- 1Pharmaceutical Care Services, King Abdullah Bin Abdulaziz University Hospital, Riyadh, Saudi Arabia
- 2College of Pharmacy, Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia
- 3Children's Health Department, King Abdullah Bin Abdulaziz University Hospital, Riyadh, Saudi Arabia
- 4College of Medicine, Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia
- 5Department of Pediatrics, Faculty of Medicine, University of Ottawa, Ottawa, ON, Canada
- 6Newborn Care, Children's Hospital of Eastern Ontario, Ottawa, ON, Canada
- 7NICU Division, Children's Health Department, King Abdullah Bin Abdulaziz University Hospital, Riyadh, Saudi Arabia
Background: A multidrug-resistant pathogen increasingly seen in newborn intensive care units, stenotrophomonas maltophilia presents treatment difficulties for preterm babies.
Case presentation: A 28-week preterm neonate developed S. maltophilia sepsis following prolonged mechanical ventilation. Initial therapy with trimethoprim- sulfamethoxazole (TMP-SMX) was ineffective, prompting a switch to levofloxacin, which led to clinical recovery and infection clearance.
Conclusion: This case highlights the need for tailored antimicrobial strategies in neonatal S. maltophilia infections. Sequential therapy with TMP-SMX and levofloxacin was effective, supporting the judicious use of fluoroquinolones in resistant cases.
Introduction
Preterm neonates face an increased risk of nosocomial infections due to their immunologic immaturity, low birth weight, and frequent exposure to invasive medical procedures such as intravascular catheterization and mechanical ventilation (1). These vulnerabilities lead to the emergence of multidrug-resistant organisms, complicating clinical management and raising morbidity and mortality (2).
Stenotrophomonas maltophilia is an opportunistic gram-negative aerobic bacillus that has emerged as a significant nosocomial pathogen, particularly in immunocompromised individuals, including neonates (3). Its intrinsic resistance to multiple classes of antibiotics presents a considerable challenge in clinical practice (4). Infections caused by S. maltophilia can impact various organ systems, including the bloodstream, respiratory tract, urinary tract, and central nervous system, with pneumonia and sepsis being the most common presentations in neonates (5).
The management of S. maltophilia infections in neonates is further complicated by limited pharmacokinetic data and safety concerns regarding effective antimicrobial agents (5). This case report highlights the successful sequential use of trimethoprim- sulfamethoxazole (TMP-SMX) followed by levofloxacin in the treatment of a preterm neonate with S. maltophilia sepsis.
Case presentation
A female preterm neonate was delivered at 28 weeks and 2 days of gestation via emergency cesarean section, necessitated by maternal antepartum hemorrhage. She was admitted to the neonatal intensive care unit (NICU) because of respiratory distress syndrome, necessitating mechanical ventilation. On the 17th day of life, the newborn exhibited clinical deterioration following a video laryngoscopic evaluation for suspected difficult intubation, probably due to aspiration.
Empirical treatment involving cloxacillin and gentamicin was commenced, yet there was no observed clinical improvement. Meropenem, gentamicin, and vancomycin were incorporated into the antibiotic regimen, leading to a temporary stabilization of the patient. Tracheal aspirate culture revealed the presence of Stenotrophomonas maltophilia and Acinetobacter baumannii. After consulting with infectious disease specialists, the decision was made to discontinue vancomycin. Instead, a regimen of ceftazidime along with trimethoprim-sulfamethoxazole (TMP-SMX) was initiated at a dosage of 12 mg/kg every 8 h for a period of 10 days. Prior to initiating TMP- SMX, both total and direct serum bilirubin levels were within normal ranges. Daily monitoring during the first three days, followed by assessments every other day, showed no significant changes.
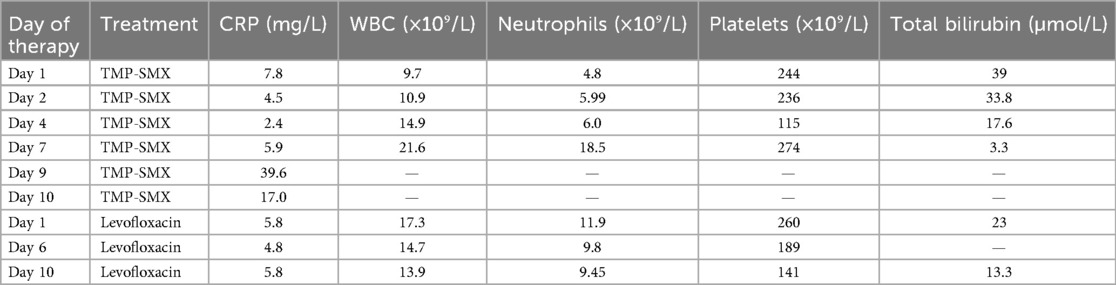
Even after finishing the TMP-SMX treatment, later tracheal aspirates still showed positive results for S. maltophilia, along with increasing oxygen requirements. As a result, levofloxacin was initiated at a dosage of 10 mg/kg twice daily for a duration of 10 days, leading to notable clinical improvement and negative follow-up cultures, thereby confirming the eradication of the infection. Throughout the hospitalization, blood cultures consistently returned negative results. The laboratory findings during TMP-SMX and levofloxacin therapy are summarized in Table 1.
Discussion
This case highlights the complexities involved in managing S. maltophilia infections in preterm neonates, especially those requiring prolonged respiratory support. The sequential approach, starting with TMP-SMX followed by levofloxacin, was guided by clinical response and microbiological data. Although TMP-SMX is the first-line therapy for S. maltophilia infections, treatment failures are not uncommon, particularly in severe or persistent cases (6).
The intrinsic resistance of S. maltophilia to multiple antibiotics necessitates a tailored, susceptibility-guided therapeutic strategy. While fluoroquinolones like levofloxacin are not typically first-line agents in neonates due to concerns about cartilage toxicity, emerging evidence supports their role in multidrug-resistant (MDR) S. maltophilia infections when conventional treatments fail (7). Our findings are consistent with the recent case series by Verma et al., which reported an 80% success rate among five preterm neonates with S. maltophilia sepsis (8). In their series, only one patient received TMP-SMX alone, while the others were treated with levofloxacin alone (three cases), levofloxacin plus amikacin (one case), or minocycline plus amikacin and TMP-SMX (one case). These findings highlight the variable use of TMP-SMX and the potential role of fluoroquinolones, either alone or in combination, as effective options in challenging cases. The evidence from recent neonatal studies and case reports on treatment efficacy for S. maltophilia infections is summarized in Table 2.
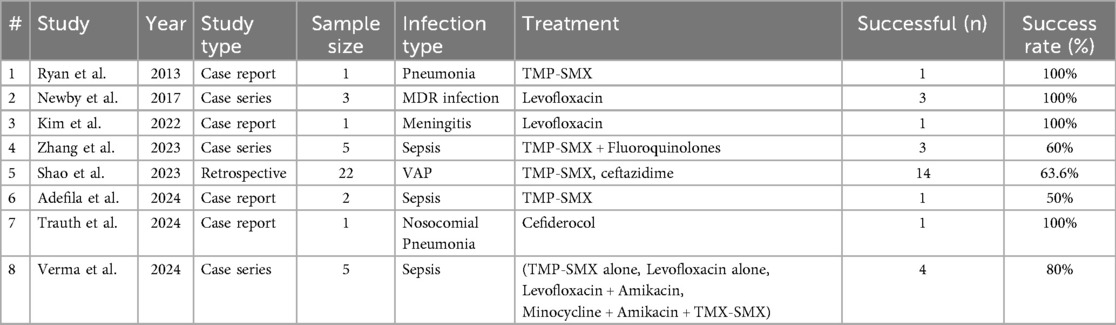
Table 2. Summarizes the evidence from recent neonatal studies and case reports on treatment efficacy for S. maltophilia infections.
Emerging literature demonstrates the successful use of alternative therapies in neonatal S. maltophilia infections. Adefila et al. reported a case successfully treated with a tailored antimicrobial approach guided by local antibiogram data (9). Similarly, cefiderocol has been explored as a novel treatment strategy, although limited clinical data and availability constraints may restrict its widespread use in NICUs (10).
Although the pharmacokinetics of levofloxacin in neonates have not been extensively studied, available data suggest adequate tissue penetration and bactericidal activity against S. maltophilia. In this case, levofloxacin was well-tolerated, with no immediate or delayed adverse effects observed. The cautious use of fluoroquinolones and close monitoring for potential side effects remains essential in optimizing outcomes and minimizing risks.
Conclusions
This case report illustrates the successful sequential antibiotic therapy for S. maltophilia infection in a preterm neonate. Early recognition, appropriate antibiotic selection, and adjustments based on clinical and microbiological data were crucial in achieving a favorable outcome. Sequential therapy with TMP-SMX followed by levofloxacin represents an effective strategy for managing MDR S. maltophilia infections in neonates. This case underscores the importance of individualized, evidence-based approaches in managing complex neonatal infections.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the patient’s legal guardian for the publication of any potentially identifiable data and images included in this article.
Author contributions
MN: Writing – original draft, Writing – review & editing. MA: Writing – review & editing. SM: Writing – original draft, Writing – review & editing. MF: Writing – review & editing. YB: Writing – review & editing. NA: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ramasethu J. Prevention and treatment of neonatal nosocomial infections. Matern Health Neonatol Perinatol. (2017) 3:1. doi: 10.1186/s40748-017-0043-3
2. Flannery DD, Chiotos K, Gerber JS, Puopolo KM. Neonatal multidrug-resistant gram-negative infection: epidemiology, mechanisms of resistance, and management. Pediatr Res. (2022) 91(2):380–91. doi: 10.1038/s41390-021-01745-7
3. Said MS, Tirthani E, Lesho E. Stenotrophomonas Maltophilia. In: StatPearls. Treasure Island, FL: StatPearls Publishing (2023).
4. Looney WJ, Narita M, Mühlemann K. Stenotrophomonas maltophilia: an emerging opportunist human pathogen. Lancet Infect Dis. (2009) 9(5):312–23. doi: 10.1016/S1473-3099(09)70083-0
5. Brooke JS. Advances in the microbiology of Stenotrophomonas maltophilia. Clin Microbiol Rev. (2021) 34(3):10–128. doi: 10.1128/CMR.00030-19
6. Ryan KL, Dersch-Mills D, Clark D. Trimethoprim–sulfamethoxazole for treatment of Stenotrophomonas maltophilia pneumonia in a neonate. Can J Hosp Pharm. (2013) 66(6):384. doi: 10.4212/cjhp.v66i6.1305
7. Newby BD, Timberlake KE, Lepp LM, Mihic T, DA D-M. Levofloxacin use in the neonate: a case series. J Pediatr Pharmacol Ther. (2017) 22(4):304–13. doi: 10.5863/1551-6776-22.4.304
8. Verma A, Patnaik SK, Suryawanshi P. Stenotrophomonas maltophilia sepsis in preterm neonates. Med J Armed Forces India. (2024) 80:S268–71. doi: 10.1016/j.mjafi.2023.01.010
9. Adefila WO, Osie I, Keita ML, Wutor BM, Yusuf AO, Hossain I, et al. Stenotrophomonas maltophilia neonatal sepsis: a case report. J Med Case Rep. (2024) 18(1):180. doi: 10.1186/s13256-024-04479-2
Keywords: Stenotrophomonas maltophilia, neonatal sepsis, multidrug resistance, trimethoprim-sulfamethoxazole, levofloxacin
Citation: Nahari M, Alaboud M, Mohinuddin S, Faden M, Balhareth Y and Alsaleem N (2025) Successful sequential therapy for Stenotrophomonas maltophilia infection in a preterm neonate: a case report. Front. Pediatr. 13:1619075. doi: 10.3389/fped.2025.1619075
Received: 27 April 2025; Accepted: 19 August 2025;
Published: 4 September 2025.
Edited by:
Bülent Taner Karadağ, Marmara University, TürkiyeReviewed by:
Suprabha K. Patnaik, Bharati Vidyapeeth’s Medical College, IndiaArjun Verma, Mahatma Gandhi Medical College and Hospital, India
Deniz Kızılırmak, Manisa Celal Bayar University, Türkiye
Copyright: © 2025 Nahari, Alaboud, Mohinuddin, Faden, Balhareth and Alsaleem. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Majed Nahari, cGgubWFqZWQxNDE0QGdtYWlsLmNvbQ==
 Majed Nahari
Majed Nahari Mohammed Alaboud3,4
Mohammed Alaboud3,4