, hyperlipidemia, tobacco use, and depression, to better isolate the contribution of migraine characteristics themselves. The goal of this study is to assess the association between migraine and stroke risk, in particular ischemic and hemorrhagic subtypes and to assess whether migraine-specific characteristics such as aura and headache frequency are independently associated with stroke risk after adjusting for known vascular comorbidities. Using the rich demographic and clinical data within the All of Us database, we aim to validate previously reported associations between migraine and stroke risk, and to determine whether these relationships persist using a more diverse and representative dataset.
Methods
Description of All of Us
The All of Us research program, was launched in 2018 (13, 14) and continues enrollment as of February 2025. The objective of this program is to develop a large and diverse health data repository that reflects the broad range of health outcomes across different populations. By capturing data from historically underrepresented groups, the All of Us program aims to improve personalized treatment and address disparities in healthcare. The database includes a wide range of data types, including electronic health record (EHR), genomic information, lifestyle data, and patient-reported outcomes. This cross-sectional case-control study was submitted for Institutional Review Board (IRB) review at Mayo Clinic and was determined to be exempt from full review. IRB approval is not required for studies using the All of Us Researcher Workbench, as it operates under a data passport model that allows authorized users to conduct research without requiring separate IRB review for each project.
Study population
This study included EHR data from the All of Us Research Program. The All of Us Controlled Tier database v7 was queried on 7/12/24, which served as the study search, or baseline date.
Migraine and stroke diagnosis, comorbid conditions and cardiovascular risk factors were based on ICD9 and ICD10 diagnosis codes, as shown in Table 1. People with migraine who had more than one diagnosis code for migraine were classified as follows: (1) if an individual had a diagnosis of migraine with aura at any time prior to the search date, they were classified as having migraine with aura; (2) if an individual had a diagnosis of chronic migraine at any time prior to the search date, they were classified as having chronic migraine; (3) individuals were classified as episodic migraine if they never had a diagnosis of chronic migraine. Based on these criteria, individuals were classified as either having episodic migraine with or without aura, or as having chronic migraine with or without aura.
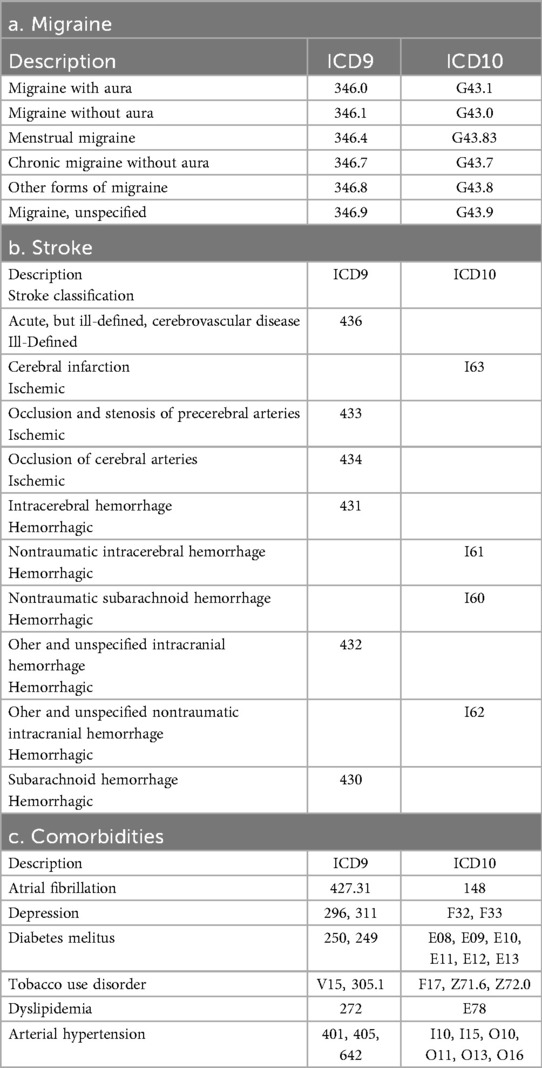
Table 1. ICD9 and ICD10 diagnosis codes for (a) migraine, (b) stroke and (c) selected comorbidities.
Data sources and statistical analyses
Data for this study was accessed and analyzed within the secure All of Us Researcher Workbench, a cloud-based platform provided by the All of Us Research Program. All analyses were performed in the integrated Jupyter Notebook environment, which facilitates interactive data exploration and code execution. Python (3.10.12) was employed as the primary programming language, given its extensive library ecosystem for data analysis and machine learning. Specifically, pandas (2.0.3) was used for data cleaning and preprocessing, NumPy (1.26.4) for numerical computations, and SciPy (1.11.2) for performing statistical analyses. The study involved case-control identification, data filtering, and exploratory data analysis, focusing on migraine and stroke-related variables. The final dataset contained complete data for demographic variables and diagnosis codes, with no missing values.
Continuous data distributions were assessed using both visual inspection and formal statistical testing. Age distributions for migraine and non-migraine groups exhibited deviations from normality (Shapiro–Wilk, p < 0.05), due to the large sample size. Nonetheless, among the candidate distributions tested (normal, exponential, gamma, and log-normal), the normal distribution offered the best overall fit and was therefore used for subsequent analyses. The percentages of individuals with and without migraine were compared using Chi-square test or independent t-test, as appropriate.
To evaluate the association between migraine and stroke risk, unadjusted and adjusted odds ratios (OR) were calculated using multivariable logistic regression which provides robustness in modeling binary outcomes and effectively captures the log odds of events. This method is particularly well-suited for scenarios where the outcome of interest, such as stroke, is rare. In such cases, ORs closely approximate risk ratios (RRs), offering a practical and interpretable measure of association. Additionally, logistic regression allows for comprehensive adjustment of multiple confounding variables.
This approach enabled the assessment of stroke risk attributable to migraine both before and after adjusting for established stroke risk factors, including age, sex at birth, hypertension, atrial fibrillation, diabetes mellitus, tobacco use, depression, and hyperlipidemia. Logistic regression models were checked for multicollinearity using Variance Inflation Factors (VIF), with all predictor variables showing VIF values below 10, indicating no multicollinearity concerns. Additionally, independence of residuals was assessed using the Durbin-Watson statistic, which was approximately 2 across all models, confirming the absence of autocorrelation. Model fit and predictive performance were evaluated using receiver operating characteristic (ROC) curves, with area under the curve (AUC) values ranging from moderate to very high (approximately 0.76–0.91), demonstrating good to very high discriminative ability (see Supplementary Material, Logistic Regression). To assess the robustness of our findings to potential misclassification of EHR data, we conducted a series of sensitivity analyses. We simulated varying degrees of exposure and outcome misclassification, including 10% underdiagnosis of migraine, 5% false positives among controls, and 5% random misclassification of both migraine and stroke diagnoses. We also modeled 5% stroke underdiagnosis and conducted a joint probabilistic bias analysis (PBA), applying 10,000 simulations based on plausible Beta-distributed values for sensitivity and specificity of both exposure and outcome. Across all scenarios in our sensitivity analyses, the association between migraine and stroke remained statistically significant. Notably, the PBA yielded an adjusted odds ratio of 2.51 (95% CI: 2.27–2.85), suggesting that diagnostic error may lead to underestimation of the true association. These findings support the robustness of our results under plausible real-world biases (see Supplementary Material, Sensitivity Analyses).
Results
Out of a total of 410,727 people in the All of Us database, we identified 31,444 individuals (7.7%) with a diagnosis of migraine (migraine group). 379,283 individuals (92.3%) did not have a migraine diagnosis (non-migraine group). The migraine group had significantly greater female (81% vs. 59%) and the same amount of non-Hispanic participants (78%) (Table 2). In the migraine group, 61.5% were White, 21.9% Other, 14.6% Black or African, 1.4% Asian, 0.4% Middle Eastern or North African, and 0.1% Native Hawaiian or Pacific Islander. In the non-migraine group, 54.9% were White, 21.4% Other, 19.4% Black or African, 3.6% Asian, 0.6% Middle Eastern or North African, and 0.1% Native Hawaiian or Pacific Islander.
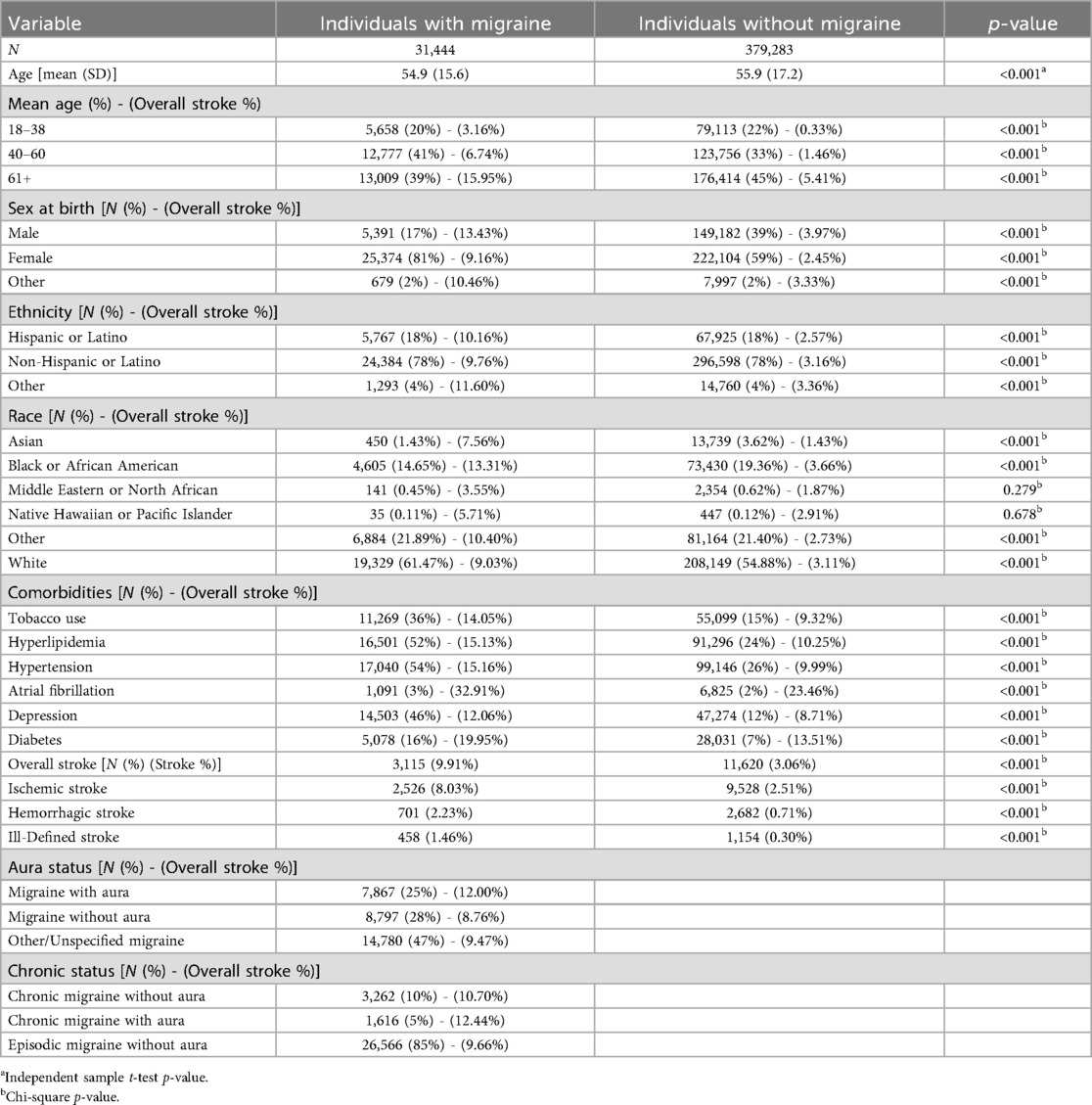
Table 2. Baseline characteristics and comorbidities of individuals with and without migraine from All of Us database, queried on 7/12/2024. P-values indicate differences in the population proportions.
Individuals with migraine compared to the non-migraine group had a significantly higher percentage of comorbidities including tobacco use (36% vs. 15%; p < 0.001), hyperlipidemia (52% vs. 24%; p < 0.001), hypertension (54% vs. 26%; p < 0.001) atrial fibrillation (3% vs. 2%; p < 0.001), depression (46% vs. 12%; p < 0.001) and diabetes (16% vs. 7%; p < 0.001). Individuals with migraine compared to the non-migraine group had a significantly higher percentage of stroke, including overall stroke type (3,115/31,444; 9.91% vs. 11,620/379,283; 3.06%; p < 0.001), ischemic stroke (2,526/31,444; 8.03% vs. 9,528/379,283; 2.51%; p < 0.001), hemorrhagic stroke (701/31,444; 2.23% vs. 2,682/ 379,283; 0.71%; p < 0.001) and ill-defined stroke (458/31,444; 1.46% vs. 1,154/379,283; 0.30%; p < 0.001).
Without adjusting for comorbidities (Table 3a), individuals with migraine had a 3.48 higher risk of stroke [OR 3.48, 95% CI (3.34; 3.63)] compared to individuals without migraine; when stratified by stroke type, risk of ischemic stroke was 3.39 higher [OR 3.39, 95%Cl (3.24, 3.55)], hemorrhagic stroke was 3.20 higher [OR 3.20, 95%Cl (2.94, 3.48)], and ill-defined stroke was 4.84 higher [OR 4.84, 95%Cl (4.34, 5.40)]. When stratified by migraine type, individuals with chronic migraine had a 4.02 higher risk of stroke [OR 4.02, 95%CI (3.67, 4.40)] when compared to non-migraine individuals, and individuals with migraine with aura had a 1.42 higher risk of stroke compared to individuals with migraine without aura [OR 1.42, 95% Cl (1.28, 1.57)].
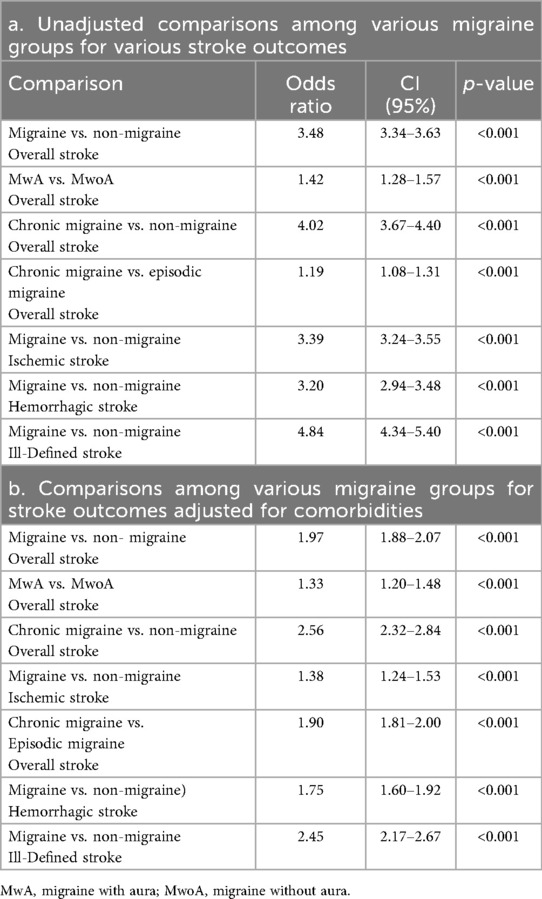
Table 3. (a) Exploratory unadjusted logistic regression analysis of migraine (and migraine type) vs. non-migraine association with stroke occurrence among participants in the All of Us database. (b) The association between migraine and stroke among participants in the All of Us database adjusted for comorbidities (hypertension, atrial fibrillation, hyperlipidemia, diabetes, tobacco use, depression and demographics (age, sex at birth).
After adjusting for comorbidities (Table 3Bb), individuals with migraine had a 1.97 higher risk of stroke [OR 1.97, 95% Cl (1.88, 2.07)] compared to individuals without migraine. Individuals with chronic migraine had a 2.56 higher risk of stroke compared to those without migraine [OR 2.65, 95% Cl (2.32, 2.84)] and a 1.90 higher risk of stroke compared to individuals with episodic migraine [OR 1.90, 95%Cl (1.81, 2.00)]. Individuals with migraine with aura had a 1.33 higher risk of stroke compared to individuals with migraine without aura [OR 1.33, 95% Cl (1.20, 1.48)]. When stratified by stroke type, individuals with migraine where at higher risk for ischemic stroke [OR 1.38, 95% CI (1.24, 1.53)], hemorrhagic stroke [OR 1.75, 95%CI (1.60, 1.92)], and ill-defined stroke [OR 2.45, 95% CI (2.17, 2.67)], compared to individuals without migraine.
Discussion
This was a retrospective case-control analysis using EHR data from the All of Us database from the controlled tier v7. We found that individuals with a migraine diagnosis compared to individuals without a migraine diagnosis had a higher risk of overall stroke, ischemic and hemorrhagic stroke. The stroke risk remained significantly higher even after adjusting for age, sex, and common comorbidities, such as depression, diabetes, atrial fibrillation, tobacco use, hyperlipidemia, and hypertension.
Interestingly, people with chronic migraine had the highest risk of stroke compared to both the non-migraine and the episodic migraine group, before and after adjusting for comorbidities. Similarly, after adjustment for co-morbidities, migraine with aura had a higher risk of stroke compared to migraine without aura.
Our findings are consistent with a number of large case-control and cohort studies (5, 15–20) and several meta-analyses as well as a recent review about migraine-associated pathophysiology and the impact on stroke risk (1, 4, 21, 22) demonstrating an elevated risk of stroke (ischemic and hemorrhagic) in individuals with migraine, particularly among those with migraine with aura (5, 11, 18, 23–27). For example, Kurth et al. (15, 16, 28), using prospective cohort data from the Nurses' Health Study II, reported an increased risk of stroke in women with migraine (28). Furthermore, using data from the Women's Health study, Kurth et al. (16) reported an increased risk of total and ischemic stroke in women with migraine with aura compared to women without migraine history, and a higher risk of hemorrhagic stroke in women with active migraine with aura (but not migraine without aura) compared to women without history of migraine (28). Androulakis et al. (11, 24) demonstrated that late-middle-aged individuals with migraine with visual aura had an increased risk of ischemic stroke compared to those with migraine without aura or non-migraine individuals, using data from the Atherosclerosis Risk in Communities (ARIC) study. Additionally, their results suggested that aura onset in older age (>50) but not in younger age (<50) associated with stroke risk. This association could reflect age-related differences in pathophysiological mechanisms, including cortical spreading depression or stroke-related processes that are not dependent on atherosclerosis or to diagnostic challenges such as potentially misclassifying ischemic stroke symptoms as aura in older individuals (24, 29). It is of note that some prospective studies have shown no association, or even an inverse association, between migraine, stroke, and vascular risk factors, such as atrial fibrillation (30) and one brain imaging study did not find differences in pathophysiology based on functional imaging findings of migraine attacks with and without aura (31). These discrepancies emphasize the need for more nuanced exploration of how migraine interacts with vascular risk profiles.
Using the US Nationwide Inpatient Sample (NIS) hospitalizations database, Patel et al. (20) reported a higher risk of ischemic and hemorrhagic stroke in individuals with migraine compared to those without migraine.
Similarly, Kuo et al. (19), in a large population-based cohort study using Taiwan's National Health Insurance claims database, reported an almost twofold higher risk of hemorrhagic stroke in individuals with migraine compared to non-migraine individuals, aligning with our results.
Lee et al. (32), utilizing the same database as Kuo et al., found an increased risk of ischemic stroke in individuals with migraine (with and without aura) compared to non-migraine group, however, in contrast to our findings, no significant association with hemorrhagic stroke was observed. Similarly, Gaist et al. (33) using data from the UK Health Improvement Network (THIN) database did not find a higher risk of hemorrhagic stroke in people with migraine. Monteith and colleagues (34), using data from the Northern Manhattan Study, found no overall association between migraine and stroke risk. However, they observed an increased risk of stroke in older people with migraine who were smokers, whereas no such association was found in non-smokers.
We found that individuals with a chronic migraine diagnosis where at a higher risk of stroke compared to those with episodic migraine (OR 1.90) and compared to individuals without a migraine (OR 2.56) diagnosis. These results suggest that headache frequency significantly increases the risk of stroke in those with migraine. Similar to our findings, Kurth et al. (35) reported an association between high migraine attack frequency and ischemic stroke in women, and MacClellan et al. (36) reported that women with probable migraine with aura that experienced over 12 attacks per year had an increased risk of stroke compared to women without migraine. Our findings suggest that aura and chronic migraine are independent risk factors that significantly increase the risk of stroke in individuals with migraine. These results highlight the importance of screening individuals with migraine for aura and other stroke risk factors, which may help mitigate the risk of stroke in these at-risk individuals. Although the association between chronic migraine and stroke is compelling, future studies will need to further clarity the interaction between headache chronicity and potentially modifiable risk-factors associated with stroke risk (37).
Our study has several limitations. We recognize that migraine, stroke, and migraine-related comorbidities can be derived from clinician notes, problem lists, diagnostic test results, or billing codes, yet, due to the concern that using multiple sources as outcome measures can introduce additional noise and potential bias to the data (38), we elected to focus on ICD9 and ICD10 diagnosis codes only for identification of these diagnoses. However, reliance on diagnostic codes from medical records may introduce measurement bias due to potential inaccuracies of migraine diagnoses. In the All of Us data repository, only 7.7% of individuals had a migraine diagnosis, which is lower than the one-year prevalence of 12% in the general population (39), suggesting that migraine is underdiagnosed in the All of Us database. Although the results indicate a significantly higher risk of ill-defined stroke in people with migraine, these findings should be interpreted with caution due to the small sample size of individuals with migraine with ill-defined stroke (n = 458, 1.46%). While our findings generally align with previous studies, some differences were observed. These discrepancies may be attributed to variations in how migraine and stroke were identified across studies (e.g., diagnosis codes vs. patient questionnaires). Additionally, differences in study groups, including variations in age, sex, sample size, and socio-demographic characteristics, and adjustments for confounders may also contribute to the observed differences.
Conclusion
The results derived from the diverse and inclusive All of Us data repository suggest that the increased risk of stroke in individuals with migraine is only partially explained by shared comorbid conditions and suggests that migraine itself is an independent risk factor for both ischemic and hemorrhagic stroke. The increased risk of stroke amongst those who have migraine with aura and those with chronic migraine warrant further research into migraine related features (migraine with vs. without aura, headache frequency, years lived with migraine) and the underlying pathophysiological mechanisms that could contribute to this increased risk of stroke. The inclusion of individuals that are typically underrepresented in biomedical research, as captured in the All of Us database, contributes to the diversity of our study population and strengthens the generalizability of our results.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: All of Us - publicly available data source.
Ethics statement
Ethical approval was not required for the studies involving humans because query of public database "All of Us". The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NS: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. CC: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing, Project administration, Resources, Validation. OD: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing. TS: Conceptualization, Investigation, Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Funding acquisition, Methodology, Software, Supervision, Visualization. ZC: . TW: Investigation, Writing – original draft, Writing – review & editing, Conceptualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. American Heart Association, 23MRFSCD1077177.
Conflict of interest
CC receives research support from the American Heart Association, the National Institutes of Health and the Department of Defense. TS, within the prior 24 months, has received consulting fees from AbbVie, Amgen, Eli Lilly, Linpharma, Lundbeck, Salvia BioElectronics, Scilex, and Theranica and royalties from UpToDate. He holds/held stock options in Aural Analytics and Nocira. He has received research funding from the American Heart Association, Henry Jackson Foundation, National Headache Foundation, National Institutes of Health, Patient Centered Outcomes Research Institute, Pfizer, Spark Neuro, and United States Department of Defense. OD receives research support from the Arizona Department of Health Services. ZC is partly supported by the National Science Foundation.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpain.2025.1646142/full#supplementary-material
References
1. Mahmoud AN, Mentias A, Elgendy AY, Qazi A, Barakat AF, Saad M, et al. Migraine and the risk of cardiovascular and cerebrovascular events: a meta-analysis of 16 cohort studies including 1 152 407 subjects. BMJ Open. (2018) 8(3):e020498. doi: 10.1136/bmjopen-2017-020498
2. Ng CYH, Tan BYQ, Teo YN, Teo YH, Syn NLX, Leow AST, et al. Myocardial infarction, stroke and cardiovascular mortality among migraine patients: a systematic review and meta-analysis. J Neurol. (2022) 269(5):2346–58. doi: 10.1007/s00415-021-10930-x
3. Hu X, Zhou Y, Zhao H, Peng C. Migraine and the risk of stroke: an updated meta-analysis of prospective cohort studies. Neurol Sci. (2017) 38:33–40. doi: 10.1007/s10072-016-2746-z
4. Ravi V, Osouli Meinagh S, Bavarsad Shahripour R. Reviewing migraine-associated pathophysiology and its impact on elevated stroke risk. Front Neurol. (2024) 15:1435208. doi: 10.3389/fneur.2024.1435208
5. Adelborg K, Szépligeti SK, Holland-Bill L, Ehrenstein V, Horváth-Puhó E, Henderson VW, et al. Migraine and risk of cardiovascular diseases: Danish population based matched cohort study. Br Med J. (2018) 360(k96):1-9. doi: 10.1136/bmj.k96
6. Øie LR, Kurth T, Gulati S, Dodick DW. Migraine and risk of stroke. J Neurol Neurosurg Psychiatry. (2020) 91:593–604. doi: 10.1136/jnnp-2018-318254
7. Kim C, Schreiner PJ, Yin Z, Whitney R, Sidney S, Ebong I, et al. Migraines, vasomotor symptoms, and cardiovascular disease in the coronary artery risk development in young adults study. Menopause. (2024) 31(3):202–8. doi: 10.1097/GME.0000000000002311
8. Hvitfeldt Fuglsang C, Pedersen L, Schmidt M, Vandenbroucke JP, Bøtker HE, Toft Sørensen H. Combined impact of migraine and pregnancy-induced hypertension on long-term risk of premature myocardial infarction and stroke. Neurology. (2024) 102:e207813. doi: 10.1212/WNL.0000000000207813
9. Rajendran A, Minhas AS, Kazzi B, Varma B, Choi E, Thakkar A, et al. Sex-specific differences in cardiovascular risk factors and implications for cardiovascular disease prevention in women. Atherosclerosis. (2023) 384:117269. doi: 10.1016/j.atherosclerosis.2023.117269
10. Tietjen GE, Maly EF. Migraine and ischemic stroke in women. A narrative review. Headache. (2020) 60(5):843–63. doi: 10.1111/head.13796
11. Androulakis XM, Kodumuri N, Giamberardino LD, Rosamond WD, Gottesman RF, Yim E, et al. Ischemic stroke subtypes and migraine with visual aura in the ARIC study. Neurology. (2016) 87(24):2527–32. doi: 10.1212/WNL.0000000000003428
12. Ramirez AH, Sulieman L, Schlueter DJ, Halvorson A, Qian J, Ratsimbazafy F, et al. The all of US research program: data quality, utility, and diversity. Patterns (N Y. (2022) 3(8):100570. doi: 10.1016/j.patter.2022.100570
13. All of Us Research Program Investigators; Denny JC, Rutter JL, Goldstein DB, Philippakis A, Smoller JW, et al. The “All of US” research program. N Engl J Med. (2019) 381(7):668–76. doi: 10.1056/NEJMsr1809937
14. Collins FS, Varmus H. A new initiative on precision medicine. N Engl J Med. (2015) 372:793–5. doi: 10.1056/NEJMp1500523
15. Kurth T, Winter AC, Eliassen AH, Dushkes R, Mukamal KJ, Rimm EB, et al. Migraine and risk of cardiovascular disease in women: prospective cohort study. Br Med J. (2016) 353(i2610):1-6. doi: 10.1136/bmj.i2610
16. Kurth T, Slomke MA, Kase CS, Cook NR, Lee IM, Gaziano JM, et al. Migraine, headache, and the risk of stroke in women: a prospective study. Neurology. (2005) 64(6):1020–6. doi: 10.1212/01.WNL.0000154528.21485.3A15781820
17. Bigal ME, Kurth T, Santanello N, Buse D, Golden W, Robbins M, et al. Migraine and cardiovascular disease: a population-based study. Neurology. (2010) 74(8):628–35. doi: 10.1212/WNL.0b013e3181d0cc8b
18. Champaloux SW, Tepper NK, Monsour M, Curtis KM, Whiteman MK, Marchbanks PA, et al. Use of combined hormonal contraceptives among women with migraines and risk of ischemic stroke. Am J Obstet Gynecol. (2017) 216(5):489.e1–7. doi: 10.1016/j.ajog.2016.12.019
19. Kuo CY, Yen MF, Chen LS, Fann CY, Chiu YH, Chen HH, et al. Increased risk of hemorrhagic stroke in patients with migraine: a population-based cohort study. PLoS One. (2013) 8(1):e55253. doi: 10.1371/journal.pone.0055253
20. Patel UK, Shah D, Malik P, Hussain M, Chauhan B, Patel D, et al. A comprehensive assessment of vascular and nonvascular risk factors associated with migraine. Cureus. (2019) 11(11):e6189. doi: 10.7759/cureus.6189
21. Zhang S, Liu H, Shi T. Association between migraine and risk of stroke: a systematic review and meta-analysis. Neurol Sci. (2022) 43:4875–89. doi: 10.1007/s10072-022-06074-z
22. Hu X, Zhou Y, Zhao H, Peng C. Migraine and the risk of stroke: an updated meta-analysis of prospective cohort studies. Neurol Sci. (2017) 38:33–40. doi: 10.1007/s10072-016-2746-z
23. Abanoz Y, Gülen Abanoz Y, Gündüz A, Uludüz D, İnce B, Yavuz B. Migraine as a risk factor for young patients with ischemic stroke: a case-control study. Neurol Sci. (2017) 38(4):611–7. doi: 10.1007/s10072-017-2810-3
24. Androulakis XM, Sen S, Kodumuri N, Zhang T, Grego J, Rosamond W, et al. Migraine age of onset and association with ischemic stroke in late life: 20 years follow-up in ARIC. Headache. (2019) 59(4):556–66. doi: 10.1111/head.13468
25. Banerjee I, Bozkurt S, Caswell-Jin JL, Kurian AW, Rubin DL. Natural language processing approaches to detect the timeline of metastatic recurrence of breast cancer. JCO Clin Cancer Inform. (2019) 3:1–12. doi: 10.1200/CCI.19.00034
26. Kuybu O, Amireh A, Davis D, Kelley RE, Javalkar V. Prevalence of ischemic stroke and atrial fibrillation in young patients with migraine national inpatient sample analysis. J Stroke Cerebrovasc Dis. (2020) 29:104972. doi: 10.1016/j.jstrokecerebrovasdis.2020.104972
27. Scutelnic A, Mattle HP, Branca M, Jung S, Reichlin T, Fischer U, et al. Migraine and atrial fibrillation: a systematic review. Eur J Neurol. (2022) 29(3):910–20. doi: 10.1111/ene.15198
28. Kurth T, Kase CS, Schürks M, Tzourio C, Buring JE. Migraine and risk of haemorrhagic stroke in women: prospective cohort study. Br Med J. (2010) 341:c3659. doi: 10.1136/bmj.c3659
29. Scutelnic A, Auf der Maur SM, Branca M, Beyeler M, Horvath T, Bücke P, et al. Field-testing the explicit diagnostic criteria for transient ischemic attack: a diagnostic accuracy study. J Neurol. (2024) 272(1):79. doi: 10.1007/s00415-024-12733-2
30. Giri S, Tronvik E, Dalen H, Ellekjær H, Loennechen JP, Olsen A, et al. Migraine and risk of atrial fibrillation: a 9-year follow-up based on the Trøndelag health study. Cephalalgia. (2024) 44(5):3331024241254517. doi: 10.1177/03331024241254517
31. Mehnert J, Fischer-Schulte L, May A. Aura phenomena do not initiate migraine attacks-findings from neuroimaging. Headache. (2023) 63:1040–4. doi: 10.1111/head.14597
32. Lee SY, Lim JS, Oh DJ, Kong IG, Choi HG. Risk of ischaemic stroke in patients with migraine: a longitudinal follow-up study using a national sample cohort in South Korea. BMJ Open. (2019) 9:e027701. doi: 10.1136/bmjopen-2018-027701
33. Gaist D, González-Pérez A, Ashina M, Rodríguez LA. Migraine and risk of hemorrhagic stroke: a study based on data from general practice. J Headache Pain. (2014) 15:74. doi: 10.1186/1129-2377-15-74
34. Monteith TS, Gardener H, Rundek T, Elkind MS, Sacco RL. Migraine and risk of stroke in older adults: northern manhattan study. Neurology. (2015) 85:715–21. doi: 10.1212/WNL.0000000000001854
35. Kurth T, Schürks M, Logroscino G, Buring JE. Migraine frequency and risk of cardiovascular disease in women. Neurology. (2009) 73:581–8. doi: 10.1212/WNL.0b013e3181ab2c20
36. MacClellan LR, Giles W, Cole J, Wozniak M, Stern B, Mitchell BD, et al. Probable migraine with visual aura and risk of ischemic stroke: the stroke prevention in young women study. Stroke. (2007) 38(9):2438–45. doi: 10.1161/STROKEAHA.107.488395
37. O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in: 32, countries (INTERSTROKE): a case-control study. Lancet. (2016) 388(10046):761–75. doi: 10.1016/S0140-6736(16)30506-2
38. Richesson RL, Rusincovitch SA, Wixted D, Batch BC, Feinglos MN, Miranda ML, et al. A comparison of phenotype definitions for diabetes mellitus. J Am Med Inform Assoc. (2013) 20(e2):e319–26. doi: 10.1136/amiajnl-2013-001952
39. GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. (2018) 17(11):954–76. doi: 10.1016/S1474-4422(18)30322-3. Erratum in: Lancet Neurol. 2021 Dec; 20(12):e7. doi: 10.1016/S1474-4422(21)00380-X.30353868
Keywords: migraine with aura, migraine without aura, stroke, chronic migraine, risk of stroke
Citation: Seah N, Chong CD, Dumitrascu OM, Schwedt TJ, Cao Z and Wu T (2025) Migraine is associated with a higher risk of ischemic and hemorrhagic stroke: an analysis of the All of Us database. Front. Pain Res. 6:1646142. doi: 10.3389/fpain.2025.1646142
Received: 12 June 2025; Accepted: 3 September 2025;
Published: 1 October 2025.
Edited by:
James Russell Couch, University of Oklahoma Health Sciences Center, United StatesReviewed by:
Ivana Galinovic, Charité University Medicine Berlin, GermanyAdrian Scutelnic, University Hospital of Bern, Switzerland
Copyright: © 2025 Seah, Chong, Dumitrascu, Schwedt, Cao and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Catherine D. Chong, Y2hvbmcuY2F0aGVyaW5lQG1heW8uZWR1
 Nick Seah1,2
Nick Seah1,2 Catherine D. Chong
Catherine D. Chong Oana M. Dumitrascu
Oana M. Dumitrascu Todd J. Schwedt
Todd J. Schwedt Teresa Wu
Teresa Wu