- 1Department of Pediatrics, Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand
- 2Division of Cardiovascular and Thoracic Surgeon, Department of Surgery, Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand
- 3Department of Family and Preventive Medicine, Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand
Introduction: Low-cardiac-output syndrome (LCOS) after cardiac surgery may lead to poor postoperative outcomes. The venous-to-arterial carbon dioxide partial pressure difference (VACO2) showed association with poor outcomes in adults with cardiac surgery, but it's validity in pediatric population is uncertain. We evaluated the association of VACO2 with LCOS-related outcomes and the correlation with other surrogate markers such as lactate levels and oxygen extraction ratio.
Methods: This prospective cohort study was conducted at an intensive care unit in a tertiary academic hospital. Children aged 1 day–18 years old undergoing elective cardiac surgery with cardiopulmonary bypass between August 2021 and December 2023 were included. Arterial and venous blood gases were collected at intensive care unit admission and at 6, 12, and 24 h postoperatively. The LCOS-related outcomes were defined as at least two of the following criteria being met within 24 h postoperatively: vasopressor-inotropic score ≥20, ejection fraction <50% on echocardiography, need for serious post-operative intervention, and death.
Results: Of the 127 included patients (median age: 44.4 months), 37 (29.1%) had a Risk Adjustment for Congenital Heart Surgery score ≥3, and 26 (20.4%) had LCOS-related outcomes. Linear mixed model regression analysis revealed that the VACO2 did not significantly differ between patients with and without LCOS-related outcomes at all four time points. VACO2 showed a fair-to-weak correlation with the oxygen extraction ratio (R2 = 0.58; p < 0.001, R2 = 0.22; p = 0.015, and R2 = 0.19; p = 0.045, at 6, 12, and 24 h postoperatively, respectively) but showed no correlation with lactate levels. A persistently high VACO2 (≥6 mmHg) at 6 h postoperatively was significantly associated with fewer 28-day inotrope-free and intensive care unit-free days.
Discussion: VACO2 was not significantly associated with LCOS-related outcomes in children after cardiac surgery with cardiopulmonary bypass. A persistently high VACO2 at 6 h postoperatively was correlated with prolonged inotrope use and a prolonged intensive care unit stay.
1 Introduction
Cardiopulmonary bypass (CPB) during open-heart surgery constitutes a potent stimulus that induces a systemic inflammatory response through the following mechanisms: blood contact with the CPB circuit, ischemia–reperfusion injury, heparin–protamine interaction, and surgical trauma (1). These mechanisms aggravate complement cascade activation, endotoxin release, and cytokine production, leading to low-cardiac-output (CO) syndrome (LCOS), which occurs in 5%–55% (2) of pediatric patients after cardiac surgery and frequently occurs 9–12 h postoperatively (3). Delayed recognition and treatment of LCOS can lead to multiorgan system failure and even death.
Serum lactate level, central venous oxygen saturation (ScvO2), and oxygen extraction ratio (O2ER) are commonly used to monitor LCOS after cardiac surgery, however, these parameters may be influenced by multiple factors that are unrelated to low CO. For example, hyperlactatemia can occur due to the stress response to surgery, use of beta-adrenergic agonists, hyperglycemia, or acute liver and renal failure (4); furthermore, normal or high ScvO2 values may be observed in the presence of mitochondrial dysfunction or the peripheral shunting effect (5). Some studies in sepsis population demonstrated unclear benefits of lactate levels and ScvO2 for guiding therapy (6, 7). Recently, a novel bedside biomarker, venous-to-arterial carbon dioxide (CO2) partial pressure difference (VACO2), has emerged, suggesting a potential utility as an adjunctive marker to facilitate the guidance of therapeutic interventions in sepsis (5, 8).
The VACO2 theoretically measures the circulatory clearance of tissue CO2 and is inversely correlated with CO (9). VACO2 is a better surrogate indicator of stagnant dysoxia than of dysoxia caused by hypoxia, anemia, or cytopathic pathology (9). A high VACO2 at the time of sepsis diagnosis in adult patients exhibited a significant correlation with both the cardiac index and other tissue perfusion parameters such as lactate levels and ScvO2 (10). A recent meta-analysis of 21 studies with 2,155 critically ill adult patients with both surgical and medical conditions demonstrated an association between high VACO2 and CO and linked this to mortality (11). However, only four of these 21 studies focused on cardiac surgery, and they all reported different associations with unfavorable outcomes. Chen et al. (12) conducted propensity-matched analysis in 228 individuals post cardiac surgery with CPB and reported a significant influence of high VACO2 on adverse outcomes with superior discrimination power than arterial lactate. Furthermore, two prospective adult studies (13, 14) indicated that high VACO2 is an independent predictor of major postoperative complication after multivariate analyses. Owing to the limited data on VACO2 in pediatric patients after cardiac surgery with CPB, the relevance of VACO2 as a predictor of poor outcomes in this population remains unclear.
In this study, we aimed to evaluate the association between VACO2 and LCOS-related outcomes in children undergoing cardiac surgery with CPB and determine its correlation with other bedside surrogate markers. The secondary objective was to examine the association between VACO2 and postoperative outcomes.
2 Materials and methods
2.1 Study design, setting, and participants
This prospective cohort study was performed in an eight-bed pediatric intensive care unit (PICU) at Songklanagarind Hospital, Hat Yai, Songkhla. Children aged 1 day–18 years with congenital or acquired cardiac disease who underwent elective open cardiac surgery with CPB and were admitted to the PICU postoperatively were included in the study. The exclusion criteria were as follows: preterm infants (gestational age <37 weeks), weight <2 kg, inability to wean off CPB, requirement for extracorporeal membrane oxygenation (ECMO) before leaving the operating room, and absence of arterial and central lines postoperatively. This study was approved by the Institutional Review Board of the Faculty of Medicine, Prince of Songkla University (Institutional Review Board approval number 64-299-1-1; date of approval: August 3, 2021). The study was conducted in accordance with Good Clinical Practice and the Helsinki Declaration of 1975.
2.2 Surgical procedures
Anesthesia was initiated according to our standardized protocol. Following incision, heparin was administered intravenously at a dosage of 3 mg/kg to achieve an activated clotting time (ACT) exceeding 400 s. ACT was monitored at 30-min intervals throughout the procedure, with an additional heparin dose of 3 mg/kg provided if the ACT fell below 400 s. Intraoperative corticosteroids were administered intravenously, based on individual anesthesiologist preferences. The priming solution for the CPB circuit included either Ringer's lactate or normal saline with mannitol, along with 20% albumin for patients weighing less than 10 kg. Leukocyte-depleted packed red blood cells were utilized when the preoperative hematocrit was below 30%. CPB was performed using a CAPIOX® FX05 Oxygenator and Stockert S5 pump, following the α-stat strategy at a target temperature of 28°C. Hypothermia was induced to varying degrees; depending on the surgical procedure. Antegrade cold blood cardioplegia was administered at a volume of 20 ml/kg to achieve cardiac arrest, with an additional 10 ml/kg given if aortic cross-clamp time exceeded 20 min. Pump flow rates were maintained between 100 and 150 ml/kg/min for infants and 2.5–3.0 L/m2/min for older patients: adjusted according to age-appropriate mean arterial pressure. Arteriovenous modified ultrafiltration was selectively applied, based on the consensus of the surgical team and perfusionist, and performed for 5 min after separating from CPB. At the conclusion of CPB intravenous protamine sulfate was administered to reverse heparin anticoagulation.
2.3 Data collection and measurement
After receiving written informed consent from the patients’ parents or legal guardians before operation, 0.3 ml blood samples were simultaneously collected from both the arterial and internal jugular central lines. This sampling was repeated at four different time points after patient arrival in the PICU: at PICU arrival (T0), 6-h (T6), 12-h (T12), and 24-h (T24) post operation. Arterial and venous blood gas readings were accepted if the samples were collected within 5 min of each other. A 1 h time gap in the collection of blood samples from the research schedule was allowed owing to unpredictable intensive care unit occupancy. Blood samples were analyzed within 1 min of blood collection using an arterial blood gas analysis machine (ABL 800 Basic Radiometer; Copenhagen, Denmark) located within the PICU. The attending staff independently provided standard post-cardiac surgery care, including fluid resuscitation, vasopressor and inotropic medication, and steroid administration without the researcher's involvement. If either the central or arterial lines were displaced within 24 h postoperatively, the remaining data were recorded as missing.
Data, including general baseline characteristics, intraoperative parameters, postoperative interventions, and outcomes, were collected until the patient was discharged. The Risk Adjustment for Congenital Heart Surgery tool (15) was used to classify the risk of mortality after congenital cardiac surgery. The vasoactive-inotropic score (VIS) was calculated using the formula by Gaies et al. (16) as follows:
Acute kidney injury was diagnosed according to the Kidney Disease-Improving Global Outcomes guidelines, 2012 (17), based on the presence of any of the following: a >0.3 g/dl increase in the serum creatinine level within 48 h, >1.5 times increase in the serum creatinine level from a known baseline value or one recorded within the preceding 7 days, and urinary volume <0.5 ml/kg/h for 6 h. The 28-day ventilator-free days (VFDs), 28-day inotrope-free days, and 28-day ICU-free days (IFDs) were defined as the number of days that the patient survived without invasive ventilation, inotropic drugs, or ICU admission during the first 28 days postoperatively, with the day after the first postoperative night considered as day 1. These variables were counted as zero for non-survivors.
The independent variables studied included the bedside surrogate markers (VACO2, O2ER, and lactate level) that were measured postoperatively. ScvO2 was not evaluated because the participants’ single-ventricle physiology might have interfered with ScvO2 interpretation. VACO2 was calculated as the central venous minus arterial CO2 level and O2ER as the ratio between the difference in arterial and central venous oxygen saturation divided by the arterial oxygen saturation.
The primary outcomes were LCOS-related outcomes, which was consisted of at least two of the following criteria within 24 h postoperatively: (1) VIS ≥20; (2) left ventricular ejection fraction <50% on echocardiography; (3) any unplanned surgery or intervention, cardiac arrest, or utilization of ECMO; and (4) death. The secondary outcomes included: 28-day VFDs, 28-day inotrope-free days, 28-day IFDs, percentage of morbidities (reintubation, significant arrhythmic events requiring medication or intervention, acute kidney injury, renal replacement therapy, and neurological complications), and mortality rate.
2.4 Statistical analyses
Statistical analyses involved descriptive analysis of means (standard deviations) for normally distributed continuous data, medians (interquartile ranges) for non-normally distributed continuous data, and percentages for categorical data. The Student's t-test or Mann–Whitney U test was used for intergroup comparison of continuous data, depending on the pattern of data distribution. Categorical data were compared using the chi-squared or Fisher's exact test, as indicated. Correlation analysis between bedside parameters was performed using Pearson's and Spearman's correlation coefficients for parametric and non-parametric variables, respectively. Linear mixed-model regression was used to compare the postoperative laboratory (lactate, VACO2, and O2ER) values between the LCOS and no-LCOS groups over time with adjusted confounder variables that might affect outcome (age, RACHS, type of repair, CPB time, intraoperative corticosteroid, intraoperative fluid balance). Receiver operating characteristic curves were used to evaluate performance of VACO2 on discriminating LCOS-related outcomes. Subgroup analysis was performed according to patient's age, type of repair, and RACHS score. Statistical significance was set at p < 0.05. All analyses were conducted using R version 4.3.1 (The R Foundation for Statistical Computing, Vienna, Austria).
2.5 Ethics statement
Ethical approval for this study was obtained from the Ethics Committee of the Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand.
3 Results
3.1 Baseline characteristics of participants
Between August 2021 and December 2023, 136 patients underwent open-heart surgery. Nine patients were excluded from the study, which included five patients who could not be weaned off CPB postoperatively and four patients who underwent emergency operations. The final analysis included 127 patients, of which 26 (20.4%) developed LCOS-related outcomes within 24 h postoperatively. Five patients (3.9%) required re-operation or reintervention, seven (5.5%) required ECMO, three (2.4%) developed cardiac arrest, and seven (5.5%) died. Factors significantly associated with LCOS-related outcomes included preoperative sepsis, a high Risk Adjustment for Congenital Heart Surgery score, long CPB time, long aortic clamp time, high amount of blood transfusion, and intraoperative corticosteroid administration (Table 1). The rates of postoperative intervention, including systemic steroid administration (60.4% vs. 24.3%, p < 0.01), blood transfusion [19.6 [10.0–34.6] vs. 6.4 [0–13.5] ml/kg, p < 0.01], and renal replacement therapy (13% vs. 0%, p = 0.002), as well as those of end-organ dysfunction and death, were higher in the LCOS group than in the no-LCOS group (Supplementary Table 1).
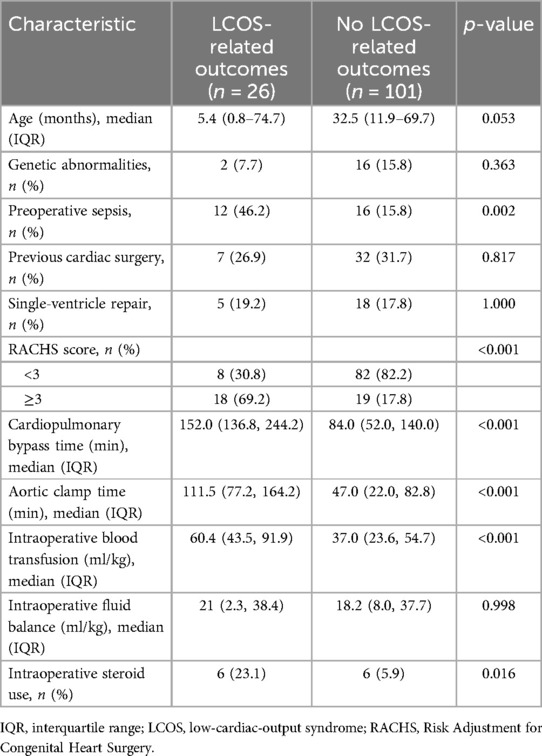
Table 1. Comparison of baseline characteristics and intraoperative parameters between patients with and without LCOS-related outcomes (n = 127).
3.2 Association between VACO2 and outcomes after cardiac surgery
The patterns of laboratory values at the four time points are illustrated in Figure 1. The overall values of three parameters in the LCOS group were higher than those in the non-LCOS group at all four time points, with the exception for the VACO2 at 24 h post operation. Univariate analysis performed to compare bedside surrogate marker values between patients with and without poor LCOS-related outcomes revealed that the LCOS group had significantly higher VACO2 values at 12 h postoperatively, higher lactate levels at all four time points, and higher O2ER values at PICU admission and at 6 h postoperatively than the no-LCOS group. Analysis of the overall unadjusted area under the curve (AUC) of VACO2 was 0.58–0.64 which was inferior to serum lactate levels in predicting LCOS events (Table 2).
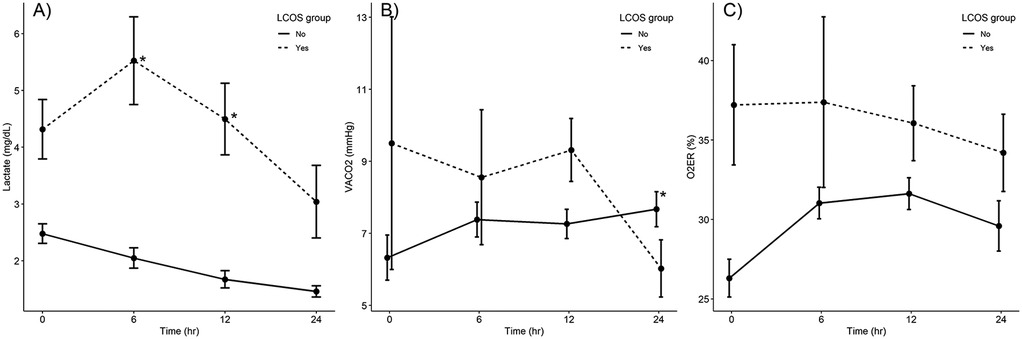
Figure 1. Comparison of laboratory values (A) lactate level, (B) VACO2, (C) O2ER between patients with and without LCOS-related outcomes at four time points (N = 127). *p < 0.05, in the linear mixed-model regression analysis. AVO2, arteriovenous oxygen saturation difference LCOS, low-cardiac-output syndrome; VACO2, venous-to-arterial carbon dioxide partial pressure difference.
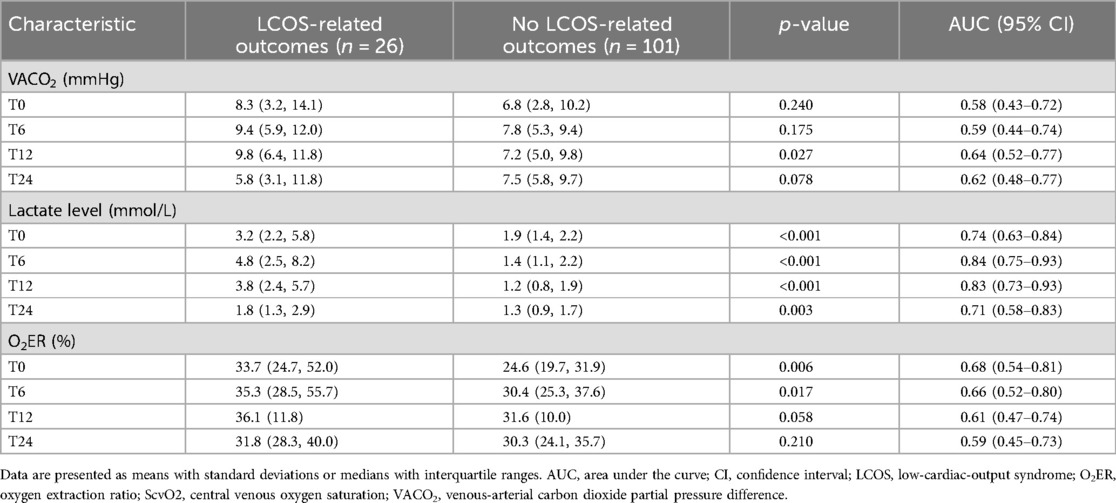
Table 2. Comparison of laboratory values between patients with and without LCOS-related outcomes (n = 127).
After performing linear mixed-model regression analysis, the relationship between lactate change and the LCOS occurrence was significantly at 6 h and 12 h postoperatively (p < 0.05), whereas the VACO2 change was significant at 24 h postoperatively (p = 0.02) and there was no relationship between O2ER change at all four time points (Figure 1).
To achieve the secondary study objective, we used a 6-mmHg cut-off, as described previously (9), to categorize the 6-h postoperative VACO2 values into two groups. The results revealed significantly fewer 28-day inotrope-free days and 28-day IFDs in patients with a VACO2 ≥6 mmHg than in patients with a VACO2 <6 mmHg (24.0 [22.0–27.0] vs. 26.5 [23.0–28.0] days, p = 0.03 and 23.0 [18.2–26.0] vs. 24.0 [22.0–27.0] days, p = 0.03, respectively) (Table 3). Subgroup analysis in patients with biventricular physiology and with aged more than one-month old revealed insignificant different outcomes (Supplementary Tables 2, 3).
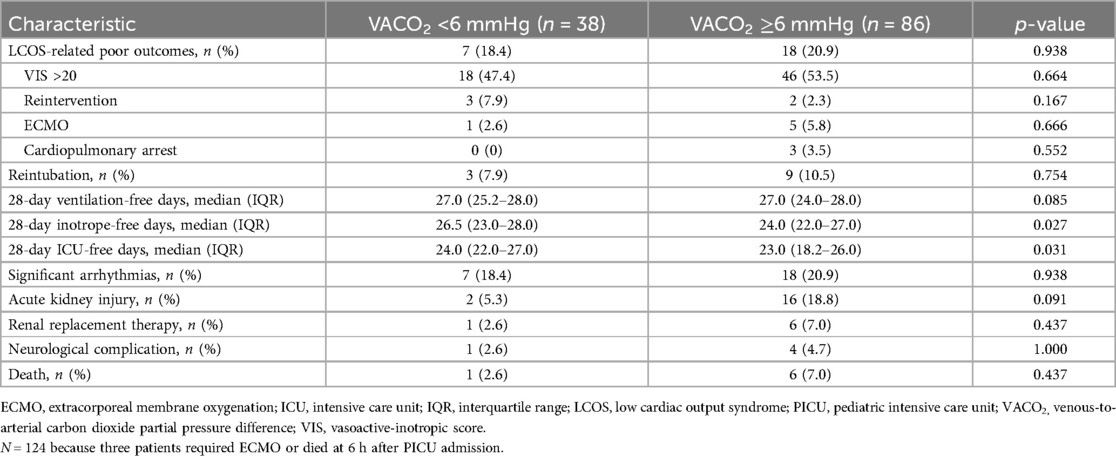
Table 3. Comparison of outcomes between patients with a VACO2 <6 mmHg and ≥6 mmHg at 6 h after PICU admission (n = 124).
3.3 Correlations between VACO2 and other parameters
The correlations between VACO2 and the other parameters (lactate level and O2ER) at the four time points are shown in Figures 2, 3. While VACO2 did not show a significant correlation with lactate levels, it demonstrated a moderate correlation with O2ER at 6 h postoperatively (r = 0.58; p < 0.001) and a weak correlation with O2ER at 12 and 24 h postoperatively (r = 0.22; p = 0.015 and r = 0.19; p = 0.045, respectively).
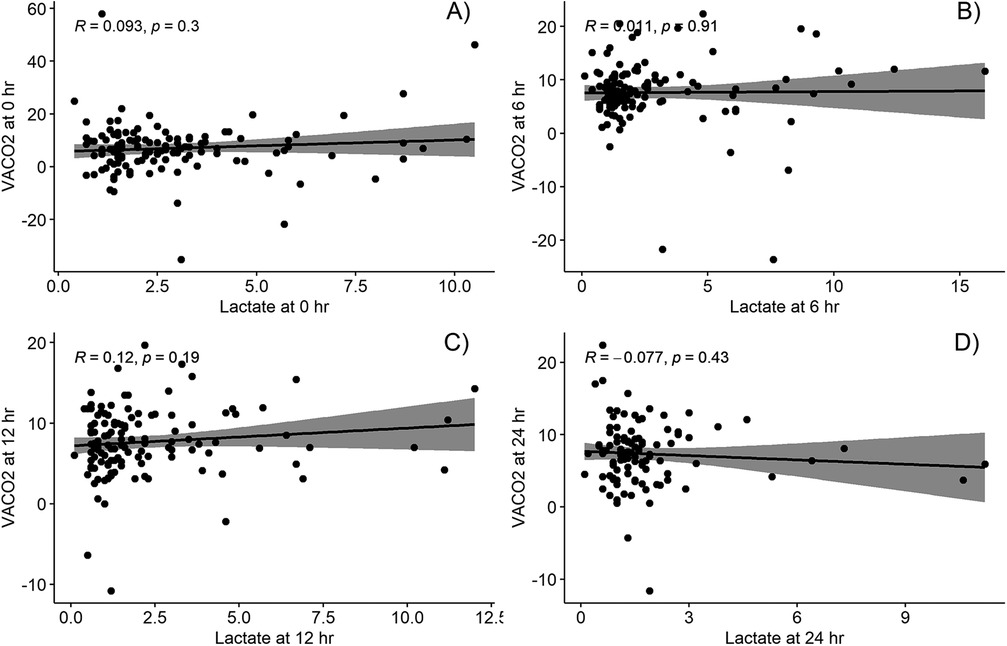
Figure 2. Correlation between venous-to-arterial carbon dioxide partial pressure difference and lactate at different timepoints; (A) at intensive care arrival, (B) at 6 h post operation, (C) at 12 h post operation, and (D) at 24 h post operation. VACO2, venous-to-arterial carbon dioxide partial pressure difference.
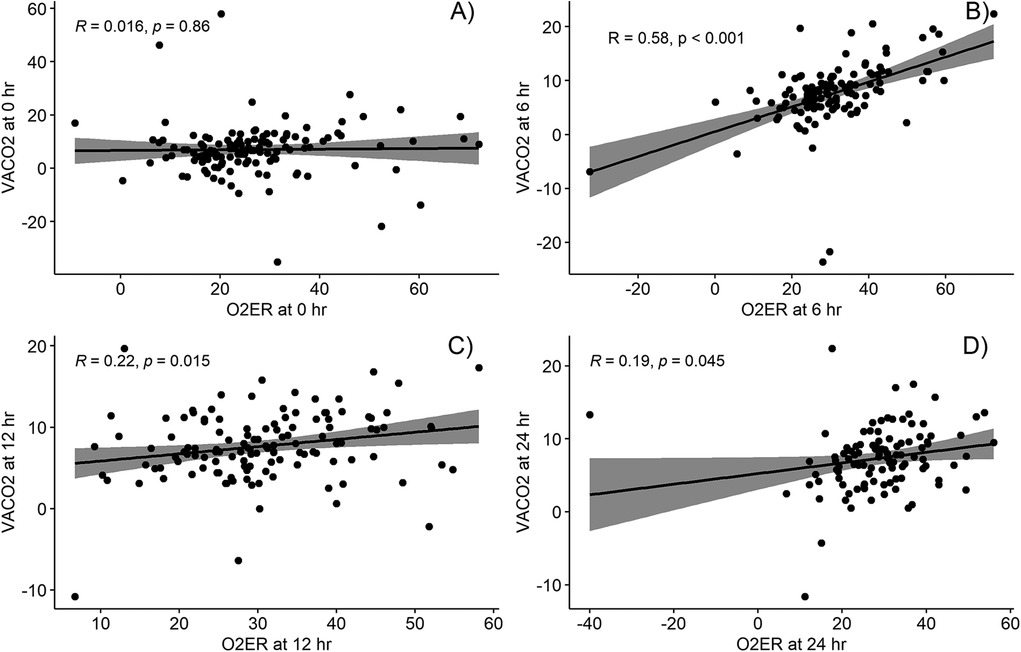
Figure 3. Correlation between venous-to-arterial carbon dioxide partial pressure difference and oxygen extraction ratio at different timepoints; (A) at intensive care arrival, (B) at 6 h post operation, (C) at 12 h post operation, and (D) at 24 h post operation. O2ER, oxygen extraction ratio; VACO2, venous-to-arterial carbon dioxide partial pressure difference.
4 Discussion
This study explores the predictive value of VACO2 in children undergoing cardiac surgery with CPB at four time points (PICU admission and 6, 12, and 24 h postoperatively) and compares it with that of other bedside indicators. The primary finding is that VACO2 shows no association with LCOS-related outcomes and has lower predictive capability than arterial lactate levels. Specifically, an elevated VACO2 at 6 h postoperatively correlates with fewer 28-day inotrope-free days and IFDs.
Our negative findings were similar to Akamatsu et al. (18) regarding the correlation with other surrogates and the association between a VACO2 ≥6 mmHg and unfavorable outcomes (prolonged extubation, duration of hospitalization, and mortality). That study was conducted retrospectively in 114 pediatric patients aged up to 18 years with single blood sampling of the VACO2 at the time of admission. However, this is in contrast with the findings of Rhodes et al. (19), who found a high VACO2 at PICU admission was linked to LCOS-related outcomes (high inotropic score, cardiac arrest, ECMO use, and unplanned surgical interventions within 48 h of PICU admission). They also found VACO2 to have a predictive ability equal to that of lactate levels and superior to that observed in the present study (AUC for VACO2, 0.69 and AUC for lactate levels; 0.64). Another prospective study, conducted in 69 China infants, linked VACO2 >12.3 mmHg within 42 h postoperatively to prolonged ventilator use and ICU stay (20). These contrast results could be attributed to different age groups within the targeted population, as these two studies were conducted in infants, whereas our study and that of Akamatsu et al. (18) were carried out in children aged up to 18 years. Studies in adults also reflect variability in the predictive power of VACO2. No association with outcomes was noted in some studies (21–23), while significant links to mortality were reported in others (12, 14, 24, 25). Overall, the discriminatory performance of VACO2 in adults ranges widely, from 0.52 to 0.83; this is similar to our findings.
The lack of significant association between VACO2 and LCOS-related outcomes in this study may be attributed to several factors. First, circulatory dynamics differ between children and adult's cardiac condition for operation. This study included all pediatric patients across a wide range of ages and congenital cardiac anomalies, encompassing both uni- and biventricular systems. Although subgroup analysis was performed in biventricular physiology group, residual lesion did not take into account. Residual cardiac lesions following total correction or staged reconstruction surgeries in children could influence VACO2 while most cardiac surgery in adults are performed within the biventricular system which do not interfere with mixing cardiac lesions. This was supported by a study on pediatric participants with sepsis who had biventricular systems demonstrated a significant association between VACO2 ≥6 mmHg and mortality (10).
Second, VACO2 measurements may be influenced by conditions such as hyperventilation and hyperoxia in the post-cardiac surgery setting. This might transiently widen the CO2 gap through acute decreases in arterial CO2 levels and increased venous CO2 levels (26, 27), potentially limiting the utility of VACO2 as a reliable marker for predicting LCOS-related outcomes.
Third, the clinical outcomes following pediatric cardiac surgery are multifaceted and not solely attributable to low CO. Factors such as anemia due to intraoperative blood loss or mitochondrial dysfunction due to CPB effects may not necessarily result in an abnormal VACO2, although they can significantly impact poor outcomes (9). Fourth, the timing of the VACO2 evaluation in previous studies differed from that in this study. Most of the adult and pediatric studies in cardiac surgery assessed VACO2 values at the time of admission. In this study, we hypothesized that the evaluation time point at the 6-h postoperative is appropriate for identifying the consequences of LCOS after patients received initial stabilization without the effect of anesthetic in the operating room. Moreover, the inflammatory response that leads to LCOS reaches peak effect at 9–12 h postoperatively (2). Because of the rapid responsiveness of VACO2 to a low circulatory flow state, persistently high VACO2 in a specific period might be better indicate outcomes than single values at admission time.
Our findings for the correlation between VACO2 and other parameters are similar to those of Rhodes et al. and Singh et al. (19, 28); we observed a moderate correlation of VACO2 with O2ER but no significant correlation with lactate levels. Similarly, the results of two studies of post cardiac surgery in adults concur with the findings in that VACO2 had weak or no correlation with lactate levels (21, 29), despite there being a strong correlation with CO (12, 20). Although Castanuela et al. (30) reported a moderate correlation of VACO2 with lactate levels at 12 h postoperatively (R2 = 0.59, p < 0.001), the correlation became weaker when analyzing the total number of sample collected (R2 = 0.25, p < 0.001). The moderate correlation of VACO2 with O2ER but not with lactate levels could be because O2ER and VACO2 change faster than lactate levels in response to circulatory flow changes.
To our knowledge, this is the first prospective study involving rigorous VACO2, O2ER, and lactate level assessment at multiple time points following open-heart surgery in a pediatric population. Although this study involved only 127 pediatric patients, the sample size was larger than previous studies. However, it has some limitations. First, the study encompassed a wide variety of patients in terms of age, cardiac abnormalities, and surgical procedures, potentially diluting the significance of the results. Subgroup analysis was performed and remained insignificant different outcomes. The power could be enhanced by increasing the sample size to perform subgroup analyses. Second, the applicability of the gold standard method such as thermodilution method via Swan–Ganz catheterization or transesophageal echocardiography for diagnosing LCOS is limited to children, especially in postoperative states. There has been no consensus on the diagnostic criteria for LCOS in the pediatric population yet. The composite criteria we had set would identify the closest consequences from LCOS. Therefore, we are unable to endorse utilizing the VACO2 as the bedside parameter in children who have undergone cardiac surgery with CPB, as there has not been strong evidence from the prospective study.
5 Conclusions
High level of VACO2 was not significantly associated with LCOS-related outcomes in children who underwent cardiac surgery with CPB. However, a persistently high VACO2 at 6 h postoperatively was related to prolonged inotropic use and a prolonged ICU stay. Further research on VACO2 as an adjunctive diagnostic parameter by combining with lactate level might improve diagnostic accuracy.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Human Research Ethics Unit, Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
PC: Data curation, Writing – original draft, Writing – review & editing. JJ: Writing – review & editing. KS: Supervision, Writing – review & editing. PD: Writing – review & editing. PV: Formal analysis, Methodology, Writing – review & editing. PP: Conceptualization, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was financially supported by the Faculty of Medicine, Prince of Songkla University (grant number 64-087-2).
Acknowledgments
We would like to thank Jirawan Jayuphan, Statistician, Department of Epidemiology, Faculty of Medicine, Prince of Songkla University, for their assistance with the data analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2025.1536089/full#supplementary-material
Abbreviations
AUC, area under the curve; CPB, cardiopulmonary bypass; CI, confidence interval; CO, cardiac output; CO2, carbon dioxide; ECMO, extracorporeal membrane oxygenation; IFDs, ICU-free days; IQR, interquartile range; LCOS, low-cardiac-output syndrome; O2ER: oxygen extraction ratio; PICU, pediatric intensive care unit; RACHS, Risk Adjustment for Congenital Heart Surgery; VACO2, venous-arterial carbon dioxide partial pressure difference; VFDs, ventilator-free days; VIS, vasoactive-inotropic score.
References
1. Shekerdemian L. Perioperative manipulation of the circulation in children with congenital heart disease. Heart. (2009) 95:1286–96. doi: 10.1136/hrt.2005.069237
2. Schoonen A, van Klei WA, van Wolfswinkel L, van Loon K. Definitions of low cardiac output syndrome after cardiac surgery and their effect on the incidence of intraoperative LCOS: a literature review and cohort study. Front Cardiovasc Med. (2022) 9:926957. doi: 10.3389/fcvm.2022.926957
3. Wernovsky G, Wypij D, Jonas RA, Mayer JE, Hanley FL, Hickey PR, et al. Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants. A comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation. (1995) 92:2226–35. doi: 10.1161/01.cir.92.8.2226
4. Fuller BM, Dellinger RP. Lactate as a hemodynamic marker in the critically ill. Curr Opin Crit Care. (2012) 18:267–72. doi: 10.1097/MCC.0b013e3283532b8a
5. Mallat J, Lemyze M, Tronchon L, Vallet B, Thevenin D. Use of venous-to-arterial carbon dioxide tension difference to guide resuscitation therapy in septic shock. World J Crit Care Med. (2016) 5:47–56. doi: 10.5492/wjccm.v5.i1.47
6. Hernández G, Ospina-Tascón GA, Damiani LP, Estenssoro E, Dubin A, Hurtado J, et al. Effect of a resuscitation strategy targeting peripheral perfusion status vs serum lactate levels on 28-day mortality among patients with septic shock: the andromeda-SHOCK randomized clinical trial. JAMA. (2019) 321:654–64. doi: 10.1001/jama.2019.0071
7. Sankar JM, Das RR, Kumar UV. Comparison of intermittent versus continuous superior venal caval oxygen saturation monitoring in early goal directed therapy in septic shock: a systematic review. J Pediatr Intensive Care. (2022) 11:267–74. doi: 10.1055/s-0041-1729742
8. Valeanu L, Bubenek-Turconi SI, Ginghina C, Balan C. Hemodynamic monitoring in sepsis-A conceptual framework of macro- and microcirculatory alterations. Diagnostics (Basel). (2021) 11: 1559. doi: 10.3390/diagnostics11091559
9. Ltaief Z, Schneider AG, Liaudet L. Pathophysiology and clinical implications of the veno-arterial PCO2 gap. Crit Care. (2021) 25:318. doi: 10.1186/s13054-021-03671-w
10. Diaztagle Fernández JJ, Rodríguez Murcia JC, Sprockel Díaz JJ. Venous-to-arterial carbon dioxide difference in the resuscitation of patients with severe sepsis and septic shock: a systematic review. Med Intensiva. (2017) 41:401–10. doi: 10.1016/j.medin.2017.03.008
11. Al Duhailib Z, Hegazy AF, Lalli R, Fiorini K, Priestap F, Iansavichene A, et al. The use of central venous to arterial carbon dioxide tension gap for outcome prediction in critically ill patients: a systematic review and meta-analysis. Crit Care Med. (2020) 48:1855–61. doi: 10.1097/CCM.0000000000004578
12. Chen T, Pan T, Luo X, Wang D. High central venous-to-arterial CO2 difference is associated with poor outcomes in patients after cardiac surgery: a propensity score analysis. Shock. (2019) 52:583–9. doi: 10.1097/SHK.0000000000001324
13. Mukai A, Suehiro K, Kimura A, Funai Y, Matsuura T, Tanaka K, et al. Comparison of the venous-arterial CO(2) to arterial-venous O(2) content difference ratio with the venous-arterial CO(2) gradient for the predictability of adverse outcomes after cardiac surgery. J Clin Monit Comput. (2020) 34:41–53. doi: 10.1007/s10877-019-00286-z
14. Moussa MD, Durand A, Leroy G, Vincent L, Lamer A, Gantois G, et al. Central venous-to-arterial PCO2 difference, arteriovenous oxygen content and outcome after adult cardiac surgery with cardiopulmonary bypass: a prospective observational study. Eur J Anaesthesiol. (2019) 36:279–89. doi: 10.1097/EJA.0000000000000949
15. Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg. (2002) 123:110–8. doi: 10.1067/mtc.2002.119064
16. Gaies MG, Jeffries HE, Niebler RA, Pasquali SK, Donohue JE, Yu S, et al. Vasoactive-inotropic score is associated with outcome after infant cardiac surgery: an analysis from the pediatric cardiac critical care consortium and virtual PICU system registries. Pediatr Crit Care Med. (2014) 15:529–37. doi: 10.1097/PCC.0000000000000153
17. Kellum JA, Lameire N, KDIGO AKI Guideline Work Group, Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (part 1). Crit Care. (2013) 17:204. doi: 10.1186/cc11454
18. Akamatsu T, Inata Y, Tachibana K, Hatachi T, Takeuchi M. Elevated central venous to arterial CO2 difference is not associated with poor clinical outcomes after cardiac surgery with cardiopulmonary bypass in children. Pediatr Crit Care Med. (2017) 18:859–62. doi: 10.1097/PCC.0000000000001229
19. Rhodes LA, Erwin WC, Borasino S, Cleveland DC, Alten JA. Central venous to arterial CO2 difference after cardiac surgery in infants and neonates. Pediatr Crit Care Med. (2017) 18:228–33. doi: 10.1097/PCC.0000000000001085
20. Gong X, Zhu L, Liu Y, Li C, Zhang M, Zhang H, et al. Elevated arterial-central venous carbon dioxide partial pressure difference indicates poor prognosis in the early postoperative period of open heart surgery in infants with congenital heart disease. Pediatr Cardiol. (2021) 42:1601–6. doi: 10.1007/s00246-021-02646-6
21. Guinot PG, Badoux L, Bernard E, Abou-Arab O, Lorne E, Dupont H. Central venous-to-arterial carbon dioxide partial pressure difference in patients undergoing cardiac surgery is not related to postoperative outcomes. J Cardiothorac Vasc Anesth. (2017) 31:1190–6. doi: 10.1053/j.jvca.2017.02.015
22. Huette P, Beyls C, Mallat J, Martineau L, Besserve P, Haye G, et al. Central venous-to-arterial CO2 difference is a poor tool to predict adverse outcomes after cardiac surgery: a retrospective study. Can J Anaesth. (2021) 68:467–76. doi: 10.1007/s12630-020-01881-4
23. Morel J, Grand N, Axiotis G, Bouchet JB, Faure M, Auboyer C, et al. High veno-arterial carbon dioxide gradient is not predictive of worst outcome after an elective cardiac surgery: a retrospective cohort study. J Clin Monit Comput. (2016) 30:783–9. doi: 10.1007/s10877-016-9855-3
24. Habicher M, von Heymann C, Spies CD, Wernecke KD, Sander M. Central venous-arterial pCO2 difference identifies microcirculatory hypoperfusion in cardiac surgical patients with normal central venous oxygen saturation: a retrospective analysis. J Cardiothorac Vasc Anesth. (2015) 29:646–55. doi: 10.1053/j.jvca.2014.09.006
25. Zante B, Reichenspurner H, Kubik M, Schefold JC, Kluge S. Increased admission central venous-arterial CO2 difference predicts ICU-mortality in adult cardiac surgery patients. Heart Lung. (2019) 48:421–7. doi: 10.1016/j.hrtlng.2019.05.015
26. Saludes P, Proença L, Gruartmoner G, Enseñat L, Pérez-Madrigal A, Espinal C, et al. Central venous-to-arterial carbon dioxide difference and the effect of venous hyperoxia: a limiting factor, or an additional marker of severity in shock? J Clin Monit Comput. (2017) 31:1203–11. doi: 10.1007/s10877-016-9954-1
27. Mallat J, Mohammad U, Lemyze M, Meddour M, Jonard M, Pepy F, et al. Acute hyperventilation increases the central venous-to-arterial pCO2 difference in stable septic shock patients. Ann Intensive Care. (2017) 7:31. doi: 10.1186/s13613-017-0258-5
28. Singh G, Pujara J, Trivedi V, Uday DD, Masaniya J, Babu MJ, et al. Correlation of venous to arterial carbon dioxide partial pressure difference with other cardiac output indices in patients undergoing intracardiac repair for tetralogy of fallot. Ann Card Anaesth. (2023) 26:171–6. doi: 10.4103/aca.aca_53_22
29. Bouchacourt JP, Hurtado FJ, Kohn E, Illescas L, Dubin A, Riva JA. Role of Pv–aCO2 gradient and Pv–aCO2/Ca-vO2 ratio during cardiac surgery: a retrospective observational study. Braz J Anesthesiol. (2023) 73:611–9. doi: 10.1016/j.bjane.2021.07.025
30. Castañuela-Sánchez V, García-Benítez L, Hernández-Suárez A, Díaz-García L, Zamora-Arámburo M, Sánchez-Cervantes A, et al. Central venous-to-arterial CO2 difference as a biomarker of outcome in children who underwent surgery for congenital heart disease. Bol Med Hosp Infant Mex. (2023) 80:253–9. doi: 10.24875/BMHIM.23000066
Keywords: cardiopulmonary bypass, carbon dioxide, congenital heart disease, post-operative period, cardiac surgery, venoarterial CO2 difference, children
Citation: Chaiwiriyawong P, Jarutach J, Saelim K, Duangpakdee P, Vichitkunakorn P and Prasertsan P (2025) Association of the central venous-to-arterial carbon dioxide difference with low cardiac output-related outcomes after cardiac surgery in children: a prospective cohort study. Front. Pediatr. 13:1536089. doi: 10.3389/fped.2025.1536089
Received: 28 November 2024; Accepted: 12 May 2025;
Published: 23 May 2025.
Edited by:
Daniel De Wolf, Ghent University Hospital, BelgiumReviewed by:
Shubhadeep Das, Narayana Superspeciality Hospital, IndiaBrian Mendel, National Cardiovascular Center Harapan Kita, Indonesia
Copyright: © 2025 Chaiwiriyawong, Jarutach, Saelim, Duangpakdee, Vichitkunakorn and Prasertsan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pharsai Prasertsan, cGhhcnNhaV8xNkB5YWhvby5jb20=
 Pornnicha Chaiwiriyawong
Pornnicha Chaiwiriyawong Jirayut Jarutach
Jirayut Jarutach Kantara Saelim
Kantara Saelim Pongsanae Duangpakdee2
Pongsanae Duangpakdee2 Polathep Vichitkunakorn
Polathep Vichitkunakorn Pharsai Prasertsan
Pharsai Prasertsan