- Pediatric Intensive Care Unit, The Second Hospital of Hebei Medical University, Shijiazhuang, China
Objective: To investigate the clinical characteristics and risk factors associated with mortality in pediatric sepsis patients, and to establish a predictive model for early identification of high-risk children.
Methods: A retrospective cohort study was conducted including 143 pediatric sepsis cases admitted to the Pediatric Intensive Care Unit of the Second Hospital of Hebei Medical University from January 2020 to December 2024. Clinical data, laboratory indicators, and treatment history were collected. Univariate and multivariate logistic regression analyses were performed to identify risk factors for mortality. A nomogram model was constructed based on significant predictors, and its predictive performance was evaluated by receiver operating characteristic (ROC) curve analysis.
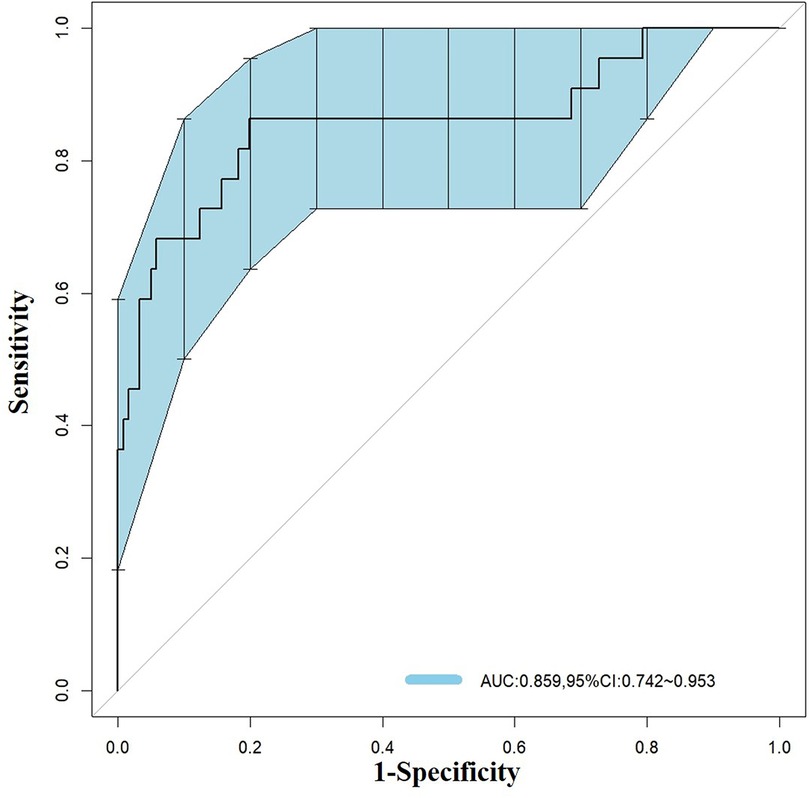
Results: Among the 143 cases, 121 survived and 22 died. Significant differences were observed between the survival and death groups in lymphocyte count, platelet count, albumin, D-dimer, liver function tests (ALT, TBIL), CALLY index, and pre-admission glucocorticoid use (P < 0.05). Multivariate analysis identified platelet count (OR = 0.992, 95% CI: 0.987–0.997), D-dimer (OR = 7.571, 95% CI: 2.642–21.698), and CALLY index (OR = 0.532, 95% CI: 0.323–0.877) as independent risk factors for mortality. The nomogram model incorporating these factors showed good predictive accuracy with an area under the ROC curve of 0.859 (95% CI = 0.742–0.953).
Conclusion: Platelet count, D-dimer level, and CALLY index are valuable indicators for assessing prognosis in pediatric sepsis and can aid in early risk stratification. The established nomogram provides a useful tool for clinical decision-making to improve outcomes in high-risk pediatric sepsis patients. Further multicenter prospective studies are warranted to validate and refine these findings.
1 Introduction
Sepsis is a life-threatening organ dysfunction caused by a dysregulated host immune response to infection and has become one of the leading causes of mortality among pediatric patients in pediatric intensive care units (PICUs) worldwide (1, 2). Despite significant advances in anti-infective therapies and intensive care technologies in recent years, the incidence and mortality rates of pediatric sepsis remain unacceptably high (3). The disease is characterized by high clinical heterogeneity and rapid progression, posing major challenges for early diagnosis and prognostic evaluation (4, 5). Therefore, timely identification of high-risk children with sepsis at an early stage of the disease has become a critical issue for clinicians.
The C-reactive protein–albumin–lymphocyte (CALLY) index is a novel composite biomarker that integrates three routinely measured laboratory parameters—C-reactive protein (CRP), serum albumin, and absolute lymphocyte count—into a single score, calculated as (lymphocyte count × albumin)/CRP. This index simultaneously reflects systemic inflammation, nutritional and hepatic status, and immune competence, all of which are closely linked to sepsis pathophysiology and prognosis (6). Originally proposed and validated in adult populations with liver disease, cancer, and systemic inflammatory conditions, the CALLY index has recently been investigated as a prognostic marker in sepsis, showing promising predictive value for mortality and adverse outcomes (7–9). However, its applicability in pediatric sepsis remains largely unexplored. Given that children with sepsis often present with unique immune responses and disease trajectories compared to adults, we hypothesized that the CALLY index might serve as a practical and readily obtainable tool for early risk stratification in pediatric patients. Therefore, we incorporated the CALLY index into our analysis to evaluate its prognostic performance in this population.
In this study, we conducted a retrospective cohort analysis of 143 pediatric sepsis patients admitted to the Pediatric Intensive Care Unit of the Second Hospital of Hebei Medical University between January 2020 and December 2024. Based on the international diagnostic criteria for pediatric sepsis (10), we systematically summarized the clinical profile of these patients and identified independent risk factors significantly associated with mortality through multivariate regression analysis. The findings of this study aim to provide an objective and quantitative basis for the early identification of high-risk pediatric sepsis cases in clinical practice. We hypothesized that certain laboratory parameters, particularly the CALLY index, platelet count, and D-dimer level, are independently associated with mortality in pediatric sepsis and can be used to develop a predictive model for early risk stratification.
2 Methods
2.1 Study population
This study adopted a retrospective cohort design and included 143 pediatric patients diagnosed with sepsis who were admitted to the PICU of the Second Hospital of Hebei Medical University between January 2020 and December 2024.
Inclusion criteria: (1) Age between 28 days and 14 years. This age range was chosen because, in our institution, patients older than 14 years are generally admitted to the adult ICU, while neonates (≤28 days) are admitted to the Neonatal Intensive Care Unit (NICU) for specialized management; (2) Complete clinical medical records; (3) Diagnosis consistent with the 2012 international pediatric sepsis criteria (6).
Exclusion criteria: (1) Age >14 years or ≤28 days; (2) Incomplete clinical data; (3) Length of hospital stay <24 h; (4) For patients with multiple hospitalizations due to sepsis, only the first admission was included for analysis.
Patients were divided into the survival group and the non-survival group based on their discharge outcomes.
This study was approved by the Ethics Committee of the Second Hospital of Hebei Medical University (Approval No. 2024-R253).
2.2 Data collection
The following clinical data were extracted from the hospital's electronic medical record system: (1) Baseline characteristics: age, sex, and comorbidities (e.g., hematologic malignancies, congenital anomalies); (2) Treatment-related factors: history of glucocorticoid use within 30 days prior to admission, central venous catheterization, mechanical ventilation, and other interventions; (3) Laboratory parameters: inflammatory markers (WBC, CRP, PCT) measured within 24 h of admission; immune function indicators (lymphocyte subsets, immunoglobulins); coagulation parameters (D-dimer, APTT, PT); liver and kidney function tests (ALT, AST, creatinine); and blood culture results.
If a parameter was measured multiple times within the first 24 h, the value closest to the time of PICU admission was recorded to best reflect the patient's baseline status before the influence of treatment interventions. The CALLY index was calculated using the following formula: CALLY = (absolute lymphocyte count × albumin)/CRP (11).
2.3 Statistical analysis
Statistical analyses were performed using SPSS version 24.0 and R version 4.3.2. For continuous variables with a normal distribution, data were expressed as mean ± standard deviation and compared between groups using the t-test. For non-normally distributed continuous variables, data were presented as median and interquartile range (IQR), and the Mann–Whitney U test was used for group comparisons. Categorical variables were expressed as frequency and percentage (%), and compared using the chi-square test. Variables with statistically significant differences in univariate analysis were included in univariate and multivariate logistic regression models. The results were reported as odds ratios (ORs), 95% confidence intervals (CIs), and P-values. Statistically significant variables from the multivariate logistic regression were used to construct a nomogram and receiver operating characteristic (ROC) curve. To assess internal validity and minimize optimism bias, model performance was further evaluated using bootstrapping with 1,000 resamples, and the optimism-corrected AUC was calculated. All statistical tests were two-tailed, and a P-value < 0.05 was considered statistically significant.
3 Results
3.1 Clinical characteristics of the two groups
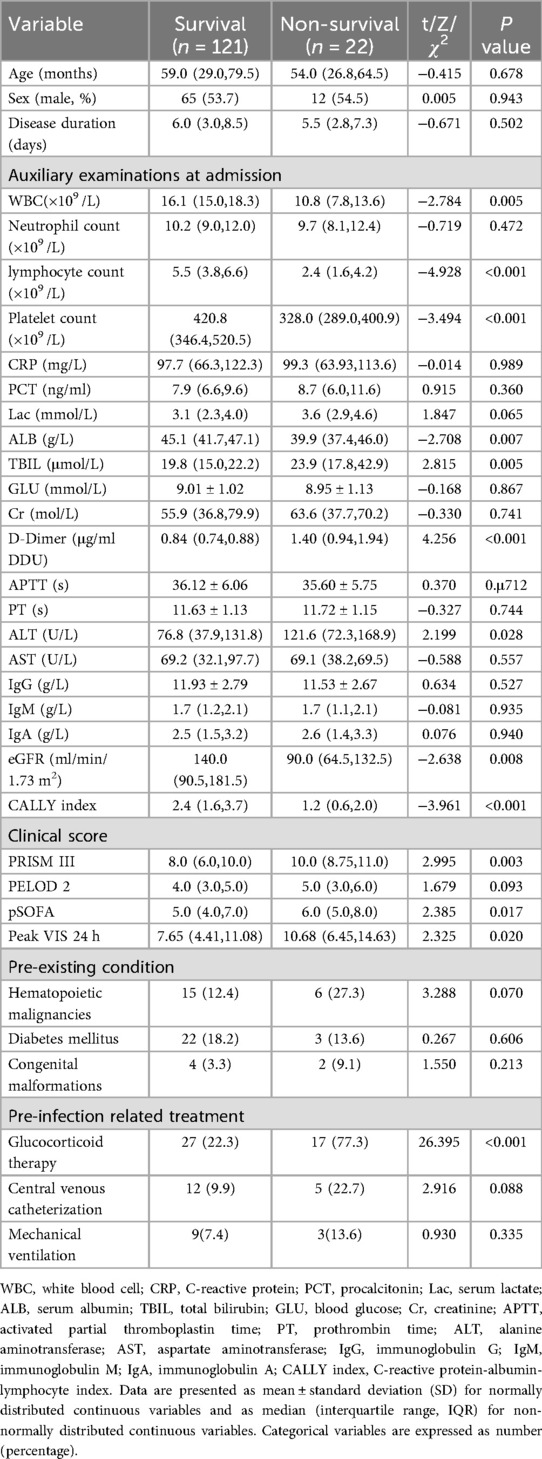
A total of 143 pediatric patients with sepsis were included in this study, of whom 121 survived and 22 died. Significant differences were observed between the survival and non-survival groups in terms of white blood cell count (WBC), lymphocyte count, platelet count, albumin (ALB), total bilirubin (TBIL), D-dimer, alanine aminotransferase (ALT), estimated glomerular filtration rate (eGFR), clinical severity scores (PRISM III and pSOFA), vasoactive-inotropic score (VIS), CALLY index, and prior use of glucocorticoids before hospitalization (P < 0.05). No statistically significant differences were found in age, sex, disease duration, neutrophil count, or PELOD-2 score between the two groups (P > 0.05) (Table 1).
3.2 Risk factor analysis for mortality in pediatric sepsis patients
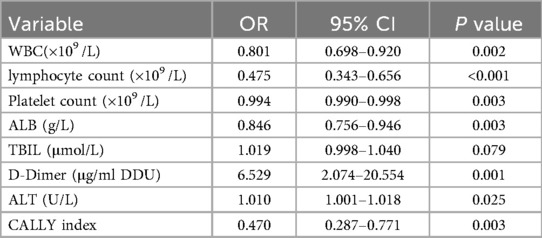
Univariate logistic regression analysis was performed for WBC, lymphocyte count, platelet count, ALB, TBIL, D-dimer, ALT, and CALLY index. The results indicated that WBC, lymphocyte count, platelet count, ALB, D-dimer, ALT, and CALLY index were significantly associated with mortality in pediatric sepsis patients (Table 2).
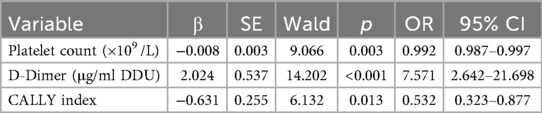
Considering the strong correlations of WBC, lymphocyte count, ALB, and ALT with the CALLY index, only variables with statistical significance in univariate analysis were included in the multivariate logistic regression model. The results showed that platelet count (OR = 0.992, 95% CI: 0.987–0.997), D-dimer (OR = 7.571, 95% CI: 2.642–21.698), and CALLY index (OR = 0.532, 95% CI: 0.323–0.877) were independent risk factors for mortality in pediatric sepsis patients (Table 3).
3.3 Development of a mortality risk model for pediatric sepsis patients
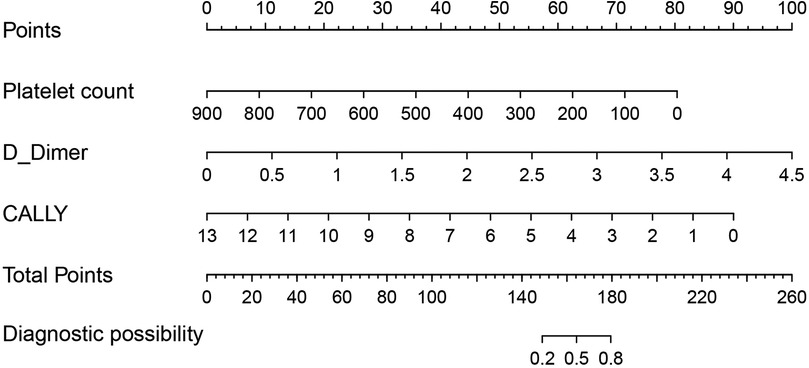
Based on the three factors identified by multivariate logistic regression analysis, a nomogram model was constructed (Figure 1). The total score, obtained by summing the points assigned to each predictive factor, corresponds to the probability of mortality risk in pediatric sepsis patients. The predictive performance of the nomogram model was evaluated using the ROC curve, which showed an area under the curve (AUC) of 0.859 (95% CI = 0.742–0.953), indicating good predictive accuracy (Figure 2).
4 Discussion
This study retrospectively analyzed the clinical data of 143 pediatric sepsis patients admitted to the Pediatric Intensive Care Unit of Hebei Medical University Second Hospital, comparing multiple clinical indicators between the survival and non-survival groups. Significant differences were observed in peripheral blood white blood cell count, lymphocyte count, platelet count, albumin, total bilirubin, D-dimer, ALT, CALLY index, and prior use of glucocorticoids before hospitalization. These findings suggest that these indicators may be closely associated with the prognosis of pediatric sepsis patients. Notably, patients in the non-survival group generally exhibited lower lymphocyte counts, platelet counts, and albumin levels, alongside higher levels of D-dimer and total bilirubin, reflecting more severe immunosuppression, coagulation dysfunction, and liver injury. The CALLY index, as a novel composite indicator reflecting nutritional and hepatic status, also demonstrated a certain discriminative ability in this study (11–13). Further regression analyses and the mortality risk prediction model indicated that platelet count, D-dimer level, and CALLY index could serve as important early reference markers for identifying high-risk pediatric sepsis patients, providing strong support for clinical risk assessment and early intervention.
The results of this study are consistent with previous research on both pediatric and adult sepsis in several aspects (14, 15). The more pronounced decrease in lymphocyte count observed in the non-survival group aligns with studies highlighting immunosuppression during severe infections (16, 17). Demonstrated that increased lymphocyte apoptosis and impaired T cell function in septic children are key mechanisms contributing to immune dysregulation and elevated mortality (18, 19). Additionally, the significantly elevated D-dimer levels in the non-survival group suggest the presence of coagulation dysfunction, which is consistent with findings in adult sepsis where D-dimer serves as an independent risk factor for poor prognosis (20, 21). This study also found that albumin levels were significantly lower in the non-survival group compared to the survival group, indicating its potential role as an early warning marker reflecting nutritional status and systemic inflammation, which aligns with multiple reports identifying hypoalbuminemia as a prognostic indicator of adverse outcomes in sepsis (22, 23). In addition to being a marker of chronic nutritional deficiency, hypoalbuminemia in sepsis also reflects endothelial dysfunction, vascular hyperpermeability, and capillary leak, all of which contribute to intravascular volume depletion, tissue edema, and organ dysfunction (24). These mechanisms may partly explain the strong association between low albumin levels and poor prognosis in septic patients.
Notably, this study also found a higher proportion of glucocorticoid use prior to hospitalization in the non-survival group, which may be related to their more severe underlying diseases and more complex immune status. Although glucocorticoids exhibit anti-inflammatory effects in certain severe infections, previous studies have indicated that inappropriate use may delay infection control and increase the risk of secondary infections, thereby adversely affecting prognosis (25, 26). Additionally, elevated liver function indicators such as ALT and TBIL suggest that the septic process may involve hepatic injury, reflecting a trend toward multi-organ dysfunction, which has also been reported in previous studies (27).
In this study, a lower CALLY index was significantly associated with increased mortality among pediatric patients with sepsis, highlighting its potential role as a prognostic biomarker in this population. The CALLY index, which integrates serum albumin, lymphocyte count, and C-reactive protein levels, provides a composite reflection of nutritional status, immune competence, and systemic inflammation—three key elements intricately linked to sepsis progression and outcomes (7, 28). Although originally developed and validated in adult populations with liver disease and systemic inflammatory conditions, our findings suggest that the CALLY index may also have meaningful clinical applicability in pediatric sepsis. Its ability to synthesize multiple clinically relevant parameters into a single, easily obtainable index makes it a practical tool for early risk stratification and outcome prediction. As such, the incorporation of the CALLY index into pediatric sepsis assessment protocols could assist clinicians in identifying high-risk patients more efficiently and guiding timely intervention strategies. Further multicenter and prospective studies are warranted to validate its utility and optimize its thresholds in the pediatric setting.
The findings of this study have important implications for clinical practice. By identifying key clinical indicators that affect the prognosis of pediatric sepsis—such as lymphocyte count, platelet count, albumin, D-dimer, and liver function-related markers—clinicians can perform early risk stratification upon admission. This enables more targeted monitoring and intervention. Especially in cases of pediatric sepsis with rapid disease progression and atypical symptoms, integrating these laboratory parameters into a comprehensive assessment can improve the sensitivity of early detection, shorten diagnostic time, and optimize treatment strategies (29). The CALLY index, as an easily obtainable composite biochemical index, demonstrated predictive value in this study, indicating its potential utility in risk assessment for pediatric sepsis and warranting further clinical validation and broader application (30).
In our PICU, immunoglobulin levels are routinely measured in all patients with suspected sepsis as part of the initial laboratory evaluation. In the present study, these parameters did not differ significantly between survivors and non-survivors. This may indicate that humoral immunity, as reflected by immunoglobulin concentrations, remains relatively preserved in pediatric sepsis, whereas cellular immunity—particularly T-lymphocyte-mediated responses—may be more significantly impaired. The pronounced lymphopenia observed in the non-survival group supports this possibility. Previous studies have shown that sepsis can induce profound T-cell depletion, functional exhaustion, and apoptosis, leading to sustained immunosuppression and worse outcomes (31). Therefore, further investigation into T-lymphocyte dynamics and function in pediatric sepsis could provide valuable insights into disease pathophysiology and guide targeted immunomodulatory therapies.
This study suggests that pre-admission use of glucocorticoids may be associated with poor prognosis, indicating that clinicians should exercise greater caution when administering glucocorticoids, especially in cases where infection control status or disease stage is not clearly established. The potential benefits and risks should be carefully evaluated (32, 33). Overall, identifying these quantifiable laboratory indicators not only aids in enhancing early recognition and intervention for critically ill pediatric patients but also provides foundational data to support the development of prognostic models for pediatric sepsis and to advance precision medicine. In the future, integrating these findings into clinical pathways or scoring systems may help improve overall diagnostic and treatment quality and reduce sepsis-related mortality in children.
Although this study systematically analyzed the clinical characteristics and prognostic indicators of pediatric sepsis, providing certain clinical guidance, several limitations remain. First, as a single-center retrospective study with a relatively small sample size, selection bias may be present. Second, this study only included indicators measured during hospitalization and lacked follow-up data on long-term outcomes such as readmission rates and neurological sequelae, which limits the scope of assessing the long-term prognosis of sepsis. Therefore, the conclusions need to be further validated in larger, multicenter prospective studies. In addition, because this was a retrospective analysis, no a priori power calculation was performed. The relatively small number of mortality events means that the sample size may be borderline for the recommended “events per variable” threshold in multivariable logistic regression, which could affect the stability of the model estimates and limit the generalizability of our findings. Nonetheless, this study offers valuable insights for the early assessment and risk identification of pediatric sepsis and lays a foundation for future mechanistic research and clinical translation.
The predictive model developed in this study—incorporating platelet count, D-dimer, and CALLY index—has the potential to facilitate early risk stratification in pediatric sepsis, enabling clinicians to identify patients at highest risk of mortality during the initial stage of PICU admission. Early recognition could allow for closer hemodynamic and laboratory monitoring, more rapid escalation of antimicrobial and organ support therapies, and consideration of adjunctive treatments such as intravenous immunoglobulin (IVIG) or plasma exchange in selected patients. While these aggressive interventions have shown potential benefits in certain adult and pediatric septic populations, robust evidence in the pediatric setting remains limited. Therefore, future multicenter prospective studies should explore whether targeted early application of such therapies, guided by validated risk prediction models, can improve survival and long-term outcomes in high-risk children with sepsis.
5 Conclusion
This study retrospectively analyzed 143 hospitalized pediatric sepsis cases and found that the deceased group showed significant differences compared to the survival group in lymphocyte count, platelet count, albumin, D-dimer, liver function indicators (ALT, TBIL), CALLY index, and pre-hospital use of glucocorticoids. These indicators can serve as important references for assessing the severity and prognosis of pediatric sepsis. In particular, platelet count, CALLY index, and D-dimer level demonstrated good clinical predictive value and hold potential for early identification of high-risk patients and guiding intervention decisions. Despite certain limitations, the findings provide valuable insights for early risk assessment and personalized management of pediatric sepsis in clinical practice. Future studies with larger sample sizes and multicenter prospective designs are needed to further validate these results and to explore additional biomarkers and scoring systems for early warning, aiming to improve the overall diagnosis, treatment, and survival rates of pediatric sepsis.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Second Hospital of Hebei Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
CW: Investigation, Software, Conceptualization, Formal analysis, Writing – original draft. LF: Writing – original draft, Data curation, Methodology. XY: Supervision, Methodology, Writing – original draft. PW: Writing – original draft, Validation, Supervision. YC: Visualization, Funding acquisition, Resources, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the Hebei Province Key R&D Program Projects (20377785D).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Long E, Borland ML, George S, Jani S, Tan E, Phillips N, et al. External validation of the phoenix sepsis score in children with suspected community-acquired sepsis. JAMA Netw Open. (2025) 8:e251412. doi: 10.1001/jamanetworkopen.2025.1412
2. Tian J, Li Q, Cai S, Wang X, Ai J, Feng G, et al. Infection-related mortality in hospitalized children: a multi-center study in China from 2016 to 2021. J Infect Public Heal. (2025) 18:102743. doi: 10.1016/j.jiph.2025.102743
3. Rosenberg DC, Snapiri O, Dizitzer Y, Sachs N, Levy D, Krause I, et al. Community-acquired staphylococcus aureus bacteremia in healthy children-13 years of experience in a pediatric tertiary center. Eur J Pediatr. (2025) 184:233. doi: 10.1007/s00431-025-06069-w
4. Wosten-van AR, la Roi-Teeuw HM, Tissing W, Jordan I, Dohna-Schwake C, Bottari G, et al. The phoenix sepsis score in pediatric oncology patients with sepsis at PICU admission: test of performance in a European multicenter cohort, 2018–2020. Pediatr Crit Care Me. (2025) 26:e177–85. doi: 10.1097/PCC.0000000000003683
5. Sanchez-Pinto LN, Daniels LA, Atreya M, Faustino E, Farris R, Geva A, et al. Phoenix sepsis criteria in critically ill children: retrospective validation using a United States nine-center dataset, 2012–2018. Pediatr Crit Care Me. (2025) 26:e155–65. doi: 10.1097/PCC.0000000000003675
6. Yang M, Lin SQ, Liu XY, Tang M, Hu CL, Wang ZW, et al. Association between C-reactive protein-albumin-lymphocyte (CALLY) index and overall survival in patients with colorectal cancer: from the investigation on nutrition status and clinical outcome of common cancers study. Front Immunol. (2023) 14:1131496. doi: 10.3389/fimmu.2023.1131496
7. Zhu D, Lin YD, Yao YZ, Qi XJ, Qian K, Lin LZ. Negative association of C-reactive protein-albumin-lymphocyte index (CALLY index) with all-cause and cause-specific mortality in patients with cancer: results from NHANES 1999–2018. BMC Cancer. (2024) 24:1499. doi: 10.1186/s12885-024-13261-y
8. Liu XY, Zhang X, Zhang Q, Ruan GT, Liu T, Xie HL, et al. The value of CRP-albumin-lymphocyte index (CALLY index) as a prognostic biomarker in patients with non-small cell lung cancer. Support Care Cancer. (2023) 31:533. doi: 10.1007/s00520-023-07997-9
9. Zhang J, Zhao Q, Liu S, Yuan N, Hu Z. Clinical predictive value of the CRP-albumin-lymphocyte index for prognosis of critically ill patients with sepsis in intensive care unit: a retrospective single-center observational study. Front Public Health. (2024) 12:1395134. doi: 10.3389/fpubh.2024.1395134
10. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intens Care Med. (2013) 39:165–228. doi: 10.1007/s00134-012-2769-8
11. Saridas A, Cetinkaya R. The prognostic value of the CALLY index in sepsis: a composite biomarker reflecting inflammation, nutrition, and immunity. Diagnostics. (2025) 15:1026. doi: 10.3390/diagnostics15081026
12. Radkhah H, Zooravar D, Shateri-Amiri B, Saffar H, Najjari K, Hazaveh MM. Predictive value of complete blood count (CBC)-derived indices-C-reactive-protein-albumin-lymphocyte index (CALLY), glucose-to-lymphocyte ratio (GLR), prognostic nutritional index (PNI), hemoglobin, albumin, lymphocyte, platelet (HALP), and controlling nutritional status (COUNT)-on body composition changes after bariatric surgery. Obes Surg. (2025) 35:544–55. doi: 10.1007/s11695-024-07643-1
13. Lin X, Zhang L, Zheng Y, Hong X, Zheng H, Huang T, et al. A comprehensive prognosis model for adult septic shock: SOFAplusCALLY index. Eur J Med Res. (2025) 30:111. doi: 10.1186/s40001-025-02379-9
14. Chen J, Huang H, Zhang R, Fu Y, Jing C. Risk factors associated with mortality and pathogen characteristics of bloodstream infection-induced severe sepsis in the pediatric intensive care unit: a retrospective cohort study. Front Cell Infect Mi. (2025) 15:1492208. doi: 10.3389/fcimb.2025.1492208
15. Copana-Olmos R, Casson-Rodriguez N, Diaz-Villalobos W, Urquieta-Clavel V, Tejerina-Ortiz M, Mendoza-Montoya C, et al. Sepsis in critically ill children in Bolivia: multicenter retrospective evaluation of the Phoenix criteria for sepsis in a 2023 cohort. Pediatr Crit Care Me. (2025) 26:e699–707. doi: 10.1097/PCC.0000000000003714
16. Charoensappakit A, Sae-Khow K, Vutthikraivit N, Maneesow P, Sriprasart T, Pachinburavan M, et al. Immune suppressive activities of low-density neutrophils in sepsis and potential use as a novel biomarker of sepsis-induced immune suppression. Sci Rep-UK. (2025) 15:9458. doi: 10.1038/s41598-025-92417-7
17. Lu X, Chen Y, Zhang G, Zeng X, Lai L, Qu C. Dynamic immune indicator changes as predictors of ARDS in ICU patients with sepsis: a retrospective study. Int J Gen Med. (2025) 18:1163–72. doi: 10.2147/IJGM.S501252
18. Podd BS, Banks RK, Reeder R, Telford R, Holubkov R, Carcillo J, et al. Early, persistent lymphopenia is associated with prolonged multiple organ failure and mortality in septic children. Crit Care Med. (2023) 51:1766–76. doi: 10.1097/CCM.0000000000005993
19. Kernan KF, Ghaloul-Gonzalez L, Vockley J, Lamb J, Hollingshead D, Chandran U, et al. Prevalence of pathogenic and potentially pathogenic inborn error of immunity associated variants in children with severe sepsis. J Clin Immunol. (2022) 42:350–64. doi: 10.1007/s10875-021-01183-4
20. Wang X, Wei C, He D, Huang D, Zhao Y, Ran L, et al. Incidence and risk factor of sepsis in patients with severe community-acquired pneumonia: a Chinese, single-center, retrospective study. Bmc Infect Dis. (2025) 25:649. doi: 10.1186/s12879-025-11027-w
21. Long X, Hu Z, Song C, Zhang J. Association between D-dimer to lymphocyte ratio and in hospital all-cause mortality in elderly patients with sepsis: a cohort of 1123 patients. Front Cell Infect Mi. (2024) 14:1507992. doi: 10.3389/fcimb.2024.1507992
22. Liu Z, Chen X, Zhang L. A retrospective analysis of the correlation between the glucose-to-albumin ratio and 28-day mortality in sepsis patients. BMC Infect Dis. (2025) 25:715. doi: 10.1186/s12879-025-11092-1
23. Ponce-Orozco O, Vicente-Hernandez B, Ramirez-Ochoa S, Zepeda-Gutierrez LA, Ambriz-Alarcon MA, Cervantes-Guevara G, et al. Prognostic value of the lactate/albumin ratio in sepsis-related mortality: an exploratory study in a tertiary care center with limited resources in Western Mexico. J Clin Med. (2025) 14:2825. doi: 10.3390/jcm14082825
24. Fernandez-Sarmiento J, Hernandez-Sarmiento R, Salazar MP, Barrera S, Castilla V, Duque C. The association between hypoalbuminemia and microcirculation, endothelium, and glycocalyx disorders in children with sepsis. Microcirculation. (2023) 30:e12829. doi: 10.1111/micc.12829
25. Liu R, Yu Z, Xiao C, Xu F, Xiao S, He J, et al. Epidemiology and clinical characteristics of pediatric sepsis in PICUs in Southwest China: a prospective multicenter study. Pediatr Crit Care Me. (2024) 25:425–33. doi: 10.1097/PCC.0000000000003450
26. Sun M, Chen Y, Jin Z, Yang B, Zhu M. Causal association between medication use and sepsis: a two-sample Mendelian randomization study. Shock. (2025) 64(1):47–55. doi: 10.1097/SHK.0000000000002582
27. Van Nynatten LR, Patel MA, Daley M, Miller MR, Cepinskas G, Slessarev M, et al. Putative biomarkers of hepatic dysfunction in critically ill sepsis patients. Clin Exp Med. (2025) 25:28. doi: 10.1007/s10238-024-01545-3
28. Fu S, Chen Z, Wu H. Association between CRP-albumin-lymphocyte (CALLY) index and asthma-COPD overlap: analysis of NHANES 2015–2018 data. Bmc Pulm Med. (2025) 25:257. doi: 10.1186/s12890-025-03705-x
29. Kortz TB, Holloway A, Agulnik A, He D, Rivera SG, Abbas Q, et al. Prevalence, aetiology, and hospital outcomes of paediatric acute critical illness in resource-constrained settings (global PARITY): a multicentre, international, point prevalence and prospective cohort study. Lancet Glob Health. (2025) 13:e212–21. doi: 10.1016/S2214-109X(24)00450-9
30. Pan Y, Liu Z, Tu R, Feng X, Yu F, Wei M, et al. The value of the CRP-albumin-lymphocyte index (CALLY index) as a prognostic biomarker in acute ischemic stroke. Sci Rep-UK. (2025) 15:13672. doi: 10.1038/s41598-025-97538-7
31. Heidarian M, Griffith TS, Badovinac VP. Sepsis-induced changes in differentiation, maintenance, and function of memory CD8T cell subsets. Front Immunol. (2023) 14:1130009. doi: 10.3389/fimmu.2023.1130009
32. Xu Z, Huang M. A dynamic nomogram for predicting 28-day mortality in septic shock: a Chinese retrospective cohort study. Peerj. (2024) 12:e16723. doi: 10.7717/peerj.16723
Keywords: children, sepsis, mortality risk factors, CALLY index, albumin
Citation: Wang C, Feng L, Yang X, Wang P and Chen Y (2025) Risk factors for mortality and development of a predictive model in pediatric sepsis. Front. Pediatr. 13:1661086. doi: 10.3389/fped.2025.1661086
Received: 7 July 2025; Accepted: 27 August 2025;
Published: 22 September 2025.
Edited by:
Ryan J. Stark, Vanderbilt University Medical Center, United StatesReviewed by:
Matthew Solomon, Vanderbilt University Medical Center, United StatesEbru Melek Benligül, Tınaztepe University, Türkiye
Copyright: © 2025 Wang, Feng, Yang, Wang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuan Chen, eXVhbmNoZW5AaGJtdS5lZHUuY24=
 Caizhen Wang
Caizhen Wang Lijie Feng
Lijie Feng