Abstract
Generalized arterial calcification of infancy (GACI) is an extremely rare autosomal recessive condition characterized by the storage of calcium at the level of internal elastic membrane of arteries. The main consequences are intimal fibrous thickening and arterial occlusion. We present the case of a preterm male infant, born from an improperly dispensed pregnancy. At birth, the newborn presented generalized edema and hypotonia, and abolished heart sounds, without response to stimulation. Despite the mechanical ventilation, the infant died 2 h after birth. The death was clinically presumed to be related to the maternal infection with cytomegalovirus (CMV) and Toxoplasma gondii. The infant's mother affirmed the history of 6 previous miscarriages and a non-consanguineous marriage. At autopsy, microscopic examination showed generalized vasculitis secondary to minimal calcification of the large and medium-sized vessels of the lungs, liver, and tongue. These findings supported the diagnosis of GACI. Hydrothorax, non-infective ascites, and necrosis of the brain parenchyma were also associated. The premature infant died due to tonsillar herniation associated with decreased vessel compliance and refractory pulmonary hypertension thus leading to congestive cardiac failure. CMV was not detected on histopathological assessment nor were signs of any other infections. To the best of our knowledge, this is the first case of GACI occurring in a baby from a mother co-infected with CMV and T. gondii.
Introduction
Bryant and White first described the generalized arterial calcification of infancy (GACI) in 1901 after performing the autopsy of a 6-months-old child (1). It is a rare fatal disease that presents in early infancy (2). With 50 cases reported before 1971 (3) and another 150 reported worldwide since then (4–7), it occurs with an estimated frequency of 1:390,000 infants (2).
GACI is considered idiopathic or a metastatic calcification of the large and medium-sized arteries secondary to advanced renal diseases, anomalies of the cardiovascular system, hypervitaminosis D, or parathyroid abnormalities (4, 8–13). Most recent theories refer to GACI as a genetic disease that might be caused by mutations in the ectonucleotide pyrophosphatase/phosphodiesterase 1 gene (ENPP1). ENPP1 gene is known to inhibit the storage of calcium at the level of soft tissues. Its mutation is inherited in an autosomal recessive pattern and is mostly seen in relation to consanguinity (4, 8–10).
At autopsy, GACI was reported in infants between 4 days and 20 months after birth (3–7). In this paper, we present the fatal case of the youngest newborn, which was reported in Medline literature, with non-consanguinity related GACI and the first instance in which the mother had a co-infection with CMV and T. gondii.
Case report
Clinical history
A 42-year-old, gravida 13, para 7, non-consanguineous married pregnant woman, in her 32nd week of pregnancy, was admitted to the Emergency Unit for polyhydramnios and pre-labor rupture of membranes (PROM). She declared an improperly dispensed pregnancy, with no regular gynecological consultations. She also affirmed that she had experienced 6 previous miscarriages.
Emergency cesarean section was performed and a male fetus was prematurely delivered. His Appearance, Pulse, Grimace, Activity, and Respiration (APGAR) scores were 1 at 1 min, 2 at 5 min, and 3 at 10-, 15-, and 20 min. At birth, the newborn presented generalized edema, cyanotic skin with petechiae, and generalized hypotonia, bradycardia, abolished heart sounds, without response to stimulation. As no spontaneous respiration occurred immediately after birth, endotracheal intubation, mechanical ventilation as well as continuous positive inotrope support was provided. Ultrasound examination revealed bilateral pleural effusion, ascites, and pericardial effusion. Despite the aggressive treatment, 2 h after being delivered, the infant died and an autopsy was requested. The mother granted her signed consent for the autopsy to be performed.
Maternal investigations
Intrauterine infection was detected and serum examinations were performed, in order to rule out Toxoplasmosis, Other agents, Rubella, Cytomegalovirus, and Herpes Simplex (TORCH) syndrome. The paraclinical examinations indicated normal ranges for anti-hepatitis B and C and anti-rubella antibodies, same as for Immunoglobulin M (IgM) anti-CMV, anti-rubella, and anti-Toxoplasma gondii. High serum values were detected for anti-CMV Immunoglobulin G (IgG) (414.5 U/mL; normal range 0–0.5 U/mL) and anti-T. gondii IgG (55.30 U/mL; normal range 0–1 U/mL). All the biochemical tests, for detection of IgG/IgM, were performed through electrochemiluminescent immunoassay using Cobas e 411 analyzer and the diagnostic kits from the same manufacturer (Roche Diagnostics GmbH, Mannheim, Germany).
Autopsy findings
The 2,850 g preterm baby presented cyanotic skin and generalized edema, with hydrothorax, non-infective ascites, and hydrocele. The heart and the large vessels were macroscopically unremarkable. Protein dystrophy was seen in the myocardial fibers (Figure 1), without signs of myocardial ischemia or histological modifications of the coronary arteries.
Figure 1
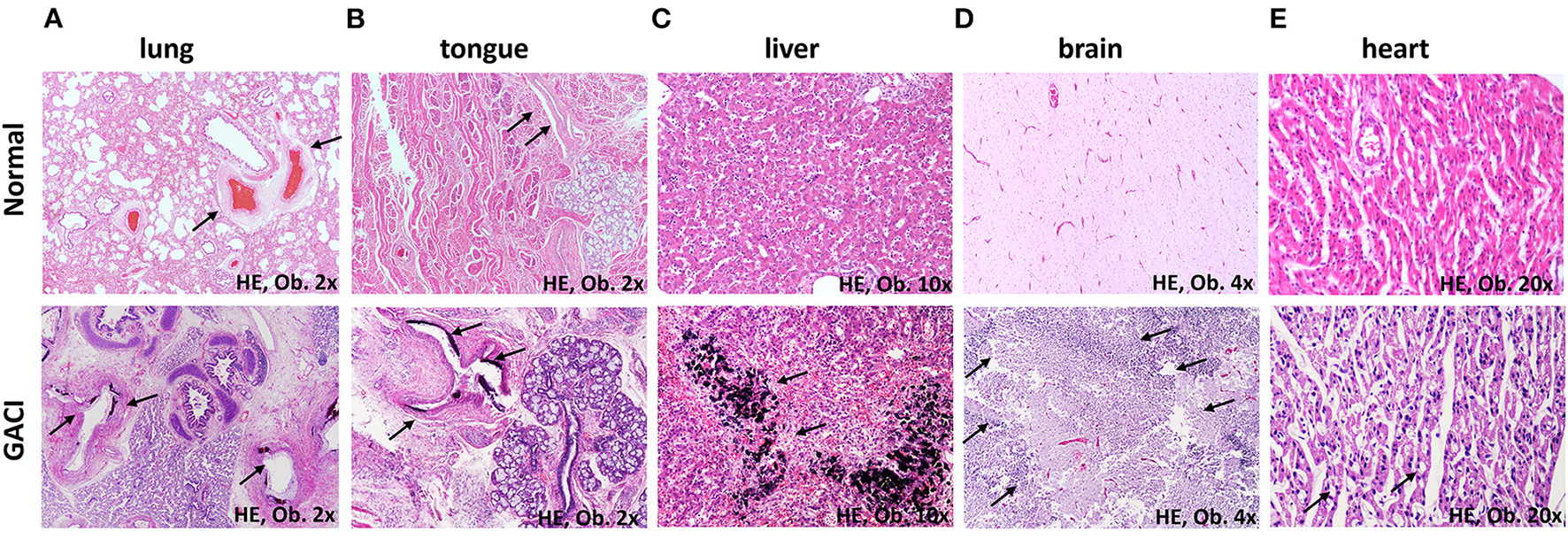
Microscopic findings of the multisystemic GACI compared with normal structures (arrows): (A) Calcifications of the medium-sized arteries of the lung. (B) Intimal calcifications of the arteries of the tongue. (C) Calcifications of the hepatocytes. (D) Necrosis of the brain parenchyma. (E) Hydropic changes of the myocardial fibers.
Bilateral dystelectasis of the lungs was macroscopically described. Microscopic examination of the lung parenchyma revealed a predominance of vascular abnormalities, without pulmonary edema, hyaline membranes, bronchopneumonia, or other modifications of the lung parenchyma. The intima of large and medium-sized arteries showed marked thickness with degenerative calcifications of lamina elastica interna (Figure 1). In the intima, a proliferation of myofibroblasts that expressed Smooth Muscle Actin (SMA) and Cluster of Differentiation 34 (CD34) was predominant, without proliferation of Cluster of Differentiation 31 (CD31) -marked endothelial cells (Figure 2). Myointimal calcifications at the level of the hepatic vessels associated with necrosis of the perivascular hepatocytes (Figure 1).
Figure 2
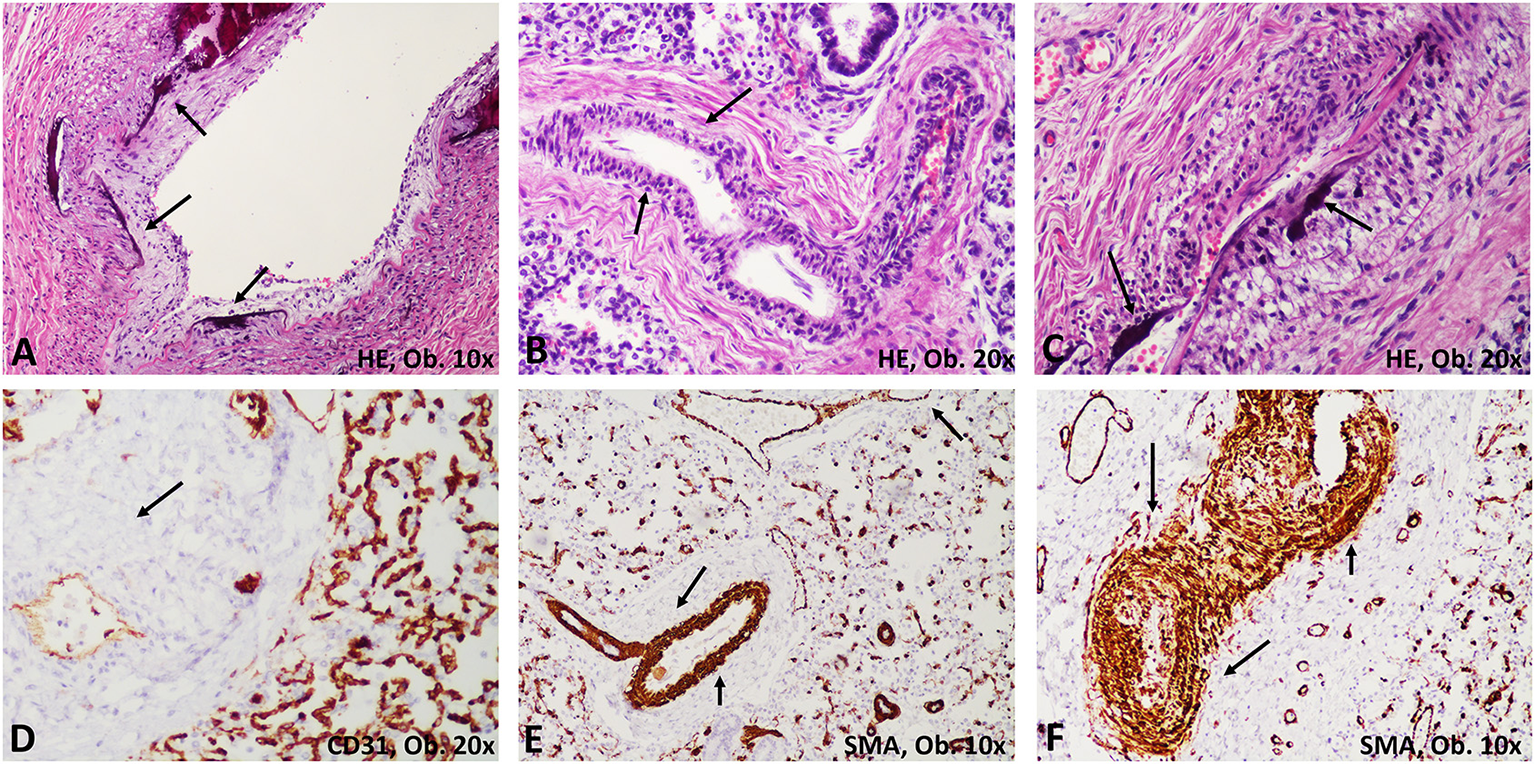
Histological modifications of the pulmonary arteries (arrows). (A) Calcifications of the lamina elastica; (B,C) Thickening of the intima with calcifications and stenosis of the arterial lumen. (D) The proliferated cells are negative for CD31. (E,F) Compared with normal arteries, marked proliferation of myofibroblasts is emphasized with smooth muscle actin (SMA).
At the base of the tongue and in the lower third of the pharynx, hemorrhagic areas of 7–12 mm were seen. Microscopically, the calcification of the intimal layer of the arteries was identified as similar to that of the pulmonary vessels (Figure 1).
Cerebral edema, tonsillar herniation, and extensive areas of necrosis were seen in the brain parenchyma (Figure 1). Death was identified as a result of acute respiratory failure, which was mainly induced by compression of the central respiratory centers and the external compression of the lung tissue leading to persistent pulmonary hypertension and heart failure.
No histological signs of CMV (e.g., ductular proliferation or cholestatis in the liver; the presence of giant cells; cytopathic changes; CMV inclusions) were seen and no immunohistochemical (IHC) positivity for CMV was proved in any of the examined organs (brain, kidney, spleen, lymph nodes, liver, lungs) (14). No neuronal degeneration or leukomalacia, as indicators of toxoplasmosis (15), was detected in the tissues harvested at autopsy.
Discussion
GACI is an unusual and uncommon cause of death among newborns. This is the only case in our university hospital that has been seen in over a decade. Over the same period, almost 200 autopsies were performed annually, one-third of which were autopsies of neonates.
As a non-usual disease, only limited data about the microscopic aspects of GACI have been gathered. GACI is defined by marked calcification of the internal elastic membrane of the large and medium-sized arteries, fibroblastic proliferation in the intima, and a giant cell reaction (3, 6, 11). Coronary arteries were mostly described to be narrowed, with ventricular dysfunction or myocardial infarction as the major complications (7, 11, 16, 17). In our case, no signs of myocardial ischemia, myocarditis, nor foci of calcification were seen in the coronaries. Also, no giant cells were identified. Myointimal calcifications of the walls of the arteries were seen in the lung, liver, and base of the tongue. The proliferated cells proved to be myofibroblasts which were marked by CD34 and SMA but not by CD31 (18). No other cases with tongue involvement were reported till now.
Although necrosis of the hepatocytes and brain parenchyma might be related to CMV or Toxoplasma infection of the mother, previous data denied any possible connection between GACI and viral infections such as Coxsackie B viremia (13). In our case, we were also not able to prove the existence of encephalitis caused by a primary infection in the mother. In a previously published article, neurologic manifestations were reported in patients with GACI, with magnetic resonance imaging (MRI) proved strokes, gliosis, bilateral occipital necrosis, and cystic encephalomalacia (2) but no histopathological findings were shown. As miscarriage, hydrops, polyhydramnios, and fetal distress were seen in our and other reported cases (3, 19), it can be supposed that GACI might be a favoring factor rather than a consequence of intrauterine infections. On the other hand, in the present case, the mother's paraclinical tests indicated high serum values for anti-CMV IgG and anti-T. gondii IgG, but not for the IgM. This data indicated a chronic maternal infection that was probably not transmitted to the fetus during pregnancy, as the histological examination of the tissues harvested from the autopsy confirmed.
Although GACI has long been considered an idiopathic disease, the most recent case reports showed a close relation between ENPP1 gene mutations and consanguinity (13, 20). In our case, the infant was born from a non-consanguineously married woman, who indeed suffered from multiple unexplained miscarriages. Genetic investigations were not requested by the mother.
Untreated, death of the infant occurs before the age of 6 months by myocardial ischemia and cardiorespiratory arrest (6, 19). In any baby with pulmonary hypertension and hydramnios, GACI should be suspected (6). When diagnosed early, by fetal ultrasound, calcium chelator therapy with sodium thiosulfate or other bisphosphonates that solubilize calcium depositions, along with magnesium supplementation might prolong life until adolescence or early adulthood (2, 6, 17, 19). Although no curative therapy exists, extracorporeal membrane oxygenation along with supportive therapy might be the preferred therapy of choice (19).
The present unusual case was presented to highlight the need to more attentively evaluate patients with TORCH syndrome. Even if neurological or cardiovascular disorders might be seen in such infants, GACI should be considered a possibility.
Funding
This study was partially funded by the CNCS - UEFISCDI, project number PN-III-P4-ID-PCE2020-1540 - Director of Project MS. The English proofread was done by Cambridge Proofreading LLC Professional Team.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent was obtained from the newborn mother to perform the autopsy and publish the scientific results.
Author contributions
SG drafted the paper and performed the design of the study. DB performed the autopsy and contributed to the case description, histopathological assessment, and literature review. IJ and EF contributed to histopathological and immunohistochemical assessment. RS performed the clinical management of the case and interpretation of the clinical data. MS participated at the design of the project and funding of the study. EF participated at the autopsy, contributed to macroscopic, and conferred the final agreement for publication. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
- APGAR
Appearance, Pulse, Grimace, Activity and Respiration
- CD
Cluster of Differentiation
- CMV
Cytomegalovirus
- ENPP1
Ectonucleotide pyrophosphatase/phosphodiesterase 1
- GACI
Generalized arterial calcification of infancy
- Ig
Immunoglobulin
- IHC
Immunohistochemistry
- MRI
Magnetic Resonance Imaging
- PROM
Pre-labor rupture of membranes
- SMA
Smooth Muscle Actin
- TORCH
Toxoplasmosis, Other agents, Rubella, Cytomegalovirus, Herpes Simplex.
Abbreviations
References
1.
Bryant JH White WH . A case of calcification of the arteries and obliterative endarteritis, associated with hydronephrosis, in a child aged six months. Guys Hosp Rep. (1901) 55:17.
2.
Staretz-Chacham O Shukrun R Barel O Pode-Shakked B Pleniceanu O Anikster Y et al . Novel homozygous ENPP1 mutation causes generalized arterial calcifications of infancy, thrombocytopenia, and cardiovascular and central nervous system syndrome. Am J Med Genet A. (2019) 179:2112–8. 10.1002/ajmg.a.61334
3.
Parker RJ Smith EH Stoneman ME . Generalised arterial calcification of infancy. Clin Radiol. (1971) 22:69–73. 10.1016/s0009-9260(71)80014-4
4.
Rutsch F Boyer P Nitschke Y Ruf N Lorenz-Depierieux B Wittkampf T et al . Hypophosphatemia, hyperphosphaturia, and bisphosphonate treatment are associated with survival beyond infancy in generalized arterial calcification of infancy. Circ Cardiovasc Genet. (2008) 1:133–40. 10.1161/CIRCGENETICS.108.797704
5.
Nagaraj BR Jain P Thomas DA Raghu M . Sonological appearance of idiopathic arterial calcification in fetus: a rare case. Indian J Radiol Imaging. (2009) 19:248–51. 10.4103/0971-3026.54876
6.
Attia TH Abd Alhamed MM Selim MF Haggag MS Fathalla D . Idiopathic arterial calcification of infancy: case report. J Radiol Case Rep. (2015) 9:32–40. 10.3941/jrcr.v9i11.2622
7.
Yapicioglu-Yildizdas H Ozbarlas N Erdem S Yilmaz MB Ozlu F Buyukkurt S et al . Two newborn babies with generalized arterial calcification of infancy, two new mutations. Turk J Pediatr. (2016) 58:419–23. 10.24953/turkjped.2016.04.013
8.
Dlamini N Splitt M Durkan A Siddiqui A Padayachee S Hobbins S et al . Generalized arterial calcification of infancy: phenotypic spectrum among three siblings including one case without obvious arterial calcifications. Am J Med Genet A. (2009) 149A:456–60. 10.1002/ajmg.a.32646
9.
Nitschke Y Rutsch F . Generalized arterial calcification of infancy and pseudoxanthoma elasticum: two sides of the same coin. Front Genet. (2012) 3:302. 10.3389/fgene.2012.00302
10.
Yunfeng L Tongyan H Jing W Xiaomei T . Case report: a novel genetic mutation causes idiopathic infantile arterial calcification in preterm infants. Front Genet. (2021) 12:763916. 10.3389/fgene.2021.763916
11.
De Vilder EY Vanakker OM . From variome to phenome: pathogenesis, diagnosis and management of ectopic mineralization disorders. World J Clin Cases. (2015) 3:556–74. 10.12998/wjcc.v3.i7.556
12.
Moran JJ Becker SM . Idiopathic arterial calcification of infancy; report of 2 cases occurring in siblings, and review of the literature. Am J Clin Pathol. (1959) 31:517–29. 10.1093/ajcp/31.6.517
13.
Stryker WA . Arterial calcification in infancy with special reference to the coronary arteries. Am J Pathol. (1946) 22:1007–31.
14.
Souder JP Grimm E Pinninti S Boppana S Hsu E Horslen S et al . Congenital cytomegalovirus and hepatic failure: an underrecognized complication. Pediatr Infect Dis J. (2022) 41:e49–e53. 10.1097/INF.0000000000003381
15.
Gutierrez-Exposito D Arteche-Villasol N Vallejo-García R Ferreras-Estrada MC Ferre I Sanchez-Sanchez R et al . Characterization of fetal brain damage in early abortions of ovine toxoplasmosis. Vet Pathol. (2020) 57:535–44. 10.1177/0300985820921539
16.
Nael A Siaghani PJ Chen D Romansky SG Shane L . Idiopathic Infantile arterial calcification: a possible cause of refractory cardiopulmonary failure in infancy. Case Rep Pathol. (2014) 2014:189850. 10.1155/2014/189850
17.
Gurzu S Ciortea D Munteanu T Kezdi-Zaharia I Jung I . Mesenchymal-to-endothelial transition in Kaposi sarcoma: a histogenetic hypothesis based on a case series and literature review. PLoS ONE. (2013) 8:e71530. 10.1371/journal.pone.0071530
18.
Donuru A Kandula V Oliver E Saul D . Generalized arterial calcification of infancy. Radiol Cardiothorac Imaging. (2020) 2:e190226. 10.1148/ryct.2020190226
19.
Deshpande SR Kasniya G Cuadrado AR Maher KO . Idiopathic infantile arterial calcification: a case report of successful extracorporeal membrane oxygenation support. Int J Artif Organs. (2017) 39:575–9. 10.5301/ijao.5000544
20.
Dayapala A Rathnayake IL Pethiyagoda P . A case of idiopathic arterial calcification of infancy diagnosed at autopsy. Ceylon Med J. (2016) 61:137–8. 10.4038/cmj.v61i3.8354
Summary
Keywords
vascular calcification, neonatal prematurity, autopsy, toxoplasmosis, histology
Citation
Gurzu S, Burlacu D, Sánta R, Jung I, Slevin M and Fulop E (2022) Case Report: Coexistence of generalized arterial calcification of infancy (GACI) and maternal infections with cytomegalovirus and Toxoplasma gondii-unexpected fatal complication in a newborn. Front. Pediatr. 10:922379. doi: 10.3389/fped.2022.922379
Received
17 April 2022
Accepted
15 June 2022
Published
18 August 2022
Volume
10 - 2022
Edited by
Olivier Abbo, Hôpital Des Enfants, CHU Toulouse, France
Reviewed by
Sanjeevani Masavkar, Lokmanya Tilak Municipal Medical College, India; Ehsan Ahmadpour, Tabriz University of Medical Sciences, Iran; Veeranoot Nissapatorn, Walailak University, Thailand
Updates
Copyright
© 2022 Gurzu, Burlacu, Sánta, Jung, Slevin and Fulop.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Diana Burlacu dianaburlacu@yahoo.com
†These authors have contributed equally to this work
This article was submitted to Pediatric Pulmonology, a section of the journal Frontiers in Pediatrics
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.